Abstract
Background:
Cervical cancer screening remains unsatisfactory in some regions due to hindrances. This study aims to explore fundamental elements in training patient navigators and their involvement in promoting screening knowledge and practices.
Methods:
This systematic review study included only English published articles between 2014 and 2019 from PubMed/Medline, EBSCO, Science Direct, and Wiley online library.
Results:
Healthcare professionals trained patient navigators in 3 days regarding screening basics, along with group discussions and role-plays. They delivered effective health education and navigation assistance.
Conclusion:
The group education session facilitated by patient navigators, coupled with navigation care, resulted in a high screening rate.
Keywords: cervical cancer, community health workers, health education, patient navigation, promotora, training
Introduction
Cervical cancer is the fourth common cancer diagnosed among women worldwide, and in 2018, 569,847 women diagnosed with cervical cancer. 1 More than 270,000 women worldwide die every year due to cervical cancer, and 85% of these deaths occur in developing countries. 2 The global age-standardized incidence rate (ASIR) is 13·1 per 100,000 women-years, and the global age-standardized mortality rate (ASMR) is 6·9 per 100,000, with the highest ASIR in Southern Africa (43·1), Eastern Africa (40·1), and lowest ASIR in Western Asia (4·1) and Australia and New Zealand (6·0). 3 Early diagnosis of cervical cancer increases the survival rate, reduce treatment costs, 4 and further reduce morbidity and mortality. 2 Even though the incidence of cervical cancer can be reduced by 80% through the utilization of cervical cancer screening services, 5,6 the screening rates of cervical cancer remains unsatisfactory in some regions due to underutilized screening services. 7 Screening rates for cervical cancer in 2013 in Mexico was 20.7% and less than 50% in Hungary, Italy, Japan, Latvia, Estonia, Slovak Rep, and Lithuania, 8 while the general screening rate in 55 Low-middle income countries was 44%. 9 There are several screening hindrances, including women’s fear of screening procedures thinking might lead to their infertility, 10 poor attitude toward screening for cervical cancer triggered by anticipation of pain, male involvement in the screening procedure, lack of privacy and fear to receive CCS results, 11 and knowledge deficit about cervical cancer and screening. 12 Even though various approaches such as health education have been implemented in different countries to promote cervical cancer screening uptake, the screening rate remains low because the approaches do not address multiple screening hindrances. Therefore, there is a demand for an intervention approach that can rectify the shortcomings of the existing approaches and address multiple screening hindrances collectively. 13
Patient Navigation
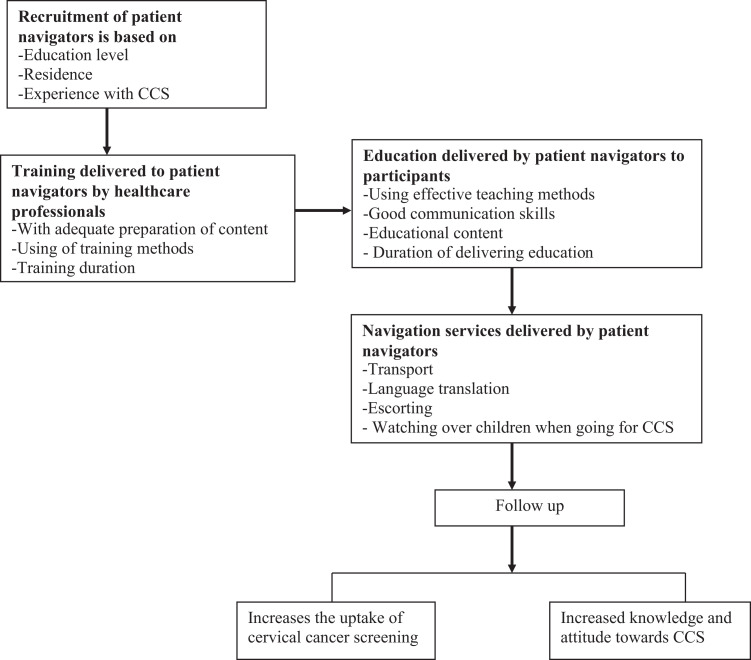
Due to the increased barriers in the uptake of breast and colorectal cancer screening services, Freeman introduced the patient navigation approach in 1990 to promote behavior in uptake screening services. 14 The patient navigation approach is widely applied to promote awareness of cervical cancer and cervical cancer screening (CCS) behavior. 14 Patient navigators are native lay individuals living in the same community of potential interventional participants and helping women with/without abnormal CCS overcome screening barriers. 15 -18 The patient navigators educate women regarding CCS and help them overcome barriers in the uptake of CCS services, increasing women intention and promote positive beliefs to uptake CCS services. 16 -21 Even though patient navigation is important in promoting screening uptake, it remains underutilized mainly in many regions, 22 and there is still a lack of studies reporting on the training of patient navigators and the whole process of the patient navigation process. The study aims to explore fundamental elements in training patient navigators and their involvement in promoting public cervical cancer screening knowledge and practices. The research questions for this review are; ① How should patient navigators be trained? ② How do patient navigators promote community awareness on CCS? ③ What are the impacts of patient navigation to the community? The conceptual framework involves recruiting patient navigators, training them under a well-developed model, and patient navigators delivering structured patient navigation intervention to community women. 23 -26 Refer Figure 1.
Figure 1.
Conceptual framework.
Significance of the Study
This study will help researchers implement effective patient navigation intervention that will result in a precise outcome.
Methods
Study Selection Criteria and Search Strategy
This study is a systematic review conducted to examine the effective ways of training patient navigators on CCS and the model of delivering patient navigation intervention to communities. This review was registered in PROSPERO International prospective register of systematic reviews with ID No CRD42020157594 (https://www.crd.york.ac.uk/prospero/#myprospero). The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyzes) guideline was followed in performing this systematic review. Only English published articles from 2014 to 2019, randomized control trials (RCTs), quasi-experimental studies and cohort study were included in the study. Articles were searched from PubMed/Medline, EBSCO, Science Direct, and Wiley online library. Search terms were uterine cervical neoplasms, cervical cancer, community health workers, patient navigators, promotora, primary health workers, social support networks, patient navigation, and coach.
Example of Search Strategy From PubMed Central (PMC)
The following search strategies were used: (((Uterine Cervical Neoplasms [MeSH Terms]) OR cervical cancer)) AND (((((((Community Health Workers[MeSH Terms]) OR patient navigators) OR Promotora) OR Primary Health Workers) OR social support networks) OR Patient Navigation[MeSH Major Topic]) OR COACH). The search was only limited to publication date from 01st January 2014 to 03rd May 2019. The search was performed on 17th November 2019.
