Abstract
Background:
Adequate bowel preparation prior to colonoscopy is essential for visualization of the colonic mucosa to maximize adenoma and polyp detection. The risk of inadequate bowel cleansing is heightened if the patient is older, male, overweight, and has comorbidities, such as diabetes. This post hoc analysis of the combined MORA and NOCT clinical trials explores the efficacy of evening/morning split-dose regimens of NER1006 (PLENVU®, Norgine Ltd), a 1-liter polyethylene glycol (PEG) bowel preparation, to evaluate its bowel-cleansing efficacy in patients at risk for inadequate cleansing.
Methods:
Patients requiring colonoscopy were randomized to receive evening/morning split-dosing of either NER1006, 2-liter (2L) PEG and ascorbate, or oral sulfate solution (OSS). Bowel-cleansing efficacy was assessed by treatment-blinded central readers using the validated Harefield Cleansing Scale (HCS).
Results:
Split-dose NER1006 was associated with high levels of cleansing, ranging between 87.0% and 94.0% across all patient subtypes (n = 551), including patients with obesity or diabetes. However, patients aged >65 years and <45 years showed significantly greater rates of successful cleansing than patients aged 45–65 years (94.0% versus 94.2% versus 87.0%, p = 0.002). The high-risk patient subgroup, which included obese males aged ⩾60 years, had significantly improved overall and high-quality bowel-cleansing success rates of 100% (33/33) and 72.7% (27/33) on the HCS with NER1006, compared with 86.7% (26/30) and 50% (15/30) with the comparator solutions (p = 0.015 and p = 0.033, respectively). In this high-risk subgroup, adenoma detection was greater per patient receiving NER1006 versus the comparator group (1.82 versus 0.93, p = 0.041). NER1006 was the only treatment that enabled the detection of patients with ⩾5 adenomas [9.1% (3/33) versus 0/30, p = 0.047].
Conclusion:
NER1006 effectively cleansed a broad range of patients and offered superior bowel cleansing versus 2LPEG/OSS in patients at increased risk of colorectal cancer. Future research should establish whether more effective cleansing also enables improved adenoma detection.
Plain language summary
A low-volume bowel preparation solution to better detect lesions associated with colorectal cancer during colonoscopy
Colorectal cancer (CRC) is the fourth most commonly diagnosed cancer in the world. Obese men over the age of 65 years are at particularly increased risk of developing CRC. If the changes in their large intestine (colon) could be seen more clearly during a colonoscopy (where a small camera is inserted via the anus to examine the bowels from the inside), patients who need treatment would be diagnosed earlier, thus improving their chances of survival. In this paper we discuss the use of a bowel preparation solution that is more convenient for patients (less to drink) but also cleans bowels more effectively, meaning more lesions are detected than when other solutions are used. This improved cleansing, and thus better visualization, occurred in a range of patients, including those at higher risk of CRC, such as older, overweight men.
Keywords: 2LPEG/OSS, age, bowel cleansing, colorectal cancer, HCS, NER1006, obese males, special populations, ultra-low-volume PEG
Introduction
Colonoscopy for colorectal cancer (CRC) screening has been shown to reduce the incidence and mortality of CRC, leading to its introduction in many countries worldwide.1–4 In order to maximize the chance of detecting adenomas and polyps, complete visualization of the colonic mucosa is essential during colonoscopy. This is dependent on effective pre-procedural bowel preparation to attain an adequate level of bowel cleansing.5–8 Adequate bowel cleansing is also a factor in other measures of successful and high-quality colonoscopy, namely adenoma detection rate (ADR) and cecal intubation. 9 The European Society of Gastrointestinal Endoscopy states that colonoscopy centers should aim to achieve adequate bowel cleansing in at least 90% of procedures, with a quality target of ⩾95% of colonoscopies. 10
Despite the importance of adequate bowel preparation for colonoscopy, reports suggest that between 13% and 30% of bowel preparations for colonoscopy result in inadequate cleansing.9,11–15 The risk of having inadequate cleansing after undergoing bowel preparation frequently points to older age, male sex, and being overweight.12–14,16–20 These characteristics are also independent risk factors for increased CRC incidence and mortality.21–23 Old age is associated with immobilization, which leads to delayed gastrointestinal motility and increases the chances of poor bowel preparation. 19 In a large study involving over 25,000 individuals undergoing colonoscopy, ADR was higher in males, compared with females, and in patients with an increased body mass index (BMI). 24 The likelihood of inadequate bowel preparation increases cumulatively with each additional risk factor, for example, age, sex, and BMI. Moreover, comorbidities, such as diabetes, hypertension, stroke, dementia, cirrhosis, and constipation, are frequently associated with inadequate bowel preparation.12–14,16,19
Despite the identification of certain patient characteristics that may be associated with inadequate bowel preparation, there is a lack of data investigating the cleansing performance of bowel preparations in these subgroups. NER1006 (PLENVU®, Norgine Ltd) is a 1-liter (1L) polyethylene glycol (PEG) bowel preparation, which has been optimized for effective bowel cleansing.25–28 The efficacy and safety of NER1006 have been established across three phase III clinical trials and in studies of real-world colonoscopy practice.25–27,29 The aim of this post hoc analysis was to examine bowel-cleansing efficacy with overnight split-dosing of NER1006 in patient subgroups, examining the effect of both patient characteristics and other clinically relevant factors, using combined data from two phase III randomized controlled trials.
