Abstract
Purpose
We aimed to investigate the association between daily sunlight exposure duration and fractures in older Korean adults with osteoporosis.
Materials and Methods
We utilized data from the 2008–2011 Korea National Health and Nutrition Examination Survey. Osteoporosis was diagnosed based on a T-score of ≤−2.5 using dual energy X-ray absorptiometry. The duration of daily sunlight exposure and fracture were assessed via intensive health interviews by trained staff using standardized health questionnaires. Fracture was defined as one or more fractures of the femur, wrist, and spine.
Results
A total of 638 patients with osteoporosis aged ≥65 years were included. The odds ratio (OR) of total fractures was 0.55 times lower in the group with ≥5 h of daily sunlight exposure than in the group with <5 h of exposure after adjusting for age, sex, family history of osteoporosis or fracture, body mass index, bone mineral density of the femoral neck, serum 25-hydroxyvitamin D, current smoking, alcohol intake, daily calcium intake, and physical activity [95% confidence interval (CI) 0.31–0.97, p=0.040]. In patients with vitamin D insufficiency, the OR of total fracture was 0.52 times lower in the group with ≥5 h of daily sunlight exposure than in the group with less exposure after adjusting the above variables (95% CI 0.28–0.97, p=0.041).
Conclusion
Sunlight exposure for ≥5 h a day was significantly associated with a decreased OR of fracture in older Korean adults with osteoporosis. This association was also significant in patients with vitamin D insufficiency.
Keywords: Sunlight exposure, fracture, osteoporosis, serum vitamin D insufficiency
INTRODUCTION
Osteoporosis is a major public health problem worldwide and a socioeconomic burden.1,2 It is characterized by low bone mineral density and is associated with an increased risk of low-trauma fractures.3 Osteoporotic fractures increase disability and mortality in older people and decrease quality of life.2 Therefore, risk factor identification to reduce fracture incidence is essential for the implementation of preventive measures.4
Protective relationships between hip fracture outcomes and self-reported lifetime sun exposure in older adults have been investigated. In previous studies, sun exposure was classified into 6-point scales (0–5; never, seldom, now and then, regularly, often, very often) according to sunlight exposure degree, and hip fracture risk decreased dose dependently.5,6 One study found a statistically significant correlation between hip fracture incidence, ultraviolet (UV) radiation, and latitude in older adults. The risk of hip fracture in North Sweden was higher than that in South Sweden, suggesting that environmental factors have a protective effect.7 Accordingly, we focused on the effect of sunlight exposure on overall fractures, including hip fracture.
Cumulative UV radiation exposure is an important determinant for skeletal health.8 Studies have suggested that UV radiation is one of the few environmental exposures that can protect against hip fracture.4 Sun exposure is recommended for bone health; however, to the best our knowledge, the quantification of sunlight exposure time has not been investigated in patients with osteoporosis. Therefore, in this study, we aimed to investigate the association between daily sunlight exposure duration and fracture in older Korean adults with osteoporosis using data from the Korea National Health and Nutrition Examination Survey (KNHANES). Furthermore, we aimed to further investigate the association based on serum 25-hydroxyvitamin D levels.
MATERIALS AND METHODS
Study population
This cross-sectional study utilized data from the 2008–2011 KNHANES. The KNHANES is a nationwide population-based, cross sectional health examination and survey annually conducted by the Korean Ministry of Health and Welfare and the Division of Chronic Disease Surveillance of the Korean Centers for Disease Control and Prevention.
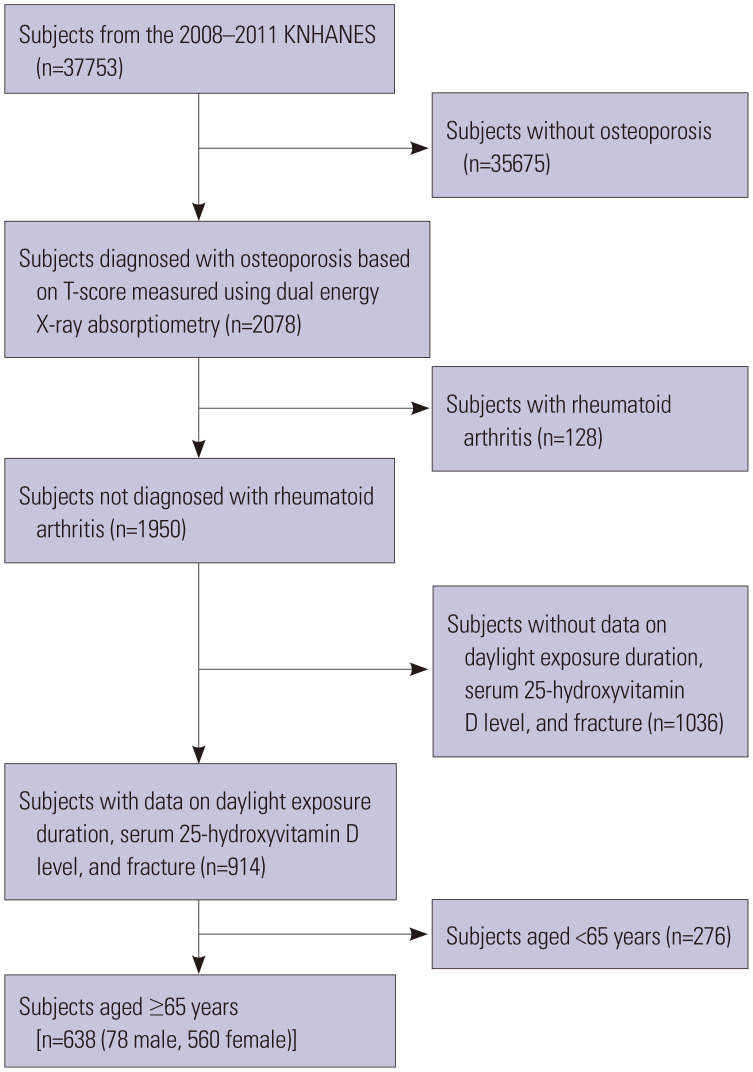
