Abstract
Introduction
This study aimed to evaluate the parents’ willingness and attitudes concerning the COVID‐19 vaccine.
Method
This cross‐sectional study was performed using a self‐administered online survey, covering parents’ and their children's characteristics, parents’ willingness and attitudes towards the COVID‐19 vaccine. A total of 1035 parents participated.
Results
Analysis showed that 36.3% of parents were willing to have their children receive the COVID‐19 vaccine and that 59.9% were willing to receive it themselves. In addition, 83.9% were willing to have their children vaccinated with the COVID‐19 vaccine if the mortality rates associated with COVID‐19 in children increased following a mutation. After adjusting for significant variables, willingness to receive the COVID‐19 vaccine (AOR = 24.91; 95% CI = 10.93‐56.76), willingness for their children to participate in a COVID‐19 vaccine trial (AOR = 11.87; 95% CI = 2.41‐58.40] and advising others to receive the COVID‐19 vaccine [AOR = 7.82; 95% CI = 2.50‐24.49] were associated with greater parents’ willingness for their children to receive the COVID‐19 vaccine.
Conclusions
Parents’ willingness for their children to receive the COVID‐19 vaccine was low. The only characteristics of either parents or children found to affect the parents’ willingness for children to receive the COVID‐19 vaccine was the parents being healthcare workers. Parents’ willingness and positive attitudes towards the COVID‐19 vaccine are factors that increase acceptance of the COVID‐19 vaccine for their children.
What's known
At the beginning of the COVID‐19 outbreak, only a small number of children were suffering from COVID‐19.
Most infected children were asymptomatic or had only mild symptoms.
Although a small number of children develop significant illnesses, they can still contaminate others.
A safe and effective COVID‐19 vaccine will therefore have both direct and indirect benefits.
Parents’ willingness and attitudes concerning the COVID‐19 vaccine are very crucial.
What's new
Parents’ willingness to have their children receive the COVID‐19 vaccine was low.
The only characteristic of either parents or children found to affect parents’ willingness for their children to receive the COVID‐19 vaccine was the parents being healthcare workers.
Parents’ willingness and positive attitudes towards the COVID‐19 vaccine are factors that increase acceptance of the COVID‐19 vaccine for their children.
1. INTRODUCTION
As of 3 April 2021, more than 130 million confirmed cases of COVID‐19 worldwide, including 2.8 million deaths, had been reported to the World Health Organization (WHO). Five hundred and forty‐seven million doses of the COVID‐19 vaccine have been administered. 1 As of 2 April 2021, there were a possible 104 vaccine candidates, 291 trials had been performed and 13 vaccines had been approved. The Sinovac:Coronavac vaccine has been approved in Turkey. Phase 3 vaccine studies have been conducted in Turkey, Chile, Brazil, Indonesia, China and the Philippines, and approval has been issued in 17 countries. The phase 3 trials conducted in Turkey have involved individuals aged 18‐59. 2 , 3 The Sinovac:Coronavac vaccine has an efficacy level above 83% based on the final results of the phase 3 trials. COVID‐19 vaccination in Turkey began on 14 January 2021. The vaccine is administered in two doses at an interval of 28 days. COVID‐19 vaccine is planned to be administered free of charge to every Turkish citizen. The Ministry of Health has prioritised the provision of the COVID‐19 vaccine, starting with healthcare workers and followed by individuals over 18 years, according to age, disease and occupational status. As of 03 April 2021, more than 16.6 million doses of the COVID‐19 vaccine had been administered in Turkey. 4 However, it remains uncertain whether or not the vaccine will be administered to children.
At the beginning of the COVID‐19 outbreak, only a small number of children were suffering from COVID‐19. Most infected children were asymptomatic or had only mild symptoms. Most recent data show that an increasing number of children are becoming infected, and children represent that 11.5% of all COVID‐19 cases in the United States. Some children have multisystem inflammatory syndrome (MIS‐C). 5 Increasing numbers of case reports and case series concerning severe clinical manifestations in children show that the disease has changed. Although a small number of children develop significant illnesses, these can still contaminate others. A safe and effective COVID‐19 vaccine will therefore have both direct and indirect benefits. 6 COVID‐19 vaccination is likely to provide many benefits, such as reducing severe illness in children, resulting in fewer illnesses in families, normalising the economy, opening schools, reducing inequalities and reducing stress. However, effective herd immunity is needed for this to happen. Children will also need to receive the COVID‐19 vaccine for effective herd immunity to be achieved. Enrolling children in early vaccination studies too early risks exposing them to excessive research risks. However, waiting too long can unfairly deprive children and their families of the benefits of a vaccine and can even delay the emergence of an effective response by a year or more. 7
Parents have the right to decide whether or not their children should be vaccinated. Therefore, it is important to understand parents’ willingness to have their children receive the COVID‐19 vaccine and the barriers to and facilitators of COVID‐19 vaccination. In previous studies, numerous factors such as anxiety about COVID‐19, children's illnesses and vaccination status and parents’ education status have affected parents’ willingness to allow their children to receive the COVID‐19 vaccine. The most common barrier reported by parents in the context of COVID‐19 vaccination is the safety and effectiveness of the vaccine. 8 , 9 , 10 This study aimed to evaluate the Turkish parents’ willingness and attitudes about the COVID‐19 vaccine.
2. METHOD
This cross‐sectional study employed a self‐administered online survey as the data collection tool. The research was conducted in Turkey between 8 and 21 February 2021. Parents with children under the age of 18 were included. The sample size was calculated at 971, with Zα = 1.96 for a 95% confidence interval, a predicted acceptable margin of error d = 0.03 and a 65% estimated vaccination rate. One thousand and thirty‐five parents participated.
