Abstract
Objective:
Although specialized early intervention services (EISs) for psychosis promote engagement in care, a substantial number of individuals who receive these services are discharged from care earlier than expected. The main goal of this study was to examine predictors of early discharge in a large sample of individuals enrolled in an EIS program in the United States.
Methods:
This cohort study (N=1,349) used programmatic data from OnTrackNY, an EIS program that delivers evidence-based interventions to youths across New York State experiencing a first episode of nonaffective psychosis. The main outcome was “early discharge,” which was operationalized as discharge prior to completing 12 months of treatment. Cox proportional hazard regression models were used to assess the association between sociodemographic, clinical, and support system predictors and early discharge.
Results:
The estimated probability of discharge before 1 year was 32%. Participants who at baseline had poor medication adherence, had no health insurance, were living alone or with nonparental family, or were using cannabis were at higher risk of leaving services within the first 12 months after enrollment. Individuals with higher social functioning were at lower risk of being discharged early from OnTrackNY, but those with higher occupational functioning were at a higher risk.
Conclusions:
Predictors of early discharge from EISs largely overlapped with previously identified predictors of poor prognosis in early psychosis. However, the association between early discharge and high occupational functioning indicates that trajectories leading up to discharge are heterogeneous.
Substantial evidence indicates that multidisciplinary, team-based, specialized early intervention services (EISs) for young people experiencing psychosis lead to better outcomes in symptoms and social functioning, compared with usual care (1, 2). These therapeutic benefits, however, are influenced by the degree to which participants engage with or stay in treatment (3). Although these programs utilize assertive engagement strategies designed to connect with young people and individualized interventions delivered according to their needs and preferences, many people receiving these services leave treatment sooner than would be recommended by the treatment team (4). Although there is no consensus on how long EIS programs should last, many provide services for 2 to 3 years (5). Treatment response to these services is heterogeneous; however, it is ordinarily assumed that individuals leaving services before 12 months who otherwise continue to meet criteria may have stopped services earlier than indicated for maximizing treatment effects (6). Although some participants disengage from treatment because of negative experiences with care, others may decide to leave early because they feel that services are no longer required or because they are moving away from the area served.
An increasing body of literature evaluates factors related to disengagement or early discharge from these services. These include duration of untreated psychosis, increased symptom severity, forensic history, lack of family support, and factors specific to ethnicity and culture (7). Some findings, however, are inconsistent. For instance, some studies have reported that clients living alone are more likely to leave services, whereas others have found the opposite (4, 7). Nevertheless, a recent systematic review found that individuals with lower levels of family support, reduced adherence to medication, and higher substance use were more likely to leave these services before expected (8).
In the aforementioned review, predictors such as symptomatology and social and occupational functioning were inconsistently associated with early discharge, despite the fact that these are usually the main outcomes in EISs and mental health services in general (9). Other limitations of the current evidence base include the relatively small samples in most studies (8), the limited number of reports from EIS programs based in the United States, and the lack of information regarding health system–level predictors, such as type of health services organization and financing. Health system factors are crucial, especially when comparing health services in the United States to those of countries with universal health coverage, such as the United Kingdom, Canada, and Australia.
Accordingly, the goal of this study was to use programmatic data to identify predictors of early discharge from treatment— sociodemographic and clinical predictors and predictors related to the support system, health care, and housing—in a large sample of individuals enrolled in an EIS program in the United States called OnTrackNY. On the basis of previous research, we hypothesized that lack of family support, poor medication adherence, and increased substance use would be associated with early discharge.
METHODS
Research Design
This was a cohort study that used programmatic data from OnTrackNY, an EIS program that delivers person-centered, recovery-oriented, culturally competent, EIS in a framework of shared decision making to young individuals experiencing a first episode of nonaffective psychosis across New York State (NYS) (10–13). The program offers evidence-based interventions, including medication management, case management, individual and group therapies (including cognitive-behavioral-oriented therapy, family support, and psychoeducation), supported employment and education, and peer services for individuals. OnTrackNY has a blended funding model that includes billing for services and grant funding from state and federal sources to support nonbillable services and care for those who are uninsured. Teams are required to accept all appropriate referrals without regard for the ability to pay or insurance status.