Among the 37753 subjects of the 2008–2011 KNHANES, 2078 patients were diagnosed with osteoporosis using dual-energy X-ray absorptiometry. Of these, 128 patients with physician-diagnosed rheumatoid arthritis, a cause of secondary osteoporosis and a risk factor for fracture,1 were excluded. From the remaining 1950 patients, those without data on daily sunlight exposure duration, fracture, or serum 25-hydroxyvitamin levels were further excluded. Finally, 638 subjects aged ≥65 years were included in the analysis (Fig. 1).
Fig. 1. Flow diagram of the selection of study subjects. KNHANES, Korea National Health and Nutrition Examination Survey.
All participants provided written informed consent before participation in the study, and the KNHANES was conducted following ethical approval by the Institutional Review Board of the Korea Centers for Disease Control and Prevention (No. 2008-04EXP-01-C, 2009-01CON-03-2C, 2010-02CON-21-C, and 2011-02CON-06C). The protocol of this study was approved by the Institutional Review Board of Yonsei University, Seoul, Korea (No. 4-2020-0267).
Data collection
In our study, variables used in the Fracture Risk Assessment Tool for evaluating the 10-year fracture probability developed by the World Health Organization9 were considered when adjusting the risk factors, and the value was calculated.
Subjects were interviewed by trained staff using standardized health questionnaires, which included questions on demographic information, medical history, parental history of osteoporosis diagnosis or fracture, history of smoking and alcohol intake, and daily sunlight exposure duration. In regards to femur, wrist, and spine fractures, the questionnaire was designed to collect information on whether or not the patient had ever been diagnosed with these fractures. Subjects with one or more fractures of the femur, wrist, and spine were classified into the fracture group. Bone mineral density of the total femur, femoral neck, and spine was examined using dual-energy X-ray absorptiometry in postmenopausal female and male aged ≥50 years. Osteoporosis was diagnosed based on a T-score of ≤−2.5. The bone mineral density of the femoral neck was also included in the analysis.
Daily sunlight exposure duration was assessed using surveys and categorized as <5 h or ≥5 h. A questionnaire was surveyed on the average of the time spent directly being exposed to the sun without wearing sunglasses or a hat during the day after 19 years of age. Body mass index (BMI) was calculated by dividing weight (kg) by the square of height (m2). Current smoking was defined as lifetime consumption of more than five packs of cigarettes (100 cigarettes) and still smoking cigarettes. Monthly alcohol intake was defined as drinking more than once a month during the past year. Physical activity was defined as engaging in moderate or vigorous exercise on a regular basis (≥20 min at a time, at least 3 times per week).10 Daily calcium intake was calculated from all foods consumed during the day through a 24-hour recall survey. Serum 25-hydroxyvitamin D levels were measured with a radioimmunoassay kit (DiaSorin Inc., Stillwater, MN, USA) using a gamma counter (1470 WIZARD; PerkinElmer Inc., Waltham, MA, USA). The 25-hydroxyvitamin D level for effective fracture prevention and preservation of bone mineral density is over 75 nmol/L.11 Therefore, our study used 75 nmol/L as the criterion for assessing vitamin deficiency.
Statistical analysis
The KNHANES uses a stratified, multistage, clustered probability sampling method for selection a representative sample of the non-institutionalized, civilian Korean population. Therefore, the statistical analyses in this study were conducted by adopting stratification, clustering, and weight variables.
The characteristics of the subjects classified according to the presence of total fracture and subtype (femur, wrist, spine) are expressed as means and standard deviations for continuous variables and as numbers and percentages for categorical variables. An independent t-test was used to compare the continuous variables and a chi-squared test for categorical variables. Differences between subjects with ≥5 h and <5 h daily sunlight exposure were evaluated using a chi-squared test based on the presence of total fracture.
