Abstract
Objective
To evaluate the efficacy and safety of the Janus kinase-1-preferential inhibitor filgotinib versus placebo or tumour necrosis factor-α inhibitor therapy in patients with active rheumatoid arthritis (RA) despite ongoing treatment with methotrexate (MTX).
Methods
This 52-week, multicentre, double-blind, placebo-controlled and active-controlled phase III trial evaluated once-daily oral filgotinib in patients with RA randomised 3:3:2:3 to filgotinib 200 mg (FIL200) or filgotinib 100 mg (FIL100), subcutaneous adalimumab 40 mg biweekly, or placebo (through week 24), all with stable weekly background MTX. The primary endpoint was the proportion of patients achieving 20% improvement in American College of Rheumatology criteria (ACR20) at week 12. Additional efficacy outcomes were assessed sequentially. Safety was assessed from adverse events and laboratory abnormalities.
Results
The proportion of patients (n=1755 randomised and treated) achieving ACR20 at week 12 was significantly higher for FIL200 (76.6%) and FIL100 (69.8%) versus placebo (49.9%; treatment difference (95% CI), 26.7% (20.6% to 32.8%) and 19.9% (13.6% to 26.2%), respectively; both p<0.001). Filgotinib was superior to placebo in key secondary endpoints assessing RA signs and symptoms, physical function and structural damage. FIL200 was non-inferior to adalimumab in terms of Disease Activity Score in 28 joints with C reactive protein ≤3.2 at week 12 (p<0.001); FIL100 did not achieve non-inferiority. Adverse events and laboratory abnormalities were comparable among active treatment arms.
Conclusions
Filgotinib improved RA signs and symptoms, improved physical function, inhibited radiographic progression and was well tolerated in patients with RA with inadequate response to MTX. FIL200 was non-inferior to adalimumab.
Trial registration number
Keywords: arthritis, rheumatoid, antirheumatic agents, therapeutics
Key messages.
What is already known about this subject?
Methotrexate (MTX) is the recommended initial treatment for rheumatoid arthritis, with tumour necrosis factor α inhibitors (TNFαi) as common second-line therapy in patients with inadequate response.
Oral therapies that match or exceed TNFαi efficacy in this population are still needed.
Filgotinib—a once-daily, oral, Janus kinase-1-preferential inhibitor—with or without MTX is superior relative to placebo treatment in patients with rheumatoid arthritis with inadequate response to MTX or prior biologic failure.
What does this study add?
This is the first study to evaluate filgotinib compared with TNFαi standard therapy or placebo with stable background MTX in patients with rheumatoid arthritis with inadequate response to MTX but without prior biologic failure, and to include a radiographic endpoint.
Filgotinib treatment reduced rheumatoid arthritis signs and symptoms, improved physical function, inhibited radiographic progression and appeared well tolerated for up to 52 weeks in this population.
How might this impact on clinical practice or future developments?
Filgotinib with background MTX could be considered a treatment option in patients with rheumatoid arthritis with inadequate response to MTX.
Introduction
Scientific innovations have changed the landscape of rheumatoid arthritis (RA) treatment. The cornerstone of RA treatment remains disease-modifying antirheumatic drugs (DMARDs), including conventional synthetic DMARDs (csDMARDs), of which methotrexate (MTX) is the gold standard, and biologic DMARDs (bDMARDs) such as those targeting cytokines (eg, tumour necrosis factor α (TNFα), interleukin 6 or interleukin 1) and B or T cells. Availability of TNFα inhibitors (TNFαi) in the late 1990s, non-TNFαi biologics in the 2000s and recently the targeted synthetic DMARDs has helped to reduce disease severity in patients with RA. Advances in RA management have further improved patient outcomes by focusing on treat-to-target strategies, pain and inflammation reduction, and administration convenience, in addition to efficacy and safety.1 2 Despite this focus, many patients do not achieve long-term responses with currently available therapies3; in one study, only 10%–21% of patients initiating csDMARDs and 12%–24% initiating TNFαi therapy achieved remission within 12 months.4 Potential innovations that may further improve patient outcomes in RA include new oral therapies that perform as well as, or better than, existing standard of care (SOC), particularly in patients with intolerance or inadequate response to bDMARDs (bDMARD-IR).
The FINCH phase 3 programme was developed to study filgotinib, a Janus-associated kinase (JAK)-1-preferential inhibitor, for RA treatment. In FINCH 2, filgotinib significantly improved efficacy versus placebo in bDMARD-IR patients with active RA.5 FINCH 3 examined filgotinib use in patients with MTX-naïve RA. To address the MTX-IR population, the FINCH 1 study examined filgotinib versus placebo or adalimumab, all with background MTX, in MTX-IR patients with active RA.
Methods
Study design and conduct
This randomised, double-blind, 52-week, placebo-controlled and active-controlled phase III trial was conducted at 303 sites in 30 countries from 30 August 2016 to 20 June 2019. The protocol and statistical analysis plan are provided in online supplemental files 1–3. All patients provided written informed consent. An independent data monitoring committee reviewed safety data periodically. An independent adjudication committee periodically reviewed all potential major cardiovascular adverse events (MACE) and thromboembolic events.
annrheumdis-2020-219214supp001.pdf (383.3KB, pdf)
annrheumdis-2020-219214supp002.pdf (245.4KB, pdf)
annrheumdis-2020-219214supp003.pdf (34.6KB, pdf)
Study participants
Eligible patients were ≥18 years old at the time of consent and met the 2010 American College of Rheumatology (ACR)/European League Against Rheumatism criteria for RA diagnosis.6 Patients had active moderate-to-severe RA, defined as ≥6 swollen joints and ≥6 tender joints (both at screening and on day 1 despite ongoing MTX treatment for ≥12 weeks and stable at 7.5–25 mg/week for ≥4 weeks). Additional inclusion criteria were seropositivity for anticyclic citrullinated peptide (anti-CCP) antibodies or rheumatoid factor (RF); ≥1 joint erosion on hand/wrist and foot radiographs, or ≥3 erosions if negative for RF and anti-CCP; or serum C reactive protein (CRP) ≥6 mg/L. Key exclusion criteria included previous use of JAK inhibitors (JAKi) or adalimumab, prior non-response or intolerance to any bDMARD, and recent use of csDMARDs other than MTX or stably dosed hydroxychloroquine or chloroquine; concomitant, stably dosed non-steroidal anti-inflammatory drugs or glucocorticoids (≤10 mg/day prednisone/equivalent) were permitted.
Interventions
Eligible patients were randomly assigned (3:3:2:3) to oral filgotinib 200 mg (FIL200) or filgotinib 100 mg (FIL100) once daily, subcutaneous adalimumab 40 mg every 2 weeks, or placebo, all with stable background MTX; other concomitant medications were to be kept stable as much as possible. Study participants were blinded to treatment and received placebo tablets matching FIL200 and/or FIL100; patients not assigned to active adalimumab received matching placebo injections. At week 24, placebo-treated patients were rerandomised (1:1) to FIL200 or FIL100 and continued background MTX. Per protocol, patients without adequate treatment response (<20% improvement from baseline in either swollen joint count 66 or tender joint count 68) at week 14 or two consecutive visits after week 30 discontinued study treatment but continued study visits, using investigator-specified SOC RA therapy.
Endpoints and assessments
The primary efficacy endpoint was ACR20 response (20% improvement in ACR criteria)7 at week 12. Key secondary efficacy endpoints tested hierarchically at week 12 (unless otherwise specified) were change from baseline score on the Health Assessment Questionnaire-Disability Index (HAQ-DI),8 9 proportion of patients with Disease Activity Score in 28 joints with CRP (DAS28(CRP)) <2.6,10 change from baseline van der Heijde modified total Sharp score (mTSS)11 at week 24 (radiographic assessment details in online supplemental methods), non-inferiority of filgotinib versus adalimumab for a proportion of patients with DAS28(CRP) ≤3.2, change from baseline Short Form-36 Physical Component Summary12 and Functional Assessment of Chronic Illness Therapy-Fatigue score,13 superiority of filgotinib versus adalimumab for a proportion of patients with DAS28(CRP) ≤3.2, non-inferiority of filgotinib versus adalimumab for a proportion of patients with DAS28(CRP) <2.6, and superiority of filgotinib versus adalimumab for a proportion of patients with DAS28(CRP) <2.6. Other secondary endpoints included ACR50/70; low disease activity defined as Clinical Disease Activity Index (CDAI) ≤10 or Simplified Disease Activity Index (SDAI) ≤1114; and remission defined as CDAI ≤2.8, SDAI ≤3.3 or Boolean remission.15 Safety was assessed from laboratory tests and adverse events (AEs). Positively adjudicated MACE and thromboembolic events were reported.
annrheumdis-2020-219214supp004.pdf (1.2MB, pdf)
Statistical analysis
A sample size of 450 patients per filgotinib and placebo group was estimated to provide >90% power at a two-sided α of 0.05 to test the superiority of FIL200 versus placebo for change from baseline mTSS at week 24, based on other RA studies with radiography.16–18 This sample size also provided >95% power to detect a 20% difference in ACR20 for filgotinib versus placebo. Assuming similar DAS28(CRP) ≤3.2 response rates for filgotinib and adalimumab, approximately 300 adalimumab-treated patients were required to ensure >90% power at a two-sided α of 0.05 to demonstrate non-inferiority of FIL200 versus adalimumab. Consistent with regulatory guidance, non-inferiority assessments were based on the method of Liu et al,19 which does not require a prespecified fixed non-inferiority margin or constancy and assay sensitivity assumptions.20 Non-inferiority testing assessed whether the effect of each filgotinib dose (response rate difference between filgotinib and placebo) preserves >50% of the effect of adalimumab (difference in response rate between adalimumab and placebo). The 50% non-inferiority margin of DAS28(CRP) ≤3.2 and <2.6 at weeks 12 and 24 based on FINCH 1 data are presented in online supplemental table S1.
