Abstract
Novel coronavirus is a family of viruses that usually leads to respiratory illness. This coronavirus pandemic has affected human life drastically, and there is a chance that this virus persists on raw foods of animal origin. Also, food that is served to the customers by retail sectors passes through different operational steps, which involves multiple touchpoints by the food handlers on the surface of the food or to the food directly. This may lead to the spreading of the coronavirus through the food sector if proper hygiene, sanitization, and disinfection, social distancing, and other preventive measures are not followed. This chapter will give an overview of the type of foodborne viruses and their effects on human health. It will also provide an understanding of the possibilities of transmitting coronavirus disease (COVID-19) through food and food packaging. The review will also focus on the preventive measures, hygiene practices, and safety precautions that should be adopted by the food handlers or food business owners to mitigate the risk of transmitting COVID-19 in the food service and retail sector. Essential aspects of the food safety management system with respect to COVID-19 will be discussed, which should be followed by all the food companies. Finally, the role of different dietary supplements and bioactive ingredients of foods and herbs will be discussed that are known to improve the human immune system, which will fight against the virus.
Keywords: COVID-19, Dietary supplements, Food packaging, Food safety management, Personal hygiene and sanitization, Preventive measures
11.1. Introduction
Viruses are gaining particular interest in their behavior and are entirely different from bacteria. It has been noticed that most foodborne viruses are harmful in nature and cause a detrimental effect on human health. Viruses are microorganisms that are generally very small and tiny, having a diameter ranging from 0.02 to 0.4 μm, whereas bacteria usually range between 0.5 and 5 μm. Transmission of viruses to humans may happen in different ways, but most of the foodborne viruses are infected via the gastrointestinal tract and are excreted through feces or vomitus.1 Though the consumption of contaminated food has been clearly implicated as the source of viral infections, the proportion of infection that can be caused due to the consumption of the contaminated food is still an unknown fact. The most common food-induced viruses are noroviruses (NoV) and hepatitis A virus (HAV), which is a threat to human health worldwide. Some other viruses like rotaviruses, enteroviruses, and astroviruses are also considered critical foodborne viruses; however, to a lesser extent,2 , 3 vomiting and diarrhea are the most common symptoms of viral gastroenteritis, which may be severe to some extent and also causes death in a few cases.3
The name coronavirus came from the Latin word “corona,” which refers to “crown” or “halo” due to the morphological characterization of the virus. Very recently, a novel strain of coronavirus was identified. The current COVID-19 pandemic primarily originated in Wuhan, China.4, 5, 6, 7, 8 The initial infection was originated from a Wuhan seafood market where various types of seafood, as well as live animals, were sold. The seafood market was closed on January 1, 2020 when the initial two to three cases were identified from the same location. The infection started spreading very rapidly, and on January 21, 2020, the transmission of this virus from human to human was first reported by Chinese Health Authorities. As a result, case counts had increased rapidly and have spread all over the world in several countries.9
Though it is still unclear if the market is the original source of this virus, the spread of the virus was noticed to increase more rapidly due to the vast crowd and multiple touchpoints in the market area.10 Coronavirus (CoV) is thought to be zoonotic, which means it may pass from animals to humans, which generally happens if any infected animal is killed and the same is consumed.11
CoV has been identified in various animals such as bats, cats, rats, and chickens, which has been reported to cause respiratory tract and gastrointestinal diseases.12, 13, 14, 15, 16, 17 A new strain, namely severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has also been identified, which is a virus having positive-stranded RNA covered by a lipid bilayer.18 Pneumonia and fever are the common symptoms of coronavirus infections, the severity of which depends from person to person. Fever, cough, chest discomfort, and dyspnea are some of the clinical symptoms of these kinds of viruses.17 , 19 It has been reported that most of the transmission occurs by the spread of large droplets, which generates when a patient coughs or sneezes.20 , 21
The virus can also spread from the surfaces that are touched by some infected person, including food or food packaging.22 It may be that the food or the packaging has the virus on it, and when someone touches those infected packs and then touch their own body parts like mouth, nose, or eyes, the person may get infected with the virus. The chance of this virus getting transmitted through food is found to be less common than the transmission from one person to another.23 Even if contaminated food is consumed, there is no evidence that swallowing the contaminated food leads to any infection.24 The virus needs to be transmitted to the respiratory system—into the nose, sinuses, or lungs to act on the same and spread the infection. To follow good food safety practices, it is always important to wash hands with hand wash for at least 20 s or at least sanitize hands with 70% alcohol after handling any kind of packages or before preparing or eating food.25 This may reduce the risk of illness from common foodborne pathogens. It is also believed that properly cooked food may kill the virus.26
To manage food safety risks and also the chances of food contamination, the food industry should strictly follow the Food Safety Management Systems (FSMS) based on the Hazard Analysis and Critical Control Point (HACCP) principles.27 , 28 According to the FSMS, the prerequisite programs are mandatory requirements, which include good hygiene practices, cleaning, sanitation and sanitization, area zoning (high risk and low risk), supplier evaluation and control, storage, logistics and supply chain, housekeeping, personnel hygiene, and also medical checkup to ensures fitness.29 These are all part of Good Manufacturing Practices (GMP), which helps to control the hygiene at each stage of the food supply chain to prevent any type of food contamination. The employers should also have FSMS and HACCP team who will identify all the food safety–related risks and take necessary precautions to eliminate the same from the system.30 , 31 After the outbreak of this pandemic, there are additional requirements for the food industries which should be maintained effectively to prevent the spread of this virus and also to improve the hygiene and sanitization practices. Food industries should also implement policies as per ISO 22,00032 to protect food workers from getting affected by COVID-19 and also restrict the transmission of the virus by any means.33
There is a lot of interest to strengthen or boost immunity in the wake of the COVID 19 pandemic, which can be the first line of defense to fight against the virus. A well-balanced diet and being active physically and mentally can contribute to improve anyone’s immunity and lead a healthy life. Many natural ingredients are known to boost the immune system. Some herbs and spices have been well known since ancient times for their medicinal properties, particularly in Asia. According to the World Health Organization,34 herbal medicines are used as the primary health care by around 80% of the world’s population across Europe and South Asia. India is the hub for many herbs and spices that are used for making this traditional medicine. The herbs have antiinflammatory properties and also help in building natural immunity to overcome the adverse effects of COVID-19. Most of these herbs, such as basil, fenugreek, ginger, garlic, and turmeric, are safe to consume and do not have any side effects like allopathic medicines, e.g., antibiotics.26
The main objective of this review is to provide an overview of the most common foodborne viruses and their effects on human health. The possibilities of transmitting COVID-19 through food and food packaging will be discussed along with the precautionary measures to avoid the risk of transmission. This should be adopted by the food handlers or food business owners to mitigate the risk of transmitting COVID-19 in the foodservice and retail sector. The new requirements of the FSMS will be discussed, which needs to be implemented in all food-related industries and followed religiously. Finally, dietary supplements that provide essential sources of vitamins, minerals, zinc, etc. will be focused on to boost the immune system, which can help to fight the virus.