Multivariate logistic regression analysis was performed to analyze the association between daily sunlight exposure duration and the odds ratio (OR) of total fracture. Relative risks were estimated in terms of ORs and 95% confidence intervals (CIs). We adjusted for multiple variables that showed significant associations in the univariate analysis and those based on clinical relevance. After calculating crude ORs (model 1), model 2 was adjusted for age, sex, parental history of osteoporosis diagnosis or fracture, bone mineral density of the femoral neck, serum 25-hydroxyvitamin D level, and BMI. Model 3 was further adjusted for current smoking, alcohol intake, daily calcium intake, and physical activity. All logistic regression analysis variables were examined for multicollinearity, and only those variables with a variance inflation factor <5 were used. All statistical analyses were performed using IBM SPSS version 25 (IBM Corp., Armonk, NY, USA). The level of statistical significance was set at p<0.05, and p values were two-tailed.
RESULTS
Demographic characteristics of the subjects
A total of 638 subjects were included in this study (Fig. 1). Table 1 shows the demographic characteristics of the subjects according to total fracture. The prevalence rates of total fracture and non-fracture were 17.4% (n=111) and 82.6% (n=527), respectively.
Table 1. Demographic Characteristics according to Fracture in Older Korean Adults with Osteoporosis.
| Characteristic | Fracture | p value | ||
|---|---|---|---|---|
| No (n=527) | Yes (n=111) | |||
| Age (yr) | 72.50±0.28 | 74.47±0.58 | 0.003 | |
| Female | 459 (85.3) | 101 (89.1) | 0.365 | |
| BMI (kg/m2) | 23.30±0.18 | 23.10±0.35 | 0.610 | |
| BMD of the femoral neck (g/cm2) | 0.53±0.01 | 0.50±0.01 | 0.002 | |
| T-score of the femoral neck | −2.60±0.05 | −2.86±0.07 | 0.002 | |
| 25-hydroxyvitamin D (nmol/L) | 45.42±1.21 | 46.36±2.07 | 0.698 | |
| Daily calcium intake (mg) | 389.50±43.75 | 308.65±23.10 | 0.044 | |
| Osteoporosis diagnosis or parental history of fracture | 68 (12.6) | 15 (17.7) | 0.314 | |
| Current smoking | 0.019 | |||
| Yes | 47 (10.8) | 5 (3.5) | ||
| No | 476 (89.2) | 106 (96.5) | ||
| Monthly alcohol intake | 0.816 | |||
| Yes | 104 (18.4) | 18 (17.4) | ||
| No | 419 (81.6) | 93 (82.6) | ||
| Physical activity* | 0.002 | |||
| Yes | 250 (47.4) | 37 (27.7) | ||
| No | 273 (52.6) | 74 (72.3) | ||
| 10-year fracture probability (%)† | 3.39±0.08 | 5.71±0.25 | <0.001 | |
| Daily sunlight exposure | 0.030 | |||
| <5 h | 355 (72.3) | 87 (83.1) | ||
| ≥5 h | 172 (27.7) | 24 (16.9) | ||
BMI, body mass index; BMD, bone mineral density.
Data were obtained from the 2008–2011 Korean National Health and Nutrition Examination Survey. p values were calculated using an independent t-test or chi-squared test. Continuous variables are expressed as means and standard deviations, and categorical variables are expressed as unweighted numbers and percentages.
*Defined as engaging in moderate or vigorous exercise on a regular basis (≥20 min at a time, at least three times per week), †Calculated using the Fracture Risk Assessment Tool according to the World Health Organization.
Of all 638 patients, 560 were female; 78 were male; and 196 (31%) had ≥5 h of daily sunlight exposure. Those in the fracture group were older and had a higher 10-year fracture probability than those in the group without fracture. Bone mineral density and T-scores of the femoral neck, daily calcium intake, current smoking, and regular physical activity, as well as daily sunlight exposure duration, were lower in the fracture group (all p<0.05). No significant differences were found in sex, BMI, serum 25-hydroxyvitamin D levels, parental history of osteoporosis diagnosis or fracture, and alcohol intake between the two groups (all p>0.05).
Regarding subtype (femur, wrist, spine) of fractures, 14 patients were diagnosed with femoral fracture; 68, wrist fracture; and 41, spine fracture. Female sex was predominantly associated with wrist fracture, and in patients with spine fracture, alcohol intake was less prevalent (all p<0.05, data not shown).
Association between daily sunlight exposure duration and fracture and subtype (femur, wrist, spine) fractures
Table 2 shows the ORs and 95% CIs for fracture and fracture subtype (femur, wrist, spine) according to duration of daily sunlight exposure in 638 patients with osteoporosis aged ≥65 years. The model was adjusted for age, sex, parental history of osteoporosis diagnosis or fracture, bone mineral density of the femoral neck, BMI, serum 25-hydroxyvitamin D, current smoking, alcohol intake, physical activity, and daily calcium intake. The OR for fracture was 0.55 times lower in the group with ≥5 h of daily sunlight exposure than in the group with <5 h of exposure (95% CI 0.31–0.97 for model 3). Moreover, the OR for femoral fracture was 0.18 times lower in the group with ≥5 h of daily sunlight exposure than in the group with <5 h of exposure (95% CI 0.03–0.91 for model 2), although there was no significant association in the final model.