Type I error rate was controlled by hierarchical testing of primary and key secondary endpoints at a two-sided α of 0.05 (online supplemental figure S1). The primary analysis tested the superiority of FIL200 versus placebo for ACR20 at week 12 using a logistic regression model, with treatment and stratification factors included as covariates. Hypothesis testing for key secondary endpoints commenced only after the primary endpoint reached statistical significance and proceeded sequentially until a null hypothesis was not rejected, after which exploratory p values are reported for the remaining hypotheses.
All analyses were based on data from patients who received ≥1 dose of study drug. For binary endpoints, a logistic regression model including treatment and stratification factors (geographical region, prior exposure to bDMARDs, and RF or CCP antibody positivity at screening) was used. Treatment effect on continuous endpoint change from baseline was evaluated using a mixed-effects model for repeated measures, with treatment, visit, treatment by visit interaction, stratification factors and baseline value included as fixed effects and subject as a random effect. Patients who required rescue therapy or had missing values were defined as non-responders, and non-responder imputation (NRI) was employed for primary and key secondary binary endpoint analyses. Multiple imputation was conducted to determine the impact of NRI on the robustness of results (online supplemental methods and table S2).21 22 Safety analyses of AEs and laboratory data were summarised by treatment group using descriptive statistics.
Patient and public involvement
Patients and the public were not involved in the design, conduct, reporting or dissemination of this research.
Results
Study participants
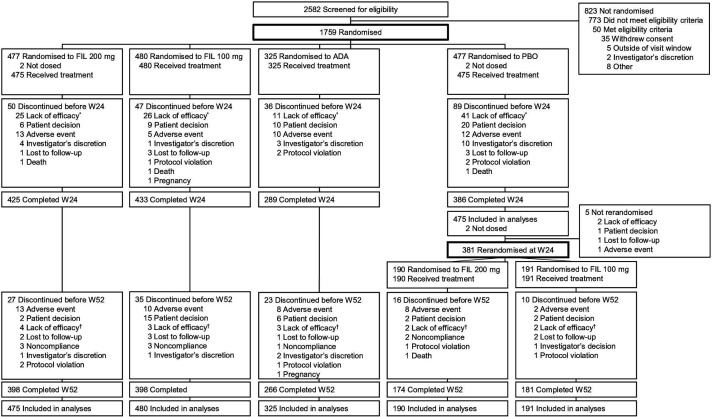
A total of 1755 patients received study treatment (enrolment by country; online supplemental figure S2), and 87.4% completed the study visits through the 24-week placebo-controlled period. The reasons for discontinuation are summarised in figure 1. At week 14, 4.8% of FIL200-treated, 6.0% of FIL100-treated, 4.0% of adalimumab-treated and 8.6% of placebo-treated patients had inadequate response to treatment and were mandated to SOC. After week 24, four patients receiving FIL200, three receiving FIL100, three receiving adalimumab and two in each placebo-to-filgotinib arm discontinued study drug due to lack of efficacy. Baseline demographics, concomitant medications and disease characteristics were similar among the treatment arms (table 1).
Figure 1.
Patient disposition. *23 (4.8%) patients treated with filgotinib 200 mg, 29 (6.0%) patients treated with filgotinib 100 mg, 13 (4.0%) patients treated with adalimumab, and 41 (8.6%) patients treated with placebo did not have adequate response to treatment per protocol at week 14. †3 (0.7%) patients treated with filgotinib 200 mg, 2 (0.5%) patients treated with filgotinib 100 mg, 3 (1.0%) patients treated with adalimumab, 0 patient treated with placebo and rerandomised to filgotinib 200 mg at week 24, and 4 (2.2%) patients treated with placebo and rerandomised to filgotinib 100 mg at week 24 failed to maintain response to treatment per protocol after week 30. ADA, adalimumab; FIL, filgotinib; PBO, placebo; W, week.
Table 1.
Baseline demographics and disease characteristics
| FIL200 (n=475) |
FIL100 (n=480) |
ADA (n=325) |
PBO (n=475) |
Total (N=1755) |
|
| Sex at birth, n (%), female | 379 (79.8) | 399 (83.1) | 266 (81.8) | 391 (82.3) | 1435 (81.8) |
| Age, years | 52±12.8 | 53±12.6 | 53±12.9 | 53±12.8 | 53±12.7 |
| Weight, kg | 70.6±17.5 | 69.9±16.9 | 71.5±17.4 | 70.6±16.8 | 70.6±17.1 |
| Body mass index, kg/m2 | 26.7±5.7 | 26.4±5.8 | 26.9±6.0 | 27.0±5.9 | 26.7±5.8 |
| Race, n (%) | |||||
| White | 312 (65.7) | 324 (67.5) | 229 (70.5) | 319 (67.2) | 1184 (67.5) |
| Asian | 122 (25.7) | 115 (24.0) | 65 (20.0) | 109 (22.9) | 411 (23.4) |
| American Indian/Alaska Native | 27 (5.7) | 27 (5.6) | 20 (6.2) | 29 (6.1) | 103 (5.9) |
| Black/African American | 6 (1.3) | 7 (1.5) | 10 (3.1) | 12 (2.5) | 35 (2.0) |
| Other* | 8 (1.7) | 6 (1.3) | 1 (0.3) | 5 (1.1) | 20 (1.1) |
| Not permitted | 0 | 1 (0.2) | 0 | 1 (0.2) | 2 (0.1) |
| Ethnicity, n (%) | |||||
| Not Hispanic or Latino | 404 (85.1) | 399 (83.1) | 268 (82.5) | 400 (84.2) | 1471 (83.8) |
| Duration of RA diagnosis, years | 7.3±7.4 | 8.5±8.2 | 8.0±7.4 | 7.3±7.2 | 7.8±7.6 |
| hsCRP, mg/L | 16.1±21.0 | 16.7±23.0 | 14.6±18.0 | 16.3±24.1 | 16.0±21.9 |
| Median (Q1, Q3) | 8.8 (3.6, 21.2) | 9.0 (3.9, 20.7) | 8.0 (3.4, 17.2) | 7.5 (3.3, 19.8) | 8.2 (3.6, 19.9) |
| ≥6 mg/L, n (%) | 298 (62.7) | 295 (61.5) | 197 (60.6) | 274 (57.7) | 1064 (60.6) |
| RF-positive, n (%) | 352 (74.1) | 362 (75.4) | 241 (74.2) | 365 (76.8)† | 1320 (75.2)† |
| Anti-CCP-positive, n (%) | 380 (80.0) | 381 (79.4) | 253 (77.8)‡ | 378 (79.6) | 1392 (79.3)‡ |
| RF and anti-CCP positive, n (%) | 331 (69.7) | 332 (69.2) | 219 (67.4)‡ | 333 (70.1)† | 1215 (69.2)†‡ |
| mTSS units§ | 32.5±47.9 | 36.7±53.1 | 34.8±55.0 | 31.6±53.2 | 33.8±52.1 |
| Median (Q1, Q3) | 12.0 (2.0, 43.5) | 13.0 (2.5, 52.5) | 12.5 (2.0, 43.5) | 11.5 (2.0, 37.0) | 12.0 (2.0, 43.5) |
| Erosion score >0, n (%)¶ | 399 (84.0) | 411 (85.6) | 277 (85.2) | 404 (85.1) | 1491 (85.0) |
| JSN score | 18.5±25.6 | 19.9±27.3 | 19.6±28.2 | 17.6±26.9 | 18.8±26.9 |
| bDMARD-naïve, n (%) | 458 (96.4) | 464 (96.7) | 317 (97.5) | 469 (98.7) | 1708 (97.3) |
| MTX dose, mg/week** | 15.3±4.9 | 15.5±4.8 | 15.4±4.8 | 14.9±4.5 | 15.3±4.8 |
| Concurrent oral steroids, n (%) | 229 (48.2) | 229 (47.7) | 140 (43.1) | 217 (45.7) | 815 (46.4) |
| ≤5 mg/day, n (%)†† | 152 (66.4) | 160 (69.9) | 96 (68.6) | 152 (70.0) | 560 (68.7) |
| Steroid dose, mg/day‡‡ | 6.2±3.4 | 6.1±2.5 | 5.9±2.2 | 5.9±2.5 | 6.0±2.8 |
| Concurrent antimalarials, n (%) | 64 (13.5) | 59 (12.3) | 39 (12.0) | 63 (13.3) | 225 (12.8) |
| DAS28(CRP) | 5.8±0.9 | 5.7±1.0 | 5.7±0.9 | 5.7±0.9 | 5.7±0.9 |
| SDAI | 41.2±12.3 | 40.2±12.8 | 40.6±11.9 | 41.2±12.4 | 40.8±12.4 |
| CDAI | 39.5±11.9 | 38.6±12.2 | 39.2±11.5 | 39.6±11.7 | 39.2±11.8 |
| SJC66 | 15±8.5 | 15±8.5 | 16±8.4 | 16±8.5 | 16±8.5 |
| TJC68 | 25±13.5 | 25±13.4 | 24±13.2 | 24±13.5 | 24±13.4 |
| SGA, VAS, mm | 67±19.2 | 65±19.7 | 67±19.1 | 68±18.7 | 67±19.2 |
| PGA, VAS, mm | 66±16.0 | 65±16.5 | 67±15.5 | 66±16.2 | 66±16.1 |
| Pain, VAS, mm | 65±20.4 | 64±20.1 | 64±19.5 | 66±19.0 | 65±19.8 |
| HAQ-DI | 1.6±0.6 | 1.6±0.6 | 1.6±0.6 | 1.6±0.6 | 1.6±0.6 |
| SF-36 PCS§§ | 33.4±7.2 | 33.6±7.8 | 32.8±7.7 | 32.9±7.1 | 33.2±7.4 |
| SF-36 MCS¶¶ | 43.9±10.4 | 44.6±10.4 | 44.1±10.4 | 43.4±11.0 | 44.0±10.6 |
| FACIT-F¶¶ | 27.6±10.7 | 27.8±10.6 | 27.2±10.2 | 26.9±10.3 | 27.4±10.5 |
Values are mean±SD.