The OnTrackNY program includes a system for collecting data on outcomes and care processes. Data are collected quarterly for each client by using standardized admission, follow-up, and discharge forms, which are completed by clinicians through chart review and reports from participants and their families. These data are primarily used for quality improvement. Deidentified data are permitted to be used for research. For this study, all protected health information was removed from the data set. The NYS Psychiatric Institute Institutional Review Board approved the study procedures. The study sample included individuals ages 16 to 30 who were enrolled from October 2013 through October 2018.
Outcome
Early discharge was conceptualized as being discharged prior to reaching 12 months of treatment since enrollment in OnTrackNY. The 12-month cutoff was selected on the basis of comparable studies from different settings (8).
Predictors
We defined sociodemographic, clinical, support system, and health care– and housing-related predictors for OnTrackNY participants leaving the program within 12 months of being enrolled. On the basis of previous literature, our analysis included the following groups of variables at baseline as predictors of discharge within 12 months.
Sociodemographic variables.
Sociodemographic variables included age (continuous), sex (male or female), race (white, Black, Asian, or other) and ethnicity (Hispanic and non-Hispanic), highest education completed (less than high school, some college, college/postgraduate degree, or high school diploma/GED), and insurance type (uninsured, private, public, or other or unknown).
Clinical variables.
Clinical variables included medication adherence as judged by the treating prescriber (not adherent, adherent, not prescribed, or unknown), any substance use (yes or no), cannabis use (yes or no), self-injurious behavior (yes or no), suicidal ideation or attempt (yes or no), hospitalization for psychiatric reasons (yes or no), and time to first service contact after the onset of psychosis (continuous). The Mental Illness Research, Education and Clinical Center Global Assessment of Functioning Scale (MIRECC-GAF), which includes the symptoms (MIRECC-GAF symptoms), social functioning (MIRECC-GAF-SF), and occupational functioning (MIRECC-GAF-OF) subscales, was also included. The MIRECC-GAF-OF assesses the participant’s average level of functioning in his or her primary role as worker, student, or homemaker during the 30 days prior to assessment. The MIRECC-GAF-SF takes into account social interaction with friends and family, quality and quantity of relationships, ability to develop new relationships, and interpersonal conflicts in the previous 30 days. The MIRECC-GAF symptoms subscale captures the participant’s highest level of symptoms during the follow-up period (or the past 3 months for the baseline assessment) and is rated on the basis of suicidality, mood, anxiety, and psychotic symptoms. For all three subscales, scores range from 0 to 100; scores <50 are considered in the impaired range, while scores of ≥70 represent good functioning. These scores were recoded into a dichotomous variable and a categorical variable as further described below. MIRECC-GAF scoring reliability among OnTrack clinicians has been reported in a prior publication (12).
Support system.
Support system variables included the following: living situation (alone, or with parents, other family member, or other), family contact (daily, monthly or less, or weekly), has a support person (yes or no), and employment status of the support person (competitive employment, not in labor force, unemployed looking for work, other or unknown, or other employment).
Health care– and housing-related variables.
Variables related to health care and housing were health insurance status (uninsured, private, public, or other or unknown) and homelessness in the past 90 days (yes or no). These variables were included because they have not been explored previously and are key to understanding health care delivery in the United States, especially among people with severe mental disorders.
Data Analysis
The Kaplan-Meier estimator was used to estimate the cumulative incidence of early discharge from OnTrackNY. The time to event was defined as the number of days from enrollment to date of discharge for those who were discharged during the first year. Participants who did not have a full year of follow-up (because of rolling enrollment of the cohort) but who had not been discharged were considered right-censored. Right-censoring is a common form of missing data in time-to-event analysis in which the event (in this case discharge) is not observed because it occurs after the end of the study observation window. Participants who are right-censored are not considered discharged but contribute their available person-time to the analysis. Cox proportional hazard regression models, which are used to analyze time-to-event data with censoring, tested the association between baseline predictors and time to early discharge. Separate models were fit for each predictor, adjusting for site type (urban or rural), sex, age, race-ethnicity, and admission year. The assumption of proportional hazards was tested graphically and through the Schoenfeld’s test. Following the level-of-functioning categories suggested by Niv et al. (14), the MIRECC-GAF scores were first recoded as a categorical variable (<40 versus ≥40) and then categorized as a three-level variable: dysfunctional (<40), borderline (40–69), and fully functional (≥70). As in previous analyses, each model was adjusted by baseline sociodemographic variables. This analysis was motivated by the notion that the association between MIRECC-GAF and the outcome may vary by level of functioning.
