Abstract
Background:
A lack of lumbopelvic-hip complex (LPHC) stability is often associated with altered pitching mechanics, thus increasing pain and injury susceptibility. The single-leg squat (SLS) is a simple diagnostic tool used to examine LPHC stability.
Purpose:
To examine the relationship between trunk compensatory kinematics during the SLS and kinematics at foot contact during the windmill pitch.
Study Design:
Descriptive laboratory study.
Methods:
Participants included 55 youth and high school softball pitchers (mean age, 12.6 ± 2.2 years; height, 160.0 ± 11.0 cm; weight, 60.8 ± 15.5 kg). Kinematic data were collected at 100 Hz using an electromagnetic tracking device. Participants were asked to complete an SLS on each leg, then throw 3 fastballs at maximal effort. Values of trunk flexion, trunk lateral flexion, and trunk rotation at peak depth of the SLS were used as the dependent variables in 3 separate backward-elimination regression analyses. Independent variables examined at foot contact of the pitch were as follows: trunk flexion, trunk lateral flexion, trunk rotation, center of mass, stride length, and stride knee valgus.
Results:
The SLS trunk rotation regression (F(1,56) = 4.980, P = .030) revealed that trunk flexion predicted SLS trunk rotation (SE = 0.068, t = 2.232, P = .030) and explained approximately 7% of the variance in SLS trunk rotation (R 2 = 0.083, adjusted R 2 = 0.066). The SLS trunk flexion regression (F(1,56) = 5.755, P = 0.020) revealed that stride knee valgus significantly predicted SLS trunk flexion (SE = 0.256, t = 2.399, P = .020) and explained approximately 8% of variance in SLS trunk flexion (R 2 = 0.095, adjusted R 2 = 0.078).
Conclusion:
Additional trunk rotation and trunk flexion at peak depth of the SLS showed increased knee valgus and trunk flexion at foot contact of the pitch, both of which indicate poor LPHC stability during the softball pitch and may increase the potential for injury.
Clinical Relevance:
Players and coaches should implement SLS analyses to determine their players’ risk for injury and compensation due to poor core stability.
Keywords: core stability, lumbopelvic-hip stability, pitching injury susceptibility, windmill softball pitch
Despite the perception that pitching is an upper-extremity activity, proper utilization of the lower extremity and trunk is needed for optimal performance and decreased injury susceptibility. ** Softball pitching is a full-body dynamic and sequential movement that relies heavily on lower-extremity contribution to achieve maximal pitch velocity, control, accuracy, and proper mechanics. This total-body dynamic movement is the result of the integrated, multisegmented system of the body acting as a kinetic chain. Kinetic chain efficiency is accomplished when the proximal or lower extremity can generate and produce maximal energy and force to be transferred through the trunk and on to the distal upper extremity and into the ball. Any alteration in force generation or transfer results in a disruption in the kinetic chain, placing undue stress on injury-susceptible joints. 6,19,23,44,45 While most literature regarding softball pitching mechanics focuses solely on the upper extremity, 26 –29,34,35,42,51,52 research has shown the importance of proximal to distal sequencing via the kinetic chain. 6,19,44
Typically, dynamic upper extremity movements utilize the proximal lower extremity to generate 50% to 55% of the total energy generated at the distal end of the chain. 6,17,19,44 However, for the efficient transfer of energy from the lower to upper extremity, there must be lumbopelvic-hip complex (LPHC) stability. 6,18,19,44,45 Stability of the LPHC during dynamic upper-extremity movements is commonly associated with gluteal muscle activation resulting in pelvic stability. 5,20,21,25,30,35,37 –39 It has been theorized that the LPHC provides the proximal stability for distal mobility, highlighting the role of the LPHC in providing a stable platform against which distal muscles can pull and accelerate. 18 Therefore, we define LPHC control as the ability to stabilize the LPHC in an effort to mobilize segments distal to the trunk. Specific to dynamic upper extremity movement, we see the effect of LPHC control in trunk kinematics and pitch volume. 1,11,27 –29,34,36 Additionally, it is known that the musculature of the lower extremity is active during the softball pitch, 35 and it is the activation of the gluteal musculature in both the drive and stride leg that controls the trunk in softball pitching. 35
