Abstract
Background:
Combined anterior cruciate ligament (ACL) reconstruction (ACLR) and anterolateral ligament reconstruction (ALLR) are performed with the intention to restore native knee kinematics after ACL tears. There continue to be varying results as to the difference in kinematics between combined and isolated procedures, including anterior tibial translation (ATT) and internal tibial rotation (IR).
Purpose:
To perform a systematic review and meta-analysis to evaluate the kinematic changes of a combined ACLR/ALLR versus isolated ACLR and to assess the effects of different fixation techniques.
Study Design:
Systematic review.
Methods:
We conducted a systematic review and meta-analysis of 15 human cadaveric biomechanical studies evaluating combined ACLR/ALLR versus isolated ACLR and their effects on ATT and IR in 149 specimens. The primary outcomes were ATT and IR. Secondary outcomes included graft type and size as well as fixation methods such as type, angle, tension, and position of fixation. Meta-regression was used to examine the effect of various cofactors on the resulting measures.
Results:
Compared with isolated ACLR, combined ACLR/ALLR decreased ATT and IR by 0.01 mm (95% CI, –0.059 to 0.079 mm; P = .777) and 1.64° (95% CI, 1.30°-1.98°; P < .001), respectively. Regarding ACLR/ALLR, increasing the knee flexion angle and applied IR force led to a significant reduction in IR (P < .001 and P = .044, respectively). There was also a significant reduction in IR in combined procedures with semitendinosus ALL graft, higher flexion fixation angles, and tension but no change in IR with differing femoral fixation points (P < .001, P < .001, and P = .268, respectively). Multivariate meta-regression showed that the use of tibial-sided suture anchor fixation significantly reduced IR (P < .001).
Conclusion:
These results suggest that a combined ACLR/ALLR procedure significantly decreases IR compared with isolated ACLR, especially at higher knee flexion angles. Semitendinosus ALL graft, fixation at higher knee flexion, increased tensioning, and tibial-sided interference screw fixation in ALLR may help to further reduce IR.
Keywords: anterolateral ligament reconstruction, biomechanics, kinematics, knee
In 1879, Paul Segond initially described a pathognomonic anterolateral tibial avulsion fracture associated with anterior cruciate ligament (ACL) tears. 2,35 Since then, multiple studies 1,22,35,37 have described an anterolateral ligament (ALL) with varying terminology and anatomic findings. Histologically, the ALL has been noted as compact collagen fibers in parallel orientation consistent with a ligamentous and tendinous structure. 39 In subsequent studies, 9–10,19,21,26,27,36,38 the ALL has been described as a distinct ligament of the knee that functions to provide rotational support to the knee and has injury rates upward of 90% in the setting of concomitant ACL injury.
For many years, anterolateral extra-articular procedures were performed in isolation and in combination with ACL reconstruction (ACLR) to help restore joint kinematics and decrease failure rates. These procedures fell out of favor due to concerns regarding knee overconstraint and the potential development of osteoarthritis. The topic has since returned to the spotlight in an attempt to restore joint kinematics, decrease ACL graft stresses, and ultimately lower rates of ACL graft failure. 7,8 Sonnery-Cottet et al 32 reported a 2.5-times lower ACL graft failure rate in the setting of young athletes participating in pivoting sports when ALL reconstruction (ALLR) was combined with ACLR. They also noted greater odds of returning to preinjury level of sports with a combined technique.
Although there have been clinical studies 5,7,8,17,29,32 that support combined reconstruction, there are biomechanical studies that do and do not recommend a combined approach. 11,15,16,23,29,30 The purpose of this study was to perform a systematic review and meta-analysis of biomechanical data to evaluate the kinematic changes of a combined ACLR/ALLR compared with isolated ACLR as well as to assess the effects of different fixation techniques.
