Abstract
Nonalcoholic fatty liver disease (NAFLD) is one of the most common causes of chronic liver disease in the world. The rising prevalence of nonalcoholic steatohepatitis (NASH) has led to a 170% increase in NASH cirrhosis as the listing indication for liver transplantation from 2004 to 2013. As of 2018, NASH has overtaken hepatitis C as an indication for liver transplantation in the USA. After liver transplantation, the allograft often develops recurrent NAFLD among patients with known NASH cirrhosis. In addition to recurrent disease, de novo NAFLD has been reported in patients with other indications for liver transplantation. In this review, we will discuss the risk factors associated with recurrent and de novo NAFLD, natural course of the disease, and management strategies after liver transplantation.
Keywords: Nonalcoholic fatty liver disease, Nonalcoholic steatohepatitis, Post-transplant, Recurrent NAFLD, De novo NAFLD, Recurrent NASH, De novo NASH
Introduction
Nonalcoholic fatty liver disease (NAFLD) is the leading cause of chronic liver disease in the western world, and is strongly associated with metabolic syndrome, often referred to as the liver manifestation of metabolic syndrome.1 NAFLD is also among the most common indications for orthotopic liver transplantation (OLT) in the USA.2 The metabolic syndrome persists after liver transplant and is often further exacerbated among NAFLD patients, thereby leading to recurrence of NAFLD in the allograft.3,4 Aside from recurrent NAFLD, patients transplanted for other etiologies of liver disease are also at risk of new onset metabolic syndrome and de novo NAFLD in the allograft due to post-OLT weight gain and immunosuppression side effects.5 Differentiating between recurrent versus de novo NAFLD is challenging and is currently limited to pre-OLT identification of NAFLD. In this review, we will discuss recurrent and de novo NAFLD, their associated risk factors, natural course of the disease, diagnosis, and management strategies.
Epidemiology
NAFLD is the most common etiology of chronic liver disease, with a global prevalence of 25%. Regions with higher prevalence include the Middle East (31.8%) and South America (30.4%), while in North America, the estimated prevalence is 24.1%.6 The rise in the prevalence of NAFLD over the last three decades has mirrored the global epidemic of obesity, type 2 diabetes mellitus (T2DM), and metabolic syndrome. A recent study estimated a 63% increase in the prevalence of nonalcoholic steatohepatitis (NASH) in the USA by 2030, accompanied by a 168% rise in decompensated NASH cirrhosis patients.7 With such a steep increase in the incidence and prevalence of NASH and metabolic syndrome, there has been a parallel rise in NASH-related decompensated cirrhosis, recently surpassing hepatitis C (commonly referred to as HCV) as an indication for OLT in the USA.2,8
The initial studies reviewing recurrence of NAFLD post-OLT based on protocol liver biopsies demonstrated universal 100% recurrence within 5-years compared to 25% of de novo NAFLD post-OLT.3 Follow up studies have shown variable results, with recurrence rates for steatosis ranging from 8% to 100% in known NASH patients, with follow-up ranging from 1 year to >5 years post-OLT; recurrent NASH rates over a similar follow up period ranged between 38–57%. In comparison, incidence of de novo NAFLD varied from 18% to up to 78% for steatosis over a similar range of follow-up, while de novo NASH ranged from 13% to 17%.3–5,9–15 Recurrent NAFLD after transplant is more common compared to de novo NAFLD. It is important to note that all the above studies utilized histology to arrive at the diagnosis, with biopsies being pursued based on institutional protocols or due to abnormal liver labs. Recurrent NAFLD was reported at lower rates when imaging, specifically computed tomography (CT), was utilized, with 1-year recurrence of 12% and 5-year recurrence of 33%.16
Histology and diagnosis
NAFLD encompasses a wide spectrum of histopathological states, which includes simple hepatic steatosis or nonalcoholic fatty liver (NAFL) to NASH highlighted by hepatocyte injury and inflammation which may or may not be accompanied by fibrosis.1 Quantitative histological scoring systems, like the NAFLD activity score and the Steatosis, Activity, Fibrosis assessment, have been identified and widely used to diagnose NAFLD.17,18 In contrast, no histological scoring systems currently exist to assess NAFLD in the post-transplant allograft. As such, differentiating between recurrent NAFLD and de novo NAFLD is limited to its clinical diagnosis based on pre-existing disease prior to OLT.19
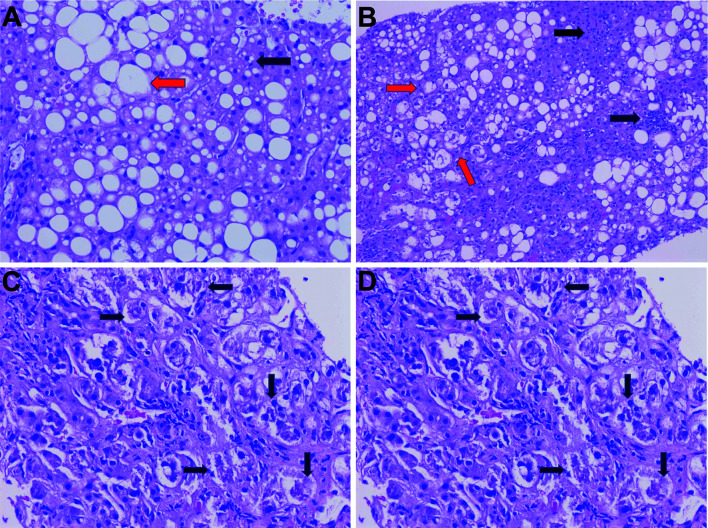
Liver biopsy remains the gold standard for diagnosis of post-OLT NAFLD/NASH (Fig. 1). There are multiple possible causes for elevated liver enzymes post-OLT that are not easily differentiated without a biopsy. The indications for biopsy in a post-OLT patient include confirmation of NAFLD (recurrent or de novo), fibrosis, or elevated liver enzymes that require further evaluation.20 While liver biopsy is safe in the post-OLT patient with low risk of complications, it remains an invasive test.21 Currently available noninvasive tests can help to direct clinic care but often lack the granularity offered by histology from a liver biopsy.