Examination of LPHC control and stability is commonly performed through the assessment of a single-leg squat (SLS). 7,40,47,50 The SLS is a reliable assessment of LPHC strength, 7,49 sport performance, 12,40 and lower-extremity pain. 13 Those with reduced LPHC stability often display compensatory mechanics of knee valgus, pelvic tilt, trunk lean, and trunk rotation. 18 The functional stability of the LPHC is fundamentally supplied through the activation of the gluteal muscle group. Specifically, the gluteal muscle group allows for stabilization of the trunk over single-leg support. Thus, SLS assessment of LPHC stability emphasizes weakness in the gluteal muscle group resulting in kinematic compensations of knee valgus, trunk flexion, and trunk rotation. 7,40,47,50
An examination of the literature regarding LPHC stability and upper-extremity dynamic movement, specifically in baseball, revealed that a lack of LPHC stability during the SLS is often associated with altered pitching mechanics, thus increasing pain and injury susceptibility. 21,40,50 Based on the known compensatory patterns displayed in SLS assessment, we hypothesized that individuals who display greater knee valgus, trunk flexion, and/or trunk rotation during the SLS may also display trunk compensations during a dynamic upper-extremity movement, such as the windmill softball pitch. Trunk kinematics during the windmill pitch have previously been shown to differentiate those softball pitchers who currently experience upper-extremity pain from those who do not. More specifically, those with upper-extremity pain display differences in trunk flexion, trunk rotation, stride length, and center of mass positioning during the windmill pitch. Therefore, it seems plausible that those who display poor LPHC stability via SLS compensation may also exhibit trunk and lower-extremity pathomechanics during the windmill pitch previously associated with upper-extremity pain.
With the known injury susceptibility in windmill softball pitching, 2,8 –10,22,28,43,46 a thorough understanding of the association of LPHC stability and pitching mechanics is needed. The purpose of this study was to examine the relationship between trunk compensatory kinematics during the SLS and kinematics during foot contact of the windmill pitch. We hypothesized that there would be a relationship between SLS compensations and pitch kinematics previously associated with injury. In using a simple clinical assessment, such as the SLS, athletes, coaches, parents, and clinicians can identify potential risk factors that may predispose the athlete to previously recognized potentially injurious movement patterns during the softball pitch.
Methods
A total of 55 youth and high school softball pitchers (mean age, 12.6 ± 2.2 years; height, 160.0 ± 11.0 cm; weight, 60.8 ± 15.5 kg) were recruited to participate. Inclusion criteria included no lower- or upper-extremity injuries in the past 6 months and no history of surgery to the upper or lower extremity. The university’s institutional review board approved all testing protocols. Before data collection, all testing procedures were explained to each participant and informed assent and parental consent were obtained.
Participants reported to the laboratory for testing before engaging in any throwing or vigorous physical activity that day. After the study explanation, 14 electromagnetic sensors (Flock of Birds; Ascension Technologies Inc) were affixed to the skin: (1) posterior trunk at the first thoracic vertebrae (T1) spinous process; (2) posterior pelvis at the first sacral vertebrae (S1); (3-4) flat broad portion of the acromion (bilaterally); (5-6) bilateral upper arm at the deltoid tuberosity; (7-8) posterior distal forearm (bilaterally), approximately halfway between the radial and ulnar styloid processes; (9) dorsum of throwing-side hand, approximately halfway along the third metacarpal; (10-11) lateral thigh (bilaterally), approximately halfway between the greater trochanter and lateral condyle of the knee; (12-13) lateral shank (bilaterally), approximately halfway between the lateral condyle of the knee and lateral malleolus; and (14) dorsum of nonthrowing side foot, approximately halfway along the second metatarsal. A 15th sensor was attached to a movable plexiglass stylus for the digitization of bony landmarks. Sensor attachment sites are displayed in Figure 1.
Figure 1.