RESULTS
Descriptive Findings
The Kaplan-Meier estimator of discharge within the first year of follow-up is plotted in Figure 1. The number of clients at risk (N=1,349), the cumulative number of clients discharged, and the cumulative number of clients censored for each follow-up point is shown in Table 1. The estimated probability of discharge before 1 year of follow-up was 32% (95% confidence interval [CI]=0.29–0.34).
FIGURE 1.
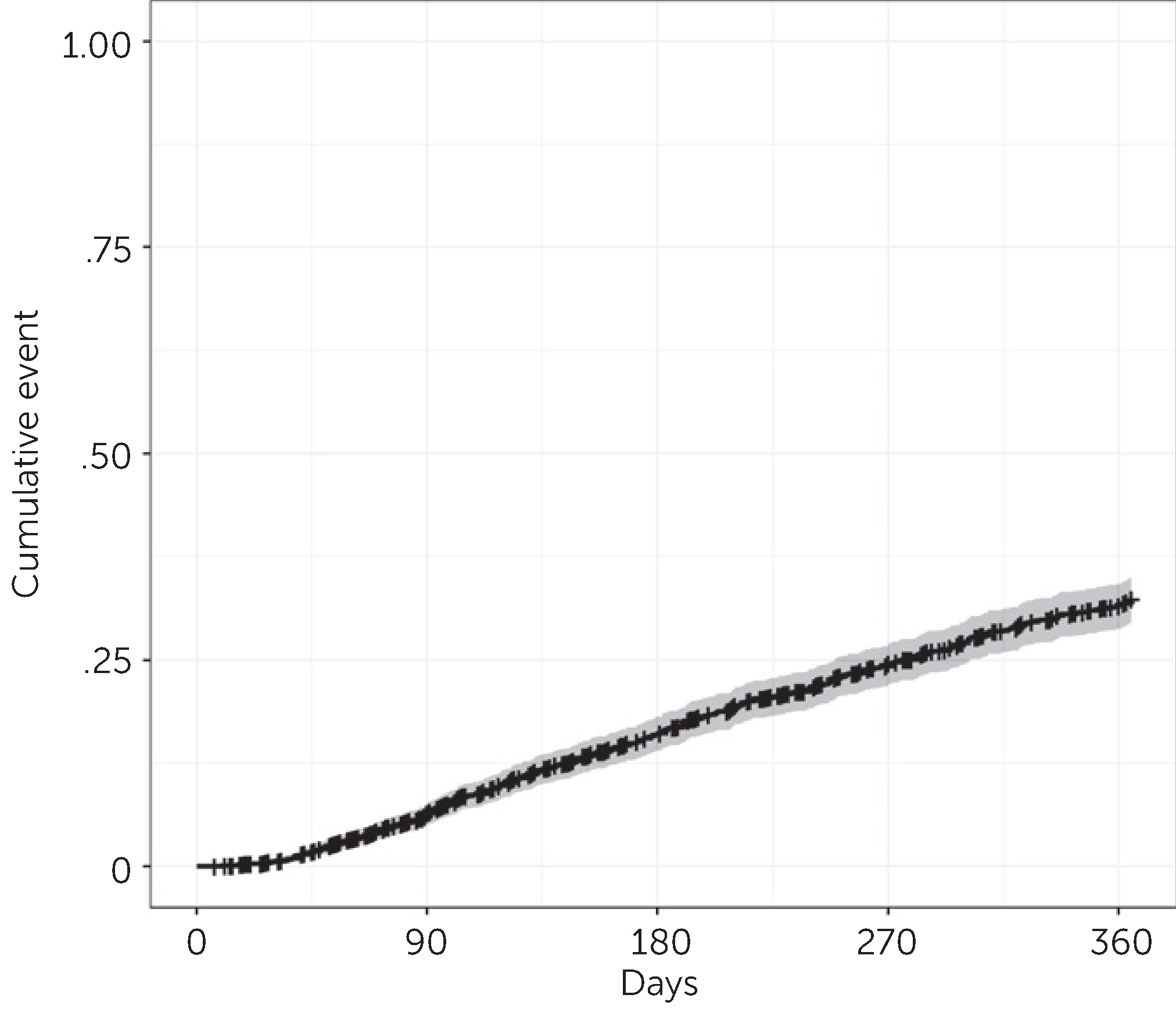
Kaplan-Meier plot based on early discharge events among 1,349 clients of OnTrackNY
TABLE 1.
