Abstract
Objective
To evaluate whether a 4-month physical activity (PA) group program and visits to sociocultural organizations improve emotional state, social support levels and health-related quality of life in elderly individuals with depression and/or anxiety and/or loneliness.
Methods
This will be a multicentre, randomized, two-group clinical trial with a 1-year follow-up. Participants will be 150 primary care patients aged >64 years allocated equally to a control group and an intervention group. Inclusion criteria are Beck Depression Inventory (BDI-II) score ≥14 and/or General Anxiety Disorder (GAD-7) scale score ≥10 and/or Duke-UNC-11 scale score ≥32. The intervention group will participate in a 4-month group PA program. The program will comprise two walks per week and a monthly visit to a sociocultural facility.
Results
Measured outcomes are clinical remission of depression (BDI-II score <14) and anxiety (GAD-7 scale score <10), improved social support (reduction in DUKE-UNC-11 score), improved quality of life and/or response to the intervention at 4 and 12 months post-intervention. Intervention satisfaction and adherence and post-intervention links with sociocultural organizations will also be assessed.
Conclusion
The findings could encourage the provision of activity-based community interventions for older individuals.
Keywords: Physical activity, primary care, elderly, anxiety, depression, social problem, loneliness
Trial registration
Jordi Gol i Gurina Foundation Protocol Record CEI 19/031-P (27/03/2019)
ClinicalTrials.gov Identifier: NCT04072185. Date of Registration: 28/08/2019 https://clinicaltrials.gov/ct2/show/NCT04072185?cond=physical+activity+as+a+measure&cntry=ES&draw=2&rank=1
Introduction
Background
In 2020, the percentage of people aged >64 years in Spain was 19.8% 1 (9.28 million) and this figure is expected to increase to 25.2% in 2033, according to the National Statistics Institute. 2 Promoting longer, healthier lives is now a primary priority for health care researchers.
Older people are more vulnerable to loneliness and social isolation. 3 Research has linked social isolation and loneliness with higher risks for a variety of physical and mental conditions. 4
The prevalence of chronic or frequent loneliness in Spain has been estimated as 11.5% for individuals aged ≥60 years. 5 According to the 2017 European Health Survey in Spain carried out by the Ministry of Health, Consumer Affairs and Social Welfare, the prevalence of depression and chronic anxiety was, respectively, 10.64% and 8.25% in participants aged 65 to 74 years, 13.73% and 9.49% for those aged 75 to 84 years and 11.36% and 6.68% for those aged >85 years. 6
Health-related quality of life (HRQoL) is defined as the perception of the physical, mental and social effects of disease on well-being. 7 HRQoL is considered an important health outcome; an essential public health measure of physical and social functioning, mental health and well-being; and a useful way of evaluating population-based intervention programs. 8 Poor perceived HRQoL is associated with older age, lower social class, lack of social support, high levels of depression, low self-esteem, sex (female), chronic medical conditions, high body mass index and sedentary lifestyle. 9
Several studies have shown that physical activity (PA) is one of the most important resources to improve health 10 and HRQoL 11 in older adults, at both the physical and emotional levels. 12 Numerous studies suggest that PA and leisure activities reduce loneliness, 13 depression 14 and anxiety, 15 and are associated with improved mental well-being. 16 Review studies suggest that social activity group interventions that target specific groups can alleviate social isolation and loneliness, 17 depression18,19 and psychological distress among older adults. 20 Such interventions can also improve well-being and mental health by creating and consolidating social support networks, which enable the development of bonds between individuals through the exchange of feelings, thoughts and experiences. 21
The large variability in aerobic PA intervention protocols may explain why outcomes regarding the relationship between aerobic PA and psychological well-being and HRQoL are inconsistent. More research is needed to confirm the effect of aerobic PA on psychological well-being and HRQoL, and to determine how PA can be encouraged. The aim of this study is to evaluate whether a 4-month PA group program and a visit to sociocultural organizations can improve the emotional state, social support level and HRQoL of a sample of individuals aged >64 years with anxiety and/or depression and/or lacking social support. We will also examine whether the intervention group continue to be more active than the control group after the intervention. To our knowledge, this issue has not been previously investigated.
