Abstract
The present study examined the relationships between emotional well‐being (positive and negative affect), sleep‐related variables (sleep quality, sleep duration, and change in sleep quality and duration compared to weeks before lockdown), and worrying about coronavirus disease (COVID‐19) challenges during the beginning of the outbreak in Europe. In addition, four different coping strategies were investigated. The study was conducted in Germany with data from 665 participants (53.8% female; 18–73 years), who completed an online questionnaire in April 2020. The results revealed that COVID‐19 worry was associated with impaired well‐being and sleep. Meaning‐ and problem‐focused coping were the most frequently used coping strategies, and showed positive associations with well‐being and sleep. Social and avoidance coping were associated with decreased well‐being and worse sleep outcomes. Three coping strategies showed moderating effects. People who worried more showed higher levels of positive affect when they used problem‐focused coping compared to those who did not. Similarly, highly worried participants showed lower levels of negative affect when they reported using meaning‐focused coping more often. In contrast, social coping increased the risk of high negative affect levels in worried participants. In conclusion, problem‐focused and meaning‐focused coping strategies seemed to be most effective in coping with COVID‐19 challenges.
Keywords: coping, COVID‐19, sleep, well‐being, worrying
1. INTRODUCTION
The newly emerged SARS‐CoV‐2 virus, first discovered in China at the end of 2019 (Lu et al., 2020), had spread around the globe within the first few months of 2020, and instantly posed a great challenge for countries, the society, and people alike. Job loss, home schooling, and social isolation, due to the lockdown restrictions as well as the risk of infecting oneself and loved ones, are examples of what people were confronted with during the beginning of the COVID‐19 pandemic in several countries. For many, the COVID‐19 pandemic constituted an ongoing source of worrying and stress, which may have led to impaired well‐being and sleeping problems, as studies have suggested (American Psychiatric Association, 2020; Rajkumar, 2020; Sønderskov et al., 2020; Umucu & Lee, 2020; Zacher & Rudolph, 2020). Stressful live events usually trigger the use of certain coping strategies to reduce stress and enhance well‐being and sleep (Lazarus & Folkman, 1984). However, not all coping strategies are equally efficient in doing so, and some may even have adverse effects. Therefore, in this study, we examined the relationships between worrying, well‐being, sleep, and coping strategies, and further investigated the protective role of COVID‐19‐related coping efforts on the relationship between COVID‐19‐related worrying, emotional well‐being, and sleep.
1.1. Worrying about COVID‐19 and its effects on well‐being and sleep
The ongoing COVID‐19 pandemic has profoundly changed the lives of people worldwide. Suddenly people had to worry about the things they previously considered naturally given. During the early stages of the COVID‐19 pandemic, people worried about the possibility of becoming infected with the SARS‐CoV‐2 virus, their future, and the social or psychological effects of lockdown measures. Among these concerns, the most prominent according to general surveys (American Psychiatric Association, 2020; Qiu et al., 2020; Statista, 2020) were worrying for oneself and even more so for loved ones about contracting COVID‐19 and worrying about a possible negative impact on the future economy. Worrying can be defined as an uncontrollable chain of thoughts and images accompanied by negative feelings (Andrews & Borkovec, 1988; Verkuil et al., 2007). In accordance with the transactional model of stress and coping from Lazarus and Folkman (1984), which represents the theoretical framework of this study, worrying about COVID‐19 can be considered a form of primary stress appraisal. Primary appraisal stands for the first evaluation of a stressor, represented here by the COVID‐19 pandemic; it can be defined as either positive, irrelevant, or dangerous. According to the transactional model, stress occurs when an external or internal demand exceeds a person's individual resources to handle a specific stressor. We assume that the more the people are worried about the COVID‐19 pandemic, the more likely they are to regard the COVID‐19 as a potentially dangerous stressor, and experience lower well‐being. A recent study from Zacher and Rudolph (2020) supports this assumption. The authors found that during the period between March and May in 2020, positive affect levels and life satisfaction decreased in the German population. In addition, Sønderskov et al. (2020) reported lower well‐being scores during the COVID‐19 pandemic in a Danish sample compared to a sample from 2016, and Sibley et al. (2020) found that people during the lockdown in New Zealand reported higher levels of mental distress.
Stress increases the risk for various health issues (Andrews & Borkovec, 1988; Borkovec et al., 1983; Brosschot & Van Der Doef, 2006), and it also has negative effects on a person's overall well‐being (Ganster & Rosen, 2013; Lazarus & Folkman, 1984). Worrying specifically was found in previous research to be associated with higher levels of negative affect and lower levels of positive affect (McLaughlin et al., 2007; Paolini et al., 2006). Also, a recent study by Umucu and Lee (2020) found that COVID‐19 stress was associated with decreased well‐being. Furthermore, Zacher and Rudolph (2020) also reported higher levels of threat appraisal to be related to lower positive affect, higher negative affect, and lower life satisfaction. Based on these findings and the transactional model of stress and coping (see below), we assume that people who show higher levels of worrying about the COVID‐19 pandemic also report lower levels of positive affect and higher levels of negative affect.
Another important indicator of a person's overall health is sleep, since many studies have found positive relationships between sleep and health (Benham & Charak, 2019; Fernandez‐Mendoza et al., 2020). However, despite there being many studies stating that stress can have negative effects on sleep (Liu et al., 2016; Sadeh et al., 2004; Yang et al., 2018), literature regarding the association between worrying and sleep is still scarce. Some studies have reported sleep disturbance due to worrying to be a prominent issue. In a study by Marques et al. (2016), 33.2% of the study sample reported frequent sleep disturbance due to worry. In a study by Dregan et al. (2013), 37.9% of the participants who reported having sleep problems named worrying as the main reason. Furthermore, people who attributed sleep disturbance to worrying were also more stressed in general (Kelly, 2003; Marques et al., 2016). Studies on the COVID‐19 pandemic and its effects on sleep reported on the one hand positive changes such as later sleep onset‐wakeup times, reduced social jetlag, reduced sleep restriction, and longer sleep duration, and on the other hand negative changes such as more sleep disturbances, and a decrease in sleep quality (Blume et al., 2020; Hetkamp et al., 2020; Marelli et al., 2020; Sinha et al., 2020). Lockdown restrictions seemed to have both positive and negative effects on sleep in the general population, yet in a study by Mandelkorn et al. (2020), more than half of the participants (58%) reported that they were unsatisfied with their sleep during the early stages of the pandemic. Kocevska et al. (2020) also found both negative and positive changes in sleep quality. Research investigating the associations between stress, worrying, and sleep during the COVID‐19 pandemic is still scarce. Xiao et al. (2020) observed worse sleep quality in the Chinese medical staff who reported more stress. Huang and Zhao (2020) also found that health care workers, who represent a highly stressed occupational group during the pandemic, to report lower sleep quality compared to others, and Kocevska et al. (2020) found that worrying about COVID‐19 is associated with worse sleep quality. Fortunately, people are not completely helpless during challenging times because they usually do have ways to cope with situations like the COVID‐19 pandemic and its negative effects on well‐being and sleep.
1.2. Coping with the COVID‐19 pandemic, well‐being, and sleep
Since the COVID‐19 pandemic represents a source of great stress, people had to find ways to deal with new challenges and negative feelings. However, there are many ways to cope with stressful live events. Coping means any cognitive or behavioural effort to master external or internal challenges, when personal resources are viewed as insufficient (Folkman & Lazarus, 1988). Research has shown that which strategy is best varies in different contexts and therefore strategies cannot generally be differentiated as good and bad (Folkman et al., 1986). Concerning COVID‐19, many different coping strategies, such as seeking social support from friends and family, accepting the situation, reacting with humour, avoiding information, or buying stocks are imaginable. The coping strategies most often used to deal with the COVID‐19 pandemic have not been sufficiently investigated. Folkman and Lazarus (1980) originally differentiated problem‐focused and emotion‐focused strategies. In recent research, many researchers have attempted to structure different coping strategies into broader concepts, such as approach and avoidance, or cognitive and behavioural coping strategies (Skinner et al., 2003). In 1997, Carver developed the COPE inventory, which assesses 14 different coping strategies and is currently one of the most used coping questionnaires (Kato, 2015). Although such a detailed differentiation clearly has its advantages, it also makes research on coping very heterogeneous, which is why we focus on four broader concepts of coping strategies that are based on the COPE inventory before (Baumstarck et al., 2017; Zacher & Rudolph, 2020). The four coping styles are problem‐focused, meaning‐focused, social, and avoidance coping.