Kaplan-Meier estimate of discharge probability in the first 12 months after enrollment among 1,349 clients of OnTrackNYa
| Month |
|||||
|---|---|---|---|---|---|
| Variable | Admission | 3 | 6 | 9 | 12 |
| Number at risk | 1,349 | 1,175 | 963 | 790 | 645 |
| Cumulative number of clients discharged | 0 | 79 | 198 | 289 | 361 |
| Cumulative number of clients censored | 0 | 95 | 188 | 270 | 343 |
Discharge probability was estimated by the Kaplan-Meier statistic as follows: 3 month, .06 (95% confidence interval [CI]=.051–.077); 6 month, .16 (95% CI = .14–.18); 9 month, .25 (95% CI = .22–.27);12 month, .32 (95% CI = .29–.34).
Predictors of Early Discharge
The results of a Cox proportional hazards model containing all sociodemographic variables predicting discharge in the first year of follow-up are presented in Table 2. The estimated hazard ratios and 95% CIs for each predictor of interest are presented in Table 3. These estimates are from models that included one predictor of interest and all sociodemographic covariates. Baseline medication adherence, health insurance status, living situation, and cannabis use were significantly associated with early discharge. Clients who were not adherent to medication at baseline had a higher estimated hazard of early discharge, compared with those who were adherent (HR=1.86). Similarly, clients who were not prescribed medication at baseline or had unknown prescription status at baseline had a higher hazard of early discharge, compared with those who were medication adherent (not prescribed, HR=1.97; unknown, HR=1.74). Clients who were uninsured at baseline had 2.56 times the hazard of early discharge, compared with clients with private insurance at baseline. Clients living alone or with nonparental family at baseline had a higher estimated hazard of early discharge, compared with those who lived with parents (alone, HR=1.87; nonparental family, HR=1.69). Finally, those who used cannabis at baseline had 1.37 times the hazard of early discharge, compared with those who did not use cannabis at baseline.
TABLE 2.
Analysis of variables as predictors of early discharge among 1,349 clients of OnTrackNY
| Variable | N | Hazard ratio | 95% CI | p |
|---|---|---|---|---|
| Age | 1.01 | .97–1.04 | .770 | |
| Site type | ||||
| Urban (reference) | 806 | |||
| Rural | 535 | 1.02 | .82–1.28 | .858 |
| Sex | ||||
| Male (reference) | 992 | |||
| Female | 349 | .99 | .78–1.26 | .946 |
| Race-ethnicity | ||||
| Non-Hispanic white (reference) | 368 | .050 | ||
| Asian | 112 | 1.19 | .80–1.79 | .394 |
| Black (Non-Hispanic) | 489 | 1.00 | .76–1.31 | .974 |
| Hispanic | 355 | .89 | .65–1.20 | .431 |
| Other | 17 | 2.46 | .24–4.90 | .010 |
| Year of admission | ||||
| 2018 (reference) | 408 | .008 | ||
| 2013 | 24 | .58 | .23–1.44 | .240 |
| 2014 | 98 | .74 | .47–1.19 | .212 |
| 2015 | 140 | .74 | .49–1.12 | .148 |
| 2016 | 210 | .86 | .61–1.23 | .411 |
| 2017 | 461 | 1.23 | .92–1.65 | .162 |
TABLE 3.