Fig. 1. Post-liver transplant NAFLD histology findings.
(A) Macrovesicular steatosis with presence of both small droplet (black arrow) and large droplet (H&E, 200×). (B) Steatohepatitis with several hepatocytes exhibiting ballooning degeneration (red arrow) and chronic lobular inflammation (black arrows) (H&E, 100×). (C) Mallory-Denk bodies (black arrows) in ballooned hepatocytes (H&E, 200×). (D) Characteristic centrizonal pericellular fibrosis in steatohepatitis radiating around a terminal branch of the central vein. Note the ballooned hepatocytes (black arrows) (Masson-Trichrome stain, 100×). H&E, hematoxylin-eosin.
Steatosis is commonly encountered after liver transplantation. Steatosis is often noted incidentally on imaging for protocol testing or on imaging done for abnormal liver enzymes.19 To identify steatosis, ultrasound requires the presence of moderate or greater degree of steatosis, defined as >30% involvement of hepatic parenchyma. Ultrasound carries a sensitivity of 65% and specificity of 75% to identify hepatic steatosis. CT scan’s ability to identify steatosis is similar to that of ultrasound. In comparison, magnetic resonance imaging (MRI) is vastly superior at identifying steatosis, with 90% sensitivity and 91% specificity.22 However, imaging modalities are unable to differentiate between NAFL and NASH, as their strengths lie in identifying patients who may need more specific testing or monitoring of steatosis.
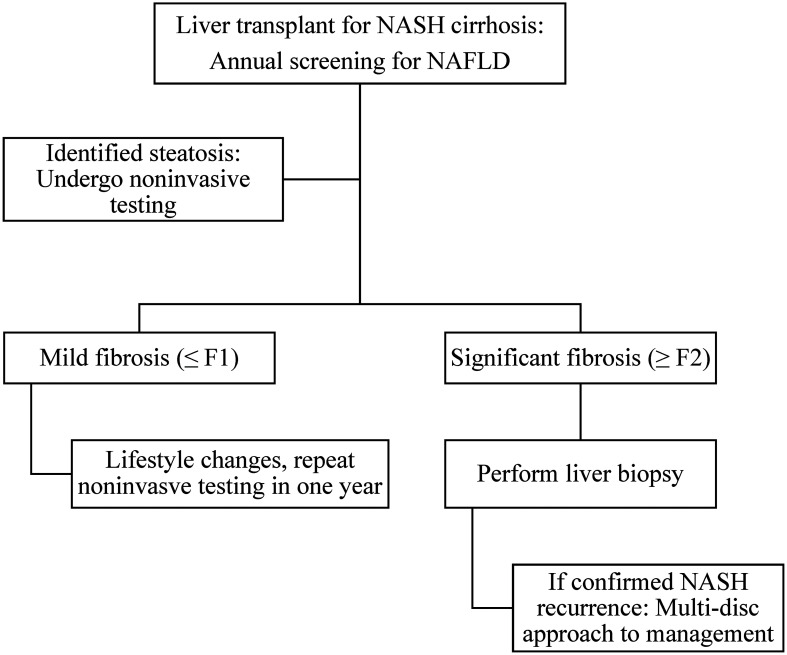
The use of noninvasive testing for fibrosis assessment in patients with chronic liver disease is increasingly common. There is a growing body of literature in post-OLT patients; however, they carry a few limitations. The allograft itself may have post-surgical preservation injury or presurgical changes of fibrosis that increase graft stiffness. Acute cellular rejection or presence of inflammation can influence liver stiffness measurements.23 A meta-analysis evaluating noninvasive methods to identify fibrosis after transplant revealed that transient elastography performed better than serum biomarkers, such as the aspartate aminotransferase to platelet ratio index and FIB-4. However, most of the studies included in this analysis had evaluated recurrent HCV and none looked specifically into NAFLD recurrence, so more data is required in this population.24 Magnetic resonance elastography (commonly known as MRE) has been studied in small cohorts to identify fibrosis in post-OLT patients.25 However, there is a relative lack of evidence regarding MRE in NAFLD patients post-OLT. Fibrosis assessment remains helpful to the clinician in identifying patients with advanced fibrosis. Noninvasive testing has some potential advantages in post-OLT monitoring of NAFLD given its limited side effects. Patients who have an established diagnosis of recurrent or de novo NAFLD can likely be followed with serial noninvasive testing to determine if they have advancing fibrotic disease. These changes likely need confirmation with biopsy, however, given the current lack of data regarding fibrosis monitoring and the myriad of factors that can influence these markers in transplant patients. A proposed algorithm for screening and diagnostic evaluation is included in Figure 2.
Fig. 2. Screening algorithm for post-liver transplant patients.
Annual screening for NAFLD is recommended, with an ultrasound. If NAFLD is identified or suspected by ultrasound or elevated liver enzymes, noninvasive testing can be performed by a combination of transient elastography with serum biomarkers, such as FIB-4. If mild fibrosis (≤F1) is present, lifestyle changes, including diet and weight loss, are recommended. If significant fibrosis (≥F2) is suspected, a liver biopsy is recommended. If findings are confirmed, a multidisciplinary approach should be adopted to assist with weight loss and management of metabolic syndrome co-morbidities.