Hypotheses
The following hypotheses will be tested: 1) PA will improve emotional state, level of social support and quality of life of participants aged >64 years who are experiencing anxiety and/or depression and/or lack social support; 2) The intervention group will be more active than the control group; 3) The intervention group will remain more active once the intervention is over, and will maintain PA for an extended period; 4) The intervention group will develop more links with sociocultural organizations than the control group.
Objectives
The study objectives are as follows:
To evaluate whether PA improves the emotional state, social support and quality of life of a sample of people aged >64 years experiencing anxiety and/or depression and/or lacking in social support.
To evaluate whether participation in a 4-month PA program prolongs improvements in emotional state, level of social support and quality of life in a sample of people aged >64 years experiencing anxiety and/or depression and/or social isolation and/or loneliness, by assessing participants 12 months after the intervention.
To measure whether the adherence to PA is maintained at 12 months after the intervention.
To measure whether the intervention group develops links to sociocultural organizations and whether these links are maintained.
Methods/design
This will be a multicentre randomized clinical trial involving two groups, with a follow-up period of 1 year. The study population is patients aged >64 years assigned to three primary care teams (PCTs) in different locations: Sant Joan de Vilatorrada (12,721 patients), Súria (8956 patients) and Manresa (23,351 patients). These areas were chosen to incorporate patients living in urban, semi-urban and rural areas.
The inclusion criteria will be as follows: Meets the criteria of depression or anxiety at the time of the study (Beck Depression Inventory [BDI-II] score ≥14 and/or General Anxiety Disorder scale [GAD-7] score ≥10 and/or DUKE-UNC-11 scale score <28); possibility of follow-up for 1 year by the same PCT; ability to read and write in Spanish or Catalan; participants can be sedentary or active; previous PA level will not be taken into account.
The following exclusion criteria will be used: Diagnosis of dementia or moderate cognitive impairment; higher level of depression (BDI-II score ≥28); dependency disorders owing to the abuse of alcohol or other drugs; currently receiving psychological therapy from a mental health clinic; physical illness at an advanced stage (terminal cancer, arthritic pathology with severe functional limitation, advanced dementia that makes social interaction difficult); any temporary physical or mental impediment to being able to walk 1 hour a day, 2 days a week; failure to sign the consent form.
Intervention
The intervention group will participate in a group PA program for 4 months consisting of walking 2 days a week. As the study participants are elderly people, the initially proposed PA is aerobic and of low intensity (up to 3 metabolic equivalents (METs)).22 The intensity will be gradually increased to a moderate or vigorous level, according to the capabilities of each participant.
A doctor and a nurse will accompany the group and supervise participants, advising about the walking pace and the distance to be covered. They will also control the activity intensity using the conversation test, according to participants’ physical capacities and underlying pathologies. The conversation test allows the control of activity intensity according to the perception of the person performing the activity. The test classifies the intensity of effort as intense, moderate or light, and relates this intensity to the ability to engage in a conversation during exercise (light: person can sing or talk non-stop; moderate: breathing is comfortable enough to allow conversation; intense: person cannot talk while exercising). One of the two companions will walk in front with the participants in better physical condition and the other companion will remain at the back with the rest of the participants. A leader will be chosen from among the participants to support the companions.
The distance travelled is not the main objective of the study; the objective is to foster social relationships with participants and enable their enjoyment of the outdoor activity.
Participants will always be accompanied by a doctor and a nurse who will encourage group cohesion and empower the participants. Each day, one participant will choose the walk and lead the excursion. We aim to use empowerment to encourage the active participation of the individuals and the group, and to promote social cohesion. 23
To unite the group and discourage dropout, a voluntary WhatsApp group will be created to remember the outings, share photographs that are taken during the walks, periodically praise the participants’ achievements and enquire about those who do not attend or are ill. If a participant consistently fails to show up for the walks and does not respond to WhatsApp messages, the doctor will phone them to ask how they are.