Inclusion and Exclusion Criteria
Studies were included if they focused on cervical cancer, patient navigation, and patient navigators who had no healthcare professional background. The primary intervention was patient navigation delivered by patient navigators. The primary outcome was CCS uptake, while the secondary outcome focused on changes in the level of knowledge on cervical cancer and CCS. Studies were RCTs, quasi-experimental, or cohort studies and available at full text. Studies were excluded if they reported patient navigation on post-diagnosed women with abnormal CCS, lacked details about patient navigator’s training, and only focused on training of patient navigators without reported how patient navigators delivered the intervention to communities. Studies were further excluded if patient navigation interventions focused on breast cancer, prostate, colorectal cancer, ovarian cancer, mental health, diabetes, hypertension, HPV vaccination, HPV Self-Sampling, blood pressure measurement, child nutrition, sexually transmitted infections, HIV/AIDS, and cost-effectiveness. Review studies, qualitative studies, cross-sectional quantitative studies, commentaries, letters, and study protocols were excluded. Moreover, studies were excluded if healthcare professionals delivered patient navigation interventions or patient navigators delivered only navigation assistance without education. Studies were excluded if full papers could not be found.
Population
In this review, patient navigators are defined as native lay people having no medical professional background, recruited based on criteria and trained by nurses or physicians to become patient navigators 16,19,27,28 to promote access to timely diagnosis and treatment of cervical cancer by eliminating barriers to care. 29 They should have a high school or college educational level 15,19 living in the same community and helping women with/without abnormal CCS to overcome screening barriers, 15 -18 through delivering education intervention about CCS and providing navigation assistance services.
Intervention
The intervention involved the training of patient navigators by healthcare professionals. After that, patient navigators delivered patient navigation to community women, including health education and navigation assistance services to promote CCS uptake and changes in the knowledge level of cervical cancer and cervical cancer screening.
Comparator(s)/Control
There is no comparator (s)/ control reported in the review.
Outcome Measures
The outcome measures for studies included in this review were the completion of screening tests in the allocated period and changes in the level of knowledge on cervical cancer and screening.
Data Extraction and Analysis
Due to data heterogeneity, a systematic review was conducted to explore fundamental elements in training patient navigators and their involvement in promoting public cervical cancer screening knowledge and practices. After initial screening, the full texts relevant to the topic were reviewed independently by 2 authors (JFM and KD). Extraction of data was performed and entered in a data charting form in Microsoft Excel. Any emerged disagreement concerning inclusion and exclusion from the final review, the third author (MAG) got involved. After the data were entered into a data charting form, the authors (JFM and KD) reviewed the data to identify the review’s key focus areas. The results of the review are reported according to the PRISMA Statement. 30
Risk of Bias
The interventional studies’ quality was evaluated using an effective public health practice project (EPHPP) tool, which contains 6 components: selection bias, study design, confounders, blinding, data collection method and withdrawals/ dropouts. Each component is rated as weak (1 point), moderate (2 points), and strong component (3 points). The maximum total score per study is 3.00. Based on their total score, the quality of studies is rated as weak (1.00-1.50), moderate (1.51-2.50) or strong (2.51-3.00). 31 The records underwent final assessment according to the EPHPP tool along with established inclusion and exclusion criteria.
Ethical Approval
Ethical approval was not sought because the study involved reviewed previously published articles and did not directly involve human participants.
Results
Study Characteristics
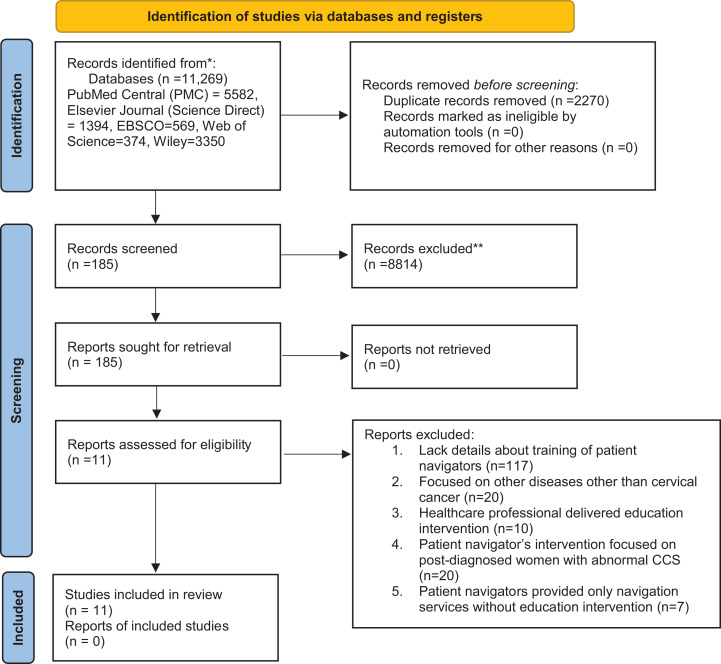
Records identified through databases on the first search were (n = 11,269) and reduced to (n = 8999) after duplicates were removed. After screened titles and abstracts, the records further reduced to (n = 185), while (n = 8814) records were excluded because their titles and abstracts did not conform to the topic or the study designs. Full-text articles were assessed for eligibility, and 11 articles were included in this review, while 174 articles were discarded. Refer Figure 2. The included 11 studies were (6 RCTs, 4 quasi-experiment design, and 1 cohort design) with 3372 participants from 6 countries (USA, Kenya, Canada, Hongkong-China, Nigeria, and Turkey). Nine studies 17,19,21,24,28,32 -35 were conducted in communities, while 2 studies 36,37 were conducted in healthcare facilities.
Figure 2.
PRISMA 2020 flow diagram for new systematic reviews which included searches of databases and registers only. *Consider, if feasible to do so, reporting the number of records identified from each database or register searched (rather than the total number across all databases/registers). **If automation tools were used, indicate how many records were excluded by a human and how many were excluded by automation tools. From: Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71.
Recruitment of Patient Navigators
All 11 studies in this review focused on the evaluation of patient navigation intervention delivered by patient navigators. The majority of 5 papers 19,21,32,33,36 synonymously named patient navigators as community health workers (CHWs), 3 papers 17,24,37 promotora, while others titled peer leaders or lay health educators, 28 peer health educators, 34 and female teachers. 35 Regarding the recruitment of patient navigators into the study, most papers reported educational background and being familiar with culture as recruitment criteria; 1 study 19 noted that patient navigators were recruited from churches aged between 40-60 years old, with a high school level of education and had never worked in cervical cancer program. One study 21 selected patient navigators from churches based on interest, availability, and commitment to the project. Two studies 24,28 reported that community leaders proposed the potential patient navigators who were trusted, lived and familiar with the community’s values and culture. One paper 34 reported that patient navigators had completed secondary school education, volunteered to be trained, and community role models. One study 37 showed that the recruited patient navigators was bilingual in both Spanish and English. Refer to Table 1.
Table 1.