Analysis of variables as predictors of early discharge among 1,349 clients of OnTrackNY, adjusted by site type, age, race-ethnicity, sex, and year of admission
| Variable | N | Hazard ratio | 95% CI | p |
|---|---|---|---|---|
| Highest education completed | ||||
| Less than high school (reference) | 384 | |||
| College or postgraduate degree | 150 | .91 | .58–1.43 | .683 |
| High school diploma or GED | 265 | .96 | .70–1.31 | .778 |
| Some college | 539 | .78 | .59–1.03 | .084 |
| Employed at admission | ||||
| No (reference) | 1,127 | |||
| Yes | 214 | 1.09 | .83–1.44 | .529 |
| Medication adherence | ||||
| Adherent (reference) | 949 | |||
| Not adherent | 190 | 1.86 | 1.42–2.42 | <.001 |
| Not prescribed | 70 | 1.97 | 1.33–2.92 | .001 |
| Unknown | 132 | 1.74 | 1.26–2.40 | .001 |
| Any substance use | ||||
| No (reference) | 650 | |||
| Yes | 691 | 1.17 | .94–1.44 | .152 |
| Cannabis use | ||||
| No (reference) | 801 | |||
| Yes | 540 | 1.37 | 1.11–1.70 | .004 |
| MIRECC-GAFa | ||||
| Symptoms | ||||
| Dichotomous | ||||
| Dysfunctional (<40) (reference) | 1,021 | |||
| Not dysfunctional (≥40) | 304 | 1.09 | .85–1.40 | .491 |
| Categorical | ||||
| Dysfunctional (reference) | ||||
| Borderline | 1,021 | 1.04 | .80–1.35 | .784 |
| Fully functional | 277 | 1.88 | .98–3.60 | .058 |
| Fully functional versus borderline | 27 | 1.81 | .92–3.56 | .084 |
| Social functioning | ||||
| Dichotomous | ||||
| Dysfunctional (<40) (reference) | 153 | |||
| Not dysfunctional (≥40) | 1,169 | .70 | .53–.94 | .016 |
| Categorical | ||||
| Dysfunctional (reference) | 153 | |||
| Borderline | 812 | .67 | .50–.90 | .008 |
| Fully functional | 357 | .80 | .57–1.12 | .186 |
| Fully functional versus borderline | 1.20 | .94–1.53 | .150 | |
| Occupational functioning | ||||
| Dichotomous | ||||
| Dysfunctional (<40) (reference) | 879 | |||
| Not dysfunctional (≥40) | 441 | .98 | .79–1.22 | .863 |
| Categorical | ||||
| Dysfunctional (reference) | 879 | |||
| Borderline | 322 | .84 | .65–1.08 | .173 |
| Fully functional | 119 | 1.42 | 1.02–1.98 | .036 |
| Fully functional versus borderline | 1.70 | 1.17–2.49 | .006 | |
| Self-injurious behavior | ||||
| No (reference) | 1,259 | |||
| Yes | 82 | 1.40 | .95–2.06 | .087 |
| Suicidal ideation or attempt | ||||
| No (reference) | 978 | |||
| Yes | 363 | 1.15 | .91–1.45 | .237 |
| Ever hospitalized | ||||
| No (reference) | 1,155 | |||
| Yes | 185 | .79 | .60–1.05 | .099 |
| Time to first service contact Living situation | 1.00 | 1.00–1.00 | .322 | |
| Parents (reference) | 1,108 | |||
| Alone | 63 | 1.87 | 1.24–2.82 | .003 |
| Nonparental family | 109 | 1.69 | 1.2–2.40 | .003 |
| Other | 60 | 1.43 | .90–2.26 | .130 |
| Has support person | ||||
| No (reference) | 100 | |||
| Yes | 1,241 | .72 | .50–1.03 | .073 |
| Family contact | ||||
| Daily | 1,210 | 1.54 | .86–2.75 | .150 |
| Monthly or less | 29 | 1.40 | .94–2.08 | .096 |
| Weekly (reference) | 82 | |||
| Homelessness in past 90 days | ||||
| No (reference) | 1266 | |||
| Yes | 74 | 1.42 | .95–2.13 | .087 |
| Health insurance | ||||
| Private (reference) | 509 | |||
| Other or unknown | 85 | 1.34 | .85–2.11 | .206 |
| Public | 677 | 1.24 | .98–1.58 | .79 |
| Uninsured | 70 | 2.56 | 1.71–3.82 | <.001 |
Possible scores on the three subscales (symptoms, social functioning, and occupational functioning) of the Mental Illness Research, Education and Clinical Center Global Assessment of Functioning scale (MIRECC-GAF) range from 0 to 100; scores <50 are considered in the impaired range while scores of ≥70 represent good functioning; scores categorized as a three-level variable: dysfunctional (<40), borderline (40–69), and fully functional (≥70).