Methods
Article Screening
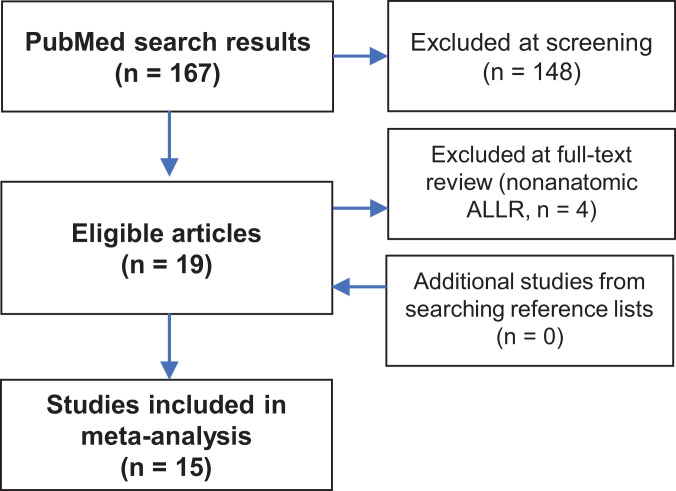
We searched the PubMed database on June 11, 2020, for articles evaluating the knee kinematics of isolated ACLR versus combined ACLR/ALLR in a biomechanical model with anterior tibial translation (ATT) and internal tibial rotation (IR) as the primary outcomes. The search field entered was as follows: (Anterolateral[All Fields] OR ALL[All Fields] OR ALLR[All Fields]) AND (ACL[All Fields] OR Anterior Cruciate[All Fields]) AND Biomechanical[All Fields]. Two authors (S.R.K. and B.M.C.) independently screened the resulting 167 articles for inclusion or exclusion using Abstrackr software (Brown University). Disagreements were reviewed by both reviewers, who discussed them and together made the final decision whether to include or exclude the references. Inclusion criteria were biomechanical studies of isolated ACLR versus combined ACLR/ALLR on human cadavers that reported mean ATT and IR with standard deviation and sample size. The 2 reviewers agreed on inclusion of 15 articles and added 4 additional articles during conflict resolution creating a total of 19 articles for full-text review.
Full-text review eliminated 4 additional articles (each included lateral extra-articular tenodesis of the iliotibial [IT] band rather than ALLR). The reference sections of the remaining articles were screened for additional studies, but none met inclusion criteria, leaving 15 studies to be evaluated (Figure 1). § These articles were then evaluated for quality using the Quality Appraisal for Cadaveric Studies scale, which is a validated means for assessing the quality of cadaveric studies. 41
Figure 1.
Flowchart showing the screening process for included studies. ALLR, anterolateral ligament reconstruction.
Data Collection
Data were collected from each included study for sample size, force applied during testing, mean ATT, mean IR, graft type and size used, implants used for fixation of ACLR and ALLR on both femur and tibia, fixation angle of ALLR, graft fixation tension of ACLR/ALLR, and femoral position of ALLR fixation (anterior or posterior to lateral epicondyle of fibular collateral ligament [FCL] insertion).
Included Studies
The 15 included studies (Table 1) represented 149 specimens (mean age at death, 60.2 years). Each study had a variety of protocols under which specimens were treated, and each of these specimen groups were subsequently tested for its effects on ATT and/or IR. Six studies were performed using a robotic system, while the others used custom devices. The manner in which the anterolateral defect was performed differed between studies. Seven studies were performed using a detailed dissection followed by sectioning of the ALL and Kaplan fibers. Eight studies performed an isolated sectioning of the ALL or anterolateral capsule. Anterior and IR forces varied between studies, ranging from 88 N to 134 N anterior-directed forces versus 5 to 8 N·m IR forces. The studies also varied in the number of flexion/fixation angles and fixation tensions tested (Table 2). Data regarding other ALLR procedures were excluded.
TABLE 1.
Characteristics of Included Studies a
| Lead Author | Year of Publication | Total Sample Size | Number of Cohorts or Protocols | Mean Age of Cadavers (y) | QUACS Scale b |
|---|---|---|---|---|---|
| Nitri 24 | 2016 | 10 | 9 | 49.3 | 85 |
| Schon 29 | 2016 | 10 | 63 | 55.9 | 92 |
| Tavlo 35 | 2016 | 18 | 4 | 77.8 | 77 |
| Inderhaug 15 | 2017 | 12 | 20 | 57 | 92 |
| Inderhaug 16 | 2017 | 12 | 30 | 49 | 92 |
| Guenther 12 | 2017 | 7 | 3 | 53.7 | 84 |
| Noyes 25 | 2017 | 7 | 3 | 57 | 85 |
| Geeslin 11 | 2018 | 9 | 28 | 56 | 85 |
| Nielson 23 | 2018 | 8 | 1 | NR | 85 |
| Jette 17 | 2019 | 12 | 4 | 70 | 85 |
| Smith 30 | 2019 | 12 | 3 | 35.8 | 85 |
| Katakura 18 | 2019 | 12 | 1 | 74.5 | 85 |
| Delaloye 5 | 2020 | 6 | 7 | 65.2 | 92 |
| Yasuma 43 | 2020 | 6 | 1 | 79.5 | 92 |
| Trentacosta 37 | 2020 | 8 | 4 | 62.6 | 85 |
a NR, not reported; QUACS, Quality Appraisal for Cadaveric Studies.
b Scored on a scale of 0 to 100, with higher scores correlating with higher study quality.
TABLE 2.