Summary Regarding the 11 Articles Included in the Review.
| Abbreviated citation | Study aim | Study setting | Country of origin | Priority population | Study design | Position title | Sample size | Intervention summary | Outcome measures | Results (training outcome) |
|---|---|---|---|---|---|---|---|---|---|---|
| (Thompson, Carosso, Jhingan, Wang, & Holte, 2017) | The use of Promotora and video education to increase Cervical cancer Screening Among Rural Latinas | A rural agricultural region where approximately 67% of the population are of Latino | USA (Yakima Valley of Washington State) | Being out of adherence with current recommendations for Pap test screening, 21 to 64 years old, and having no a prior Hysterectomy | 3-arm randomized controlled trial | Promotora | Control (usual care) (n = 147), low intensity (video) intervention arm (n = 150) and high intensity (video + promotora) intervention arm (n = 146) | Promotora were trained for 3 days on procedures for approaching households and delivering the intervention, cervical cancer screening facts and tracking and documentation procedures. Women in the high-intensity arm received a promotora-led educational session in their home. The educational session included watching the video with the promotora followed by discussion. A local resource sheet listing means for overcoming barriers to care such as financial aid, transportation, and childcare was provided. | The primary outcome was completion of a Pap test within the 7 months after randomization. Secondary outcomes included changes in knowledge level. | We see that significantly more women underwent Pap test within 7 months of randomization in the high-intensity arm (n = 578 [53.4%]). We found significant increases in the knowledge factors overall for all the variables in all arms. |
| (Han et al, 2017) | To assess the impact of CHW intervention focused on building health literacy skills among Korean American women. | Community churches | USA, Baltimore, Maryland—Washington, DC | Women aged 21 to 65 years, had not had a Pap test within the past 24 months, and were able to read and write Korean or English | A cluster-randomized wait list control design | Community health workers (CHW) | 560 women agreed to participate: (intervention: n = 278; control: n = 282) | CHWs had at least a high school level of education. CHWs received 16 hours of training over 3 days, CHWs learned key medical terminology in cervical cancer screening and screening of relevant medical instructions. Initially, the intervention group received brochure tailored individual risk factors for cervical cancer, followed by CHWs delivered a health literacy skills training in 1 ½ to 2-hour-long group meeting. At the end of session, participants received DVD and picture guidebook. CHWs made monthly telephone calls provide navigation assistance over a 6-month period. | Outcome measure were participants characteristics, Pap test use in 6 months, and changes in cancer knowledge | At 6 months, 54.5% of those in the intervention group received Pap test. The mean increase in health literacy was 7.0 points (95% CI = 4.9, 9.0) higher on average in women in the intervention group than women in the control group |
| (Rosser, Njoroge, & Huchko, 2015) | To find out whether the health talk provided by CHWs promote changes in knowledge level and screening rates | Rural health facilities | Kenya, East Africa | Non-pregnant women aged 23 years old, had not previously screened, could speak native or English language, willing to provide informed consent | 2-Arm Randomized Controlled Trial (RCT) | Community health worker (CHW) | Intervention (N = 207) and control (N = 212) arm | CHWs attended 1-day training learned and practiced teaching materials. Participants in the intervention arm participated in the group health talk delivered by CHWs. The intervention consisted of a 30-minute interactive talk about cervical cancer, risk factors, how screening is performed, what screening results mean, and treatment options. The flipchart was used. | The primary outcome was change in knowledge level. Secondary outcome was perception of personal cervical cancer risk. The follow up was 3-months. | Knowledge scores in the intervention arm increased 26.4% (8.7 to 11.0 points) compared to only a 17.6% increase (8.5 to 10.0 points) in the control arm. Over half of all participants in the intervention arm (N = 122/207; 58.9%) underwent screening |
| (Mojica, Morales-campos, Carmona, & Ouyang, 2015) | Latinas attending the education-plus-navigation intervention would increase their knowledge of cervical cancer and would report receipt of Pap test | Community-based organizations | West and south sides of San Antonio, Texas. USA | Women aged 18 to 65 years and had never had a Pap test or not had 1 in the past 3 | A single-arm, nonrandomized, pre–post design | Community Health Worker (CHW) | 691 participants were recruited into the study, while 535 attended the education | 2-week of CHWs training to discuss study protocols on data collection procedure, cervical cancer risks, screening tests and guidelines by project coordinator. CHWs provided 1 group session education to the community about cervical cancer risks, screening guidelines, and benefit of early detection in convenient places using English or Spanish in 90 minutes. Bilingual flip charts, with visual content such as culturally relevant pictures and graphics to establish a connection between the information. After session, CHWs provided health informational sheets on cervical cancer and cervical cancer screening. CHWs provided navigation service; scheduled appointment, help women to identify low or free cost screening service, reminder, follow-up calls before and after clinic appointments. |
The primary outcome was receipt of Pap test. Secondary outcomes were knowledge of screening guidelines, knowledge of the benefits of early detection, and beliefs on early detection. | 158 (72%) participants at pretest and 176 (80%) at posttest correctly answered questions (P = 0.03) and 25% (n = 174) of eligible participants reported having screened for cervical cancer |
| (Schuster et al, 2015) | To evaluate the screening adherence within 6 months aforementioned health literacy-focused intervention delivered by CHWs | Community churches | USA Johns Hopkins University School of Nursing | Women aged 21 to 65 years old, had not had Pap test within the last 24 months, able to read and write Korean or English, and willing to provide written consent | Cluster-randomized controlled trial | Community health workers (CHWs) | Participants in the intervention group (n = 245) and participants in the control group (n = 43) | CHWs in received 3-day training from CHWs coordinator regarding predisposing, enabling, and reinforcing factors consistently found to affect cancer-screening behaviors. Intervention group received a brochure containing specific health messages and information tailored to individual risk factors. Thereafter, CHWs delivered a 2-hour education to participants on English medical terminology in the context of cervical cancer screening. At the end of the education session, participants received a DVD and a picture guidebook that detailed the health literacy content covered in the class. Navigational assistance included making a screening appointment, providing transportation and translation services, and/or completing paperwork. | Participants were required to complete screening within 6 months but the follow up were 3-monthly after the education | Out of 276 participants in the interventional group received brochure and CHW health literacy program, 85% participants were screened against 15% in the control group |
| (Dunn et al, 2017) | To assess the impact of Cancer Awareness: Ready for Education and Screening (CARES) on cervical screening facilitated by community-based peer leaders and CARES program staff. | Community-based intervention | Toronto, Canada | Women aged 21-69 years old | Cohort study | Peer leaders or lay health educators | 331 participated in the CARES cohort | 42 peer leaders or lay health educators, attended a 3-day training session delivered by research stuff that included orientation of their roles, content about cervical cancer, cancer screening, adult learning principles, communication skills, group facilitation skills, woman centered decision-making, cross-cultural sensitivity, time management, challenging situations, and research documentation. Even after the training, research stuff kept providing on-going mentorship either face-to-face or through telephone Peer leaders shared the content orally in the language of the group regarding information about cervical cancer screening. Educational materials consisted of a simple PowerPoint presentation with Slides contained visual imagery. Linguistic, childcare, transportation, and guiding women to access screening were navigation services | The primary outcome was the participation in the screening program in the 8 months. | 26% had screened against 9% in the control group |