The online survey was administered via Google Forms and was distributed to the parents via Facebook, WhatsApp and mail groups. Participants were informed about the study's purpose, the duration of the questionnaire, the identity of researchers and how the data would be stored in an section at the beginning of the form. Written informed consent was obtained from online before the respondents completed the questionnaire. The questionnaire was developed based on a review of the relevant literature. 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 It was then tested on 15 parents and adjusted for accuracy and clarity. The self‐administered survey consisted of 25 questions capable of completion in 5 minutes. This investigated parents’ and their children's characteristics, parents’ willingness and attitudes towards the COVID‐19 vaccine. Parents were asked to provide socio‐demographic characteristics (age, gender, education level, perceived economic status, occupation and number of children) and characteristics of their children [age, gender, chronic disease, vaccination status in the childhood immunisation program, receipt of paid for vaccines (Meningococcal vaccine, HPV vaccine and Rotavirus vaccine) in addition to the childhood immunisation program and whether they or their children had a history of COVID‐19 diagnosis]. Parents were then asked about their willingness to allow their children or themselves to receive the COVID‐19 vaccine. Possible responses were “no,” “undecided” and “yes.” We also asked parents about their willingness to enroll their children or themselves in trials for COVID‐19 and vaccination, with response categories of no and yes. Parents were also asked about their willingness to have their children vaccinated with the COVID‐19 vaccine if mortality rates associated with the disease increased among children following a mutation. We also asked questions that evaluating parents’ attitudes towards the COVID‐19 vaccine.
The study data were entered onto and analysed on IBM SPSS Statistics 21.0 software. Categorical variables were expressed as frequencies and proportions and were compared using the χ2 test. Parents’ willingness to have their children vaccinated with the COVID‐19 vaccine was used as the dependent variable. Independent variables with P values <.05 at binary analysis were then adjusted in a multivariate logistic regression model.
Permission for the study was granted by the Turkish Republic Ministry of Health Scientific Research Platform to carry out the study. It was also approved by the Ondokuz Mayıs University Clinical Research Ethical Committee (2021/29).
3. RESULTS
One thousand and thirty‐five parents participated in this study. Over half of the parents were 30‐39 years old (53.3%), 77.8% were female, 82.8% were educated to university level or higher, 76.2% perceived their economic status as average, 43.6% were healthcare workers, 42.3% had two children and 19.7% had a history of COVID‐19 diagnosis. Additionally, 59.9% of parents were willing to receive the COVID‐19 vaccine. Nearly half the children in this study were 0‐6 years old (49.8%), 52.0% were male, 4.4% had a chronic disease, 11.8% had a history of COVID‐19 diagnosis and 97.1% had been routinely vaccinated under the childhood immunisation program. The rate of parents’ willingness to allow their children to receive the COVID‐19 vaccine was 36.3% (Table 1).
TABLE 1.
Characteristics of parents and their children
| n (%) | |
|---|---|
| Parents | |
| Age groups | |
| 18‐29 y | 130 (12.6) |
| 30‐39 y | 552 (53.3) |
| ≥40 y | 353 (34.1) |
| Gender | |
| Male | 230 (22.2) |
| Female | 805 (77.8) |
| Education | |
| High school or below | 178 (17.2) |
| University or above | 857 (82.8) |
| Perceived economic status | |
| Low | 43 (4.2) |
| Medium | 789 (76.2) |
| High | 203 (19.6) |
| Occupation | |
| Non‐HCW | 584 (56.4) |
| HCW | 451 (43.6) |
| History of COVID‐19 diagnosis | |
| No | 831 (80.3) |
| Yes | 204 (19.7) |
| Number of children | |
| 1 | 446 (43.1) |
| 2 | 438 (42.3) |
| ≥3 | 151 (14.6) |
| Willingness to receive the COVID‐19 vaccine themselves | |
| Refuse | 152 (14.7) |
| Hesitant | 263 (25.4) |
| Accept | 620 (59.9) |
| Children | |
| Age groups | |
| 0‐6 y | 515 (49.8) |
| 7‐12 y | 299 (28.9) |
| 13‐17 y | 221 (21.4) |
| Gender | |
| Male | 538 (52.0) |
| Female | 497 (48.0) |
| History of COVID‐19 diagnosis | |
| No | 913 (88.2) |
| Yes | 122 (11.8) |
| Chronic disease | |
| No | 989 (95.6) |
| Yes | 46 (4.4) |
| Vaccinated routinely under the National Expanded Program on Immunisation | |
| No | 30 (2.9) |
| Yes | 1005 (97.1) |
| Parents’ willingness to have the COVID‐19 vaccine administered to their children | |
| Refuse | 291 (28.1) |
| Hesitant | 368 (35.6) |
| Accept | 376 (36.3) |
No statistically significant association was observed between parents’ willingness to allow their children to receive the COVID‐19 vaccine and parental gender (P = .142) or parental history of COVID‐19 diagnosis (P = .163). Parents’ willingness to allow their children to receive the COVID‐19 vaccine differed significantly in terms of parental age groups (P = .005), education levels (P < .001), perceived economic status (P = .001), occupation (P < .001) and number of children (P = .047). Willingness to allow their children to receive the COVID‐19 vaccine was higher among parents aged 40 or older compared with those aged 18‐29 years old (43.1% vs 30.8%), among those educated to university level or higher compared with high school or lower (39.2% vs 22.5%), those with high economic status compared with low economic status (46.8% vs 20.9%), HCWs compared with non‐HCWs (47.2% vs 27.9%), and those with only one child compared with those three or more (39.0% vs 27.8%) (Table 2). There was no statistically significant association between parents’ willingness to allow their children to receive the COVID‐19 vaccine and the child characteristics of age groups (P = .176), gender (P = .135), history of COVID‐19 diagnosis (P = .506), chronic disease (P = .928) and routine vaccination status (P = .729).
TABLE 2.