Problem‐focused coping is directly aimed at the stressor (Carver, 2011), and is positively associated with stress‐related growth, quality of life, and positive affect (Göral et al., 2006; Moskowitz et al., 2009; Shermeyer et al., 2019; Smith et al., 2008). Recent studies from Umucu and Lee (2020) and Zacher and Rudolph (2020) confirm these findings for COVID‐19‐specific problem‐focused coping. The association between problem‐focused coping and negative affect is ambiguous. Some studies found a negative association (Moskowitz et al., 2009; Shermeyer et al., 2019), while others were not able to confirm these results (Smith et al., 2008; Zacher & Rudolph, 2020). Meaning‐focused coping refers to searching for meaning in adversity (Carver, 2011). It is associated with better quality of life, higher levels of positive affect, and lower levels of negative affect (Hofstetter et al., 2005; Moskowitz et al., 2009; Pogrebtsova et al., 2018). Meaning‐focused coping regarding COVID‐19 was also positively related to general well‐being and positive affect (Umucu & Lee, 2020; Zacher & Rudolph, 2020). Social coping refers to seeking social support, and shows no association with positive affect, and a positive association with negative affect in previous research (Moskowitz et al., 2009; Smith et al., 2008). Studies investigating social coping during the COVID‐19 pandemic were, for the most part, able to confirm these results (Umucu & Lee, 2020; Zacher & Rudolph, 2020). Through the use of avoidance coping people attempt to escape a current stressful situation (Carver, 2011). To date, avoidance coping seems to be a rather dysfunctional coping style, since it shows negative associations with stress‐related growth and positive affect as well as positive associations with depression, anger, and negative affect (Moskowitz et al., 2009; Smith et al., 2008). Zacher and Rudolph (2020) confirmed a positive relationship between COVID‐19‐related avoidance strategies and negative affect.
Research on coping and sleep is still scarce, especially considering the effects of COVID‐19. Morin et al. (2003) found no differences in the usage of problem‐focused coping in people with insomnia and good sleepers, although others have reported positive effects of problem‐focused coping on sleep duration and quality (Faber & Schlarb, 2016; Morin et al., 2003). Meaning‐focused coping was found to be positively related to sleep quality by Hofstetter et al. (2005). To the best of our knowledge, no study has investigated the association between social coping, especially during the COVID‐19 pandemic, and sleep. Avoidance coping was related to sleep disturbances, an indicator of sleep quality, in one study (Hoyt et al., 2009) and not related to sleep quality in another study (Hofstetter et al., 2005). Findings regarding the association between avoidance coping and sleep quality are thus so far inconclusive. Sleep duration was not related to avoidance coping in a study by Sadeh et al. (2004). Even though many studies have directly linked different coping strategies with good or bad outcomes for well‐being and sleep, it is important to investigate whether coping strategies might efficiently buffer associations between stressors and well‐being or sleep outcomes (see Dardas & Ahmad, 2015).
1.3. Coping as a moderator between COVID‐19 worry, well‐being, and sleep
So far, studies concerning COVID‐19‐specific coping and well‐being during the early stages of the COVID‐19 pandemic focused on the associations between stress appraisal, the use of coping strategies, and aspects of well‐being. However, to the best of our knowledge, no study has tested possible moderation effects of COVID‐19‐specific coping on the relationship between COVID‐19‐related stress or worry and aspects of well‐being. It is possible, however, that certain coping strategies could buffer or even enhance the relationships between COVID‐19 worry, well‐being, and sleep, and therefore may be considered as effective or ineffective coping strategies. For this reason, we investigated moderation effects of the aforementioned four coping strategies in relation to COVID‐19 worry, well‐being and sleep.
1.4. Aims of the study
Previous research linked greater worrying and stress with worse outcomes for well‐being and sleep in general as well as for well‐being during the early stages of the COVID‐19 pandemic. However, the relationship between stress or worrying due to COVID‐19 and sleep has not been sufficiently examined so far. Therefore, the first aim of this study was to investigate whether well‐being (positive and negative affect), sleep quality and duration, and changes in sleep quality and duration due to the COVID‐19 pandemic were associated with COVID‐19 worry during the early stages of the COVID‐19 outbreak in Germany in 2020. Based on the transactional model of stress and coping and the results of previous research, we expect higher levels of worrying about COVID‐19 to be associated with greater negative affect, lower positive affect, and worse sleep parameters (poor sleep quality, short sleep duration, negative changes in sleep quality, and duration).
The second aim of the study was to examine which COVID‐19‐specific coping strategies were used most often during the early stages of the COVID‐19 pandemic. The third aim was to investigate how COVID‐19‐specific coping relates to well‐being and sleep. Based on previous findings, we expect positive relations for problem‐ and meaning‐focused coping with well‐being and sleep. In addition, we expect social coping to be positively related to negative affect and to be unrelated to positive affect. Regarding the association between social coping and sleep, no predictions could be postulated. We expect greater avoidance coping to be associated with lower well‐being. Even though research about avoidance coping and subjective sleep quality is scarce and inconclusive, we assume avoidance coping might further be related to worse sleep quality and a negative change in sleep quality due to the COVID‐19 pandemic, since it was found to be related to sleep disturbances, an aspect of sleep quality, in a study before and also shows negative relationships with various subjective well‐being measures. No associations between avoidance coping and sleep duration or changes in sleep duration due to the COVID‐19 pandemic are expected.
The fourth aim of the study was to explore whether the four coping strategies examined were useful in dealing with COVID‐19. Therefore, the possible moderating effects of the coping strategies on the relationship between COVID‐19 worries and well‐being (positive and negative affect) as well as on the relationship between COVID‐19 worries and sleep (sleep quality and duration) will be investigated.
2. METHODS
The study was approved by the institutional Ethics Committee and all participants gave informed consent. Data collection took place from 1 to 19 April 2020, during which time lockdown restrictions were in force in Germany. The nationwide lockdown began on 22 March and lasted until 3 May. Schools, stores (with the exception of supermarkets, drug stores, and pharmacies), as well as many nonessential companies were closed. Employees were asked to work at home. Travelling was restricted and international borders were closed. Furthermore, a contact ban was imposed, which only committed contact to only one other person apart from one's own household outdoors.
2.1. Participants
A total of 692 participants completed the online questionnaire, that was distributed via social media and mailing lists in Germany. Three outliers and 24 underaged participants were excluded. The remaining sample consisted of 665 participants, whose age ranged from 18 to 73, with a mean age of 36 (SD = 14). Of the total study sample, 53.8% were female (one person reported as diverse); 47.5% reported having a university degree; 19.6% completed vocational training; 57.7% were currently employed, and worked for more than 20 h a week, 14.3% worked less than 20 h due to the COVID‐19 pandemic, 8.6% reported being unemployed or working less than 20 h, 16.6% were students and 2.9% reported being retired. Participants' professions represented a variety of different work sectors (e.g., finance, administration, healthcare, security, education, science, or building industry). None of the participants were tested positive for COVID‐19 infection; 42 participants reported having or had COVID‐19 like symptoms, but not a test result. Seventy‐seven percent of the study sample reported good or very good sleep quality during the beginning of the COVID‐19 pandemic, and 78.8% of the study sample slept on average seven or more hours a night. Most of the study sample reported no changes in sleep quality (65.2%) or duration (52.9%). A decline in sleep quality was reported by 23.3%, and an improvement in sleep quality was reported by 11.6% of the study sample. Similarly, sleep duration decreased for 15.3% of the participants and increased for 31.8%.