Risk factors for NAFLD in allograft
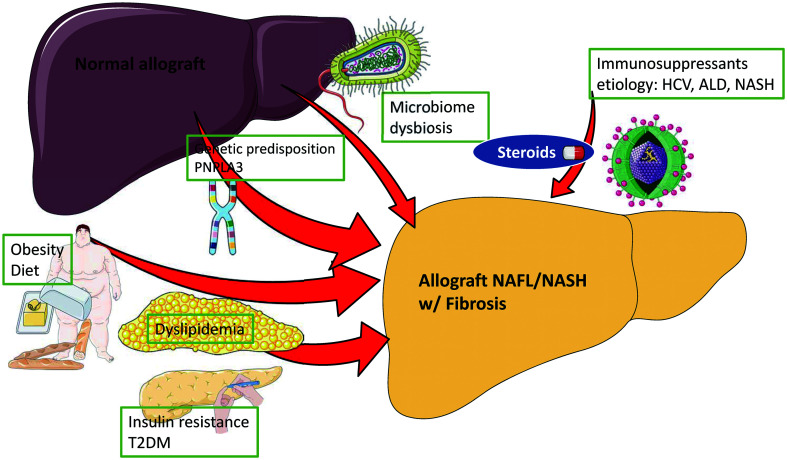
Historically, the pathogenesis of NAFLD was postulated to be a “tale of two hits”, beginning with fat deposition in the liver and followed by inflammation; however, our current understanding suggests that NAFLD is a complex disorder with multiple pathways, all contributing to steatosis, inflammation, and fibrosis.26,27 A combination of environmental factors in genetically-predisposed individuals leads to insulin resistance, altered lipid homeostasis, dysbiosis of gut microbiome leading to hepatic steatosis, and initiation of the inflammatory cascade leading to steatohepatitis and fibrosis development by activation of stellate cells.28 Significant investigative effort has been put forth to understand this process in the non-transplant setting. On the other hand, the pathogenesis of recurrent or de novo NAFLD post-OLT has not been well delineated but similar processes (Fig. 3) are suspected to play a role in post-OLT NAFLD.
Fig. 3. Factors involved in the pathogenesis of post-liver transplant NAFLD.
Factors similar to non-transplant NAFLD are suspected to play a role in post-liver transplant NAFLD. In addition, some post-transplant factors have also been shown to be associated with post-transplant NAFLD.
Post-transplant patients carry multiple risk factors for developing NAFLD in the allograft, including pre-OLT body mass index (BMI), significant weight gain after OLT, pre-existing metabolic syndrome risk factors in patients with NASH cirrhosis pre-OLT, and high likelihood of developing metabolic syndrome post-OLT due to immunosuppressants and donor graft characteristics. These are summarized in Table 1.
Table 1. Summary of factors associated with post-liver transplant NAFLD.
| Increased risk | Possible risk | Possible protection |
|---|---|---|
| Obesity | Sarcopenia | Everolimus |
| T2DM | CNI therapy | |
| Hyperlipidemia | Donor graft steatosis | |
| PNPLA3 polymorphism | ||
| Corticosteroid therapy | ||
| Indications: NASH, ALD, HCV |
Obesity and sarcopenia
Obesity remains a well-known risk factor for NAFLD. Among studies reviewing pre-OLT BMI, two retrospective studies reported pre-OLT BMI as an associated risk factor for post-OLT NAFLD.4,29 In comparison, post-OLT BMI, often calculated at time of the liver biopsy, was noted to carry a higher risk for post-OLT NAFLD.4,5,29–31 Weight gain post-OLT carried the highest odds ratio (19.38 [95%CI: 3.5–107.4]) in a small retrospective study of 68 patients, with weight gain defined as an increase in BMI by greater than 10%.13 This risk of post-OLT NAFLD needs to be balanced against the expected weight gain early after liver transplantation in the majority of patients who are sarcopenic and against studies supporting survival and graft benefit with post-OLT weight gain.32 Worsening sarcopenia post-OLT was associated with increased risk of new onset diabetes mellites in a single small study;33 however, studies associating sarcopenia to post-OLT NAFLD are lacking. Future studies should consider focusing on assessing the ratio between gain in skeletal muscle mass versus overall weight gain in order to improve our understanding of obesity and post-OLT NAFLD.
Insulin resistance and diabetes mellitus
Insulin resistance is often viewed as the defining feature of metabolic syndrome and is strongly associated with NAFLD.1 While multiple studies looking at pre-existing T2DM and post-OLT NAFLD have failed to show a significant association.3,4,12,13,15,29,31 some have shown an increased risk of post-OLT NAFLD among known diabetic patients.30,34,35 New onset T2DM after liver transplantation, in particular poorly controlled T2DM, was associated with a higher risk of post-OLT NAFLD.5,29,30,36 Tight glucose control, sparing using of corticosteroids, and early referrals to endocrinology should be considered to decrease the risk of NAFLD disease progression in this patient population.19,37
Hypertension
While pre-OLT hypertension remains a key part of metabolic syndrome and strongly associated with NAFLD, it lacks any significant association to post-OLT NAFLD.4,9,12,13,15,29,31 Onset of post-OLT hypertension is common, but has not shown any significant association on multivariate analysis across multiple studies to date,4,12,15,16,29,30,38 except for a single study by Dumortier et al.5 that showed a positive association. A potential reason for a surprising lack of association could be related to the duration of follow-up in the above studies.
Hyperlipidemia
Pre-OLT hyperlipidemia was not associated with an increased risk of post-OLT NAFLD despite its known association to NAFLD.4,9,13,15,29,31 In contrast, post-OLT hyperlipidemia had mixed results in multivariate analysis, with a few studies supporting a positive association to post-OLT NAFLD,4,5,29 while others failed to show a significant association.15,16,30,31
Immunosuppression
Immunosuppressants are linked to multiple aspects of metabolic syndrome, with post-OLT corticosteroid treatment known to increase risk of obesity, worsening existing T2DM, increasing the risk of new onset diabetes mellitus, hypertension, and hyperlipidemia.20 Studies directly linking post-OLT NAFLD to corticosteroids use and duration are limited to two small retrospective studies.3,39 Despite limited data, use of corticosteroids should be minimized with early tapers.