Table 2. Unadjusted and Adjusted ORs (95% CI) of Fracture and Fracture Subtype (Femur, Wrist, Spine) according to Daily Sunlight Exposure Duration in Older Korean Adults with Osteoporosis from the KNHANES 2008–2011.
| Multivariate model | Model 1 OR (95% CI) |
Model 2 OR (95% CI) |
Model 3 OR (95% CI) |
|
|---|---|---|---|---|
| Total fracture (n=111) | ||||
| Sunlight exposure <5 h | Reference | Reference | Reference | |
| Sunlight exposure ≥5 h | 0.53 (0.30–0.95) p=0.032 |
0.53 (0.29–0.97) p=0.039 |
0.55 (0.31–0.97) p=0.040 |
|
| Femoral fracture (n=14) | ||||
| Sunlight exposure <5 h | Reference | Reference | Reference | |
| Sunlight exposure ≥5 h | 0.20 (0.04–0.95) p=0.043 |
0.18 (0.03–0.91) p=0.038 |
0.21 (0.04–1.19) p=0.077 |
|
| Wrist fracture (n=68) | ||||
| Sunlight exposure <5 h | Reference | Reference | Reference | |
| Sunlight exposure ≥5 h | 0.60 (0.30–1.22) p=0.159 |
0.59 (0.28–1.22) p=0.152 |
0.49 (0.24–1.02) p=0.055 |
|
| Spine fracture (n=41) | ||||
| Sunlight exposure <5 h | Reference | Reference | Reference | |
| Sunlight exposure ≥5 h | 0.67 (0.28–1.63) p=0.374 |
0.75 (0.30–1.91) p=0.550 |
0.72 (0.26–1.98) p=0.523 |
|
OR, odds ratio; CI, confidence interval; KNHANES, Korean National Health and Nutrition Examination Survey.
Model 1 was crude. Model 2 was adjusted for age, sex, parental history of osteoporosis diagnosis or fracture, body mass index, bone mineral density of the femoral neck, and serum 25-hydroxyvitamin D. Model 3 was adjusted for current smoking, alcohol intake, daily calcium intake, and physical activity in addition to Model 2's variables.
Association between daily sunlight exposure duration and fracture based on serum 25-hydroxyvitamin D level
Table 3 shows the ORs and 95% CIs for fracture according to daily sunlight exposure duration and serum 25-hydroxyvitamin D level. Among the 638 subjects, 583 (91.38%) had vitamin D insufficiency. This model was also adjusted for age, sex, parental history of osteoporosis diagnosis or fracture, bone mineral density of the femoral neck, BMI, serum 25-hydroxyvitamin D, current smoking, alcohol intake, physical activity, and daily calcium intake.
Table 3. Unadjusted and Adjusted ORs (95% CI) of Total Fracture according to Daily Sunlight Exposure Duration and Serum 25-Hydroxyvitamin D Level in Older Korean Adults with Osteoporosis from the KNHANES 2008–2011.
| Multivariate model | Model 1 OR (95% CI) |
Model 2 OR (95% CI) |
Model 3 OR (95% CI) |
||
|---|---|---|---|---|---|
| Serum 25-hydroxyvitamin D <75 nmol/L | |||||
| Total fracture (n=102) | |||||
| Sunlight exposure <5 h | Reference | Reference | Reference | ||
| Sunlight exposure ≥5 h | 0.51 (0.27–0.94) p=0.031 |
0.51 (0.28–0.96) p=0.036 |
0.52 (0.28–0.97) p=0.041 |
||
| Serum 25-hydroxyvitamin D ≥75 nmol/L | |||||
| Total fracture (n=9) | |||||
| Sunlight exposure <5 h | Reference | Reference | Reference | ||
| Sunlight exposure ≥5 h | 0.68 (0.11–4.28) p=0.666 |
1.01 (0.15–6.69) p=0.991 |
0.98 (0.16–6.17) p=0.985 |
||
OR, odds ratio; CI, confidence interval; KNHANES, Korean National Health and Nutrition Examination Survey.
Model 1 was crude. Model 2 was adjusted for age, sex, parental history of osteoporosis diagnosis or fracture, body mass index, bone mineral density of the femoral neck, and serum 25-hydroxyvitamin D. Model 3 was adjusted for current smoking, alcohol intake, daily calcium intake, and physical activity in addition to Model 2's variables.