11.2. Viruses and their transmission
11.2.1. Foodborne viruses
Foodborne viruses are derived from the gastrointestinal tract of a human.37 These viruses are found in food and water as a result of poor hygiene practices, sewage systems, or contamination by food handlers. There are numerous viruses that are found in the human gut, among which only a few are reported as the most common foodborne pathogens, for example, NoV and HAV (Table 11.1 ).35, 36, 37 Rotaviruses (group B and C) and hepatitis E virus outbreaks also occur frequently due to food and water contamination. Among all these viruses, NoV causes infection in people irrespective of their ages and is considered to be the most common mode of foodborne infection worldwide. Studies report that NoV infection occurs highest in children but also occurs in adults.35 , 38 HAV is also a waterborne virus, which is known to occur in several countries.39 This virus is seen to be more active in developing countries rather than in undeveloped countries where it is less common. The infection very rarely occurs among young children in their early childhood and remains asymptomatic.4 However, most of the adults also remain susceptible to infection by HAV.2 , 40
Table 11.1.
List of foodborne viruses and their sources.
| Name of virus/Illness | Source of contamination | Transmission via food products |
|---|---|---|
| Hepatovirus A/Hepatitis A | Water, human stool | Meat, raw beef, shellfish, fruits, and vegetables |
| Orthohepevirus/Hepatitis E | Pork liver | Pork |
| Norovirus/Gastroenteritis | Water, food, human stool | Meat, berry fruit, oyster, and shellfish |
11.2.2. Coronavirus disease (COVID-19) transmission via food
It is very unlikely that humans can get infected with COVID-19 through food or its packaging.23 It causes respiratory illness, which is primarily transmitted through contact of one person to another and also by the spread of respiratory droplets that are generated through coughs/sneezing droplets produced by the infected person and reaches the nose, mouth, or eyes of the other person.41
To date, there is no report or evidence available, which confirms that COVID-19 is transmitted via food or its associated packaging.23 This virus cannot grow in food, and they need an animal or human host to grow and multiply. The source of the COVID-19 is understood to be animals, but the exact source is still unknown to all. However, studies have shown that low temperature has a significant influence on the persistence of SARS-CoV-2 and other coronaviruses. It has been reported that the virus remains actively stable in frozen and refrigerated food.42 The virus is known to be transmitted through droplets of infected persons, which may be present in the air and is a result of sneezing or touching an infected surface, e.g., doorknobs or shaking hands with the infected person and then touching their own face. Recent studies reported that the virus remains viable for up to 72 h on plastic material and stainless steel, up to 4 hours on copper, and up to 24 h on cardboard.43 , 44
In some cases, there may be cases who are asymptomatic and do not show any signs or symptoms of the disease at all or at a very mild level. However, asymptomatic infected people also are capable of spreading the virus.45 This proves that the practice of personal hygiene and appropriate use of PPE is compulsory for all who work in the food industry, irrespective of their outward health condition. To maintain a virus-free working environment, food business owners should introduce very high-level security and staff management, which should include temperature monitoring, sickness reporting, sanitization, and so forth.46, 47, 48, 49
11.3. Nanotechnology-based active and intelligent packaging on combating COVID-19
Although we are now aware that transmission of COVID-19 through food is not reported by any researchers, there is a chance that the virus can survive on the surface of the package, which in turn can pass from one person to the other during the entire supply chain. The development of polymers or biopolymers with antiviral properties can lead to an area of interest for scientists to minimize the risk of spreading COVID-19 through the food packaging material.50 The spread of viruses like HAV and human norovirus (HuNoV) have already been shown to be controlled through various polymers and biopolymers, which contain the antiviral agent.37 Warnes et al.51 reported that polymers developed with copper had released the copper ions which helped in inactivating the HuCoV-229E virus on copper surfaces. van Doremalen et al.52 recently observed that SARS-CoV-2 is most stable and sustained on copper and plastic surfaces and the viability of the virus could be detected up to 72 h. Some other studies showed that the use of nanomaterial coatings or films containing copper, silver, and zinc nanoparticles has the capability to fight against SARS-CoV-2 which prevented the contamination of food packaging material and reduces the transmission of the virus (Fig. 11.1 ).53
Figure 11.1.
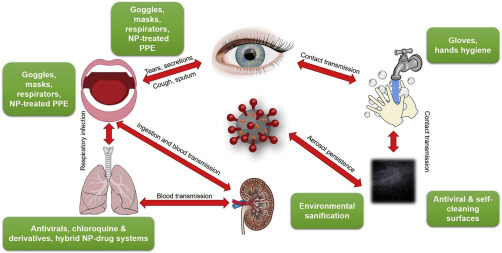
Transmission pathways of SARS-CoV-2. NP, nanoparticle; PPE, personal protective equipment.