| (Wong, Choi, Law, Chan, & So, 2019) | To examine whether CHW-led intervention can enhance cancer knowledge and screening intention among South Asian ethnic minorities in these communities | Non-governmental organizations | Hong Kong, China | Women aged 25 or above, with previous sexual activity, no previous cervical cancer screening in the past 5 years, no previous cancer diagnosis, and no educational intervention on cervical cancer screening in the past year. | Randomized wait-list controlled trial | Community Health Worker (CHW) | 42 participants allocated to either the CHW-led intervention (n = 21) or wait-list control arm (n = 21). | Two nurses and 1 psychologist delivered CHW training about the disease (risk factors, signs and symptoms, and associated myths and misconceptions, and measures for early detection). Topics included currently available screening tests, consequences of delaying cancer detection, barriers against the uptake of screening services, and possible strategies to overcome these barriers, as well as influencing their community peers to engage in cancer prevention practices. Short lectures and teaching strategies were Group games, group discussion, real-life video, role play and demonstrations. CHWs delivered 30 minutes intervention using a structured PowerPoint slide with a video clip. Information booklet was provided to each participant to recap what they had learned A monthly telephone follow-up and the provision of navigation assistance | The primary outcome was cervical screening uptake in 3 months, and secondary outcome were, Readiness to Undergo Screening, Screening Beliefs, Socio-demographic information | The use of the multimedia approach would enable a more effective education of individuals with lower literacy levels. Participants (100% in the control arm and 95.2% in the intervention arm) indicating that they would undergo a Pap test within the next month. |
| (Fleming et al, 2018) | To assess the Promotora-Led Charla Intervention in promoting cervical cancer screening, knowledge, and beliefs | Community-based facilities (eg, FSH youth center, church, etc.). | USA | Women aged 21-70 years, able to speak and read Spanish or English, and able to provide written informed consent | single-arm study used a pretest-posttest design | Promotora, community health educator (CHE) | 60 women | Promotora were selected from the community through community leaders. Promotoras received training through 3 educational sessions on role and function of promotoras, significance of health disparities in their community, cervical cancer screening guidelines, HPV transmission, HPV vaccines, cervical cancer causation, and local Pap testing resources. Role-plays were used. Charlas are small tailored group discussions (chats) on targeted health topics. Promotora conducted a total of 6 charlas (sessions) lasting about 75 minutes each. The navigation service provided was scheduling appointments | Uptake of pap test in 3 months, cervical cancer/HPV knowledge, socio demographic characteristics | 20 participants had received a Pap test (65%). Repeated measures ANOVAs revealed a significant increase in HPV knowledge and Pap test self-efficacy (F [1,59] >22.7, Ps < .0001) following participation in the charla. |
| (Molokwu, Penaranda, Flores, & Shokar, 2015) | To evaluate the effect of a promotora-led educational program on HPV and cervical cancer | Clinical setting | USA | Women aged 30 to 65 years old, had a uterus, had no history of cervical cancer, without hysterectomy, or pregnant. | Quasi-experimental study | Promotora | A total of 347 women were approached, and 31.7 % met the inclusion criteria and agreed to participate in the study | Promotora were trained in 3 initial sessions followed by continued review and supervision during the study period. Promotora were trained on cause of cervical cancer, risk factors, basic Pathophysiology, as well as disease progression and communication skills. CHWs delivered a 1 hour educational session covered information on important basic cervical cancer facts: what is cervical cancer, who gets cervical cancer, how do women get cervical cancer, causes of cervical cancer, role of HPV in causing cervical cancer, symptoms of cervical cancer, risk factors for cervical cancer, screening guidelines for cervical cancer, and prevention of HPV. Educational sessions were carried out on an individual or small group basis. Sessions were also held in English or Spanish based on participants identified preferred language. | Participant’s knowledge level and social demographic characteristics | Participants showed an improvement of knowledge level on cervical cancer and HPV infection from a mean score of 10.8 (SD 3.43) out of a possible score of 18 to a mean score of 16.0 (SD1.51) (P < 0.001). |
| (Ayla Bayık Temel, Şafak Dağhan, Şenay Kaymakçı, Renginar Öztürk Dönmez, & Zeynep Arabacı, 2017) | To encourage teachers to teach and share the knowledge with the women who attend their classes and courses in public training centers, and also to evaluate the diffuseness of the teachers’ training efforts on the students’ Pap smear test (PST) behaviors. Screening knowledge and to evaluate the uptake of screening service |
Public training centers | Turkey | Females studying at the public training centers | Quasi-experimental with pre-intervention and post-intervention | Female teachers | 64 volunteering students | Teachers attended a training session that took 60 minutes covered content about anatomy, physiology of reproductive system, cervical cancer symptoms, risk factors, early detection, prevention, treatment methods, and PST. The training session was carried out in the form of lectures and group discussions. CD, documents, brochure, and magnet with a message (Don’t be afraid of cancer, learn how to prevent and share your knowledge) were given out to the participants for self-learning and to reinforce their memories. At the end of the training program, the teachers transferred the knowledge to their volunteer students (n = 64) through the lecture method. | To evaluate the effect of a structured teaching program on cervical cancer screening on the knowledge and practice of teachers after t the 6 months | The mean score of knowledge of the teachers in terms of cervical cancer risk factors and its early diagnosis was 7.75 ± 5.60 (Min = 1, Max = 18) before the training and 17.68 ± 3.79 (Min = 12, Max = 25) after the training. After the knowledge transferred to students, 67% of all the students had undergone PST and had positive behavior change on PST |
| (Mbachu, Dim, & Ezeoke, 2017) | To examine the effectiveness of peer health education on perception, willingness to screen and uptake of cervical cancer screening by women | Community churches | Enugu state, Nigeria. | Women aged 21 years old or more; currently sexually active or have been in the past; and never been diagnosed with any cancer | Community-based randomized, A before and after intervention study | Peer health educators | 283 participants | The peer health educators completed secondary school. Education, role models and well respected in the community. An 18-hour peer educators’ training workshop was provided over a 3-day period covered basic information of cervical cancer; burden of cervical cancer, risks, prevention, screening tests and guidelines, existing myths. After the training, the peer health educators provided Group session consisted of 45-60 min on what the cervix is and how it can be kept healthy; definition of cervical cancer; burden of cervical cancer in Nigeria relative to other settings; risk factors, symptoms and signs of cervical cancer; prevention and treatment options for cervical cancer; and healthy living with cervical cancer | Outcome measures were perception of individual risk for cervical cancer and benefits of screening, willingness to screen, actual practice of screening, preferred method, frequency of screening and reasons for screening | The proportion of participants who screened for cervical cancer increased from 30 (10.5%) before the intervention to 49 (17.3%) after the intervention. Higher proportions of participants 219 (77.4%) perceived cervical cancer to be as serious as other cancers (P < 0.001); and felt themselves at risk of developing cervical cancer 113 (40%) (P = 0.01). Majority who reported that screening for the disease would be highly beneficial increased significantly from 145 (50.9%) to 195 (68.9%) after the intervention (P = 0.01). |
Training of Patient Navigators
Most of the papers reported 3 days to be adequate in training patient navigators such that; 5 studies 17,19,21,28,34 reported that patient navigators were trained for 3 consecutive days, with a total of 16 hours 19 or 18-hour. 34 Even though different papers have reported different content to be covered during the training of patient navigators, basic knowledge of cervical cancer is most often reported, such as cervical cancer meaning, causes, risk factors, prevention and roles of patient navigators coupled with roles of patient navigators. In 3-day training, patient navigators learned the following; 1 paper 17 showed that the training covered content related to approaching households procedure, delivering patient navigation intervention, tracking and documentation procedures. One paper 19 reported that patient navigators learned key medical terminology used in cervical cancer screening, screening relevant medical instructions (e.g., appointment slips, follow-up instructions) and familiarity with appropriate steps to navigate the health care system for Pap test screening. One paper 21 showed that Patient navigators learned predisposing, enabling, and reinforcing factors consistently found to affect cancer screening behaviors. One paper 28 reported that the training covered orientation of patient navigators roles, content about cervical cancer, cancer screening, adult learning principles, communication skills, group facilitation skills, woman-centered decision-making, cross-cultural sensitivity, time management, challenging situations, and research documentation. One paper showed that in 3-day training, patient navigators learned information about cervical cancer burden, risks, prevention, screening tests and guidelines, and existing myths.