*Includes patients recorded as Native Hawaiian/Pacific Islander and ‘Other’. Race was not recorded for one patient receiving FIL100 and one patient receiving PBO due to local regulations.
†n=1 missing.
‡n=2 missing.
§Campaign A: FIL200, n=467; FIL100, n=471; ADA, n=319; PBO, n=466.
¶Campaign A: FIL200, n=8 missing; FIL100, n=9 missing; ADA, n=6 missing; PBO, n=9 missing.
**FIL100, n=479; ADA, n=324.
††Percent of patients with concurrent oral corticosteroid use on first dosing date.
‡‡FIL200, n=226; FIL100, n=229; ADA, n=140; PBO, n=217.
§§FIL200, n=473; FIL100, n=479; ADA, n=323; PBO, n=474.
¶¶FIL200, n=472; FIL100, n=477; ADA, n=319; PBO, n=469.
ADA, adalimumab; anti-CCP, anticyclic citrullinated protein antibody; bDMARD, biologic disease-modifying antirheumatic drug; CDAI, Clinical Disease Activity Index; DAS28(CRP), Disease Activity Score in 28 joints with C reactive protein; FACIT-F, Functional Assessment of Chronic Illness Therapy-Fatigue; FIL100, filgotinib 100 mg; FIL200, filgotinib 200 mg; HAQ-DI, Health Assessment Questionnaire-Disability Index; hsCRP, high-sensitivity C reactive protein; JSN, joint space narrowing; MCS, Mental Component Summary; mTSS, van der Heijde modified total Sharp score; MTX, methotrexate; PBO, placebo; PCS, Physical Component Summary; PGA, Physician’s Global Assessment; Q1, first quartile; Q3, third quartile; RA, rheumatoid arthritis; RF, rheumatoid factor; SDAI, Simplified Disease Activity Index; SF-36, Short Form-36; SGA, Subject’s Global Assessment; SJC66, swollen joint count of 66 joints; TJC68, tender joint count of 68 joints; VAS, visual analogue scale.
Efficacy
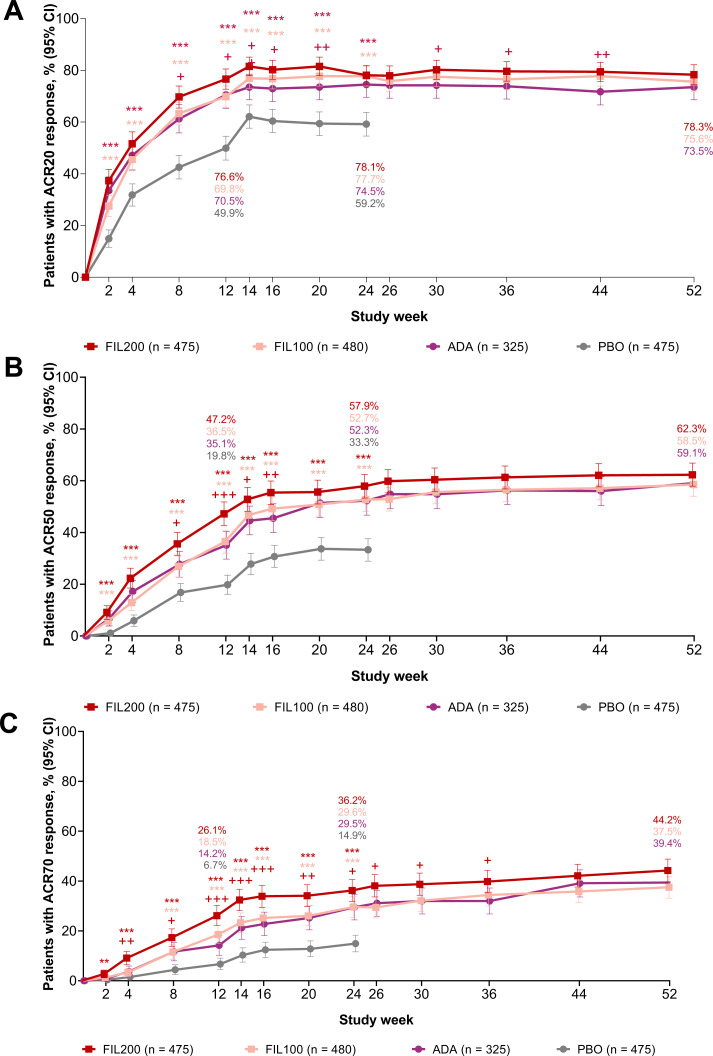
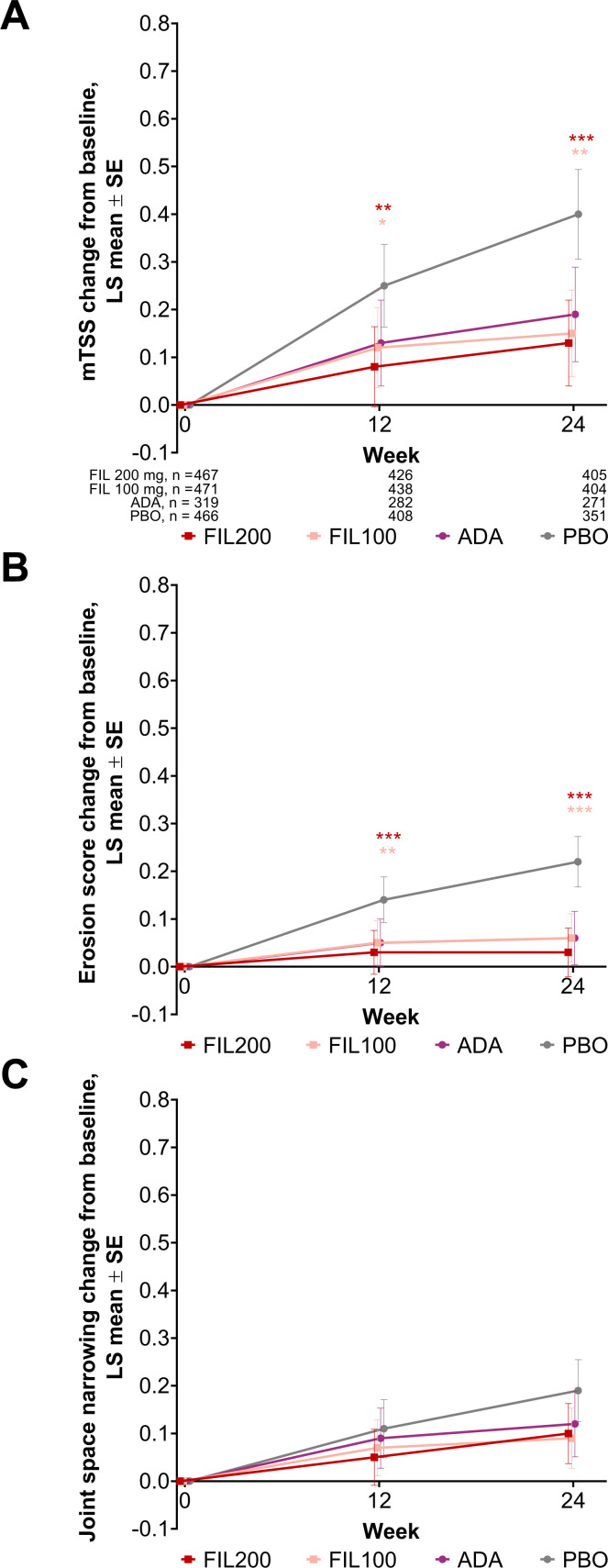
ACR20 responses at week 12 were significantly greater in patients receiving filgotinib versus placebo: 76.6% for FIL200 and 69.8% for FIL100 vs 49.9% for placebo (all p<0.001) (table 2, figure 2A). Significant improvements at week 12 with filgotinib versus placebo treatment were also observed in key secondary endpoints, including HAQ-DI and DAS28(CRP) <2.6 (all p<0.001) (table 2). Radiographic progression of structural joint damage was significantly reduced in both filgotinib dose arms versus placebo at week 24 (p<0.001 for FIL200; p=0.001 for FIL100) (figure 3). FIL200 was non-inferior to adalimumab at week 12 for DAS28(CRP) ≤3.2 (p<0.001); FIL100 did not achieve non-inferiority versus adalimumab for this measure (p=0.054) (table 2).