This figure is reproduced with permission from Sportelli.32
11.4. Food safety management system during COVID-19
During the COVID-19 situation, the FSMS should be reviewed by all the food business owners or food packaging-related industries where the implementation of different policies should be documented and the effectiveness to be monitored on a regular basis.29 Defined or specific food safety HACCP should be in place for managing the emergency situations like COVID-19 outbreak. Following initiatives to be taken by all industries to maintain the Food Safety and Quality Management system.32 , 54
11.4.1. Internal audits
An internal audit program should be conducted to review the changes that have been introduced due to the response of the COVID-19 pandemic. Personal hygiene policy and facility housekeeping policies should be of greater emphasis. A remote site audit can be performed to maintain social distancing norms. There may be a need for emergency supplier approval for raw materials/packaging materials because of the shortage of material production at the supplier end due to fewer available workers or plant shutdowns. In such cases, before approving the alternate supplier, a remote/virtual audit should be conducted and observations to be recorded to overcome the shortage of supplies from the approved suppliers and to ensure continuity of production. However, this may include increased risk, which needs to be managed by the food safety and HACCP team.32 , 55
For food-related raw materials, the risk of allergens, the shelf life of the product, potential fraud or substitution, and product specification should be given more importance during the audit. For changing the packaging material suppliers, it is essential to understand if there are any differences in specification between the new and former product. The review should be focused more on the migration of chemicals into food (where there is direct food contact), product shelf life, product stability during storage, and transport.56
11.4.2. Site security and food defense
11.4.2.1. Temporary workers
It is very likely that during the COVID-19 crisis, all manufacturing sites will have a shortage of workers, and they need to make temporary arrangements for workers or increase the working hours due to production demand and slower line speeds. An alternate arrangement of temporary workers may increase the potential risk of the site. There may be violation of site policies, for instance, secret filming on phones or passing confidential data or chances of sabotage-related issues.57 Site visitor’s access to the site needs to be reviewed and may be restricted during the period of COVID-19. Acceptance of visitors to the site should be defined, which should cover general visitors, service providers including pest control, service engineers, laundry services, courier agency, vehicle drivers and emergency services. Health declaration to be taken from all types of visitors before giving access to the site.29
11.4.2.2. Entry-exit policy
The entry-exit policy should be reviewed and necessary changes to be implemented following personal hygiene, and also to ensure protection from any kind of allergen or microbial cross-contamination. Sickness reporting methodologies should be part of the daily training and monitoring. The movement of people from one area to the other should be restricted and should not be compromised.56
11.4.2.3. Maintenance
Planned preventive maintenance programs should be reviewed and implemented to run the plant without any unacceptable risk of breakdown. The shutdown of machines and equipment should be planned well in advance to meet the production requirement without any downtime or loss in production.58
11.4.3. Staff facilities
Changing areas and locker rooms should be designed in such a way that there is effective social distancing maintained at peak times, especially during the start and end of the shift. Additional space for changing or storage should be provided so that there is no person-to-person contact and also to confirm that the safety aspect is not compromised. Personal protective equipment (PPE) should be issued to all workers, and if required, additional PPEs also may be provided during this pandemic.59 Mostly disposable PPEs are advisable; however, if any PPE is expected to reissue, there should be a provision that those are cleaned appropriately after use, it is numbered for easy identification and traceability, and last but not least, clean and hygienic storage areas should be available to store the PPE between shifts. Hand washing and sanitizing activity is always on high priority in food factories. Management should ensure hands are washed periodically, followed by sanitization.60 Sanitizers should be provided in abundant quantity and placed near each and every work station. Frequency of handwashing and sanitization should be defined for proper effectiveness; wherever possible, automated soap/sanitizer dispensers should be used to avoid direct contact.27
11.4.4. Housekeeping and hygiene practices
Cleaning frequency should be increased with particular attention to direct touchpoints like doors, handles, etc. The effectiveness of cleaning equipment should be monitored during the start and end of every shift to avoid any type of cross-contamination.61 Specific cleaning or fumigation should be done if any employee is detected with COVID-19 at the workplace to ensure the safety of other employees. The pest management program should also be in place and a record to be maintained.30 , 37 , 63, 62
11.4.5. Vulnerability assessment/fraud prevention
It has been noticed that whenever there is a shortage of supply in materials, there is a rise in price for the raw materials, which increases the risk of fraudsters entering the market with substituted products at a very reasonable rate and also false claims. It is very important to verify all the details if the management decides to buy raw materials from alternative sources. All the technical terms and conditions to be evaluated and potential risk should be assessed to prevent any fraud.64
The site should closely monitor and evaluate the suppliers and also review the risk rating and contingency plan to increase testing or inspection procedures to identify the appropriate risk of the materials.55
11.4.6. Personnel
As already mentioned, during the COVID-19 crisis, it is very likely that due to sickness and self-isolation during this pandemic, there will be a shortage of workers for which additional employees are appointed for meeting the requirements. Safety and security should be ensured by the owners as well as monitoring or surveillance system should be strong to ensure that there is no fraud or sabotage during any phase of the entire supply chain.65
11.4.7. Training
It is particularly important that training is provided for all new and temporary employees taken on, which should additionally include all practices which should include personal hygiene procedures, entry-exit practices, social distancing, allergen management, sickness reporting, and so forth, which are specially implemented for COVID-19.66 Sickness reporting is the crucial component that is included as one of the new procedures which will reduce the risk of spreading COVID-19. This is mainly for the safety of all employees (permanent and temporary workers), which should be monitored and a record maintained.67
11.4.8. Medical screening
Medical screening should be done for the COVID-19 affected employee after his/her return to work. COVID negative test report to be provided to ensure there is no more infection, which should be communicated to all other employees for their safety.67 Management should ensure all employees get proper treatment and medical facilities to combat and overcome the situation.66
11.5. Precautionary measures to control COVID-19 in the food sector
The spread of the COVID-19 virus in the foodservice sector can be controlled by following the below precautionary measures. This will also ensure food safety requirements and will be beneficial for all individuals. The preventive measures, hygiene practices, and safety precautions should be adopted by the food handlers or food business owners to mitigate the risk of transmission of COVID-19.24 , 68 , 102
11.5.1. Hand hygiene
