Abstract
Aim
This study examined the influence of pandemic fatigue on clinical nurses’ mental health, sleep quality and job contentment, with resilience as a mediator.
Background
Pandemic fatigue is an emerging health concern among frontline clinical nurses as a consequence of the ongoing coronavirus pandemic and the various measures implemented to slow the spread of infection. As yet, no studies have investigated the link between pandemic fatigue and resilience, mental health, sleep quality and job contentment in frontline clinical nurses.
Methods
This was a descriptive, cross‐sectional study involving 255 frontline clinical nurses in the Philippines. The Pandemic Fatigue Questionnaire, Brief Resilience Scale, Job Contentment Scale and the Sleep Quality Scale were used to collect data through an online survey.
Results
The mean pandemic fatigue score was 3.086 (out of 5). Being vaccinated (β = 0.231, p < .001) and increased staffing levels (β = −0.488, p < .01) were associated with decreased pandemic fatigue in clinical nurses. Resilience partially mediated the relationships between (a) pandemic fatigue and mental health (β = −0.488, p < .001), (b) pandemic fatigue and sleep quality (β = −0.326, p < .001) and (c) pandemic fatigue and job contentment (β = −0.395, p < .001).
Conclusion
Clinical nurses who received a COVID‐19 vaccine and those who perceived sufficient staffing in their units reported lower levels of pandemic fatigue. Resilience reduces the effects of pandemic fatigue on clinical nurses’ mental health, sleep quality and job contentment.
Implications for Nursing Management
By providing frontline nurses with access to COVID‐19 vaccines and ensuring sufficient staffing levels, nurse managers could effectively reduce or prevent pandemic fatigue and improve their mental health. Implementing resilience‐promoting measures are essential to support nurses’ mental health, promote their sleep quality and foster job satisfaction.
Keywords: COVID‐19, job contentment, mental health, nursing, pandemic fatigue, resilience
1. INTRODUCTION
Pandemic fatigue (PF) is an emerging health concern among individuals during the COVID‐19 pandemic. PF, which is defined as physical and mental tiredness, may occur during a pandemic as a consequence of the interruptions in the usual routines and activities of an individual due to various measures implemented to decrease virus transmission (e.g. lockdown, quarantine, social distancing) (World Health Organization, 2020). Evidence has shown a growing number of people experience pandemic fatigue a few months after the initial implementation of a national lockdown or curfew order in Canada (Nitschke et al., 2021). This trend has also been observed in Western countries in which significant increases in loneliness, fatigue, boredom, worry and extreme sadness were seen among the general public from the first few weeks to the fourth month of the implementation of mobility restrictions (Brodeur et al., 2021). Research from the Philippines, India and Saudi Arabia has also revealed similar patterns (Labrague & Ballad, 2021; Majumdar et al., 2020; Meo et al., 2020) in which individuals increasingly became fatigued as the lockdown continued, underscoring the importance of implementing measures to effectively support individuals during the pandemic and to prevent negative impacts of the prolonged lockdown or stay‐at‐home orders.
Manifestations of pandemic fatigue include physical and mental tiredness, reduced motivation, distractibility, periodic outbursts of emotion and increased fear (Australian Psychological Society, 2020; World Health Organization, 2020). Other symptoms associated with pandemic fatigue include body weakness, sleep problems, hopelessness, sadness, loneliness, overthinking, increased worry, irritability and a lack of concentration (Labrague & Ballad, 2021; Majumbar et al., 2020). A higher degree of pandemic fatigue is attributed to poorer physical, mental, behavioural and cognitive health and may adversely affect nurses’ overall work performance, leading to poorer patient care provision (Cho & Steege, 2021). Therefore, it is essential that organisational strategies are in place to effectively manage this growing issue.
Frontline health care workers, including clinical nurses who work directly with COVID‐19 patients, are particularly vulnerable to developing mental and psychological issues. Substantial evidence has reported higher prevalence rates of anxiety, emotional exhaustion, depression, mental distress, fatigue and post‐traumatic stress disorder among nurses during the height of the pandemic (Labrague, 2021; Usher et al., 2020). As frontline health care workers, clinical nurses face a tremendous amount of stress due to several factors, including increased patient workloads, lack of reliable PPEs, long work shifts in PPE, constant changes in COVID‐19 protocols and a lack of relevant experience caring for highly infectious patients (Goh et al., 2021; Leng et al., 2021). Moreover, the high transmissibility rate of the virus further increases nurses’ fear of becoming infected and infecting others, thereby increasing their risk of mental fatigue (Labrague & Los Santos, 2021). Collectively, these elements potentially increase nurses’ risk of developing pandemic fatigue, adversely affecting their overall health and clinical performance and eventually leading to poor nursing care provision and poorer patient outcomes (del Carmen Giménez‐Espert et al., 2020; Labrague & Los Santos, 2021). Studies have demonstrated that a greater proportion of nurses, particularly those directly taking care of COVID‐19 patients, experienced a significant amount of fatigue during the peak of the pandemic (Jang et al., 2021). The incidence of moderate‐to‐high fatigue levels during the pandemic ranged from 35.06% to 72.2%, with more nurses experiencing physical fatigue than mental fatigue (Zhan et al., 2020; Zou et al., 2021). However, despite this evidence, it is unclear whether pandemic fatigue affects nurses’ mental health, sleep patterns and job contentment.
With the ongoing nursing staff shortage along with the increasing number of nurses being infected by the virus, the need to sustain an adequate nursing workforce is a critical issue. It is necessary that organisational measures be implemented to address the negative impact of the pandemic, including pandemic fatigue, on nurses’ job contentment and their health and well‐being. However, reducing the negative impact of pandemic fatigue on clinical nurses requires bolstering their effective coping skills and resilience.