Table 2.
Primary and key secondary efficacy outcomes during the placebo-controlled period*
| FIL200 (n=475) |
FIL100 (n=480) |
ADA (n=325) |
PBO (n=475) |
|
| Primary outcome | ||||
| ACR20, week 12 | ||||
| n/N | 364/475 | 335/480 | 229/325 | 237/475 |
| % (95% CI) | 76.6 (72.7 to 80.5) | 69.8 (65.6 to 74.0) | 70.5 (65.3 to 75.6) | 49.9 (45.3 to 54.5) |
| Difference vs PBO (95% CI)† | 26.7 (20.6 to 32.8) | 19.9 (13.6 to 26.2) | 20.6 (13.6 to 27.5) | |
| P value vs placebo | <0.001 | <0.001 | <0.001‡ | |
| Key secondary outcomes with hierarchical testing | ||||
| HAQ-DI change from baseline to week 12 | ||||
| N | 457 | 459 | 311 | 435 |
| Mean±SD | −0.69±0.61 | −0.56±0.56 | −0.61±0.56 | −0.42±0.54 |
| Difference vs PBO (95% CI)† | −0.29 (−0.36 to −0.22) | −0.17 (−0.24 to −0.10) | −0.20 (−0.28 to −0.13) | |
| P value vs PBO | <0.001 | <0.001 | <0.001‡ | |
| DAS28(CRP) <2.6, week 12 | ||||
| n/N | 162/475 | 114/480 | 77/325 | 44/475 |
| % (95% CI) | 34.1 (29.7 to 38.5) | 23.8 (19.8 to 27.7) | 23.7 (18.9 to 28.5) | 9.3 (6.6 to 12.0) |
| Difference vs PBO (95% CI)† | 24.8 (19.6 to 30.0) | 14.5 (9.7 to 19.3) | 14.4 (8.9 to 20.0) | |
| P value vs PBO | <0.001 | <0.001 | <0.001‡ | |
| mTSS change from baseline to week 24 | ||||
| N | 405 | 404 | 271 | 351 |
| Mean±SD | 0.13±0.9 | 0.17±0.91 | 0.16±0.95 | 0.37±1.42 |
| Difference vs PBO (95% CI)† | −0.27 (−0.43 to −0.12) | −0.25 (−0.40 to −0.10) | −0.22 (−0.39 to −0.05) | |
| P value vs PBO | <0.001 | 0.001 | 0.012‡ | |
| Non-inferiority DAS28(CRP) ≤3.2, week 12 | ||||
| n/N | 236/475 | 186/480 | 141/325 | 111/475 |
| % (95% CI) | 49.7 (45.1 to 54.3) | 38.8 (34.3 to 43.2) | 43.4 (37.8 to 48.9) | 23.4 (19.5 to 27.3) |
| P value vs ADA | <0.001 | 0.054 | ||
| Key secondary outcomes without multiplicity adjustment | ||||
| SF-36 PCS change from baseline to week 12 | ||||
| N | 459 | 463 | 310 | 440 |
| Mean±SD | 9.2±8.1 | 8.5±7.7 | 8.4±7.9 | 5.8±7.1 |
| Difference vs PBO (95% CI)† | 3.7 (2.8 to 4.6) | 3.1 (2.2 to 4.0) | 2.6 (1.6 to 3.6) | |
| Exploratory p value vs PBO | <0.001 | <0.001 | <0.001 | |
| FACIT-F change from baseline to week 12 | ||||
| N | 452 | 455 | 304 | 432 |
| Mean±SD | 9.2±9.8 | 9.1±10.2 | 8.8±9.2 | 6.8±9.9 |
| Difference vs PBO (95% CI)† | 2.8 (1.7 to 3.9) | 2.6 (1.5 to 3.7) | 2.1 (0.9 to 3.3) | |
| Exploratory p value vs PBO | <0.001 | <0.001 | <0.001 | |
| Superiority DAS28(CRP) ≤3.2, week 12 | ||||
| Difference vs ADA (95% CI)† | 6.3 (−1.0 to 13.6) | −4.6 (−11.8 to 2.6) | ||
| Exploratory p value vs ADA | 0.069 | 0.18 | ||
| Non-inferiority DAS28(CRP) <2.6, week 12 | ||||
| Exploratory p value vs ADA | <0.001 | 0.002 | ||
| Superiority DAS28(CRP) <2.6, week 12 | ||||
| Difference vs ADA (95% CI)† | 10.4 (3.9 to 17.0) | 0.1 (−6.2 to 6.3) | ||
| Exploratory p value vs ADA | 0.001 | 0.99 | ||
*Hierarchical testing according to prespecified, US Food and Drug Administration-reviewed, statistical analysis plan. Patients who had missing values were defined as non-responders, and NRI was employed for both primary and key secondary analyses.
†Difference in response rates vs placebo or ADA for categorical outcomes; least-squares mean difference vs placebo or ADA for continuous outcomes.
‡Exploratory p value without multiplicity adjustment.
ACR20, American College of Rheumatology criteria 20% decrease from baseline; ADA, adalimumab; DAS28(CRP), Disease Activity Score in 28 joints with C reactive protein; FACIT-F, Functional Assessment of Chronic Illness Therapy-Fatigue; FIL100, filgotinib 100 mg; FIL200, filgotinib 200 mg; HAQ-DI, Health Assessment Questionnaire-Disability Index; mTSS, van der Heijde modified total Sharp score; NRI, non-responder imputation; PBO, placebo; SF-36 PCS, Short Form 36 Physical Component Summary.
Figure 2.
Proportions of patients achieving (A) ACR20, (B) ACR50 and (C) ACR70 through week 52. Error bars show 95% CI. Additional statistical details are available in online supplemental table S3 and all response rates in online supplemental table S7. **p<0.01, ***p<0.001 versus PBO, not adjusted for multiplicity and should be considered exploratory except for ACR20 for FIL200 and FIL100 versus PBO at week 12. +p<0.05, ++p<0.01,+++p<0.001 versus ADA, not adjusted for multiplicity and should be considered exploratory. ACR20/50/70, 20%/50%/70% improvement from baseline by the American College of Rheumatology core criteria; ADA, adalimumab; FIL100, filgotinib 100 mg; FIL200, filgotinib 200 mg; PBO, placebo.
Figure 3.
Radiographic progression through week 24. (A) mTSS change from baseline, (B) erosion score change from baseline and (C) joint space narrowing change from baseline. Data from campaign A (through week 24) are shown. Supporting data are shown in online supplemental table S4. Patient numbers at each time point in (B) and (C) are the same as for (A). Error bars represent the SE of the LS mean. *p<0.05, **p<0.01, ***p<0.001 versus PBO, not adjusted for multiplicity and should be considered exploratory except for mTSS change from baseline following FIL200 and FIL100 versus PBO at week 24. Difference for mTSS change from baseline at week 24 following treatment with FIL200 or FIL100 versus ADA was explored and was not significant for either dose. ADA, adalimumab; FIL100, filgotinib 100 mg; FIL200, filgotinib 200 mg; LS, least-squares; mTSS, van der Heijde modified total Sharp score; PBO, placebo.
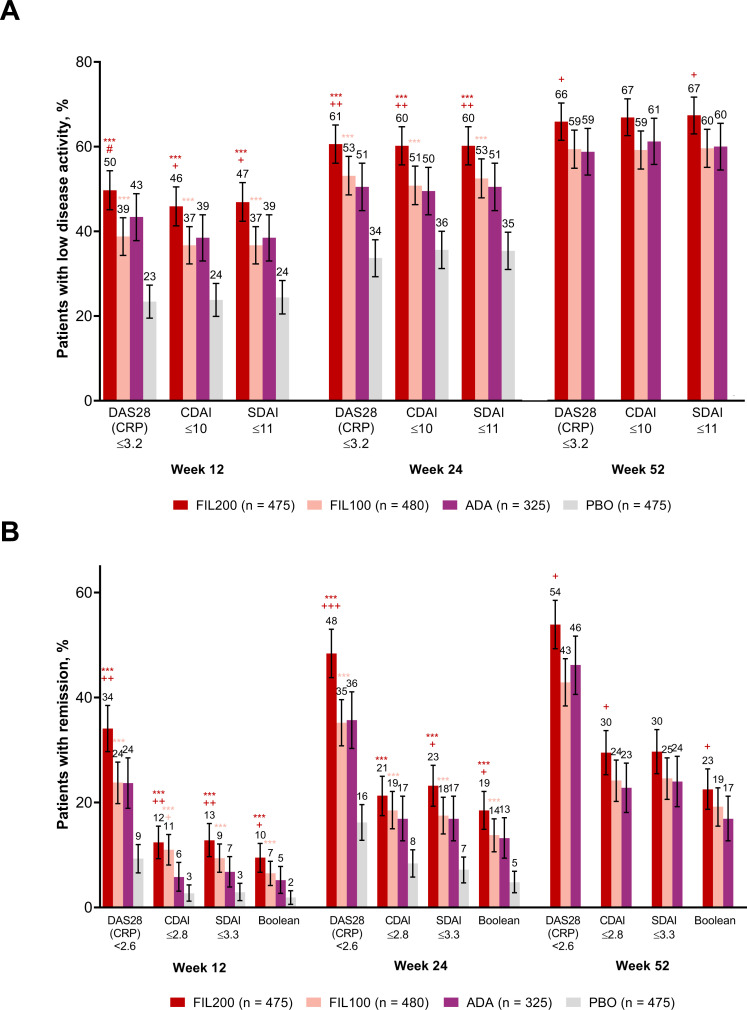
The remaining key secondary endpoints were not adjusted for multiplicity and are presented as exploratory analyses (table 2). ACR50/70 responses at week 12 were higher following FIL200 (47.2%/26.1%), FIL100 (36.5%/18.5%) or adalimumab (35.1%/14.2%) compared with placebo (19.8%/6.7%) (figure 2B, C). Response rates for DAS28(CRP) ≤3.2 at week 12 were higher in both filgotinib dose arms and placebo (table 2). Patients receiving filgotinib achieved higher rates of remission and low disease activity across several composite disease measures (DAS28(CRP), CDAI, SDAI, Boolean remission) versus placebo at weeks 12 and 24 (figure 4A, B). Filgotinib efficacy was sustained through week 52 (figures 2A–C and 4A, B, online supplemental tables S3 and S4, figure S3).