Baseline MIRECC-GAF symptom scores were not significantly associated with discharge within the first year. However, higher baseline MIRECC-GAF social functioning scores were associated with a lower hazard of discharge, compared with lower scores (Table 3). For instance, individuals with a borderline score (score of 40–69) had a lower hazard, compared with those with a dysfunctional score (<40) (HR=0.67). When the MIRECC-GAF occupational functioning score was considered as a three-category variable, those with the highest baseline score (fully functional) had a higher hazard of discharge within the first year, compared with those with a dysfunctional score (HR=1.42) and those with a borderline score (HR=1.70). Overall, higher social functioning scores were associated with a lower likelihood of leaving OnTrackNY; in contrast, the highest category of scores (fully functional) in occupational functioning was associated with higher likelihood of leaving the program within a year, compared with the two lower score categories.
DISCUSSION
Early discharge rates in this study were somewhat similar to those reported in previous studies, which ranged from 12% to 56%, according to a recent systematic review (8). Prior research has noted substantial between-study heterogeneity in the way the outcome is conceptualized and measured (7, 8, 15), which makes comparison between studies challenging. This study adopted a pragmatic definition for early discharge, which was defined as clients who left the program within the first 12 months and, therefore, did not receive the recommended dose of treatment. However, it may be erroneous to assume that those who were discharged early “disengaged” from services, because individuals may leave treatment early for various reasons. For some, leaving treatment may reflect that services are not meeting their self-perceived needs; others may leave treatment because of the belief that treatment goals have been met or because of general life circumstances, such as moving away. Similarly, trajectories and prognosis associated with first-episode psychosis are notoriously heterogeneous, and “early” versus later discharge could also reflect differences in underlying psychopathology, including initial episodes of psychosis that completely resolve, leaving the individual without a need for care.
The main results of this study indicate that clients with poor clinician-rated medication adherence, no health insurance, and cannabis use and those who were living alone or with nonparental family at enrollment were at higher risk of discharge within the first 12 months. Moreover, scores on two of the three subscales (MIRECC-GAF-OF and MIRECC-GAF-SF) were associated with early discharge, when the measures were included as categorical variables with three levels of functioning. Specifically, those with higher social functioning were at lower risk of early disenrollment from OnTrackNY; however, higher occupational functioning was associated with a higher risk of leaving the program. This may indicate that individuals with high social functioning tend to stay in services for a longer period, but those with high occupational functioning may decide to leave early because they do not need services or are having trouble taking the time for EISs if they are otherwise busy with work or school. The reasons behind these findings, however, are not entirely clear, and further research is needed to unpack and understand this phenomenon with more nuance.
Most of the predictors of early discharge identified in our study are consistent with the literature and support our hypotheses, except for the association between health insurance and early discharge. The finding that lack of insurance was a predictor of early discharge might be particularly relevant to the way in which the mental health system is organized in the United States and may indicate that this decentralized approach negatively affects engagement in mental health treatment, even within a specialized service setting that serves people regardless of insurance status (11). Conversely, lack of insurance may reflect underlying disadvantage that drives both lack of access to insurance and heightened risk of dropout. However, this finding may not be replicable or relevant in contexts in which tax-funded, universal-coverage health care systems provide specialized care (e.g., the United Kingdom and Canada). Focusing on context-specific and health system–related predictors offers an opportunity for intervention, given that such factors can be targeted by introducing policies and other structural modifications.
Most research to date has explored early discharge based on clinicians’ ratings (7). It is known, nonetheless, that clients, providers, and even family members may have differing opinions and perspectives regarding engagement, participation in treatment, and satisfaction with services. Clients who have left particular programs before expected may say that these programs were not relevant for their needs and that they have had negative experiences with service providers; in contrast, mental health professionals may indicate that early discharge was mainly due to lack of insight, language and cultural barriers, and stigma (16). The divergent perceptions support the importance of examining these issues from different perspectives and triangulating the views of clients, relatives, and providers. In addition, we should assume that it may not be possible to engage all clients, even when working within a multifaceted, engagement-oriented program such as OnTrackNY. Clients need choices and make choices; they are not all the same, even when they have similar mental health conditions. Person-centered researchers have emphasized that there might be a lack of fit between what any given client wants and needs and what the service in question is providing (17). From this vantage point, expanded research concerning programmatic drivers of disengagement is critically important (18–20) to increase the appeal of mental health services.