Human hands are the primary source of spreading this virus.69 Foodservice operation activities directly involve touching the food or through the food packaging material (utensils, trays, packets/pouches, etc.). Nonfood surfaces like door handles, doorbells, handrails, etc., also come in contact during the supply chain. Hence maintaining hygiene practices by the food handlers is very important for their daily operation.37
As per the Centers for Disease Control and Prevention (CDC), washing hands frequently with soap for a minimum of 20 s and sanitization by 70% alcohol is the most essential and critical step to mitigate the risk of spreading the coronavirus during the foodservice operation.39 In addition to the above precautions, food handlers should also maintain hygiene in the kitchen to wash and sanitize hands frequently, especially after a bio break.70 Appropriate PPE like gowns, gloves, masks, hair nets, etc., to be provided to all employees who need to be changed as and when necessary to prevent the spreading of any germs.59 Hands should also be washed and gloves should be changed in case of handling raw meat or poultry products after coughing/sneezing or blowing the nose. Once the disposable gloves, gowns, hair nets, shoe covers are used, those should be scrapped appropriately and the record maintained.71
11.5.2. Sanitization process
Sanitizers are the agents that are used to minimize the microbial load from the environment or contact surface to an acceptable level, which has been given by the different organizations and as per food safety regulation.70 There are different sanitizers and disinfectants which should be used by the food handlers for different applications at various concentrations as per the severity of the infection that can be spread by the coronavirus.74, 73, 72
Surfaces that directly comes in contact with the food should be sanitized frequently to prevent and reduce the transmission of coronavirus. Before and after each use of the food-contact surfaces, food handlers should follow the proper cleaning and sanitization practices once every 2 h, especially during this pandemic.75 It has been reported that the use of sodium hypochlorite at 50–100 ppm concentration is the most effective and cheaper sanitizer, which is mostly used in various industries for disinfecting food contact surfaces.25 , 76 Surfaces like doors, chairs, tables, etc. which are nonfood, should also be sanitized at regular intervals with an appropriate concentration of sanitizer.61
In the retail sector, fresh produce is sold as cut fruits and vegetables in a packaged container. For this, the fruits and vegetables are manually cut, washed, and cleaned before packing the same in containers.77 In such cases, there is a considerable chance of contamination as there are multiple touchpoints. Hence, food handlers should ensure that the fruits and vegetables are cut, maintaining all hygiene practices like using clean hands, sanitized cutting boards, knives, and sanitization of the containers/packages before packing to eliminate the risk of spreading of COVID-19 through surfaces and equipment.78
11.5.3. Social distancing
Maintaining social distance is an essential and crucial guideline that will help to slow down the risk of COVID-19 spread from one person to another. CDC and other food safety authorities have clearly recommended that a space of at least 2 m should be maintained in the workplace or in public.79 , 80 Food handlers need to strictly follow the same and limit the presence of workers in close contact during the working hours at the workplace, especially where food is prepared in the kitchen or packed in a particular area which will curtail the hazard of spreading COVID-19.81 The employees should avoid gathering at one place during a shift change, tea breaks, and training, and should always maintain a safe distance.37
11.5.4. Temperature monitoring
All food sectors should follow temperature monitoring by trained/skilled personnel at the workplace by using thermometer guns or infrared thermometers while each person enters the premises and also at an interval of 4 h in between their job.82 If fever is found to be 100.4°F or higher, the employee should be sent back and not allowed to perform the job until he/she is found to be fit.83
Employers/the owners should revise the sick leave policies on account of COVID-19 and extend support to their staff to ensure that they get sufficient time to take care of and recover from the virus infection. Full recovery from COVID-19 is mostly found to be around 14–21 days depending on the patient’s immunity, physical health, and, most notably, the severity of the infection.80 , 84 All those employees along with their family members who are detected as COVID-19 positive should stay at home in quarantine until they recover fully and test negative.85 , 86 Symptoms such as coughing, shortness of breath, loss of smell, and fever are mostly observed as symptoms of COVID-19;87 if anyone seems to have any of the above symptoms should stay at home until the time they are free from the usual symptoms. If any food worker is tested COVID-19 positive, the employer should inform all the stakeholders, quarantine the infected person as well as associated workers who came in contact with him in the last two to three days. The company should also provide necessary support to the affected person’s family in whatever way possible.88
11.5.5. Customer safety
Due to the COVID-19 outbreak, people have restricted themselves from going out to restaurants. To attract customers and also to provide no-contact service, many restaurants are now offering no-contact ordering of food and also home delivery to reduce the risk of transmission. Nowadays, contactless deliveries are encouraged by most people than dine-in. All food business operators should maintain and abide by all rules and regulations following food safety authorities to continue their business.89
It has been directed that hand sanitizers should be available in sufficient quantities at entrances and also in the waiting lounge of restaurants. Dining room tables and chairs should be sanitized after each use. High touchpoints like doors, restrooms, and computers should be frequently cleaned and sanitized.61 Contactless orders should be taken through weblink or mobile apps. Social distancing should be maintained between each table so that the virus spread is less even during peak hours. Handling of cash/cards should be avoided and contactless payment gateways to be introduced without which there may be a chance of spreading the new coronavirus.90
11.6. Bioactive compounds and their role in the prevention of coronavirus
World Health Organization (WHO) has declared COVID-19 as a pandemic worldwide. It is clear that people all over the world are at high risk due to the community transmission of this virus; however, individuals can take few essential measures that may help them to fight against this pandemic.37
The effect or risk of getting affected with COVID-19 is much higher in people having some preexisting diseases or comorbidities like diabetes, cancer, hypertension, cardiac problems, and respiratory illness.93, 92, 91 The risk level is also high for elderly people as immunity, in general, reduces as we grow older. In the younger generation, if someone is a nonsmoker, COVID 19 may result in a minor infection due to the immunity which helps to combat the virus. Below are some of the measures which we can undertake to improve our immunity. Galanakis et al.93 has explained in detail the role of food ingredients and bioactive compounds like bioactive peptides, polysaccharides, bioactive lipids, and natural polyphenols, which help in improving the immune system and prevention from COVID 19.94
11.6.1. Diet and supplements to boost immunity
The food we eat plays a crucial role in our overall health and immunity. During this pandemic, a low carbohydrate diet and high protein diet is advised by many physicians to keep the balance (Fig. 11.2 ).95 Consumption of fruits and vegetables will boost up immunity, which is usually rich in beta carotene, ascorbic acid, and other vitamins. Also, foods cooked with mushrooms, tomatoes, and other green vegetables are very good options to build flexibility to fight against any kind of bacterial or viral infections. It is also recommended to consume food that includes whole grains, legumes, nuts, and animal source foods.95
Figure 11.2.