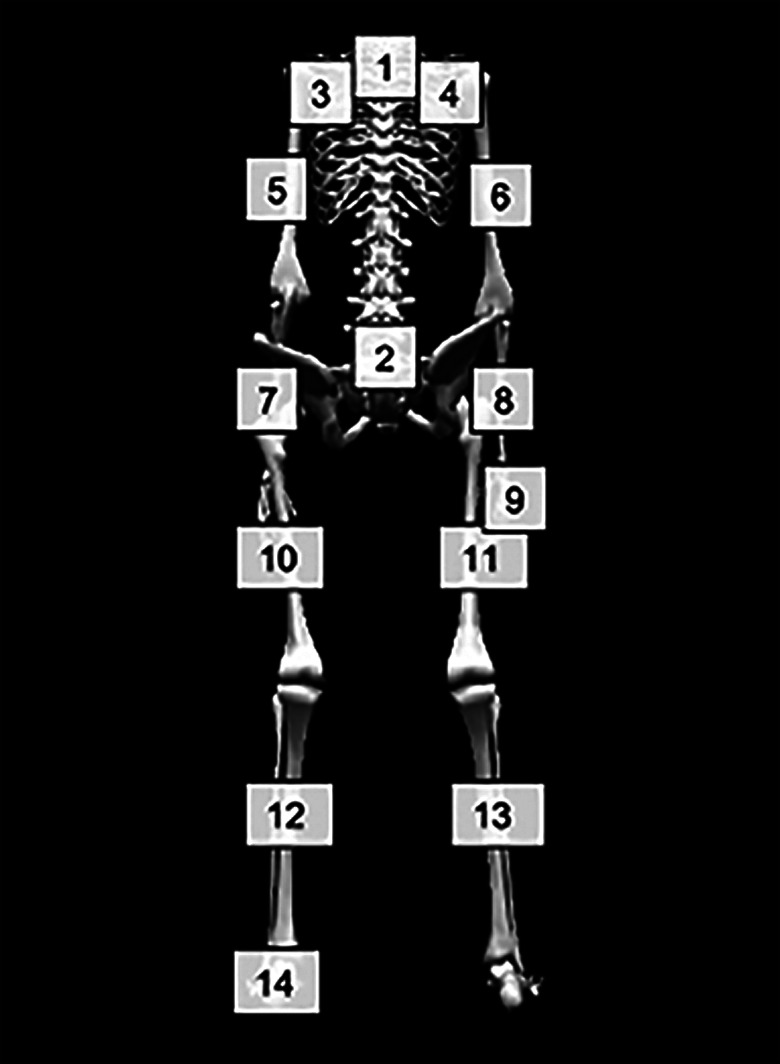
Image showing sensor attachment sites by body segment.
Kinematic data were collected at 100 Hz using an electromagnetic tracking device (trakSTAR; Ascension Technologies Inc) synchronized with The MotionMonitor software (Innovative Sports Training). 16,24 The digitized medial and lateral aspect of each joint, and the calculated midpoint between those 2 points, were used to develop a linked segment model. 30,31,53,54 Shoulder and hip joint centers were estimated using previously established rotation methods. 15,48 Raw data regarding sensor position and orientation were independently filtered along each global axis using a fourth-order Butterworth filter with a cutoff frequency of 20 Hz. The world axis was represented with the positive Y-axis in the vertical direction, anterior to the Y-axis and in the direction of movement was the positive X-axis, and orthogonal and to the right of X and Y was the positive Z-axis. Position and orientation of body segments were consistent with recommendations from the International Society of Biomechanics. 53,54
After sensor attachment and system calibration, participants performed an SLS repetition on their stride (glove-arm side) leg. 40 Participants were instructed to cross their arms over their chest, flex the nontesting knee to 90°, and to squat as low as they could while maintaining single-leg balance. After reaching peak depth, participants ascended to the starting position without letting their nontesting foot touch the ground and without letting their nontesting leg touch the testing leg. 12,40,49 A failed trial consisted of the nontesting leg touching the ground or resting on the testing leg. Cadence for the SLS was self-selected by the participant. 12,40,49 Participants were allowed to practice the task until they were comfortable performing a correct SLS, however they were not instructed on how to perform the SLS. This was to ensure that the participant’s preferred movement was not altered, and that measurement of the SLS was reflective of the participant’s current state of stability and skill.
After SLS performance, participants were allotted an unlimited amount of time to prepare for full-effort pitching. Individual pregame routines were allowed to ensure that each participant could most closely mimic in-game effort levels. 1 Once participants indicated they were ready, they performed 3 full-effort fastball pitches to a catcher at regulation distance (43 ft; 13.1 m).
The pitching motion was examined at foot contact when the pitcher made initial stride foot contact with the ground (force plate). The drive leg was defined as the leg ipsilateral to the pitching arm, and the stride leg was defined as the leg contralateral to the pitching arm. Center of mass (COM) position was calculated as a percentage of the pitch, with 0% representing COM directly over the drive leg and 100% representing COM directly over the stride leg. Stride length was calculated as a percentage of the participant’s body height.
