Prone position quickly imposed as a cornerstone in the management of patients with acute respiratory distress syndrome (ARDS) induced by coronavirus disease 2019 (COVID-19) [1, 2]. The response to prone position, in terms of oxygenation and respiratory mechanics, would differ according to the potential for lung recruitment in supine position in COVID-19-ARDS [3]. Recruitment-to-inflation ratio (R/I), which is measurable with almost all modern respirators, allows, at bedside, the distinction between patients with a low or high potential for lung recruitment [4], including in those with COVID-19-ARDS [5]. This tool may henceforth help clinicians to set adequate positive end-expiratory pressure (PEEP) levels in ARDS [4]. Although not yet studied, the effects of other ventilatory strategies in ARDS should also depend on the R/I. Therefore, we conducted a prospective observational study to assess the effect of prone position in COVID-19-ARDS on respiratory mechanics and oxygenation according to the R/I ratio.
Consecutive sedated and curarized adult patients with moderate-to-severe COVID-19-ARDS in whom prone position was decided were included. In the absence of universally validated cut-off value, the median R/I ratio of the cohort was used to classify patients as high and low recruiters. Measurements (Supplementary Materials), including R/I, accounting for the presence of complete airway closure, were performed just before, 2 ± 0.5 h after prone positioning, and 2 ± 0.5 h after supine repositioning.
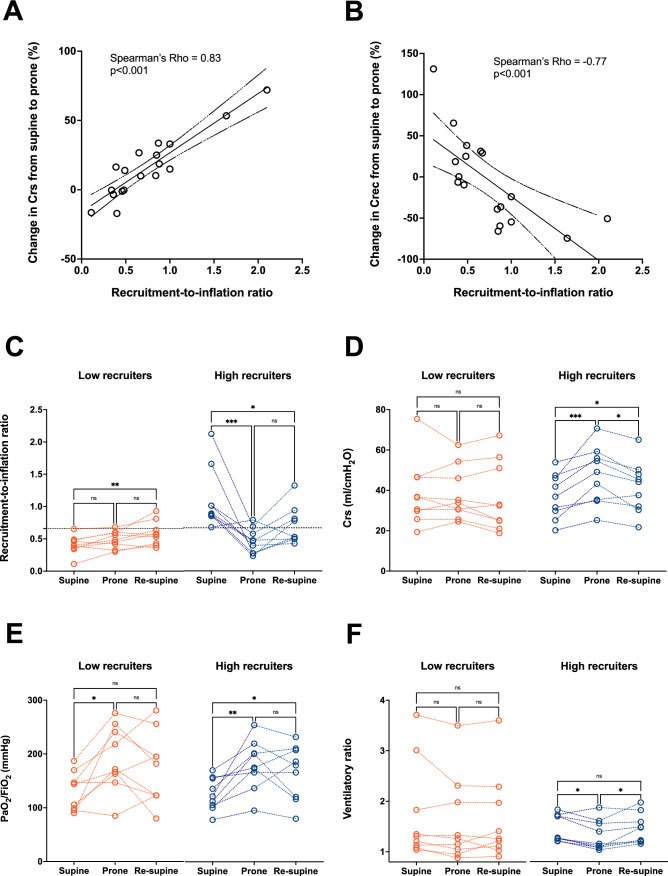
A total of 18 patients (age: 63 [59–69] years; sex ratio: 1.6) were included (Supplementary Table S1). Relative changes of the compliance of both the respiratory system (Crs) and the recruited lung (Crec) from supine to prone position were strongly correlated (positively and negatively, respectively) with the R/I at baseline (Fig. 1A, B). The median R/I was 0.66 [0.4–0.91], separating low (R/I: 0.4 [0.35–0.49]) and high (R/I: 0.88 [0.84–1.32]) recruiters. Baseline characteristics did not significantly differ between low and high recruiters, except for the recruited volume, Crec and PEEP-induced increase in oxygenation (Supplementary Table S1). As compared to baseline, turned to prone position, high recruiters exhibited a reduction in R/I together with better Crs, oxygenation and ventilatory ratio when low recruiters had better oxygenation only (Fig. 1C–F). Moved back to supine position, oxygenation and Crs were kept improved, whilst low recruiters did not change.
Fig. 1.
Effects of prone positioning on lung mechanics and oxygenation according to recruitment-to-inflation ratio. The continuous line shows the linear regression (with 95% confidence intervals in dashed lines) between recruitment-to-inflation (R/I) ratio in supine position and changes in compliance of the respiratory system (Crs) at low positive end-expiratory pressure (PEEP) (Panel A) and changes in compliance of the recruited lung (Crec) (Panel B) in 18 patients with COVID-19-related acute respiratory distress syndrome. For low recruiters (n = 9, orange circle) and high recruiters (n = 9, blue circle) defined by R/I under or above the median value of the cohort (0.66), respectively, individual values of R/I (Panel C), Crs at low PEEP (Panel D), arterial partial pressure of oxygen to fraction of inspired oxygen (PaO2/FiO2, Panel E) and ventilatory ratio (Panel F) are reported in supine position, prone position and after repositioning in the supine position (re-supine). *P < 0.05; **P < 0.01; ***P < 0.001 in one-way ANOVA for repeated measures or Friedman test, as appropriate
In addition to confirming benefits on oxygenation of prone position in COVID-ARDS [2], we found that the higher the potential for lung recruitment in supine position, the greater the improvement in respiratory mechanics in prone position. The increase in Crs along with the reduction in ventilatory ratio and the gain in oxygenation suggests a true lung recruitment in high recruiters in prone position, also explaining the decrease in R/I and Crec. The fact that prone has a major impact on R/I should prompt physician to reassess this parameter after each change in position, notably if it used to individualize PEEP levels. Finally, our results suggest that prone position has differential effects in low and high recruiters as both oxygenation and respiratory mechanics remained improved after repositioning in supine only in high recruiters. Thus, prone position may have greater physiological benefits for high recruiters with COVID-19-ARDS.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
None.
Declarations
Conflicts of interest
The authors declare they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of our institutional research committee and with the 1964 Declaration of Helsinki and its later amendments. This study was approved by our institutional review board (Comité d’Ethique du CHU de Lyon).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med. 2021;47:60–73. doi: 10.1007/s00134-020-06294-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Langer T, Brioni M, Guzzardella A, et al. Prone position in intubated, mechanically ventilated patients with COVID-19: a multi-centric study of more than 1000 patients. Crit Care. 2021;25:128. doi: 10.1186/s13054-021-03552-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L, Camporota L. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 2020;46:1099–1102. doi: 10.1007/s00134-020-06033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen L, Del Sorbo L, Grieco DL, Junhasavasdikul D, Rittayamai N, Soliman I, Sklar MC, Rauseo M, Ferguson ND, Fan E, Richard JM, Brochard L. Potential for lung recruitment estimated by the recruitment-to-inflation ratio in acute respiratory distress syndrome. A Clinical Trial. Am J Respir Crit Care Med. 2020;201:178–187. doi: 10.1164/rccm.201902-0334OC. [DOI] [PubMed] [Google Scholar]
- 5.Stevic N, Chatelain E, Dargent A, Argaud L, Cour M, Guérin C. Lung recruitability evaluated by recruitment-to-inflation ratio and lung ultrasound in COVID-19 acute respiratory distress syndrome. Am J Respir Crit Care Med. 2021;203:1025–1027. doi: 10.1164/rccm.202012-4447LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.