Insulin resistance, hypertension, and hyperlipidemia are well recognized side effects of calcineurin inhibitors (CNIs), with tacrolimus more strongly associated with insulin resistance, while cyclosporine is known to worsen hypertension.19,20 Studies linking CNI therapy to NAFLD are few, with a single retrospective study associating tacrolimus use with increased risk of post-OLT NAFLD on multivariate analysis,5 while other studies’ findings have failed to support this association.4,15,29,30
Retrospective studies reviewing mammalian target of rapamycin (i.e. mTOR) inhibitors are limited in size and have not shown any significant association to post-OLT NAFLD.5,13,29,30 In a randomized multicenter study, decreasing exposures to tacrolimus by adding everolimus was associated with less weight gain over 2-year follow up, suggesting potential protective effects against onset of metabolic syndrome and post-OLT NAFLD.40
Other factors
NASH is a well-known, strong risk factor for recurrent NAFLD in the allograft. In addition to NASH, alcohol-related liver disease (ALD) cirrhosis and HCV cirrhosis (as primary etiologies of liver disease) were noted to carry a higher risk for de novo NASH in small retrospective studies, while auto-immune etiologies seemed to carry the lowest risk of de novo NAFLD.5,29,30 Finkenstedt et al.16 highlighted the role of recipient genetics, showing that the presence of G-allele in rs738409 of PNPLA3, a known risk factor for NASH, among OLT recipients increased their risk for graft steatosis based on CT imaging. Donor graft steatosis led to mixed results from small studies, with two studies5,31 suggesting increased risk of post-OLT NAFLD, while multiple studies failed to show any significant association.11,12,29,30 Factors associated with the liver transplantation, such as the model for end-stage liver disease score at transplant4,12,29,38 and cold or warm ischemia time, did not carry any significant risk.10,12
Natural history and outcomes
Long-term follow-up studies of NAFLD in the nontransplant setting have found a slowly progressive disease, with time to progression between stages of fibrosis approximated as ∼7 years per stage for NASH patients.41 As noted above, allograft NAFL and NASH was more common in the recurrent NAFLD group when compared to de novo NAFLD. Despite recurrent steatosis and inflammation in both groups, risk of progression to advanced fibrosis (≥F3 stage) and cirrhosis was overall low in both groups, with a few exceptions; decompensated cirrhosis or graft loss due to post-OLT NAFLD was uncommon.
Studies reviewing patients transplanted for NASH or cryptogenic cirrhosis presumed to be NASH, demonstrated the prevalence of advanced fibrosis to be 2–5% at 5 years, 5–10% at 10 years, and up to 24% in one of the studies that followed patients up to 15 years.3,4,9,15 The single exception to this was the French study by Vallin et al.,42 which reported the prevalence of advanced fibrosis at 71.4% in its recurrent NAFLD group at 5 years. Progression to advanced fibrosis was mixed in the de novo group, with a 10-year prevalence rate of 2.3% for advanced fibrosis reported by Dumortier et al.5 compared against the significantly higher prevalence of 20% for advanced fibrosis reported by Galvin et al.30 A possible explanation for such discrepancy between the two studies could be due to a difference in patient characteristics, with the latter group having a higher BMI and higher prevalence of T2DM. In studies comparing progression of fibrosis between recurrent and de novo NAFLD groups, mixed results were noted with higher rates of advanced fibrosis at 5 years in the recurrent NAFLD group compared to the de novo NAFLD group.42 These findings were not supported by two larger studies, which showed no significant difference in fibrosis progression between recurrent and de novo NAFLD.29,38 As such, we suspect that the risk of progressive fibrosis is not statistically different between recurrent and de novo NAFLD, but further studies with a closer assessment of individual risk factors to fibrosis accompanied with protocoled liver biopsies are needed.
Post-OLT NAFL or NASH, either recurrent or de novo, were not associated with decreased survival or graft loss across retrospective studies, with up to 15 years follow-up data.29,30,38 Similarly, post-OLT NAFLD was not associated with a higher risk of cardiovascular events or cardiovascular mortality.29,38 While these findings are re-assuring, further studies are needed to support these results. The reported 1-, 3-, and 5-year survival rates are similar in patients transplanted for NASH compared to ALD, viral hepatitis, or autoimmune diseases, with the exception of lower survival in patients with NASH and concomitant hepatocellular carcinoma compared to other indications.43,44
Prevention and management
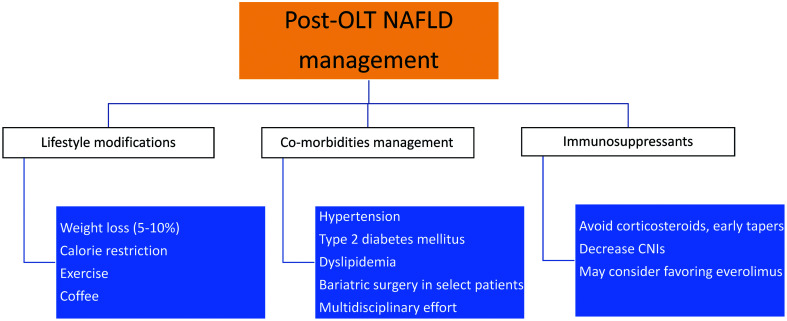
Currently, there are no Food and Drug Administration approved treatment options available for NAFLD in the pre-transplant setting, and no drugs have been studied or approved for post-transplant NAFLD. Management for post-OLT NAFLD is extrapolated from non-transplant NAFLD management and relies heavily on lifestyle modification and optimization of their metabolic and medical comorbidities, as summarized in Figure 4.
Fig. 4. Management for post-liver transplant NAFLD.
The cornerstone for management of post-OLT NAFLD is weight loss by lifestyle modifications. When present, metabolic comorbidities should be tightly controlled, with early involvement of consultants for a multidisciplinary approach. Bariatric surgery may be an option for a select few patients. Immunosuppression optimization should focus on protecting the graft but, when feasible, these corrections should be pursued to decrease their side effects.