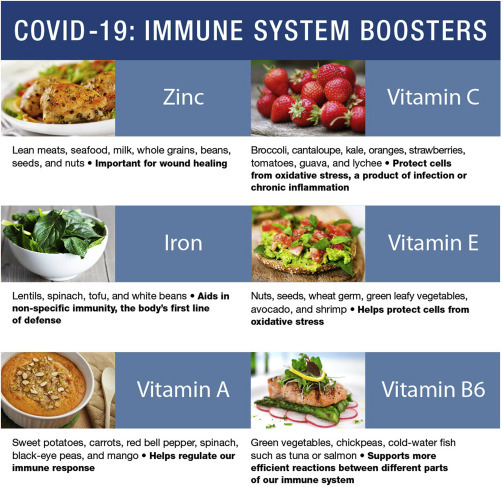
Foods as immune boosters.
Image has been reproduced from an open access webpage published by Albin,45 hence no permission required.
Supplements rich in omega 3 and 6 fatty acids and also known as some natural immunity boosters like ginger, gooseberries (amla), and turmeric, which can be a part of our daily diet. Several herbs like garlic, black cumin, and different kinds of nuts are known to help in boosting immunity and are excellent sources of protein and vitamin E. Yogurt and fermented foods should also be included in the regular diet. Apart from the above-mentioned diets, few common supplements can be used, which are known to boost immunity and also to fight against the COVID-19 virus.34
Vitamin C is considered to be a very crucial supplement in boosting immunity. It is well known to prevent the common cold and also acts as an antioxidant that defends against any kind of damage occurred due to oxidative stress. For severe infections like sepsis and acute respiratory distress syndrome (ARDS), a high dose of intravenous vitamin C has shown significant improvement in managing the symptoms in patients.96
In our present lifestyle and also due to the current pandemic situation, everyone is mostly staying at home and not having any exposure to sunlight, which in turn is resulting in a deficiency of vitamin D. Additional supplements of vitamin D are seen to control respiratory tract–related illness. Most people nowadays are deficient in vitamin D, and doctors suggest taking a supplement of vitamin D, which will help to improve the immune system. Food sources of vitamin D are fatty fishes, fish liver oils, cheese, and egg yolks. Fortified foods with vitamin D can also be chosen as an alternative source of vitamin D.96
Zinc is essential for white blood corpuscles (WBC), which helps to fight against viral infections. Consumption of zinc supplements improves immunity, which makes people less susceptible to cold, cough, and other viral infections.97
The berries and flowers of elderberry contain many antioxidants and vitamins that are very important in boosting our immune system. It is known to ease cold and flu, fight against influenza, lessen stress, inflammation, and also to protect from heart-related diseases. Elderberries contain very important nutrients and minerals like phosphorus, potassium, iron, copper, vitamins, proteins, and dietary fiber. It is also known to have antibacterial and antifungal properties.98
Functional food plants like garlic, tea, ginger, turmeric, pomegranate, black pepper, and honey possess immunomodulatory and antiviral properties, which are known to improve immunity in various ways, keeping away common cold and flu.99
Garlic has been known as the best for its antiviral properties and herbal remedies from ancient days. Several sulfur-containing compounds, like sulfoxide, proteins, and polyphenols, are present in garlic, which strengthens the immune system. Best results are observed when crushed garlic is consumed with honey.100 , 101
11.7. Conclusion
The COVID-19 disease resulted in a huge outbreak of respiratory illness, which originated from China. The food operators or food business owners should follow all the general hygiene rules to mitigate the risk of transmission of COVID-19 in the retail sector. Precautionary measures like hand sanitization, social distancing, personal hygiene, and contactless approaches should be maintained so that transmission does not happen from one person to another. All food business owners should strictly abide by the FSMS. Dietary supplements such as vitamin C, zinc, probiotics, and other compounds are known to boost immunity, which will reduce the risk of getting affected by COVID-19 or any other virus easily. More research needs to be conducted on novel approaches like the introduction of nanofibers, nanomaterials, and bioactive compounds over the conventional practices of overcoming such pandemic situations and ensuring food safety.
Acknowledgments
Continuous support and infrastructural facility provided to the first author from ALPLA India Pvt. Ltd., Regional Head Quarters, Hyderabad, is acknowledged with thanks.
The infrastructural support provided to the second author by FORE School of Management, New Delhi, in completing this Book Chapter is gratefully acknowledged.
References
- 1.CDC . June 1, 2020. How COVID-19 spreads? Last reviewed. [Google Scholar]
- 2.Koopmans M., Duizer E. Foodborne viruses: an emerging problem. Int J Food Microbiol. 2004;90(1):23–41. doi: 10.1016/S0168-1605(03)00169-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bosch A., Gkogka E., Le Guyader F.S., Loisy-Hamon F., Lee A., van Lieshout L. Foodborne viruses: detection, risk assessment, and control options in food processing. Int J Food Microbiol. 2018;28:110–128. doi: 10.1016/j.ijfoodmicro.2018.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S.M., Lau E.H.Y., Wong J.Y., Xing X., Xiang N., Wu Y., Li C., Chen Q., Li D., Liu T., Zhao J., Liu M., Tu W., Chen C., Jin L., Yang R., Wang Q., Zhou S., Wang R., Liu H., Luo Y., Liu Y., Shao G., Li H., Tao Z., Yang Y., Deng Z., Liu B., Ma Z., Zhang Y., Shi G., Lam T.T.Y., Wu J.T., Gao G.F., Cowling B.J., Yang B., Leung G.M., Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jalava K. First respiratory transmitted foodborne outbreak? Int J Hyg Environ Health. 2020;226:113490. doi: 10.1016/j.ijheh.2020.113490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO) 2020. 2019-nCoV situation reports.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports [Google Scholar]