In patients with serum 25-hydroxyvitamin D <75 nmol/L, daily sunlight exposure was significantly associated with a reduction in the OR for fracture. The OR for fracture was 0.52 times lower in the group with ≥5 h of daily sunlight exposure than in the group with less exposure (95% CI 0.28–0.97 for model 3). However, in patients with serum 25-hydroxyvitamin D ≥75 nmol/L, daily sunlight exposure was not significantly associated with the OR for fracture. Since the number of patients with serum 25-hydroxyvitamin D ≥75 nmol/L was small in this study and vitamin D inadequacy is common among South Koreans,12 we changed the cutoff of vitamin D deficiency to 50 nmol/L according to another definition13 and reanalyzed. With a lower cutoff value of 50 nmol/L, in patients with serum 25-hydroxyvitamin D ≥50 nmol/L, daily sunlight exposure was significantly associated with a reduction in the OR for fracture. The OR for fracture was 0.45 times lower in the group with ≥5 h of daily sunlight exposure than in the group with less exposure (95% CI 0.22–0.94 for model 3) (Supplementary Table 1, only online).
DISCUSSION
This cross-sectional study of data from the 2008–2011 KNHANES showed that longer sunlight exposure of ≥5 h decreased the OR for fracture among older Korean adults with osteoporosis. Previous studies have reported that the incidence of distal forearm and hip fractures has seasonal variations that decrease in summer and increase in winter.14,15 However, to our knowledge, this study is the first to quantitatively investigate a direct association between sunlight exposure duration and fracture in older adults with osteoporosis.
A low level of vitamin D is known as a risk factor for fall16,17 and fracture,18,19 especially as a predictor of major osteoporotic fracture.20 Older people seldom stay outside in the sunshine and often lack sufficient vitamin D.21 In addition, the hydroxylation of vitamin D into active metabolites decreases with age.21 Vitamin D deficiency resulting from this ultimately leads to increase bone turnover and cortical bone loss.21 Vitamin D also helps neuromuscular function remain in an optimal state and increases balance and muscle strength and coordination.22 Along these pathways, vitamin D deficiency may contribute to the pathogenesis of fracture.21
However, despite there being a correlation between sunlight exposure duration and serum 25-hydroxyvitamin D levels, longer duration of daily sunlight exposure resulted in reduced fracture OR in subjects with serum 25-hydroxyvitamin D insufficiency in our study. We performed a mediation analysis23 of 25-hydroxyvitamin D levels that mediate the association of sunlight exposure and fracture, and the result was 3.41%. This implies that sunlight exposure may play a role in the prevention of fracture independent of serum 25-hydroxyvitamin D. A few studies support this finding.8,24 One study showed no correlation between UV index and serum 25-hydroxyvitamin D levels in older adults with hip fracture.24 Furthermore, sunlight exposure may have a direct effect on bone or bone metabolism apart from vitamin D synthesis. Research has indicated that cumulative increases in sun exposure, independent of vitamin D concentration, have a protective effect against fracture in older females8 and against osteoporotic fracture in older adults.5,6 In addition, a recent study suggested that decreased sunlight exposure during daytime negatively affects nocturnal melatonin peak.25 Melatonin influences bone metabolism by stimulating bone growth and inhibiting osteoclast activity,26 and one study reported that decreased serum melatonin levels are associated with increased bone loss in postmenopausal female.27 Although there are few data on sun exposure in terms of bone health,28 it needs further study because its biological mechanism of action about bone is still unknown.
One third of older adults in the community and 60% of older adults in long-term care experience a fall accident at least once a year.29 Of these, the greatest problem is hip fracture, which accounts for more than 20% of all orthopedic patients,30 and the morbidity, mortality and economic costs of hip fractures are high, particularly in older individuals.31 Research has shown that hip fracture is one of the most serious osteoporotic complications,4 and one study showed that female aged 65 years or older who had their first hip fracture event were four times more likely to undergo subsequent episodes, compared to the general population.32 Therefore, prevention of femoral fracture among fractures is important, which can be expected with greater sunlight exposure. In the present study, although it was not significant in the final model, the effect of daily sunlight exposure ≥5 h reduced the OR for fracture in older adults with osteoporosis by 82%, compared with daily sunlight exposure <5 h, and the prevention effect on femoral fracture was relatively higher.