Prevention
Pre-transplant identification of risk factors, such as obesity, sarcopenia, and uncontrolled T2DM, should be optimized aggressively prior to transplant. Bariatric surgery has been studied among NAFLD patients, with excellent improvement in steatosis, steatohepatitis, and fibrosis, while laparoscopic bariatric surgery approaches have been shown to be safe in compensated cirrhosis patients.45–47 In the transplant setting, simultaneous sleeve gastrectomy during OLT has been compared to weight loss pre-OLT, with lower rates of graft loss and new onset T2DM reported in the sleeve gastrectomy group.48 These approaches require a multidisciplinary effort at large volume transplant centers with clinical experience and expertise, and further studies are required to optimize patient selection and timing of bariatric surgery in the pre-transplant setting. Sarcopenia, while not directly associated with post-OLT NAFLD, is an important predictor of OLT outcomes and hence requires aggressive management with early intervention, optimization of nutrition in combination with muscle toning and strengthening exercise programs that would improve post-OLT outcomes.49
Aside from recipient optimization, donor graft allocation has been an area of contention among NASH recipients, as steatosis and PNPLA3 polymorphism in donor graft may potentially add to the risk of post-OLT NAFLD. In the era of donor shortage accompanied by a surge in prevalence of NAFLD within the potential donor pool, optimization strategies and prospective studies are needed to decrease ischemia/reperfusion injury and to better understand the long-term effects of these on the natural course and risk of post-OLT NAFLD.50
Prevention of post-OLT NAFLD requires a multidisciplinary approach to avoid excess weight gain post-liver transplant, treatment of metabolic comorbidities as discussed below, and among patients without metabolic syndrome, implementing routine screening for glucose intolerance, hypertension, and hyperlipidemia.19,20
Lifestyle modification
The management for all NAFLD patients, whether pre- or post-OLT, should start with lifestyle modification, with the goal of gradual but sustained weight loss. However, in the initial few weeks to months after liver transplantation, patients are still recovering from their sarcopenic and debilitated state and often need to gain weight and muscle mass. The data discussed below are from studies in non-transplant NAFLD patients, and the optimal time of initiating these recommendations should be tailored to individual patients based on their recovery and risk factors.
Weight loss has been shown to improve all histological features of NAFLD, with 5% of weight loss required for improvement in steatosis, 7% required for steatohepatitis reduction, and 10% over 12 months for fibrosis regression.51 While longitudinal studies to confirm similar changes in post-OLT NAFLD are lacking, we would suggest similar goals for these patients. Weight loss is best achieved through a calorie deficit, and the daily deficit goal should be adjusted based on the patient’s basal metabolic rate. The Mediterranean diet, often higher in monosaturated fatty acids, has been shown to reduce steatosis. In general, despite multiple options for macronutrient-specific diets studied, when choosing isocaloric diets, no significant difference in weight loss has been noted in patients choosing low-fat, low-carbohydrate, or high-protein diets; we would still recommend a diet low in carbohydrate for improving insulin resistance. Lastly, weight loss is challenging and diet modifications often require expert guidance; hence, choosing a multidisciplinary approach with the assistance of a nutritionist is recommended.52
Exercise offers a synergistic effect in hepatic fat mobilization when paired with calorie restriction, and either aerobic or resistance exercises, or both, may be pursued based on the patient’s cardiopulmonary fitness, as both exercises lead to similar improvement in hepatic steatosis.53 Drinking coffee confers a protective effect against multiple chronic liver diseases, including NAFLD, ALD, and viral hepatitis.54 Patients should, therefore, be encouraged to drink 1–2 cups of unsweetened filtered coffee daily. The association of prebiotics, probiotics, and the gut microbiome to metabolic syndrome and NAFLD are areas of great interest with emerging data, but their benefits in the post-OLT NAFLD population needs to be explored further. Similarly, circadian rhythm, the importance of good sleep hygiene, and optimal sleep duration of 7–8 h/night have been shown to be associated with NAFLD, but further studies are needed to study their association to post-OLT NAFLD patients.
Management of comorbidities
Management of the majority of comorbidities among post-OLT patients is comparable to the general population, but the increased risk of renal insufficiency in post-OLT patients from their immunosuppressive therapy needs to be remembered. Drug-to-drug interactions with immunosuppressants should be evaluated when initiating newer therapies. Initial hypertension management should begin with sodium restriction, weight loss, and exercise, followed by first-line therapy with dihydropyridine calcium channel blockers, such as amlodipine or nifedipine, as they counteract the vasoconstrictive effect of CNIs.55 Second-line therapy options include beta-blockers in patients without proteinuria, while an angiotensin converting enzyme inhibitor or angiotensin receptor blocker should be used in patients with T2DM and proteinuria.20 Statin therapy should be initiated for dyslipidemia if lifestyle modification fails to correct elevated low-density lipoprotein cholesterol levels (>100 mg/dL when fasting), while closely monitoring for hepatotoxicity and drug-to-drug interaction with CNIs. Initial therapy for hypertriglyceridemia includes fish oil, up to 4 g per day, followed by fibrate therapy if persistently elevated.19,20
Diabetes management often requires endocrine consultation, as patients routinely need insulin therapy among both pre-existing T2DM and new onset diabetes patients, especially when corticosteroids are a part of their immunosuppression regimen. Oral hypoglycemic agents, thiazolidinediones, glucagon-like peptide-1 analogues, and dipeptidyl peptidase-4 inhibitors have been studied in non-transplant NAFLD patients, yielding promising results, and may be considered as the preferred therapeutic options post-OLT as well.19,52 Bariatric surgery after liver transplant can lead to significant weight loss and decreased insulin requirement, as shown in a small study of select patients.56
Immunosuppression
Immunosuppressant therapy is vital in improving allograft survival and outcomes but, unfortunately, they are accompanied by multiple side effects, including altered metabolic homeostasis. Among the immunosuppressants, corticosteroids carry the highest risk of diabetes, hypertension, obesity, and hyperlipidemia, and as such early tapering regimens are recommended.20 CNIs are linked to hypertension, diabetes, and hyperlipidemia, as discussed previously and dose reduction should be considered in patients with these comorbidities, especially when they remain refractory to medical therapy.19,20 The mTOR inhibitors are associated with significant hyperlipidemia, and an alternate immunosuppressant should be considered when hyperlipidemia remains uncontrolled.57 Among the mTOR inhibitors, everolimus has been associated with decreased weight gain in a small study, but longitudinal studies are needed to extend this benefit to post-NAFLD population.40
Conclusions
The epidemic of NAFLD, in parallel with obesity and metabolic syndrome, is expected to worsen and add to the growing burden of the post-liver transplant population. After liver transplantation, both recurrent and de novo NAFLD are common, and their prevalence will likely rise in the upcoming decades. Future basic science studies should help identify any differences between the pathogenesis of non-transplant versus post-OLT NAFLD. Clinically, longitudinal studies are needed to characterize the natural disease course of post-OLT NAFLD, using protocoled follow-up with noninvasive studies ideally paired with liver biopsies. Among the noninvasive tests, fibrosis assessment tools such as transient elastography and MRE, are of interest to assess disease progression. Additionally, management strategies and their effects on post-OLT NAFLD require long-term studies, with a focus on cardiovascular complications in addition to allograft and survival outcomes. As our post-liver transplant population continues to age, filling the aforementioned knowledge gaps will help to improve the transplant community’s ability to better serve them.