2.2. Measurement instruments
The online questionnaire included questions about demographics, current employment status, and the following measures.
2.2.1. Worry about COVID‐19
At the time of the inquiry no published questionnaire assessing COVID‐19 worries was available. On the basis of a study in which items about worrying were adapted to the Ebola crisis in 2014 (Thompson et al., 2017), we created six items to assess three important aspects of worrying about COVID‐19, which have already been described. Two items measured worrying about a possible infection (I am scared of getting infected by the COVID‐19 pathogen, the possibility of contracting COVID‐19 is bothering me), two items measured worrying about the future (I worry about my future because of the current COVID‐19 pandemic, the possible consequences due to the COVID‐19 pandemic are stressing me), and two items measured worrying about lifestyle limitations and burdens (I feel constricted in my way of life, my life changed significantly due to the COVID‐19 pandemic). Participants were asked to rate on a 5‐point Likert scale how well every item applied to them (1 = not at all, 5 = exactly). To test dimensionality, we performed a confirmatory factor analysis with three components (consisting of two items as described above) and one higher order factor using LISREL. This second‐order factor model provided a good fit with χ2 (6) = 10.50, p = 0.11 (RMSEA = 0.033; CFI = 0.998; RFI = 0.988). Second‐order factor loadings (0.92, 0.51, 0.46) were significant (p´s < 0.001). Because we were interested in a global measure of COVID‐19 worry, one mean score of all six items was computed (α = 0.75).
2.2.2. Positive and negative affect
To assess the positive and negative affect, the Positive and Negative Affect Schedule (PANAS) was used (Breyer & Bluemke, 2016; Watson et al., 1988). The PANAS measures positive and negative affect with 10 items each, which can be summarized into one mean score each for positive and negative affect. Every item represents an adjective, and the participants rate how intensely they felt this specific emotion or feeling during the past two weeks. Items are answered on a scale from 1 (not at all) to 5 (extremely). The reliability and validity of the PANAS are satisfactory (Breyer & Bluemke, 2016). The reliabilities of positive and negative affect for this study were satisfactory (α = 0.85; 0.82, respectively).
2.2.3. Sleep duration and subjective sleep quality
Sleep duration and subjective sleep quality were measured using items of the Pittsburg Sleep Quality Index (PSQI; Backhaus & Riemann, 1996; Buysse et al., 1989). The PSQI is a widely used instrument to measure sleep quality—consisting of seven subscales—which offers good validity and reliability (Backhaus & Riemann, 1996). For sleep duration, the participants rated how long, on average, they slept in the past two weeks. Unlike in the original questionnaire, we decided to use sleep duration as a continuous variable to not lose variance. Subjective sleep quality was measured with the ‘sleep quality’‐subscale, asking participants to rate their overall sleep quality for the past two weeks. We used an eight‐point format, and added two additional items (on most days in the last two weeks I slept well; my sleep in the last two weeks was not restorative). All the three items were correlated (r = 0.76 and above), and therefore, aggregated into one mean score, with higher scores indicating better subjective sleep quality. The reliability of sleep quality for this study was good (α = 0.93).
2.2.4. Change in sleep quality and sleep duration
We used two single‐item measures of sleep quality and duration from the PSQI (Buysse et al., 1989) and adapted the response format to assess subjective change due to the COVID‐19 pandemic. Participants were asked to rate on a 5‐point‐Likert scale their sleep quality (Compared to the time before the COVID‐19 pandemic, I now sleep 1 = a lot worse, 5 = a lot better) and their sleep duration (Compared to …. I now sleep 1 = much shorter, 5 = much longer).
2.2.5. COVID‐19‐specific coping
Coping strategies were measured with the Brief‐COPE from Carver (1997), which was adapted to the consequences of the COVID‐19 pandemic. The Brief‐COPE is a short form of the COPE inventory, one of the most frequently used coping questionnaires (Kato, 2015), and includes 14 different coping strategies, each measured by two items (Carver, 1997). Two items assessing self‐blame were not included, due to inadequacy in the context of the COVID‐19 pandemic. Two items measuring religious coping were also excluded, as they did not fit to our proposed higher‐order coping strategies. All the 12 measured coping strategies of the Brief‐COPE were reduced into four higher order coping strategies, similar to those used by Baumstarck et al. (2017), Litman (2006), and Zacher and Rudolph (2020). Acceptance, positive reframing, and humour items were subsumed under the construct of meaning‐focused coping (α = 0.68). Problem‐focused coping included active coping and planning items (α = 0.75). Self‐distraction, behavioural disengagement, denial, and substance use items were summarized as avoidance coping (α = 0.53), and instrumental support, emotional support, and venting items as social coping (α = 0.77).
2.2.6. Control variables
Peoples' preferred sleep time and sleep quality are strongly influenced by individuals' chronotype. Late chronotypes tend to have later sleep onset and offset times and report a lower sleep quality compared to early chronotypes (Roenneberg & Merrow, 2007; Roeser, Meule, et al., 2012). Late chronotypes also show lower levels of well‐being and higher levels of stress compared to early chronotypes (Buschkens et al., 2010; Roeser, Obergfell, et al., 2012). Therefore, we included chronotype as a control variable. Chronotype was measured using the Composite Scale of Morningness (CSM; Randler, 2014; Smith et al., 1989), which is a widely used chronotype self‐reporting questionnaire to assess daily preferences for activity. The CSM consists of 13 items, which can be aggregated into one global score. Higher values indicate a greater tendency toward morningness. Values range from 22 to 55. According to Randler (2008), the CSM scale offers good psychometric properties. Reliability was α = 0.90.
In addition, we included age, gender, and education as control variables because they showed significant correlations with the relevant variables (see Table 2). Education was operationalized as a dichotomous variable that differentiated between participants with a university degree and those with less education.
TABLE 2.
Bivariate correlations
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 COVID‐19 worry | 1 | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| 2 Positive affect | −0.18*** | 1 | – | – | – | – | – | – | – | – | – | – | – | – | – |
| 3 Negative affect | 0.55*** | −0.16*** | 1 | – | – | – | – | – | – | – | – | – | – | – | – |
| 4 Sleep quality | −0.30*** | 0.36*** | −0.36*** | 1 | – | – | – | – | – | – | – | – | – | – | – |
| 5 Change in SQ | −0.27*** | 0.23*** | −0.28*** | 0.58*** | 1 | – | – | – | – | – | – | – | – | – | – |
| 6 Sleep duration | −0.08* | 0.02 | −0.04 | 0.29*** | 0.20*** | 1 | – | – | – | – | – | – | – | – | – |
| 7 Change in SD | −0.10* | 0.09* | −0.12** | 0.31*** | 0.40*** | 0.50*** | 1 | – | – | – | – | – | – | – | – |
| 8 Chronotype | −0.09* | 0.21*** | −0.11** | 0.12** | −0.00 | −0.13** | −0.07 | 1 | – | – | – | – | – | – | – |
| 9 Problem‐f. coping | 0.13** | 0.32*** | −0.00 | 0.10* | 0.10* | 0.06 | 0.16*** | 0.08* | 1 | – | – | – | – | – | – |
| 10 Meaning‐f. coping | −0.25*** | 0.30*** | −0.24*** | 0.26*** | 0.25*** | 0.18*** | 0.20*** | −0.03 | 0.39*** | 1 | – | – | – | – | – |
| 11 Social coping | 0.34*** | −0.01 | 0.43*** | −0.10* | −0.07 | 0.06 | 0.03 | −0.14*** | 0.31*** | 0.06 | 1 | – | – | – | – |
| 12 Avoidance coping | 0.24*** | −0.14*** | 0.32*** | −0.17*** | −0.13** | 0.01 | −0.04 | −0.10* | −0.01 | −0.06 | 0.17*** | 1 | – | – | – |
| 13 Education | 0.02 | 0.11** | 0.00 | 0.03 | 0.03 | −0.05 | 0.01 | 0.08* | 0.10* | 0.09* | 0.09* | −0.21** | 1 | – | – |
| 14 Gender | 0.15** | −0.15** | 0.14** | −0.14** | −0.03 | 0.06 | 0.05 | −0.04 | 0.13** | −0.10* | 0.23** | 0.02 | 0.00 | 1 | – |
| 15 Age | 0.01 | 0.08* | −0.14** | 0.01 | −0.08* | −0.26** | −0.19** | 0.22** | −0.07 | −0.19** | −0.16** | −0.17** | 0.13** | −0.09* | 1 |
Note: N = 665.
