Abstract
Purpose
Severe acute respiratory syndrome coronavirus 2, which causes coronavirus disease 2019 (COVID-19), has spread worldwide. Global health systems, including emergency medical systems, are suffering from a lack of medical resources. Using a method for classifying patients visiting the emergency department (ED), we aimed to investigate trends in emergency medical system usage during the COVID-19 epidemic in Korea.
Materials and Methods
This retrospective observational study included patients who visited emergency medical institutions registered with the National Emergency Department Information System database from January 1, 2017 to May 31, 2020. The primary outcome was identification of changes in the distribution of patients visiting the ED according to the type of emergency medical institution. The secondary outcome was a detailed comparison of Korean Triage and Acuity Scale (KTAS) levels and patient distributions before and during the infectious disaster crisis period.
Results
Severe patients visited regional emergency centers (RECs) and local emergency centers (LECs) more frequently during the COVID-19 period, and disposition status warranting admission to the intensive care unit or resulting in death was more common in RECs and LECs during the COVID-19 period [RECs, before COVID-19: 300686 (6.3%), during COVID-19: 33548 (8.0%) (p<0.001); LECs, before COVID-19: 373593 (3.7%), during COVID-19: 38873 (4.5%) (p<0.001)].
Conclusion
During the COVID-19 period, severe patients were shifted to advanced emergency medical institutions, and the KTAS better reflected severe patients. Patient distribution according to the stage of emergency medical institution improved, and validation of the KTAS triage increased more in RECs.
Keywords: Coronavirus disease 2019, emergency medical system, emergency department
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2, which causes coronavirus disease 2019 (COVID-19), was first identified in Wuhan, China in December 2019 and has spread worldwide.1 Since the World Health Organization declared the COVID-19 outbreak in January 2020, 27 million cases and 900000 deaths have been confirmed worldwide as of September 2020, and the disease has had a direct impact on medical systems, in addition to social and economic consequences.2 Global health systems are suffering from a lack of negative-pressure isolation rooms and medical resources, difficulties in transporting patients using public medical ambulances, and other challenges.3 The disease has elicited overall changes in global health systems, including emergency medical systems.
In South Korea, confirmed cases began to emerge in January 2020. For the first 4 weeks after the initial patient, the disease spread slowly, and all confirmed COVID-19 patients were admitted to negative-pressure isolation rooms. However, the number of confirmed patients increased rapidly to approximately 5000 patients within the next 6 weeks, mainly in the Daegu and Gyeongbuk regions, and South Korea urgently required various changes due to the severe scarcity of medical resources triggered by the large number of confirmed patients. The Korea Centers for Disease Control and Prevention adjusted the infectious disease disaster crisis stage by raising it gradually to yellow-orange-red and also instituted social and behavior changes among the people, such as “social distancing.” Further, patients with respiratory symptoms and fever were asked to not visit the hospital immediately, but were subjected to follow-up symptom observation and COVID-19 testing after self-isolation.4 With emergency medical institutions conducting screening tests for COVID-19, patients suspected of COVID-19 were admitted to isolation rooms or transferred to specialized national medical institutions. As regional emergency centers (RECs) began to suffer from increasing overcrowding, patients with mild symptoms or tolerable conditions were advised to visit other lower-level medical institutions or were followed up at home with conservative care.
In 2004, the National Emergency Department Information System (NEDIS) was launched to identify and collect medical information of patients visiting emergency medical institutions in real time. Among the medical records collected, information gleaned from The Korean Triage and Acuity Scale (KTAS) was first introduced in 2017 to solve problems related with delays in the treatment of critical patients, overcrowding in the emergency department (ED), and the low reliability of the preexisting triage classification system for patients visiting the ED.5 The KTAS is a patient classification system that covers the prehospital to hospital stages and determines a patient's priority and urgency by applying the patient's chief complaint and condition according to signs and symptoms. The KTAS has been used as an indicator to monitor whether emergency systems are operating well, such as toxicology,6 trauma,7 pediatric patient,8 and cardiac arrest.9 This has been validated in many ways.10,11
In South Korea, emergency medical institutions are divided into three stages; however, ED visits entail a combination of mild and severe patients, regardless of the stage of the emergency institution. The present study was conducted to confirm the distribution of patients at the stage of the emergency institution comparing that before and during the COVID-19 period.
MATERIALS AND METHODS
Study designs
This retrospective observational study conducted included patients who visited emergency medical institutions registered with the NEDIS from January 1, 2017 to May 31, 2020. The reference time point was before and after January 28, 2020, when the infectious disease crisis stage was declared “orange.” Thereafter, local public health centers, local medical centers, and emergency medical centers were designated COVID-19 screening centers, and they began patient screening and recommending COVID-19 testing to symptomatic patients who had fever or respiratory symptoms rather than an immediate hospital visit.
The impact of COVID-19 on the emergency system was analyzed by comparing patient trends during the COVID-19 epidemic period (January 28, 2020 to May 2020) with that during the preceding period. In addition to the change in the number of patients, the distribution of KTAS levels was analyzed in terms of how the severity of the patients changed during the epidemic period, and disposition status at the ED was used to analyze patient outcome variables.