Methods
Study design
This is a post hoc analysis using combined data from two randomized, multicenter, and colonoscopist- and central reader-blinded phase III trials evaluating the bowel-cleansing efficacy, safety, and tolerability of NER1006 in adults undergoing colonoscopy [Morning Arm study (MORA); Nocturnal Pause Arm study (NOCT)]. The designs and main results of these trials have been reported in detail previously.25,26
All patients who received the split-dosing from the clinical trials were included, while patients receiving morning-only dosing were excluded.25,26 Patients aged 18–85 years undergoing colonoscopy for screening, surveillance, or diagnostic purposes were eligible for both studies.
Bowel-cleansing efficacy was assessed by treatment-blinded central readers using the validated Harefield Cleansing Scale (HCS). 30 This scale assesses cleansing in each of five bowel segments (the ascending colon/cecum, transverse colon, descending colon, sigmoid colon, and rectum) as 0 (irremovable, heavy, hard stools), 1 (semi-solid, only partially removable stools), 2 (brown liquid/fully removable semi-solid stools), 3 (clear liquid), or 4 (clean and empty). Overall, cleansing success is attained if scores of ⩾2 are recorded for all five bowel segments. High-quality bowel cleansing is defined by a score of 3 or 4 in each bowel segment.
The MORA study received Ethical Review Board approval in all participating countries (Commissie Medische Ethiek UZ Leuven, 20 October 2014; Comité de Protection des Personnes Ile-de-France X, 4 November 2014; Ethik-Kommission der Medizinischen Fakultät der Universität Würzburg, 15 October 2014; Komisja Bioetyczna przy Dolnośląskiej Izbie Lekarskiej we Wrocławiu, 12 October 2014; Hospital Clínico San Carlos Comité Ético de Investigación Clínica, 6 November 2014; and NRES Committee West Midlands – Coventry and Warwickshire, 15 September 2014). The study was approved by all Italian Ethical Review boards on 20 November 2014. The NOCT study received United States Ethical Review Board approval on 21 August 2014. Both studies were conducted in accordance with the Declaration of Helsinki, with all patients providing written informed consent.
Assessments
A post hoc analysis was conducted to investigate the bowel-cleansing efficacy of NER1006 in patient subgroups stratified by individual patient characteristics and other clinically relevant groups. Both trials contained a NER1006 arm in which it was administered as a 2-day evening/morning split-dosing regimen, and the trials were combined for this analysis to increase the numbers of patients in each subgroup. Analyses were conducted using the modified full analysis set (mFAS), which comprised all eligible patients who were randomized and received the study drug (based on patient diary entries).
Two measures of cleansing efficacy were assessed in all subgroups: overall bowel-cleansing success (HCS grade A or B) and the mean number of high-quality cleansed segments (HCS segment score 3 or 4) per patient.
Analyses were evaluated in subgroups according to patient characteristics, namely sex (male or female), age (<45 years, 45–65 years, or >65 years), and BMI (<25 kg/m2, 25–<30 kg/m2, or ⩾30 kg/m2), and other clinically relevant subgroups, such as the reason for colonoscopy (screening, surveillance, or diagnosis), time from the end of bowel preparation to start of colonoscopy (<6 h or ⩾6 h), renal function status (normal or mild-to-moderate impairment), and diabetes (presence or absence).
In order to assess the impact of multiple risk factors on lesion detection and bowel-cleansing performance, a comparative analysis of NER1006 versus comparator bowel preparations was conducted in all patients who were male, aged 60 years or older, and who were clinically obese (had a BMI ⩾30 kg/m2). Patients meeting all these criteria and with available HCS cleansing grades from both site colonoscopists and central readers were combined from MORA and NOCT depending on whether they received 2-day evening/morning split-dosed NER1006 or comparator preparations [2-liter PEG (2LPEG) or oral sulfate solution (OSS)]. HCS cleansing performance, polyp detection rate (PDR), ADR, ADR5+ (five or more adenomas), and mean polyps (MPP) and adenomas per patient (MAP) were compared.
Statistical analysis
Statistical analyses were performed using the statistical packages SAS version 9.2 (SAS Institute, Cary, NC, USA) and R version 4.0.2 (The R Foundation for Statistical Computing, 2020). Patient-level demographic and cleansing data (overall HCS cleansing grades and HCS segmental scores) from the clinical trials MORA and NOCT were used in these post hoc analyses. A combined analysis of overall bowel-cleansing success was conducted using a variance-weighted combination of the difference in proportions with overall cleansing success in NOCT and MORA. p-Values for the difference between subgroups assessed by the Chi-square heterogeneity test were applied to combined success rate estimates from each of the subgroups. Adequate-quality cleansing success rates were compared using the two-sided t-test. For the combined mean number of high-quality segments achieved with NER1006 in the subgroups, the individual numbers of high-quality segments recorded in each colonoscopy were collected, and the mean ± standard deviation was calculated for each subgroup.
