Abstract
Background:
Periodontal regeneration remains one of the crucial issues in the field of periodontology. Periodontal intrabony defects could be treated by surgical intervention through various alloplastic bone graft substitutes. The Food and Drug Administration approved, Novabone putty is one of the recently marketed bone graft substitutes, which has been used in the present study. This study also incorporates the placement of platelet-rich fibrin (PRF) in combination with Novabone putty.
Materials and Methods:
Twenty patients were included in the study and were allocated to either Group A or Group B through randomization. Group A included the placement of Novabone putty in the periodontal intrabony defects, whereas Group B included the placement of Novabone putty along with PRF. Statistical analysis of plaque index, gingival index, probing pocket depth, relative attachment level, and intraoral periapical radiographs was performed.
Results:
Statistical more significant difference (P < 0.05) in probing pocket depth, and relative attachment level was observed in Group B (Novabone putty and PRF) in comparison to Group A (Novabone putty).
Conclusion:
Evaluation of efficacy of Novabone putty along with PRF produced more favorable results in relative attachment level gain and more reduction in probing pocket depth when compared to Novabone putty alone.
Keywords: Chronic periodontitis, novabone putty, platelet-rich fibrin
Introduction
Periodontitis is an inflammatory disease characterized by the destruction of the periodontium as a response to insults elicited by microbial accumulations on tooth surfaces. These responses tend to result in a variety of intraosseous defects of various architecture.[1]
The primary goal of periodontal therapy is to decrease the progression of periodontal disease to maintain natural dentition in health and function. This goal can be accomplished by nonsurgical therapy in patients with mild-to-moderate periodontitis, whereas in advanced cases, particularly in the presence of intrabony defects, surgical procedures that regenerate the supporting periodontal tissues may be employed.[2]
Bone replacement grafts or bone grafts are graft substitutes that provide a structural framework for clot development, remodeling, and maturation and aids in supporting bone formation in osseous defects. Ideal characteristics of bone replacement grafts are: nontoxic, nonantigenic, resistant to infection, strong and resilient no root resorption or ankylosis, easily adaptable, minimal surgical procedure, ready, and sufficiently available to stimulate new attachment and also able to trigger osteogenesis, cementogenesis, and formation of a functional periodontal ligament. In the league to restore lost attachment, a variety of materials have been investigated. Numerous studies have shown varying degrees of success through the implantation of different forms of bone. The ideal bone replacement graft material among all has always been autogenous bone, which was first used for reconstructing osseous defects produced by periodontal disease by Hegedus in 1923. Although autogenous bone grafts have always been considered as the gold standard for grafting procedures, their difficulty in procurement and the need for an additional surgical site limits its use. These considerations prompted the search for the substitute of autogenous grafts, which led to the development of alloplastic materials that are biocompatible, biodegradable, possess the good osteogenic potential and are readily available. Alloplasts are synthetic, inorganic, biocompatible, and bioactive bone graft substitutes, which promote healing through osteoconduction.[2]
A new kind of putty formulation of bioactive glass with glycerin and polyethylene glycol as an additive, which is the Food and Drug Administration approved for orthopedic and dental use is presently being marketed as Novabone Putty, which enhances the handling characteristics and may augment graft solidity by not allowing migration of graft particles from the defect site [Figure 1].[3]
Figure 1.

Novabone putty
Novabone putty is an osteoconductive bioactive device used for grafting osseous defects. It is a premixed composite of bioactive calcium phosphosilicate particulate and a synthetic, absorbable binder. The bioactive particulate is composed solely of elements that occur naturally in normal bone (Ca, P, Na, Si, O). The absorbable binder consists of polyethylene glycol and glycerin. Platelet-rich fibrin (PRF), was developed in France by Choukroun et al. in 2001 is a second-generation platelet concentrate which accelerates soft- and hard-tissue healing. PRF is a strictly autologous fibrin matrix containing a large quantity of platelets and leukocyte cytokines.[4]
Therefore, this study pertaining to this new combination of putty and PRF compares with putty alone is an attempt to evaluate the regenerative properties of novabone putty with or without PRF.
Materials and Methods
This randomized control trial was carried out in the Department of Periodontics and Implantology. Depending on the prevalence obtained in the pilot study, 95% confidence interval, 5% allowable error, and 80% power of the study, a sample size of 20 patients was estimated to be included in the study.
Inclusion criteria
Patients between the age group 25 and 55 years, who were diagnosed with chronic generalized periodontitis as per 1999 classification of periodontal diseases and conditions, with probing pocket depth of ≥5 mm in one or more teeth with radiographic evidence of vertical bone loss, without any history of systemic disease with minimum 28 teeth present in the oral cavity were included in this study.
Exclusion criteria
Patients showing unacceptable oral hygiene during presurgical (Phase I) period, pregnant women and lactating mothers, smokers, patients undergoing active orthodontic treatment, patients with systemically compromised status were excluded.
Study design
Written informed consent form explaining the nature of the study and surgical procedure were signed by each patient.