One paper 32 showed that patient navigators were trained for 2 weeks to learn about data collection procedure, cervical cancer risks, screening tests and guidelines, screening experiences and misconceptions. One paper 37 showed that patient navigators were trained in several topics, including cervical cancer cause, risk factors, basic Pathophysiology, disease progression, HPV knowledge, and communication skills to improve their ability to deliver the intervention in both English and Spanish. One paper 24 reported that patient navigators received knowledge and skills-based training through 3 educational sessions. One paper 35 reported that patient navigator’s training included 1 theoretical session lasting for taking 60 minutes covered anatomy and physiology of the reproductive system, cervical cancer symptoms, risk factors, early detection, prevention, treatment methods, and PST. One paper 33 reported that the training covered cervical cancer risk factors, signs and symptoms, myths and misconceptions, measures for early detection, screening tests, consequences of delaying cancer detection, barriers in the uptake of screening services, and possible strategies to overcome these barriers, as well as to influence their community peers to engage in cancer prevention practices. One paper 24 showed that the training covered patient navigator’s role and function, significance of health disparities in their community, cervical cancer screening guidelines, HPV transmission, HPV vaccines, and cervical cancer causation. It further covers content regarding local Pap testing resources, how to motivate women, how to encourage a dialogue with women, schedule a Pap test through community resources, and conduct reminder phone calls.
Most of the papers reported that patient navigators are trained by healthcare professionals such that 3 papers 21,28,37 reported that study coordinators conducted patient navigator’s training. One paper 33 reported that nurses delivered the training. Two papers 28,37 show that even after the training, the facilitators kept providing on-going mentorship either face-to-face or through telephone to discuss specific problems or issues related to the participants and address questions that came up during the educational sessions. One paper 35 reported that patient navigators completed pre-test surveys on cervical cancer knowledge, attitudes, beliefs and socio-demographics, information sources, and cervical cancer screening barriers. Even though different techniques in delivering health education are reported in different papers, lectures, discussion, role-play, and take-home learning materials are most often mentioned. One paper 33 reported that the patient navigators training was conducted through short lectures, recapitulation, debriefing sessions, coupled with other teaching strategies such as group games, group discussion, real-life video enhanced patient navigators awareness, scenario-based role-play and demonstrations. One paper 24 showed that role-playing was used during training to help patient navigators gain confidence. One paper 35 reported that the training sessions were carried out in the form of lectures and group discussions, and after the training, patient navigators were provided with CD, documents, brochure, and magnet with a message (Don’t be afraid of cancer, learn how to prevent and share your knowledge) for self-learning and to reinforce their memories. Refer to Table 1.
Patient Navigation Intervention (Health Education and Navigation Assistance) Delivered by Patient Navigators
Most of the studies reported that women who received patient navigation aged (ranging 18 to 70) years, never screened previously, willing to participate, non-pregnant, no history of hysterectomy and able to speak the native language or English. One study 17 reported that women who received patient navigation intervention were out of adherence with current recommendations for Pap test screening, 21 to 64 years old, and having no prior Hysterectomy. Two papers 19,21 reported that participants aged 21 to 65, had not had a Pap test within the past 24 months and could read and write Korean or English. One study 36 reported that participants were non-pregnant women, aged 23 years old, had not previously been screened, could speak native or English language, and willing to provide informed consent. One study 28 reported that participants in the intervention were aged 21-69 years old. One paper 32 reported that participants aged 18 to 65 years old who had never had a Pap test or not had 1 in the past 3 years. Two studies 33,34 showed that participants in the study aged 25 or above, with previous sexual activity, no previous cervical cancer screening in the past 5 years, no previous cancer diagnosis, and had not received educational intervention on cervical cancer screening in the past year. One study 37 reported that participants in the intervention aged 30 to 65 years old, with no history of cervical cancer, hysterectomy, and not pregnant. One study 24 showed that women in the intervention were 21-70 years old, able to speak and read Spanish or English and provide written informed consent.
One study 17 reported that eligible participants were identified by systematic electronic medical record review and were contacted by clinic staff. Seven papers 17,21,32 -34,36,37 reported that participants signed consent and were administered pre-intervention baseline surveys by patient navigators. Three papers 32,33,37 reported that the baseline survey assessed knowledge, attitudes, beliefs and socio-demographics about CCS. One paper 17 reported that patient navigators delivered intervention within the first 30 days after consent was received and baseline survey completed.
Many studies reported that patient navigation intervention begins with community health workers delivering health education with various education techniques and later provide navigation assistance to the needy. One paper 17 reported that the educational session included watching 13 minutes of culturally appropriate video with patient navigators, which contained information about CCS. The participants had the opportunity to discuss relevant issues with patient navigators. Two papers 19,21 reported that the intervention groups initially received brochure tailored individual risk factors for cervical cancer, followed by patient navigators education intervention. One paper 36 showed that patient navigators delivered health talk session covered the content of cervical cancer, risk factors, how screening is performed, what screening results mean, treatment options, barriers and stigma or fear associated with screening. One paper 28 reported that patient navigators delivered health education regarding cervical cancer screening. One paper 32 showed that health education content was cervical cancer risks, screening guidelines, and early detection benefits. One paper 33 reported that health education was delivered on cervical cancer and prevention, coupled with a video clip. One paper 37 showed that health education session covered information on important basic cervical cancer facts: what is cervical cancer, who gets cervical cancer, how do women get cervical cancer, causes of cervical cancer, the role of HPV in causing cervical cancer, symptoms of cervical cancer, risk factors for cervical cancer, screening guidelines for cervical cancer, and prevention of HPV. One paper 24 reported that during the health education session, participants learned about cervical cancer screening guidelines, HPV transmission, HPV vaccines, and cervical cancer causation. One paper 34 reported that patient navigators delivered health education on what the cervix is and how it can be kept healthy, the definition of cervical cancer, burden of cervical cancer, risk factors, symptoms and signs of cervical cancer; prevention and treatment options for cervical cancer; and healthy living with cervical cancer. One paper 35 reported that participants learned about the anatomy, physiology of the reproductive system, cervical cancer symptoms, risk factors, early detection, prevention, treatment methods, and PST.
Many studies often reported the utilization of group education session than individual education session, and a 1-time health education session duration ranging from 30 minutes to 90 minutes. Seven papers 17,21,24,28,32,34,36 reported that the interventions were delivered in-group education session. One paper 37 reported that educational sessions were carried out on an individual or small group. One paper 19 showed that the duration of the education session was 1 ½-2-hours. Two papers 33,36 reported that the education session took 30-minutes. One paper 21 reported that the health education intervention was conducted for 2-hours. One paper 32 reported that the education session lasted for 1 ½ hour. One paper 37 reported that the health education intervention was delivered for 1-hour. One paper 24 showed that participants received health education for 75-minutes. One paper 34 reported that the intervention was conducted for 45-60 minutes.