The 3 fastball pitch trials were averaged, processed using a customized MATLAB script (R2010a; MathWorks), and analyzed using SPSS Statistics 24 software (IBM). All data were considered normal according to the Shapiro-Wilk test of normality. Values of trunk flexion, trunk lateral flexion, and trunk rotation at peak depth of the SLS were used as the dependent variables in 3 separate backward linear regression analyses, 1 for each dependent variable. Independent variables included the following kinematics at foot contact during the windmill pitch: trunk flexion; trunk lateral flexion; trunk rotation; COM; stride length; and stride knee valgus. Each regression began by fitting the full model and then eliminated variables with a greater than 10% probability of an association by chance alone (P > .10) to arrive at a final restricted model. The alpha level was set a priori to α = .05.
Results
Mean kinematics during the pitch and SLS are presented in Table 1. The backward regression involving SLS trunk rotation was statistically significant, F(1, 56) = 4.980, P = .030, and revealed trunk flexion predicted SLS trunk rotation (SE = 0.068; t = 2.232; P = .030). This regression equation explained approximately 7% of the variance in SLS trunk rotation (R 2 = 0.083; adjusted R 2 = 0.066). The backward regression involving SLS trunk flexion was also statistically significant, F(1,56) = 5.755, P = .020, and revealed stride knee valgus significantly predicted SLS trunk flexion (SE = 0.256; t = 2.399; P = .020). This regression equation explained approximately 8% of variance in SLS trunk flexion (R 2 = 0.095; adjusted R 2 = 0.078). The regression analysis involving SLS trunk lateral flexion was not statistically significant. A summary of the regression models is displayed in Table 2.
Table 1.
Kinematic Data During the Pitch and SLS a
| Variable | |
|---|---|
| SLS | |
| Peak trunk flexion, deg b | 21.10 ± 12.45 |
| Peak trunk rotation, deg c | –1.85 ± 6.26 |
| Peak trunk lateral flexion, deg d | –3.35 ± 8.03 |
| Pitching motion at foot contact | |
| Trunk flexion, deg b | 4.45 ± 11.92 |
| Trunk rotation, deg c | –59.51 ± 14.26 |
| Trunk lateral flexion, deg d | –7.86 ± 10.37 |
| Center of mass, % e | 45.70 ± 5.10 |
| Stride length, m | 0.92 ± 0.17 |
| Stride knee flexion, deg | –25.73 ± 10.28 |
| Stride knee valgus, deg | 1.43 ± 6.24 |
a Data are reported as mean ± SD unless otherwise indicated. SLS, single-leg squat.
b Positive value = forward flexion.
c Negative value = toward pitching arm.
d Negative value = toward glove arm.
e 0% represents center of mass directly over the drive leg and 100% represents center of mass directly over the stride leg.
Table 2.
Summary Table of Regression Analyses a
| SLS Trunk Flexion | SLS Trunk Lateral Flexion | SLS Trunk Rotation | ||||
|---|---|---|---|---|---|---|
| Full Model | Restricted Model |
Full Model | Restricted Model |
Full Model | Restricted Model |
|
| R 2 | 0.167 | 0.095 b | 0.095 | NA | 0.146 | 0.083 b |
| SE estimate | 12.15 | 11.96 | 8.17 | 6.18 | 6.05 | |
| Beta Values | ||||||
| Trunk flexion | 0.152 | — | 0.227 | — | 0.307 b | 0.288 b |
| Trunk rotation | –0.082 | — | –0.107 | — | –0.207 | — |
| Trunk lateral flexion | 0.246 | — | 0.030 | — | –0.032 | — |
| Stride length | 0.126 | — | 0.037 | — | 0.030 | — |
| COM, % | –0.088 | — | 0.191 | — | 0.086 | — |
| Stance knee flexion | –0.028 | — | 0.125 | — | –0.095 | — |
| Stance knee valgus | 0.326 b | 0.308 b | –0.107 | — | 0.148 | — |
a Dashes indicate variable data are not included in the final restricted model. COM, center of mass; NA, not available; SLS, single-leg squat.
b Statistically significant (P < .05).
Discussion
The key findings of this study showed that (1) more trunk flexion in the SLS was associated with more knee valgus at foot contact of the softball pitch and (2) more trunk rotation during the SLS was associated with more trunk flexion at foot contact of the softball pitch (Figures 2 and 3). Both increased trunk rotation and increased trunk flexion during the SLS are typically considered flaws or compensations for those who present with less LPHC strength and stability. Often, youth athletes with LPHC weakness resort to performing the SLS with greater trunk flexion versus knee flexion. 18 Similarly, these athletes with underdeveloped LPHC stability will often rotate toward the free leg. Therefore, both trunk flexion and trunk rotation at peak depth of the SLS are regularly indicative of poor LPHC stability. 18
Figure 2.