Acknowledgments
Some figures were created with “Biological illustration” (http://smart.servier.com) by Servier, used under the Creative Commons Attributions 3.0 Unported License, and modified by Akshay Shetty.
Abbreviations
- ALD
alcohol-related liver disease
- BMI
body mass index
- CNI
calcineurin inhibitor
- CT
computed tomography
- HCV
hepatitis C virus
- MRE
magnetic resonance elastography
- MRI
magnetic resonance imaging
- NAFL
nonalcoholic fatty liver
- NAFLD
nonalcoholic fatty liver disease
- NASH
nonalcoholic steatohepatitis
- OLT
orthotopic liver transplant
- T2DM
type 2 diabetes mellitus
References
- 1.Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328–357. doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 2.Kwong A, Kim WR, Lake JR, Smith JM, Schladt DP, Skeans MA, et al. OPTN/SRTR 2018 annual data report: Liver. Am J Transplant. 2020;20(Suppl s1):193–299. doi: 10.1111/ajt.15674. [DOI] [PubMed] [Google Scholar]
- 3.Contos MJ, Cales W, Sterling RK, Luketic VA, Shiffman ML, Mills AS, et al. Development of nonalcoholic fatty liver disease after orthotopic liver transplantation for cryptogenic cirrhosis. Liver Transpl. 2001;7(4):363–373. doi: 10.1053/jlts.2001.23011. [DOI] [PubMed] [Google Scholar]
- 4.Dureja P, Mellinger J, Agni R, Chang F, Avey G, Lucey M, et al. NAFLD recurrence in liver transplant recipients. Transplantation. 2011;91(6):684–689. doi: 10.1097/TP.0b013e31820b6b84. [DOI] [PubMed] [Google Scholar]
- 5.Dumortier J, Giostra E, Belbouab S, Morard I, Guillaud O, Spahr L, et al. Non-alcoholic fatty liver disease in liver transplant recipients: another story of “seed and soil”. Am J Gastroenterol. 2010;105(3):613–620. doi: 10.1038/ajg.2009.717. [DOI] [PubMed] [Google Scholar]
- 6.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 7.Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67(1):123–133. doi: 10.1002/hep.29466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldberg D, Ditah IC, Saeian K, Lalehzari M, Aronsohn A, Gorospe EC, et al. Changes in the prevalence of hepatitis C virus infection, nonalcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the waitlist for liver transplantation. Gastroenterology. 2017;152(5):1090–1099.e1. doi: 10.1053/j.gastro.2017.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bhati C, Idowu MO, Sanyal AJ, Rivera M, Driscoll C, Stravitz RT, et al. Long-term outcomes in patients undergoing liver transplantation for nonalcoholic steatohepatitis-related cirrhosis. Transplantation. 2017;101(8):1867–1874. doi: 10.1097/TP.0000000000001709. [DOI] [PubMed] [Google Scholar]
- 10.El Atrache MM, Abouljoud MS, Divine G, Yoshida A, Kim DY, Kazimi MM, et al. Recurrence of non-alcoholic steatohepatitis and cryptogenic cirrhosis following orthotopic liver transplantation in the context of the metabolic syndrome. Clin Transplant. 2012;26(5):E505–E512. doi: 10.1111/ctr.12014. [DOI] [PubMed] [Google Scholar]
- 11.Lim LG, Cheng CL, Wee A, Lim SG, Lee YM, Sutedja DS, et al. Prevalence and clinical associations of posttransplant fatty liver disease. Liver Int. 2007;27(1):76–80. doi: 10.1111/j.1478-3231.2006.01396.x. [DOI] [PubMed] [Google Scholar]
- 12.Malik SM, Devera ME, Fontes P, Shaikh O, Sasatomi E, Ahmad J. Recurrent disease following liver transplantation for nonalcoholic steatohepatitis cirrhosis. Liver Transpl. 2009;15(12):1843–1851. doi: 10.1002/lt.21943. [DOI] [PubMed] [Google Scholar]
- 13.Seo S, Maganti K, Khehra M, Ramsamooj R, Tsodikov A, Bowlus C, et al. De novo nonalcoholic fatty liver disease after liver transplantation. Liver Transpl. 2007;13(6):844–847. doi: 10.1002/lt.20932. [DOI] [PubMed] [Google Scholar]
- 14.Sourianarayanane A, Arikapudi S, McCullough AJ, Humar A. Nonalcoholic steatohepatitis recurrence and rate of fibrosis progression following liver transplantation. Eur J Gastroenterol Hepatol. 2017;29(4):481–487. doi: 10.1097/MEG.0000000000000820. [DOI] [PubMed] [Google Scholar]
- 15.Yalamanchili K, Saadeh S, Klintmalm GB, Jennings LW, Davis GL. Nonalcoholic fatty liver disease after liver transplantation for cryptogenic cirrhosis or nonalcoholic fatty liver disease. Liver Transpl. 2010;16(4):431–439. doi: 10.1002/lt.22004. [DOI] [PubMed] [Google Scholar]
- 16.Finkenstedt A, Auer C, Glodny B, Posch U, Steitzer H, Lanzer G, et al. Patatin-like phospholipase domain-containing protein 3 rs738409-G in recipients of liver transplants is a risk factor for graft steatosis. Clin Gastroenterol Hepatol. 2013;11(12):1667–1672. doi: 10.1016/j.cgh.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 17.Bedossa P, Poitou C, Veyrie N, Bouillot JL, Basdevant A, Paradis V, et al. Histopathological algorithm and scoring system for evaluation of liver lesions in morbidly obese patients. Hepatology. 2012;56(5):1751–1759. doi: 10.1002/hep.25889. [DOI] [PubMed] [Google Scholar]
- 18.Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41(6):1313–1321. doi: 10.1002/hep.20701. [DOI] [PubMed] [Google Scholar]