We performed kappa statistics analysis to compare the inter-observer variability between the cleansing scores rated by central readers and site colonoscopists. 31
Results
Patient population
The patient demographics of the combined MORA and NOCT trials are presented in Table 1. The patients’ compliance with NER1006 in different subgroups of patients across the two clinical trials was consistently high (Table 2). The number of patients in the different subgroups that had their colonoscopy within or after 6 h from end of bowel preparation with NER1006 are reported in Table 3. Across the two trials in the mFAS dataset, a total of 551 patients received evening/morning split-dose NER1006, featuring 275 from the MORA trial and 276 from NOCT. There were 33 and 30 patients in the combined NER1006 and comparator groups, respectively, who were male, aged ⩾60 years, and had a BMI ⩾30 kg/m2.
Table 1.
Patient demographics.
| Parameters | Subgroups | % (n/N) |
|---|---|---|
| Sex | Male | 46.3 (255/551) |
| Female | 53.7 (296/551) | |
| Age (years) | >65 | 22.1 (122/551) |
| 45–65 | 65.3 (360/551) | |
| <45 | 12.5 (69/551) | |
| BMI (kg/m2) | ⩾30 | 34.3 (189/551) |
| 25–<30 | 38.3 (211/551) | |
| <25 | 27.4 (151/551) | |
| Reason for colonoscopy | Screening | 55.2 (304/551) |
| Surveillance | 27.2 (150/551) | |
| Diagnostic | 17.6 (97/551) | |
| Renal insufficiency | None | 31.9 (166/521) |
| Mild-to-moderate | 68.1 (355/521) | |
| Time from end of prep to colonoscopy (hours) | <6 | 58.0 (302/521) |
| ⩾6 | 42.0 (219/521) | |
| Diabetes | Yes | 8.5 (47/551) |
| No | 91.5 (504/551) |
BMI, body mass index
Table 2.
NER1006 2-day treatment compliance (⩾75%) by subgroup [modified full analysis set (mFAS)].
| Parameter | Subgroup | NOCT | MORA | Combined | |||
|---|---|---|---|---|---|---|---|
| N | n (%) | N | n (%) | N | n (%) | ||
| Sex | Male | 135 | 131 (97) | 108 | 97 (89.8) | 243 | 228 (93.8) |
| Female | 127 | 124 (97.6) | 154 | 138 (89.6) | 281 | 262 (93.2) | |
| Age (years) | >65 | 48 | 47 (97.9) | 70 | 62 (88.6) | 118 | 109 (92.4) |
| 45–65 | 192 | 186 (96.9) | 149 | 135 (90.6) | 341 | 321 (94.1) | |
| <45 | 22 | 22 (100.0) | 43 | 38 (88.4) | 65 | 60 (92.3) | |
| BMI (kg/m2) | ⩾30 | 108 | 104 (96.3) | 71 | 61 (85.9) | 179 | 165 (92.2) |
| 25–<30 | 101 | 101 (100.0) | 99 | 86 (86.9) | 200 | 187 (93.5) | |
| <25 | 53 | 50 (94.3) | 91 | 87 (95.6) | 144 | 137 (95.1) | |
| Reason for colonoscopy | Screening | 154 | 150 (97.4) | 133 | 116 (87.2) | 287 | 266 (92.7) |
| Surveillance | 80 | 77 (96.3) | 63 | 56 (88.9) | 143 | 133 (93.0) | |
| Diagnostic | 28 | 28 (100.0) | 66 | 63 (95.5) | 94 | 91 (96.8) | |
| Renal insufficiency | None | 95 | 92 (96.8) | 71 | 65 (91.5) | 166 | 157 (94.6) |
| Mild/Moderate | 166 | 162 (97.6) | 189 | 168 (88.9) | 355 | 330 (93.0) | |
| Time from end of prep to colonoscopy (hours) | <6 | 181 | 175 (96.7) | 121 | 110 (90.9) | 302 | 285 (94.4) |
| ⩾6 | 79 | 78 (98.7) | 140 | 125 (89.3) | 219 | 203 (92.7) | |
| Diabetes | Yes | 27 | 27 (100.0) | 15 | 12 (80.0) | 42 | 39 (92.9) |
| No | 235 | 228 (97.0) | 247 | 223 (90.3) | 482 | 451 (93.6) | |
BMI, body mass index; N, the number of subjects in the subgroup; n, the number of subjects with ⩾75% treatment compliance.
Table 3.
The number of patients in different subgroups who underwent colonoscopy within or after 6 h from end of bowel preparation with NER1006 and obtained readable videos with Harefield Cleansing Scale grades assigned by central readers [modified full analysis set (mFAS)].
| Parameter | Subgroup | <6 h, n | ⩾6 h, n |
|---|---|---|---|
| Sex | Male | 147 | 88 |
| Female | 151 | 129 | |
| Age (years) | >65 | 72 | 45 |
| 45–65 | 198 | 135 | |
| <45 | 28 | 37 | |
| BMI (kg/m2) | ⩾30 | 97 | 78 |
| 25–<30 | 121 | 77 | |
| <25 | 80 | 62 | |
| Reason for colonoscopy | Screening | 160 | 121 |
| Surveillance | 87 | 54 | |
| Diagnostic | 51 | 42 | |
| Renal insufficiency | None | 111 | 54 |
| Mild/Moderate | 185 | 162 | |
| Diabetes | Yes | 271 | 204 |
| No | 27 | 13 |
BMI, body mass index.