For this study, we extracted data from the NEDIS registry as of June 1, 2020 and obtained permission to use the data from the National Medical Center.
Patients and variables
Patients of all ages who visited local emergency institutions, local emergency centers (LECs), and RECs nationwide from January 2017, when the NEDIS began recording KTAS data, to May 31, 2020, were considered. Patients with errors in data collection were excluded. Data were extracted from the NEDIS, including age, sex, spectrum of disease (disease or non-disease), means of transportation, KTAS level, type of final treatment place at the ED (general emergency care area, general isolation area, or negative-pressure isolation area), stay time at ED, and disposition status at the ED. Cases involving errors in the data entry process were excluded. In terms of patient distribution, severe patients were defined as those admitted to the intensive care unit (ICU) or expired patients, whereas mild patients were defined as those discharged from the ED or those admitted to the general ward. Emergency medical institutions included the following: RECs, LECs, and local emergency departments (LEDs).
NEDIS database
Data were obtained from the NEDIS database, which has been administrated by the National Emergency Medical Center in South Korea from 2004 and is updated in real-time. The NEDIS is an emergency information network that includes clinical and administrative data for all patients who have visited EDs in 402 participating emergency medical institutions nationwide.12 NEDIS data include sex, age (age is grouped into 10-year categories), classification of emergency medical institution, type of patient insurance, symptom onset time, intentionality, spectrum of disease (disease or non-disease, such as trauma, hanging, and drug intoxication), trauma mechanism, means of transportation (direct visit to ED or transfer) chief complaint, level of consciousness at presentation, KTAS level (from 2017), type of final treatment place, time variables (visit, discharge, and admission), disposition status at the ED (ED discharge, admission to general ward, admission to ICU, death, or transfer to another hospital), and diagnosis at discharge.
Korean Triage and Acuity Scale
The KTAS was developed based on the Canadian Triage and Acuity Scale that has been used since 2012, and it has been applied nationwide since 2016. It is a system used to classify patients who visit the ED; it considers the first secondary steps implemented based on the patient's symptoms and applies the patient's urgency and priority in the ED. The system has been divided into five stages (levels I to V), and severity decreases as it goes up to level V, which reflects an almost mild patient.13 The KTAS was implemented by nationally certified professionals.
Outcomes
The primary outcome was identification of changes in the distribution of patients visiting the ED according to each stage of the emergency medical institution during the infectious disaster crisis period, compared with the preceding period, and the secondary outcome was a detailed comparison of KTAS levels and patient distribution between the pre-COVID-19 period and COVID-19 period, according to disposition status at the ED.
Ethics
This study protocol was approved by the Institutional Review Board of the National Medical Center (IRB No. NMC-2007-026), and the need for informed consent was waived because data were accumulated in an anonymized state, which did not include personal information. Furthermore, the study protocol was exempted from deliberation by the Ethics Committee.
Statistical analysis
The analysis included the following variables: age and sex, among the demographic and sociological variables, as well as means of transportation, spectrum of disease, initial KTAS level, type of final treatment place at the ED, disposition status at the ED, and stay time at the ED. The general characteristics of the patients are presented as medians (min-max) for continuous variables and frequencies (percentages) for categorical variables. The distribution of the data was verified using the Kolmogorov-Smirnov test. Differences between pre- and postspread of COVID-19 were assessed using the independent t test or Mann-Whitney U test for continuous variables and the chisquare test or Fisher's exact test for categorical variables. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA), and p values<0.05 were considered statistically significant.
RESULTS
Patient enrolment
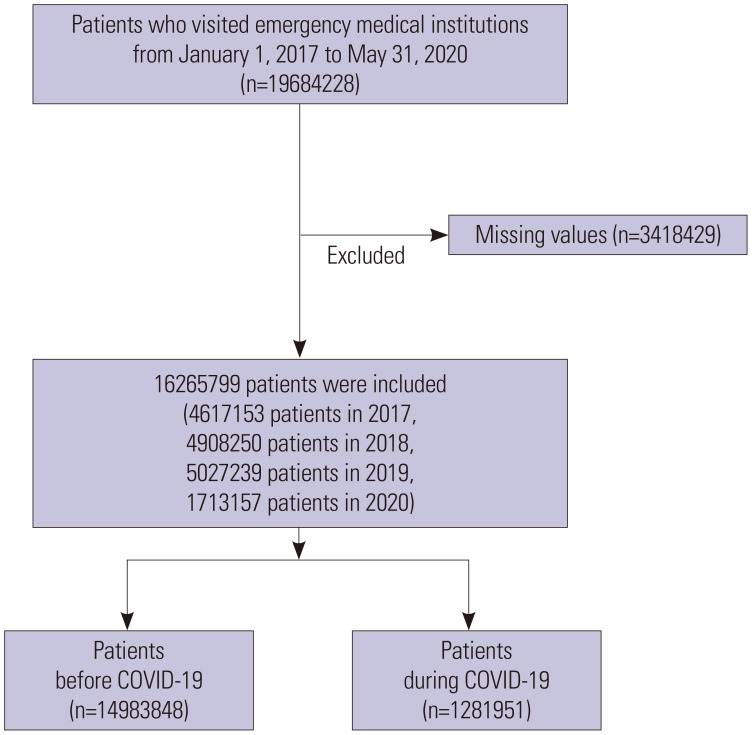
Of the 19684228 patients who visited emergency medical institutions from January 1, 2017, to May 31, 2020, a total of 16265799 patients, excluding 3418429 patients with missing values, were included. Of the included patients, 14983848 patients visited emergency medical institutions before the COVID-19 period, and 1281951 patients visited emergency medical institutions during the COVID-19 period (Fig. 1). There was no significant difference in the number and proportion of patients visiting RECs, LECs, and LEDs during each period.
