Abstract
Background:
The current techniques for medial malleolar osteotomy may lead to posterior tibial tendon injury and have a high rate of malunion.
Purpose:
To describe a novel partial step-cut medial malleolar osteotomy technique and evaluate its technical feasibility and its advantages compared with traditional methods.
Study Design:
Case series; Level of evidence, 4.
Methods:
The novel technique consisted of osteotomy of the anterior one-third to two-thirds of the medial malleolus. A total of 19 ankles (18 patients) with osteochondral lesions of the talus underwent the novel osteotomy technique before osteochondral reconstruction. All patients were evaluated for more than 2 years. Radiographs were analyzed for postoperative displacement and malunion, and postoperative ankle function was evaluated according to the American Orthopaedic Foot & Ankle Society (AOFAS) ankle-hindfoot scale and the visual analog scale (VAS) for pain.
Results:
The partial step-cut osteotomy technique was able to provide adequate intra-articular exposure without disturbing the posterior tibial tendon. The 19 ankles healed at a mean of 7.3 ± 1.5 weeks (range, 6-12 weeks). There was slight incongruence in 4 ankles, with a displacement of 1.0 ± 0.1 mm proximally and 0.3 ± 0.1 mm medially. The mean postoperative AOFAS and VAS scores improved compared with preoperatively, from 54.2 ± 12.1 to 84.6 ± 6.6 and from 6.4 ± 1.0 to 1.8 ± 1.3, respectively (P < .001 for both). No intraoperative tendon injuries were observed.
Conclusion:
Results indicated that partial step-cut osteotomy is a reliable and effective method for providing enough exposure, avoiding displacement after reduction, and not disturbing the anatomic structures behind the medial malleolus.
Keywords: displacement, mechanical stability, osteochondral lesions, talar fracture
Osteochondral lesions of the talus (OLTs) are the most common articular cartilage defects in the ankle joint. The condition may lead to disability because of chronic pain and limited weightbearing capacity. OLTs are frequently seen in patients with ankle fractures or ankle sprains. 4,20 The treatment strategies and techniques for osteochondral defects of the ankle have advanced dramatically in the past decade, but treatment options still remain controversial.
Multiple surgical options exist to treat OLTs, and many are dependent on the stage, location, and size of the lesion. Access to the ankle joint with smaller lesions can often be performed through arthroscopic techniques. Arthroscopic treatment with microfracture is recommended for lesions smaller than 150 mm2. Lesions larger than 150 mm2 have a lower success rate when treated purely through microfracture, and some sort of open grafting is likely utilized. Medial or lateral malleolar osteotomy is always performed to achieve adequate intra-articular exposure for autologous bone cartilage transplantation or other transplantation procedures. 2,10,12,15
In 2007, Elias et al 7 showed that OLTs are more frequently located in the medial talar dome. Access to the medial half of the talus can be challenging, even with osteotomy. Some earlier methods, including straight transverse, inverted U- or V-shape, or crescentic osteotomy, provided limited exposure of the lesions, as these osteotomy techniques are performed at or below the level of the ankle joint. The more recent biplane chevron and step-cut osteotomy techniques provide wider exposure, a broad cancellous surface for healing, and greater intrinsic theoretical stability. 9,18 However, Bull et al 3 showed that biplane chevron medial malleolar osteotomy fixed with 2 lag screws had a 30% malunion rate, with an average of 2 mm of incongruence on final follow-up radiographs. Displacement after osteotomy can lead to advanced ankle osteoarthritis. 10 In addition, there is always a risk of injuries to the posterior tibial tendon behind the medial malleolus, so care needs to be taken to protect anatomic structures during osteotomy. 9,15,18
The aim of the current study was to evaluate a partial step-cut technique consisting of osteotomy to only the anterior one-third to two-thirds of the medial malleolus (depending on the OLT location). We hypothesized that this novel osteotomy technique will expose the talus adequately and can safely avoid injuries to the anatomic structures posterior to the medial malleolus.