This study had some limitations. First, this was a cross-sectional study. Thus, a causal relationship between daily sunlight exposure duration and fracture could not be assessed. Second, due to the small number of subjects in our study, there is a possibility of selection bias in selecting subjects. In addition, in the subgroup analysis according to the fracture type and serum 25-hydroxyvitamin D level, the sample size was further reduced. A prospective longitudinal study with a larger sample should be conducted to verify this relationship. Third, because sunlight exposure is a subjective variable in self-reported questionnaire, recall and reporting biases might have occurred. However, KNHANES survey interviews were conducted by well-trained staff to obtain consistent and reliable answers. Furthermore, a study reported that plasma 25-hydroxyvitamin D level reflects only recent sun exposure.33 However, a recent study has shown that one-time measurement of plasma 25-hydroxyvitamin D levels could reasonably reflect long-term vitamin D status and sun exposure.34 Therefore, our study is considered appropriate for the analysis of the association with fracture risk. Fourth, UV exposure and sunlight absorption can differ significantly depending on geographic location, time of season and day, race, occupation, outdoor activity, lifestyle factors, and sunscreen usage.4 In our study, we were unable to collect detailed information on the variables related to sun exposure because structured cross-sectional KNHANES data were used. Therefore, research should be conducted to minimize the effect of various ambient UV exposure levels. However, since the subjects of our study have similar conditions, such as skin types, race, latitude, climate, etc., factors that can affect UV exposure and sunlight absorption are considered relatively controlled. Fifth, the 5 hours we used as a cut-off for sunlight exposure duration in our study is a high value. In Western countries, the recommended daily sunlight exposure duration needed to maintain adequate stores of vitamin D is 15–30 min,35 and a study in South Asians living in the United Kingdom revealed that more than 90 min was required for raising vitamin D concentrations.36 However, 271.3 minutes of sun exposure at 15 o'clock in December were required for sufficient vitamin D3 synthesis in Naha, Japan, which is located at a similar latitude to South Korea (Naha: 26°12'N, 127°41'E, 27.5 m; South Korea: 35°95'N, 128°25'E).37 Considering this, it is reasonable to categorize the duration of exposure to sunlight as 5 hours. Moreover, data regarding the duration of exposure to sunlight in KNHANES were collected through health interviews by trained staff members as a categorical variable based on the cut-off of 5 hours of sun exposure per day. Since exposure to sunlight for 5 hours a day is unlikely to occur in everyday life, further studies using dose–response relations or continuous variables are needed. Sixth, previous history of fracture was not reflected in our study. Further study is necessary to consider prior history of fracture, as it can increase the risk of subsequent fracture. Seventh, the association of daily sunlight exposure duration and OR for fracture differed depending on the cutoff of vitamin D deficiency. Further prospective study with larger sample will be needed.
Nevertheless, this is the first study to quantitatively investigate associations between sunlight exposure duration and fracture in older adults with osteoporosis. By presenting environmental factors, we suggest sunlight exposure as a novel protective factor against fracture in older individuals with osteoporosis. We provide an important theoretical basis for various treatments and preventive approaches for fractures in these individuals. Increasing sunlight exposure in older adults with osteoporosis and vitamin D insufficiency would also likely prevent fractures. The implications of our findings could be further developed in future prospective and longitudinal studies.
In conclusion, this quantitative cross-sectional analysis of data from the 2008–2011 KNHANES revealed that the OR of fracture decreased with longer sunlight exposure in patients with osteoporosis aged ≥65 years. The OR of fracture was lowered by 0.55 times in the group with daily sunlight exposure of ≥5 h than in the group with less sunlight exposure (p=0.040). In addition, even if the serum 25-hydroxyvitamin D level was <75 nmol/L, the OR of fracture was lowered by 0.52 in patients exposed to sunlight for ≥5 h daily than in those exposed to sunlight for <5 h daily (p=0.041). Hence, increasing daily levels of sunlight exposure could be an early preventive strategy against fractures in older adults with osteoporosis.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: all authors.
- Data curation: Hye Jun Lee and Choon Ok Kim.
- Formal analysis: Hye Jun Lee.
- Investigation: Hye Jun Lee.
- Methodology: Hye Jun Lee and Choon Ok Kim.
- Project administration: Choon Ok Kim and Duk Chul Lee.
- Resources: Hye Jun Lee.
- Software: Hye Jun Lee.
- Supervision: Choon Ok Kim and Duk Chul Lee.
- Validation: Choon Ok Kim and Duk Chul Lee.
- Visualization: Hye Jun Lee.
- Writing—original draft: Hye Jun Lee.
- Writing—review & editing: Choon Ok Kim and Duk Chul Lee.
- Approval of final manuscript: all authors.