A comparison of parent and child characteristics in terms of parents’ willingness to have the COVID‐19 vaccine administered to their children
| Parents’ willingness to have the COVID‐19 vaccine administered to their children | |||
|---|---|---|---|
|
Accept n = 376 |
Refuse or hesitant n = 659 |
P | |
| n (%) | n (%) | ||
| Parents | |||
| Age groups | |||
| 18‐29 y | 40 (30.8) | 90 (69.2) | .005 |
| 30‐39 y | 184 (33.3) | 368 (66.7) | |
| ≥40 y | 152 (43.1) | 201 (56.9) | |
| Gender | |||
| Male | 93 (40.4) | 137 (59.6) | .142 |
| Female | 283 (35.2) | 522 (64.8) | |
| Education level | |||
| High school or below | 40 (22.5) | 138 (77.5) | <.001 |
| University or above | 336 (39.2) | 521 (60.8) | |
| Perceived economic status | |||
| Low | 9 (20.9) | 34 (79.1) | .001 |
| Medium | 272 (34.5) | 517 (65.5) | |
| High | 95 (46.8) | 108 (53.2) | |
| Occupation | |||
| Non‐HCWs | 163 (27.9) | 421 (72.1) | <.001 |
| HCWs | 213 (47.2) | 238 (52.8) | |
| History of COVID‐19 diagnosis | |||
| No | 305 (36.7) | 526 (63.3) | .613 |
| Yes | 71 (34.8) | 133 (65.2) | |
| Number of children | |||
| 1 | 174 (39.0) | 272 (61.0) | .047 |
| 2 | 160 (36.5) | 278 (63.5) | |
| ≥3 | 42 (27.8) | 109 (72.2) | |
| Children | |||
| Age groups | |||
| 0‐6 y | 178 (34.6) | 337 (65.4) | .176 |
| 7‐12 y | 106 (35.5) | 193 (64.5) | |
| 13‐17 y | 92 (41.6) | 129 (58.4) | |
| Gender | |||
| Boy | 207 (38.5) | 331 (61.5) | .135 |
| Girl | 169 (34.0) | 328 (66.0) | |
| History of COVID‐19 diagnosis | |||
| No | 335 (36.7) | 578 (63.3) | .506 |
| Yes | 41 (33.6) | 81 (66.4) | |
| Chronic disease | |||
| No | 359 (36.3) | 630 (63.7) | .928 |
| Yes | 17 (37.0) | 29 (63.0) | |
| Vaccinated routinely under the National Expanded Program on Immunisation | |||
| No | 10 (33.3) | 20 (66.7) | .729 |
| Yes | 366 (36.4) | 639 (63.6) | |
Bold values indicate statistically significant.
Parents who were willing to receive the COVID‐19 vaccine (59.4%) were more willing than hesitant parents (1.9%) to allow their children to be given the COVID‐19 vaccine (P < .001). In addition, 83.9% of parents were willing to have their children receive the COVID‐19 vaccine if the mortality rates associated with COVID‐19 in children increased following a mutation. Parents who were willing to allow their children to be vaccinated with the COVID‐19 vaccine (42.5%) in the event of a post‐mutation increase in COVID‐19 related mortality in children were also more willing to allow their children to receive the COVID‐19 vaccine than hesitant parents (4.2%) (P < .001). The rate of parents’ willingness to enroll their children in trials for COVID‐19 vaccination was 4.4%, whereas willingness to enroll themselves in such trials stood at 21.0%. Parents who were willing to enroll their children in trials for COVID‐19 vaccination (93.5%) were more willing to allow their children to receive the COVID‐19 vaccine than hesitant parents (33.7%) (P < .001). Moreover, parents who were willing to enroll themselves in trials for COVID‐19 vaccination (69.6%) were also more willing to allow their children to receive the COVID‐19 vaccine than parents who would refuse or who were hesitant (27.5%) (P < .001) (Table 3).
TABLE 3.
A comparison of parents’ willingness to have the COVID‐19 vaccine administered to their children and willingness and attitudes concerning the COVID‐19 vaccine
| Parents’ willingness to have the COVID‐19 vaccine administered to their children | ||||
|---|---|---|---|---|
|
Accept n = 376 |
Refuse or hesitant n = 659 |
Total n = 1035 |
P | |
| n (%) | n (%) | n (%) | ||
| Willing to receive the COVID‐19 vaccine | ||||
| No* | 8 (1.9) | 407 (98.1) | 415 (40.1) | <.001 |
| Yes | 368 (59.4) | 252 (40.6) | 620 (59.9) | |
| Willing to participate in the COVID‐19 vaccine trial | ||||
| No | 225 (27.5) | 593 (72.5) | 818 (79.0) | <.001 |
| Yes | 151 (69.6) | 66 (30.4) | 217 (21.0) | |
| Willing to allow their children to participate in a COVID‐19 vaccine trial | ||||
| No | 333 (33.7) | 656 (66.3) | 989 (95.6) | <.001 |
| Yes | 43 (93.5) | 3 (6.5) | 46 (4.4) | |
| Willing to allow the COVID‐19 vaccine to be given to their children if children catch COVID‐19 and mortality increases following a mutation | ||||
| No | 7 (4.2) | 160 (95.8) | 167 (16.1) | <.001 |
| Yes | 369 (42.5) | 499 (57.5) | 868 (83.9) | |
| Vaccination of their children with paid‐for vaccines in addition to the NEPI | ||||
| No | 187 (31.6) | 405 (68.4) | 592 (57.2) | <.001 |
| Yes | 189 (42.7) | 254 (57.3) | 443 (42.8) | |
| Advising others to receive the COVID‐19 vaccine | ||||
| No | 4 (1.3) | 309 (98.7) | 313 (30.2) | <.001 |
| Yes | 372 (51.5) | 350 (48.5) | 722 (69.8) | |
| Worrying that they or their children may have COVID‐19 | ||||
| No | 38 (19.3) | 159 (80.7) | 197 (19.0) | <.001 |
| Yes | 338 (40.3) | 500 (59.7) | 838 (81.0) | |
| Believing that the COVID‐19 vaccine will end the pandemic | ||||
| No | 133 (21.2) | 494 (78.8) | 627 (60.6) | <.001 |
| Yes | 243 (59.6) | 165 (40.4) | 408 (39.4) | |
| Stating that everyone should be vaccinated for herd immunity against COVID‐19 | ||||
| No | 18 (4.8) | 360 (95.2) | 378 (36.5) | <.001 |
| Yes | 358 (54.5) | 299 (45.5) | 657 (63.5) | |
| Frequency of encountering information about the COVID‐19 vaccine on social media in the previous month | ||||
| Rarely sometimes | 99 (30.6) | 225 (69.4) | 324 (31.3) | .009 |
| Usually always | 277 (39.0) | 434(61.0) | 711 (68.7) | |
| Content of information about the COVID‐19 vaccine on social media | ||||
| Negative | 106 (25.9) | 304 (74.1) | 410 (39.6) | <.001 |
| Positive | 270 (43.2) | 355 (56.8) | 625 (60.4) | |
Refuse or hesitant; NEPI: National Expanded Program on Immunisation.