Methods
This study was approved by the ethics committee of our hospital, and informed consent was obtained from each patient enrolled. A total of 18 patients (19 ankles) underwent autologous osteoperiosteal or osteochondral grafting procedures for OLTs through partial step-cut medial malleolar osteotomy (Figure 1) from August 2015 to October 2016. All patients had experienced a traumatic event to the ankle within 2 years of their initial hospital visit, and 1 patient had a bilateral injury. All patients had ankle pain that was resistant to nonsurgical treatment including rest, oral nonsteroidal anti-inflammatory drugs, and cast immobilization. We excluded patients with an immature skeleton so as not to disturb bone growth. Patients with arthritic changes in their ankle joint or deformities to the axis of the ankle on plain radiographs were also excluded.
Figure 1.
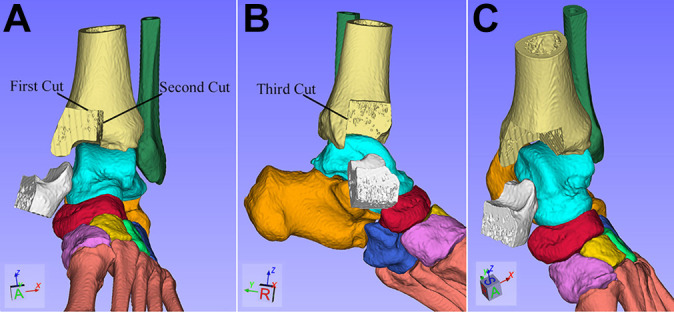
Diagram of the partial step-cut osteotomy technique. (A) The first cut was made approximately 1.5 to 2.0 cm above the anterior margin of the distal tibia at the ankle joint in the transverse plane, and the second cut was made approximately 1.5 to 2.0 cm lateral to the axilla on the medial tibial plafond in the sagittal plane. (B) The depth of these 2 cuts involved the anterior one-third to two-thirds of the medial malleolus in the sagittal plane. The third cut was made in the coronal plane to join the above 2 cuts. (C) The osteotomized medial malleolus was then reflected plantarward on the deltoid ligament to expose the medial part of the talar dome.
We recorded the duration of surgery, which was defined as the time from incision to the completion of osteotomy. All patients were evaluated clinically and radiographically before surgery and as part of the follow-up. For the clinical evaluation, the visual analog scale (VAS) for pain and the American Orthopaedic Foot & Ankle Society (AOFAS) ankle-hindfoot scale were administered. During the preoperative examination, magnetic resonance imaging (MRI) (3.0-T Discovery MR750; GE Healthcare) was performed to measure the size and location of the lesions. The OLT size was measured via the following formula using a picture archiving and communication system (Centricity Enterprise Web V3.0; GE Healthcare): area = abπ/4 = coronal length × sagittal length × 0.79 (calculated from the maximum coronal and sagittal length on MRI). 5,14 We also reconfirmed the defect size intraoperatively. Postoperative radiographs obtained at 6, 8, and 12 weeks and at final follow-up were evaluated. Displacement was measured accurately on the final follow-up radiographs through the picture archiving and communication system. Healing was determined to be complete when bone bridging on all osteotomy cortices was noted on postoperative radiographs. To avoid potential bias, a single investigator (C.Y.), who was a trained musculoskeletal radiologist, measured osteotomy displacement on all scans.
Surgical Technique
The osteotomy technique was performed as follows with the patient under spinal anesthesia.
Step 1
The anterior and medial sides of the medial malleolus were exposed through an incision slightly anterior to the midline and curved at the malleolus (Figure 2A). Anterior and posterior skin flaps were developed, leaving the periosteum of the tibia intact. An incision was made in the anterior capsule, exposing the medial malleolus.
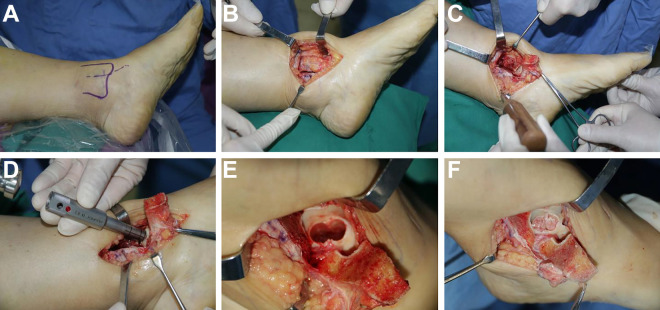
Figure 2.