Resilience is defined as ‘a complex and dynamic process which when present and sustained enables nurses to positively adapt to workplace stressors, avoid psychological harm and continue to provide safe, high‐quality patient care’ (Cooper et al., 2020; pp. 567). Positive consequences attributed to a higher level of resilience in nurses was shown to include the following: increased job satisfaction, reduced turnover, increased psychological well‐being and higher patient satisfaction (Cooper et al., 2020; Hart et al., 2014). There is also compelling evidence showing the value of fostering resilience in nurses when facing traumatic events, emergencies and disasters, and infectious disease outbreaks (Pollock et al., 2020; Son et al., 2019). Reports during the height of the pandemic confirm previous findings regarding the benefits of boosting the resilience of frontline health care workers. Resilient nurses during the pandemic tended to experience less stress and emotional exhaustion, had reduced levels of anxiety and post‐traumatic stress and had a lower incidence of depression compared to non‐resilient nurses (Roberts et al., 2021; Yoruk & Guler, 2021). Moreover, bolstering resilience may potentially reduce the effects of the various pandemic‐related stressors on hospital nurses’ psychological, mental and emotional health (Labrague & Los Santos, 2021; Lorente et al., 2021), in turn, sustaining their job performance and reducing turnover intention (Labrague & Los Santos, 2021). However, while it is known that resilience acts as a protective factor against the negative effects of the pandemic (Cooper et al., 2020), the mechanism by which resilience reduces the negative effects of pandemic fatigue on nurses’ mental health, sleep quality and job contentment remains unclear. This information is vital to assess the extent to which resilience influences nursing outcomes during a pandemic and will help to formulate interventions that better support the mental health and overall well‐being of clinical nurses.
2. METHODS
2.1. Research design
This was a quantitative, cross‐sectional study using an online survey.
2.2. Sample and setting
This study involved frontline clinical nurses in the Central Region of the Philippines. This region is comprised of 50 government and 25 privately owned hospitals, with approximately 3,000 employed nurses. In this study, registered nurses (RNs) assigned to 50 units from 14 hospitals (7 government and 7 private hospitals) within the region were recruited to take part in the study. These hospitals were randomly selected from a list of all hospitals in the region consisting of 5 small capacity hospital (< 100 beds), 4 medium capacity hospital (101 – 250 beds) and 5 large capacity hospital (> 250 beds). For inclusion in the study, nurses were required to be (1) currently working as a clinical nurse, (2) a licensed registered nurse and (3) with at least 6 months of work experience at their current organisation. G Power software was used to identify the required sample size. For a statistical power of 80%, a small effect size (0.05) and an alpha at 0.05, the required sample size was 242. Invitations to participate in the study were sent by email to 300 clinical nurses of which 255 responded.
2.3. Instrumentation
The Pandemic Fatigue Questionnaire was used to assess clinical nurses’ mental and physical fatigue associated with the COVID‐19 pandemic (Labrague & Ballad, 2021). This scale is a unidimensional measure of pandemic fatigue and consists of 10 items, which are answered using a Likert scale (0 for ‘never’ to 5 for ‘always’). The scale was originally designed to assess pandemic fatigue in the young adult population in the Philippines (Labrague & Ballad, 2021). Higher scores on the scale represent higher levels of pandemic fatigue. The scale has excellent construct, concurrent and criterion validity, and the internal consistency of the scale was shown to be acceptable (Labrague & Ballad, 2021).
The Brief Resilience Scale was used to examine nurses’ capacity to rebound from stressful or undesirable situations caused by the COVID‐19 pandemic and from other measures to control its transmission (Smith et al., 2008). The scale consists of five items which are answered using a Likert scale (0 for ‘does not describe me at all’ to 5 for ‘describes me very well’). Higher scores represent greater resilience. The criterion validity and reliability of the scale are within an acceptable range (0.90) (Labrague & de los Santos, 2021; Smith et al., 2008).
The Job Contentment Scale was used to measure job contentment in nurses during the coronavirus pandemic (Taunton et al., 2004). The scale consists of seven items that are rated on Likert scale (1 for ‘strongly disagree’ to 5 for ‘strongly agree’). Higher mean scores represent higher levels of job contentment. The concurrent and criterion validity of this scale was found to be excellent, while its reliability was acceptable (0.91) (Taunton et al., 2004).
Nurses’ sleep quality was assessed using a single‐item measure (Snyder et al., 2018). Nurses rated the quality of their sleep in the past 7 days using a Likert scale that ranged from 0 (‘poor’) to 10 (‘excellent’). The scale was originally designed to measure sleep quality among patients with sleep disturbance and was found to be useful to measure sleep quality among the general population as well (de los Santos & Labrague, 2021). The criterion and concurrent validity and the reliability of the scale are acceptable (Snyder et al., 2018; de los Santos & Labrague, 2021).
The internal consistencies of the scales used in our research were as follows: Pandemic Fatigue Questionnaire, α = 91; Brief Resilience Scale, α = 88; Job Contentment Scale, α = 89; and Sleep Quality Scale, α = 90.
2.4. Ethical considerations and data collection
Ethics approval for the study was obtained from the Samar State University Institutional Research Ethics Review Committee (IRERC) (IRERC EA‐001‐E). Due to several restrictions concerning data collection, the questionnaire was created using an online survey using Google Forms. The survey link was then sent to the valid email addresses and/or social media accounts of the participants. The introductory page of the online survey provided basic details of the study, as well as a consent letter. Nurses who opted to participate in the study signed the consent form by clicking the button ‘Yes I confirm my participation in the study.’, while those who did not want to participate clicked ‘No, I don't want to participate’. No personal information was collected in the online survey to ensure participant anonymity. To encourage a high response rate, we sent weekly reminders to nurses’ email addresses asking them to complete the survey. The online survey data collection was conducted from January to February 2021, during which a second wave of the coronavirus pandemic in the Philippines was declared by the health agency.