SUPPLEMENTARY MATERIAL
Unadjusted and Adjusted ORs (95% CI) of Total Fracture according to Daily Sunlight Exposure Duration and Serum 25-Hydroxyvitamin D Level in Korean Elderly with Osteoporosis from the KNHANES 2008–2011
References
- 1.World Health Organization. WHO technical report series 843. Geneva, Switzerland: World Health Organization; 1994. Assessment of fracture risk in screening for osteoporosis. [PubMed] [Google Scholar]
- 2.Cummings SR, Kelsey JL, Nevitt MC, O'Dowd KJ. Epidemiology of osteoporosis and osteoporotic fractures. Epidemiol Rev. 1985;7:178–208. doi: 10.1093/oxfordjournals.epirev.a036281. [DOI] [PubMed] [Google Scholar]
- 3.Srikanth V, Fryer J, Venn A, Blizzard L, Newman L, Cooley H, et al. The association between non-melanoma skin cancer and osteoporotic fractures--a population-based record linkage study. Osteoporos Int. 2007;18:687–692. doi: 10.1007/s00198-006-0303-y. [DOI] [PubMed] [Google Scholar]
- 4.Perroud HA, Dagatti MS, Amigot B, Levit GP, Tomat MF, Morosano ME, et al. The association between osteoporotic hip fractures and actinic lesions as a biomarker for cumulative sun exposure in older people-a retrospective case-control study in Argentina. J Bone Miner Metab. 2017;35:324–329. doi: 10.1007/s00774-016-0759-6. [DOI] [PubMed] [Google Scholar]
- 5.Johnell O, Gullberg B, Kanis JA, Allander E, Elffors L, Dequeker J, et al. Risk factors for hip fracture in European women: the MEDOS Study. Mediterranean Osteoporosis Study. J Bone Miner Res. 1995;10:1802–1815. doi: 10.1002/jbmr.5650101125. [DOI] [PubMed] [Google Scholar]
- 6.Kanis J, Johnell O, Gullberg B, Allander E, Elffors L, Ranstam J, et al. Risk factors for hip fracture in men from southern Europe: the MEDOS Study. Osteoporos Int. 1999;9:45–54. doi: 10.1007/s001980050115. [DOI] [PubMed] [Google Scholar]
- 7.Nilson F, Moniruzzaman S, Andersson R. A comparison of hip fracture incidence rates among elderly in Sweden by latitude and sunlight exposure. Scand J Public Health. 2014;42:201–206. doi: 10.1177/1403494813510794. [DOI] [PubMed] [Google Scholar]
- 8.Thompson MJW, Aitken DA, Otahal P, Cicolini J, Winzenberg TM, Jones G. The relationship between cumulative lifetime ultraviolet radiation exposure, bone mineral density, falls risk and fractures in older adults. Osteoporos Int. 2017;28:2061–2068. doi: 10.1007/s00198-017-4001-8. [DOI] [PubMed] [Google Scholar]
- 9.University of Sheffield, Centre for Metabolic Bone Diseases. FRAX Fracture Risk Assessment. [accessed on 2020 September 29]. Available at: https://www.sheffield.ac.uk/FRAX/
- 10.Lee YH, Kim JE, Roh YH, Choi HR, Rhee Y, Kang DR, et al. The combination of vitamin D deficiency and mild to moderate chronic kidney disease is associated with low bone mineral density and deteriorated femoral microarchitecture: Results from the KNHANES 2008-2011. J Clin Endocrinol Metab. 2014;99:3879–3888. doi: 10.1210/jc.2013-3764. [DOI] [PubMed] [Google Scholar]
- 11.Vieth R. What is the optimal vitamin D status for health. Prog Biophys Mol Biol. 2006;92:26–32. doi: 10.1016/j.pbiomolbio.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 12.Chung YS, Chung DJ, Kang MI, Kim IJ, Koh JM, Min YK, et al. Vitamin D repletion in Korean postmenopausal women with osteoporosis. Yonsei Med J. 2016;57:923–927. doi: 10.3349/ymj.2016.57.4.923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu X, Baylin A, Levy PD. Vitamin D deficiency and insufficiency among US adults: prevalence, predictors and clinical implications. Br J Nutr. 2018;119:928–936. doi: 10.1017/S0007114518000491. [DOI] [PubMed] [Google Scholar]
- 14.Jacobsen SJ, Sargent DJ, Atkinson EJ, O'Fallon WM, Melton LJ., 3rd Contribution of weather to the seasonality of distal forearm fractures: a population-based study in Rochester, Minnesota. Osteoporos Int. 1999;9:254–259. doi: 10.1007/s001980050145. [DOI] [PubMed] [Google Scholar]
- 15.Douglas S, Bunyan A, Chiu KH, Twaddle B, Maffulli N. Seasonal variation of hip fracture at three latitudes. Injury. 2000;31:11–19. doi: 10.1016/s0020-1383(99)00192-8. [DOI] [PubMed] [Google Scholar]
- 16.Semba RD, Garrett E, Johnson BA, Guralnik JM, Fried LP. Vitamin D deficiency among older women with and without disability. Am J Clin Nutr. 2000;72:1529–1534. doi: 10.1093/ajcn/72.6.1529. [DOI] [PubMed] [Google Scholar]
- 17.Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY, et al. Effect of vitamin D on falls: a metaanalysis. JAMA. 2004;291:1999–2006. doi: 10.1001/jama.291.16.1999. [DOI] [PubMed] [Google Scholar]