Fig. 1. Flowchart of patients who visited emergency departments using NEDIS data before and during COVID-19. NEDIS, National Emergency Department Information System; COVID-19, coronavirus disease 2019.
General characteristics of the patients
Among the included patients, 50.3% patients were male, most patients were aged 50–59 years, and the number of patients aged <10 years of age was the least. Pre-COVID-19 patients with disease visited EDs 72.8% more than non-disease patients, and similarly, patients with disease visited more than those without during COVID-19. In terms of transportation, direct visits were the most frequent. In regards to KTAS level, level IV in the initial KTAS triage was the highest, both before and during COVID-19, followed by level III, and level I was the least. Regarding the type of final treatment place at the ED, most patients were finally treated in the general emergency care area; however, final treatment at general isolation and negative-pressure isolation areas increased significantly during the COVID-19 period. With respect to disposition status at the ED, most patients were discharged from the ED; however, during the COVID-19 period, ED discharge decreased to 71.2%, compared to that in the pre-COVID-19 period, and the ICU admission rate increased to 4.8%. In terms of patient distribution, severe patients conducted more visits during the COVID-19 period than before (Table 1).
Table 1. General Characteristics of Patients Who Visited Emergency Medical Institutions Before and During the COVID-19 Period.
| Variables | Total (n=16265799) | Before COVID-19 (01.01.2017–01.27.2020) (n=14983848) |
During COVID-19 (01.28.2020–05.31.2020) (n=1281951) |
p value | |
|---|---|---|---|---|---|
| Male sex (%) | 8196198 (50.3) | 7537132 (50.3) | 659066 (51.4) | <0.0001 | |
| Age (yr) | <0.0001 | ||||
| 0–9 | 481797 (3.0) | 460511 (3.1) | 21286 (1.7) | ||
| 10–19 | 1281734 (7.9) | 1208632 (8.1) | 73102 (5.7) | ||
| 20–29 | 2050473 (12.6) | 1879090 (12.6) | 171383 (13.3) | ||
| 30–39 | 2112667 (13.0) | 1951379 (13.0) | 161288 (12.6) | ||
| 40–49 | 2161683 (13.3) | 1994685 (13.3) | 166998 (13.0) | ||
| 50–59 | 2641801 (16.2) | 2434166 (16.3) | 207635 (16.2) | ||
| 60–69 | 2193109 (13.5) | 2005413 (13.4) | 187696 (14.6) | ||
| 70–79 | 1903824 (11.7) | 1744624 (11.6) | 159200 (12.4) | ||
| ≥80 | 1438711 (8.8) | 1305348 (8.7) | 133633 (10.4) | ||
| Spectrum of disease | <0.0001 | ||||
| Disease | 11842267(72.8) | 10896530 (72.7) | 945737 (73.7) | ||
| Non-disease | 4423532 (27.2) | 4087318 (27.2) | 336214 (26.2) | ||
| Means of transportation | <0.0001 | ||||
| Direct visit | 14457183 (88.8) | 13316329 (88.8) | 1137183 (88.7) | ||
| Transfer in | 1812287 (11.2) | 1667519 (11.1) | 144768 (11.3) | ||
| Initial KTAS triage level | <0.0001 | ||||
| I | 207076 (1.3) | 186775 (1.3) | 20301 (1.6) | ||
| II | 1041602 (6.4) | 960536 (6.4) | 81039 (6.3) | ||
| III | 6035125 (37.1) | 5531101 (36.9) | 504024 (39.3) | ||
| IV | 7348616 (45.2) | 6797600 (45.4) | 551016 (43.0) | ||
| V | 1633380 (10.0) | 1507809 (10.1) | 125571 (9.8) | ||
| Type of final treatment place at ED | <0.0001 | ||||
| General emergency care area | 16065568 (98.8) | 14845002 (99.1) | 1220566 (95.2) | ||
| General isolation area | 142423 (0.9) | 110682 (0.7) | 31741 (2.5) | ||
| Negative-pressure isolation area | 57808 (0.4) | 28164 (0.2) | 29644 (2.3) | ||
| Stay time at ED according to KTAS level | |||||
| Median (Q1, Q3) | |||||
| I | 320 (133, 759) | 132 (53, 314) | 148 (59, 391) | <0.0001 | |
| II | 223 (123, 424) | 222 (123, 423) | 231 (127, 436) | <0.0001 | |
| III | 174 (108, 299) | 173 (108, 297) | 182 (110, 322) | <0.0001 | |
| IV | 105 (55, 178) | 105 (55, 178) | 102 (52, 178) | <0.0001 | |
| V | 57 (22, 118) | 57 (22, 115) | 51 (20, 110) | <0.0001 | |
| Disposition status at ED | <0.0001 | ||||
| ED discharge | 12017487 (73.9) | 11098669 (74.0) | 918818 (71.2) | ||
| Admission to general ward | 3191597 (19.6) | 2924559 (19.5) | 267038 (20.8) | ||
| Admission to intensive care unit | 644985 (4.0) | 583801 (3.9) | 61884 (4.8) | ||
| Transfer to other hospital | 307377 (1.9) | 283234 (1.9) | 24143 (1.9) | ||
| Expiry | 104353 (0.6) | 93585 (0.6) | 10768 (0.8) | ||
| Disposition status: admission to intensive care unit or expiry at ED | <0.0001 | ||||
| Yes | 749338 (4.6) | 677386 (4.5) | 71952 (5.6) | ||
| No | 15516461 (95.4) | 14306462 (95.5) | 129999 (94.4) | ||
COVID-19, coronavirus disease 2019; KTAS, Korean Triage and Acuity Scale; ED, emergency department.