Following the studies of Rejeski and Mihalko 24 we wish to emphasize that PA programs involve much more than the performance of simple physical acts. Indeed, it seems very reasonable to infer that how programs are run and the input that participants have in their design are as critical, if not more important, to quality-of-life outcomes than meeting specific criteria for frequency, intensity and duration of PA.
Each month, as part of the walk, participants will visit a council-owned sociocultural facility to encourage a connection with the community. These visits will consist of a presentation about the centre, the activities that take place there and how to access those activities.
The control group will receive usual care in primary care centres. The usual care in primary care centres comprises regular control visits for chronic diseases and spontaneous visits for acute diseases.
Ethics approval and consent to participate
In accordance with Law 14/2007 of 3 July on biomedical research and human rights (BOE of 4 July 2007), all patients recruited to a study must be informed verbally and in writing of the objectives, methodology, tests and interventions that they may receive if they agree to participate. Only those who give their informed consent in writing will be included in the study. The document explaining the study will be written in easily understandable language. The study protocol was approved by the IDIAPJGol Clinical Research Ethics Committee (CEI 19/031-P). The researchers undertake to maintain the confidentiality of the data. If the intervention is shown to be effective, the control group will receive the same intervention once the study has ended.
Outcomes
Variables and measurement methods
Primary outcomes
Clinical remission of depression and/or response to the intervention once the intervention has been completed, at 4 months after the start of the study. Clinical remission is considered as BDI-II score <14; response to the intervention is defined as a reduction in the baseline score. 25 The BDI-II 26 is a multiple-choice self-report questionnaire comprising 21 items. Each question has four possible responses, according to the severity of the symptoms (from 0 to 3; producing a total from 0 to 63). The Spanish version of the BDI-II, developed by Sanz et al., 27 was used.
Remission of clinical anxiety and/or response to the intervention once the intervention has ended, 4 months after the start of the study. Clinical remission is considered as a GAD-7 scale score <10 points; response to the intervention is defined as a reduction in the score compared with the baseline. The GAD-7 scale 28 is a simple, self-administered test. Participants are asked to rate the frequency of seven anxiety symptoms over the preceding 2 weeks on a 4-point Likert scale of 0 to 3 (‘not at all’, ‘several days’, ‘more than half of the days’ and ‘almost every day’), giving a maximum score of 21. A score ≥10 indicates anxiety disorders, with a sensitivity of 89% and a specificity of 82%. The scale has been validated in Spanish by García-Campayo et al. 29
Improvements in social support once the intervention has finished, 4 months after the start of the study. Improvements in social support are defined as a reduction in the DUKE-UNC-11 Functional Social Support Questionnaire score with respect to the baseline, and good social support (score <32 points). The DUKE-UNC-11 was designed by Broadhead et al. 30 to measure perceived functional social support and validated for the Spanish population by Bellón Saameño et al. 31 It is a self-administered 11-item instrument and responses are scored on a 5-point Likert-type scale. The scale is simple and brief and evaluates perceived social support, confidential social support (the possibility of having people to communicate with) and affective social support (expressions of love, affection and empathy). In the Spanish version, a cutoff point was chosen at the 15th percentile, which corresponds to a score <32, to divide participants into two groups (normal or low support). 31
Improved quality of life once the intervention has been completed, 4 months after the start of the study. Quality-of-life improvement is considered as a reduction in the EuroQol questionnaire (EQ-5D) score with respect to baseline. The EQ-5D is a generic instrument that measures HRQoL and can be used both for healthy individuals (general population) and patients with different pathologies. The EQ-5D is self-administered and assesses health status descriptively on five health dimensions (mobility, personal care, daily activities, pain/discomfort, and anxiety/depression) and three levels of severity (without problems, some problems or moderate problems, and severe problems). The EQ-5D also uses a vertical 20-cm visual analogue scale for general assessment, which ranges from 0 (lowest imaginable health status) to 100 (highest imaginable health status). The participants must mark the point on the vertical line that most reflects their assessment of their global health status that day. 32 A Spanish version of the scale has been validated by Badia et al. 33
Secondary outcomes
Clinical remission from depression and/or response to the intervention at 12 months.