2.5. Data analysis
Means, frequencies and standard deviations were used to present the descriptive data. Further, correlations between key study variables were analysed by ANOVA, Pearson's correlation coefficient (r) and independent t‐test. Multiple regression analyses were conducted to determine the predictors of pandemic fatigue and the effects of pandemic fatigue on mental health, sleep quality and job contentment. The mediating effect of resilience on the relationships between pandemic fatigue and the outcome variables was examined using hierarchical regression analysis. The level of statistical significance was set at p < .05.
3. RESULTS
3.1. Nurse characteristics and univariate analyses
A total of 255 clinical nurses responded to the online survey. The average age and years of nursing experience of the respondents were 31.956 and 8.799 years, respectively. The majority were female (n = 187, 73.33%), unmarried (n = 165, 64.71%) and held a BSN degree (n = 209, 81.96%). Most of the respondents were staff nurses (n = 183, 71.76%), had fulltime job status (n = 219, 85.88%) and currently worked in medium to large hospital facilities (n = 177, 69.68). The vast majority had received a COVID‐19 vaccine (n = 210, 82.35%), and less than 50% (n = 103) had attended a COVID‐19‐related training. Approximately 70% of the nurses perceived that PPE in their units was ‘sufficient’ to ‘very sufficient’; however, with regard to staffing adequacy, less than 50% reported ‘sufficient’ to ‘very sufficient’ staffing levels. Pearson correlation analysis found a significant negative correlation between staffing adequacy and pandemic fatigue (r = −0.225, p = .001). Moreover, independent t tests showed higher mean scores of the pandemic fatigue scale among nurses who received a COVID‐19 vaccine compared to those who did not (t = −3.677, p = .001) (Table 1).
TABLE 1.
Nurse characteristics and its correlation with pandemic fatigue (n = 255)
| Variables | Category | n | % | Mean | SD | Test statistic | p value |
|---|---|---|---|---|---|---|---|
| Age | 31.956 | 7.402 | 0.016 | .818 | |||
| Years of experience in nursing | 8.799 | 6.753 | −0.023 | .744 | |||
| Years of experience in the organisation | 5.434 | 5.352 | 0.038 | .587 | |||
| Gender | Male | 68 | 26.67 | 3.075 | 0.975 | −0.090 | .928 |
| Female | 187 | 73.33 | 3.090 | 0.939 | |||
| Marital status | Married | 87 | 34.12 | 3.021 | 0.965 | −0.748 | .456 |
| Unmarried | 165 | 64.71 | 3.124 | 0.934 | |||
| Education | BSN | 209 | 81.96 | 3.055 | 0.949 | −1.203 | .230 |
| MSN | 46 | 18.04 | 3.286 | 0.908 | |||
| Job status | Fulltime | 219 | 85.88 | 3.089 | 0.936 | 0.128 | .898 |
| Part time | 36 | 14.12 | 3.054 | 1.107 | |||
| Job role | Staff nurse | 183 | 71.76 | 3.055 | 0.929 | −0.750 | .454 |
| Nurse manager | 72 | 28.24 | 3.164 | 0.984 | |||
| Facility size | Small | 77 | 30.20 | 3.224 | 1.007 | 1.400 | .249 |
| Medium | 88 | 34.51 | 2.953 | 0.884 | |||
| Large | 90 | 35.29 | 3.103 | 0.943 | |||
| Attendance in COVID−19‐related trainings | Yes | 103 | 40.39 | 3.105 | 1.018 | 0.229 | .819 |
| No | 152 | 59.61 | 3.074 | 0.896 | |||
| Vaccination Status | Vaccinated | 210 | 82.35 | 2.982 | 0.903 | −3.677 | .001 |
| Not vaccinated | 45 | 17.65 | 3.615 | 0.987 | |||
| Personal Protective Adequacy | 2.466 | 0.824 | 0.122 | .080 | |||
| Very insufficient | 21 | 8.24 | |||||
| Insufficient | 57 | 22.35 | |||||
| Sufficient | 112 | 43.92 | |||||
| Very sufficient | 65 | 25.49 | |||||
| Staff Adequacy | 2.937 | 0.850 | −0.225 | .001 | |||
| Very insufficient | 31 | 12.16 | |||||
| Insufficient | 103 | 40.39 | |||||
| Sufficient | 84 | 32.94 | |||||
| Very sufficient | 37 | 14.51 | |||||
| Mental Health | 3.893 | 0.957 | |||||
| Job Contentment | 3.432 | 0.907 | |||||
| Sleep Quality | 6.427 | 2.279 | |||||
| Pandemic Fatigue | 3.086 | 0.944 |
3.2. Descriptive statistics of the key study variables
The mean pandemic fatigue score was 3.086 (SD: 0.944). The mean scores for the job contentment and mental health measures were above the midpoint, with mean scores of 3.432 (SD: 0.9077) and 3.893 (SD: 0.957), respectively. Out of a maximum score of 10, the mean sleep quality score was 6.427 (SD: 2.279).
3.3. Predictors of pandemic fatigue
Among the variables, only vaccination status (β = 0.231, p < .001) and staffing adequacy (β = −0.488, p < .01) were significant predictors. Nurses who received a COVID‐19 vaccine reported a lower score on the pandemic fatigue scale than those who were not yet vaccinated. Further, nurses who perceived adequate staffing within their unit experienced lower levels of pandemic fatigue. The model explained 13.39% of the variance of pandemic fatigue (F = 13.394; p < .001) (Table 2).
TABLE 2.