The most frequent strategy used by patient navigators to deliver health education was through visual teaching strategies such as using PowerPoint, flip charts, and other pictures. Two papers 28,33 reported that the education sessions were conducted using a simple PowerPoint presentation with slides containing visual imagery. One paper 35 showed that health education was delivered through lecture. One paper 32 showed that bilingual flip charts with visual content such as culturally relevant pictures and graphics were used to establish a connection between the information during the health education session. One paper 34 reported that didactic teaching were utilized. Two papers 32,37 reported that the health education was delivered in native language or English. Four papers 32,34,36,37 reported that participants completed a post-test survey at the end of the intervention.
Many papers commonly reported that women were provided with take-home learning materials for a recap after health education, where booklet was often mentioned. Two papers 19,21 reported that participants received DVD and picture guidebooks that detailed the health literacy content covered in the class to help them feel confident at the end of the health education session. Two papers 17,32 reported that at the end of the education session, participants were provided with health informational sheets and booklets listing information about cervical cancer and cervical cancer screening; means for overcoming barriers to care such as financial aid, transportation, and childcare as well as a reminder and appointment card. One paper 33 reported that participants received booklets after health education to recap what they had learned.
Most studies reported that patient navigators conducted follow-ups after delivering health education through phone calls and physical home visits. One paper 19,33 reported that patient navigators made monthly telephone calls after the health education to reinforce participants with the new skills and knowledge acquired from the health education session and provide navigation assistance. Three papers 21,24,36 reported that the follow up was 3-months and was done by phone and in-person home visits. During follow-up, linguistic and transportation services were most often mentioned in most studies as navigational assistance. One paper 21 reported that patient navigators provided navigational assistance after health education, including scheduling screening appointments, providing transportation, translation services, and completing paperwork. One paper 28 reported that patient navigators provided linguistic services, child care, transportation, and guide women to access screening after the health education sessions. Refer to Table 1.
Outcome Measures
Five papers 17,28,32,33,36 reported that the primary outcome was the participation of women in the CCS uptake. Two papers 32,33 reported that secondary outcomes were change in knowledge of screening guidelines, benefits of early detection, and beliefs on early detection. Three papers 19,21,35 showed that participants were required to complete screening in 6-month period. Refer to Table 1.
Effect of Patient Navigation in CCS Uptake
In many studies, screening participation increased among women who received patient navigation. In 6 papers 17,19,21,24,35,36 reported that the uptake of CCS after patient navigation intervention was above 50% in each paper, ranged (53.4%-85%) and with an average of 64%. Regarding the papers that reported the uptake of screening services less than 50%, 1 paper 28 reported that 26% (31/118) of participants had screened compared to 9% 30/344) in the control group, and participants who received the intervention were 5 times more likely to screen compared to their counterparts participants in the control group. Women’s age, health education duration, increased cervical cancer knowledge, and utilization of community leaders in promoting screening were most often reported to have influenced women to screen for cervical cancer. Even though women aged < 24 years and >53 received patient navigation, they were not age-eligible for screening. The age distribution was as follow, 16 (1.3%) were 21-29 years old, 57 (17.2%) were 30-39 years old, 93 (28.1%) were 40-49 years old, 85 (25.7%) were 50-59 years old, and 80 (24.8%) were 60-69 years. One paper 32 reported that after patient navigation, 25% of eligible participants underwent cervical cancer screening, while 45% had wrong/disconnected phone numbers or no answer, 10% refused further follow-up, 7% received no navigation support, and 14% had an appointment pending because clinics ran out of funds. One paper 34 reported that the proportion of participants who screened for cervical cancer increased from 30 (10.5%) before patient navigation intervention to 49 (17.3%) after patient navigation intervention. The slight difference was influenced by a short health education session lasted for 45-60 minutes. One paper reported that after the knowledge was transferred to students by teachers, it was found that 2/3 (43%) of all the students had undergone PST and had positive behavior change on PST.
One paper 35 reported that the increased knowledge level influenced women to screen for cervical cancer. One paper 24 showed that patient navigators and community leader’s collaboration positively impacted women participation in cervical cancer screening. One paper 17 reported that cost-effectiveness for screening influenced participants to uptake CCS. One paper 28 reported that patient navigators’ assistance, such as linguistic support and other cultural support, enhanced women’s uptake of CCS. Refer to Table 1.
Knowledge Level
When examining changes in knowledge between the baseline survey and the follow-up survey, studies have reported an increased knowledge level after patient navigation because the intervention was carried out in culturally acceptable ways and women had the opportunity to ask questions for clarification. Six papers 17,19,24,32,36,37 reported a significant increase in the knowledge level. One paper 24 reported that patient navigators’ performance influenced the increased knowledge, as they provided culturally and acceptable pertinent education to participants. One paper 37 reported that participants’ knowledge increased because during the health education by patient navigators, participants felt comfortable, were able to ask questions, and the information was delivered in a way that was easy to understand. Refer to Table 1.
Discussion
The purpose of this study was to review the literature to discover the effective training of patient navigators and delivery of patient navigation intervention to communities to increase the rate of cervical cancer screening and increase the knowledge level of women. This review has included 11 studies, and most of them were conducted in community settings.
Recruitment of Patient Navigators
Most studies have shown that trained patient navigators were titled community health workers (CHWs). 19,21,32,33,36 The recruited patient navigators had a level of education from secondary school to high school, 19,34 lived in the same community of withdrawn potential participants in the intervention, 21,24,28,34 familiar with community culture, 24,28,37 and proposed by community leaders. 24,28 Other previous studies support it indicated that the patient navigators should be selected from the same cultural background as the target participants and have higher level of education. 4,17,38,39
Training of Patient Navigators
Five papers 17,19,21,28,34 reported that the patient navigator’s training was conducted in 3 days. Three day’s training duration is supported by a previous systematic scoping review of the literature. 26 Nine papers 17,19,21,24,28,32,33,35,37 reported that the training content covered the basic knowledge of cervical cancer and screening; medical terminology of cervical cancer, cervical cancer cause, risk factors, disease progression, prevention, anatomy and physiology of reproductive system, treatment options, screening guidelines, screening tests barriers in the uptake of screening services, and how to overcome barriers. Two papers 32,33 reported that the education sessions covered myths and misconceptions. Two papers 24,28 reported that participants were trained on the roles and functions of patient navigators, and two 19,24 papers showed that patient navigators were trained about navigation services. Three papers 17,28,32 reported that patient navigators were trained on data collection procedures, tracking, and documentation. Four papers 17,24,28,37 reported that patient navigators learned facilitation skills and communication skills to help them approach households and deliver the intervention. A previous systematic review supports this reported that patient navigators were trained on cervical cancer screening, guidelines, communication skills, motivation interviewing, and navigation care. 40
The patient navigators training was conducted by healthcare professional nurses or physicians 21,28,33,37 and kept providing on-going mentorship throughout the study period. 28,37 It is reported from other studies that oncologists offer training and support to patient navigators to gain basic knowledge and skills on CCS. 40 -42 Only 1 study 35 conducted the pre-intervention survey for patient navigators, demonstrating the weakness in evaluating participants. The poor evaluation is reported in another previous study to indicate that few studies completed pre and post-intervention surveys. 26 The pre-and post-intervention surveys are vital to understanding the changes in variables after the intervention. The training was conducted in lectures, 33,35 group discussions, and role-plays. 24,33 This is consistent with the previous review paper’s findings that visual aids, practices, and role-play are effective training methods to facilitate patient navigators learning. 4
Patient Navigation Intervention
Women who received patient navigation intervention were aged between 21 to 70 years old, 17,19,21,24,28,33,34 being out of adherence according to screening guidelines, 17,32 or had not screened previously, 19,21,32 -34,36 had no prior hysterectomy, 17,37 able to read and write English and native language, 19,21,24,36 non-pregnant, 36,37 and with no history of cervical cancer. 33,34,37
Before the intervention, women were administered a pre-intervention survey to assess their levels of knowledge, attitudes, beliefs, and socio-demographics. 17,21,32 -34,36,37 Initially, participants received pre-intervention materials (brochures, video clips) that gave a brief introduction of the content to be covered during the health education sessions. 17,19,21 Eleven papers 17,19,21,24,28,32 -34,36,37,43 reported that the health education covered the information about the meaning of cervical cancer, cervical cancer cause, risk factors, signs and symptoms, prevention treatment, cervical cancer guidelines, screening tests, and early detection benefits. One paper 17 reported that women were told about screening costs and where screening services can be accessed. One paper 36 showed that women during intervention learned about cervical cancer screening barriers and stigma.