Gender: 1 = male, 2 = female; one participant reported divers and was not included in the correlation with the gender variable. Education: 1 = no university degree, 2 = university degree.
* p < 0.05 ** p < 0.01 *** p < 0.001.
2.3. Statistical analysis
The first and third aim of the study were analysed based on bivariate correlations with a significance level of p < 0.05. The second aim of the study was to investigate which coping strategies were used most often during the start of the COVID‐19 pandemic and was tested via a repeated measures ANOVA with Bonferroni‐adjusted post‐hoc analyses with a significance level of p < 0.05. Moderations effects were investigated using multiple regression analyses. In the first step worrying about COVID‐19, control variables (chronotype, age, gender, education), and all four coping strategies served as predictors for the measures of well‐being (positive and negative affect) and different sleep characteristics (sleep quality and duration). In the second step interactions between worrying about COVID‐19 and the four coping strategies were included. Since response formats differed between variables, all predictors were transformed into z‐scores to avoid problems of multicollinearity (Cohen et al., 2003). We expected chronotype to be associated with worrying, coping strategies, sleep, and well‐being, and therefore included chronotype as a control variable. All calculations were conducted using IBM SPSS Statistics, version 26, and Microsoft Excel 2016. Descriptive statistics of all relevant variables are shown in Table 1.
TABLE 1.
Descriptive statistics
| M | SD | Min | Max | Skewness | Kurtosis | |
|---|---|---|---|---|---|---|
| COVID‐19 worry | 2.63 | 0.79 | 1.00 | 5.00 | 0.28 | −0.27 |
| Positive affect | 2.88 | 0.69 | 1.00 | 5.00 | 0.15 | −0.09 |
| Negative affect | 2.12 | 0.67 | 1.00 | 4.40 | 0.48 | −0.12 |
| Sleep quality | 5.79 | 1.86 | 1.00 | 8.00 | −0.72 | −0.49 |
| Change in sleep quality | 2.86 | 0.71 | 1.00 | 5.00 | −0.11 | 1.52 |
| Sleep duration | 7.49 | 1.12 | 4.00 | 12.00 | −0.04 | 1.02 |
| Change in sleep duration | 3.21 | 0.83 | 1.00 | 5.00 | 0.05 | 0.31 |
| Chronotype | 37.55 | 7.25 | 16.00 | 55.00 | −0.25 | −0.21 |
| Problem‐focused coping | 4.31 | 1.04 | 1.00 | 6.00 | −0.65 | 0.25 |
| Meaning‐focused coping | 4.41 | 0.88 | 1.83 | 6.00 | −0.37 | −0.37 |
| Social coping | 2.70 | 1.02 | 1.00 | 6.00 | 0.36 | −0.51 |
| Avoidance coping | 2.27 | 0.63 | 1.00 | 4.75 | 0.61 | 0.87 |
Note: N = 665.
3. RESULTS
Based on the four aims of this study, the results are presented in four sections. First, correlations of worrying about COVID‐19 with positive and negative affect and sleep variables are reported. Second, we explore the usage of the four different investigated coping‐strategies during the early stages of the COVID‐19 pandemic. Third, how these coping strategies relate to well‐being and sleep are described. Finally, we report whether these coping‐strategies act as moderators for the relationship between COVID‐19 worry with positive and negative affect and sleep.
3.1. Worrying about COVID‐19, well‐being, and sleep
All bivariate correlations are shown in Table 2. As expected, worrying about COVID‐19 showed a positive correlation with negative affect, and negative correlations with positive affect and all sleep variables. The higher the reported worry about COVID‐19, the higher the negative affect, and the lower the positive affect. Highly worried participants also reported lower sleep quality, shorter sleep duration, and a negative change in sleep quality and duration compared to weeks before the emergence of COVID‐19. The correlations differ in size, but the pattern of the results confirmed our hypotheses.
3.2. COVID‐19‐specific coping strategies
Descriptive statistics revealed that meaning‐ and problem‐focused coping were the most used coping strategies during the beginning of the COVID‐19 pandemic, followed by social coping and avoidance coping (see Table 1). To test whether these differences were statistically significant, we conducted a repeated measures ANOVA that included all the four coping strategies. Since Mauchly's test indicated a violation of the sphericity assumption (χ2 [5] = 75.06, p < 0.001), a Greenhouse‐Geisser correction was applied. Significant differences were found for the use of the four coping strategies (F [2.80, 1860.771] = 1161.77, p < 0.001, η 2 = 0.64). Bonferroni‐adjusted post‐hoc analysis revealed that meaning‐ and problem‐focused coping were used significantly more than social coping (M difference = 1.61, 95%‐CI [1.48,1.73], p < 0.001; M difference = 1.71, 95%‐CI [1.58,1.84], p < 0.001) and avoidance coping (M difference = 2.04, 95%‐CI [1.92,2.17], p < 0.001; 2.15, 95%‐CI [2.03,2.26], p < 0.001). Avoidance coping was used significantly less than social coping (M difference = 0.43, 95%‐CI [0.32, 0.55], p < 0.001). No significant differences were found between the usage of problem‐ and meaning‐focused coping. Control analyses (analyses of covariance) revealed that, after controlling for age, gender, and education, all significant differences remained stable.
3.3. COVID‐19‐specific coping, well‐being, and sleep
In this section, we focus on the correlations with COVID‐19‐specific coping (see Table 2). In accordance with our predictions, problem‐focused coping showed positive relationships with positive affect, sleep quality, and change in sleep quality and duration; however, unexpectedly, no relationship with negative affect and sleep duration. Meaning‐focused coping was expectedly associated with higher positive affect, lower negative affect, better sleep quality, longer sleep duration and a positive change in sleep quality and duration compared to the weeks before COVID‐19 lockdown restrictions. As we predicted, higher levels of social coping were linked to higher levels of negative affect as well as to worse sleep quality. Other variables were not related to social coping. As hypothesized, avoidance coping was negatively linked to positive affect, sleep quality, and change in sleep quality, and positively linked to negative affect. No relationship between avoidance coping and sleep duration or change in sleep duration was found. Control analyses (partial correlations) showed that all predicted correlations remained significant after controlling for age, gender, and education. In sum, the pattern of the bivariate correlations showed positive correlations for problem‐ and meaning‐focused coping and negative correlations for social and avoidance coping with factors of well‐being and sleep. However, the findings do not imply that certain strategies are generally better than others. Therefore, we focused on the protective function of coping efforts regarding the relationship between worry about COVID‐19, well‐being, and sleep.
3.4. Moderating effects of COVID‐19‐specific coping
To test the possible moderating effects of the measured coping strategies between COVID‐19 worry, well‐being, and sleep, we conducted several multiple regression analyses (see Table 3). The results show that the relationship between COVID‐19 worry and positive affect was moderated by problem‐focused coping. People with higher levels of worrying reported higher positive affect when they used problem‐focused strategies more frequently, than those who used them less frequently (see Figure 1a). These differences in positive affect levels were less pronounced in individuals with lower levels of worrying. Other coping strategies showed no moderating effect for positive affect. The relationship between worrying about COVID‐19 and negative affect was moderated by meaning‐focused and social coping. People who experienced more worrying showed lower negative affect the more frequently they reported using meaning‐focused coping. These differences were again less pronounced in individuals with lower levels of worrying (see Figure 1b). In contrast, higher levels of social coping were associated with greater negative affect in worried individuals (see Figure 1c).