Predictors of pandemic fatigue
| Variables | B | SE | Beta | t | p | 95.0% Confidence Interval | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| (Constant) | 5.313 | 0.483 | 4.361 | 6.265 | |||
| Vaccination status (R: Vaccinated) | |||||||
| Not vaccinated | 0.587 | 0.165 | 0.231 | 3.564 | .001 | 0.262 | 0.912 |
| Staffing adequacy | −0.212 | 0.074 | −0.185 | −2.844 | .005 | −0.358 | −0.065 |
R2 = 15.4; F = 13.394; p = .001
3.4. Correlation between pandemic fatigue, mental health, job contentment and sleep quality
Multiple correlations using the Pearson r correlation coefficient were conducted between key study variables. Pandemic fatigue was correlated with the three outcome variables in an expected direction—significant negative correlations were identified between pandemic fatigue and mental health (r = −0.559, p < .01), job contentment (r = −0.420, p < .01) and sleep quality (r = −0.381, p < .01) (Table 3).
TABLE 3.
Correlations between key study variables
| Variables | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Mental Health | 1 | ||||
| Job Contentment | 0.486 a | 1 | |||
| Sleep Quality | 0.513 a | 0.430 a | −0.091 | 1 | |
| Pandemic Fatigue | −0.559 a | −0.420 a | −0.166 b | −0.381 a | 1 |
p = .001.
p = .01.
3.5. Mediating effect of resilience on the association between pandemic fatigue and mental health, job contentment and sleep quality
Mediation analysis was conducted to test the hypothesized correlations between pandemic fatigue and nurses’ mental health, sleep quality and job contentment (Table 4; Figure 1). The results indicated that pandemic fatigue has a direct effect on clinical nurses’ mental health (β = −0.559, p < .001), sleep quality (β = −0.381, p < .001) and job contentment (β = −0.420, p < .001). Further, the results also identified that pandemic fatigue had a significant direct effect on nurses’ resilience (β = −0.257, p < .001). The statistical analyses showed that resilience partially mediated the association between pandemic fatigue and clinical nurses’ mental health (β = −0.488, p < .001), sleep quality (β = −0.326, p < .001) and job contentment (β = −0.395, p < .001). In other words, clinical nurses who had low scores on the pandemic fatigue scale might have high levels of resilience, which in turn would lead to better mental health, higher sleep quality and increased job contentment. The results of the Sobel test confirmed the significant mediating effect of resilience on the relationship between pandemic fatigue and mental health (z = −3.256, p = .001), sleep quality (z = −2.883, p = .003) and job contentment (z = −2.291, p = .02).
TABLE 4.
Mediating effects of resilience on the relationship between pandemic fatigue and nurse outcomes
| Model | B | SE | β | t | p | 95.0% Confidence Interval | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| Direct effects | |||||||
| Pandemic fatigue →mental health | −0.566 | 0.059 | −0.559 | −9.624 | .001 | −0.682 | −0.450 |
| Pandemic fatigue →job contentment | −0.403 | 0.061 | −0.420 | −6.606 | .001 | −0.523 | −0.283 |
| Pandemic fatigue →sleep quality | −0.918 | 0.156 | −0.381 | −5.879 | .001 | −1.226 | −0.610 |
| Resilience →mental health | 0.653 | 0.104 | 0.402 | 6.262 | .001 | 0.447 | 0.858 |
| Resilience →job contentment | 0.304 | 0.106 | 0.197 | 2.870 | .005 | 0.095 | 0.512 |
| Resilience →sleep quality | 1.143 | 0.259 | 0.295 | 4.412 | .001 | 0.632 | 1.654 |
| Pandemic fatigue →resilience | −0.160 | 0.042 | −0.257 | −3.803 | .001 | −0.243 | −0.077 |
| Indirect effects | |||||||
| Pandemic fatigue →resilience → mental health | −0.494 | 0.058 | −0.488 | −8.552 | .001 | −0.608 | −0.380 |
| Pandemic fatigue →resilience → job contentment | −0.380 | 0.063 | −0.395 | −6.027 | .001 | −0.504 | −0.255 |
| Pandemic fatigue →resilience → sleep quality | −0.787 | 0.158 | −0.326 | −4.981 | .001 | −1.099 | −0.476 |
FIGURE 1.
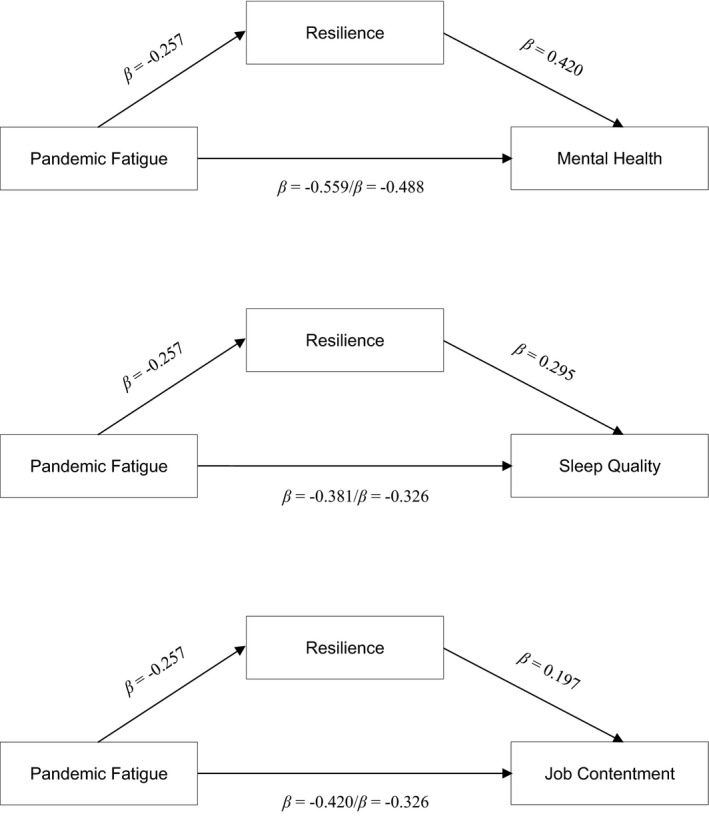
Hypothesized Models
4. DISCUSSION
Overall, the study findings provide support to the proposed hypothesized model. The results showed that nurses in the Philippines experienced moderate fatigue related to the coronavirus pandemic. Although we found no studies involving nurses that used a similar scale to measure pandemic fatigue, a previous study of the general population showed similar findings (Labrague & Ballad, 2021). The results of the current study are in line with international studies (Zhan et al., 2020; Zou et al., 2021) that showed nurses who work directly with COVID‐19 patients experience moderate‐to‐high levels of fatigue. Given the adverse consequences of fatigue, it is essential that institutional measures be in place to address this issue in nurses and promote their overall health and well‐being.