Exposure of the talus. (A) The anterior and medial sides of the medial malleolus were exposed through an incision slightly anterior to the midline and curved at the malleolus. (B) A total of 3 cuts were performed. (C) The medial malleolus was then reflected plantarward on the deltoid ligament to expose the medial osteotomized part of the talar dome. (D) The necrotic sequestrum was removed and curetted until bleeding was observed from the surrounding bone. (E) Autologous osteoperiosteal cylinder grafting of the iliac crest. (F) The harvested block was inserted into the defect with the periosteum layer parallel to the cartilage level.
Step 2
Predrilling the medial malleolus was useful to reduce the medial malleolus more accurately and easily at the end of the procedure. One hole was drilled in the medial malleolus with a 2.0-mm drill directed from the anterior to posterior side, and another hole was drilled from the medial to lateral side of the bone, approximately 0.6 to 1.2 cm above the anterior margin of the distal tibia at the ankle joint. The 2 holes were located in the near-center square of the proposed osteotomy site to facilitate fragment reduction.
Step 3
After locking the ankle in plantarflexion and then using a microsagittal saw with a broad blade (10 mm), the first cut was made approximately 1.5 to 2.0 cm above the anterior margin of the distal tibia at the ankle joint in the transverse plane. The depth of this cut involved the anterior one-third to two-thirds of the medial malleolus in the sagittal plane. The second cut was made approximately 1.5 to 2.0 cm lateral to the axilla on the medial tibial plafond (which was determined by the size of the OLT) in the sagittal plane. The depth involved the anterior two-thirds of the medial malleolus in the sagittal plane. The third cut was made in the coronal plane to join the above 2 cuts (Figure 2B). Care was taken to recognize the location of the posterior tibialis tendon during this process. The osteotomized medial malleolus was then reflected plantarward on the deltoid ligament to expose the medial side of the talar dome (Figure 2C). When performing osteotomy, care must be taken not to damage the articular surface of the tibial plafond because harm to the weightbearing surface might affect clinical outcomes. Then, after making a hole about 8 mm in diameter in the subchondral plate, the necrotic sequestrum was removed and curetted until bleeding was observed from the surrounding bone (Figure 2, D and E).
Step 4
We performed osteochondral autograft transplantation or autologous osteoperiosteal cylinder grafting to fill the defect. Osteochondral autograft transplantation was preferred for younger patients, and autologous osteoperiosteal cylinder grafting was preferred for older patients. Osteochondral autograft cylinders were harvested from the upper lateral condyle of the ipsilateral knee. Transplantation was performed using an osteochondral autograft transfer system and the press-fit technique (Arthrex). Autologous osteoperiosteal cylinders were harvested from the iliac crest with caution so as not to damage the periosteum, and they were inserted into the defect of the talus with the periosteum layer parallel to the cartilage level (Figure 2F). Subsequently, the malleolus was placed in its original position and fixed with compression using two 3.5- to 4.0-mm cancellous lag screws or 1 lag screw plus a buttress plate (Figure 3). All osteotomy sites were anatomically reduced both clinically and radiographically at the time of surgery. Deep and subcutaneous layers were closed using absorbable suture, followed by nonabsorbable horizontal mattress suture for the skin.
Figure 3.
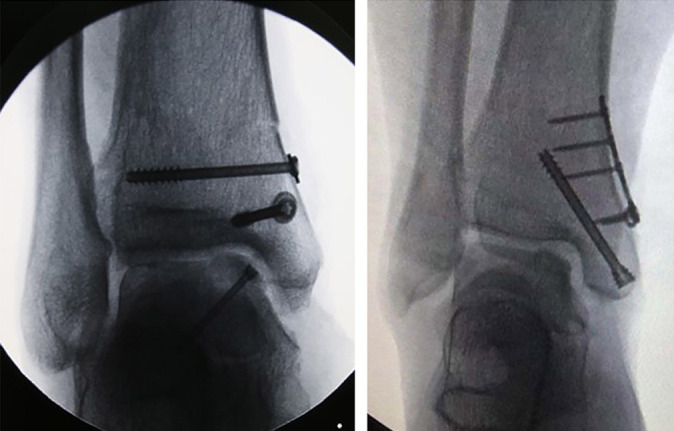
Immediate fixation after osteotomy with 2 cancellous lag screws or 1 lag screw plus a buttress plate.