Bold values indicate statistically significant.
Participants whose children had received paid‐for vaccines (ie, Meningococcal vaccine, HPV vaccine and Rotavirus vaccine) in addition to the Expanded Program on Immunisation (42.7%) were more willing to allow their children to receive the COVID‐19 vaccine than parents who had not had their children vaccinated with paid‐for vaccines (31.6%) (P < .001). We also found that 69.8% of parents said that they would advise others to receive the COVID‐19 vaccine. Parents who said they would advise others to receive the COVID‐19 vaccine (51.5%) were more willing to allow their children to receive the COVID‐19 vaccine than those who would not give such advice (1.3%) (P < .001). Eighty‐one percent of parents were worried about themselves or their children contracting COVID‐19. Parents who were worried about themselves or their children contracting COVID‐19 (40.3%) were more willing for the COVID‐19 vaccine to be given to their children than those with no such worry (19.3%) (P <.001). Analysis showed that 39.4% of parents agreed that the COVID‐19 vaccine would end the pandemic. Parents who agreed that the COVID‐19 vaccine would end the pandemic (59.6%) were more willing to allow their children to receive the COVID‐19 vaccine than those who disagree (21.2%) (P < .001). In addition, 63.5% of the parents agreed that everyone should be vaccinated to achieve herd immunity against COVID‐19. Parents who agreed that everyone should be vaccinated against COVID‐19 for herd immunity were more willing to allow their children to be given the COVID‐19 vaccine (54.5%) than those who disagreed (4.8%) (P < .001) (Table 3).
The study findings showed that 68.7% had been exposed to information related to the COVID‐19 vaccine in social media in the previous month, 60.4% being exposed to positive information. Parents who were exposed to information related to the COVID‐19 vaccine in the social media in the previous month (39.0%) were more willing to allow the COVID‐19 vaccine to be given to their children compared to those who were rarely exposed (30.6%) (P < .009). Parents who stated they were exposed to positive information related to the COVID‐19 vaccine in the social media (43.2%) were also more willing to have the COVID‐19 vaccine given to their children compared to those who were not exposed to positive information (25.9%) (P < .001) (Table 3).
A multivariate logistic regression model was constructed by including factors with P‐values <.05 at binary comparisons (Table 4). This model determined the predictors affecting parents’ willingness to allow their children to be given the COVID‐19 vaccine with an accuracy of 81.3%. The only characteristic of either parents or children found to affect parents’ willingness for their children to receive the COVID‐19 vaccine was the parents being healthcare workers. Parents’ willingness to receive the vaccine and positive attitudes toward it were factors that increase their willingness to have the COVID‐19 vaccine given to their children (Table 4).
TABLE 4.
Predictors of parents’ willingness to allow the COVID‐19 vaccine to be given to their children
| Variables | Categories | AOR* (95% CI) | P |
|---|---|---|---|
| Age groups | 18‐29 y | 1 | |
| 30‐39 y | 0.811 (0.460‐1.427) | .467 | |
| ≥40 y | 1.205 (0.634‐2.289) | .569 | |
| Education | High school or below | 1 | |
| University or above | 0.814 (0.418‐1.584) | .544 | |
| Perceived economic status | Low | 1 | |
| Medium | 1.870 (0.596‐5.869) | .283 | |
| High | 2.147 (0.637‐7.235) | .218 | |
| Occupation | Non‐HCW | 1 | |
| HCW | 1.903 (1.272‐2.849) | .002 | |
| Number of children | 1 | 1 | |
| 2 | 1.030 (0.689‐1.541) | .884 | |
| ≥3 | 0.672 (0.347‐1.300) | .237 | |
| Willing to receive the COVID‐19 vaccine | No | 1 | |
| Yes | 24.817 (10.887‐56.57) | <.001 | |
| Willing to participate in the COVID‐19 vaccine trial | No | 1 | |
| Yes | 1.728 (1.151‐2.595) | .008 | |
| Willing to allow their children to participate in a COVID‐19 vaccine trial | No | 1 | |
| Yes | 11.879 (2.409‐58.580) | .002 | |
| Willing to allow the COVID‐19 vaccine to be given to their children if children catch COVID‐19 and mortality increases following a mutation | No | 1 | |
| Yes | 3.613 (1.440‐9.062) | .006 | |
| Vaccination of their children with paid‐for vaccines in addition to the NEPI. | No | 1 | .786 |
| Yes | 0.949 (0.648‐1.389) | ||
| Advising others to receive the COVID‐19 vaccine | No | 1 | |
| Yes | 7.854 (2.506‐24.615) | <.001 | |
| Worrying that they or their children may have COVID‐19 | No | 1 | |
| Yes | 2.069 (1.246‐3.437) | .005 | |
| Believing that the COVID‐19 vaccine will end the pandemic | No | 1 | |
| Yes | 2.075 (1.447‐2.977) | <.001 | |
| Stating that everyone should be vaccinated for herd immunity against COVID‐19 | No | 1 | |
| Yes | 3.048 (1.669‐5.566) | <.001 | |
| Frequency of encountering information about the COVID‐19 vaccine on social media in the previous month | Rarely‐sometimes | 1 | |
| Usually‐always | 0.896 (0.596‐1.346) | .597 | |
| Content of information about the COVID‐19 vaccine on social media | Negative | 1 | |
| Positive | 0.850 (0.575‐1.258) | .417 |
Cox and Snell R 2 = 0.439; Nagelkerke R 2 = .602; Accuracy = 81.3.
AOR, adjusted odds ratio; variables with P < .05 in the binary analysis were adjusted in the multivariate logistic regression models; NEPI, National Expanded Program on Immunisation.
Bold values indicate statistically significant.
The main reasons for parents’ willingness to allow the COVID‐19 vaccine to be administered to their children included, in decreasing order, the need for COVID‐19 control (75.5%), the benefits of the COVID‐19 vaccine outweighing its potential harm (69.9%), and to protect not only their own families but also others (66.2%) (Figure 1). The main reasons for reluctance to allow their children to receive the COVID‐19 vaccine included lack of sufficient scientific studies (84.8%), concern about safety and side effects (76.9%), and potential inefficacy of the vaccine due to mutations (36.7%) (Figure 2).