Overall bowel-cleansing success according to patient characteristics
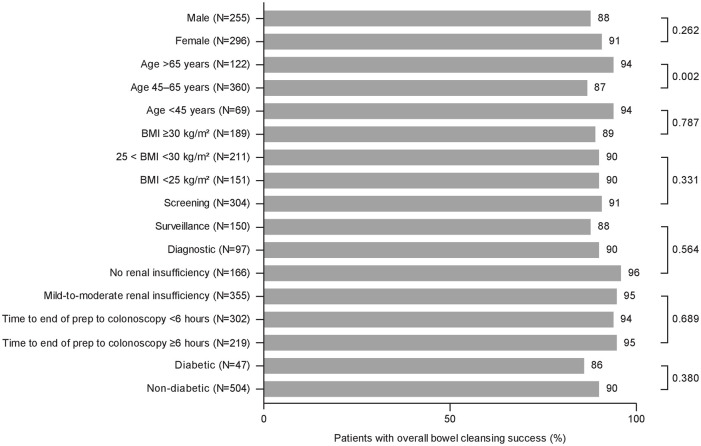
Patient characteristics for the individual and combined treatment groups have been described elsewhere.25,26,32 Overall successful bowel cleansing on the HCS in each of the subgroups is presented in Figure 1. Split-dose NER1006 was associated with high levels of cleansing across all patient types, ranging between 87.0% and 94.0% of patients. There were no statistically significant differences in successful cleansing between any of the subgroups, with the exception of age (p = 0.002). Variance-weighted successful cleansing among the combined age subgroups was 94.0% for patients aged >65 years, 87.0% for patients aged 45–65 years, and 94.2% for patients aged <45 years. Since cleansing may be expected to be worse with advanced age, we compared patients aged 70 (n = 59) and over with patients younger than 70 (n = 458). Both groups achieved adequate cleansing at rates of 94.9% and 94.3%, respectively (p = 0.853), on the HCS graded by central readers. All 17 patients (100%) aged >75 years given split-dose NER1006 attained adequate cleansing success, while 9/12 (75%) in the same age group achieved adequate cleansing when using either OSS or 2LPEG.
Figure 1.
The overall cleansing success with NER1006 across patient subgroups in the combined population.
Overall bowel-cleansing success in clinically relevant subgroups
As shown in Figure 1, the variance-weighted rates of successful cleansing were similarly high among clinically relevant subgroups receiving split-dose NER1006, ranging from 85.7% to 95.6% of patients. There were no significant differences in the rate of overall cleansing success between any of the subgroups. The rate of successful cleansing among patients with mild-to-moderate renal insufficiency was 94.5%, compared with 95.6% in patients without renal insufficiency (p = 0.564). The rate of cleansing in patients with diabetes was 85.7%, compared with 90.0% in patients without diabetes (p = 0.380).
Mean number of high-quality cleansed bowel segments
The mean number of bowel segments with high-quality cleansing on the HCS per subgroup is given in Table 4. The mean numbers of high-quality segments were similar across all subgroups, ranging from 2.1 to 2.6 per patient. Patients aged >65 years had an average of 2.2 high-quality segments, compared with 2.3 for the other age groups. Similar numbers were seen in other relevant subgroups: 2.2 for patients with diabetes versus 2.3 for patients without diabetes; 2.4 for patients with a BMI ⩾30 kg/m2 versus 2.3 for other BMI subgroups; and 2.4 for patients with renal insufficiency versus 2.6 for patients without renal insufficiency.
Table 4.
Mean number of high-quality segments in subgroups receiving NER1006.