- 7.WHO . March 19, 2020. Critical preparedness, readiness and response actions for COVID-19: interim guidance.https://www.who.int/publications-detail/critical-preparedness-readiness-and-response-actions-for-covid-19 [Google Scholar]
- 8.WHO . February 2020. World Health Organization. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19) pp. 16–24.https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf [Internet], Geneva. [Google Scholar]
- 9.Naserghandi A., Allameh S.F., Saffarpour R. All about COVID-19 in brief. New Microb New Infect. 2020;35:100678. doi: 10.1016/j.nmni.2020.100678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W., Si H.R., Zhu Y., Li B., Huang C.L., Chen H.D., Chen J., Luo Y., Guo H., Jiang R.D., Liu M.Q., Chen Y., Shen X.R., Wang X., Zheng X.S., Zhao K., Chen Q.J., Deng F., Liu L.L., Yan B., Zhan F.X., Wang Y.Y., Xiao G.F., Shi Z.L. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang L.F., Shi Z., Zhang S., Field H., Daszak P., Eaton B.T. Review of bats and SARS. Emerg Infect Dis. 2006;12:1834–1840. doi: 10.3201/eid1212.060401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holmes K.V., Lai M.M.C. Coronaviridae: the viruses and their replication. Fields Virol. 1996;3:1075–1093. [Google Scholar]
- 13.van der Hoek L., Pyrc K., Jebbink M.F., Vermeulen-Oost W., Berkhout R.J., Wolthers K.C., Wertheim-van Dillen P.M.E., Kaandorp J., Spaargaren J., Berkhout B. Identification of a new human coronavirus. Nat Med. 2004;10(4):368–373. doi: 10.1038/nm1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Monchatre-Leroy E., Boue F., Boucher J.M., Renault C., Moutou F., Ar Gouilh M., Umhang G. Identification of alpha and beta coronavirus in wildlife species in France: bats, rodents, rabbits, and hedgehogs. Virus. 2017;9(12):364. doi: 10.3390/v9120364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rodriguez-Morales A.J., Bonilla-Aldana D.K., Balbin-Ramon G.J., Rabaan A.A., Sah R., Paniz-Mondolfi A., Pagliano P., Esposito S. History is repeating itself: probable zoonotic spillover as the cause of the 2019 novel Coronavirus Epidemic. Infez Med. 2020;28(1):3–5. [PubMed] [Google Scholar]
- 16.Dhama K., SharunK, Tiwari R., Sircar S., Bhat S., Malik Y.S., Singh K.P., Chaikumpa W., Bonilla-Aldana D.K., Rodriguez-Morales A.J. Coronavirus disease: COVID-19. Clin Microbiol. 2019;33(4) doi: 10.1128/CMR.00028-20. e00028-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55:105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baranwal A., Mahato K., Srivastava A., Maurya P.K., Chandra P. Phytofabricated metallic nanoparticles and their clinical applications. RSC Adv. 2016;6(107):105996–106010. [Google Scholar]
- 21.Centers for Disease Control and Prevention [CDC] CDC; Atlanta: 2020. How coronavirus spreads. [Google Scholar]
- 22.Klein G. Spread of viruses through the food chain. Dtsch Tierarztl Wochenschr. 2004;111:312–314. [PubMed] [Google Scholar]
- 23.European Food Safety Authority [EFSA] Parma; EFSA: 2020. Coronavirus: no evidence that food is a source or transmission route. [Google Scholar]
- 24.Oakenfull R.J., Wilson A.J. Food Standards Agency; London: 2020. Qualitative risk assessment: what is the risk of food or food contact materials being A source or transmission route of SARS-CoV-2 for UK consumers? [Google Scholar]
- 25.Environmental Protection Agency List N . Environmental Protection Agency; Washington, DC: 2020. Disinfectants for use against SARS-CoV-2. [Google Scholar]
- 26.Harapan H., Itoh N., Yufika A., Winardi W., Keam S., Te H. Coronavirus disease 2019 (COVID-19): a literature review. J Infect Public Health. 2020;13:667–673. doi: 10.1016/j.jiph.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Djekic I., Tomasevic I., Radovanovic R. Quality and food safety issues revealed in certified food companies in three Western Balkans countries. Food Control. 2011;22(11):1736–1741. [Google Scholar]
- 28.Tomasevic I., Kuzmanović J., Anđelković A., Saračević M., Stojanović M.M., Djekic I. The effects of mandatory HACCP implementation on microbiological indicators of process hygiene in meat processing and retail establishments in Serbia. Meat Sci. 2016;114:54–57. doi: 10.1016/j.meatsci.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 29.BSI Group . 2020. Safe working during the covid-19 pandemic- general guidelines for organizations. Version 1. [Google Scholar]
- 30.CAC . 2003. Recommended international code of practice general principles of food hygiene. CAC/RCP 1-1969. [Google Scholar]
- 31.Dzwolak W. HACCP in small food businesses – the Polish experience. Food Control. 2014;36(1):132–137. [Google Scholar]
- 32.ISO Standard 22000 . Edition: 2. 2018. Food safety management systems — requirements for any organization in the food chain; p. 37. [Google Scholar]
- 33.Galimberti A., Cena H., Campone L., Ferri E., Dell’Agli M., Sangiovanni E. Rethinking urban and food policies to improve citizens safety after COVID-19 pandemic. Front Nutr. 2020;7(181) doi: 10.3389/fnut.2020.569542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WHO . 2020. Europe. WHO European Region – food and nutrition tips during self-quarantine.www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid 19/publications-and-technical-guidance/noncommunicable-diseases/food-and-nutrition-tips-during-self-quarantine [Google Scholar]
- 35.Codex Alimentarius . FAO/WHO; Rome, Italy: 1999. Committee on food hygiene, discussion paper on viruses in food. FAO/WHO document CX/FH99/11. [Google Scholar]