FIGURE 1.
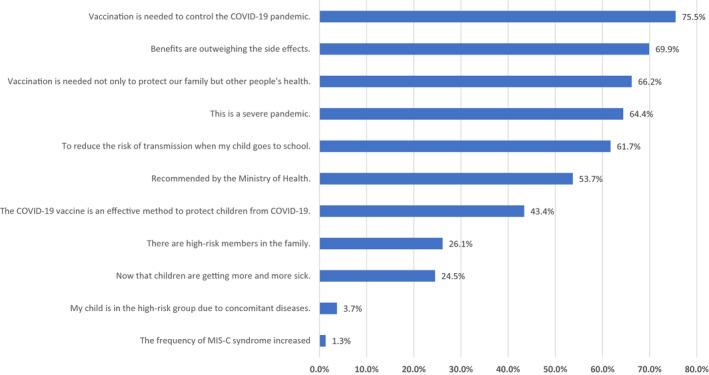
Parents’ reasons for willingness to vaccination of their children for COVID‐19 (n = 376)
FIGURE 2.
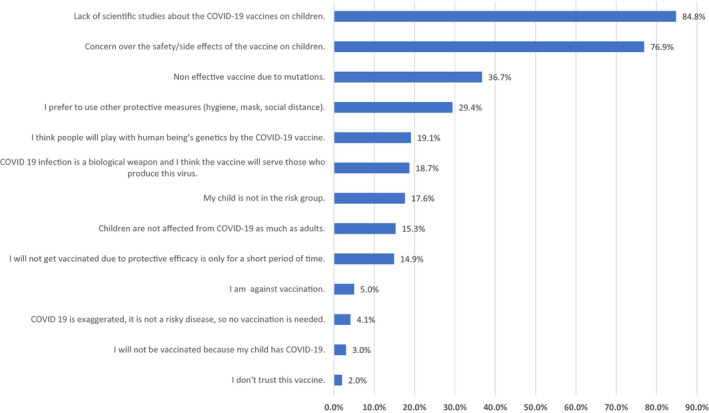
Parents’ reasons for not willing to vaccination of their children for COVID‐19 (n = 659)
4. DISCUSSIONS
This cross‐sectional study is one of the first to investigate Turkish parents’ willingness to undergo and permit COVID‐19 vaccination to provide preliminary information for future child COVID‐19 vaccination plans. Approximately one‐third of parents were willing to allow their children to receive the COVID‐19 vaccine. These results indicate that due to the high levels of vaccine hesitation and rejection of the COVID‐19 vaccine among parents, new strategies will be needed for a possible COVID‐19 vaccination program for children. Ninety‐seven percent of the study participants had allowed their children to be vaccinated under the national extended vaccination program, and 43% had been involved in the extended vaccination schedule. Understanding the reasons for parents’ willingness or reluctance to have the COVID‐19 vaccine administered to their children will therefore be of particular assistance to vaccination program planners.
Reported levels of parents’ willingness to allow the COVID‐19 vaccine to be given to their children in previous studies were 89% in England was, 12 80% in New Zealand, 18 73% in China, 10 65% in the USA, 9 and 42% in Turkey. 19 Another study reported rates of 57% for the national vaccine and 29% for the international vaccines. 16 The comparable figure in the present study was 36%. In a study conducted in a paediatric emergency department, the child's age, receipt of routine vaccinations, having the child or a parent having been vaccinated against the flu in the previous year, and worrying about their child being infected COVID‐19 were found to be associated with increased parents’ willingness to permit administration of the COVID‐19 vaccine. 9 In another study, increased parental age, male gender, being married, being education to college level or higher and higher income were associated with willingness to allow their children to receive the COVID‐19 vaccine. 13 A study evaluating vaccine hesitation and rejection in Italy identified economic hardship as a determinant of vaccine hesitation. A low level of education emerged as an indicator of complete vaccine rejection without affecting vaccine hesitations. 20 However, other studies have reported that educational level does not affect willingness to be vaccinated. 10 , 21 , 22 , 23 Healthcare worker parents are more desirous that their children should be vaccinated than non‐healthcare worker parents. This can be attributed to such parents’ witnessing the severity of the pandemic first‐hand. Similar to the present study, healthcare workers have been reported to be more willing to receive the COVID‐19 vaccine. 19 A previous study showed no difference between parents working on the frontline and those working in the management department in terms of willingness to have their children vaccinated with COVID‐19 during the pandemic. 10 In the present study, parents with one child, those over the age of 40, university graduates, parents with a high perceived socio‐economic level and healthcare workers were more willing to receive the COVID‐19 vaccines. Some studies have reported that willingness to permit vaccination was affected by the child's age and compliance with the vaccines in the current vaccination schedule. 9 , 10 The lack of a high level of willingness among parents of children with chronic diseases was consistent with the finding of a previous study. 9 These results may reflect the concerns of families of immunocompromised children about the use of live vaccines, and the public, especially those at high risk, therefore need to be given more information about the COVID‐19 vaccines. No difference was observed in children's characteristics in terms of parents’ willingness to be vaccinated. In the regression model used to evaluate parental and child characteristics together, the parents being healthcare workers was the only factor affecting parents’ willingness allow the COVID‐19 vaccine to be given to their children.