| Parameter | Subgroup (N) | Mean number of HQ segments | Standard deviation |
|---|---|---|---|
| Sex | Male (N = 255) | 2.2 | 1.83 |
| Female (N = 296) | 2.4 | 1.84 | |
| Age (years) | >65 (N = 122) | 2.2 | 1.66 |
| 45–65 (N = 360) | 2.3 | 1.88 | |
| <45 (N = 69) | 2.3 | 1.91 | |
| BMI (kg/m2) | ⩾30 (N = 189) | 2.4 | 1.90 |
| 25–<30 (N = 211) | 2.3 | 1.80 | |
| <25 (N = 151) | 2.3 | 1.81 | |
| Reason for colonoscopy | Screening (N = 304) | 2.2 | 1.80 |
| Surveillance (N = 150) | 2.3 | 1.95 | |
| Diagnostic (N = 97) | 2.5 | 1.77 | |
| Renal insufficiency | None (N = 166) | 2.6 | 1.89 |
| Mild-to-moderate (N = 355) | 2.4 | 1.76 | |
| Time from end of prep to colonoscopy (hours) | <6 (N = 302) | 2.6 | 1.83 |
| ⩾6 (N = 219) | 2.1 | 1.72 | |
| Diabetes | Yes (N = 47) | 2.2 | 2.03 |
| No (N = 504) | 2.3 | 1.82 |
BMI, body mass index; HQ, high quality
Comparative cleansing performance and lesion detection in patients with multiple risk factors for inadequate bowel preparation
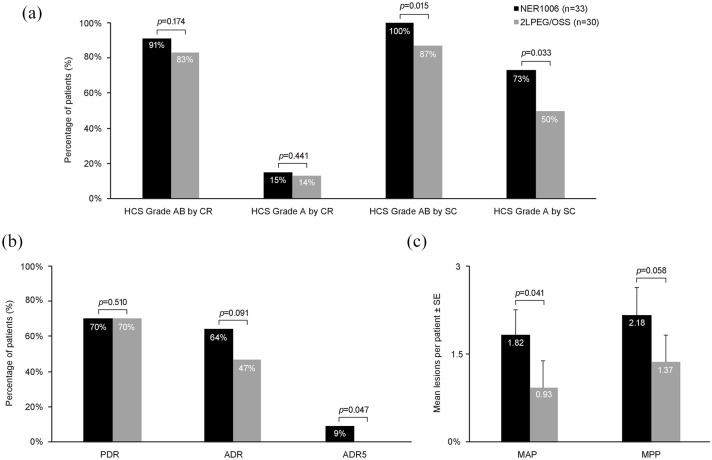
Among the obese male patients who were aged 60 years or older, there was no significant difference in either overall cleansing (HCS grade A or B) or high-quality cleansing (HCS grade A) with NER1006 when cleansing was assessed by central readers (Figure 2a). However, combined NER1006 groups attained a higher level of overall bowel-cleansing success rate of 90.9% (30/33) in these high-risk patients, compared with 82.8% (24/29) in the combined comparator group (p = 0.174). There was a low rate of high-quality cleansing in the high-risk patients when scored by central readers [15.2% (5/33) versus 13.8% (4/29), respectively; p = 0.441].
Figure 2.
Comparison of Harefield Cleansing Scale (HCS) cleansing performance and lesion detection in older male patients with high BMI. (a) Overall cleansing success (grade A+B) and high-quality cleansing (grade A) on the HCS for NER1006 or comparators, as assessed by central readers (CR) or site colonoscopists (SC). (b) Comparison of lesion detection (PDR, ADR, ADR5). (c) Mean lesions per patient (MPP and MAP) between NER1006 and comparators.
For CR assessments, n = 29 for 2LPEG/OSS due to an unreadable video.
ADR, adenoma detection rate; ADR5, five or more adenomas; PDR, polyp detection rate
Among the site colonoscopists’ assessments of the two groups with these three risk factors, both overall and high-quality cleansing success were significantly improved with NER1006 versus comparator preparations (Figure 2a). Site colonoscopists assessed that 100.0% (33/33) and 72.7% (24/33) of patients had overall and high-quality success on the HCS with NER1006, compared with 86.7% (26/30) and 50.0% (15/30) among those receiving comparator preparations (p = 0.015 and p = 0.033, respectively).
The basic lesion detection rates among this high-risk group were similar: PDR was 69.7% (23/33) for NER1006 versus 70.0% (21/30) in the combined comparator group (p = 0.510), and the ADR was 63.6% (21/33) and 46.7% (14/30), respectively (p = 0.091) (Figure 2b). Among obese males aged 60 or older and with multiple adenomas, bowel preparation with NER1006 enabled detection of 9.1% (3/33) patients with five or more adenomas (ADR5+), whereas no such patients were detected in the comparator group (p = 0.047). Similarly, when looking at the mean numbers of lesions detected per patient, significantly more adenomas per patient were detected in patients receiving NER1006 compared with those in the comparator group (MAP: 1.82 versus 0.93, p = 0.041) (Figure 2c).
Discussion
We conducted a post hoc analysis using combined data from two large, randomized controlled bowel preparation trials. The 2-day evening/morning split-dose regimen of NER1006 demonstrated successful bowel-cleansing rates of between 85.7% and 95.6% across individual patient subgroups. The mean number of bowel segments with high-quality cleansing was comparable across subgroups, which, on average, had more than two segments on the HCS with high-quality cleansing.
Previous studies have reported a multitude of factors that are associated with inadequate bowel cleansing in patients undergoing colonoscopy.12–14,16–19 Two of these studies specifically looked at factors associated with inadequate cleansing in patients undergoing bowel preparation with PEG-based preparations.19,33 In the first of these studies, 362 patients received a PEG-based bowel preparation, and the reported rate of inadequate cleansing was 28.2%. 19 Using multivariate regression analysis, they showed that age over 60 years, a history of diabetes, appendectomy, colorectal resection, or hysterectomy were independent predictors of inadequate cleansing.
The second study enrolled 715 patients receiving bowel preparation with a lower-volume 2LPEG plus ascorbate and who had a rate of inadequate preparation of 19.3%. 33 Their multivariate analysis showed that cirrhosis, low compliance with low-fiber diet prior to the colonoscopy, brown liquid rectal effluent, and a greater than 2-hour interval between last defecation and colonoscopy were factors associated with inadequate preparation.