Clinical remission from anxiety and/or response to the intervention at 12 months.
Improvements in social perceptions/situations (DUKE-UNC-11 Functional Social Support Questionnaire) at 12 months.
Improved quality of life, as measured by the EQ-5D, at 12 months.
- The following outcome variables will measure feasibility in the intervention group:
- Satisfaction with the intervention: A patient satisfaction survey will be carried out at the end of the intervention. The survey comprises five items and responses are scored on a 5-point Likert scale.
- Adherence to the intervention: The number of sessions attended will be recorded for each of the intervention group patients. Adherence to the intervention will be defined as attendance at 75% or more of the sessions.
- Adherence to PA post-intervention as assessed by the VREM questionnaire (a shorter version of the Spanish version of the Minnesota Leisure Time Physical Activity Questionnaire). Assessments will be made at 0, 4 and 12 months. The VREM assesses the quantity and quality of the PA carried out during leisure time and household chores during a year. The scale assess six activities: walking, working in the garden, playing sports or dancing, climbing stairs, going shopping on foot and cleaning the house. The first five activities are recorded for the last month and the latter for a typical week. Respondents rate those activities that may show seasonal variability (e.g. because of climate or holidays) in terms of months per year, so that a total annual estimate can be calculated. The VREM categorizes people as very active (energy expenditure >5000 MET-minutes/14 days), active (energy expenditure between 3000 and 4999 MET-minutes/14 days), moderately active (energy expenditure between 1250 and 2999 MET-minutes/14 days) and sedentary (energy expenditure <1250 MET-minutes/14 days). Ruiz-Comellas et al. 34 have validated the shorter Spanish version of this questionnaire for men and women aged >50 years.
Ties to sociocultural organizations once the intervention has been completed. Assessments will be made at 0, 4 and 12 months. The evaluation will be conducted by checking registration for courses or activities that take place in local sociocultural centres.
Possible confounding factors or effect modifiers
The following variables will be assessed as possible confounders or effect modifiers.
Pharmacological treatment. The defined daily dose will be calculated for each active ingredient taken in the follow-up period, taking into account number of days, dose dispensed and the route of drug administration. Active ingredients are defined as any antidepressant or anxiolytic medications.
Participation in other mental health therapies involving a psychologist or a psychiatrist. Patients receiving treatment at a referring mental health centre will be excluded.
Prior participation in some form of PA on a regular basis (recorded as either yes or no).
Sociodemographic variables
The following sociodemographic variables will be measured: sex, age, marital status, living alone (yes/no) and educational level (no education/did not finish secondary school/finished secondary school/higher education). The reference PCT will be categorized as rural (assigned to a general practitioner’s office), semi-urban (assigned to a PCT in an area with a population <15,000), or urban (assigned to a PCT in an area with a population ≥15,000).
Participant timeline
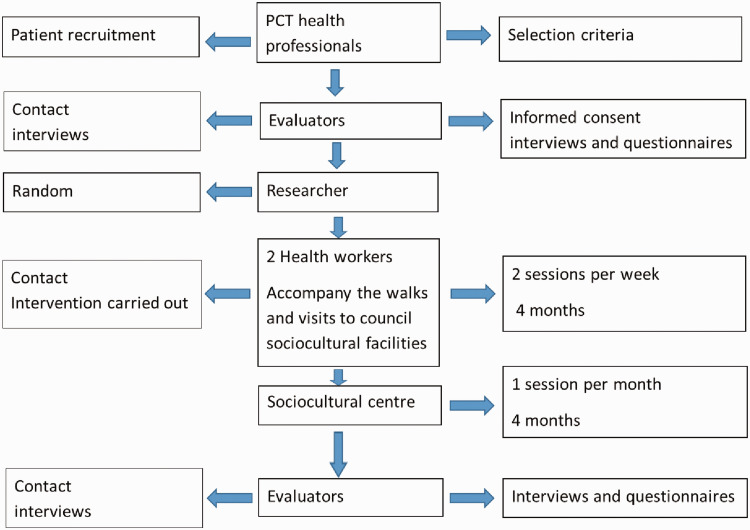
Several different types of professionals will participate in the fieldwork (Figure 1). The doctor and/or nurse to whom the patient is assigned will act as professional recruiters. Evaluators will carry out baseline interviews at 4 and 12 months, but will be blinded regarding patient group assignment. The researcher in charge of the random allocation of patients is not linked to any PCT. He will assess the inclusion and exclusion criteria and perform the random allocation once all the patients in the required sample have consented to participate. There will be two professionals for each PCT, who will accompany the group on their walks. The study will also involve professionals from the sociocultural centres.