This study expands the growing literature on specialized EISs for early psychosis. A major strength of this study was the inclusion of the largest sample to date of individuals receiving EISs within the United States. This is also one of the first studies to include health care–related predictors of early discharge, highlighting the relevance of understanding the impact of context-dependent factors. Our findings indicate that “positive” characteristics, such as higher occupational functioning, can also be associated with early discharge. This finding is not only new to the literature, but it may also help us reconceptualize the notion that early discharge is an exclusively negative outcome. Rather, it is possible that shorter or less intense early treatment might be indicated for a subgroup of individuals with early psychosis. Study limitations include lack of information about the reasons for discharge, about medications prescribed prior to 12 months ago, and about whether individuals sought alternative services to OnTrackNY. Early discharge was operationalized on the basis of clinicians’ ratings, which limited the nuances of the construct. In addition, time-varying predictors (e.g., medication adherence) were not considered, which should be taken into account when interpreting the findings over time.
CONCLUSIONS
The recent focus on expanding EIS programs nationally provides a rich opportunity for designing future research studies that help improve the field’s understanding of who benefits most from these programs, what intensity of services should be offered and for how long, and how to consider engagement and early discharge. A good first step is to more systematically characterize and operationalize early discharge and differentiate it from other related outcomes, such as disengagement or dropout, so that it can be studied in a more standardized manner to inform research and clinical practice. It is likely that very disparate constructs are currently being conflated and thus obfuscating findings. Standard operationalization might be achieved by bringing together different stakeholders (e.g., clients, relatives, and providers), reaching consensus, and defining a multifaceted and dimensional concept that reflects everyone’s point of view or by identifying differing constructs that can be parsed out and examined separately.
There should also be a focus on understanding individual reasons for leaving EIS programs, because this might provide us with new ways of understanding service pathways and the effectiveness of engagement strategies for different groups of people with early psychosis. Finally, there is a critical need to examine the effects of contextual and health care–related factors on early discharge from EISs. It is very probable that contextual factors related to accessibility of health services, local policies, and system-level issues affect an individual’s ability and desire to remain in EISs beyond their level of satisfaction with treatment.
HIGHLIGHTS.
Many individuals receiving early intervention services for psychosis leave treatment before expected.
This study identified predictors of early discharge ina large sample of individuals from an early intervention program in New York State.
Participants who at baseline had poor medication adherence, had no health insurance, were living alone or with nonparental family, or were using cannabis were at higher risk of early discharge.
Footnotes
The authors report no financial relationships with commercial interests.
Contributor Information
Franco Mascayano, Department of Epidemiology, Mailman School of Public Health, Columbia University, New York Division of Behavioral Health Services and Policies, New York State Psychiatric Institute, New York.
Els van der Ven, Department of Epidemiology, Mailman School of Public Health, Columbia University, New York School for Mental Health and Neuroscience, Maastricht University, Maastricht, Netherlands.
Gonzalo Martinez-Ales, Department of Epidemiology, Mailman School of Public Health, Columbia University, New York
Cale Basaraba, Division of Behavioral Health Services and Policies, New York State Psychiatric Institute, New York
Nev Jones, Department of Psychiatry and Behavioral Neurosciences, Morsani College of Medicine, University of South Florida, Tampa
Rufina Lee, Silberman School of Social Work, Hunter College, City University of New York, New York
Iruma Bello, Division of Behavioral Health Services and Policies, New York State Psychiatric Institute, New York
Ilana Nossel, Division of Behavioral Health Services and Policies, New York State Psychiatric Institute, New York
Stephen Smith, Division of Behavioral Health Services and Policies, New York State Psychiatric Institute, New York
Thomas E. Smith, Division of Behavioral Health Services and Policies, New York State Psychiatric Institute, New York
Melanie Wall, Division of Behavioral Health Services and Policies, New York State Psychiatric Institute, New York
Ezra Susser, Department of Epidemiology, Mailman School of Public Health, Columbia University, New York Division of Behavioral Health Services and Policies, New York State Psychiatric Institute, New York.