In the NER1006 trials, patients with previous colonic resection or cirrhosis were excluded from the study population, so no data are available for these subgroups. However, in the analysis presented here, there was no significant difference in the rate of successful bowel cleansing in patients with a history of diabetes or in patients with a >6-hour window from completing bowel preparation to start of the colonoscopy. These data suggest that NER1006 efficacy may be maintained across subgroups that have previously been associated with inadequate bowel preparation when using PEG-based bowel preparations. This makes NER1006 a suitable choice for effective pre-colonoscopy bowel preparation in different patients with varied characteristics.
The only patient factor that significantly affected the attainment of successful bowel preparation was age. In contrast to previous reports suggesting successful cleansing is reduced in patients aged >60 years, it was the 45–65-year-old age group that had a lower rate of success. The youngest (under 45) and oldest (over 65) groups had a broadly similar rate of overall cleansing (94.2% and 94.0%, respectively). Before the combination of data, weighting was performed to account for variance between the two studies, and the rate of successful cleansing in NOCT was broadly similar across age groups (<45 years: 87.5%; 45–65 years: 84.7%; >65 years: 86.0%). In MORA, higher rates of successful cleansing, compared with NOCT, were observed across all age groups but with particularly high success in the youngest and oldest groups (<45 years: 95.6%; 45–65 years: 89.2%; >65 years: 95.8%). We also analyzed patients aged 70 and over and compared them with patients younger than 70, and found adequate bowel cleansing was comparable between the two groups. Based on the original design of the MORA and NOCT clinical trials,25,26 the missing values were imputed, which led to a significant difference in the different age groups. When we removed the imputed values from the analysis, the age group (45–65 years old) showed 93.1% bowel-cleansing efficacy compared with 95.7% (p = 0.318) and 98.4% (p = 0.098) of individuals aged over 65 or less than 45 years old, respectively—the difference in age group was no longer significant.
This post hoc analysis only included patients on the evening/morning split-dose. The split-dose has consistently been found to improve the quality of bowel cleansing.34,35 Here, we showed that split-dose NER1006 was able to overcome the limitations of inadequate bowel cleansing in different subgroups; for example, NER1006 led to 100% adequate cleansing success in patients older than 75. NER1006 provided high levels of overall successful bowel cleansing (100% success according to site endoscopists and >90% success when assessed more strictly by central readers) in the 33 patients who had the three simultaneous risk factors for each of cleansing failure, colorectal adenomas, and CRC (obese, male, aged 60 or older). A similar profile of efficacy for NER1006, compared with the comparator preparations, was also observed in the general trial population.25,26,36
When assessed by site colonoscopists, significantly more patients attained high-quality cleansing (HCS grade A) in the combined NER1006 group compared with comparators. There was a notable disparity between the high-quality cleansing as scored by central readers and site colonoscopists. While only 15% of patients from the combined NER1006 group were graded high-quality by central readers, site colonoscopists graded 73% of patients as a high-quality result. It has been shown that central readers tend to rate bowel cleansing more harshly than colonoscopists performing the procedure. 37 The latter percentage is important since both gradings are independently associated with improved adenoma detection. However, the grading by site endoscopists reflects what the clinical practitioners experience in their daily work when detecting adenomas. 38 There was also a comparatively small number of patients in each treatment group who met all three risk factors in both the MORA and NOCT studies. Rates of high-quality cleansing in the multiple risk factor group were similar to the site colonoscopists’ assessments in the original populations of MORA (68.0%) and NOCT (69.9%). 36
High rates of lesions were observed among the multiple risk factors group, irrespective of bowel preparation received (PDR: around 70.0% for both treatment groups). This was higher than in the general trial populations, where PDRs were 44.0–45.7% and 44.5–48.6% in patients receiving NER1006 or comparator preparation in MORA and NOCT, respectively.25,26 While the triple-risk group sample size was small in this analysis, the higher frequency of lesion detection in these patients is likely due to a combination of risk factors. Old age, male sex, and obesity are established risk factors for increased risk of CRC mortality and development of high-risk adenomas.21–23 The overall ADRs were numerically higher for NER1006 versus the comparator solutions (63.6% versus 46.7%) but not statistically significant due to the small population size. Meanwhile, the detection rate of patients with multiple adenomas and the MAP were significantly greater in high-risk patients receiving NER1006 versus the comparators. This suggests that the higher rates of successful and high-quality cleansing may result in a greater number of lesions being detected for individual patients.
Due to the post hoc nature of the current study, individual subgroups may not be powered to detect differences in cleansing performance. It would have been useful to collect more data regarding the patients’ comorbidities, smoking status, alcohol consumption, and medication history. We did not perform correction for multiple comparisons, as the present study was exploratory. Future studies with a larger number of older, male, and obese patients would be required to ascertain the superiority of NER1006 over the comparator solutions. Moreover, prospective studies should be designed that evaluate the efficacy of low-volume products (NER1006) in subgroups with recognized risk factors for inadequacies, such as diabetes, hypertension, constipation, and cirrhosis.
In this post hoc analysis, using combined data from two randomized trials, NER1006 demonstrated high rates of bowel-cleansing success across a broad range of patients, including superior cleansing outcomes and greater adenoma detection, when compared with 2LPEG/OSS in a small group of obese men aged 60 years or older. Future research should establish whether NER1006 can improve adenoma detection in such hard-to-cleanse patients who are also at increased risk for colorectal adenomas and CRC.