Sagittal and transverse view of the SLS at peak depth. (A) Trunk flexion (orange lines) and (B) trunk rotation (orange lines) during the SLS. SLS, single-leg squat.
Figure 3.
(A) Frontal view of the front leg. Orange lines depict knee valgus. (B) Sagittal plane of the trunk. Orange lines depict trunk flexion.
The current study has linked these aforementioned SLS compensations to specific movements during the softball pitch—specifically, increased knee valgus and trunk flexion at foot contact. Increased trunk flexion at foot contact of the windmill softball pitch has been revealed as a trait in younger, less advanced pitchers, compared with older and more elite pitching populations. 26 Oliver et al 34 examined youth pitchers and presented values of trunk flexion much greater than a sample of collegiate pitchers presented by Friesen et al. 11 Contrasting values of trunk flexion display the tendency for younger athletes to rely on more distal kinetic chain segments, excluding the lower extremity, to produce pitch velocity. Specifically, it has been reported that the older, more advanced pitchers demonstrate more efficient segmental sequencing and total utilization of the kinetic chain. 26 Thus, the current findings of those with compensations in both the SLS and during pitching could be a product of poor LPHC control. As a result, the SLS can be theorized as a tool to identify weakness, not only associated with total body strength and stability, but also as a means of identifying pitchers who may be ineffective or inefficient at controlling their body throughout the windmill pitch. Although increased trunk flexion has not been associated with an increased risk of injury, poor position of the COM has been linked to upper-extremity pain. 27 With trunk flexion affecting COM distribution, it can be hypothesized that there may be a link between increased pitch trunk flexion and increased injury risk among softball pitchers. Ideally, pitchers need to create a stable and balanced base around which the distal arm segments can have a secure point from which to rotate.
Similar to increased trunk flexion, increased knee valgus during foot contact of the windmill softball pitch is also thought to be problematic. While the stride foot already makes high-velocity impact with the ground, increased knee valgus can load tissues and structures, again increasing the susceptibility of injury and incidence of pain. 41 Furthermore, lower-extremity injuries are relevant in softball pitching, 14,32 likely due to the large impact the stride foot withstands at foot contact. Reports have shown the stride foot develops ground reaction forces near 140% body weight; 14 therefore, increased knee valgus during stride foot contact is worrisome. While more trunk rotation during the SLS is considered to be a compensatory technique for the less-skilled athletes completing the SLS, increased knee valgus at foot contact of the softball pitch similarly demonstrates inefficient LPHC stability. With these findings, it can be suggested that the SLS can be used as a simple analytic technique to view pitchers’ abilities, especially in terms of LPHC stability throughout a dynamic movement.
The limitations of this study include the laboratory environment. Although asked to pitch at full-effort as in a game setting, the less-intense laboratory environment can hinder true performance level. Another limitation is that pitchers’ prior experience with SLS was not accounted for; however, it can be assumed that many of the pitchers of the same age group and region of the state would have similar training practices. Similarly, SLS peak depth was not instructed or standardized, meaning pitchers may have achieved differing levels of depth that could affect other SLS kinematics and results. It is also important to note that these regression equations did not explain a profound amount of variance within the SLS variables. It can be argued that athletes can isolate training to solely improve SLS performance and not pitch mechanics, but the idea is that as players improve their trunk and core stability, they might also be able to improve their pitch mechanics, namely core stability, upon stride foot contact. Last, the sensor fixation to the skin is potentially susceptible to movement artifact, although every effort was made to properly secure the sensors with tape and adhesive spray.
Conclusion
The present study showed that compensations during the SLS, which were previously related with upper-extremity pain, were associated with pathomechanics during the softball pitch. Therefore, those pitchers who present increased trunk flexion and rotation during the SLS may pose an increased risk of injury throughout the windmill softball pitch and should, therefore, work to develop trunk strength and stability in an effort to minimize risk of injury and improve both SLS and pitch mechanics. The SLS is a simple tool that coaches and parents can use to determine an athlete’s LPHC stability and subsequent risk of softball pitching injury. If a player presents these easily identifiable kinematics during the SLS, more care and core stability training may be given in the attempt to lessen the risk of injury and also improve softball pitching performance.