Figure 1.
Flow chart of the intervention.
PCT, primary care team.
An external evaluator will be in charge of collecting the results of the previously mentioned paper-based self-administered questionnaires. The questionnaires will be kept in a safe place to which only the evaluator has access. The test evaluator will read the questionnaires using an automatic reader and TeleForm Elite v 8.2 reading software (OpenText, Waterloo, ON, Canada).
Sample size
We calculated the sample size for independent groups required to detect a 2-point difference in the average BDI-II and GAD-7 scores and a score of 7 points on the DUKE-UNC-11 Functional Social Support Questionnaire. A control will be assigned for each case, assuming a statistical power of 80% and a confidence interval of 95%. Between 146 and 162 patients will be needed. To compensate for eventual dropouts, 180 patients will be selected and assigned to three groups of 60 patients in each PCT. Consecutive sampling will be used for recruitment in each PCT. Of these patients, half will be assigned to the control group and half to the intervention group.
Recruitment
The professionals participating in the study will consult the Historia Clínica Informatitzada de Catalunya (Computerized Medical Record of Catalonia) database using the consultation forms of their assigned patients to obtain a list of patients who meet the inclusion criteria (with an active diagnosis of depression or anxiety and little social support). Subsequently, the doctor and/or nurse responsible for the patients will review the list and confirm the selection of patients with active diagnoses, taking into account the inclusion and exclusion criteria. These patients will then be invited to complete the questionnaires. Their responses will be used to generate a final list of included patients, taking into account the cutoff points of the scales (BDI-II ≥14 and/or GAD ≥10 and/or DUKE-UNC-11 ≥32).
Methods: assignment of interventions (for controlled trials)
Allocation
The researcher responsible for randomly assigning patients to the different groups is not associated with any of the PCTs. PASW Statistics for Windows, Version 18.0 (SPSS Inc., Chicago, IL USA) will be used to randomly allocate participants to the control and intervention groups. Patients with depression, anxiety and little social support will be equally assigned between the intervention and control groups. We will also perform stratified randomization according to age and sex to increase the generalizability of the results.
Methods: data collection, management and analysis
Initially, the sociodemographic characteristics of the two groups will be ascertained. For the descriptive analyses of qualitative and quantitative variables and percentages, the average and standard deviation, or median, range and 25th to 75th percentiles, will be used.
Prior to the intervention, baseline scores on the selected questionnaires after patient randomization will be compared to confirm that there are no significant differences. After the intervention, the average scores on the different questionnaires for both groups and for different post-intervention periods will be independently compared using the Student t-test for paired samples (for normal distributions) or the Mann–Whitney U test (for non-normal distributions). We will dichotomize the scores for anxiety, depression and social support, taking into account the previously mentioned cutoffs. Differences with p < 0.05 will be considered statistically significant. PASW Statistics for Windows, Version 18.0 (SPSS Inc.) will used for statistical analysis. Data for participants lost to follow-up or who have dropped out will be analysed on an intention-to-treat basis.