Acknowledgments
Medical writing assistance was provided by Rory Elsome, London, funded by Norgine.
Footnotes
Conflict of interest statement: Sandra Baile-Maxia does not have any conflicts of interest; Bharat Amlani is an employee of Norgine; and Rodrigo Jover Martínez has received consultancy honoraries from Norgine, Merck Sharp & Dohme, Alfa-Sigma, GISupply, and CPP Pharmaceutical.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The MORA and NOCT trials and the present post hoc analysis were funded by Norgine. This study was supported by Instituto de Salud Carlos III (PI1401386, PI1701756).
Contributor Information
Sandra Baile-Maxia, Gastroenterology Department, Hospital General Universitario de Alicante, Instituto de Investigación Biomédica ISABIAL, Alicante, Spain.
Bharat Amlani, Norgine Ltd, Medical Affairs, Harefield, UK.
Rodrigo Jover Martínez, Instituto de Investigación Sanitaria ISABIAL, Servicio de Medicina Digestiva, Hospital General Universitario de Alicante, Avda Pintor Baeza, Alicante, 03010, Spain; Gastroenterology Department, Hospital General Universitario de Alicante, Instituto de Investigación Biomédica ISABIAL, Alicante, Spain.
References
- 1. Brenner H, Stock C, Hoffmeister M. Effect of screening sigmoidoscopy and screening colonoscopy on colorectal cancer incidence and mortality: systematic review and meta-analysis of randomised controlled trials and observational studies. BMJ 2014; 348: g2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lin JS, Piper MA, Perdue LA, et al. Screening for colorectal cancer: a systematic review for the U.S. preventive services task force. Rockville (MD): Agency for Healthcare Research and Quality (US), http://www.ncbi.nlm.nih.gov/books/NBK373584 (2016, accessed 26 March 2021). [PubMed] [Google Scholar]
- 3. Doubeni CA, Corley DA, Quinn VP, et al. Effectiveness of screening colonoscopy in reducing the risk of death from right and left colon cancer: a large community-based study. Gut 2018; 67: 291–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nishihara R, Wu K, Lochhead P, et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med 2013; 369: 1095–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Oh CH, Lee CK, Kim J-W, et al. Suboptimal bowel preparation significantly impairs colonoscopic detection of non-polypoid colorectal neoplasms. Dig Dis Sci 2015; 60: 2294–2303. [DOI] [PubMed] [Google Scholar]
- 6. Clark BT, Protiva P, Nagar A, et al. Quantification of adequate bowel preparation for screening or surveillance colonoscopy in men. Gastroenterology 2016; 150: 396–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Clark BT, Laine L. High-quality bowel preparation is required for detection of sessile serrated polyps. Clin Gastroenterol Hepatol 2016; 14: 1155–1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Anderson JC, Butterly LF, Robinson CM, et al. Impact of fair bowel preparation quality on adenoma and serrated polyp detection: data from the New Hampshire colonoscopy registry by using a standardized preparation-quality rating. Gastrointest Endosc 2014; 80: 463–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hassan C, Bretthauer M, Kaminski MF, et al. Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 2013; 45: 142–150. [DOI] [PubMed] [Google Scholar]
- 10. Kaminski MF, Thomas-Gibson S, Bugajski M, et al. Performance measures for lower gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. Endoscopy 2017; 49: 378–397. [DOI] [PubMed] [Google Scholar]
- 11. Johnson DA, Barkun AN, Cohen LB, et al. Optimizing adequacy of bowel cleansing for colonoscopy: recommendations from the U.S. Multi-Society Task Force on colorectal cancer. Gastrointest Endosc 2014; 80: 543–562. [DOI] [PubMed] [Google Scholar]
- 12. Hassan C, Fuccio L, Bruno M, et al. A predictive model identifies patients most likely to have inadequate bowel preparation for colonoscopy. Clin Gastroenterol Hepatol 2012; 10: 501–506. [DOI] [PubMed] [Google Scholar]
- 13. Ness RM, Manam R, Hoen H, et al. Predictors of inadequate bowel preparation for colonoscopy. Am J Gastroenterol 2001; 96: 1797–1802. [DOI] [PubMed] [Google Scholar]
- 14. Dik VK, Moons LMG, Hüyük M, et al. Predicting inadequate bowel preparation for colonoscopy in participants receiving split-dose bowel preparation: development and validation of a prediction score. Gastrointest Endosc 2015; 81: 665–672. [DOI] [PubMed] [Google Scholar]
- 15. Baile-Maxía S, Mangas-Sanjuan C, Medina-Prado L, et al. Diagnostic yield of early repeat colonoscopy after suboptimal bowel preparation in a fecal immunochemical test-based screening program. Endoscopy 2020; 52: 1093–1100. [DOI] [PubMed] [Google Scholar]
- 16. Yee R, Manoharan S, Hall C, et al. Optimizing bowel preparation for colonoscopy: what are the predictors of an inadequate preparation? Am J Surg 2015; 209: 787–792. [DOI] [PubMed] [Google Scholar]