One important finding of the study was that nurses’ vaccination status strongly predicted pandemic fatigue, with nurses who received a COVID‐19 vaccine reporting lower levels of pandemic fatigue. However, this result should be interpreted with caution because of the large disparity in the percentage of nurses who did or did not receive a vaccine. Nevertheless, it appears that being vaccinated not only ensures that nurses are provided certain immunologic protection against the virus, but it may also reduce their fear and worry of becoming infected or infecting others, resulting in lower levels of pandemic fatigue. This is vital information because previous studies conducted in the early months of the pandemic found a significant proportion of nurses in many countries who expressed unwillingness, doubts and fear of caring for patients infected with the virus due to the lack of an effective vaccine (Khattak et al., 2020; Labrague & de los Santos, 2021). However, despite this evidence, it is worth noting that a significant proportion of nurses in the current study had not yet received a COVID‐19 vaccine. By providing frontline nurses with access to COVID‐19 vaccines, the continuity of care for infected patients can be assured, and nurses’ health and well‐being can be sustained.
Adequate staffing has been consistently cited in the literature as an important determinant of patient satisfaction, missed nursing care, adverse events and care quality (Blume et al., 2021). Moreover, a nursing work environment characterized by higher staffing levels was strongly associated with increased work satisfaction, job engagement, motivation, commitment and reduced turnover in nurses (Wang et al., 2021). In our study, higher levels of nurse staffing were associated with decreased pandemic fatigue. In other words, when there is enough staff, nurses’ are able to manage their workloads, thereby reducing stress, burnout and physical and mental exhaustion.
Research during the first few months of the pandemic correlated poor staffing ratios with increased patient workloads, leading to a higher incidence of anxiety, depression, anxiety and post‐traumatic stress disorder among nurses in Canada (Havaei et al., 2021). However, despite the relative importance of adequate staffing in reducing pandemic fatigue in nurses, fewer than 50% of nurses reported that the staffing levels in their units were ‘sufficient’ or ‘very sufficient’. With an increasing surge of patients, ensuring adequate staffing remains an important challenge among nurse administrators given the number of staff nurses who are infected or under quarantine. In the Philippines, the estimated number of nurses who were infected and/or placed under quarantine since the start of the pandemic has doubled, causing excess strain on the staffing levels in many hospitals (de los Santos & Labrague, 2021). This finding underscores the importance of human resource planning to ensure adequate staffing during the pandemic while maintaining the health and well‐being of nurses.
The regression analyses demonstrated that an increased pandemic fatigue score was associated with decreased scores for the mental health, sleep quality and job contentment measures. Since the emergence of the pandemic in late 2019, numerous studies have been conducted to examine how the pandemic impacts the mental health and psychological well‐being of health care workers, including nurses. Additionally, studies have shown how the various restrictions to control the disease, such as social distancing, quarantines, and stay‐at‐home orders, further worsened fatigue levels of nurses (Roberts et al., 2021), potentially affecting affect their work effectiveness and productivity. Consistent with earlier studies (Sagherian et al., 2020), our study found poorer mental health and reduced sleep quality in frontline nurses who experienced higher pandemic fatigue levels. Research involving health care workers including doctors, pharmacists and nursing assistants has also shown that fatigue associated with the pandemic may significantly affect sleep patterns and sleep quality (Teng et al., 2020; Zou et al., 2021).
The current study also demonstrated that increased levels of pandemic fatigue may adversely affect nurses’ job contentment. Our results support earlier research which showed that many nurses experienced work dissatisfaction and increased intention to leave their work due to the threat posed by the pandemic (Zhang et al., 2021; Pourteimour et al., 2021; Labrague & de los Santos, 2020). Evidence from the pre‐pandemic period showed that persistent exposure to fatigue might negatively affect job outcomes of nurses, such as reducing their work satisfaction and job engagement, increasing the frequency of absenteeism and increasing the intent to leave the organisation and the profession (Sagherian et al., 2017). If the issue of fatigue in nurses is not addressed, this may eventually drive nurses away from the profession, further worsening staffing problems and negatively affecting the delivery and quality of nursing care, leading to low patient satisfaction and, possibly, more instances of missed care and adverse events (Cho & Steege, 2021).
Mediation analysis showed that the effects of pandemic fatigue on nurses’ mental health, sleep quality and job contentment were partially mediated by resilience. Resilience seems to decrease the negative effects of pandemic fatigue on nurses’ sleep quality, mental health and job contentment. This result provides additional knowledge concerning the mediating effect of resilience on the relationship between pandemic fatigue and nurse well‐being. It was rather expected, as resilient individuals have been shown to more effectively handle stress, anxiety and other mental health issues during the pandemic compared to non‐resilient individuals (Labrague & de los Santos, 2020; Roberts et al., 2021; Yoruk & Guler, 2021). This leads to better sleep quality and, possibly, increased job contentment.
Resilience, or an individual's ability to rebound from traumatic or highly distressful events (Cooper et al., 2020), has been recognized as an important protective factor against various mental and psychological stressors, such as disease outbreaks (Pollock et al., 2020). During the COVID‐19 pandemic, fostering resilience in nurses led to them having less fear of the disease and less psychological distress, emotional exhaustion and depression, as well as improving their quality of life (Labrague, 2021; Roberts et al., 2021; Yoruk & Guler, 2021). Other studies have associated resilience with sustained clinical performance and job engagement (Lyu et al., 2020). Further, resilience partially moderated the effects of the various pandemic‐related stressors on nurses’ experience of psychological distress (Lorente et al., 2021). This finding underscores the relevance of early interventions directed towards enhancing resilience in nurses to reduce the negative effects of pandemic fatigue on nurses’ mental health, sleep quality and job contentment.