The willingness of parents to be vaccinated in previous studies was 80% in the United States, 24 81% in Australia, 22 76% in France 23 and 69% in England 25 higher than in the present study. However, vaccine willingness in the present study was very close to the figure of 65% in reported Ireland 25 and Saudi Arabia. 21 A study from Indonesia reported willingness to be vaccinated at rates between 67% and 93%, depending on the effectiveness of the vaccine. 26 In another study from China, the vaccine willingness rate was 44.2% in the first pandemic wave and 34.8% in the third wave. 27 Developments and debates regarding COVID‐19 vaccines appear to have an impact on vaccination willingness. Vaccine efficacy, safety and out‐of‐pocket costs as well as vaccine advice and media coverage have been shown to influence pandemic vaccine choices in general populations. 28 Developments regarding different COVID‐19 vaccines in different countries may explain the variations in vaccine willingness. One study reported that approximately one quarter of parents were willing for their children to participate in a vaccine trial on the COVID‐19 vaccine. 8 The rate of adults willing to volunteer in a trial on the COVID‐19 vaccine in France was significantly higher than that of the parents in the present study. 29 In a study from Jordan, 36% of the parents and 18% of their children agreed to participate in the COVID‐19 vaccine trial. 30 In the present study, parents’ willingness for themselves and their children to participate in the vaccine trial was low. Parents’ willingness to participate in an experimental vaccination study is the most crucial determinant of whether their children will also consent to participate. 14 The results of this study showed that approving children's participation in vaccination studies was associated with parents’ willingness to allow their children to receive the COVID‐19 vaccine. Previous studies have also shown that parents’ willingness to vaccinate their children increase in line with a higher level of fear and anxiety about COVID‐19. 18 , 19 , 24 From that perspective, this study is consistent with previous research. Parents’ willingness to have their children vaccinated against COVID‐19 has increased significantly in the event of the virus is mutating, leading to increased prevalence and mortality among children. However, the mild or asymptomatic course of COVID‐19 among children caused parents to feel less anxious and resulted in a low willingness to have their children vaccinated.
In terms of the difference between willingness to engage in health‐related behaviour and actual behaviour, it appears that strong incentives are needed to achieve effective vaccination. 31 Children can contribute significantly to the spread of COVID‐19 as with other respiratory viruses. Even if the pandemic slows down as a result of various control measures or even stops spreading locally, it is likely to regenerate and spread without adequate immunity. Indeed, this can be seen as recurring waves of the pandemic. If herd immunity can be achieved, this may make it possible to halt the spread of COVID‐19. Parents who believed that vaccination could end the pandemic in the present study were therefore more eager to have their children vaccinated. Vaccination of children to ensure herd immunity has proved successful in preventing many infectious diseases in whose transmission children play an essential role. 32 The numbers of parents who wished to see all members of society vaccinated for herd immunity were significantly higher among those who were willing to allow the COVID‐19 vaccine to be given to their children. One previous study reported that parental disease risk perception increased following a short education intervention aimed at increasing awareness about herd immunity and local vaccination. 33 It will therefore be useful to inform parents about the individual and social benefits associated with the COVID‐19 vaccination. In the present study, parents with a greater willingness to have their children vaccinated also reported recommending the COVID‐19 vaccine to others. Parents who had previously had paid‐for vaccinations administered to their children were more willing to allow them to receive the COVID‐19 vaccine for their children. Positive thoughts and behaviors concerning the vaccine and awareness of the vaccine's protective effects against infectious diseases on the part of parents positively affect the willingness to vaccinate.
The frequency at which parents encounter information about the COVID‐19 vaccine on social media and their encountering positive information about the COVID‐19 vaccine both increase vaccine willingness. 10 Logically, such supporting information can increase parents’ confidence in COVID‐19 vaccines and lessen their anxiety. Greater exposure to negative information about COVID‐19 vaccination was associated with lower parental vaccine acceptance. Previous research has shown that individuals are more likely to absorb negative information than positive information during a disease outbreak. 34 While social media are a powerful tool for disseminating information, there are concerns about false data, unverified rumours and even malicious misinformation appearing on these platforms. 35 Global misinformation has spread through social media during the COVID‐19 pandemic, and this may pose challenges for future COVID‐19 vaccination programs. 36 , 37 , 38 Univariate analysis in the present study revealed that those parents who usually or always encountered information about vaccination on social media and those who encountered positive information on social media were more willing to allow their children to receive the COVID‐19 vaccine. The multivariate logistic regression model, in which all parents’ willingness and attitudes were evaluated together, showed that the frequency of exposure to and content of the information about the COVID‐19 vaccine on social media was not effective. This situation shows that social media alone are not an influential factor in decision making. The usage of other information sources may have affected this. It has also been observed that even if the information encountered is untrue, it nevertheless spread as rapidly as if it were correct during the pandemic period. 38 It may be concluded that parents take other factors into account when making decisions for their children.
The parents may be unwilling to have their children vaccinated due to some safety and side effect concerns related to the COVID‐19 vaccine being newly released. One recent study showed that participants were willing to maintain social distancing measures for more than 12 months even if an effective COVID‐19 vaccination had been found. Participants from higher‐risk groups were also willing to wait significantly longer for an effective vaccine than low‐risk participants. 39 In the present study, some parents preferred to use other preventive methods instead of vaccines. Parents’ concerns about side effects and safety were greater than those reported in a previous multinational cohort study. 9 One‐third of the parents do not think that their children are in the risk group and that children are as much affected by the disease as adults. Studies have identified conspiracy theories regarding COVID‐19 and vaccines against it as a fundamental obstacle to vaccination in studies. 40 , 41 In the present study, a number of parents claimed that the virus is a biological weapon intended to manipulate human genetic material through vaccination and that the threat posed by COVID‐19 is exaggerated.
Reasons for parents being willing to have their children vaccinated were compatible with previous studies, including the fact that the vaccine is an effective method for controlling the disease, that the benefits of the vaccine outweigh its disadvantages, and that the vaccine is necessary not only for their children but also for herd immunity. 19 , 42 , 43 Effective herd immunity will require paediatric vaccination. The vaccination of children is likely to have both direct benefits (protecting children against rare, but severe cases of paediatric COVID‐19 and against postinfectious conditions such as multisystem inflammatory syndrome [MIS‐C]) and indirect benefits (protecting others by reducing the spread of the disease). 6 Most infected children are asymptomatic or have only mild symptoms. However, more recent data show that an increasing number of children are becoming infected. Children with underlying health conditions can become seriously ill, and some experience MIS‐C. 5 In the present study, the reasons for some parents’ willingness to allow their children to be vaccinated included the fact that paediatric cases become increasingly sick, that their children have other diseases and the triggering MIS‐C syndrome.