Figure 4.
Proportions of patients achieving (A) low disease activity and (B) DAS28(CRP) <2.6 or remission at weeks 12, 24 and 52. Error bars show 95% CI. Additional statistical details are available in online supplemental table S3. *p<0.05, **p<0.01, ***p<0.001 versus placebo, not adjusted for multiplicity and should be considered exploratory except for FIL200 and FIL100 versus placebo for DAS28(CRP) <2.6 at week 12. #Non-inferior versus adalimumab. +p<0.05, ++p<0.01, +++p<0.001 versus ADA, not adjusted for multiplicity and should be considered exploratory. ADA, adalimumab; Boolean, Boolean remission; CDAI, Clinical Disease Activity Index; DAS28(CRP), Disease Activity Score in 28 joints with C reactive protein; FIL100, filgotinib 100 mg; FIL200, filgotinib 200 mg; PBO, placebo; SDAI, Simplified Disease Activity Index.
Changes from baseline in ACR and DAS28(CRP) components at week 12 were generally consistent with the primary and key secondary efficacy outcomes, although the effect of FIL versus adalimumab or placebo treatment was more pronounced for high-sensitivity CRP compared with other measures (online supplemental table S5). However, in post-hoc exploratory analyses, FIL200 was non-inferior to adalimumab for CDAI low disease activity and remission at weeks 12 and 24 (online supplemental table S3). In a subanalysis of proportion of patients achieving ACR20 at week 12 across countries, the placebo response rate ranged from 36.8% to 59.2% and was highest in group B (predominantly Eastern Europe) and group C (Mexico and Argentina) (online supplemental table S6).
Safety
Treatment-emergent AEs (TEAEs) are presented in table 3. The incidence of serious TEAEs during the active-controlled period through week 52 was similar among all original active treatment arms and in patients rerandomised from placebo to filgotinib. During the placebo-controlled period, malignancy (excluding non-melanoma skin cancer) was reported in five patients: one (0.2%), one (0.3%) and three (0.6%) patients receiving FIL100, adalimumab and placebo, respectively. Venous thromboembolism (VTE) was reported in three patients: one (0.2%) receiving FIL200 and two (0.4%) receiving placebo. Adjudicated MACE occurred in four patients: one (0.2%) receiving FIL100, one (0.3%) receiving adalimumab and two (0.4%) receiving placebo. All patients with VTE and MACE had at least one risk factor, and no patient with deep vein thrombosis (DVT) or pulmonary embolism had a platelet count measurement above 600×109/L.
Table 3.
Treatment-emergent adverse events through week 24 and week 52
| PBO-controlled period (weeks 0–24) | Weeks 0–52 | |||||||||
| FIL200 (n=475) |
FIL100 (n=480) |
ADA (n=325) |
PBO (n=475) |
FIL200 (n=475) |
FIL100 (n=480) |
ADA (n=325) |
PBO | |||
| On FIL200 period (n=190) |
On FIL100 period (n=191) |
On PBO period (n=475) |
||||||||
| TEAEs, n (%) | ||||||||||
| Any TEAE | 287 (60.4) | 287 (59.8) | 186 (57.2) | 252 (53.1) | 352 (74.1) | 350 (72.9) | 239 (73.5) | 92 (48.4) | 97 (50.8) | 254 (53.5) |
| TE SAE | 21 (4.4) | 24 (5.0) | 14 (4.3) | 20 (4.2) | 35 (7.4) | 40 (8.3) | 22 (6.8) | 7 (3.7) | 8 (4.2) | 21 (4.4) |
| TEAE leading to treatment discontinuation | 15 (3.2) | 9 (1.9) | 13 (4.0) | 15 (3.2) | 26 (5.5) | 15 (3.1) | 18 (5.5) | 6 (3.2) | 2 (1.0) | 15 (3.2) |
| Deaths | 2 (0.4) | 1 (0.2) | 0 | 2 (0.4) | 3 (0.6) | 1 (0.2) | 1 (0.3) | 1 (0.5) | 1 (0.5) | 2 (0.4) |
| TEAEs in >5% of patients* | ||||||||||
| Nasopharyngitis | 31 (6.5) | 29 (6.0) | 15 (4.6) | 25 (5.3) | 43 (9.1) | 48 (10.0) | 24 (7.4) | 7 (3.7) | 6 (3.1) | 25 (5.3) |
| URTI | 25 (5.3) | 33 (6.9) | 17 (5.2) | 14 (2.9) | 41 (8.6) | 49 (10.2) | 21 (6.5) | 8 (4.2) | 6 (3.1) | 14 (2.9) |
| ALT increased | 13 (2.7) | 15 (3.1) | 14 (4.3) | 11 (2.3) | 17 (3.6) | 25 (5.2) | 22 (6.8) | 7 (3.7) | 3 (1.6) | 11 (2.3) |
| AST increased | 9 (1.9) | 14 (2.9) | 11 (3.4) | 9 (1.9) | 12 (2.5) | 20 (4.2) | 18 (5.5) | 8 (4.2) | 3 (1.6) | 9 (1.9) |
| Nausea | 19 (4.0) | 10 (2.1) | 4 (1.2) | 7 (1.5) | 26 (5.5) | 16 (3.3) | 6 (1.8) | 4 (2.1) | 1 (0.5) | 7 (1.5) |
| Urinary tract infection | 11 (2.3) | 8 (1.7) | 8 (2.5) | 5 (1.1) | 19 (4.0) | 20 (4.2) | 17 (5.2) | 10 (5.3) | 8 (4.2) | 6 (1.3) |
| TEAEs of special interest | ||||||||||
| Infectious AEs | 133 (28.0) | 128 (26.7) | 88 (27.1) | 105 (22.1) | 206 (43.4) | 194 (40.4) | 129 (39.7) | 45 (23.7) | 39 (20.4) | 106 (22.3) |
| Serious infectious AEs | 8 (1.7) | 8 (1.7) | 8 (2.5) | 4 (0.8) | 13 (2.7) | 13 (2.7) | 10 (3.1) | 1 (0.5) | 2 (1.0) | 4 (0.8) |
| Herpes zoster | 2 (0.4) | 2 (0.4) | 2 (0.6) | 2 (0.4) | 6 (1.3) | 4 (0.8) | 2 (0.6) | 2 (1.1) | 1 (0.5) | 2 (0.4) |
| Hepatitis B or C | 0 | 0 | 1 (0.3) | 0 | 1 (0.2) | 1 (0.2) | 1 (0.3) | 1 (0.5) | 1 (0.5) | 0 |
| Opportunistic infections | 0 | 0 | 1 (0.3) | 0 | 0 | 0 | 2 (0.6) | 0 | 0 | 0 |
| Active tuberculosis | 0 | 0 | 0 | 0 | 0 | 0 | 1 (0.3) | 0 | 0 | 0 |
| MACE† | 0 | 1 (0.2) | 1 (0.3) | 2 (0.4) | 0 | 2 (0.4) | 1 (0.3) | 1 (0.5) | 1 (0.5) | 2 (0.4) |
| Malignancy | ||||||||||
| Excluding NMSC | 0 | 1 (0.2) | 1 (0.3) | 3 (0.6) | 2 (0.4) | 2 (0.4) | 2 (0.6) | 0 | 0 | 3 (0.6) |
| NMSC | 0 | 0 | 0 | 0 | 1 (0.2) | 1 (0.2) | 0 | 0 | 0 | 0 |
| VTE† | 1 (0.2) | 0 | 0 | 2 (0.4) | 1 (0.2) | 0 | 1 (0.3) | 1 (0.5) | 0 | 2 (0.4) |
| GI perforation | 0 | 0 | 0 | 0 | 1 (0.2) | 0 | 0 | 0 | 0 | 0 |
*TEAEs occurring in >5% of patients in a single treatment arm during either study period.
†Positively adjudicated.
ADA, adalimumab; AE, adverse event; ALT, alanine aminotransferase; AST, aspartate aminotransferase; FIL100, filgotinib 100 mg; FIL200, filgotinib 200 mg; GI, gastrointestinal; MACE, major adverse cardiac event; NMSC, non-melanoma skin cancer; PBO, placebo; SAE, serious AE; TE, treatment-emergent; TEAE, treatment-emergent AE; URTI, upper respiratory tract infection; VTE, venous thromboembolism.