Study Protocols of Included Studies a
| Lead Author | ALLR Site Femur | ALLR Femoral/Tibial Fixation Method | Graft Type, ACLR/ALLR | ALLR Knee Fixation Angle, deg | ALLR Fixation Tension, N | Tested Knee Flexion Angle, deg | ATT/IR Forces, N/N·m |
|---|---|---|---|---|---|---|---|
| Nitri 24 | P | IS/IS | BTB/ST | 75 | 88 | 0, 15, 30, 45, 60, 75, 90, 105, 120 | 88/5 |
| Schon 29 | P | IS/CL | BTB/ST | 0, 15, 30, 45, 60, 75, 90 | 88 | 0, 15, 30, 45, 60, 75, 90, 105, 120 | 88/5 |
| Tavlo 35 | A | CL/CL | Synthetic/EHL | 30 | 50 | 0, 30, 60, 90 | NR/8.85 |
| Inderhaug 15 | P | IS/SA | BTB/gracilis | 20 | 20, 40 | 0, 10, 20, 30, 40, 50, 60, 70, 80, 90 | 90/5 |
| Inderhaug 16 | P | IS/IS | BTB/gracilis | 0, 30, 60 | 20 | 0, 10, 20, 30, 40, 50, 60, 70, 80, 90 | 90/5 |
| Guenther 12 | P | IS/IS | Quad/gracilis | 30 | 10 | 30, 60, 90 | 134/7 |
| Noyes 25 | P | SA/IS | BTB/gracilis | 60 | 8.9 | 25, 60, 90 | 100/5 |
| Trentacosta 37 | P | SA/SA | ST/TP | 0 | NR | 0, 30, 60, 90 | 100/5 |
| Geeslin 11 | P | CL/IS | BTB/ST | 30, 70 | 20, 40 | 0, 15, 30, 45, 60, 75, 90 | 88/5 |
| Nielsen 23 | P | IS/IS | Quad/gracilis | 20 | NR | NR | NR/NR |
| Jette 17 | P | IS/IS | BTB/gracilis | 0 | NR | 0, 30, 60, 90 | 90/7 |
| Smith 30 | P | SP/SP | NR/NR | 0 | NR | 0, 30, 90 | 100/5 |
| Delaloye 5 | P | BT/IS | ST/gracilis | 0 | 20 | 0, 15, 30, 45, 60, 75, 90 | 134/5 |
| Yasuma 43 | P | IS/IS | ST/gracilis | 30 | NR | 30 | NR/no IR |
| Katakura 18 | A/P | SA/SA | ST/synthetic | 20, 70 | 20 | 30 | NR/no IR |
a A, anterior to FCL attachment; ACLR, anterior cruciate ligament reconstruction; ALLR, anterolateral ligament reconstruction; ATT, anterior tibial translation; BT, bone tunnel; BTB, bone-tendon-bone; CL, clamp; EHL, extensor hallucis longus; FCL, fibular collateral ligament; IR, internal tibial rotation; IS, interference screw; No IR, no internal rotation measurements performed; NR, not reported; P, proximal to FCL attachment; Quad, quadriceps; SA, suture anchor; SP, suture post; ST, semitendinosus; TP, tibialis posterior.
Statistical Analysis
Random-effects meta-analysis was performed with OpenMeta[Analyst] (Brown University). Each group then underwent univariate metaregression to determine the effect of covariates including knee flexion angle, ATT/IR force, ACL graft type/size/fixation method, ALL graft type/size/fixation location/fixation method/fixation tension and knee flexion angle at ALL fixation on ATT and IR. Subsequent multivariate metaregression was performed to account for the differences in variables previously studied and to show their effect on ATT and IR. Statistical significance was set at P < .05.
Results
Anterior Translation
The results of the meta-analysis indicated that under a mean force of 91 N, ATT decreased by an overall mean of 0.01 mm (95% CI, –0.059 to 0.079 mm; P = .777) in combined ACLR/ALLR compared with isolated ACLR.
Univariate meta-regression showed that with an increased anterior force applied to the knee or an increased ACL tension at fixation, there was a larger reduction in ATT in ACLR/ALLR versus ACLR (P = .015 and .033, respectively). For combined ACLR/ALLR, the use of a bone-tendon-bone (BTB) ACL graft compared with hamstring or quadriceps tendon ACL graft resulted in a smaller reduction in ATT (P = .006; Table 3). Under multivariate meta-regression, only graft type showed continued effect, with a lower mean decrease of 0.547 mm (95% CI, 0.165-0.987 mm), of ATT for BTB ACL graft versus hamstring and quadriceps tendon ACL grafts (P = .028).
TABLE 3.