% units are rounded up.
General characteristics of patients visiting regional emergency centers
Table 2 shows the general characteristics of the 5189878 patients who visited RECs, and their overall trends were similar to the general characteristics shown in Table 1. In both periods, more patients in the disease category visited an ED than those in the non-disease category, and disease patients visited more frequently during the COVID-19 period than before. At the initial KTAS triage, level III was the most common during both periods, and final patient treatment in general isolation and negative-pressure isolation areas increased during COVID-19. According to KTAS level, level II had the longest duration of stay at the ED, while level V had the shortest, and the time difference between the two periods was greatest at level I. ED discharge decreased and admission to ICU increased during COVID-19.
Table 2. General Characteristics of Patients Who Visited Regional Emergency Centers Before and During the COVID-19 Period.
| Variables | Total (n=5189878) | Before COVID-19 (01.01.2017–01.27.2020) (n=4771013) |
During COVID-19 (01.28.2020–05.31.2020) (n=418865) |
p value | |
|---|---|---|---|---|---|
| Male sex (%) | 2664169 (51.3) | 2444518 (51.2) | 219651 (52.4) | <0.0001 | |
| Age (yr) | <0.0001 | ||||
| 0–9 | 215436 (4.2) | 205462 (4.3) | 9974 (2.4) | ||
| 10–19 | 384066 (7.4) | 361664 (7.6) | 22402 (5.4) | ||
| 20–29 | 581878 (11.2) | 533107 (11.2) | 48771 (11.6) | ||
| 30–39 | 608275 (11.7) | 561028 (11.8) | 47247 (11.3) | ||
| 40–49 | 646881 (12.5) | 596554 (12.5) | 50327 (12.0) | ||
| 50–59 | 845033 (16.3) | 777401 (16.3) | 67632 (16.2) | ||
| 60–69 | 747672 (14.4) | 681396 (14.3) | 66276 (15.8) | ||
| 70–79 | 672233 (13.0) | 614162 (12.9) | 58071 (13.9) | ||
| ≥80 | 488404 (9.4) | 440239 (9.2) | 48165 (11.5) | ||
| Spectrum of disease | <0.0001 | ||||
| Disease | 3891302 (75.0) | 3572920 (74.9) | 318382 (76.0) | ||
| Non-disease | 1298576 (25.0) | 1198093 (25.1) | 100483 (24.0) | ||
| Means of transportation | 0.2376 | ||||
| Direct visit | 4331170 (83.5) | 3981882 (83.5) | 349288 (83.4) | ||
| Transfer in | 858708 (16.5) | 789131 (16.5) | 69577 (16.6) | ||
| Initial KTAS triage level | <0.0001 | ||||
| I | 90082 (1.7) | 81031 (1.7) | 9051 (2.2) | ||
| II | 464790 (9.0) | 427176 (9.0) | 37614 (9.0) | ||
| III | 2266959 (43.7) | 2070974 (43.4) | 195985 (46.8) | ||
| IV | 1974088 (38.0) | 1828794 (38.3) | 145294 (34.7) | ||
| V | 393959 (7.6) | 363038 (7.6) | 30921 (7.4) | ||
| Type of final treatment place at ED | <0.0001 | ||||
| General emergency care area | 5088000 (98.0) | 4693554 (98.4) | 394446 (94.2) | ||
| General isolation area | 81234 (1.6) | 66239 (1.4) | 14995 (3.6) | ||
| Negative-pressure isolation area | 20644 (0.4) | 11220 (0.2) | 9424 (2.3) | ||
| Stay time at ED according to KTAS level | |||||
| Median (Q1, Q3) | |||||
| I | 196 (84, 411) | 194 (84, 403) | 217 (88, 493) | <0.0001 | |
| II | 245 (141, 427) | 243 (141, 424) | 257 (147, 464) | <0.0001 | |
| III | 342 (207, 342) | 206 (131, 340) | 219 (136, 367) | <0.0001 | |
| IV | 123 (70, 373) | 123 (70, 212) | 126 (71, 218) | <0.0001 | |
| V | 72 (31, 140) | 72 (31, 141) | 67 (28, 135) | <0.0001 | |
| Disposition status at ED | <0.0001 | ||||
| ED discharge | 3602908 (69.4) | 3324972 (69.7) | 277936 (66.4) | ||
| Admission to general ward | 1152262 (22.2) | 1052890 (22.1) | 99372 (23.7) | ||
| Admission to intensive care unit | 298676 (5.8) | 269123 (5.6) | 29553 (7.1) | ||
| Transfer to other hospital | 100474 (1.9) | 92465 (1.9) | 8009 (1.9) | ||