The perceived risk can be reduced by recognising that vaccines can cause mild and very rarely severe side effects. As the most reliable source of information about vaccination, doctors are in a unique position to lead parents away from vaccine hesitation and towards acceptance. Face‐to‐face interventions may be more effective in populations, where a lack of awareness or understanding of vaccination has been identified as a barrier to vaccination (eg, where people are unaware of new or optional vaccines). 44 Parents who are hesitant about vaccination rely less on physicians. 45 At this point, trusted reporters, politicians and scientists can also help provide accurate information and reassurance. Studies have emphasised that informative news portals should co‐operate with government officials, the media and other organisations. 46
There are a number of limitations to this study. First, the research involved an online survey, and the assessment was based on the parents’ self‐reports. However, these reports may not reflect their actual vaccination behaviour. Therefore, new research will be needed to investigate parents’ actual vaccination behaviour and attitudes when vaccination programs for children commence. Second, there are insufficient data regarding the safety and efficacy of the COVID‐19 vaccine in children. Third, other factors that might contribute to parents’ willingness to accept the COVID‐19 vaccine for their children, including vaccination attitudes, the existence of parental chronic diseases, vaccination history and prior adverse or side effects of vaccines, were not investigated. However, this is the first study to evaluate parents’ willingness and attitudes towards the COVID‐19 vaccine after starting the COVID‐19 vaccination program for adults had commenced in Turkey.
5. CONCLUSION
Parents’ willingness to allow the COVID‐19 vaccine to be administered to their children was at a low level. The only characteristic of either parents or children found to affect parents’ willingness for their children to receive the COVID‐19 vaccine was the parents being healthcare workers. Parents’ willingness and positive attitudes towards the COVID‐19 vaccine are factors that increase their willingness to allow their children to receive the COVID‐19 vaccine. This indicates that because of the high level of parental hesitation and rejection of the COVID‐19 vaccine, educational programs will be needed for parents regarding possible COVID‐19 vaccination for children.
DISCLOSURE
The authors declare that they have no known competing financial interests or personal relationships that could have influenced the work reported in this paper.
AUTHOR CONTRIBUTIONS
Conceptualisation: MY and MKS; Methodology: MY and MKS; Formal analysis and investigation: MY and MKS; Material preparation and data collection: MY and MKS; Writing—original draft preparation: MY and MKS; Resources: MY and MKS; Writing—Review & Editing: MY and MKS; Supervision: MKS. All authors read and approved the final manuscript.
ACKNOWLEDGEMENT
The authors would like to thank all participants for their time and excellent co‐operation.
Yılmaz M, Sahin MK. Parents’ willingness and attitudes concerning the COVID‐19 vaccine: A cross‐sectional study. Int J Clin Pract. 2021;75:e14364. 10.1111/ijcp.14364
REFERENCES
- 1. World Health Organization . WHO Coronavirus Disease (COVID‐19) Dashboard; 2021. https://covid19.who.int/?gclid=CjwKCAiAyc2BBhAaEiwA44‐wW_qFuWO0Dhq49Oy8vfudaaRz3fJa7l_SvL2YR5AOUnVicTRq4AkkmxoC8PIQAvD_BwE. Accessed April 03, 2021.
- 2. McGill COVID19 Vaccine Tracker Team . COVID19 Vaccine Tracker. https://covid19.trackvaccines.org/. Accessed April 03, 2021.
- 3. Health Institutes of Turkey . Clinical Trial For SARS‐CoV‐2 Vaccine (COVID‐19). https://clinicaltrials.gov/ct2/show/NCT04582344. Accessed March 15, 2021.
- 4. Turkish Republic Ministry of Health . T.C Sağlık Bakanlığı COVID‐19 aşısı bilgilendirme platformu. https://covid19asi.saglik.gov.tr/. Accessed April 03, 2021.
- 5. Jiang LI, Tang K, Levin M, et al. COVID‐19 and multisystem inflammatory syndrome in children and adolescents. Lancet Infect Dis. 2020;20:e276‐e288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Klass P, Ratner AJ. Vaccinating children against covid‐19 ‐ the lessons of measles. N Engl J Med. 2021;384:589‐591. [DOI] [PubMed] [Google Scholar]
- 7. Mintz K, Jardas E, Shah S, Grady C, Danis M, Wendler D. Enrolling minors in COVID‐19 vaccine trials. Pediatrics. 2021;147:e2020040717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Goldman RD, Staubli G, Cotanda CP, et al. Factors associated with parents’ willingness to enroll their children in trials for COVID‐19 vaccination. Hum Vaccines Immunother. 2020; 17 1607‐1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Goldman RD, Yan TD, Seiler M, et al. Caregiver willingness to vaccinate their children against COVID‐19: Cross sectional survey. Vaccine. 2020;38 7668‐7673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhang KC, Fang Y, Cao HE, et al. Parental acceptability of COVID‐19 vaccination for children under the age of 18 years: cross‐sectional online survey. JMIR Pediatr Parent. 2020;3:e24827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. AlHajri B, Alenezi D, Alfouzan H, et al. Willingness of parents to vaccinate their children against influenza and the novel coronavirus disease‐2019. J Pediatr. 2021;231:298‐299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bell S, Clarke R, Mounier‐Jack S, Walker JL, Paterson P. Parents' and guardians' views on the acceptability of a future COVID‐19 vaccine: a multi‐methods study in England. Vaccine. 2020;38 7789‐7798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Davis MM, Zickafoose JS, Halvorson AE, Parents' PSW. Likelihood to vaccinate their children and themselves against COVID‐19. medRxiv. 2020:1‐9. 10.1101/2020.11.10.20228759v1 [DOI] [Google Scholar]
- 14. Goldman RD, Marneni SR, Seiler M, et al. Caregivers' willingness to accept expedited vaccine research during the COVID‐19 pandemic: a cross‐sectional survey. Clin Ther. 2020;42:2124‐2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hetherington E, Edwards SA, MacDonald SE, et al. Covid‐19 vaccination intentions among Canadian parents of 9–12 year old children: results from the All Our Families longitudinal cohort. medRxiv. 2020:1‐13. 10.1101/2020.11.24.20237834v1 [DOI] [Google Scholar]