4.1. Limitations of the study
This study has some limitations. First, the clinical nurses included in this study were located in one geographical area of the Philippines. Therefore, future studies that involve nurses from other areas of the country may provide more generalizable results. The use of self‐report scales may potentially cause response bias. Further, establishing a causal link between the investigated variables is not possible because of the cross‐sectional nature of the research design. We recommend that future studies should utilize a more rigorous research design (e.g. randomized controlled trials) to test the efficacy of resilience interventions in reducing pandemic fatigue and other mental health issues in nurses during the current COVID‐19 pandemic. The partially mediating effect of resilience on the relationship between pandemic fatigue and clinical nurses’ mental health, sleep quality and job contentment indicates that other factors may not have been accounted for in this study. Hence, future studies should explore other personal factors (e.g. emotional intelligence, sense of coherence, coping, self‐efficacy) and organisational factors (e.g. adequacy of hospital resources, staffing levels, accreditation levels and the number of admitted patients) that might affect nurses’ well‐being.
4.2. Implications to nursing management
Given the adverse effects of pandemic‐associated fatigue on nurses’ mental health, sleep quality and job contentment, it is essential that measures to address pandemic fatigue be prioritized and implemented by hospital and nurse administrators. Ensuring adequate organisational support, access to mental health services and providing a safe nursing work environment will better support clinical nurses and promote their health and well‐being.
Because the vaccination status of clinical nurses strongly predicted pandemic fatigue, hospital administrators should ensure that nurses are provided access to COVID‐19 vaccines. This will ensure that nurses are immunologically protected from the virus, resulting in reduced pandemic fatigue, sustained work performance and better provision of patient care. Adequate staffing as an important predictor of pandemic fatigue highlights the importance of ensuring a sufficient workforce, particularly in COVID‐19‐designated units. Allocating more nurses to COVID‐19 units, providing adequate rest breaks and shorter duty hours and providing flexible scheduling may be helpful to reduce mental and physical pandemic‐associated fatigue in clinical nurses (Rieckert et al., 2021).
The mediating role of resilience underscores the importance of introducing interventions that focus on boosting resilience in nurses through empirically driven strategies, including educational interventions, mindfulness‐based resilience programmes and mindfulness self‐care (Badu et al., 2020). With the current restrictions regarding in‐person contact, resilience interventions delivered virtually, including cognitive behavioural therapy, online resilience webinars and workshop, and an interprofessional web‐based debriefing intervention (Azizoddin et al., 2020; Weiner et al., 2020) were shown to harness nurses’ resilience and sustain their mental health. Resilience in frontline nurses can be best supported by adequate organisational support and supportive leadership, including the implementation of a resilient work environment, adequate patient–nurse ratio, flexible work schedule, adequate supplies and equipment (e.g. PPEs), up‐to‐date information regarding the virus and mental health resources.
5. CONCLUSION
This study provides additional knowledge regarding the state of pandemic fatigue among clinical nurses who are on the frontline of the coronavirus pandemic. Overall, clinical nurses reported moderate levels of fatigue, with nurses who received a COVID‐19 vaccine and those who perceived adequate staffing reporting significantly lower levels of pandemic‐related fatigue. Further, resilience was seen to reduce the negative effects of pandemic fatigue on clinical nurses’ mental health, sleep quality and job contentment. Resilience‐promoting interventions may be vital to effectively support frontline clinical nurses’ mental health, improve their sleep quality and foster job satisfaction during the pandemic.
CONFLICT OF INTEREST
All authors declare no conflict of interest.
ETHICAL APPROVAL
This study received ethical approval from Samar State University Institutional Research Ethics Review Committee (IRERC) (IRERC EA‐001‐E).
ACKNOWLEDGEMENT
The authors would like to acknowledge and thank all nurses who participated in the study.
Labrague LJ. Pandemic fatigue and clinical nurses’ mental health, sleep quality and job contentment during the covid‐19 pandemic: The mediating role of resilience. J Nurs Manag. 2021;29:1992–2001. 10.1111/jonm.13383
Funding information
This study is non‐funded
REFERENCES
- Australian Psychological Society . (2020). Managing Lockdown Fatigue. The Australian Psychological Society. Limited. Accessed on October 5, 2020 https://www.psychology.org.au/getmedia/74e7a437‐997c‐4eea‐a49c‐30726ce94cf0/20APS‐IS‐COVID‐19‐Public‐Lockdown‐fatigue.pdf [Google Scholar]
- Azizoddin, D. R. , Vella Gray, K. , Dundin, A. , & Szyld, D. (2020). Bolstering clinician resilience through an interprofessional, webbased nightly debriefing program for emergency departments during the COVID‐19 pandemic. Journal of Interprofessional Care, 34(5), 711–715. [DOI] [PubMed] [Google Scholar]
- Badu, E. , O’Brien, A. P. , Mitchell, R. , Rubin, M. , James, C. , McNeil, K. , Nguyen, K. , & Giles, M. (2020). Workplace stress and resilience in the Australian nursing workforce: A comprehensive integrative review. International Journal of Mental Health Nursing, 29(1), 5–34. 10.1111/inm.12662 [DOI] [PubMed] [Google Scholar]