Through week 24, death was reported in five patients: two (0.4%) receiving FIL200 (both attributed to septic shock), one (0.2%) receiving FIL100 (myocardial infarction) and two (0.4%) receiving placebo (one toxic reaction to amoxicillin/clavulanic acid and one non-TEAE septic shock). Four additional deaths occurred in the active-controlled period: one patient receiving FIL200 (alveolitis), one receiving adalimumab (sepsis), one placebo-treated patient rerandomised to FIL200 (acute DVT) and one placebo-treated patient rerandomised to FIL100 (primary varicella). Additional details of the DVT-associated and primary varicella-associated deaths are provided in online supplemental results.
Overall, infectious and serious infectious TEAEs occurred more frequently in patients receiving filgotinib or adalimumab versus placebo through week 24. Serious infections occurring in >2 patients were pneumonia (13 patients), cellulitis (3 patients) and bronchitis (3 patients). Through week 24, herpes zoster (excluding primary varicella) occurred in all treatment arms in 0.4% of patients receiving either filgotinib dose or placebo and in 0.6% of patients receiving adalimumab. Through week 52, serious infections occurred in 2.7%, 2.7% and 3.1% and herpes zoster occurred in 1.3%, 0.8% and 0.6% of patients receiving FIL200, FIL100 and adalimumab, respectively. In 14% of patients randomised in Asia (online supplemental figure S2), the frequency of herpes zoster was 1%, 3% and 0% for patients receiving FIL200, FIL100 and adalimumab, respectively, through week 52, and 2% in placebo-treated patients through week 24. Both reported opportunistic infections were in patients receiving adalimumab: one patient with Pneumocystis jirovecii pneumonia before week 24 and one patient with active Mycobacterium tuberculosis after week 24.
Grade 3/4 changes in laboratory values are shown in table 4. Mean haemoglobin levels were stable or increased across all treatment arms, with no imbalance in individual decreased haemoglobin events or grade 3 changes. Decreases in neutrophil and lymphocyte levels were seen in filgotinib-treated and adalimumab-treated patients. Grade ≥3 lymphopaenia and neutropaenia were more frequent in patients receiving filgotinib versus placebo. The majority of white cell count abnormalities were grade 1/2, not associated with infection, and resolved at follow-up testing. No grade ≥3 changes in platelet counts were observed. Higher mean creatinine levels were observed in patients receiving filgotinib versus adalimumab or placebo. Grade 3/4 serum creatinine elevations were reported in three patients: one receiving FIL100 and two receiving placebo, all before week 24. Mean creatine kinase and low-density lipoprotein (LDL) and high-density lipoprotein (HDL) cholesterol levels were increased in patients treated with filgotinib versus placebo, without meaningful change in the LDL to HDL cholesterol ratio.
Table 4.
Laboratory values and grade ≥3 abnormalities through week 24 and week 52
| PBO-controlled period (weeks 0–24) | Weeks 0–52 | |||||||||
| FIL200 (n=475) |
FIL100 (n=480) |
ADA (n=325) |
PBO (n=475) |
FIL200 (n=475) |
FIL100 (n=480) |
ADA (n=325) |
PBO | |||
| On FIL200 period (n=190) |
On FIL100 period (n=191) |
On PBO period (n=475) |
||||||||
| Haemoglobin, g/L | 2 (11) | 1 (10) | 2 (10) | 0 (9) | 5 (11) | 3 (11) | 5 (10) | 5 (9) | 2 (9) | NA |
| Grade 3, n (%) | 2 (0.4) | 3 (0.6) | 2 (0.6) | 4 (0.9) | 4 (0.8) | 5 (1.0) | 3 (0.9) | 0 | 0 | 4 (0.9) |
| Neutrophils, 109/L | −1.0 (1.9) | −0.9 (2.0) | −1.2 (2.0) | −0.2 (1.9) | −1.0 (2.0) | −0.9 (1.9) | −1.3 (2.3) | −0.8 (1.8) | −0.5 (1.7) | NA |
| Grade 3 or 4, n (%) | 5 (1.1) | 5 (1.0)* | 1 (0.3) | 2 (0.4) | 5 (1.1) | 6 (1.3) | 1 (0.3) | 0 | 1 (0.5) | 2 (0.4) |
| Lymphocytes, 109/L | −0.1 (0.6) | −0.1 (0.6) | 0.3 (0.6) | −0.1 (0.5) | −0.2 (0.6) | −0.1 (0.5) | 0.4 (0.6) | −0.1 (0.5) | −0.0 (0.6) | NA |
| Grade 3 or 4†, n (%) | 11 (2.3)* | 6 (1.3) | 2 (0.6) | 3 (0.6) | 15 (3.2) | 11 (2.3) | 3 (0.9) | 4 (2.1) | 2 (1.1) | 3 (0.6) |
| Platelets, 109/L | −30 (61.0) | −28 (62.4) | −34 (63.8) | −8 (65.3) | −26 (66.8) | −31 (56.6) | −31 (70.9) | −17 (59.2) | −7 (65.2) | NA |
| ALT, U/L | 6 (23.8) | 4 (20.7) | 6 (19.2) | 2 (19.2) | 6 (33.0) | 6 (23.7) | 6 (18.7) | 5 (25.3) | 2 (18.3) | NA |
| Grade 3 or 4, n (%) | 3 (0.6) | 4 (0.8) | 6 (1.9) | 5 (1.1) | 9 (1.9) | 8 (1.7) | 8 (2.5) | 2 (1.1) | 0 | 5 (1.1) |
| AST, U/L | 6 (16.8) | 5 (14.0) | 4 (13.2) | 2 (14.3) | 7 (22.7) | 6 (14.5) | 4 (12.6) | 6 (18.9) | 3 (15.3) | NA |
| Grade 3 or 4, n (%) | 3 (0.6) | 2 (0.4) | 2 (0.6) | 1 (0.2) | 6 (1.3) | 3 (0.6) | 3 (0.9) | 1 (0.5) | 0 | 1 (0.2) |
| Creatinine, mg/dL | 0.1 (0.1) | 0.1 (0.1) | 0.0 (0.1) | 0.0 (0.1) | 0.1 (0.1) | 0.1 (0.1) | 0.0 (0.1) | 0.1 (0.1) | 0.0 (0.1) | NA |
| Grade 3 or 4, n (%) | 0 | 1 (0.2) | 0 | 2 (0.4) | 0 | 1 (0.2) | 0 | 0 | 0 | 2 (0.4) |
| Creatine kinase, U/L | 54 (89.5) | 34 (64.4) | 9 (70.1) | 4 (78.6) | 56 (92.3) | 37 (63.9) | 15 (77.0) | 57 (163.6) | 26 (46.5) | NA |
| Grade 3 or 4, n (%) | 4 (0.8)‡ | 2 (0.4)* | 1 (0.3) | 3 (0.6) | 6 (1.3) | 3 (0.6) | 1 (0.3) | 1 (0.5) | 0 | 3 (0.6) |
| LDL cholesterol, mg/dL§ | 15 (29.1) | 12 (25.9) | 7 (21.7) | 5 (23.4) | 24 (27.6) | 20 (26.8) | 12 (25.0) | 13 (29.6) | 10 (22.7) | NA |
| % change | 16 (29.2) | 13 (27.7) | 9 (20.5) | 7 (23.6) | 25 (29.3) | 21 (28.5) | 12 (22.6) | 13 (22.9) | 11 (21.3) | NA |
| HDL cholesterol, mg/dL§ | 12 (14.9) | 5 (12.8) | 3 (11.8) | −1 (11.0) | 13 (14.4) | 7 (13.3) | 4 (11.0) | 12 (11.7) | 6 (14.3) | NA |
| % change | 21 (25.7) | 11 (22.0) | 7 (20.6) | 0 (20.5) | 24 (26.5) | 14 (23.4) | 9 (20.1) | 24 (22.6) | 11 (26.3) | NA |
| LDL:HDL ratio§ | −0.1 (0.6) | 0.1 (0.6) | 0.0 (0.5) | 0.1 (0.7) | 0.0 (0.6) | 0.1 (0.6) | 0.1 (0.5) | −0.2 (0.6) | 0.0 (0.5) | NA |
| % change | −0.6 (31.1) | 6.4 (36.4) | 4.5 (23.6) | 10.3 (29.2) | 3.8 (30.8) | 9.5 (29.5) | 6.0 (24.5) | −6.5 (23.0) | 2.6 (23.6) | NA |
Absolute values are presented as mean (SD) change from baseline at weeks 24 and 52 unless otherwise specified.
Severity was graded using Common Terminology Criteria for Adverse Events Version 4.03.
*Grade 4 in one patient.
†Lymphocytes decreased.
‡Grade 4 in two patients.
§Fasting values; not available for all patients.
ADA, adalimumab; ALT, alanine aminotransferase; AST, aspartate aminotransferase; FIL100, filgotinib 100 mg; FIL200, filgotinib 200 mg; HDL, high-density lipoprotein; LDL, low-density lipoprotein; NA, not assessed; PBO, placebo.
Discussion
The FINCH 1 study assessed filgotinib, an oral JAK-1-preferential inhibitor, to address the unmet needs for RA treatment in MTX-IR patients. Two doses of filgotinib were compared with adalimumab and placebo, all with background MTX. Both filgotinib doses were superior to placebo for ACR20 response and hierarchical key secondary endpoints evaluating signs and symptoms, physical function and structural damage. Although conclusions are limited for tests without multiplicity adjustment, proportions of patients achieving various measures of low disease activity and remission were generally consistent with DAS28(CRP) <2.6 and DAS28(CRP) ≤3.2 response results.