- 36.Yekta R., Dastjerdi L.V., Norouzbeigia S., Mortazavianb A.M. Food Control; 2020. Food products as potential carriers of SARS-CoV-2. Published online on 11th November, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ceylan Z., Meral R., Cetinkaya T. Relevance of SARS-CoV-2 in food safety and food hygiene: potential preventive measures, suggestions and nanotechnological approaches. Virus Dis. 2020;31(2):154–160. doi: 10.1007/s13337-020-00611-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Codex Alimentarius . 2020. Food hygiene: basic texts.http://www.fao.org/3/a1552e/a1552e00.pdf Accessed 10-Sep-20. [Google Scholar]
- 39.Mast E.E., Alter M.J. Epidemiology of viral hepatitis. Semin Virol. 1993;4:273–283. [Google Scholar]
- 40.Pintó R.M., Saiz J.C. In: Human Viruses in Water. Perspectives in Medical Virology Series. Zuckerman A.J, Mushahwar I.K., editors. Vol. 17. Elsevier; Amsterdam, The Netherlands: 2007. Enteric hepatitis viruses; pp. 39–67. [Google Scholar]
- 41.The Lancet . 2019. Infectious diseases challenges of coronavirus disease. Lancet Infect. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Han J., Zhang X., He S., Jia P. Can the coronavirus disease be transmitted from food? A review of evidence, risks, policies and knowledge gaps. Environ Chem Lett. 2021:5–16. doi: 10.1007/s10311-020-01101-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thippareddi H., Balamurugan S., Patel J., Singh M., Brassard J. Coronaviruses – potential human threat from foodborne transmission? Lebensm Wiss Technol (Food Sci) 2020:134–110147. doi: 10.1016/j.lwt.2020.110147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Food and Drug Administration [FDA] FDA; White Oak Campus: 2020. Food safety and the coronavirus disease 2019 (COVID-19) [Google Scholar]
- 45.Kaul D. An overview of coronaviruses including the SARS-2 coronavirus - molecular biology, epidemiology and clinical implications. Cur Med Res Pract. 2020;10:54–64. doi: 10.1016/j.cmrp.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yu P., Zhu J., Zhang Z., Han Y. A familial cluster of infection associated with the 2019 novel coronavirus indicating possible person-to-person transmission during the incubation period. J Infect. 2020;221(11):1757–1761. doi: 10.1093/infdis/jiaa077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pan X., Chen D., Xia Y., Wu X., Li T., Qu X., Zhou L., Liu J. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. Lancet Infect Dis. 2020;20(4):410–411. doi: 10.1016/S1473-3099(20)30114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tong Z.D., Tang A., Li K.F., Li P., Wang H.L., Yi J.P., Zhang Y.L., Yan J.B. Potential presymptomatic transmission of SARS-CoV-2, Zhejiang Province, China. Emerg Infect Dis. 2020;26(5) doi: 10.3201/eid2605.200198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kimball A., Hatfield K.M., Arons M., James A., Taylor J., Spicer K., Bardossy A.C., Oakley L.P., Tanwar S., Chisty Z., Bell J.M., Methner M., Harney J., Jacobs J.R., Carlson C.M., McLaughlin H.P., Stone N., Clark S., Brostrom-Smith C., Page L.C., Kay M., Lewis J., Russell D., Hiatt B., Gant J., Duchin J.S., Clark T.A., Honein M.A., Reddy S.C., Jernigan J.A. Asymptomatic and Presymptomatic SARS-CoV-2 Infections in residents of a long-term care skilled nursing facility — King County, Washington. Morb Mortal Wkly Rep (MMWR) 2020;69(13):377–381. doi: 10.15585/mmwr.mm6913e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Randazzo W., Fabra M.J., Falcó I., López-Rubio A., Sánchez G. Polymers and biopolymers with antiviral activity: potential applications for improving food safety. Compr Rev Food Sci. 2018;17:754–768. doi: 10.1111/1541-4337.12349. [DOI] [PubMed] [Google Scholar]
- 51.Warnes S.L., Summersgill E.N., Keevil C.W. Inactivation of murine norovirus on a range of copper alloy surfaces is accompanied by loss of capsid integrity. Appl Environ Microbiol. 2015;81(3):1085–1091. doi: 10.1128/AEM.03280-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.van Doremalen N., Bushmaker T., Morris D., Holbrook M., Gamble A., Williamson B., Lloyd‐Smith J. Aerosol and surface stability of HCoV‐19 (SARS‐CoV‐2) compared to SARS‐CoV‐1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sportelli M.C., Longano D., Bonerba E., Tantillo G., Torsi L., Sabbatini L., Cioffi N., Ditaranto N. Electrochemical preparation of synergistic nanoantimicrobials. Molecules. 2020;25:49. doi: 10.3390/molecules25010049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.WHO . April 07, 2020. COVID-19 and food safety: guidance for food businesses: interim guidance. [Google Scholar]
- 55.Foundation FSSC 22000 . 2020. Scheme documents, verson 5. Issued on November, 2020, Netherlands. [Google Scholar]
- 56.Nakat Z., Bou-Mitri C. COVID-19 and the food industry: readiness assessment. Food Control. 2021;121:107661. doi: 10.1016/j.foodcont.2020.107661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Szymendera S.D., OSHA . Occupational Safety and Health Administration, Department of Labor’s; April 6, 2020. Interim guidance for workers and employers of workers at increased risk of occupational exposure. [Google Scholar]
- 58.Ong S.W., Tan Y.K., Chia P.Y., Lee T.H., Ng O.T., Wong M.S., Marimuthu K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. J Am Med Assoc. 2020;323(16):1610–1612. doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.WHO . 2020. Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages. [Google Scholar]
- 60.WHO. WHO save lives: clean your hands in the context of Covid 19. Rome, Italy: World Health Organisation & Food and Agriculture Organization of the United Nations.