Postoperative Care
The patients were allowed to begin passive range of motion exercises 2 weeks after surgery and active range of motion exercises after that, and partial weightbearing was encouraged with an ankle support at 6 weeks postoperatively. Unprotected weightbearing, as tolerated, was permitted after clinical and radiological confirmation of union at the osteotomy site.
Statistical Analysis
Continuous variables are expressed as mean ± SD. Data analysis was performed using the paired Student t test or Fisher exact test. Statistical significance was defined as P < .05. Statistical analysis was performed using SPSS Version 21.0 (IBM).
Results
The characteristics of the study patients are shown in Table 1. The mean patient age was 38.3 ± 9.0 years (range, 19-52 years), and the mean lesion size according to MRI was 2.0 ± 0.4 cm2 (range, 1.2-2.8 cm2). Of the 19 ankles, 5 (26.3%) had an uncontained-type OLT, and 14 (73.7%) had a contained-type OLT. The right side was affected in 13 (68.4%) ankles. The lesions were located in zones 1 (n = 2), 4 (n = 15), and 7 (n = 2) according to the 9-zone anatomic grid system of the talar dome by Elias et al 7 (Figure 4). There were 6 ankles (31.6%) that had undergone prior surgery. Overall, 3 ankles (15.8%) underwent osteotomy combined with anterior talofibular ligament reconstruction. The majority of ankles (13/19; 68.4%) underwent osteotomy secured with 2 lag screws; the remaining 6 ankles (31.6%) received a buttress plate in addition to a lag screw. The mean osteotomy time was 12.6 ± 1.9 minutes (range, 10-16 minutes).
Table 1.
Characteristics of Study Patients a
| Patient | Age, y | Sex | Side Affected | Lesion Size, cm2 | Containment Type | Zone b | Previous Intervention | Associated Procedure | Type of Fixation | Osteotomy Time, min |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 47 | M | R | 2.8 | Uncontained | 1 | — | — | 2 lag screws | 12 |
| 2 | 35 | M | R | 2.5 | Uncontained | 4 | — | ATFL reconstruction | Plate + 1 lag screw | 13 |
| 3 | 25 | M | R | 2.2 | Contained | 4 | Debridement | — | 2 lag screws | 16 |
| 4 | 43 | M | L | 2.1 | Contained | 4 | — | — | 2 lag screws | 11 |
| 5 | 19 | M | R | 2.4 | Uncontained | 4 | — | ATFL reconstruction | 2 lag screws | 15 |
| 6 | 38 | F | R | 2.5 | Uncontained | 4 | Debridement | — | 2 lag screws | 14 |
| 7 | 40 | F | R | 2 | Contained | 4 | — | — | Plate + 1 lag screw | 15 |
| 8 | 48 | M | R | 1.8 | Contained | 4 | — | — | Plate + 1 lag screw | 11 |
| 9 | 52 | M | R | 1.2 | Contained | 4 | Microfracture | — | Plate + 1 lag screw | 14 |
| 10 | 43 | M | L | 1.5 | Contained | 4 | — | — | Plate + 1 lag screw | 12 |
| 11 | 36 | F | R | 2.2 | Contained | 4 | — | — | Plate + 1 lag screw | 12 |
| 12 | 42 | M | Bilateral | 1.6 (L); 2 (R) | Contained (both sides) | 4 (both sides) | — | — | 2 lag screws (both sides) | 10 (L); 11 (R) |
| 13 | 26 | M | R | 1.8 | Contained | 7 | — | — | 2 lag screws | 13 |
| 14 | 38 | M | L | 1.9 | Contained | 4 | Synovectomy | — | 2 lag screws | 12 |
| 15 | 42 | M | R | 2.2 | Contained | 1 | Microfracture | — | 2 lag screws | 15 |
| 16 | 28 | F | L | 1.6 | Uncontained | 4 | — | ATFL reconstruction | 2 lag screws | 10 |
| 17 | 38 | M | R | 1.8 | Contained | 4 | Debridement | — | 2 lag screws | 10 |
| 18 | 50 | M | L | 2.4 | Contained | 7 | — | — | 2 lag screws | 14 |
a Dashes indicate that the category is not applicable. ATFL, anterior talofibular ligament; F, female; L, left; M, male; R, right.
b According to the 9-zone grid scheme of Elias et al. 7
Figure 4.