Results of Univariate Analysis for Factors Affecting Anterior Tibial Translation a
| Comparison by Variable | Difference in Anterior Tibial Translation, Mean (95% CI) | P |
|---|---|---|
| Knee flexion angle | –0.001 (–0.003 to 0.001) mm/deg | .530 |
| Anterior force applied | 0.008 (0.002 to 0.014) mm/N | .015 |
| ACL graft type (BTB graft vs hamstring or quadriceps graft) | –0.576 (–1.036 to –0.058) mm | .006 |
| ACL graft diameter | –0.172 (–0.391 to 0.047) mm/mm diameter | .124 |
| ACL femoral fixation type (Interference screw vs suspensory or suture-post) | –0.424 (–0.723 to –0.125) mm | .005 |
| ACL tibial fixation type (suspensory fixation vs interference screw) | –0.100 (–0.458 to 0.257) mm | .582 |
| ACL fixation angle | 0.009 (–0.004 to 0.022) mm/deg | .168 |
| ACL fixation tension | 0.014 (0.001 to 0.026) mm/N | .033 |
| ALL graft diameter | –2.454 (–8.132 to 3.225) mm/mm diameter | .397 |
| ALL femoral fixation type (suture-post fixation vs interference screw) | 0.228 (–0.195 to 0.650) mm | .291 |
| ALL tibial fixation type (suture-post vs interference screw) | 0.212 (–0.212 to 0.635) mm | .328 |
| ALL fixation angle | –0.002 (–0.004 to 0.001) mm/deg | .145 |
| ALL fixation tension | –0.002 (–0.005 to 0.000) mm/N | .095 |
| ALL femoral fixation location (anterior FCL/LE vs posterior FCL/LE) | 0.110 (–0.314 to 0.534) mm | .611 |
a Bolded P values indicate statistical significance. ACL, anterior cruciate ligament; ALL, anterolateral ligament; BTB, bone-tendon-bone; FCL/LE, fibular collateral ligament/lateral epicondyle.
Internal Rotation
With regard to IR, meta-analysis showed that under a mean IR torque of 6 N·m, there was a mean overall decrease in IR of 1.64° (95% CI, 1.30°-1.98°; P < .001) in combined ACLR/ALLR compared with isolated ACLR.
Univariate metaregression showed with increased knee flexion angle, increased IR force, and increased ALLR graft fixation tension that there was a statistically significant reduction in IR with the addition of an ALLR (P < .001, P = .044, P < .001, respectively). There was also a statistically significant reduction in IR when a semitendinosus ALLR graft was used versus gracilis or tibialis posterior as well as with ALLR tibial suture anchor fixation versus interference screw fixation (P < .001, P < .001, respectively). There was no statistically significant change in IR based upon ALL femoral fixation location (P = .268) (Table 4).
TABLE 4.
Results of Univariate Analysis for Factors Affecting Internal Rotation
| Comparison by Variable | Difference in Internal Rotation, Mean (95% CI) | P |
|---|---|---|
| Knee flexion angle | 0.02 (0.01 to 0.03) deg | <.001 |
| Internal rotation force applied | 0.58 (0.015 to 1.147) deg/N·m | .044 |
| ACL graft type (BTB graft vs hamstring or quadriceps graft) | 0.001 (–1.292 to 1.294) mm | .999 |
| ACL graft diameter | –0.301 (–1.116 to 0.514) mm/mm diameter | .469 |
| ACL femoral fixation (interference screw vs suspensory or suture-post) | –0.066 (–1.052 to 0.920) mm | .896 |
| ACL tibial fixation (suspensory vs interference screw) | –2.12 (–3.99 to –0.255) deg | .026 |
| ACL fixation angle | –0.003 (–0.038 to 0.031) mm/deg | .850 |
| ACL fixation tension | 0.115 (0.079 to 0.150) deg/N | <.001 |
| ALL graft type (semitendinosus vs gracilis or tibialis posterior) | 2.65 (2.02 to 3.28) deg | <.001 |
| ALL femoral fixation (suture anchor vs interference screw) | 0.026 (–1.347 to 1.398) deg | .971 |
| ALL tibial fixation (suture anchor vs interference screw) | –3.16 (–3.60 to –2.71) deg | <.001 |
| ALL fixation angle | 0.023 (0.011 to 0.036) deg/deg flexion | <.001 |
| ALL fixation tension | 0.021 (0.011 to 0.032) deg/N | <.001 |
| ALL femoral fixation location (anterior FCL/LE vs posterior FCL/LE) | –1.062 (–2.940 to 0.816) mm | .268 |
a Bolded P values indicate statistical significance. ACL, anterior cruciate ligament; ALL, anterolateral ligament; BTB, bone-tendon-bone; FCL/LE, fibular collateral ligament/lateral epicondyle.