- 17. Mahmood S, Farooqui SM, Madhoun MF. Predictors of inadequate bowel preparation for colonoscopy: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol 2018; 30: 819–826. [DOI] [PubMed] [Google Scholar]
- 18. Gandhi K, Tofani C, Sokach C, et al. Patient characteristics associated with quality of colonoscopy preparation: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 2018; 16: 357–369.e10. [DOI] [PubMed] [Google Scholar]
- 19. Chung YW, Han DS, Park KH, et al. Patient factors predictive of inadequate bowel preparation using polyethylene glycol: a prospective study in Korea. J Clin Gastroenterol 2009; 43: 448–452. [DOI] [PubMed] [Google Scholar]
- 20. Borg BB, Gupta NK, Zuckerman GR, et al. Impact of obesity on bowel preparation for colonoscopy. Clin Gastroenterol Hepatol 2009; 7: 670–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Corley DA, Jensen CD, Marks AR, et al. Variation of adenoma prevalence by age, sex, race, and colon location in a large population: implications for screening and quality programs. Clin Gastroenterol Hepatol 2013; 11: 172–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shaukat A, Dostal A, Menk J, et al. BMI is a risk factor for colorectal cancer mortality. Dig Dis Sci 2017; 62: 2511–2517. [DOI] [PubMed] [Google Scholar]
- 23. Bayerdörffer E, Mannes GA, Ochsenkühn T, et al. Increased risk of ‘high-risk’ colorectal adenomas in overweight men. Gastroenterology 1993; 104: 137–144. [DOI] [PubMed] [Google Scholar]
- 24. Waldmann E, Heinze G, Ferlitsch A, et al. Risk factors cannot explain the higher prevalence rates of precancerous colorectal lesions in men. Br J Cancer 2016; 115: 1421–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. DeMicco MP, Clayton LB, Pilot J, et al. Novel 1 L polyethylene glycol-based bowel preparation NER1006 for overall and right-sided colon cleansing: a randomized controlled phase 3 trial versus trisulfate. Gastrointest Endosc 2018; 87: 677–687.e3. [DOI] [PubMed] [Google Scholar]
- 26. Bisschops R, Manning J, Clayton LB, et al. Colon cleansing efficacy and safety with 1 L NER1006 versus 2 L polyethylene glycol + ascorbate: a randomized phase 3 trial. Endoscopy 2019; 51: 60–72. [DOI] [PubMed] [Google Scholar]
- 27. Schreiber S, Baumgart DC, Drenth JPH, et al. Colon cleansing efficacy and safety with 1 L NER1006 versus sodium picosulfate with magnesium citrate: a randomized phase 3 trial. Endoscopy 2019; 51: 73–84. [DOI] [PubMed] [Google Scholar]
- 28. Plenvu powder for oral solution. Summary of Product Characteristics (SmPC) – (eMC), https://www.medicines.org.uk/emc/product/8578 (2020, accessed 26 March 2021).
- 29. Maida M, Sinagra E, Morreale GC, et al. Effectiveness of very low-volume preparation for colonoscopy: a prospective, multicenter observational study. World J Gastroenterol 2020; 26: 1950–1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Halphen M, Heresbach D, Gruss H-J, et al. Validation of the Harefield cleansing scale: a tool for the evaluation of bowel cleansing quality in both research and clinical practice. Gastrointest Endosc 2013; 78: 121–131. [DOI] [PubMed] [Google Scholar]
- 31. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–174. [PubMed] [Google Scholar]
- 32. Epstein MS, Benamouzig R, Halonen J, et al. High-quality colon cleansing and multiple neoplasia detection with 1L NER1006 versus mid-volume options: post hoc analysis of phase 3 clinical trials. Endosc Int Open 2020; 8: E628–E635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shin SY, Ga KS, Kim IY, et al. Predictive factors for inadequate bowel preparation using low-volume polyethylene glycol (PEG) plus ascorbic acid for an outpatient colonoscopy. Sci Rep 2019; 9: 19715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Martel M, Barkun AN, Menard C, et al. Split-dose preparations are superior to day-before bowel cleansing regimens: a meta-analysis. Gastroenterology 2015; 149: 79–88. [DOI] [PubMed] [Google Scholar]
- 35. Shah H, Desai D, Samant H, et al. Comparison of split-dosing vs non-split (morning) dosing regimen for assessment of quality of bowel preparation for colonoscopy. World J Gastrointest Endosc 2014; 6: 606–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Repici A, Coron E, Sharma P, et al. Improved high-quality colon cleansing with 1L NER1006 versus 2L polyethylene glycol + ascorbate or oral sulfate solution. Dig Liver Dis 2019; 51: 1671–1677. [DOI] [PubMed] [Google Scholar]
- 37. Ell C, Fischbach W, Bronisch H-J, et al. Randomized trial of low-volume PEG solution versus standard PEG + electrolytes for bowel cleansing before colonoscopy. Am J Gastroenterol 2008; 103: 883–893. [DOI] [PubMed] [Google Scholar]
- 38. Hassan C, Manning J, Álvarez González MA, et al. Improved detection of colorectal adenomas by high-quality colon cleansing. Endosc Int Open 2020; 8: E928–E937. [DOI] [PMC free article] [PubMed] [Google Scholar]