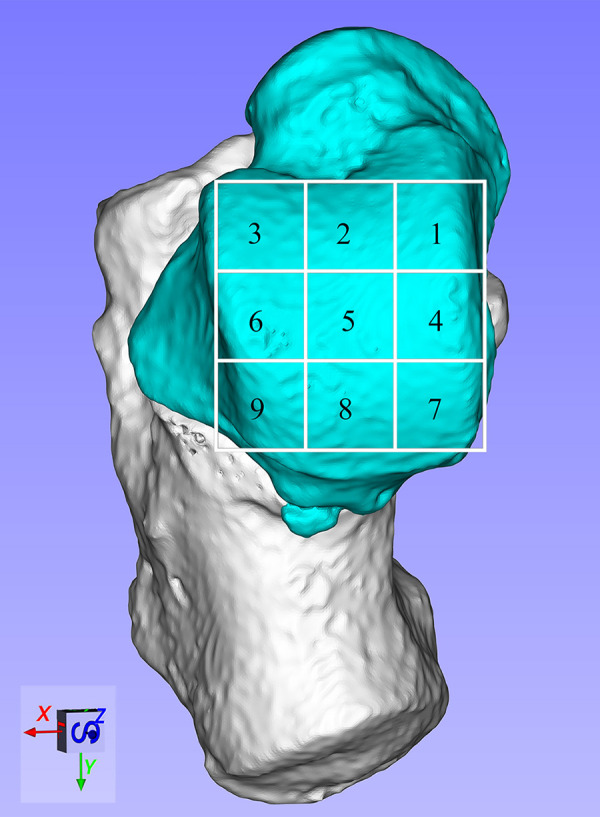
The 9-zone anatomic grid scheme of the talar dome used to indicate the location of the osteochondral lesion of the talus. Zones 1, 4, and 7 are positioned on the medial talus, and zones 1, 2, and 3 are positioned anteriorly.
All patients were available for a minimum 24-month follow-up (mean, 31.9 ± 4.1 months [range, 26-40 months]). By the final follow-up, the articular surface of the tibial plafond at the malleolar osteotomy site was smooth in all cases visually (Figure 5). After magnifying the radiographs, displacement was measured in 4 cases and indicated a mean displacement of 1.0 ± 0.1 mm proximally and 0.3 ± 0.1 mm medially. In detail, 1 of 6 ankles fixed with a buttress plate plus a lag screw had measurable incongruence, with a displacement of 1.0 mm proximally and 0.3 mm medially. Moreover, 3 of 13 ankles fixed with 2 screws had measurable incongruence, with a displacement averaging 1.0 ± 0.2 mm proximally and 0.3 ± 0.2 mm medially. There was no difference statistically in the occurrence of displacement between the 2 types of fixation (P = .593). By the 6-week postoperative follow-up, nearly half (9/19; 47.4%) of the cases were clinically and radiographically healed, and all of the cases achieved union by 12 weeks (Figure 5). The mean time to healing based on radiographs was 7.4 ± 1.7 weeks (range, 6-12 weeks) for fixation with 2 screws, 7.0 ± 1.1 weeks (range, 6-8 weeks) for 1 screw plus 1 buttress plate, and 7.3 ± 1.5 weeks (range, 6-12 weeks) overall. There was no significant difference statistically between the 2 types of fixation with respect to bone healing time (P = .611).
Figure 5.

Follow-up radiographs demonstrating union after osteotomy.
Before surgery, the mean VAS score was 6.4 ± 1.0, and the mean AOFAS score was 54.2 ± 12.1. At the last follow-up, the mean VAS and AOFAS scores had improved significantly to 1.8 ± 1.3 and 84.6 ± 6.6, respectively (P < .001 for both). Detailed results are shown in Table 2. All patients were able to return to recreational sports or at least moderately heavy labor. No patients had hardware problems, but in 12 cases the patients still elected to have hardware removed at a mean of 12.2 ± 1.9 weeks postoperatively. No other complications such as intraoperative tendon injuries, ankle joint stiffness, or postoperative infections were observed.
Table 2.