Footnotes
Final revision submitted August 25, 2020; accepted November 3, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: J.R.D. has received research support from Arthrex, Biomet, DJO, Mitek, and Smith & Nephew; consulting fees from Arthrex, In2Bones, and Theralase; speaking fees from Arthrex; and royalties from Arthrex, In2Bones, and Oakstone Publishing; and has stock/stock options from Theralase and Topical Gear. J.R.A. has received consulting fees from Halyard Health and nonconsulting fees from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Auburn University (protocol No. 18-121 EP 1803).
References
- 1. Barfield J, Anz AW, Andrews J, Oliver GD. Relationship of glove arm kinematics with established pitching kinematic and kinetic variables among youth baseball pitchers. Orthop J Sports Med. 2018;6(7):2325967118784937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Barfield J, Oliver GD. What do we know about youth softball pitching and injury? Sports Medicine Open. 2018;4(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barrentine SW, Fleisig GS, Whiteside JA, Escamilla RF, Andrews JR. Biomechanics of windmill softball pitching with implications about injury mechanisms at the shoulder and elbow. J Orthop Sports Phys Ther. 1998;28(6):405–415. [DOI] [PubMed] [Google Scholar]
- 4. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19(4):404–420. [DOI] [PubMed] [Google Scholar]
- 5. Campbell BM, Stodden DF, Nixon MK. Lower extremity muscle activation during baseball pitching. J Strength Cond Res. 2010;24(4):964–971. [DOI] [PubMed] [Google Scholar]
- 6. Chu SK, Jayabalan P, Kibler WB, Press J. The kinetic chain revisited: new concepts on throwing mechanics and injury. PM R. 2016;8(3_suppl):S69–S77. [DOI] [PubMed] [Google Scholar]
- 7. Claiborne TL, Armstrong A, Gandhi V, Pincivero DM. Relationship between hip and knee strength and knee valgus during a single leg squat. J Appl Biomech. 2006;22(1):41–50. [DOI] [PubMed] [Google Scholar]
- 8. Corben JS, Cerrone SA, Soviero JE, Kwiecien SY, Nicholas SJ, McHugh MP. Performance demands in softball pitching: a comprehensive muscle fatigue study. Am J Sports Med. 2015;43(8):2035–2041. [DOI] [PubMed] [Google Scholar]
- 9. Downs J, Friesen K, Anz AW, Dugas JR, Andrews J, Oliver GD. Effects of a simulated game on pitching kinematics in youth softball pitcher. Int J Sports Med. 2020;41(3):189–195. [DOI] [PubMed] [Google Scholar]
- 10. Feeley BT, Schisel J, Agel J. Pitch counts in youth baseball and softball: a historical review. Clin J Sport Med. 2018;28(4):401–405. [DOI] [PubMed] [Google Scholar]
- 11. Friesen KB, Barfield JW, Murrah WM, Dugas JR, Andrews JR, Oliver GD. The association of upper-body kinematics and earned run average of national collegiate athletic association division I softball pitchers. J Strength Cond Res. Published online July 22, 2019. doi:10.1519/JSC.0000000000003287 [DOI] [PubMed] [Google Scholar]
- 12. Gilmer GG, Gascon SS, Oliver GD. Classification of lumbopelvic-hip complex instability on kinematics amongst female team handball athletes. J Sci Med Sport. 2018;21(8):805–810. [DOI] [PubMed] [Google Scholar]
- 13. Graci V, Salsich GB. Trunk and lower extremity segment kinematics and their relationship to pain following movement instruction during a single-leg squat in females with dynamic knee valgus and patellofemoral pain. J Sci Med Sport. 2015;18(3):343–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Guido JA, Jr, Werner SL, Meister K. Lower-extremity ground reaction forces in youth windmill softball pitchers. J Strength Cond Res. 2009;23(6):1873–1876. [DOI] [PubMed] [Google Scholar]
- 15. Huang YH, Wu TY, Learman KE, Tsai YS. A comparison of throwing kinematics between youth baseball players with and without a history of medial elbow pain. Chin J Physiol. 2010;53(3):160–166. [DOI] [PubMed] [Google Scholar]