Multivariate analysis showed that only implant type on the tibial side of the ALLR resulted in statistically significant differences with the use of a suture anchor, leading to a smaller reduction in IR difference by 2.49° (95% CI, 1.86°-3.11°) as compared with the use of an interference screw (P < .001).
Discussion
The 15 high-quality biomechanical studies that we included in our review determined that combined ACLR/ALLR decreased IR compared with isolated ACLR, while there was no statistically significant effect on ATT. The resultant decrease in IR was more pronounced at increased knee flexion angle and with increased rotational forces applied to the knee. We also noted that use of a semitendinosus ALL graft, fixation at higher flexion angles, and fixation with increased tension have a significant effect on the mean difference of IR in univariate analysis. These are important aspects to understand when treating patients with ACL injuries that help to better define potential surgical indications and techniques for a combined reconstructive approach. 24,34
In our review, combined ACLR/ALLR had a stronger effect on decreasing IR compared with ATT. With a mean IR torque of 6 N·m, we saw a decrease in IR of 1.64° with the addition of an ALLR. Whether this is clinically significant remains to be determined, although many previous studies have shown the importance of the ALL in regard to IR. These results are in line with Parsons et al, 26 who performed a cadaveric biomechanical study and demonstrated that the ALL was an important stabilizer for IR at flexion angles >35° but had less impact upon ATT at all flexion angles. They found the ALL to contribute 30% to 45% of the restraint with a 5-N·m IR force at 35° to 90° yet only a 5% contribution near full extension. Rasmussen et al 27 showed that when the ALL was sectioned, there was an increase in IR by 2.8° with a simulated pivot shift. Other studies 16,24,25,29 have shown that with isolated ACLR, there is a residual 2° to 6° of IR. Ruiz et al 28 evaluated the role of combined sectioning of the ACL/ALL and showed that the addition of a sectioned ALL with a previously sectioned ACL increased IR by 2.4°. Although there is no consensus on the residual IR threshold warranting an ALLR, it may be of benefit in individuals with hyperlaxity or high-grade preoperative pivot shift or those participating in high-level pivoting sports. 24,34
When evaluating the proper graft type, there is no clear consensus on which graft to use in combined reconstruction. In our study, we showed an increased difference in mean IR when a semitendinosus graft is used for ALLR versus gracilis or tibialis posterior tendon graft. Other studies 13,30,40 have suggested the use of numerus grafts including gracilis, semitendinosus, or even minimally invasive synthetic grafts. A study by Wytrykowski et al 42 showed the stiffness and highest maximum load to failure of the ALL to be 21 N/mm and 141 N, respectively. In the same study, they demonstrated that a gracilis graft has a higher stiffness and maximum load while the IT band more closely resembles the ALL.
There is also no consensus on the proper ALL fixation angle or tension. We noted in our study that when the ALL graft in combined procedures was fixed at higher knee flexion angles and under higher tensions, IR was further decreased than with isolated procedures, even though this did not remain significant in multivariate analysis. Multiple studies 1,24,31,33,44 have recommended different fixation angles, including full extension, 30°, 70°, 75°, and 90°. Schon et al 29 looked at 7 different graft fixation angles from 0° to 90° with 88 N of tension and found that there was no difference in knee kinematics based on fixation angle, but they did note overconstraint at all fixation angles. Geeslin et al 11 also noted overconstraint at differing fixation angles, even with lower graft tensions of 20 N and 40 N, which is in contrast to multiple studies 5,15,16,23,30 that showed no overconstraint at lower fixation tensions. Although the clinical relevance of overconstraint remains to be determined, a way to prevent it may be to perform ALLR at lower fixation angles and tensions.
With regard to ALL fixation type, there are few studies that specifically report on fixation methods. We noted that the use of a tibial interference screw had a greater effect on reducing IR compared with suture anchor fixation. A porcine study 3 also showed that interference screw fixation through 1 tibial tunnel had a higher load to failure compared with suture anchors.
Over the years, graft location has also been a topic of interest. Many of the reconstructive techniques are based on early ALL anatomic papers. 1,6,19 Although there is less variation in proposed tibial-sided graft position between the fibular head and the Gerdy tubercle, there has been debate regarding the femoral graft position site and whether to place it anteriorly or posteriorly to the lateral epicondyle or FCL insertion point. 4,14,18,20 Our study showed no significant difference in ATT or IR when comparing an anterior or posterior femoral graft placement in relation to the FCL or lateral epicondyle.