Radiographic and Functional Results a
| Patient | Medial Displacement, mm | Proximal Displacement, mm | AOFAS Score | VAS Score | Time to Heal, wk | ||
|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | ||||
| 1 | 0.2 | 1 | 65 | 78 | 7.5 | 2 | 6 |
| 2 | 0.3 | 1 | 50 | 81 | 6.5 | 3.5 | 8 |
| 3 | 0 | 0 | 60 | 92 | 6 | 2 | 6 |
| 4 | 0 | 0 | 44 | 90 | 7 | 0 | 8 |
| 5 | 0 | 0 | 64 | 87 | 7 | 0 | 8 |
| 6 | 0.5 | 1 | 58 | 70 | 6.5 | 0 | 6 |
| 7 | 0 | 0 | 40 | 82 | 5 | 2.5 | 6 |
| 8 | 0 | 0 | 55 | 80 | 6.5 | 3 | 6 |
| 9 | 0 | 0 | 50 | 91 | 8 | 4 | 8 |
| 10 | 0 | 0 | 66 | 88 | 5 | 2 | 6 |
| 11 | 0 | 0 | 44 | 87 | 5 | 0.5 | 6 |
| 12 (L) | 0 | 0 | 58 | 79 | 7 | 2 | 8 |
| 12 (R) | 0 | 0 | 69 | 98 | 7 | 0 | 8 |
| 13 | 0.2 | 0.9 | 64 | 82 | 6.5 | 2.5 | 6 |
| 14 | 0 | 0 | 75 | 87 | 6 | 2 | 12 |
| 15 | 0 | 0 | 32 | 88 | 5.5 | 1.5 | 8 |
| 16 | 0 | 0 | 59 | 77 | 8 | 4 | 8 |
| 17 | 0 | 0 | 41 | 80 | 7 | 2 | 8 |
| 18 | 0 | 0 | 36 | 90 | 5 | 1 | 6 |
a AOFAS, American Orthopaedic Foot & Ankle Society; L, left; R, right; VAS, visual analog scale.
Discussion
Symptomatic OLTs with failure of nonoperative management often require operative treatment. Lesions that fail to heal after appropriate arthroscopic treatment may then require open treatment through exposure by medial malleolar osteotomy. In the current study, we treated large (>1.5 cm2) talar OCTs or smaller lesions that had failed index arthroscopic debridement with microfracture through osteochondral autograft/allograft transfer or bulk allograft reconstruction through medial malleolar osteotomy.
The primary purpose of osteotomy is to provide enough space to allow grafting, and various medial malleolar osteotomy techniques have been introduced for osteoperiosteal or osteochondral grafting. 1,6,17,21 Recently, the commonly used biplane chevron and step-cut osteotomy techniques were shown to offer wide exposure because they are performed above the level of the ankle joint. 9,13,18 In our experience, anterior two-thirds step-cut osteotomy with the ankle at maximal plantarflexion can also provide enough space for osteochondral or osteoperiosteal grafting because the talar articular cartilage moves forward compared with the neutral position when the ankle is at maximal plantarflexion. In our series, 2 lesions in anatomic zone 1, 15 in zone 4, and 2 in zone 7 were explored and treated successfully with osteoperiosteal grafting or osteochondral grafting through this osteotomy technique. We do not conclude that partial step-cut osteotomy is suitable for all medial OLTs, especially for posteromedial OLTs, but most medial lesions would be exposed enough by this type of osteotomy.