- 18.Michaëlsson K, Melhus H, Bellocco R, Wolk A. Dietary calcium and vitamin D intake in relation to osteoporotic fracture risk. Bone. 2003;32:694–703. doi: 10.1016/s8756-3282(03)00048-6. [DOI] [PubMed] [Google Scholar]
- 19.Woolf AD, Akesson K. Preventing fractures in elderly people. BMJ. 2003;327:89–95. doi: 10.1136/bmj.327.7406.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Looker AC. Serum 25-hydroxyvitamin D and risk of major osteoporotic fractures in older U.S. adults. J Bone Miner Res. 2013;28:997–1006. doi: 10.1002/jbmr.1828. [DOI] [PubMed] [Google Scholar]
- 21.Lips P, Netelenbos JC. Vitamin D deficiency and hip fracture. Tijdschr Gerontol Geriatr. 1985;16:239–245. [PubMed] [Google Scholar]
- 22.Pérez-López FR. Vitamin D and its implications for musculoskeletal health in women: an update. Maturitas. 2007;58:117–137. doi: 10.1016/j.maturitas.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 23.Bahk J, Yun SC, Kim YM, Khang YH. Impact of unintended pregnancy on maternal mental health: a causal analysis using follow up data of the Panel Study on Korean Children (PSKC) BMC Pregnancy Childbirth. 2015;15:85. doi: 10.1186/s12884-015-0505-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Niikura T, Oe K, Sakai Y, Iwakura T, Fukui T, Nishimoto H, et al. Insufficiency and deficiency of vitamin D in elderly patients with fragility fractures of the hip in the Japanese population. J Orthop Surg. 2019;27:2309499019877517. doi: 10.1177/2309499019877517. [DOI] [PubMed] [Google Scholar]
- 25.Smolensky MH, Sackett-Lundeen LL, Portaluppi F. Nocturnal light pollution and underexposure to daytime sunlight: complementary mechanisms of circadian disruption and related diseases. Chronobiol Int. 2015;32:1029–1048. doi: 10.3109/07420528.2015.1072002. [DOI] [PubMed] [Google Scholar]
- 26.Vriend J, Reiter RJ. Melatonin, bone regulation and the ubiquitinproteasome connection: a review. Life Sci. 2016;145:152–160. doi: 10.1016/j.lfs.2015.12.031. [DOI] [PubMed] [Google Scholar]
- 27.Ostrowska Z, Kos-Kudla B, Marek B, Swietochowska E, Górski J. Assessment of the relationship between circadian variations of salivary melatonin levels and type I collagen metabolism in postmenopausal obese women. Neuro Endocrinol Lett. 2001;22:121–127. [PubMed] [Google Scholar]
- 28.Kopiczko A. Determinants of bone health in adults Polish women: the influence of physical activity, nutrition, sun exposure and biological factors. PLoS One. 2020;15:e0238127. doi: 10.1371/journal.pone.0238127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stinchcombe A, Kuran N, Powell S. Report summary. Seniors' Falls in Canada: Second Report: key highlights. Chronic Dis Inj Can. 2014;34:171–174. [PubMed] [Google Scholar]
- 30.Hoffenberg R, James OFW, Brocklehurst JC, Green ID, Horrocks P, Kanis JA, et al. Fractured neck of femur: prevention and management. Summary and recommendations of a report of the Royal College of Physicians. J R Coll Physicians Lond. 1989;23:8–12. [PMC free article] [PubMed] [Google Scholar]
- 31.Kanis JA, Pitt FA. Epidemiology of osteoporosis. Bone. 1992;13:S7–S15. doi: 10.1016/s8756-3282(09)80004-5. [DOI] [PubMed] [Google Scholar]
- 32.Hagino H, Sawaguchi T, Endo N, Ito Y, Nakano T, Watanabe Y. The risk of a second hip fracture in patients after their first hip fracture. Calcif Tissue Int. 2012;90:14–21. doi: 10.1007/s00223-011-9545-6. [DOI] [PubMed] [Google Scholar]
- 33.Vieth R. Vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety. Am J Clin Nutr. 1999;69:842–856. doi: 10.1093/ajcn/69.5.842. [DOI] [PubMed] [Google Scholar]
- 34.Liang G, Nan H, Qureshi AA, Han J. Pre-diagnostic plasma 25-hydroxyvitamin D levels and risk of non-melanoma skin cancer in women. PLoS One. 2012;7:e35211. doi: 10.1371/journal.pone.0035211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006;81:353–373. doi: 10.4065/81.3.353. [DOI] [PubMed] [Google Scholar]
- 36.Farrar MD, Webb AR, Kift R, Durkin MT, Allan D, Herbert A, et al. Efficacy of a dose range of simulated sunlight exposures in raising vitamin D status in South Asian adults: Implications for targeted guidance on sun exposure. Am J Clin Nutr. 2013;97:1210–1216. doi: 10.3945/ajcn.112.052639. [DOI] [PubMed] [Google Scholar]
- 37.Miyauchi M, Hirai C, Nakajima H. The solar exposure time required for vitamin D3 synthesis in the human body estimated by numerical simulation and observation in Japan. J Nutr Sci Vitaminol (Tokyo) 2013;59:257–263. doi: 10.3177/jnsv.59.257. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Unadjusted and Adjusted ORs (95% CI) of Total Fracture according to Daily Sunlight Exposure Duration and Serum 25-Hydroxyvitamin D Level in Korean Elderly with Osteoporosis from the KNHANES 2008–2011