| Expiry | 35558 (0.7) | 31563 (0.7) | 3995 (1.0) | ||
| Disposition status: admission to intensive care unit or expiry at ED | <0.0001 | ||||
| Yes | 334234 (6.4) | 300686 (6.3) | 33548 (8.0) | ||
| No | 4855644 (93.6) | 4470327 (93.7) | 385317 (92.0) | ||
COVID-19, coronavirus disease 2019; KTAS, Korean Triage and Acuity Scale; ED, emergency department.
Statistical analysis between emergency medical institutions before and during COVID-19
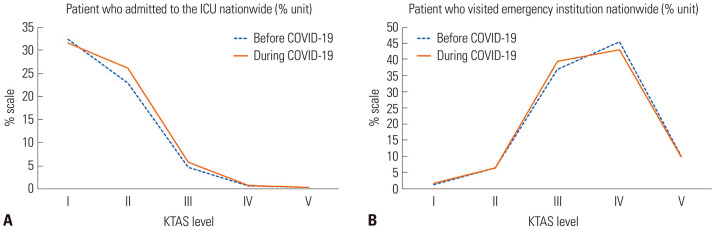
Comparing emergency medical institutions, we noted that LECs were most commonly visited during both periods (67.4% before COVID-19 and 70% during COVID-19). In regards to the initial KTAS triage, level III was the most common at RECs (43.4% before COVID-19 and 46.8% during COVID-19), and level IV was the most common at LECs during both periods (48.8% before COVID-19 and 47.1% during COVID-19). However, at LEDs, level IV was the most common before COVID-19, whereas level III was the most common during the COVID-19 period. In terms of disposition status at the ED, ED discharge was the most common during both periods, followed by admission to the general ward and then to the ICU. The proportion of patients admitted to the ICU increased at RECs and LECs during COVID-19, and the gap between KTAS levels III and IV at RECs was wider (Table 3 and Fig. 2).
Table 3. Statistical Analysis Comparing Emergency Medical Institutions Before and During the COVID-19 Period.
| Variables | Before COVID-19 (01.01.2017–01.27.2020) | During COVID-19 (01.28.2020–05.31.2020) | p value | |||||
|---|---|---|---|---|---|---|---|---|
| REC | LEC | LED | REC | LEC | LED | |||
| Patient visit | 4771013 (31.8) | 10964832(67.4) | 106715(0.8) | 418865(32.7) | 858712 (70) | 4374(0.3) | <0.001 | |
| Male sex (%) | 244518 (51.2) | 5018991 (49.7) | 73623 (70) | 219651 (52.4) | 436810 (50.9) | 2605 (59.6) | <0.001 | |
| Initial KTAS triage level | <0.001 | |||||||
| I | 81031(1.7) | 104800 (1.0) | 944 (0.9) | 9051 (2.2) | 11246 (1.3) | 4 (0.1) | ||
| II | 427176 (9.0) | 495341 (4.9) | 38046 (35.7) | 37614 (9.0) | 43388 (5.0) | 37 (0.9) | ||
| III | 2070674 (43.4) | 3444144 (34.1) | 15983 (15.0) | 195985 (46.8) | 306062 (35.6) | 1977 (45.2) | ||
| IV | 1828794 (38.3) | 4927306 (48.8) | 41500 (38.9) | 145294 (34.7) | 404774 (47.1) | 948 (21.7) | ||
| V | 363038 (7.6) | 1134529 (11.2) | 10242 (9.6) | 30921 (7.4) | 93242 (10.9) | 1408 (32.2) | ||
| Disposition status at ED | <0.001 | |||||||
| ED discharge | 3324972 (69.7) | 7716629 (76.4) | 57068 (53.5) | 277936 (66.4) | 936800 (74.2) | 4082 (93.3) | ||
| Admission to general ward | 1052890 (22.0) | 1826172 (18.1) | 45497 (42.6) | 99372 (23.7) | 164726 (19.5) | 240 (5.5) | ||
| Admission to intensive care unit | 269123 (5.6) | 312282 (3.1) | 2396 (2.3) | 29553 (7.1) | 31603 (3.7) | 28 (0.6) | ||
| Transfer to other hospital | 92465 (1.9) | 189726 (1.9) | 1043 (1.0) | 8009 (1.9) | 16113 (1.9) | 21 (0.5) | ||
| Expiry | 31563 (0.7) | 61311 (0.6) | 711 (0.7) | 3995 (1.0) | 6770 (0.8) | 3 (0.1) | ||
| Disposition status: admission to intensive care unit or expiry at ED | <0.001 | |||||||
| Yes | 300686 (6.3) | 373593 (3.7) | 3107 (2.9) | 33548 (8.0) | 38873 (4.5) | 31 (0.7) | ||
| No | 4470327 (93.7) | 9732527 (96.3) | 103608 (97.1) | 385317 (92.0) | 820339 (95.5) | 4343 (99.3) | ||
COVID-19, coronavirus disease 2019; REC, regional emergency center; LEC, local emergency center; LED, local emergency department, KTAS, Korean Triage and Acuity Scale; ED, emergency department.