- 61.CDC . April 1, 2020. Cleaning and disinfection for community facilities. [Google Scholar]
- 62.BRC global standard for food safety. BRC Trading Ltd; London, UK: 2018. Issue: 8. [Google Scholar]
- 63.IFS . IFS Management GmbH; Berlin, Germany: 2017. IFS Food, version 6.1. [Google Scholar]
- 64.CISA . March 19, 2020. Guidance on the essential critical infrastructure workforce. [Google Scholar]
- 65.Duda-Chodak A., Lukasiewicz M., Zię´c G., Florkiewicz A., Filipiak-Florkiewicz A. Covid-19 pandemic and food: present knowledge, risks, consumers fears and safety. Trends Food Sci Technol. 2020;105:145–160. doi: 10.1016/j.tifs.2020.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.CDC . May 2020. Businesses and employers responding to coronavirus disease 2019 (COVID-19): interim guidance. [Google Scholar]
- 67.CDC . March 11, 2020. Check and record everyday (CARE) [Google Scholar]
- 68.Bilal M., Nazir M.S., Parra-Saldivar R., Iqbal H.M. 2019-nCoV/COVID-19 approaches to viral vaccine development and preventive measures. J Pure Appl Microbiol. 2020;14(1):25–29. [Google Scholar]
- 69.CDC . May 17, 2020. Hand hygiene recommendations. [Google Scholar]
- 70.Kampf G., Todt D., Pfaender S., Steinmann E. Review: persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104:246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.CDC . 2020. Human coronavirus types.www.cdc.gov/coronavirus/types.html Retrieved from: Accessed 7-Oct-20. [Google Scholar]
- 72.Fraser A.M., Pascall M.A. 2010. Cleaning and sanitization of food-contact surfaces in retail/food service establishments.http://www.foodsafetymagazine.com Available online at: Accessed 12-Nov-20. [Google Scholar]
- 73.EPA frequent questions about disinfectants and coronavirus (COVID-19). United states environmental protection agency. April 29, 2020. [Google Scholar]
- 74.EPA . May 28, 2020. List N: disinfectants for use against SARS-CoV-2. United states environmental protection agency. [Google Scholar]
- 75.CDC . April 28, 2020. Cleaning and disinfecting your facility. [Google Scholar]
- 76.Fukuzaki S. Mechanisms of actions of sodium hypochlorite in cleaning and disinfection processes. Biocontrol Sci. 2006;11(4):147–157. doi: 10.4265/bio.11.147. [DOI] [PubMed] [Google Scholar]
- 77.Yépiz-Gómez M.S., Gerba C.P., Bright K.R. Survival of respiratory viruses on fresh produce. Food Environ Virol. 2013;5:150–156. doi: 10.1007/s12560-013-9114-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sapers G.M. Efficacy of washing and sanitizing methods for disinfection of fresh fruit and vegetable products. Food Technol Biotechnol. 2001;39(4):305–311. [Google Scholar]
- 79.Gov U. K . May 11, 2020. Working safely during COVID-19 in factories, plants and warehouses. [Google Scholar]
- 80.IDFA . March 31, 2020. Emergency prevention measures to achieve physical (social) distancing in food manufacturing facilities as related to COVID-19. [Google Scholar]
- 81.WHO . April 22, 2020. COVID-19 and Food Safety: guidance for competent authorities responsible for national food safety control systems in Interim guidance. [Rome, Italy] [Google Scholar]
- 82.FBIA . March 30, 2020. Screening food industry employees for COVID-19 symptoms or exposure. [Google Scholar]
- 83.ILO. International Labor Organization . 2020. The six-step COVID-19 business continuity plan. April 1, 2020. [Google Scholar]
- 84.FBIA . March 25, 2020. FBIA’s food industry recommended protocols when employee/visitor/customer test positive for COVID-19. [Google Scholar]
- 85.WHO . May 10, 2020. Contact tracing in the context of COVID-19. [Google Scholar]
- 86.Zhang H., Chen R., Chen J., Chen B. COVID-19 Transmission within a family cluster in Yancheng, China. Front Med. 2020;7:387. doi: 10.3389/fmed.2020.00387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bienkov A. 2020. Coronavirus: loss of smell and taste may be hidden symptom of COVID-19 – business insider. [Google Scholar]
- 88.Olaimat A.N., Shahbaz H.M., Fatima N., Munir S., Holley R.A. Food safety during and after the era of COVID-19 pandemic. Front Microbiol. 2020;11:1854. doi: 10.3389/fmicb.2020.01854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rizou M., Galanakis I.M., Aldawoud T.M.S., Galanakis C.M. Safety of foods, food supply chain and environment within the COVID-19 pandemic. Trends Food Sci Technol. 2020;102:293–299. doi: 10.1016/j.tifs.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.CDC . 2020. Workplaces and businesses, considerations for restaurant and bar operators. USA department of health and human services. Accessed on 26th December. [Google Scholar]
- 91.Sampath Kumar N.S., Chintagunta A.D., Jeevan Kumar S.P., Roy S., Kumar M. Immunotherapeutics for Covid-19 and post vaccination surveillance. 3 Biotech. 2020;10(12):527. doi: 10.1007/s13205-020-02522-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Singh S., Prakash C., Ramakrishna S. Three-dimensional printing in the fight against novel virus COVID-19: technology helping society during an infectious disease pandemic. Technol Soc. 2020;62:101305. doi: 10.1016/j.techsoc.2020.101305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Djekic I., Nikolić A., Uzunović M., Marijke A., Liu A., Han J., Brnčić M., Knežević N., Papademas P., Lemoniati K. Covid-19 pandemic effects on food safety—multi-country survey study. Food Control. 2021;122:107800. doi: 10.1016/j.foodcont.2020.107800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Galanakis C.M., Aldawoud T.M.S., Rizou M., Rowan N.J., Ibrahim S.A. Food ingredients and active compounds against the coronavirus disease (COVID-19) pandemic: a comprehensive review. Foods. 2020;9:1701. doi: 10.3390/foods9111701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Albin J. UT Southwestern Medical Centre; Dallas: 2020. Quarantine cuisine: easy meals to support a healthy immune system. COVID; prevention.https://utswmed.org/medblog/easy-immune-boosting-food-covid19/ [Google Scholar]
- 96.Shakoor H., Feehan J., Al Dhaheri A.S., Ali H.I., Platat C., Ismail L.C., Apostolopoulos V., Stojanovskaa L. Immune-boosting role of vitamins D, C, E, zinc, selenium and omega-3 fatty acids: could they help against COVID-19? J Maturitus. 2021;143:1–9. doi: 10.1016/j.maturitas.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kumar A., Kubota Y., Chernov M., Kasuya H. Potential role of zinc supplementation in prophylaxis and treatment of COVID-19. Med Hypotheses. 2020;144:109848. doi: 10.1016/j.mehy.2020.109848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hawkins J., Baker C., Cherry L. Black elderberry (Sambucus nigra) supplementation effectively treats upper respiratory symptoms: a meta-analysis of randomized, controlled clinical trials. Compl Ther Med. 2019;42:361–365. doi: 10.1016/j.ctim.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 99.Arshad M.S., Khan U., Sadiq A., Khalid W., Hussain M., Yasmeen A., Asghar Z., Rehana H. Coronavirus disease (COVID‐19) and immunity booster green foods: a mini review. Food Sci Nutr. 2020;8(8):3971–3976. doi: 10.1002/fsn3.1719. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 100.Sahoo B.M., Banik B.K. Medicinal plants: source for immunosuppressive agents. Immunol: Curr Res. 2018;2:106. [Google Scholar]
- 101.Anywar G., Kakudidi E., Byamukama R., Mukonzo J., Schubert A., Oryem‐Origa H. Medicinal plants used by traditional medicine practitioners to boost the immune system in people living with HIV/AIDS in Uganda. Eur J Integr Med. 2019;35:101011. [Google Scholar]
- 102.WHO . 07 April 2020. COVID-19 and food safety: Guidance for food businesses: Interim guidance. [Google Scholar]