TABLE 3.
Moderating effects of coping
| Criteria | |||||
|---|---|---|---|---|---|
| Negative affect | Positive affect | ||||
| Step | Predictor | β | p | β | p |
| 1 | Age | −0.11 | 0.001 | 0.07 | 0.04 |
| Gender | 0.01 | 0.88 | −0.14 | <0.001 | |
| Education | 0.04 | 0.23 | 0.04 | 0.22 | |
| Chronotype | 0.01 | 0.87 | 0.15 | <0.001 | |
| COVID‐19 worry | 0.40 | <0.001 | −0.14 | 0.001 | |
| Problem‐focused coping | −0.10 | 0.003 | 0.29 | <0.001 | |
| Meaning‐focused coping | −0.13 | <0.001 | 0.15 | <0.001 | |
| Social coping | 0.29 | <0.001 | 0.01 | 0.74 | |
| Avoidance coping | 0.15 | <0.001 | −0.06 | 0.11 | |
| – | F(9654) = 55.34, p < 0.001, R 2 = 0.43 | F(9654) = 22.41, p < 0.001, R 2 = 0.23 | |||
| 2 | Worry x Problem | 0.04 | 0.32 | 0.10 | 0.01 |
| Worry x Meaning | −0.09 | 0.008 | −0.04 | 0.30 | |
| Worry x Social | 0.07 | 0.03 | −0.05 | 0.23 | |
| Worry x Avoidance | 0.02 | 0.45 | 0.04 | 0.23 | |
| – | F(13,650) = 40.01, p < 0.001, R 2 = 0.43 | F(13,650) = 16.18, p < 0.001, R 2 = 0.23 | |||
Note: N = 665.
Gender: 1 = male, 2 = female. Education: 1 = no university degree, 2 = university degree.
FIGURE 1.
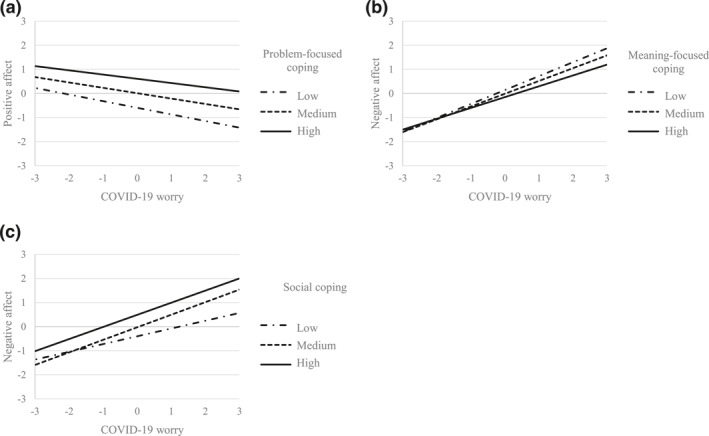
Moderating effects of (a) problem‐focused, (b) meaning‐focused and (c) social coping strategies on the relationship between COVID‐19 worry and positive and negative affect (variables are z‐standardised). Depicted are conditional regressions. One standard deviation below and above was used to categorize coping
The regression analysis for moderating effects on change in sleep quality revealed marginally significant moderating effects of problem‐focused coping (ß worryxproblem = 0.06, p = 0.10), meaning‐focused coping (ß worryxmeaning = 0.06, p = 0.06), and social coping (ß worryxsocial = −0.06, p = 0.09) with significant regression models (F [4660] = 16.77, R 2 = 0.09, p < 0.001; F [4,660] = 20.80, R 2 = 0.011, p < 0.001; F [4660] = 13.49, R 2 = 0.07, p < 0.001). These moderating effects are comparable to those of coping on positive and negative affect regarding strength and direction. Higher levels of problem‐ and meaning‐focused coping were associated with positive changes in sleep quality for highly worried participants, and higher levels of social coping were associated with negative changes in sleep quality. For sleep quality and duration, and change in sleep duration, no moderating effects were found.
4. DISCUSSION
The results of this study demonstrated that worrying about COVID‐19, a form of primary stress appraisal, is associated with aspects of well‐being and different sleep characteristics. Our findings that people who worried more about COVID‐19 experienced lower levels of positive affect and higher levels of negative affect support previous research by Umucu and Lee (2020) and Zacher and Rudolph (2020) regarding relations between primary stress appraisal due to COVID‐19 and measures of well‐being during the beginning of the pandemic. Our results further elucidate associations between COVID‐19 worry and sleep, which thus far have still been insufficiently examined. Worrying about COVID‐19 was linked to various sleep parameters (sleep quality, sleep duration, and change in sleep quality and duration compared to the weeks before the COVID‐19 lockdown) in a negative way and therefore might be a possible risk factor for impaired sleep. Though the global measure of COVID‐19 worry in our study was associated with negative reports of well‐being and sleep we do not know, however, whether the strength of these relationships varies depending on the specific content of the COVID‐19 worries. Various COVID‐19 worries must not necessarily be equally stressful to different people and therefore may lead to differences in their relationships with other variables, as results of Taylor et al. (2020) indicate for well‐being measures. Yet, systematic research is needed to test the significance of these findings.
Our results further revealed that the two most frequently used coping strategies to deal with negative changes during the early stages of the ongoing COVID‐19 pandemic were meaning‐ and problem‐focused coping, which fortunately were also related to better outcomes for peoples' well‐being. Overall, meaning‐focused coping seemed to be the best strategy to deal with the stressful consequences of the COVID‐19 pandemic. It showed positive relationships to all well‐being and sleep measures. High levels of positive reappraisal and humour, however, might also bear the risk of underestimating the perilous effects that COVID‐19 can have on people's physical or mental health. Therefore, further research is needed to elucidate how and why COVID‐19 coping strategies are used, and whether seemingly positive coping strategies, such as meaning‐focused coping, may also show negative relationships depending on the specific situation, stressor, or person. Many years back Lazarus and Folkman (1984) already pointed out that efficient coping strategy depend on the specific situation and person. Problem‐focused coping as well seemed to be a useful coping mechanism since it showed positive correlations with positive affect. Surprisingly, there was no association with negative affect. A possible explanation for a non‐existent relationship with negative affect might be the dimensionality of the PANAS. Negative affect is measured by emotions that refer to social relationships (e.g., hostile, guilty, ashamed) which do not directly relate to problem‐focused coping. Positive affect, however, includes states of positive arousal (attentive, inspired, active) which is stronger associated with problem‐solving strategies.
So far, few studies concerning sleep during the COVID‐19 pandemic and its relationship to different coping strategies are available, which highlights the importance of our findings that meaning‐ and problem‐focused coping also showed positive correlations with people's sleep quality and duration. Since problem‐ and meaning‐focused coping are positively related to well‐being and sleep practitioners might be able to enhance these in COVID‐19 affected populations by implementing interventions that highlight the importance of different coping strategies and provide guidance and instructions on how to use them. The question remains, why problem‐focused coping was only related to sleep quality but not to sleep duration. It is possible that sleep duration is closer linked to positive than negative affect, as our results suggest, and problem‐focused coping as well only showed relations to positive affect. Considering a possible mediating effect, this might explain the missing link with sleep duration.
Social and avoidance coping showed only negative relationships with well‐being and sleep but were also used less frequently than meaning‐focused and problem‐focused coping. Social coping displayed a negative correlation with negative affect and sleep quality, and no correlation with any of the remaining variables. Even though social coping consequently seems to be a rather dysfunctional coping strategy, social support per se is not harmful after all, as many studies have confirmed (Taylor, 2011). It is possible that the action of seeking social support reflects a certain helplessness of individuals to cope with the ongoing situation by themselves. Consequently, having social support is an important protective factor for people's overall well‐being and health; however, relying on others to solve a problem might not be the best strategy to cope with stress. Avoidance coping was the strategy which showed the most negative relationships to well‐being and sleep but was also used least often. Avoidance coping was associated with negative outcomes for all well‐being and sleep measures except for sleep duration and change in sleep duration to which it was not related. Therefore, ignoring COVID‐19, denying it, or diverting oneself does not seem to be a recommendable coping strategy to deal with the consequences of the COVID‐19 pandemic. These findings are in line with previous research, which also links avoidance coping with several indicators of impaired well‐being (Moskowitz et al., 2009; Smith et al., 2008; Zacher & Rudolph, 2020).