There are several limitations of this study. It includes a small number of heterogeneous studies available for inclusion. We included only studies that included comparisons of isolated ACLR versus combined ACLR/ALLR and did not look at studies or portions of included studies that focused on lateral extra-articular tenodesis procedures. It must also be noted that we did not compare the difference of placing the ALL graft superficial or deep to the FCL as is emphasized in lateral extra-articular tenodesis procedures. A majority of studies did not specify their technique in terms of graft placement above or below the FCL. There was a noted difference in how the anterolateral defect was created with several studies sectioning both the ALL and Kaplan fibers versus only performing a sectioning of the isolated ALL or anterolateral capsule. It has been previously reported that the deep IT band may play a larger role in controlling IR and that an anterolateral defect model that does not include the deep IT band may not adequately represent an anterolateral injury. 25,30 The included studies also showed heterogenicity in testing protocols, including flexion angles and fixation techniques, and thus, meta-regression was performed to account for these differences and to determine whether they have any effect upon ATT or IR. It must also be noted that we neither compared the effect of combined versus isolated procedures on the full kinematics of the pivot shift, which is a common indication for performing a combined procedure, nor did we include studies evaluating the changes in ACL graft forces after ALLR. Each of these studies were cadaveric studies that can be interpreted only at time zero and do not take into consideration the tissue regeneration and rehabilitation that take place after in vivo surgery. It was also noted that the cadavers used had a mean age much older than the young, active population in which we typically see a higher rate of ACL tears. We were not able to deduce any development of osteoarthritis, graft failure rates, or clinical parameters due to the nature of the cadaveric studies. Another limitation is that we did not compare kinematic results of combined ACLR/ALLR or isolated ACLR to the intact knee and did not specifically evaluate overconstraint after each procedure. Ultimately, although we did see statistical significance from a biomechanical model, we cannot determine if it is truly clinically significant.
Conclusion
This systematic review and meta-analysis of 15 high-quality biomechanical cadaveric studies showed decrease in IR of 1.6° with combined ACLR/ALLR versus isolated ACLR. Semitendinosus ALL graft, fixation at higher knee flexion, increased tensioning, and tibial-sided interference screw fixation in ALLR may help to further reduce IR laxity compared with an isolated ACLR.
Footnotes
Final revision submitted November 4, 2020; accepted December 16, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: E.G.H. has received research support Arthrex and Sequoia Medical, consulting fees from DePuy, educational payments from Smith & Nephew, and hospitality payments from Wright Medical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223(4):321–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Campos JC, Chung CB, Lektrakul, et al. Pathogenesis of the Segond fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology. 2001;219(2):381–386. [DOI] [PubMed] [Google Scholar]
- 3. Costa RN, Nadal RR, Saggin PRF, Lopes Junior OV, Spinelli LF, Israel CL. Biomechanical evaluation of different tibial fixation methods in the reconstruction of the anterolateral ligament in swine bones. Rev Bras Ortop. 2019;54:183–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Daggett M, Ockuly AC, Cullen M, et al. Femoral origin of the anterolateral ligament: an anatomic analysis. Arthroscopy. 2016;32(5):835–841. [DOI] [PubMed] [Google Scholar]
- 5. Delaloye J, Hartog C, Blatter S, et al. Anterolateral ligament reconstruction and modified lemaire lateral extra-articular tenodesis improve stability after anterior cruciate ligament reconstruction: a biomechanical study. Arthroscopy. 2020;36(7):1942–1950. [DOI] [PubMed] [Google Scholar]
- 6. Dodds AL, Halewood C, Gupte CM, Williams A, Amis AA. The anterolateral ligament: anatomy, length changes and association with the Segond fracture. Bone Joint J. 2014;96-B(3):325–331. [DOI] [PubMed] [Google Scholar]
- 7. Duthon VB, Magnussen RA, Servien E, et al. ACL reconstruction and extra-articular tenodesis. Clin Sports Med. 2013;32:141–153. [DOI] [PubMed] [Google Scholar]