- 16. Keeley DW, McClary MA, Anguiano-Molina G, Oliver GD, Dougherty C, Torry MR. Reliability of an electromagnetic tracking system in describing pitching mechanics. Sports Technology. 2015;8:112–117. [Google Scholar]
- 17. Kibler WB. Biomechanical analysis of the shoulder during tennis activities. Clin Sports Med. 1995;14(1):79–85. [PubMed] [Google Scholar]
- 18. Kibler WB, Press J, Sciascia A. The role of core stability in athletic function. Sports Med. 2006;36(3):189–198. [DOI] [PubMed] [Google Scholar]
- 19. Kibler WB, Wilkes T, Sciascia A. Mechanics and pathomechanics in the overhead athlete. Clin Sports Med. 2013;32(4):637–651. [DOI] [PubMed] [Google Scholar]
- 20. Laudner KG, Wong R, Latal JR, Meister K. Descriptive profile of lumbopelvic control in collegiate baseball pitchers. J Strength Cond Res. 2018;32(4):1150–1154. [DOI] [PubMed] [Google Scholar]
- 21. Laudner KG, Wong R, Meister K. The influence of lumbopelvic control on shoulder and elbow kinetics in elite baseball pitchers. J Shoulder Elbow Surg. 2019;28(2):330–334. [DOI] [PubMed] [Google Scholar]
- 22. Lear A, Patel N. Softball pitching and injury. Curr Sports Med Rep. 2016;15(5):336–341. [DOI] [PubMed] [Google Scholar]
- 23. Naito K, Takagi T, Kubota H, Maruyama T. Multi-body dynamic coupling mechanism for generating throwing arm velocity during baseball pitching. Hum Mov Sci. 2017;54:363–376. [DOI] [PubMed] [Google Scholar]
- 24. Nakagawa TH, Moriya ÉTU, Maciel CD, Serrão FV. Test-retest reliability of three-dimensional kinematics using an electromagnetic tracking system during single-leg squat and stepping maneuver. Gait Posture. 2014;39(1):141–146. [DOI] [PubMed] [Google Scholar]
- 25. Oliver GD. Relationship between gluteal muscle activation and upper extremity kinematics and kinetics in softball position players. Med Biol Eng Comput. 2014;52(3):265–270. [DOI] [PubMed] [Google Scholar]
- 26. Oliver GD, Dwelly PM, Kwon YH. Kinematic motion of the windmill softball pitch in prepubescent and pubescent girls. J Strength Cond Res. 2010;24(9):2400–2407. [DOI] [PubMed] [Google Scholar]
- 27. Oliver GD, Friesen K, Barfield J, et al. Association of upper extremity pain with softball pitching kinematics and kinetics. Orthop J Sports Med. 2019;7(8):2325967119865171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Oliver GD, Gilmer G, Anz AW, et al. Upper extremity pain and pitching mechanics in NCAA Division I softball. Int J Sports Med. 2018;39:929–935. [DOI] [PubMed] [Google Scholar]
- 29. Oliver GD, Gilmer G, Friesen K, Plummer H, Anz AW, Andrews J. Functional differences in softball pitchers with and without upper extremity pain. J Sci Med Sport. 2019;22:1079–1083. [DOI] [PubMed] [Google Scholar]
- 30. Oliver GD, Keeley DW. Gluteal muscle group activation and its relationship with pelvis and torso kinematics in high-school baseball pitchers. J Strength Cond Res. 2010;24(11):3015–3022. [DOI] [PubMed] [Google Scholar]
- 31. Oliver GD, Keeley DW. Pelvis and torso kinematics and their relationship to shoulder kinematics in high-school baseball pitchers. J Strength Cond Res. 2010;24(12):3241–3246. [DOI] [PubMed] [Google Scholar]
- 32. Oliver GD, Plummer H. Ground reaction forces, kinematics, and muscle activations during the windmill softball pitch. J Sports Sci. 2011;29(10):1071–1077. [DOI] [PubMed] [Google Scholar]
- 33. Oliver GD, Plummer H, Brambeck A. Hip and glenohumeral passive range of motion in collegiate softball players. Int J Sports Phys Ther. 2016;11(5):738–745. [PMC free article] [PubMed] [Google Scholar]
- 34. Oliver GD, Plummer H, Washington JK, Saper M, Dugas JR, Andrews JR. Pitching mechanics in female youth fastpitch softball. Int J Sports Phys Ther. 2018;13(3):493–500. [PMC free article] [PubMed] [Google Scholar]
- 35. Oliver GD, Plummer HA, Keeley DW. Muscle activation patterns of the upper and lower extremity during the windmill softball pitch. J Strength Cond Res. 2011;25(6):1653–1658. [DOI] [PubMed] [Google Scholar]