Discussion
This article describes a study protocol to investigate the effectiveness of a group PA program. The main objective is to determine if this program improves psychological mood (anxiety and depression), social support and quality of life in a sample of people aged >64 years with anxiety and/or depression and/or lacking social support. A secondary objective is to promote an active lifestyle and socialization in older people. Social support especially protects elderly people from loneliness and can have a beneficial effect on mental health problems.18,20 Several studies show that PA reduces loneliness and is associated with better mental health status.13,15,16,19
Our findings may encourage implementation of community interventions for older individuals. This population is more susceptible to social isolation, anxiety and depression, for which medical treatments are not always effective. If we can demonstrate the effectiveness of this intervention, it could be incorporated into the social prescription services available in primary care centres. Previous studies have shown that PA has a positive effect on anxiety, depression and quality of life.12,19 It has also been found that social support interventions promote change and maintenance of PA through the creation of social networks, which generate supportive relationships that promote behavioural change. 35
A major strength of our study is that the naturalistic design is as close as possible to the usual clinical practice in primary care. Therefore, this intervention could be easily implemented in primary care settings with minimal organizational and structural modifications.
One anticipated limitation is that the participants will be elderly people with anxiety and/or depression and other comorbidities, particularly musculoskeletal problems, which may limit their PA and thus their adherence to the intervention. Additionally, the generalizability of the results may be limited, as the sample includes only elderly patients with no functional limitations and able to walk 1 hour a day for 2 days a week; individuals with poorer functional status will be excluded. Another limitation is that PA will be assessed using the validated VREM. As with any self-report PA measure, the VREM is prone to measurement errors, probably stemming from memory biases, social desirability bias and errors of item interpretation. 36 The VREM, therefore, has disadvantages compared with objective methods. However, the Minnesota Leisure Time Physical Activity Questionnaire has been evaluated in several studies, 37 including studies of Spanish participants. 38
Acknowledgements
We would like to thank the Unitat de Suport a la Recerca de Catalunya Central of the Institut Català de la Salut for their support.
Footnotes
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This research received the following funding: Prize for the Best Family Doctor’s Research Project, awarded by the 40th SEMERGEN National Congress, Palma, Spain (20 October 2018), and the Second Prize Aid for Research and Innovation, awarded by the Institut Català de la Salut in central Catalonia (15 December 2017).
ORCID iDs: Anna Ruiz-Comellas https://orcid.org/0000-0002-2848-2326
Josep Vidal-Alaball https://orcid.org/0000-0002-3527-4242
References
- 1.Fernández R. Población de España mayor de 65 años en el 2020. Madrid. Niels Terfehr. Available from: https://es.statista.com/estadisticas/630678/poblacion-de-espana-mayor-de-65-anos/ (2020).
- 2.Instituto Nacional de Estadística. Gregorio Izquierdo. Proyecciones de población mayor de 65 en España. Available from: https://www.ine.es/prensa/pp_2018_2068.pdf (2018).
- 3.Dury R. Social isolation and loneliness in the elderly: an exploration of some of the issues. Br J Community Nurs 2014; 19: 125–128. Available from: http: //www.magonlinelibrary.com/doi/10.12968/bjcn.2014.19.3.125 [DOI] [PubMed] [Google Scholar]
- 4.Cacioppo JT, Cacioppo S. Older adults reporting social isolation or loneliness show poorer cognitive function 4 years later. Evid Based Nurs 2014; 17: 59–60. Available from: https://ebn.bmj.com/lookup/doi/10.1136/eb-2013-101379 [DOI] [PubMed] [Google Scholar]
- 5.Yang K, Victor C. Age and loneliness in 25 European nations. Ageing Soc 2011; 31: 1368–1388. Available from: https://www.cambridge.org/core/product/identifier/S0144686X1000139X/type/journal_article [Google Scholar]
- 6.Ministerio de Sanidad, Consumo y Bienestar Social. Encuesta Nacional de Salud. España 2017. Madrid. Available from: https://www.mscbs.gob.es/estadEstudios/estadisticas/encuestaNacional/encuestaNac2017/ENSE2017_notatecnica.pdf (2018).