Furthermore, three of the four coping strategies moderated the relationship between worrying about COVID‐19 and well‐being. Worried participants who engaged in problem‐focused coping showed higher levels of positive affect, than those who did not. Interestingly, problem‐focused coping was the only coping strategy showing moderation effects on positive affect. As we mentioned above, positive and negative affect are not opposites of one dimension but include different emotional domains. One possible interpretation for this finding could be that instrumental actions regulate (dampen) the negative correlation between worry and positive arousal because of their energizing function. The function of meaning‐focused coping might be palliative because worried people who used meaning‐focused coping more often reported lower levels of negative affect than to those who used meaning‐focused coping less often. Thus, both coping strategies are adaptive during the COVID‐19 pandemic but unfold their stress‐regulating potential in different emotional states. Social coping on the other hand had a negative moderating effect on worried individuals. People who experienced higher levels of negative affect than those who did not use social coping. This may be because they asked for social support but not necessarily receiving it. Furthermore, relying on others may not be helpful in dealing with negative emotions.
Similar results were found for the moderating effects of coping on change in sleep quality, although the results were only marginally significant. Problem‐ and meaning‐focused coping were associated with less negative effects of COVID‐19 worry on the change in sleep quality, whereas social coping was associated with enhanced negative effects of COVID‐19 worry in highly worried participants. Why the examined coping strategies did not moderate the relationship between worrying about COVID‐19 and the other sleep parameters needs to be further investigated. One possible explanation might be that coping strategies primarily influence people's well‐being and mood, which might then subsequently have a positive or negative effect on sleep in the next step. It is also possible that sleep is more affected by other factors such as working hours or childcare. Overall, these results highlight the importance of investigating different coping strategies people use to cope with the negative effects of the COVID‐19 pandemic. Given that the study was conducted in Germany, the question of generalizability is obvious. There is evidence that there are cultural differences in the use of coping strategies and the experience of wellbeing (Chun et al., 2002). However, it is unclear whether these also exist in times of a pandemic. Further account should be taken to the spread of the virus, lockdown measures, or policies that are introduced and withdrawn at different times. Our data allow no comparisons. However, it would be interesting to further investigate whether these findings are generalizable to different forms of stressors and experiences of people living in other countries.
5. LIMITATIONS
Although the present study highlights important associations between aspects of well‐being, sleep, worrying, and different coping strategies used during the early stages of the COVID‐19 pandemic, it is also limited in certain ways. First, the results of this study rely on cross‐sectional data, which is not applicable to causal interpretations. Further research is needed to investigate causal relationships, or to include a broader set of control variables, such as current work situation, childcare, financial status, or social isolation. In particular, longitudinal data could offer the possibility of modelling changes over time. We had no information about the well‐being status of our study sample before the pandemic and therefore cannot make any statement about changes in well‐being due to the COVID‐19 pandemic. Our study sample also included a high percentage of highly educated individuals, which limits generalization to the general population. Furthermore, we relied on self‐reports in this study. These estimations may be influenced by the current cognitive and emotional states or common method variance, and consequently, may not be sufficiently accurate. In addition, this study sample consisted of German participants. It is possible that reactions to and perceptions of COVID‐19 challenges are not comparable to other parts of the world, considering the diverse strategies used by different countries to manage the COVID‐19 pandemic as well as the varied welfare and health care systems. There is no data that compares to what extent the results vary depending on country‐specific differences or variations in current lockdown restrictions.
6. CONCLUSIONS
These results showed that COVID‐19 worry, a form of primary stress appraisal, was an important factor for people's overall well‐being and sleep during the early stages of the COVID‐19 pandemic. However, negative associations between COVID‐19 worry and well‐being can be attenuated by using coping strategies. In particular, meaning‐ and problem‐focused strategies proved to be the most beneficial and the most used coping strategies. It seems many people have advantageous coping strategies at their disposal, which help to regulate COVID‐19‐related impairments to their general well‐being by actively solving the current problem or by adjusting one's cognitive standards and assumptions regarding it.
CONFLICT OF INTEREST
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
ACKNOWLEDGEMENT
Open access funding enabled and organized by Projekt DEAL.
Saalwirth, C. , & Leipold, B. (2021). Well‐being and sleep in stressful times of the COVID‐19 pandemic: Relations to worrying and different coping strategies. Stress and Health, 37(5), 973–985. 10.1002/smi.3057
DATA AVAILABILITY STATEMENT
The data supporting the findings of this study are available from the corresponding author Saalwirth, C. on request. Raw data were generated at the Bundeswehr University Munich, Germany.
REFERENCES
- American Psychiatric Association . (2020). New Poll: COVID‐19 impacting mental well‐being: Americans feeling anxious, especially for loved ones; Older adults are less anxious. Retrieved from https://www.psychiatry.org/newsroom/news‐releases/new‐poll‐covid‐19‐impacting‐mental‐well‐being‐americans‐feeling‐anxious‐especially‐for‐loved‐ones‐older‐adults‐are‐less‐anxious [Google Scholar]
- Andrews, V. H. , & Borkovec, T. D. (1988). The differential effects of inductions of worry, somatic anxiety, and depression on emotional experience. Journal of Behavior Therapy and Experimental Psychiatry, 19(1), 21–26. 10.1016/0005-7916(88)90006-7 [DOI] [PubMed] [Google Scholar]
- Backhaus, J. , & Riemann, D. (1996). Schlafstörungen bewältigen: Informationen und Anleitung zur Selbsthilfe. Beltz. [Google Scholar]
- Baumstarck, K. , Alessandrini, M. , Hamidou, Z. , Auquier, P. , Leroy, T. , & Boyer, L. (2017). Assessment of coping: A new French four‐factor structure of the brief COPE inventory. Health and Quality of Life Outcomes, 15(1), 1–9. 10.1186/s12955-016-0581-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benham, G. , & Charak, R. (2019). Stress and sleep remain significant predictors of health after controlling for negative affect. Stress and Health, 35(1), 59–68. 10.1002/smi.2840 [DOI] [PubMed] [Google Scholar]
- Blume, C. , Schmidt, M. H. , & Cajochen, C. (2020). Effects of the COVID‐19 lockdown on human sleep and rest‐activity rhythms. Current Biology, 30(14), R795–R797. 10.1016/j.cub.2020.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkovec, T. D. , Robinson, E. , Pruzinsky, T. , & DePree, J. A. (1983). Preliminary exploration of worry: Some characteristics and processes. Behaviour Research and Therapy, 21(1), 9–16. 10.1016/0005-7967(83)90121-3 [DOI] [PubMed] [Google Scholar]