- 36. Oliver GD, Washington JK, Friesen KB, Anz AW, Dugas JR, Andrews JR. The effects of a pre-throwing program on collegiate NCAA Division I softball pitchers’ biomechanical measures of hip and shoulder range of motion. J Orthop Res Ther. 2018;2018(2). [Google Scholar]
- 37. Oliver GD, Washington JK, Gascon S, Plummer H, Escamilla RF, Andrews J. Effects of hip abduction fatigue on trunk and shoulder kinematics during throwing and passive hip rotational range of motion. J Sport Rehabil. 2019;28(4):304–310. [DOI] [PubMed] [Google Scholar]
- 38. Oliver GD, Weimar WH, Plummer HA. Gluteus medius and scapula muscle activations in youth baseball pitchers. J Strength Cond Res. 2015;29(6):1494–1499. [DOI] [PubMed] [Google Scholar]
- 39. Plummer H, Oliver GD. The relationship between gluteal muscle activation and throwing kinematics in baseball and softball catchers. J Strength Cond Res. 2014;28(1):87–96. [DOI] [PubMed] [Google Scholar]
- 40. Plummer H, Oliver GD, Powers CM, Michener LA. Trunk lean during a single-leg squat is associated with trunk lean during pitching. Int J Sports Phys Ther. 2018;13:58–65. [PMC free article] [PubMed] [Google Scholar]
- 41. Powers C. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33(11):639–646. [DOI] [PubMed] [Google Scholar]
- 42. Rojas IL, Provencher MT, Bhatia S, et al. Biceps activity during windmill softball pitching: injury implications and comparison with overhand throwing. Am J Sports Med. 2009;37(3):558–565. [DOI] [PubMed] [Google Scholar]
- 43. Sauers EL, Dykstra DL, Bay RC, Bliven KH, Snyder AR. Upper extremity injury history, current pain rating, and health-related quality of life in female softball pitchers. J Sport Rehabil. 2011;20(1):100–114. [DOI] [PubMed] [Google Scholar]
- 44. Sciascia A, Cromwell R. Kinetic chain rehabilitation: a theoretical framework. Rehabil Res Pract. 2012;2012:853037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sciascia A, Monaco M. When is the patient truly “ready to return,” a.k.a. kinetic chain homeostasis. In: Kelly JD IV, ed. Elite Techniques in Shoulder Arthroscopy. Springer International Publishing Switzerland; 2016:317–327. [Google Scholar]
- 46. Skillington SA, Brophy RH, Wright RW, Smith MV. Effect of pitching consecutive days in youth fast-pitch softball tournaments on objective shoulder strength and subjective shoulder symptoms. Am J Sports Med. 2017;45(6):1413–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Stickler L, Finley M, Gulgin H. Relationship between hip and core strength and frontal plane alignment during a single leg squat. Phys Ther Sport. 2015;16(1):66–71. [DOI] [PubMed] [Google Scholar]
- 48. Veeger HE. The position of the rotation center of the glenohumeral joint. J Biomech. 2000;33(12):1711–1715. [DOI] [PubMed] [Google Scholar]
- 49. Washington JK, Gilmer G, Oliver GD. Acute hip abduction fatigue on lumbopelvic-hip complex stability in softball players. Int J Sports Med. 2018;39(7):571–575. [DOI] [PubMed] [Google Scholar]
- 50. Wasserberger K, Barfield J, Anz AW, Andrews J, Oliver GD. Using the single leg squat as an assessment of stride leg knee mechanics in adolescent baseball pitchers. J Sci Med Sport. 2019;22:1254–1259. [DOI] [PubMed] [Google Scholar]
- 51. Werner SL, Guido JA, McNeice RP, Richardson JL, Delude NA, Stewart GW. Biomechanics of youth windmill softball pitching. Am J Sports Med. 2005;33(4):552–560. [DOI] [PubMed] [Google Scholar]
- 52. Werner SL, Jones DG, Guido JA, Jr, Brunet ME. Kinematics and kinetics of elite windmill softball pitching. Am J Sports Med. 2006;34(4):597–603. [DOI] [PubMed] [Google Scholar]
- 53. Wu G, Siegler S, Allard P, et al. ISB recommendation on definitions of joint coordinate system of various joints for reporting of human joint motion---part I: ankle, hip, and spine. J Biomech. 2002;35(4):543–548. [DOI] [PubMed] [Google Scholar]
- 54. Wu G, van der Helm FCT, Veeger HEJ, et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion—Part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38(5):981–992. [DOI] [PubMed] [Google Scholar]