Stability is another important concern for medial malleolar osteotomy. Nonunion, rotational deformities, and translation of the medial malleolus at the osteotomy site can result from instability. 3,19 Kim et al 11 reported that osteotomy displacement led to unsatisfactory results. When the articular surface of the tibial plafond at the malleolar osteotomy site was even, second-look arthroscopic surgery revealed a well-healed surface of the osteotomy site, however when the articular surface of the tibial plafond at the malleolar osteotomy site was uneven, the articular surface of the osteotomy site was filled with fibrous tissue, and VAS and AOFAS scores were significantly worse. 11 Osteotomy displacement can eventually lead to advanced ankle osteoarthritis. Gaulrapp and colleagues 8 found that osteotomy displacement led to osteoarthritis and less than favorable outcomes. They reported arthritic changes in up to 50% of ankles in 22 patients within 5 years of treatment. 8
Stability of the osteotomy site depends on the type of osteotomy and type of fixation. 3,9,11,18 In the past, oblique osteotomy resulted in natural instability, although it can provide wide exposure. 15 Numerous authors have reported that oblique osteotomy provided access to medial talar dome lesions for bulk talar allograft/autograft reconstruction. 3,16 In each case, superomedial displacement was acknowledged as a potential complication after medial malleolar osteotomy. Currently, step-cut osteotomy has been widely used because of its intrinsic stability, but studies have still reported a high malunion rate. 3 We speculate that the reason for the complications was that the whole medial malleolus is resected completely during the procedure. As a result, fixed osteotomy has limited ability against supination, adduction, or abduction before healing, which may cause osteotomy displacement and consequently an uneven articular surface of the tibial plafond. In our series, no cases had an uneven articular surface of the tibial plafond at the malleolar osteotomy site visually, and the measured results were much lower than those reported by Bull and colleagues. 3 Also, all ankles in the current study achieved union at 7.3 ± 1.5 weeks, which is similar to the union time of chevron-type medial malleolar osteotomy. 13
The type of fixation plays an important role in the prevention of osteotomy displacement. 3,11 The buttress plate has been shown to provide more reliable support for osteotomy than screws. 9 We did not obtain similar results at follow-up, although we did when performing fixation; perhaps more participants are needed to confirm our findings. Because of the stability of our osteotomy method, patients were allowed intensive motion exercises at 2 weeks postoperatively, followed by partial weightbearing exercises. As a result, no patients complained of any joint stiffness during the follow-up, and the AOFAS scores after surgery significantly increased compared with preoperatively.
For medial malleolar osteotomy, the posterior tibial tendon passes posterior to the medial malleolus, so the posterior tibial tendon sheath must be incised to explore the posterior tibialis tendon and protect it during osteotomy. This procedure prolongs the operation time. As the important anatomic structures behind the medial malleolus are not disturbed during partial step-cut osteotomy, only 12.6 ± 1.9 minutes were spent on the procedure, which is much shorter than the surgery duration for biplane chevron or step-cut osteotomy.
One limitation of this study was the lack of a control group. Another is that the follow-up was so short that we cannot comment on arthritic changes using the technique. We also realize that broad treatment recommendations cannot be based on a review of a small number of patients. However, we found that partial step-cut medial malleolar osteotomy can provide excellent exposure for the medial part of the talar dome without disturbing the anatomic structures behind the medial malleolus and can preserve structural stability in the early postoperative stage while maintaining the advantages of traditional osteotomy methods.
Conclusion
According to our study results, the novel partial step-cut osteotomy technique was able to explore most OLTs located in the medial aspect of the talus and offer enough space for osteochondral or osteoperiosteal grafting. Furthermore, the anatomic structures behind the medial malleolus did not need to be deliberately protected, which shortened the osteotomy time. Results indicated that the procedure provides excellent intrinsic stability, allowing early rehabilitation for patients.
Footnotes
Final revision submitted September 2, 2020; accepted September 25, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: This research was supported by the Key Research and Development Program of Shandong Province (No. 2019GSF108092) and the Jinan Science and Technology Development Project (No. 201805012). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from The Second Hospital of Shandong University.