% units are rounded up.
Fig. 2. Before- and during-COVID-19 comparison of (A) the number of patients visiting emergency institutions and (B) the number of patients admitted to the ICU at regional emergency centers. COVID-19, coronavirus disease 2019; ICU, intensive care unit.
Comparison of the emergency medical institutions, initial KTAS triage levels, and disposition status at the ED before and during COVID-19 in a regional emergency center
KTAS level III was the most common during both periods (43.4% before COVID-19 and 46.8% during COVID-19), followed by level IV (38.3% before COVID-19 and 34.7% during COVID-19). From levels I to V, ED discharge increased, and ICU admission rate decreased during both periods (Table 4).
Table 4. Statistical Analysis Comparing KTAS Level and Disposition Status at Regional Emergency Centers Before and During the COVID-19 Period.
| Variables | Before COVID-19 (01.01.2017–01.27.2020) | During COVID-19 (01.28.2020 –05.31.2020) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| KTAS level | I | II | III | IV | V | I | II | III | IV | V | |
| Patient | 81031 (1.7) | 427176 (9.0) | 2070974 (43.4) | 1828794 (38.3) | 363038 (7.6) | 9051 (2.2) | 37614 (9.0) | 195985 (46.8) | 145294 (34.7) | 30921 (7.4) | |
| Disposition status at ED | |||||||||||
| ED discharge | 6411 (7.9) | 160857 (37.7) | 1259847 (60.8) | 1559246 (85.3) | 338611 (93.3) | 586 (6.5) | 12940 (34.4) | 111896 (57.1) | 123539 (85.0) | 28975 (93.7) | |
| Admission to general ward | 12287 (15.2) | 132914 (31.1) | 649559 (31.4) | 236263 (12.9) | 21867 (6.0) | 1342 (14.8) | 11700 (31.1) | 65563 (33.5) | 19031 (13.1) | 1736 (5.6) | |
| Admission to intensive care unit | 33301 (41.1) | 111837 (26.2) | 110973 (5.4) | 11913 (0.7) | 1099 (0.3) | 3563 (39.4) | 11080 (29.5) | 13695 (7.0) | 1130 (0.8) | 85 (0.3) | |
| Transfer to other hospital | 3811 (4.7) | 17600 (4.1) | 48446 (2.3) | 21178 (1.2) | 1430 (0.4) | 398 (4.4) | 1402 (3.7) | 4517 (2.3) | 1576 (1.1) | 116 (0.4) | |
| Expiry | 25221 (31.1) | 3968 (0.9) | 2149 (0.1) | 194 (0.0) | 31 (0.0) | 3162 (34.9) | 492 (1.3) | 314 (0.2) | 18 (0.0) | 9 (0.0) | |
| Stay time at ED | 194 (84, 403) | 243 (141, 424) | 206 (131, 340) | 123 (70, 212) | 72 (31, 141) | 217 (88, 493) | 257 (147, 464) | 219 (136, 367) | 126 (71, 218) | 67 (28, 135) | |
| Disposition status: admission to intensive care unit or expiry at ED | |||||||||||
| Yes | 58522 (72.2) | 115805 (27.1) | 113122 (5.5) | 12107 (0.7) | 1130 (0.3) | 6725 (74.3) | 11572 (30.8) | 14009 (7.2) | 1148 (0.8) | 94 (0.3) | |
| No | 22509 (27.8) | 311371 (72.9) | 1957852 (94.5) | 1816687 (99.3) | 361908 (99.7) | 2326 (25.7) | 26042 (69.2) | 181976 (92.9) | 144146 (99.2) | 30827 (99.7) | |
COVID-19, coronavirus disease 2019; KTAS, Korean Triage and Acuity Scale; ED, emergency department.