- 19.Germani G, Laryea M, Rubbia-Brandt L, Egawa H, Burra P, O'Grady J, et al. Management of recurrent and de novo NAFLD/NASH after liver transplantation. Transplantation. 2019;103(1):57–67. doi: 10.1097/TP.0000000000002485. [DOI] [PubMed] [Google Scholar]
- 20.Lucey MR, Terrault N, Ojo L, Hay JE, Neuberger J, Blumberg E, et al. Long-term management of the successful adult liver transplant: 2012 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Liver Transpl. 2013;19(1):3–26. doi: 10.1002/lt.23566. [DOI] [PubMed] [Google Scholar]
- 21.Alten TA, Negm AA, Voigtländer T, Jaeckel E, Lehner F, Brauner C, et al. Safety and performance of liver biopsies in liver transplant recipients. Clin Transplant. 2014;28(5):585–589. doi: 10.1111/ctr.12352. [DOI] [PubMed] [Google Scholar]
- 22.van Werven, Jr, Marsman HA, Nederveen AJ, Smits NJ, ten Kate FJ, van Gulik TM, et al. Assessment of hepatic steatosis in patients undergoing liver resection: comparison of US, CT, T1-weighted dual-echo MR imaging, and point-resolved 1H MR spectroscopy. Radiology. 2010;256(1):159–168. doi: 10.1148/radiol.10091790. [DOI] [PubMed] [Google Scholar]
- 23.Crespo G, Castro-Narro G, García-Juárez I, Benítez C, Ruiz P, Sastre L, et al. Usefulness of liver stiffness measurement during acute cellular rejection in liver transplantation. Liver Transpl. 2016;22(3):298–304. doi: 10.1002/lt.24376. [DOI] [PubMed] [Google Scholar]
- 24.Bhat M, Tazari M, Sebastiani G. Performance of transient elastography and serum fibrosis biomarkers for non-invasive evaluation of recurrent fibrosis after liver transplantation: A meta-analysis. PLoS One. 2017;12(9):e0185192. doi: 10.1371/journal.pone.0185192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh S, Venkatesh SK, Keaveny A, Adam S, Miller FH, Asbach P, et al. Diagnostic accuracy of magnetic resonance elastography in liver transplant recipients: A pooled analysis. Ann Hepatol. 2016;15(3):363–376. doi: 10.5604/16652681.1198808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buzzetti E, Pinzani M, Tsochatzis EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD) Metabolism. 2016;65(8):1038–1048. doi: 10.1016/j.metabol.2015.12.012. [DOI] [PubMed] [Google Scholar]
- 27.Day CP, James OF. Steatohepatitis: a tale of two “hits”? Gastroenterology. 1998;114(4):842–845. doi: 10.1016/s0016-5085(98)70599-2. [DOI] [PubMed] [Google Scholar]
- 28.Manne V, Handa P, Kowdley KV. Pathophysiology of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. Clin Liver Dis. 2018;22(1):23–37. doi: 10.1016/j.cld.2017.08.007. [DOI] [PubMed] [Google Scholar]
- 29.Hejlova I, Honsova E, Sticova E, Lanska V, Hucl T, Spicak J, et al. Prevalence and risk factors of steatosis after liver transplantation and patient outcomes. Liver Transpl. 2016;22(5):644–655. doi: 10.1002/lt.24393. [DOI] [PubMed] [Google Scholar]
- 30.Galvin Z, Rajakumar R, Chen E, Adeyi O, Selzner M, Grant D, et al. Predictors of de novo nonalcoholic fatty liver disease after liver transplantation and associated fibrosis. Liver Transpl. 2019;25(1):56–67. doi: 10.1002/lt.25338. [DOI] [PubMed] [Google Scholar]
- 31.Kim H, Lee K, Lee KW, Yi NJ, Lee HW, Hong G, et al. Histologically proven non-alcoholic fatty liver disease and clinically related factors in recipients after liver transplantation. Clin Transplant. 2014;28(5):521–529. doi: 10.1111/ctr.12343. [DOI] [PubMed] [Google Scholar]
- 32.Martinez-Camacho A, Fortune BE, Gralla J, Bambha K. Early weight changes after liver transplantation significantly impact patient and graft survival. Eur J Gastroenterol Hepatol. 2016;28(1):107–115. doi: 10.1097/MEG.0000000000000490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tsien C, Garber A, Narayanan A, Shah SN, Barnes D, Eghtesad B, et al. Post-liver transplantation sarcopenia in cirrhosis: a prospective evaluation. J Gastroenterol Hepatol. 2014;29(6):1250–1257. doi: 10.1111/jgh.12524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Noureddin M, Sanyal AJ. Pathogenesis of NASH: The impact of multiple pathways. Curr Hepatol Rep. 2018;17(4):350–360. doi: 10.1007/s11901-018-0425-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saeed N, Glass L, Sharma P, Shannon C, Sonnenday CJ, Tincopa MA. Incidence and risks for nonalcoholic fatty liver disease and steatohepatitis post-liver transplant: systematic review and meta-analysis. Transplantation. 2019;103(11):e345–e354. doi: 10.1097/TP.0000000000002916. [DOI] [PubMed] [Google Scholar]
- 36.Sprinzl MF, Weinmann A, Lohse N, Tönissen H, Koch S, Schattenberg J, et al. Metabolic syndrome and its association with fatty liver disease after orthotopic liver transplantation. Transpl Int. 2013;26(1):67–74. doi: 10.1111/j.1432-2277.2012.01576.x. [DOI] [PubMed] [Google Scholar]
- 37.Alvarez-Sotomayor D, Satorres C, Rodríguez-Medina B, Herrero I, de la Mata M, Serrano T, et al. Controlling diabetes after liver transplantation: Room for improvement. Transplantation. 2016;100(10):e66–e73. doi: 10.1097/TP.0000000000001399. [DOI] [PubMed] [Google Scholar]
- 38.Narayanan P, Mara K, Izzy M, Dierkhising R, Heimbach J, Allen AM, et al. Recurrent or de novo allograft steatosis and long-term outcomes after liver transplantation. Transplantation. 2019;103(1):e14–e21. doi: 10.1097/TP.0000000000002317. [DOI] [PubMed] [Google Scholar]