- 8. Engebretsen L, Lew WD, Lewis JL, Hunter RE. The effect of an iliotibial tenodesis on intraarticular graft forces and knee joint motion. Am J Sports Med. 1990;18(2):169–176. [DOI] [PubMed] [Google Scholar]
- 9. Ferretti A, Monaco E, Ponzo A, et al. Combined intra-articular and extra-articular reconstruction in anterior cruciate ligament-deficient knee: 25 years later. Arthroscopy. 2016;32(10):2039–2047. [DOI] [PubMed] [Google Scholar]
- 10. Ferretti A, Monaco E, Fabbri M, Maestri B, De Carli A. Prevalence and classification of injuries of anterolateral complex in acute anterior cruciate ligament tears. Arthroscopy. 2017;33(1):147–154. [DOI] [PubMed] [Google Scholar]
- 11. Geeslin AG, Moatshe G, Chala J, et al. Anterolateral knee extra-articular stabilizers: a robotic study comparing anterolateral ligament reconstruction and modified Lemaire lateral extra-articular tenodesis. Am J Sports Med. 2018;46(3):607–616. [DOI] [PubMed] [Google Scholar]
- 12. Guenther D, Irarrázaval S, Bell KM, et al. The role of extra-articular tenodesis in combined ACL and anterolateral capsular injury. J Bone Joint Surg Am. 2017;99(19):1654–1660. [DOI] [PubMed] [Google Scholar]
- 13. Helito CP, Bonadio MB, Gobbi RG, et al. Combined intra- and extra-articular reconstruction of the anterior cruciate ligament: the reconstruction of the knee anterolateral ligament. Arthrosc Tech. 2015;4(3):e239–e244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Imbert P, Lutz C, Dagget M, et al. Isometric characteristics of the anterolateral ligament of the knee: a cadaveric navigation study. Arthroscopy. 2016;32(10):2017–2024. [DOI] [PubMed] [Google Scholar]
- 15. Inderhaug E, Stephen JM, Williams A, Amis AA. Anterolateral tenodesis or anterolateral ligament complex reconstruction: effect of flexion angle at graft fixation when combined with ACL reconstruction. Am J Sports Med. 2017;45(13):3089–3097. [DOI] [PubMed] [Google Scholar]
- 16. Inderhaug E, Stephen JM, Williams A, Amis AA. Biomechanical comparison of anterolateral procedures combined with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(2):347–354. [DOI] [PubMed] [Google Scholar]
- 17. Jette C, Guiterrez D, Sastre S, Llusa M, Combalia A. Biomechanical comparison of anterolateral ligament anatomical reconstruction with a semi-anatomical lateral extra-articular tenodesis. a cadaveric study. Knee. 2019;26(5):1003–1009. [DOI] [PubMed] [Google Scholar]
- 18. Katakura M, Koga H, Nakamura T, et al. Biomechanical effects of additional anterolateral structure reconstruction with different femoral attachment sites on anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47(14):3373–3380. [DOI] [PubMed] [Google Scholar]
- 19. Kennedy MI, Claes S, Fuso FAF, et al. The anterolateral ligament: an anatomic, radiographic, and biomechanical analysis. Am J Sports Med. 2015;43:1606–1615. [DOI] [PubMed] [Google Scholar]
- 20. Kernkamp WA, Van de Velde SK, Hosseini A, et al. In vivo anterolateral ligament length change in the healthy knee during functional activities—a combined magnetic resonance and dual fluoroscopic imaging analysis. Arthroscopy. 2017;33(1):133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Monaco E, Fabbri M, Mazza D, et al. The effect of sequential tearing of the anterior cruciate and anterolateral ligament on anterior translation and the pivot-shift phenomenon: a cadaveric study using navigation. Arthroscopy. 2018;34(4):1009–1014. [DOI] [PubMed] [Google Scholar]
- 22. Moorman CT III, LaPrade RF. Anatomy and biomechanics of the posterolateral corner of the knee. J Knee Surg. 2005;18(2):137–145. [DOI] [PubMed] [Google Scholar]
- 23. Nielsen ET, Stentz-Oleson K, de Raedt S, et al. Influence of the anterolateral ligament on knee laxity: a biomechanical cadaveric study measuring knee kinematics in 6 degrees of freedom using dynamic radiostereometric analysis. Orthop J Sports Med. 2018;6(8):2325967118789699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nitri M, Rasmussen MT, Williams BT, et al. An in vitro robotic assessment of the anterolateral ligament, part 2: anterolateral ligament reconstruction combined with anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(3):593–601. [DOI] [PubMed] [Google Scholar]
- 25. Noyes FR, Huser LE, Jurgensmeier D, Walsh J, Levy MS. Is an anterolateral ligament reconstruction required in ACL-reconstructed knees with associated injury to the anterolateral structures? A robotic analysis of rotational knee stability. Am J Sports Med. 2017;45(5):1018–1027. [DOI] [PubMed] [Google Scholar]