% units are rounded. Differences before and after spread of COVID-19 for categorical variables according to KTAS level were assessed using the chi-square test. Differences by KTAS level for the “Disposition status at ED” variable were statistically significant (p<.001). Differences by KTAS level for the “Disposition status: admission to intensive care unit or expiry at ED” variable were statistically significant (p<0.001), except “KTAS Level V” (p=0.8257). Differences between before and after spread of COVID-19 for the “Stay time at ED” variable according to KTAS level were assessed using the independent t-test and each difference by KTAS level was statistically significant (p<0.001).
DISCUSSION
This study is the first to identify changes in emergency medical systems in Korea using NEDIS data during the COVID-19 period. The number of patients visiting an ED decreased during the COVID-19 period, and patient dispersion according to the staged severity in each emergency medical institution was better distributed during the COVID-19 period. During the COVID-19 period, KTAS levels I, II, and III at the initial triage increased at RECs. Furthermore, the number of severe patients decreased, whereas the number of mild patients increased at LEDs, resulting in improved patient distribution across the stages of emergency medical institutions. Validation of the KTAS increased due to the high rate of admission to the ICU of patients with levels I, II, and III.
During the COVID-19 period, the proportion of patients with KTAS levels IV and V decreased, the proportion of pediatric patients decreased, and the proportion of older adult patients increased. Comparing emergency medical institutions, we noted that fewer patients visiting LEDs presented with KTAS levels I and II and more had levels III, IV, and V, whereas patients visiting RECs showed an increased tendency towards KTAS levels I, II, and III. Overcrowding in the ED due to an increase in mild patients visiting RECs has been a matter of concern,14 and it was not been well resolved, with difficulties arising due to various factors.15 In 2015, even during the Middle East respiratory syndrome outbreak, the proportion of patients who visited the emergency room decreased, and low-acuity diseases decreased more sharply.16 This trend seems to be more pronounced during the COVID-19 period. Furthermore, in a comparison of KTAS level and disposition status at the ED, the proportion of severe patients before COVID-19 increased during the COVID-19 period at KTAS levels I to V, and the KTAS reflected the severity of the patients well during COVID-19. These results effectively revealed the reinforcement of the staged role of the emergency medical system and the validity of the KTAS.
In a comparison of disposition status at the ED among emergency medical institutions, the hospitalization rate in general wards and ICUs at LEDs decreased, and in RECs, admission to the ICU increased and ED discharge decreased. In regards to patients discharged at the ED after examination without hospitalization, the number of mild patients increased at LEDs, and the number of severe patients showed centralization at RECs due to the increasing number of patients admitted to the ICU.
The use of negative-pressure isolation and general isolation rooms increased and stay time at the ED increased at KTAS levels I–III. Stay time at the ED increased more in RECs during the COVID-19 period. As COVID-19 is a nosocomial transmission virus, the use of isolation rooms has increased because it is recommended to use an isolation room during the diagnosis process.17 The stay time at the ED was prolonged as time was required for the COVID-19 diagnostic results to be reported, and it is presumed that the prolonged stay time at the ED is because ED isolation rooms have predominantly been built at RECs.
This is the first study of the impact of COVID-19 on emergency medical systems in South Korea, and similar studies in foreign countries are limited. In the United States, the number of patients visiting the ED decreased by 43% during COVID-19, compared to that before COVID-19, and it decreased more among women and children. The proportion of infectious disease-related visits was much higher during the early pandemic period.18 In Venice, Italy, where a nationwide lockdown strategy was implemented to prevent the spread of COVID-19, the number of patients visiting the ED decreased by 50%, and the rate of major trauma decreased due to lockdown.19 In Osaka, Japan, the number of patients visiting the ED also decreased, and the proportion of patients facing difficulty in hospital acceptance increased.3 Our study is meaningful because it is based on the NEDIS, which is highly reliable as it is mandatory for all emergency medical institutions to participate in it.
This study has some limitations. First, this study analyzed retrospective data and had limitations in data interpretation, although it was a large-population, nationwide study. Second, the regional gap according to the number of confirmed patients and differences between regional emergency medical institutions were not reflected. Third, this study shows that emergency medical care systems are shifting toward the proper direction due to COVID-19; however, it has failed to propose changes that would be appropriate in post-COVID situations. Further well-designed research and discussion are imperative.
During the COVID-19 period, severe patients were shifted to advanced emergency medical institutions, and the KTAS better reflected severe patients. Patient distribution to appropriate emergency medical institutions improved, supporting the validity of KTAS triage.
ACKNOWLEDGEMENTS
This study was supported from the National Medical Center. NEDIS data are administrated by the National Medical Center, and financial support was provided by the Ministry of Health and Welfare.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Oh Hyun Kim and Hyun Kim.
- Data curation: Yu Hyun Park.
- Formal analysis: Yu Hyun Park and Chan Young Kang.
- Funding acquisition: Young Sun Ro.
- Investigation: Young Sun Ro.
- Methodology: Sun Ju Kim.
- Project administration: Sun Ju Kim, Oh Hyun Kim, and Young Sun Ro.
- Resources: Hyun Kim and Young Sun Ro.
- Software: Chan Young Kang.
- Supervision: Oh Hyun Kim.