The intervention was delivered in group education session, 17,21,24,28,32,34,36 for duration ranged from 1 hour to 2 hours. 19,21,24,32,34,37 The education was delivered in English or native language 32,37 through lecture, 28,33,43 along with the use of the visual display to facilitate the easy understanding of content.28, 32 ,33 Immediately after the health education session, the post-intervention survey was administered. 32,34,36,37 and they received a guidebook, booklets, or informational sheets to help them recap what they had learned. 17,19,21,32,33 After the health education, the follow up was conducted in 3 monthly through telephone to provide navigation services. 21,24,36 The navigation services provided were linguistic, child care, transportation, screening appointment, reminder, follow-up calls, and cost-effective screening services, 21,28 consistent with the previous study findings. 42
Outcome Measures
The primary outcome after patient navigation intervention was the uptake of cervical cancer screening, 17,28,32,33,36 which is consistent with the previous study, 40 and secondary outcomes were changes in the level of knowledge, beliefs and attitude. 17,19,24,32,33,36,37 Participants were required to complete the screening tests within 6 months. 19,21,35
Effect of Patient Navigation
Nine papers 17,19,21,24,28,32,34 -36 showed that the intervention delivered by patient navigators resulted in higher rates of screening. The participation in the screening was influenced by involved community leaders in the intervention process, 24 availability of screening cost-effectiveness, 17 and provision of navigation services. 28 Six papers 17,19,24,32,36,37 showed that there was an increase in knowledge level after the intervention.
Limitations of the Study
Even though meta-analysis is important, data were synthesized qualitatively because of data heterogeneity. Most of the studies in this review were conducted in developed countries such as the United States of America, with very few from low-middle income countries, limiting the discussion of patient navigation applicability in low-middle income countries. Only studies available in the English language were included in this review because of lack of translation skills and limited fund, and studies without full texts were excluded due to lack of access, which both might have caused to miss important studies to contribute essential information in this review.
Implications
Despite limitations, the results of these studies have substantial implications for addressing cervical cancer screening hindrances. Many countries still experiencing a small proportion of cervical cancer screening uptake, the integration of patient navigation approach in their countries, and effective recruitment, training, and implementation of intervention as reported from this review will promote screening rates, strengthen follow-up care, and cost-effectiveness.
Conclusion
Three-day training of patient navigators by the healthcare profession is adequate to cover the basic information of CCS. Researchers should select the basics of CCS that of great importance for training patient navigators. Role-play, group discussion, visual materials, pre-reading enhance the learning environment for patient navigators. The group health education session facilitated by patient navigators coupled with navigation assistance resulted in a high screening rate and increased participant’s knowledge level.
Summary Box
What is already known on this subject?
Patient navigators are responsible for influencing women to uptake cervical cancer screening, as they provide emotional support, education, and navigation cares such as escorting and scheduling appointments.
What does this study add?
Three-day training of patient navigators is adequate to cover the basic information of CCS. Researchers should select the basics of CCS that of great importance for training patient navigators. The group education sessions facilitated by patient navigators coupled with navigation assistance result in a high screening and knowledge level.
Acknowledgments
Authors extend their gratitude to the school of nursing of Zhengzhou University in China and University of Dodoma in Tanzania for their encouragement. We also thank the individual contributions from Dr. Golden Masika and Vincent Bankanie who are the lecturers at the University of Dodoma for their guidance in research methodology.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Changying Chen  https://orcid.org/0000-0003-0139-6396
https://orcid.org/0000-0003-0139-6396
References
- 1. Rahman R, Clark MD, Collins Z, et al. Cervical cancer screening decentralized policy adaptation: an African rural-context-specific systematic literature review. Global Health Action. 2019;12(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shobeiri F, Javad MT, Parsa P. Effects of group training based on the health belief model on knowledge and behavior regarding the Pap smear test in Iranian women: a quasi-experimental study. Asian Pac J Cancer Prev. 2016;17(6):2871–2876. [PubMed] [Google Scholar]
- 3. Arbyn M, Weiderpass E, Bruni L, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8(2):e191–e203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bellhouse S, French DP, Mcwilliams L, Firth J, Yorke J. Are community-based health worker interventions an effective approach for early diagnosis of cancer? A systematic review and meta-analysis. Psycho-Oncology. 2018;27(4):1089–1099. [DOI] [PubMed] [Google Scholar]
- 5. Morrison PB. Preventing Cervical Cancer in Rural Tanzania: A Program Model for Health Worker Trainings. Texas Medical Center Dissertations; 2015. [Google Scholar]
- 6. Ali SF, Ayub S, Manzoor NF, et al. Knowledge and awareness about cervical cancer and its prevention amongst interns and nursing staff in tertiary care hospitals in Karachi, Pakistan. PLoS One. 2010;5(6):e11059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Urasa M, Darj E. Knowledge of cervical cancer and screening practices of nurses at a regional hospital in Tanzania. Afr Health Sci. 2011;11(1):48–57. [PMC free article] [PubMed] [Google Scholar]
- 8. OECD. “Screening, Survival and Mortality for Cervical Cancer,” in Health at a Glance 2015: OECD Indicators. OECD Publishing; 2015:1–220. [Google Scholar]
- 9. Lemp JM, De Neve JW, Bussmann H, et al. Lifetime prevalence of cervical cancer screening in 55 low-and middle-income countries. JAMA. 2020;324(15):1532–1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Getahun T, Kaba M, Derseh BT. Intention to screen for cervical cancer in Debre Berhan town, Amhara Regional State, Ethiopia: application of theory of planned behavior. J Cancer Epidemiol. 2020;2020:3024578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lyimo FS, Beran TN. Demographic, knowledge, attitudinal, and accessibility factors associated with uptake of cervical cancer screening among women in a rural district of Tanzania: three public policy implications. BMC Public Health. 2012;12(1):22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pernga P, Perng W, Ngoma T, et al. Promoters of and barriers to cervical cancer screening in a rural setting in Tanzania. Int J Gynaecol Obstet. 2013;123(3):221–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Szalacha LA, Kue J, Menon U. Knowledge and beliefs regarding breast and cervical cancer screening among Mexican-heritage Latinas. Cancer Nurs. 2017;40(5):420–427. [DOI] [PubMed] [Google Scholar]