- 16. Yigit M, Ozkaya‐Parlakay A, Senel E. Evaluation of COVID‐19 vaccine refusal in parents. Pediatr Infect Dis J. 2021;40 e134‐e136. [DOI] [PubMed] [Google Scholar]
- 17. Yılmazbaş NP. Did covid‐19 pandemic changed parents’ approach to vaccination? Erciyes Med J. 2020;43 130‐134. [Google Scholar]
- 18. Jeffs E, Lucas N, Walls T. CoVID‐19: parent and caregiver concerns about reopening New Zealand schools. J Paediatr Child Health. 2021;57:403‐408. [DOI] [PubMed] [Google Scholar]
- 19. Akarsu B, Canbay Ozdemir D, Ayhan Baser D, Aksoy H, Fidanci I, Cankurtaran M. While studies on COVID‐19 vaccine is ongoing, the public's thoughts and attitudes to the future COVID‐19 vaccine. Int J Clin Pract. 2021;75:e13891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bertoncello C, Ferro A, Fonzo M, et al. Socioeconomic determinants in vaccine hesitancy and vaccine refusal in Italy. Vaccines (Basel). 2020;8 276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Al‐Mohaithef M, Padhi BK. Determinants of COVID‐19 vaccine acceptance in Saudi Arabia: a web‐based national survey. J Multidiscip Healthc. 2020;13:1657‐1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Faasse K, Newby J. Public perceptions of COVID‐19 in Australia: perceived risk, knowledge, health‐protective behaviors, and vaccine intentions. Front Psychol. 2020;11:551004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ward JK, Alleaume C, Peretti‐Watel P, et al.; Group C . The French public's attitudes to a future COVID‐19 vaccine: the politicization of a public health issue. Soc Sci Med. 2020;265:113414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Thunstrom L, Ashworth M, Finnoff D, Newbold S. Hesitancy towards a COVID‐19 vaccine and prospects for herd immunity. SSRN Electron J. 2020:1‐51. 10.2139/ssrn.3593098 [DOI] [Google Scholar]
- 25. Murphy J, Vallières F, Bentall RP, et al. Psychological characteristics associated with COVID‐19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Harapan H, Wagner AL, Yufika A, et al. Acceptance of a COVID‐19 vaccine in Southeast Asia: a cross‐sectional study in Indonesia. Front Public Health. 2020;8:381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wang K, Wong E‐Y, Ho K‐F, et al. Change of willingness to accept COVID‐19 Vaccine and reasons of vaccine hesitancy of working people at different waves of local epidemic in Hong Kong, China: repeated cross‐sectional surveys. Vaccines (Basel). 2021;9:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Determann D, Korfage IJ, Lambooij MS, et al. Acceptance of vaccinations in pandemic outbreaks: a discrete choice experiment. PLoS One. 2014;9:e102505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Detoc M, Bruel S, Frappe P, Tardy B, Botelho‐Nevers E, Gagneux‐Brunon A. Intention to participate in a COVID‐19 vaccine clinical trial and to get vaccinated against COVID‐19 in France during the pandemic. Vaccine. 2020;38:7002‐7006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Abu‐Farha RK, Alzoubi KH, Khabour OF. Public willingness to participate in COVID‐19 vaccine clinical trials: a study from Jordan. Patient Prefer Adher. 2020;14:2451‐2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McEachan RRC, Conner M, Taylor NJ, Lawton RJ. Prospective prediction of health‐related behaviours with the Theory of Planned Behaviour: a meta‐analysis. Health Psychol Rev. 2011;5 97‐144. [Google Scholar]
- 32. Velavan TP, Pollard AJ, Kremsner PG. Herd immunity and vaccination of children for COVID‐19. Int J Infect Dis. 2020;98:14‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Griffith BC, Ulrich AK, Becker AB, et al. Does education about local vaccination rates and the importance of herd immunity change US parents' concern about measles? Vaccine. 2020;38 8040‐8048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Covello VT. Best practices in public health risk and crisis communication. J Health Commun. 2003;8:5‐8. [DOI] [PubMed] [Google Scholar]
- 35. Seo M. Amplifying panic and facilitating prevention: multifaceted effects of traditional and social media use during the 2015 MERS crisis in South Korea. Journal Mass Commun Q. 2019;98:221‐240. [Google Scholar]
- 36. Tangcharoensathien V, Calleja N, Nguyen T, et al. Framework for managing the COVID‐19 infodemic: methods and results of an online, crowdsourced WHO technical consultation. J Med Internet Res. 2020;22:e19659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bao H, Cao B, Xiong Y, Tang W. Digital media's role in the COVID‐19 pandemic. JMIR Mhealth Uhealth. 2020;8:e20156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ball P, Maxmen A. The epic battle against coronavirus misinformation and conspiracy theories. Nature. 2020;581 371‐374. [DOI] [PubMed] [Google Scholar]
- 39. Tervonen T, Jimenez‐Moreno AC, Krucien N, Gelhorn H, Marsh K, Heidenreich S. Willingness to wait for a vaccine against COVID‐19: results of a preference survey. Patient. 2021;14:373‐377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sallam M, Dababseh D, Eid H, et al. High rates of COVID‐19 Vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines (Basel). 2021;9 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Salali GD, Uysal MS. COVID‐19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychol Med. 2020;1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bell S, Clarke R, Paterson P, Mounier‐Jack S. Parents' and guardians' views and experiences of accessing routine childhood vaccinations during the coronavirus (COVID‐19) pandemic: a mixed methods study in England. PLoS One. 2020;15:e0244049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Dodd RH, Pickles K, Nickel B, et al. Concerns and motivations about COVID‐19 vaccination. Lancet Infect Dis. 2021;21:161‐163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kaufman J, Ryan R, Walsh L, et al. Face‐to‐face interventions for informing or educating parents about early childhood vaccination. Cochrane Database Syst Rev. 2018;5:CD010038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Reuben R, Aitken D, Freedman JL, Einstein G. Mistrust of the medical profession and higher disgust sensitivity predict parental vaccine hesitancy. PLoS One. 2020;15:e0237755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Marco‐Franco JE, Pita‐Barros P, Vivas‐Orts D, Gonzalez‐de‐Julian S, Vivas‐Consuelo D. COVID‐19, fake news, and vaccines: should regulation be implemented? Int J Env Res Pub He. 2021;18 744. [DOI] [PMC free article] [PubMed] [Google Scholar]