- 39.Hanouneh IA, Macaron C, Lopez R, Feldstein AE, Yerian L, Eghtesad B, et al. Recurrence of disease following liver transplantation: Nonalcoholic steatohepatitis vs hepatitis C virus infection. Int J Organ Transplant Med. 2011;2(2):57–65. [PMC free article] [PubMed] [Google Scholar]
- 40.Charlton M, Rinella M, Patel D, McCague K, Heimbach J, Watt K. Everolimus is associated with less weight gain than tacrolimus 2 years after liver transplantation: Results of a randomized multicenter study. Transplantation. 2017;101(12):2873–2882. doi: 10.1097/TP.0000000000001913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Satapathy SK, Sanyal AJ. Epidemiology and natural history of nonalcoholic fatty liver disease. Semin Liver Dis. 2015;35(3):221–235. doi: 10.1055/s-0035-1562943. [DOI] [PubMed] [Google Scholar]
- 42.Vallin M, Guillaud O, Boillot O, Hervieu V, Scoazec JY, Dumortier J. Recurrent or de novo nonalcoholic fatty liver disease after liver transplantation: natural history based on liver biopsy analysis. Liver Transpl. 2014;20(9):1064–1071. doi: 10.1002/lt.23936. [DOI] [PubMed] [Google Scholar]
- 43.Pais R, Barritt AS, Calmus Y, Scatton O, Runge T, Lebray P, et al. NAFLD and liver transplantation: Current burden and expected challenges. J Hepatol. 2016;65(6):1245–1257. doi: 10.1016/j.jhep.2016.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang X, Li J, Riaz DR, Shi G, Liu C, Dai Y. Outcomes of liver transplantation for nonalcoholic steatohepatitis: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2014;12(3):394–402.e1. doi: 10.1016/j.cgh.2013.09.023. [DOI] [PubMed] [Google Scholar]
- 45.Mummadi RR, Kasturi KS, Chennareddygari S, Sood GK. Effect of bariatric surgery on nonalcoholic fatty liver disease: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2008;6(12):1396–1402. doi: 10.1016/j.cgh.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 46.Nickel F, Tapking C, Benner L, Sollors J, Billeter AT, Kenngott HG, et al. Bariatric surgery as an efficient treatment for non-alcoholic fatty liver disease in a prospective study with 1-year follow-up : BariScan study. Obes Surg. 2018;28(5):1342–1350. doi: 10.1007/s11695-017-3012-z. [DOI] [PubMed] [Google Scholar]
- 47.Cobb WS, Heniford BT, Burns JM, Carbonell AM, Matthews BD, Kercher KW. Cirrhosis is not a contraindication to laparoscopic surgery. Surg Endosc. 2005;19(3):418–423. doi: 10.1007/s00464-004-8722-3. [DOI] [PubMed] [Google Scholar]
- 48.Zamora-Valdes D, Watt KD, Kellogg TA, Poterucha JJ, Di CeccoSR, Francisco-Ziller NM, et al. Long-term outcomes of patients undergoing simultaneous liver transplantation and sleeve gastrectomy. Hepatology. 2018;68(2):485–495. doi: 10.1002/hep.29848. [DOI] [PubMed] [Google Scholar]
- 49.Carey EJ, Lai JC, Sonnenday C, Tapper EB, Tandon P, Duarte-Rojo A, et al. A North American expert opinion statement on sarcopenia in liver transplantation. Hepatology. 2019;70(5):1816–1829. doi: 10.1002/hep.30828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pezzati D, Ghinolfi D, De Simone P, Balzano E, Filipponi F. Strategies to optimize the use of marginal donors in liver transplantation. World J Hepatol. 2015;7(26):2636–2647. doi: 10.4254/wjh.v7.i26.2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, Torres-Gonzalez A, Gra-Oramas B, Gonzalez-Fabian L, et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology. 2015;149(2):367–378.e5. doi: 10.1053/j.gastro.2015.04.005. quiz e14-5. [DOI] [PubMed] [Google Scholar]
- 52.Shetty A, Syn WK. Current treatment options for nonalcoholic fatty liver disease. Curr Opin Gastroenterol. 2019;35(3):168–176. doi: 10.1097/MOG.0000000000000528. [DOI] [PubMed] [Google Scholar]
- 53.Golabi P, Locklear CT, Austin P, Afdhal S, Byrns M, Gerber L, et al. Effectiveness of exercise in hepatic fat mobilization in non-alcoholic fatty liver disease: Systematic review. World J Gastroenterol. 2016;22(27):6318–6327. doi: 10.3748/wjg.v22.i27.6318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hodge A, Lim S, Goh E, Wong O, Marsh P, Knight V, et al. Coffee intake is associated with a lower liver stiffness in patients with non-alcoholic fatty liver disease, hepatitis C, and hepatitis B. Nutrients. 2017;9(1):56. doi: 10.3390/nu9010056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Textor SC, Taler SJ, Canzanello VJ, Schwartz L, Augustine JE. Posttransplantation hypertension related to calcineurin inhibitors. Liver Transpl. 2000;6(5):521–530. doi: 10.1053/jlts.2000.9737. [DOI] [PubMed] [Google Scholar]
- 56.Morris MC, Jung AD, Kim Y, Lee TC, Kaiser TE, Thompson JR, et al. Delayed sleeve gastrectomy following liver transplantation: A 5-year experience. Liver Transpl. 2019;25(11):1673–1681. doi: 10.1002/lt.25637. [DOI] [PubMed] [Google Scholar]
- 57.Neff GW, Montalbano M, Tzakis AG. Ten years of sirolimus therapy in orthotopic liver transplant recipients. Transplant Proc. 2003;35(3 Suppl):209S–216S. doi: 10.1016/s0041-1345(03)00217-3. [DOI] [PubMed] [Google Scholar]