- Breyer, B. , & Bluemke, M. (2016). Deutsche version der positive and negative affect schudule PANAS (GESIS panel). Zusammenstellung Sozialwissenschaftlicher Items Und Skalen(October), 1–16. 10.6102/zis242 [DOI] [Google Scholar]
- Brosschot, J. F. , & Van Der Doef, M. (2006). Daily worrying and somatic health complaints: Testing the effectiveness of a simple worry reduction intervention. Psychology & Health, 21(1), 19–31. 10.1080/14768320500105346 [DOI] [Google Scholar]
- Buschkens, J. , Graham, D. , & Cottrell, D. (2010). Well‐being under chronic stress: Is morningness an advantage? Stress and Health, 26(4), 330–340. 10.1002/smi.1300 [DOI] [Google Scholar]
- Buysse, D. J. , Reynolds, C. F. , Monk, T. H. , Berman, S. R. , & Kupfer, D. J. (1989). The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Carver, C. S. (1997). You want to measure coping but your protocol' too long: Consider the brief cope. International Journal of Behavioral Medicine, 4(1), 92–100. 10.1207/s15327558ijbm0401_6 [DOI] [PubMed] [Google Scholar]
- Carver, C. S. (2011). Coping. In The handbook of stress science: Biology, psychology, and health (pp. 221–229). Springer Publishing Company. [Google Scholar]
- Chun, C.‐A. , Moos, R. H. , & Cronkite, R. C. (2002). Culture: A fundamental context for the stress and coping paradigm. In Handbook of multicultural perspectives on stress and coping (pp. 29–53). Springer US. 10.1007/0-387-26238-5_2 [DOI] [Google Scholar]
- Cohen, J. , Cohen, P. , West, S. G. , & Aiken, L. S. (2003). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Erlbaum. [Google Scholar]
- Dardas, L. A. , & Ahmad, M. M. (2015). Coping strategies as mediators and moderators between stress and quality of life among parents of children with Autistic Disorder. Stress Health, 31(1), 5–12. 10.1002/smi.2513 [DOI] [PubMed] [Google Scholar]
- Dregan, A. , Lallukka, T. , & Armstrong, D. (2013). Potential pathways from biopsychosocial risk factors to sleep loss due to worry: A population‐based investigation. Journal of Public Mental Health, 12(1), 43–50. 10.1108/17465721311304230 [DOI] [Google Scholar]
- Faber, J. , & Schlarb, A. A. (2016). The relation of sleep, distress, and coping strategies‐what male and female students can learn from each other? Health, 08(13), 1356–1367. 10.4236/health.2016.813136 [DOI] [Google Scholar]
- Fernandez‐Mendoza, J. , He, F. , Calhoun, S. L. , Vgontzas, A. N. , Liao, D. , & Bixler, E. O. (2020). Objective short sleep duration increases the risk of all‐cause mortality associated with possible vascular cognitive impairment. Sleep Health, 6(1), 71–78. 10.1016/j.sleh.2019.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman, S. , & Lazarus, R. S. (1980). An analysis of coping in a middle‐aged community sample. Journal of Health and Social Behavior, 21(3), 219. 10.2307/2136617 [DOI] [PubMed] [Google Scholar]
- Folkman, S. , & Lazarus, R. S. (1988). The relationship between coping and emotion: Implications for theory and research. Social Science & Medicine, 26(3), 309–317. 10.1016/0277-9536(88)90395-4 [DOI] [PubMed] [Google Scholar]
- Folkman, S. , Lazarus, R. S. , Dunkel‐Schetter, C. , DeLongis, A. , & Gruen, R. J. (1986). Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. Journal of Personality and Social Psychology, 50(5), 992–1003. 10.1037/0022-3514.50.5.992 [DOI] [PubMed] [Google Scholar]
- Ganster, D. C. , & Rosen, C. C. (2013). Work stress and employee health. Journal of Management, 39(5), 1085–1122. 10.1177/0149206313475815 [DOI] [Google Scholar]
- Göral, F. S. , Kesimci, A. , & Gençöz, T. (2006). Roles of the controllability of the event and coping strategies on stress‐related growth in a Turkish sample. Stress and Health, 22(5), 297–303. 10.1002/smi.1107 [DOI] [Google Scholar]
- Hetkamp, M. , Schweda, A. , Bäuerle, A. , Weismüller, B. , Kohler, H. , Musche, V. , Dörrie, N. , Schöbel, C. , Teufel, M. , & Skoda, E.‐M. (2020). Sleep disturbances, fear, and generalized anxiety during the COVID‐19 shut down phase in Germany: Relation to infection rates, deaths, and German stock index DAX. Sleep Medicine, 75(January), 350–353. 10.1016/j.sleep.2020.08.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofstetter, J. R. , Lysaker, P. H. , & Mayeda, A. R. (2005). Quality of sleep in patients with schizophrenia is associated with quality of life and coping. BMC Psychiatry, 5(1), 13. 10.1186/1471-244X-5-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyt, M. A. , Thomas, K. S. , Epstein, D. R. , & Dirksen, S. R. (2009). Coping style and sleep quality in men with cancer. Annals of Behavioral Medicine, 37(1), 88–93. 10.1007/s12160-009-9079-6 [DOI] [PubMed] [Google Scholar]
- Huang, Y. , & Zhao, N. (2020). Generalized anxiety disorder, depressive symptoms and sleep quality during COVID‐19 outbreak in China: A web‐based cross‐sectional survey. Psychiatry Research, 288(January), 112954. 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato, T. (2015). Frequently used coping scales: A meta‐analysis. Stress Health, 31(4), 315–323. 10.1002/smi.2557 [DOI] [PubMed] [Google Scholar]
- Kelly, W. E. (2003). Some correlates of sleep disturbance ascribed to worry. Individual Differences Research, 1(2), 137–146. [Google Scholar]
- Kocevska, D. , Blanken, T. F. , Van Someren, E. J. W. , & Rösler, L. (2020). Sleep quality during the COVID‐19 pandemic: Not one size fits all. Sleep Medicine, 76(January), 86–88. 10.1016/j.sleep.2020.09.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus, R. S. , & Folkman, S. (1984). Stress, appraisal, and coping. Springer Publishing Company. http://link.springer.com/10.1007/978‐1‐4419‐1005‐9_215 [Google Scholar]
- Litman, J. A. (2006). The COPE inventory: Dimensionality and relationships with approach‐ and avoidance‐motives and positive and negative traits. Personality and Individual Differences, 41(2), 273–284. 10.1016/j.paid.2005.11.032 [DOI] [Google Scholar]
- Liu, X. , Liu, C. , Tian, X. , Zou, G. , Li, G. , Kong, L. , & Li, P. (2016). Associations of perceived stress, resilience and social support with sleep disturbance among community‐dwelling adults. Stress Health, 32(5), 578–586. 10.1002/smi.2664 [DOI] [PubMed] [Google Scholar]
- Lu, H. , Stratton, C. W. , & Tang, Y. W. (2020). Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. Journal of Medical Virology, 92(4), 401–402. 10.1002/jmv.25678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandelkorn, U. , Genzer, S. , Choshen‐Hillel, S. , Reiter, J. , Meira e Cruz, M. , Hochner, H. , Kheirandish‐Gozal, L. , Gozal, D. , & Gileles‐Hillel, A. (2020). Escalation of sleep disturbances amid the COVID‐19 pandemic: A cross‐sectional international study. Journal of Clinical Sleep Medicine, 17, 45–53. 10.5664/jcsm.8800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marelli, S. , Castelnuovo, A. , Somma, A. , Castronovo, V. , Mombelli, S. , Bottoni, D. , Leitner, C. , Fossati, A. , & Ferini‐Strambi, L. (2020). Impact of COVID‐19 lockdown on sleep quality in university students and administration staff. Journal of Neurology, 268, 8–15. 10.1007/s00415-020-10056-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques, D. R. , Gomes, A. A. , Ferreira, M. F. , & de Azevedo, M. H. P. (2016). Don't worry, sleep well: Predictors of sleep loss over worry. Sleep and Biological Rhythms, 14(3), 309–318. 10.1007/s41105-016-0060-z [DOI] [Google Scholar]