- 26. Parsons EM, Gee AO, Spiekerman C, Cavanagh PR. The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med. 2015;43(2):669–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rasmussen MT, Nitri M, Williams BT, et al. An in vitro robotic assessment of the anterolateral ligament, part 1: secondary role of the anterolateral ligament in the setting of an anterior cruciate ligament injury. Am J Sports Med. 2016;44(3):585–592. [DOI] [PubMed] [Google Scholar]
- 28. Ruiz N, Filippi GJ, Gagniere B, et al. The comparative role of anterior cruciate ligament and anterolateral structures in controlling passive internal rotation of the knee: a biomechanical study. Arthroscopy. 2016;32(6):1053–1062. [DOI] [PubMed] [Google Scholar]
- 29. Schon JM, Moatshe G, Brady AW, et al. Anatomic anterolateral ligament reconstruction of the knee leads to over constraint at any fixation angle. Am J Sports Med. 2016;44(10):2546–2556. [DOI] [PubMed] [Google Scholar]
- 30. Smith PA, Thomas DM, Pomajzl RJ, Bley JA, Pfeiffer FM, Cook JL. A biomechanical study of the role of the anterolateral ligament and the deep iliotibial band for control of a simulated pivot shift with comparison of minimally invasive extra-articular anterolateral tendon graft reconstruction versus modified Lemaire reconstruction after anterior cruciate ligament reconstruction. Arthroscopy. 2019;35(5):1473–1483. [DOI] [PubMed] [Google Scholar]
- 31. Spencer L, Burkhart TA, Tran MN, et al. Biomechanical analysis of simulated clinical testing and reconstruction of the anterolateral ligament of the knee. Am J Sports Med. 2015;43(9):2189–2197. [DOI] [PubMed] [Google Scholar]
- 32. Sonnery-Cottet B, Saithna A, Cavalier M, et al. Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: a prospective comparative study of 502 patients from the SANTI study group. Am J Sports Med. 2017;45(7):1547–1557. [DOI] [PubMed] [Google Scholar]
- 33. Sonnery-Cottet B, Saithna A, Blakeney WG, et al. Anterolateral ligament reconstruction protects the repaired medial meniscus: a comparative study of 383 anterior cruciate ligament reconstructions from the SANTI study group with a minimum follow-up of 2 years. Am J Sports Med. 2018;46(8):1819–1826. [DOI] [PubMed] [Google Scholar]
- 34. Sonnery-Cottet B, Lutz C, Dagget M, et al. The involvement of the anterolateral ligament in rotational control of the knee. Am J Sports Med. 2016;44(5):1209–1214. [DOI] [PubMed] [Google Scholar]
- 35. Tavlo M, Eljaja S, Jensen JT, Siersma VD, Krogsgaard MR. The role of the anterolateral ligament in ACL insufficient and reconstructed knees on rotatory stability: a biomechanical study on human cadavers. Scand J Med Sci Sports. 2016;26(8):960–966. [DOI] [PubMed] [Google Scholar]
- 36. Terry GC, Norwood LA, Hughston JV, Caldwell KM. How iliotibial tract injuries of the knee combine with acute anterior cruciate ligament tears to influence abnormal anterior tibial displacement. Am J Sports Med. 1993;21(1):55–60. [DOI] [PubMed] [Google Scholar]
- 37. Trentacosta N, Pace JL, Metzger M. Biomechanical evaluation of pediatric anterior cruciate ligament (ACL) reconstruction techniques with and without the anterolateral ligament (ALL). J Pediatr Orthop. 2020:40(1):8–16. [DOI] [PubMed] [Google Scholar]
- 38. Vieira EL, Vieira EA, da Silva RT, et al. An anatomic study of the iliotibial tract. Arthroscopy. 2007;23(3):269–274. [DOI] [PubMed] [Google Scholar]
- 39. Vincent JP, Magnussen RA, Gezmez F, et al. The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):147–152. [DOI] [PubMed] [Google Scholar]
- 40. Wagih AM, Elguindy AM. Percutaneous reconstruction of the anterolateral ligament of the knee with a polyester tape. Arthrosc Tech. 2016;5(4):e691–e697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wilke J, Krause F, Niederer D, et al. Appraising the methodological quality of cadaveric studies: validation of the QUACS scale. J Anat. 2015;226(5):440–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wytrykowski K, Swider P, Reina N, et al. Cadaveric study comparing the biomechanical properties of grafts used for knee anterolateral ligament reconstruction. Arthroscopy. 2016;32(11):2288–2294. [DOI] [PubMed] [Google Scholar]
- 43. Yasuma S, Nozaki M, Murase A, et al. Anterolateral ligament reconstruction as an augmented procedure for double-bundle anterior cruciate ligament reconstruction restores rotational stability: quantitative evaluation of the pivot shift test using an inertial sensor. Knee. 2020;27(2):397–405. [DOI] [PubMed] [Google Scholar]
- 44. Zens M, Niemeyer P, Ruhhammer K, et al. Length changes of the anterolateral ligament during passive knee motion: a human cadaveric study. Am J Sports Med. 2015;43(10):2545–2552. [DOI] [PubMed] [Google Scholar]