- Blume, K. S. , Dietermann, K. , Kirchner‐Heklau, U. , Winter, V. , Fleischer, S. , Kreidl, L. M. , Meyer, G. , & Schreyögg, J. (2021). Staffing levels and nursing‐sensitive patient outcomes: Umbrella review and qualitative study. Health Services Research. Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodeur, A. , Clark, A. E. , Fleche, S. , & Powdthavee, N. (2021). COVID‐19, lockdowns and well‐being: Evidence from Google Trends. Journal of Public Economics, 193, 104346. 10.1016/j.jpubeco.2020.104346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho, H. , & Steege, L. M. (2021). Nurse fatigue and nurse, patient safety, and organizational outcomes: A systematic review. Western Journal of Nursing Research, 0193945921990892. 10.1177/0193945921990892 [DOI] [PubMed] [Google Scholar]
- Cooper, A. L. , Brown, J. A. , Rees, C. S. , & Leslie, G. D. (2020). Nurse resilience: A concept analysis. International Journal of Mental Health Nursing, 29(4), 553–575. 10.1111/inm.12721 [DOI] [PubMed] [Google Scholar]
- del Carmen Giménez‐Espert, M. , Prado‐Gascó, V. , & Soto‐Rubio, A. (2020). Psychosocial Risks, Work Engagement, and Job Satisfaction of Nurses During COVID‐19 Pandemic. Frontiers in Public Health, 8, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de los Santos, J. A. A. , Labrague, L. J . (2021). The impact of fear of COVID‐19 on job stress, and turnover intentions of frontline nurses in the community: A cross‐sectional study in the Philippines. Traumatology, 27(1), 52–59. [Google Scholar]
- Goh, Y. S. , Ow Yong, Q. Y. J. , Chen, T. H. M. , Ho, S. H. C. , Chee, Y. I. C. , & Chee, T. T. (2021). The Impact of COVID‐19 on nurses working in a University Health System in Singapore: A qualitative descriptive study. International Journal of Mental Health Nursing, 30(3), 643–652. 10.1111/inm.12826 [DOI] [PubMed] [Google Scholar]
- Hart, P. L. , Brannan, J. D. , & De Chesnay, M. (2014). Resilience in nurses: An integrative review. Journal of Nursing Management, 22(6), 720–734. 10.1111/j.1365-2834.2012.01485.x [DOI] [PubMed] [Google Scholar]
- Havaei, F. , Ma, A. , Staempfli, S. , & MacPhee, M. (2021). Nurses’ workplace conditions impacting their mental health during COVID‐19: A cross‐sectional survey study. Healthcare, 9(1), 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang, H. J. , Kim, O. , Kim, S. , Kim, M. S. , Choi, J. A. , Kim, B. , Dan, H. , & Jung, H. (2021). Factors affecting physical and mental fatigue among female hospital nurses: The korea nurses’ health study. Healthcare, 9(2), 201–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khattak, S. R. , Saeed, I. , Rehman, S. U. , & Fayaz, M. (2020). Impact of fear of COVID‐19 pandemic on the mental health of nurses in Pakistan. Journal of Loss and Trauma, 1–15. [Google Scholar]
- Labrague, L. (2021). Psychological resilience, coping behaviors, and social support among healthcare workers during the COVID‐19 pandemic: A systematic review of quantitative studies. Journal of Nursing Management. Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague, L. , & Ballad, C. A. (2021). Lockdown fatigue among college students during the COVID‐19 pandemic: Predictive role of personal resilience, coping behaviors. and health. Perspective in Psychiatric Care. Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague, L. J. , & de los Santos, J. A. A. (2021). Prevalence and predictors of coronaphobia among frontline hospital and public health nurses. Public Health Nursing, 38(3), 382–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague, L. J. , & de Los Santos, J. A. A. (2021). Fear of Covid‐19, psychological distress, work satisfaction and turnover intention among frontline nurses. Journal of Nursing Management, 29(3), 395–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrague, L. J. , & de los Santos, J. A. A. (2020). COVID‐19 anxiety among front‐line nurses: Predictive role of organisational support, personal resilience and social support. Journal of Nursing Management, 28(7), 1653–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leng, M. , Wei, L. , Shi, X. , Cao, G. , Wei, Y. , Xu, H. , Wei, H. (2021). Mental distress and influencing factors in nurses caring for patients with COVID‐19. Nursing in Critical Care, 26(2), 94–101. [DOI] [PubMed] [Google Scholar]
- Lorente, L. , Vera, M. , & Peiró, T. (2021). Nurses´ stressors and psychological distress during the COVID‐19 pandemic: The mediating role of coping and resilience. Journal of Advanced Nursing, 77(3), 1335–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyu, H. , Yao, M. , Zhang, D. , & Liu, X. (2020). The Relationship Among Organizational Identity, Psychological Resilience and Work Engagement of the First‐Line Nurses in the Prevention and Control of COVID‐19 Based on Structural Equation Model. Risk Management and Healthcare Policy, 13, 2379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majumdar, P. , Biswas, A. , & Sahu, S. (2020). COVID‐19 pandemic and lockdown: Cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronobiology International, 37(8), 1191–1200. [DOI] [PubMed] [Google Scholar]