- 7.Urzúa MA. Calidad de vida relacionada con la salud: elementos conceptuales. Rev Med Chil 2010; 138: 358–365. [PubMed] [Google Scholar]
- 8.Romero M, Vivas-Consuelo D, Alvis-Guzman N. Is health related quality of life (HRQoL) a valid indicator for health systems evaluation? Springerplus 2013; 2: 664. Available from: https://springerplus.springeropen.com/articles/10.1186/2193-1801-2-664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lubetkin EI, Jia H, Franks P, et al. Relationship among sociodemographic factors, clinical conditions, and health-related quality of life: examining the EQ-5D in the U.S. general population. Qual Life Res 2005; 14: 2187–2196. Available from: http: //link.springer.com/10.1007/s11136-005-8028-5 [DOI] [PubMed] [Google Scholar]
- 10.Delle A, Bassi M, Boccaletti ES, et al. Promoting well-being in old age: the psychological benefits of two training programs of adapted physical activity. Front Psychol 2018; 9: 828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koolhaas CM, Dhana K, Van Rooij F, et al. Physical activity types and health-related quality of life among middle-aged and elderly adults: the Rotterdam study. J Nutr Heal Aging 2018; 22: 246–253. [DOI] [PubMed] [Google Scholar]
- 12.Mochcovitch MD, Deslandes AC, Freire RC, et al. The effects of regular physical activity on anxiety symptoms in healthy older adults: a systematic review. Rev Bras Psiquiatr 2016; 38: 255–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lampinen P, Heikkinen RL, Kauppinen M, et al. Activity as a predictor of mental well-being among older adults. Aging Ment Health 2006; 10: 454–466. [DOI] [PubMed] [Google Scholar]
- 14.Ku PW, Steptoe A, Liao Y, et al. Prospective relationship between objectively measured light physical activity and depressive symptoms in later life. Int J Geriatr Psychiatry 2018; 33: 58–65. [DOI] [PubMed] [Google Scholar]
- 15.Guszkowska M. Effects of exercise on anxiety, depression and mood. Psychiatr Pol 2004; 38: 611–620. [PubMed] [Google Scholar]
- 16.Sarró-Maluquer M, Ferrer-Feliu A, Rando-Matos Y, et al. Depresión en ancianos: prevalencia y factores asociados [Depression in the elderly: prevalence and associated factors]. Semergen 2013; 39: 354–360. [DOI] [PubMed] [Google Scholar]
- 17.Cattan M, White M, Bond J, et al. Preventing social isolation and loneliness among older people: a systematic review of health promotion interventions. Ageing Soc 2005; 25: 41–67. [DOI] [PubMed] [Google Scholar]
- 18.Prince MJ, Harwood RH, Blizard RA, et al. Social support deficits, loneliness and life events as risk factors for depression in old age: The Gospel Oak Project VI. Psychol Med 1997; 27: 323–332. [DOI] [PubMed] [Google Scholar]
- 19.McHugh JE, Lawlor BA. Exercise and social support are associated with psychological distress outcomes in a population of community-dwelling older adults. J Heal Psychol 2012; 17: 833–844. [DOI] [PubMed] [Google Scholar]
- 20.Thorsteinsson EB, Brown RF. Mediators and moderators of the stress or fatigue relationship in nonclinical samples. J Psychosom Res 2009; 66: 21–29. [DOI] [PubMed] [Google Scholar]
- 21.Guallar-Castillón P, Peralta PSO, Banegas JR, et al. Actividad física y calidad de vida de la población adulta mayor en España. Med Clin (Barc) 2004; 123: 606–610. [DOI] [PubMed] [Google Scholar]
- 22.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sport Exerc 2011; 43: 1575–1581. [DOI] [PubMed] [Google Scholar]