- McLaughlin, K. A. , Borkovec, T. D. , & Sibrava, N. J. (2007). The effects of worry and rumination on affect states and cognitive activity. Behavior Therapy, 38(1), 23–38. 10.1016/j.beth.2006.03.003 [DOI] [PubMed] [Google Scholar]
- Morin, C. M. , Rodrigue, S. , & Ivers, H. (2003). Role of stress, arousal, and coping skills in primary insomnia. Psychosomatic Medicine, 65(2), 259–267. 10.1097/01.PSY.0000030391.09558.A3 [DOI] [PubMed] [Google Scholar]
- Moskowitz, J. T. , Hult, J. R. , Bussolari, C. , & Acree, M. (2009). What works in coping with HIV? A meta‐analysis with implications for coping with serious illness. Psychological Bulletin, 135(1), 121–141. 10.1037/a0014210 [DOI] [PubMed] [Google Scholar]
- Paolini, L. , Yanez, A. P. , & Kelly, W. E. (2006). An examination of worry and life satisfaction among college students. Individual Differences Research, 4(5), 331–339. [Google Scholar]
- Pogrebtsova, E. , Craig, J. , Chris, A. , O'Shea, D. , & González‐Morales, M. G. (2018). Exploring daily affective changes in university students with a mindful positive reappraisal intervention: A daily diary randomized controlled trial. Stress and Health, 34(1), 46–58. 10.1002/smi.2759 [DOI] [PubMed] [Google Scholar]
- Qiu, J. , Shen, B. , Zhao, M. , Wang, Z. , Xie, B. , & Xu, Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID‐19 epidemic: Implications and policy recommendations. General Psychiatry, 33(2), e100213. 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar, R. P. (2020). COVID‐19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 52(January), 102066. 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randler, C. (2008). Psychometric properties of the German version of the composite scale of morningness. Biological Rhythm Research, 39(2), 151–161. 10.1080/09291010701424796 [DOI] [Google Scholar]
- Randler, C. (2014). CSM. Composite scale of morningness–deutsche fassung. In Leibniz‐Zentrum Für Psychologische Information Und Dokumentation (ZPID) (Hrsg.), Elektronisches Testarchiv. Trier, ZPID. 10.23668/psycharchives.440 [DOI] [Google Scholar]
- Roenneberg, T. , & Merrow, M. (2007). Entrainment of the human circadian clock. Cold Spring Harbor Symposia on Quantitative Biology, 72(1), 293–299. 10.1101/sqb.2007.72.043 [DOI] [PubMed] [Google Scholar]
- Roeser, K. , Meule, A. , Schwerdtle, B. , Kübler, A. , & Schlarb, A. A. (2012). Subjective sleep quality exclusively mediates the relationship between morningness‐eveningness preference and self‐perceived stress response. Chronobiology International, 29(7), 955–960. 10.3109/07420528.2012.699124 [DOI] [PubMed] [Google Scholar]
- Roeser, K. , Obergfell, F. , Meule, A. , Vögele, C. , Schlarb, A. A. , & Kübler, A. (2012). Of larks and hearts ‐ morningness/eveningness, heart rate variability and cardiovascular stress response at different times of day. Physiology & Behavior, 106(2), 151–157. 10.1016/j.physbeh.2012.01.023 [DOI] [PubMed] [Google Scholar]
- Sadeh, A. , Keinan, G. , & Daon, K. (2004). Effects of stress on sleep: The moderating role of coping style. Health Psychology, 23(5), 542–545. 10.1037/0278-6133.23.5.542 [DOI] [PubMed] [Google Scholar]
- Shermeyer, L. , Morrow, M. T. , & Mediate, N. (2019). College students' daily coping, mood, and quality of life: Benefits of problem‐focused engagement. Stress and Health, 35(2), 211–216. 10.1002/smi.2847 [DOI] [PubMed] [Google Scholar]
- Sibley, C. G. , Greaves, L. M. , Satherley, N. , Wilson, M. S. , Overall, N. C. , Lee, C. H. J. , Milojev, P. , Bulbulia, J. , Osborne, D. , Milfont, T. L. , Houkamau, C. A. , Duck, I. M. , Vickers‐Jones, R. , & Barlow, F. K. (2020). Effects of the COVID‐19 pandemic and nationwide lockdown on trust, attitudes toward government, and well‐being. American Psychologist, 75(5), 618–630. 10.1037/amp0000662 [DOI] [PubMed] [Google Scholar]
- Sinha, M. , Pande, B. , & Sinha, R. (2020). Impact of COVID‐19 lockdown on sleep‐wake schedule and associated lifestyle related behavior: A national survey. Journal of Public Health Research, 9(3), 239–245. 10.4081/jphr.2020.1826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner, E. A. , Edge, K. , Altman, J. , & Sherwood, H. (2003). Searching for the structure of coping: A review and critique of category systems for classifying ways of coping. Psychological Bulletin, 129(2), 216–269. 10.1037/0033-2909.129.2.216 [DOI] [PubMed] [Google Scholar]
- Smith, C. S. , Reilly, C. , & Midkiff, K. (1989). Evaluation of three circadian rhythm questionnaires with suggestions for an improved measure of morningness. Journal of Applied Psychology, 74(5), 728–738. 10.1037/0021-9010.74.5.728 [DOI] [PubMed] [Google Scholar]
- Smith, L. E. , Seltzer, M. M. , Tager‐Flusberg, H. , Greenberg, J. S. , & Carter, A. S. (2008). A comparative analysis of well‐being and coping among mothers of toddlers and mothers of adolescents with ASD. Journal of Autism and Developmental Disorders, 38(5), 876–889. 10.1007/s10803-007-0461-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sønderskov, K. M. , Dinesen, P. T. , Santini, Z. I. , & Østergaard, S. D. (2020). The depressive state of Denmark during the COVID‐19 pandemic. Acta Neuropsychiatrica, 32(4), 226–228. 10.1017/neu.2020.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statista . (2020). Was sind Ihre Hauptsorgen oder Bedenken bezüglich der COVID‐19/Corona‐Pandemie? Retrieved from https://de.statista.com/statistik/daten/studie/1108157/umfrage/hauptsorgen‐und‐aengste‐wegen‐der‐covid‐19‐corona‐pandemie/ [Google Scholar]
- Taylor, S. , Landry, C. A. , Paluszek, M. M. , Fergus, T. A. , McKay, D. , & Asmundson, G. J. G. (2020). Development and initial validation of the COVID stress scales. Journal of Anxiety Disorders, 72(April), 102232. 10.1016/j.janxdis.2020.102232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, S. E. (2011). Social support: A review. Oxford University Press. 10.1093/oxfordhb/9780195342819.013.0009 [DOI] [Google Scholar]
- Thompson, R. R. , Garfin, D. R. , Holman, E. A. , & Silver, R. C. (2017). Distress, worry, and functioning following a global health crisis: A national study of Americans' responses to Ebola. Clinical Psychological Science, 5(3), 513–521. 10.1177/2167702617692030 [DOI] [Google Scholar]
- Umucu, E. , & Lee, B. (2020). Examining the impact of COVID‐19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabilitation Psychology, 65(3), 193–198. 10.1037/rep0000328 [DOI] [PubMed] [Google Scholar]
- Verkuil, B. , Brosschot, J. F. , & Thayer, J. F. (2007). Capturing worry in daily life: Are trait questionnaires sufficient? Behaviour Research and Therapy, 45(8), 1835–1844. 10.1016/j.brat.2007.02.004 [DOI] [PubMed] [Google Scholar]
- Watson, D. , Clark, L. A. , & Tellegen, A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Xiao, H. , Zhang, Y. , Kong, D. , Li, S. , & Yang, N. (2020). The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID‐19) in January and february 2020 in China. Medical Science Monitor, 26, 1–8. 10.12659/MSM.923549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, B. , Wang, Y. , Cui, F. , Huang, T. , Sheng, P. , Shi, T. , Huang, C. , Lan, Y. , & Huang, Y.‐N. (2018). Association between insomnia and job stress: A meta‐analysis. Sleep and Breathing, 22(4), 1221–1231. 10.1007/s11325-018-1682-y [DOI] [PubMed] [Google Scholar]
- Zacher, H. , & Rudolph, C. W. (2020). Individual differences and changes in subjective wellbeing during the early stages of the COVID‐19 pandemic. American Psychologist, 76, 50–62. 10.1037/amp0000702 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the findings of this study are available from the corresponding author Saalwirth, C. on request. Raw data were generated at the Bundeswehr University Munich, Germany.