- Meo, S. A. , Al‐Khlaiwi, T. , Usmani, A. M. , Meo, A. S. , Klonoff, D. C. , & Hoang, T. D. (2020). Biological and epidemiological trends in the prevalence and mortality due to outbreaks of novel coronavirus COVID‐19. Journal of King Saud University‐Science, 32(4), 2495–2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nitschke, J. P. , Forbes, P. A. , Ali, N. , Cutler, J. , Apps, M. A. , Lockwood, P. L. , & Lamm, C. (2021). Resilience during uncertainty? Greater social connectedness during COVID‐19 lockdown is associated with reduced distress and fatigue. British Journal of Health Psychology, 26(2), 553–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollock, A. , Campbell, P. , Cheyne, J. , Cowie, J. , Davis, B. , McCallum, J. , Maxwell, M. (2020). Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database of Systematic Reviews, (11). Ahead of Print [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pourteimour, S. , Yaghmaei, S. , & Babamohamadi, H. (2021). The relationship between mental workload and job performance among Iranian nurses providing care to COVID‐19 patients: A cross‐sectional study. Journal of Nursing Management. Ahead of Print [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rieckert, A. , Schuit, E. , Bleijenberg, N. , ten Cate, D. , de Lange, W. , de Man‐van Ginkel, J. M. , Mathijssen, E. , Smit, L. C. , Stalpers, D. , Schoonhoven, L. , Veldhuizen, J. D. , & Trappenburg, J. C. A. (2021). How can we build and maintain the resilience of our health care professionals during COVID‐19? Recommendations based on a scoping review. British Medical Journal Open, 11(1).e043718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts, N. J. , McAloney‐Kocaman, K. , Lippiett, K. , Ray, E. , Welch, L. , & Kelly, C. (2021). Levels of resilience, anxiety and depression in nurses working in respiratory clinical areas during the COVID pandemic. Respiratory Medicine, 176.106219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagherian, K. , Steege, L. M. , Cobb, S. J. , & Cho, H. (2020). Insomnia, fatigue and psychosocial well‐being during COVID‐19 pandemic: A cross‐sectional survey of hospital nursing staff in the United States. Journal of Clinical Nursing. Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagherian, K. , Clinton, M. E. , Abu‐Saad Huijer, H. , & Geiger‐Brown, J. (2017). Fatigue, work schedules, and perceived performance in bedside care nurses. Workplace health & safety, 65(7), 304–312. [DOI] [PubMed] [Google Scholar]
- Smith, B. W. , Dalen, J. , Wiggins, K. , Tooley, E. , Christopher, P. , & Bernard, J. (2008). The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine, 15(3), 194–200. [DOI] [PubMed] [Google Scholar]
- Snyder, E. , Cai, B. , DeMuro, C. , Morrison, M. F. , & Ball, W. (2018). A new single‐item sleep quality scale: Results of psychometric evaluation in patients with chronic primary insomnia and depression. Journal of Clinical Sleep Medicine, 14(11), 1849–1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son, H. , Lee, W. J. , Kim, H. S. , Lee, K. S. , & You, M. (2019). Hospital workers’ psychological resilience after the 2015 Middle East respiratory syndrome outbreak. Social Behavior and Personality: an International Journal, 47(2), 1–13. [Google Scholar]
- Taunton, R. L. , Bott, M. J. , Koehn, M. L. , Miller, P. , Rindner, E. , Pace, K. , Elliott, C. , Bradley, K. J. , Boyle, D. , & Dunton, N. (2004). The NDNQI‐adapted index of work satisfaction. Journal of Nursing Measurement, 12(2), 101–122. [DOI] [PubMed] [Google Scholar]
- Teng, Z. , Wei, Z. , Qiu, Y. , Tan, Y. , Chen, J. , Tang, H. , Wu, H. , Wu, R. , & Huang, J. (2020). Psychological status and fatigue of frontline staff two months after the COVID‐19 pandemic outbreak in China: A cross‐sectional study. Journal of Affective Disorders, 275, 247–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher, K. , Jackson, D. , Durkin, J. , Gyamfi, N. , & Bhullar, N. (2020). Pandemic‐related behaviours and psychological outcomes; A rapid literature review to explain COVID‐19 behaviours. International Journal of Mental Health Nursing, 29(6), 1018–1034. [DOI] [PubMed] [Google Scholar]
- Wang, L. , Chen, H. , Wan, Q. , Cao, T. , Dong, X. U. , Huang, X. , Lu, H. , & Shang, S. (2021). Effects of self‐rated workload and nurse staffing on work engagement among nurses: A cross‐sectional survey. Journal of Nursing Management. Ahead of Print. [DOI] [PubMed] [Google Scholar]
- Weiner, L. , Berna, F. , Nourry, N. , Severac, F. , Vidailhet, P. , & Mengin, A. C. (2020). Efficacy of an online cognitive behavioral therapy program developed for healthcare workers during the COVID‐19 pandemic: the REduction of STress (REST) study protocol for a randomized controlled trial. Trials, 21(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World health organization (2020). Pandemic fatigue: Reinvigorating the public to prevent COVID‐19. Accessed date: March 3, 2021 https://apps.who.int/iris/bitstream/handle/10665/335820/WHO‐EURO‐2020‐1160‐40906‐55390‐eng.pdf [Google Scholar]
- Yörük, S. , & Güler, D. (2021). The relationship between psychological resilience, burnout, stress, and sociodemographic factors with depression in nurses and midwives during the COVID‐19 pandemic: A cross‐sectional study in Turkey. Perspectives in Psychiatric Care, 57(1), 390–398. [DOI] [PubMed] [Google Scholar]
- Zhan, Y.‐X. , Zhao, S.‐Y. , Yuan, J. , Liu, H. , Liu, Y.‐F. , Gui, L.‐L. , Zheng, H. , Zhou, Y.‐M. , Qiu, L.‐H. , Chen, J.‐H. , Yu, J.‐H. , & Li, S.‐Y. (2020). Prevalence and influencing factors on fatigue of first‐line nurses combating with COVID‐19 in China: A descriptive cross‐sectional study. Current Medical Science, 40(4), 625–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, S. X. , Chen, J. , Jahanshahi, A. A. , Alvarez‐Risco, A. , Dai, H. , Li, J. , & Patty‐Tito, R. M. (2021). Succumbing to the COVID‐19 pandemic—healthcare workers not satisfied and intend to leave their jobs. International Journal of Mental Health and Addiction. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou, X. , Liu, S. , Li, J. , Chen, W. , Ye, J. , Yang, Y. , … & Ling, L. (2021). Factors Associated With Healthcare Workers' Insomnia Symptoms and Fatigue in the Fight Against COVID‐19, and the Role of Organizational Support. Frontiers in Psychiatry, 12,356. 10.3389/fpsyt.2021.652717 [DOI] [PMC free article] [PubMed] [Google Scholar]