- 23.Speer PW, Jackson CB, Peterson NA. The relationship between social cohesion and empowerment: support and new implications for theory. Heal Educ Behav 2001; 28: 716–732. Available from: http://journals.sagepub.com/doi/10.1177/109019810102800605 [DOI] [PubMed] [Google Scholar]
- 24.Rejeski WJ, Mihalko SL. Physical activity and quality of life in older adults. J Gerontol A Biol Sci Med Sci 2001; 56: 23–35. Available from: https://academic.oup.com/biomedgerontology/article-lookup/doi/10.1093/gerona/56.suppl_2.23 [DOI] [PubMed] [Google Scholar]
- 25.Sanz J, Gutiérrez S, Gesteria C, et al. Criterios y baremos para interpretar el “Inventario de depresión de Beck-II” (BDI-II). Behav Psychol/ Psicologia Conductual 2014; 22: 37–59. Available from: https://www.behavioralpsycho.com/wp-content/uploads/2019/08/03.Sanz_22-1oa.pdf [Google Scholar]
- 26.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio: TX, Psychological Corporation, 1996. [Google Scholar]
- 27.Sanz J, Garcia-Vera MP, Espinosa R, et al. Adaptación española del Inventario para la Depresión de Beck-II (BDI-II): 3. Propiedades psicométricas en pacientes con trastornos psicológicos. Clínica y Salud 2005; 16: 121–142. Available from: https://www.redalyc.org/articulo.oa?id=180616104001 [Google Scholar]
- 28.Spitzer RL, Kroenke K, Williams JBW, et al. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med 2006; 166: 1092–1097. [DOI] [PubMed] [Google Scholar]
- 29.García-Campayo J, Zamorano E, Ruiz MA, et al. The assessment of generalized anxiety disorder: psychometric validation of the Spanish version of the self-administered GAD-2 scale in daily medical practice. Heal Qual Life Outcomes 2012; 10: 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Broadhead WE, Gehlbach SH, De Gruy FV, et al. The Duke UNC functional social support questionnaire: measurement of social support in family medicine patients. Med Care 1988; 26: 709–723. [DOI] [PubMed] [Google Scholar]
- 31.Bellón Saameño JA, Delgado Sánchez A, Luna Del Castillo JD, et al. Validez y fiabilidad del cuestionario de apoyo social funcional Duke-UNC- 11[Validity and reliability of the Duke-UNC-11 Functional Social Support Questionnaire]. Aten Primaria 1996; 18: 153–163. [PubMed] [Google Scholar]
- 32.Brooks R. EuroQol: the current state of play. Health Policy 1996; 37: 53–72. Available from: https://linkinghub.elsevier.com/retrieve/pii/0168851096008226 [DOI] [PubMed] [Google Scholar]
- 33.Badia X, Roset M, Montserrat S, et al. La versión española del EuroQol: descripción y aplicaciones [The Spanish version of EuroQol: a description and its applications]. Med Clin (Barc) 1999; 112: 79–85. [PubMed] [Google Scholar]
- 34.Ruiz-Comellas A, Guillem P, Baena Díez JM, et al . Validación de una versión reducida en español del cuestionario de actividad física en el tiempo libre de Minnesota (VREM). Rev Esp Salud Pública 2012; 86: 495–508. [DOI] [PubMed] [Google Scholar]
- 35.Kahn EB, Ramsey LT, Brownson RC, et al. The effectiveness of interventions to increase physical activity. A systematic review. Am J Prev Med 2002; 22: 73–107. [DOI] [PubMed] [Google Scholar]
- 36.Loprinzi PD, Cardinal BJ. . Measuring children’s physical activity and sedentary behaviors. J Exerc Sci Fit 2011; 9: 15–23. [Google Scholar]
- 37.Goran M, Poehlman E. . Total energy expenditure and energy requirements in healthy elderly persons. Metabolism 1992; 41: 744–753. [DOI] [PubMed] [Google Scholar]
- 38.Elosua R, Marrugat J, Molina L, et al . Validation of the Minnesota Leisure Time Physical Activity Questionnaire in Spanish men. MARATHON Investig. Am J Epidemiol 1994; 139: 1197–1209. [DOI] [PubMed] [Google Scholar]