These phase III results confirm those of two phase II studies investigating filgotinib with or without MTX versus placebo in MTX-IR patients23 24 and a phase III study (FINCH 2) in bDMARD-refractory patients,5 and are consistent with the results for other JAKis in MTX-IR patients with RA.18 25 26 FIL200 efficacy was statistically non-inferior to adalimumab for a proportion of patients with DAS28(CRP) ≤3.2 at week 12, a treat-to-target checkpoint,2 15 and remained non-inferior in exploratory analyses of CDAI low disease activity and remission, suggesting direct effects of JAK inhibition on high-sensitivity CRP did not impact FIL200 treatment effect. FIL100 did not attain statistical significance for non-inferiority to adalimumab for DAS28(CRP) ≤3.2 at week 12 in hierarchical testing, resulting in loss of multiplicity adjustment for subsequent comparisons and limiting possible conclusions. Filgotinib efficacy generally compared favourably with adalimumab, consistent with a recent systematic review on the efficacy of bDMARDs and JAKis in RA.27
Filgotinib benefits must be considered in the context of risks. In this study, serious TEAEs and discontinuations due to TEAEs were similar among treatment arms through week 24. Safety data remained consistent over the entire 52-week study. Adjudicated MACE and VTE were observed in all treatment arms at frequencies similar to reported background rates in patients with RA28 29; VTE remains a concern for the JAKi class.30 Infections were increased in patients treated with FIL200 versus placebo, with similar rates of serious infections across active treatment groups. The frequency of herpes zoster was low and similar across all groups through week 24; the number of uncomplicated cases increased slightly after week 24 in the filgotinib versus adalimumab treatment arms. The low frequency of herpes zoster does not appear attributable to geography; the proportion of FINCH 1 patients enrolled in Asian countries (14%) was comparable relative to similar JAKi studies (3%–18%).25 26 31 No cases of opportunistic infection or tuberculosis were observed in filgotinib-treated patients. Rates of AEs in filgotinib-treated patients were consistent with or below those from a recent meta-analysis on JAKi treatment in RA.32
Filgotinib was associated with decreases in neutrophil, lymphocyte and platelet counts and increases in lipid, creatine kinase and creatinine levels, as previously reported for filgotinib and other JAKis.5 18 23–26 There were small numerical differences in frequencies of grade 3/4 neutropaenia and lymphopaenia in patients treated with filgotinib versus placebo. Treatment with filgotinib was associated with small increases in fasting total, LDL and HDL cholesterol without affecting fasting LDL to HDL ratio, consistent with the hypothesis that JAKi treatment suppresses elevated cholesterol ester catabolism in patients with active RA and normalises their cholesterol levels towards the range in healthy volunteers.33
Limitations
The study excluded patients with prior bDMARD failure, so data cannot be extrapolated to bDMARD-experienced patients; filgotinib was previously compared with placebo in this population.5 Generalisability to patients with less active RA is potentially limited because the study enrolled patients with moderate-to-severe disease. Placebo treatment was limited to 24 weeks due to ethical concerns. An elevated placebo response was observed, consistent with RA trial data showing increasing placebo rates over the last 20 years.34 In the present study, placebo response rates were especially high in geographical group B (predominantly Eastern Europe) and group C (Mexico and Argentina); as these groups comprised 65% of randomised patients, the regional differences contributed substantially to the overall placebo response rate. Nearly 50% of placebo-treated patients achieving study endpoints present a challenge to differentiating active agents from placebo. The study was not powered to compare AEs between arms, so no definitive conclusions about safety can be reached. Additional safety data will come from the integrated safety analysis across all phase II and III filgotinib trials, long-term extension study (ClinicalTrials.gov NCT03025308) and future registries.
Conclusions
In MTX-IR patients with active RA, filgotinib plus MTX reduced RA signs and symptoms, improved physical function and inhibited progression of structural joint damage. This study demonstrated non-inferiority of FIL200 plus MTX, but not FIL100 plus MTX, to adalimumab plus MTX, based on DAS28(CRP) low disease activity. Overall, filgotinib showed a favourable benefit-to-risk profile and both doses were well tolerated.
Acknowledgments
We thank all patients and their families and the FINCH 1 investigators/site staff. Medical writing assistance was provided by Judith M Phillips, DVM, PhD, of AlphaScientia, and Emmett Glass, PhD, MBA of Red Sky Medical, both funded by Gilead Sciences.
Footnotes
Handling editor: Josef S Smolen
Presented at: Results from interim data cuts were presented at the 2019 Annual European Congress of Rheumatology, Madrid, Spain (Combe et al, Ann Rheum Dis. 2019; 78(Suppl 2):77–8) and at the 2019 American College of Rheumatology Annual Meeting, Atlanta, Georgia (Combe et al, Arthritis Rheumatol. 2019; 71(Suppl 10):A506). The FINCH 1 data were presented virtually at the 2020 Annual European Congress of Rheumatology (Combe et al, Ann Rheum Dis. 2020; 79(Suppl 1):320–1).
Contributors: FM, NM, JSS, CT and MCG contributed to the study concept and design. FM and MCG contributed to drafting the manuscript. YG and LY performed the statistical analyses. NM and JSS obtained funding. BC, AK, YT, DvdH, JAS, HSBB, UK, FM, BB, LY, YG, CT, JSS, AJ, MCG, NM, RBML, S-CB, EK and PN contributed to acquisition, analysis or interpretation of data; had full access to the data; reviewed the manuscript critically for important intellectual content; and approved the final version for publication.
Funding: The study was funded by Gilead Sciences.
Competing interests: BC received honoraria from AbbVie, Bristol-Myers Squibb, Gilead Sciences, Janssen, Lilly, Merck, Novartis, Pfizer, Roche-Chugai, Sanofi and UCB; and research grants from Novartis, Pfizer and Roche. AK received honoraria or consulting fees from AbbVie, Boehringer Ingelheim, Flexion, Genzyme, Gilead Sciences, Janssen, Novartis, Pfizer, Regeneron, Sanofi and Sun Pharma Advanced Research; was a paid instructor or speaker for AbbVie, Celgene, Flexion, Genzyme, Horizon, Merck, Novartis, Pfizer, Regeneron and Sanofi; and holds shares in Amgen, Gilead Sciences, GlaxoSmithKline, Pfizer and Sanofi. YT has received speaking fees and/or honoraria from AbbVie, Asahi Kasei, Astellas, Bristol-Myers, Chugai, Daiichi Sankyo, Eisai, Eli Lilly, Gilead, GSK, Janssen, Mitsubishi Tanabe, Novartis, Pfizer, Sanofi and YL Biologics; and research grants from AbbVie, Chugai, Daiichi Sankyo, Eisai, Mitsubishi Tanabe, Takeda and UCB. DvdH received consulting fees from AbbVie, Amgen, Astellas, AstraZeneca, BMS, Boehringer Ingelheim, Celgene, Cyxone, Daiichi Sankyo, Eisai, Eli Lilly, Galapagos, Gilead, GlaxoSmithKline, Janssen, Merck, Novartis, Pfizer, Regeneron, Roche, Sanofi, Takeda and UCB Pharma; and is the Director of Imaging Rheumatology BV. JAS, UK and S-CB report nothing to disclose. HSBB has received honoraria or consulting fees from AbbVie, Gilead Sciences, Horizon and Merck; and research grants or support from AbbVie, Sanofi, Regeneron, Eli Lilly, Pfizer, Selecta Biosciences, Gilead Sciences, Horizon, Janssen and Pfizer. FM, BB, LY and YG are employees and shareholders of Gilead Sciences. MCG has received honoraria or consulting fees from AbbVie, Amgen, BeiGene, Genentech, Gilead Sciences, Lilly Pharmaceuticals, Sanofi Genzyme, RPharm and SetPoint. He is also an employee and shareholder of Gilead Sciences. CT is an employee and shareholder of Galapagos NV. JSS, AJ and NM are former employees of Gilead Sciences and may hold shares. RBML has received honoraria or consulting fees from AbbVie, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Galapagos NV, Novartis, Pfizer and UCB. EK has received honoraria or consulting fees from AbbVie, Amgen, AstraZeneca, Bristol-Myers Squibb, Celltrion, F Hoffmann-La Roche, Genentech, Gilead Sciences, Janssen, Lilly Pharmaceuticals, Merck, Myriad Autoimmune, Pfizer, Sandoz, Sanofi Genzyme and Samsung Bioepis; has received speaking fees from AbbVie, Amgen, Bristol-Myers Squibb, F Hoffmann-La Roche, Janssen, Merck, Pfizer, Sanofi Genzyme and UCB; and has received research grants or support from AbbVie, Amgen, Gilead Sciences, Lilly Pharmaceuticals, Merck, Pfizer, PuraPharm and Sanofi. PN has received honoraria or consulting fees, grants or research support, or been a member of a speakers bureau for AbbVie, Bristol-Myers Squibb, Celgene, Gilead Sciences, Janssen, Lilly, MSD, Novartis, Pfizer, Roche, Sanofi and UCB.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Anonymised individual patient data will be shared upon request for research purposes dependent upon the nature of the request, the merit of the proposed research, the availability of the data and the intended use. The full data sharing policy for Gilead Sciences can be found at https://www.gilead.com/about/ethics-and-code-of-conduct/policies.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The trial was conducted in accordance with the Declaration of Helsinki and the International Council for Harmonisation guidelines. The protocol was approved by the institutional review board or ethics committee at each site.