- Validation: Young Sun Ro.
- Visualization: Sun Ju Kim, Hyun Kim, Oh Hyun Kim, and Young Sun Ro.
- Writing—original draft: Sun Ju Kim.
- Writing—review & editing: Sun Ju Kim, Hyun Kim, Oh Hyun Kim, and Young Sun Ro.
- Approval of final manuscript: all authors.
References
- 1.Lai CC, Wang CY, Wang YH, Hsueh SC, Ko WC, Hsueh PR. Global epidemiology of coronavirus disease 2019 (COVID-19): disease incidence, daily cumulative index, mortality, and their association with country healthcare resources and economic status. Int J Antimicrob Agents. 2020;55:105946. doi: 10.1016/j.ijantimicag.2020.105946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus disease (COVID-2019) situation report. 2020. [accessed on 2020 September 13]. Available at: https://covid19.who.int/
- 3.Katayama Y, Kiyohara K, Kitamura T, Hayashida S, Shimazu T. Influence of the COVID-19 pandemic on an emergency medical service system: a population-based, descriptive study in Osaka, Japan. Acute Med Surg. 2020;7:e534. doi: 10.1002/ams2.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Korea Centers for Disease control and Prevention. Coronavirus disease-19 main website. 2020. [accessed on 2020 September 13]. Available at: http://ncov.mohw.go.kr/en.
- 5.NEDIS. National Emergency Department Information System data. [cited 2020 September 13]. Available from: https://www.egen.or.kr/nemc/business_building_system.do.
- 6.Yoon YH, Kim JY, Choi SH. Analysis of patients with acute toxic exposure between 2009 and 2013: data from the Korea Health Insurance Review and Assessment Service and the National Emergency Department Information System. J Korean Med Sci. 2018;33:e254. doi: 10.3346/jkms.2018.33.e254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jung K, Kim I, Park SK, Cho H, Park CY, Yun JH, et al. Preventable trauma death rate after establishing a national trauma system in Korea. J Korean Med Sci. 2019;34:e65. doi: 10.3346/jkms.2019.34.e65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee B, Chang I, Kim DK, Park JD Korean Society of Pediatric Emergency Medicine. Factors associated with triage modifications using vital signs in pediatric triage: a nationwide cross-sectional study in Korea. J Korean Med Sci. 2020;35:e102. doi: 10.3346/jkms.2020.35.e102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang HJ, Kim GW, Kim H, Cho JS, Rho TH, Yoon HD, et al. Epidemiology and outcomes in out-of-hospital cardiac arrest: a report from the NEDIS-based cardiac arrest registry in Korea. J Korean Med Sci. 2015;30:95–103. doi: 10.3346/jkms.2015.30.1.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park JB, Lee J, Kim YJ, Lee JH, Lim TH. Reliability of Korean Triage and Acuity Scale: interrater agreement between two experienced nurses by real-time triage and analysis of influencing factors to disagreement of triage levels. J Korean Med Sci. 2019;34:e189. doi: 10.3346/jkms.2019.34.e189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi SW, Ko T, Hong KJ, Kim KH. Machine learning-based prediction of Korean triage and acuity scale level in emergency department patients. Healthc Inform Res. 2019;25:305–312. doi: 10.4258/hir.2019.25.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cha WC, Ahn KO, Shin SD, Park JH, Cho JS. Emergency department crowding disparity: a nationwide cross-sectional study. J Korean Med Sci. 2016;31:1331–1336. doi: 10.3346/jkms.2016.31.8.1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park JB, Lim T. Korean triage and acuity scale (KTAS) J Korean Soc Emerg Med. 2017;28:547–551. [Google Scholar]
- 14.Shin SD, Jo YH, Cheon SB, Jung SK, Kwak YH, Rhee JE, et al. Effect of emergency department overcrowding on the outcome of patient care: a pilot study. J Korean Soc Emerg Med. 2004;15:1–7. [Google Scholar]
- 15.Yarmohammadian MH, Rezaei F, Haghshenas A, Tavakoli N. Overcrowding in emergency departments: a review of strategies to decrease future challenges. J Res Med Sci. 2017;22:23. doi: 10.4103/1735-1995.200277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee SY, Khang YH, Lim HK. Impact of the 2015 Middle East respiratory syndrome outbreak on emergency care utilization and mortality in South Korea. Yonsei Med J. 2019;60:796–803. doi: 10.3349/ymj.2019.60.8.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lynch JB, Davitkov P, Anderson DJ, Bhimraj A, Cheng VC, Guzman-Cottrill J, et al. Infectious Diseases Society of America Guidelines on infection prevention for health care personnel caring for patients with suspected or known COVID-19. Clin Infect Dis; 2020. Jul 27, [Epub] Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, et al. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stella F, Alexopoulos C, Scquizzato T, Zorzi A. Impact of the COVID-19 outbreak on emergency medical system missions and emergency department visits in the Venice area. Eur J Emerg Med. 2020;27:298–300. doi: 10.1097/MEJ.0000000000000724. [DOI] [PubMed] [Google Scholar]