- 14. Bateman LB, Blakemore S, Koneru A, et al. Barriers and facilitators to cervical cancer screening, diagnosis, follow-up care and treatment: perspectives of human immunodeficiency virus-positive women and health care practitioners in Tanzania. Oncologist. 2019;24(1):69–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tong EK, Nguyen TT, Lo P. Lay health educators increase colorectal cancer screening among Hmong Americans: a cluster randomized controlled trial. Cancer. 2017;123(1):98–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Braun KL, Thomas WL, Domingo JB, et al. Reducing cancer screening disparities in Medicare beneficiaries through cancer patient navigation. J Am Geriatr Soc. 2015;63(2):365–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Thompson B, Carosso EA, Jhingan E, et al. Results of a randomized controlled trial to increase cervical cancer screening among Rural Latinas. Cancer. 2017;123(4):666–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Battaglia TA, Bak S, Heeren T, et al. Boston Patient Navigation Research Program: the impact of navigation on time to diagnostic resolution after abnormal cancer screening. Cancer Epidemiol Biomarkers Prev. 2012;21(10):1645–1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Han H, Song Y, Kim M, et al. Breast and cervical cancer screening literacy among Korean American women: a community health worker-led intervention. Am J Public Health. 2017;107(1):159–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ma GX, Fang C, Tan Y, Feng Z, Ge S, Nguyen C. Increasing cervical cancer screening among Vietnamese Americans: a community-based intervention trial. J Health Care Poor Underserved. 2015;26(2):36–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schuster ALR, Frick HD, Huh BY, Kim KB, Kim M, Han HR. Economic evaluation of a community health worker-led health literacy intervention to promote cancer screening among Korean American women. J Health Care Poor Underserved. 2015;26(2):431–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hartzler AL, Tuzzio L, Hsu C, Wagner EH. Roles and functions of community health workers in primary care. Ann Fam Med. 2018;16(3):240–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Swider SM, Martin M, Lynas C, Rothschild S. Project MATCH: training for a promotora intervention. Diabetes Educ. 2010;36(1):98–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fleming K, Simmons VN, Christy SM, et al. Educating Hispanic women about cervical cancer prevention: feasibility of a promotora-led Charla intervention in a farmworker community. Ethn Dis. 2018;28(3):169–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Koskan AM, Friedman DB, Brandt HM, Walsemann KM, Messias DKH. Preparing promotoras to deliver health programs for Hispanic communities: training processes and curricula. Health Promot Pract. 2013;14(3):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Donovan JO, Donovan CO, Nagraj S. The role of community health workers in cervical cancer screening in low-income and middle-income countries: a systematic scoping review of the literature. BMJ Glob Health. 2019;4(3):e001452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ngoma T, Mandeli J, Holland JF. Downstaging cancer in rural Africa. Int J Cancer. 2015;136(12):2875–2879. [DOI] [PubMed] [Google Scholar]
- 28. Dunn SF, Lofters AK, Ginsburg OM, et al. Cervical and breast cancer screening after CARES: a community program for immigrant and marginalized women. Am J Prev Med. 2017;52(5):589–597. [DOI] [PubMed] [Google Scholar]
- 29. Freeman HP, Rodriguez RL. History and principles of patient navigation. Cancer. 2011;117(suppl. 15):3537–3540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. PRISMA. Transparent reporting of systematic reviews and meta-analyses [Internet]. PRISMA. 2009. Accessed May 06, 2021. http://www.prisma-statement.org [Google Scholar]
- 31. Saei M, Naz G, Kariman N, Ebadi A, Ozgoli G, Ghasemi V. Educational interventions for cervical cancer screening behavior of women: a systematic review. Asian Pac J Cancer Prev. 2018;19(4):875–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mojica CM, Morales-campos DY, Carmona CM, Ouyang Y. Breast, cervical, and colorectal cancer education and navigation: results of a community health worker intervention. Health Promot Pract. 2015;17(3):353–363. [DOI] [PubMed] [Google Scholar]
- 33. Wong CL, Choi KC, Law BMH, Chan DNS, So WKW. Effects of a community health worker-led multimedia intervention on the uptake of cervical cancer screening among South Asian women: a pilot randomized controlled trial. Int J Environ Res Public Health. 2019;16(17):3072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mbachu C, Dim C, Ezeoke U. Effects of peer health education on perception and practice of screening for cervical cancer among urban residential women in South-East Nigeria: a before and after study. BMC Women’s Health. 2017;17(41):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Temel AB, Dağhan Ş, Kaymakçı Ş, Dönmez RÖ, Arabacı Z. Effect of structured training programme on the knowledge and behaviors of breast and cervical cancer screening among the female teachers in Turkey. BMC Women’s Health. 2017;17(123):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rosser JI, Njoroge B, Huchko MJ. Changing knowledge, attitudes, and behaviors regarding cervical cancer screening: the effects of an educational intervention in Rural Kenya. Patient Educ Couns. 2015;98(7):884–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Molokwu J, Penaranda E, Flores S, Shokar NK. Evaluation of the effect of a promotora-led educational intervention on cervical cancer and human papillomavirus knowledge among predominantly Hispanic primary care patients on the US-Mexico border. J Cancer Educ. 2015;31(4):742–748. [DOI] [PubMed] [Google Scholar]
- 38. Cuesta-Briand B, Bessarab D, Shahid S, Thompson SC. “Connecting tracks”: exploring the roles of an aboriginal women’s cancer support network. Health Soc Care Community. 2016;24(6):779–788. [DOI] [PubMed] [Google Scholar]
- 39. Ely GE, White C, Jones K, et al. Cervical cancer screening: exploring Appalachian patients’ barriers to follow-up care. Soc Work Health Care. 2014;53(2):83–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Roland KB, Milliken EL, Rohan EA, et al. Use of community health workers and patient navigators to improve cancer outcomes among patients served by federally qualified health centers: a systematic literature review. Health Equity. 2017;1(1):61–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Giese-Davis J, Bliss-Isberg C, Wittenberg L, et al. Peer-counseling for women newly diagnosed with breast cancer: a randomized community/research collaboration trial. Cancer. 2016;122(15):2408–2417. [DOI] [PubMed] [Google Scholar]
- 42. Freund KM. Implementation of evidence-based patient navigation programs. Acta Oncol. 2017;56(2):123–127. [DOI] [PubMed] [Google Scholar]
- 43. Bayık Temel A, Dağhan Ş, Kaymakçı Ş, Öztürk Dönmez R, Arabacı Z. Effect of structured training programme on the knowledge and behaviors of breast and cervical cancer screening among the female teachers in Turkey. BMC Women’s Health. 2017;17(1):123. [DOI] [PMC free article] [PubMed] [Google Scholar]