References
- 1. Alexander IJ, Watson JT. Step-cut osteotomy of the medial malleolus for exposure of the medial ankle joint space. Foot Ankle. 1991;11(4):242–243. [DOI] [PubMed] [Google Scholar]
- 2. Buda R, Vannini F, Castagnini F, et al. Regenerative treatment in osteochondral lesions of the talus: autologous chondrocyte implantation versus one-step bone marrow derived cells transplantation. Int Orthop. 2015;39(5):893–900. [DOI] [PubMed] [Google Scholar]
- 3. Bull PE, Berlet GC, Canini C, Hyer CF. Rate of malunion following bi-plane chevron medial malleolar osteotomy. Foot Ankle Int. 2016;37:620–626. [DOI] [PubMed] [Google Scholar]
- 4. Chan KB, Lui TH. Role of ankle arthroscopy in management of acute ankle fracture. Arthroscopy. 2016;32(11):2373–2380. [DOI] [PubMed] [Google Scholar]
- 5. Choi WJ, Park KK, Kim BS, Lee JW. Osteochondral lesion of the talus: is there a critical defect size for poor outcome? Am J Sports Med. 2009;37(10):1974–1980. [DOI] [PubMed] [Google Scholar]
- 6. Cohen BE, Anderson RB. Chevron-type transmalleolar osteotomy: an approach to medial talar dome lesions. Tech Foot Ankle Surg. 2002;1(2):158–162. [Google Scholar]
- 7. Elias I, Zoga AC, Morrison WB, Besser MP, Schweitzer ME, Raikin SM. Osteochondral lesions of the talus: localization and morphologic data from 424 patients using a novel anatomical grid scheme. Foot Ankle Int. 2007;28(2):154–161. [DOI] [PubMed] [Google Scholar]
- 8. Gaulrapp H, Hagena FW, Wasmer G. Postoperative evaluation of osteochondrosis dissecans of the talus with special reference to medial malleolar osteotomy [in German]. Z Orthop Ihre Grenzgeb. 1996;134(4):346–353. [DOI] [PubMed] [Google Scholar]
- 9. Granata JD, DeCarbo WT, Hyer CF, Granata AM, Berlet GC. Exposure of the medial talar dome: bi-plane chevron medial malleolus osteotomy. Foot Ankle Spec. 2013;6(1):12–14. [DOI] [PubMed] [Google Scholar]
- 10. Jackson AT, Drayer NJ, Samona J, et al. Osteochondral allograft transplantation surgery for osteochondral lesions of the talus in athletes. J Foot Ankle Surg. 2019;58(4):623–627. [DOI] [PubMed] [Google Scholar]
- 11. Kim YS, Park EH, Kim YC, et al. Factors associated with the clinical outcomes of the osteochondral autograft transfer system in osteochondral lesions of the talus: second-look arthroscopic evaluation. Am J Sports Med. 2012;40(12):2709–2719. [DOI] [PubMed] [Google Scholar]
- 12. Kubosch EJ, Erdle B, Izadpanah K, et al. Clinical outcome and T2 assessment following autologous matrix-induced chondrogenesis in osteochondral lesions of the talus. Int Orthop. 2016;40(1):65–71. [DOI] [PubMed] [Google Scholar]
- 13. Lamb J, Murawski CD, Deyer TW, Kennedy JG. Chevron-type medial malleolar osteotomy: a functional, radiographic and quantitative T2-mapping MRI analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1283–1288. [DOI] [PubMed] [Google Scholar]
- 14. Lee KB, Bai LB, Chung JY, Seon JK. Arthroscopic microfracture for osteochondral lesions of the talus. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):247–253. [DOI] [PubMed] [Google Scholar]
- 15. Leumann A, Horisberger M, Buettner O, Mueller-Gerbl M, Valderrabano V. Medial malleolar osteotomy for the treatment of talar osteochondral lesions: anatomical and morbidity considerations. Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2133–2139. [DOI] [PubMed] [Google Scholar]
- 16. Navid DO, Myerson MS. Approach alternatives for treatment of osteochondral lesions of the talus. Foot Ankle Clin. 2012;7(3):635–649. [DOI] [PubMed] [Google Scholar]
- 17. Oznur A. Medial malleolar window approach for osteochondral lesions of the talus. Foot Ankle Int. 2001;22(10):841–842. [DOI] [PubMed] [Google Scholar]
- 18. Siegel SJ, Mount AC. Step-cut medial malleolar osteotomy: literature review and case reports. J Foot Ankle Surg. 2012;51(2):226–233. [DOI] [PubMed] [Google Scholar]
- 19. Spatt JF, Frank NG, Fox IM. Transchondral fractures of the dome of the talus. J Foot Surg. 1986;25(1):68–72. [PubMed] [Google Scholar]
- 20. Takao M, Ochi M, Uchio Y, et al. Osteochondral lesions of the talar dome associated with trauma. Arthroscopy. 2003;19(10):1061–1067. [DOI] [PubMed] [Google Scholar]
- 21. Wallen EA, Fallat LM. Crescentic transmalleolar osteotomy for optimal exposure of the medial talar dome. J Foot Surg. 1989;28(5):389–394. [PubMed] [Google Scholar]