References
- 1. Singh JA, Saag KG, Bridges SL, et al. 2015 American College of rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Rheumatol 2016;68:1–26. 10.1002/art.39480 [DOI] [PubMed] [Google Scholar]
- 2. Smolen JS, Breedveld FC, Burmester GR, et al. Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international Task force. Ann Rheum Dis 2016;75:3–15. 10.1136/annrheumdis-2015-207524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Burmester GR, Feist E, Dörner T. Emerging cell and cytokine targets in rheumatoid arthritis. Nat Rev Rheumatol 2014;10:77–88. 10.1038/nrrheum.2013.168 [DOI] [PubMed] [Google Scholar]
- 4. Furst DE, Pangan AL, Harrold LR, et al. Greater likelihood of remission in rheumatoid arthritis patients treated earlier in the disease course: results from the Consortium of rheumatology researchers of North America registry. Arthritis Care Res 2011;63:856–64. 10.1002/acr.20452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Genovese MC, Kalunian K, Gottenberg J-E, et al. Effect of Filgotinib vs placebo on clinical response in patients with moderate to severe rheumatoid arthritis refractory to disease-modifying antirheumatic drug therapy. JAMA 2019;322:315–25. 10.1001/jama.2019.9055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League against rheumatism collaborative initiative. Arthritis Rheum 2010;62:2569–81. 10.1002/art.27584 [DOI] [PubMed] [Google Scholar]
- 7. Felson DT, Anderson JJ, Boers M, et al. American College of rheumatology. Preliminary definition of improvement in rheumatoid arthritis. Arthritis Rheum 1995;38:727–35. 10.1002/art.1780380602 [DOI] [PubMed] [Google Scholar]
- 8. Fries JF, Spitz P, Kraines RG, et al. Measurement of patient outcome in arthritis. Arthritis Rheum 1980;23:137–45. 10.1002/art.1780230202 [DOI] [PubMed] [Google Scholar]
- 9. Fries JF, Spitz PW, Young DY. The dimensions of health outcomes: the health assessment questionnaire, disability and pain scales. J Rheumatol 1982;9:789–93. [PubMed] [Google Scholar]
- 10. Prevoo ML, van 't Hof MA, Kuper HH, et al. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 1995;38:44–8. 10.1002/art.1780380107 [DOI] [PubMed] [Google Scholar]
- 11. van der Heijde D. How to read radiographs according to the Sharp/van Der Heijde method. J Rheumatol 2000;27:261–3. [PubMed] [Google Scholar]
- 12. Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 13. Webster K, Cella D, Yost K. The functional assessment of chronic illness therapy (FACIT) measurement system: properties, applications, and interpretation. Health Qual Life Outcomes 2003;1:79. 10.1186/1477-7525-1-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Aletaha D, Smolen J. The simplified disease activity index (SDAI) and the clinical disease activity index (CDAI): a review of their usefulness and validity in rheumatoid arthritis. Clin Exp Rheumatol 2005;23:S100–8. [PubMed] [Google Scholar]
- 15. Felson DT, Smolen JS, Wells G, et al. American College of Rheumatology/European League against rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Arthritis Rheum 2011;63:573–86. 10.1002/art.30129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fleischmann RM, Genovese MC, Enejosa JV, et al. Safety and effectiveness of upadacitinib or adalimumab plus methotrexate in patients with rheumatoid arthritis over 48 weeks with switch to alternate therapy in patients with insufficient response. Ann Rheum Dis 2019;78:1454–62. 10.1136/annrheumdis-2019-215764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Taylor PC, Keystone EC, van der Heijde D, et al. Baricitinib versus placebo or adalimumab in rheumatoid arthritis. N Engl J Med 2017;376:652–62. 10.1056/NEJMoa1608345 [DOI] [PubMed] [Google Scholar]
- 18. van der Heijde D, Tanaka Y, Fleischmann R, et al. Tofacitinib (CP-690,550) in patients with rheumatoid arthritis receiving methotrexate: twelve-month data from a twenty-four-month phase III randomized radiographic study. Arthritis Rheum 2013;65:559–70. 10.1002/art.37816 [DOI] [PubMed] [Google Scholar]
- 19. Liu JT, Tzeng CS, Tsou HH. Establishing non-inferiority of a new treatment in a three-arm trial: apply a step-down hierarchical model in a papulopustular acne study and an oral prophylactic antibiotics study. International Journal of Statistics in Medical Research 2014;3:11–20. [Google Scholar]
- 20. U.S. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research . Non-Inferiority clinical trials to establish effectiveness: guidance for industry, 2016. Available: https://www.fda.gov/downloads/Drugs/Guidances/UCM202140.pdf [Accessed 22 Jul 2020].
- 21. Yuan Y. Sensitivity analysis in multiple imputation for missing data. SAS Institute Inc, 2014. [Google Scholar]
- 22. Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: John Wiley & Sons, Inc, 1987. [Google Scholar]
- 23. Kavanaugh A, Kremer J, Ponce L, et al. Filgotinib (GLPG0634/GS-6034), an oral selective JAK1 inhibitor, is effective as monotherapy in patients with active rheumatoid arthritis: results from a randomised, dose-finding study (DARWIN 2). Ann Rheum Dis 2017;76:1009–19. 10.1136/annrheumdis-2016-210105 [DOI] [PubMed] [Google Scholar]
- 24. Westhovens R, Taylor PC, Alten R, et al. Filgotinib (GLPG0634/GS-6034), an oral JAK1 selective inhibitor, is effective in combination with methotrexate (MTX) in patients with active rheumatoid arthritis and insufficient response to MTX: results from a randomised, dose-finding study (Darwin 1). Ann Rheum Dis 2017;76:998–1008. 10.1136/annrheumdis-2016-210104 [DOI] [PubMed] [Google Scholar]
- 25. Dougados M, van der Heijde D, Chen Y-C, et al. Baricitinib in patients with inadequate response or intolerance to conventional synthetic DMARDs: results from the RA-BUILD study. Ann Rheum Dis 2017;76:88–95. 10.1136/annrheumdis-2016-210094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fleischmann R, Pangan AL, Song I-H, et al. Upadacitinib versus placebo or adalimumab in patients with rheumatoid arthritis and an inadequate response to methotrexate: results of a phase III, double-blind, randomized controlled trial. Arthritis Rheumatol 2019;71:1788–800. 10.1002/art.41032 [DOI] [PubMed] [Google Scholar]
- 27. Kerschbaumer A, Sepriano A, Smolen JS, et al. Efficacy of pharmacological treatment in rheumatoid arthritis: a systematic literature research Informing the 2019 update of the EULAR recommendations for management of rheumatoid arthritis. Ann Rheum Dis 2020;79:744–59. 10.1136/annrheumdis-2019-216656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kim SC, Schneeweiss S, Liu J. Risk of venous thromboembolism in patients with rheumatoid arthritis. Arthritis Care Res 2013;65:1600–7. 10.1002/acr.22039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Solomon DH, Karlson EW, Rimm EB, et al. Cardiovascular morbidity and mortality in women diagnosed with rheumatoid arthritis. Circulation 2003;107:1303–7. 10.1161/01.CIR.0000054612.26458.B2 [DOI] [PubMed] [Google Scholar]
- 30. Smolen JS, Landewé RBM, Bijlsma JWJ, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis 2020;79:685–99. 10.1136/annrheumdis-2019-216655 [DOI] [PubMed] [Google Scholar]
- 31. Fleischmann R, Mysler E, Hall S, et al. Efficacy and safety of tofacitinib monotherapy, tofacitinib with methotrexate, and adalimumab with methotrexate in patients with rheumatoid arthritis (oral strategy): a phase 3b/4, double-blind, head-to-head, randomised controlled trial. Lancet 2017;390:457–68. 10.1016/S0140-6736(17)31618-5 [DOI] [PubMed] [Google Scholar]
- 32. Olivera PA, Lasa JS, Bonovas S, et al. Safety of Janus kinase inhibitors in patients with inflammatory bowel diseases or other immune-mediated diseases: a systematic review and meta-analysis. Gastroenterology 2020;158:1554–73. e12. 10.1053/j.gastro.2020.01.001 [DOI] [PubMed] [Google Scholar]
- 33. Charles-Schoeman C, Fleischmann R, Davignon J, et al. Potential mechanisms leading to the abnormal lipid profile in patients with rheumatoid arthritis versus healthy volunteers and reversal by tofacitinib. Arthritis Rheumatol 2015;67:616–25. 10.1002/art.38974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bechman K, Yates M, Norton S, et al. Placebo response in rheumatoid arthritis clinical trials. J Rheumatol 2020;47:28–34. 10.3899/jrheum.190008 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
annrheumdis-2020-219214supp001.pdf (383.3KB, pdf)
annrheumdis-2020-219214supp002.pdf (245.4KB, pdf)
annrheumdis-2020-219214supp003.pdf (34.6KB, pdf)
annrheumdis-2020-219214supp004.pdf (1.2MB, pdf)
Data Availability Statement
Data are available upon reasonable request. Anonymised individual patient data will be shared upon request for research purposes dependent upon the nature of the request, the merit of the proposed research, the availability of the data and the intended use. The full data sharing policy for Gilead Sciences can be found at https://www.gilead.com/about/ethics-and-code-of-conduct/policies.