Lisa B. Dixon, Division of Behavioral Health Services and Policies, New York State Psychiatric Institute, New York
REFERENCES
- 1.Dixon LB, Goldman HH, Srihari VH, et al. : Transforming the treatment of schizophrenia in the United States: the RAISE initiative. Annu Rev Clin Psychol 2018; 14:237–258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Correll CU, Galling B, Pawar A, et al. : Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry 2018; 75:555–565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dixon LB, Holoshitz Y, Nossel I: Treatment engagement of individuals experiencing mental illness: review and update. World Psychiatry 2016; 15:13–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doyle R, Turner N, Fanning F, et al. : First-episode psychosis and disengagement from treatment: a systematic review. Psychiatr Serv 2014; 65:603–611 [DOI] [PubMed] [Google Scholar]
- 5.Jones N, Gius B, Daley T, et al. : Coordinated specialty care discharge, transition, and step-down policies, practices, and concerns: staff and client perspectives. Psychiatr Serv (Epub ahead of print, March 19, 2020) [DOI] [PubMed]
- 6.Lutgens D, Iyer S, Joober R, et al. : A five-year randomized parallel and blinded clinical trial of an extended specialized early intervention vs. regular care in the early phase of psychotic disorders: study protocol. BMC Psychiatry 2015; 15:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lal S, Malla A: Service engagement in first-episode psychosis: current issues and future directions. Can J Psychiatry 2015; 60: 341–345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mascayano F, van der Ven E, Martinez-Ales G, et al. : Disengagement from early intervention services for psychosis: a systematic review. Psychiatr Serv. In press 2020 [DOI] [PubMed]
- 9.O’Brien A, Fahmy R, Singh SP: Disengagement from mental health services: a literature review. Soc Psychiatry Psychiatr Epidemiol 2009; 44:558–568 [DOI] [PubMed] [Google Scholar]
- 10.Mascayano F, Nossel I, Bello I, et al. : Understanding the implementation of coordinated specialty care for early psychosis in New York state: a guide using the RE-AIM framework. Early Interv Psychiatry 2019; 13:715–719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bello I, Lee R, Malinovsky I, et al. : OnTrackNY: the development of a coordinated specialty care program for individuals experiencing early psychosis. Psychiatr Serv 2017; 68:318–320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nossel I, Wall MM, Scodes J, et al. : Results of a coordinated specialty care program for early psychosis and predictors of outcomes. Psychiatr Serv 2018; 69:863–870 [DOI] [PubMed] [Google Scholar]
- 13.Marino L, Scodes J, Ngo H, et al. : Determinants of pathways to care among young adults with early psychosis entering a coordinated specialty care program. Early Interv Psychiatry (Epub ahead of print, September 10, 2019) [DOI] [PubMed]
- 14.Niv N, Cohen AN, Sullivan G, et al. : The MIRECC version of the Global Assessment of Functioning Scale: reliability and validity. Psychiatr Serv 2007; 58:529–535 [DOI] [PubMed] [Google Scholar]
- 15.Reynolds S, Kim DJ, Brown E, et al. : Defining disengagement from mental health services for individuals experiencing first episode psychosis: a systematic review. Soc Psychiatry Psychiatr Epidemiol 2019; 54:1325–1335 [DOI] [PubMed] [Google Scholar]
- 16.Smith TE, Easter A, Pollock M, et al. : Disengagement from care: perspectives of individuals with serious mental illness and of service providers. Psychiatr Serv 2013; 64:770–775 [DOI] [PubMed] [Google Scholar]
- 17.van Os J, Guloksuz S, Vijn TW, et al. : The evidence-based group-level symptom-reduction model as the organizing principle for mental health care: time for change? World Psychiatry 2019; 18:88–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones N, Tyler D: Online Tutorial: Facilitating Meaningful Engagement of Young People and Their Families in Early Intervention Programs. Alexandria, VA, National Association of State Mental Health Program Directors, 2017. https://www.nasmhpd.org/content/online-tutorial-facilitating-meaningful-engagement-young-people-and-their-families-early [Google Scholar]
- 19.Jones N, Jimenez-Solomon O: Cultural and Structural Considerations for Addressing Psychosis in Young Adults. Research webinar. Rockville, MD, Substance Use and Mental Health Services Administration, Technical Assistance Network, 2019 [Google Scholar]
- 20.Jones N: Deconstructing the intersections of race/ethnicity and disadvantage on family and service user disengagement from early intervention services. Early Interv Psychiatry 2018; 12:80 [Google Scholar]