Before 4–6 weeks of surgical intervention, each patient received initial periodontal therapy with scaling and root planning, oral prophylaxis, and oral hygiene instructions. Patients selected were subjected to the assessment of plaque index (Silness and Loe, 1964), gingival index (Loe and Silness, 1963), probing pocket depth [using UNC-15 probe with occlusal stent-Figure 2], probing depth = fixed reference point to base of pocket – fixed reference point to the gingival margin, relative attachment level [using UNC-15 probe with occlusal stent-Figure 2], and intraoral periapical radiographs. Intraoral periapical radiograph of each defect site was exposed using a long cone paralleling technique. Exposures were made using Kodak E speed films at 70 kVp, 8 mA, 0.6 s with grids. Grids were used as a fixed reference point for the evaluation of bone fill.
Figure 2.
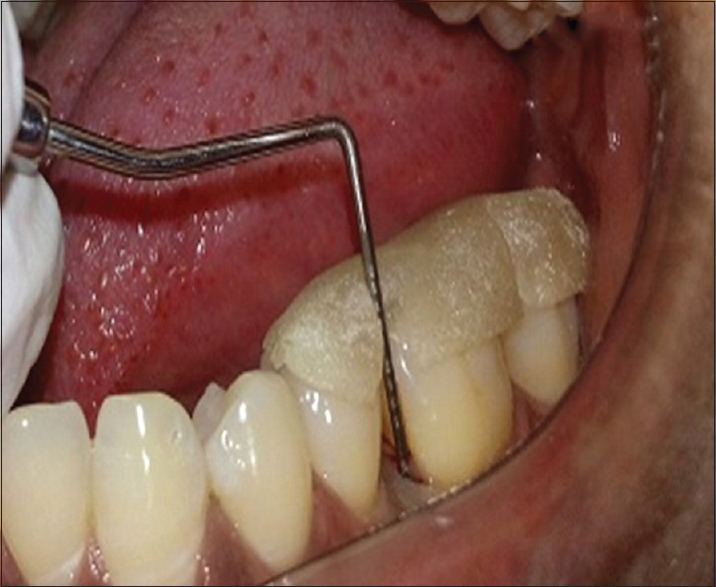
Probing pocket depth measurement using UNC-15 probe with occlusal stent
Criteria for measurement on the radiograph
The landmarks cementoenamel junction and base of the defect were marked on the image of the radiograph. The following radiographic parameters were recorded at baseline, 3 months, and 6 months postsurgery.
Do: Distance from cementoenamel junction to the base of the defect (baseline)
D3: Distance from cementoenamel junction to the base of the defect (3 months)
D6: Distance from cementoenamel junction to the base of the defect (6 months).
At 3 months,
Percentage of original defect resolved =
At 6 months
Percentage of original defect resolved = .
.
Linear measurements were made for pre- and post-operative radiographs; the landmarks cementoenamel junction and base of the defect were marked and the distance from cementoenamel junction to the base of the defect were measured in mm and with these measurements the defect fill was calculated using AUTO-CAD 2010 version software.
Preparation of platelet-rich fibrin
The required quantity of blood is drawn into 10-ml sterile test tubes without an anticoagulant and centrifuged immediately. Blood is centrifuged for 10 min at 3000 rpm.
The resultant product consists of the following three layers: top-most layer consisting of acellular platelet poor plasma, PRF clot in the middle, red blood cells at the bottom. PRF can be obtained in the form of a membrane by squeezing out the fluids in the fibrin clot [Figure 3].[5]
Figure 3.
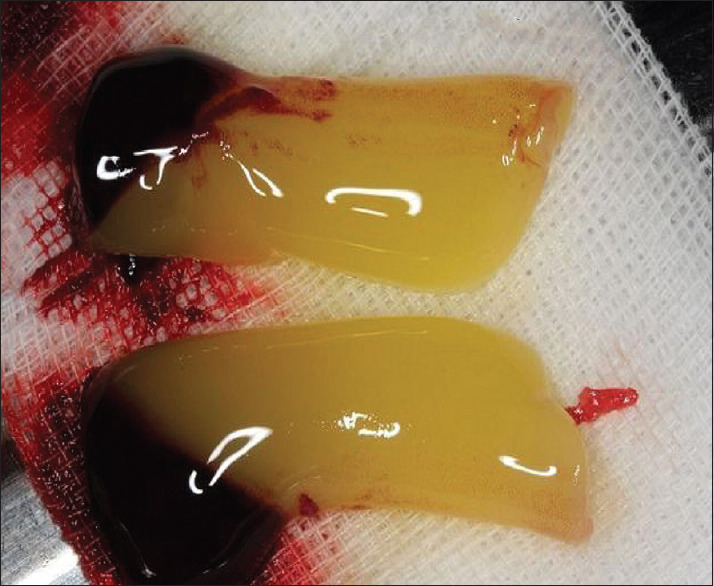
Prepared platelet rich fibrin
Surgical protocol
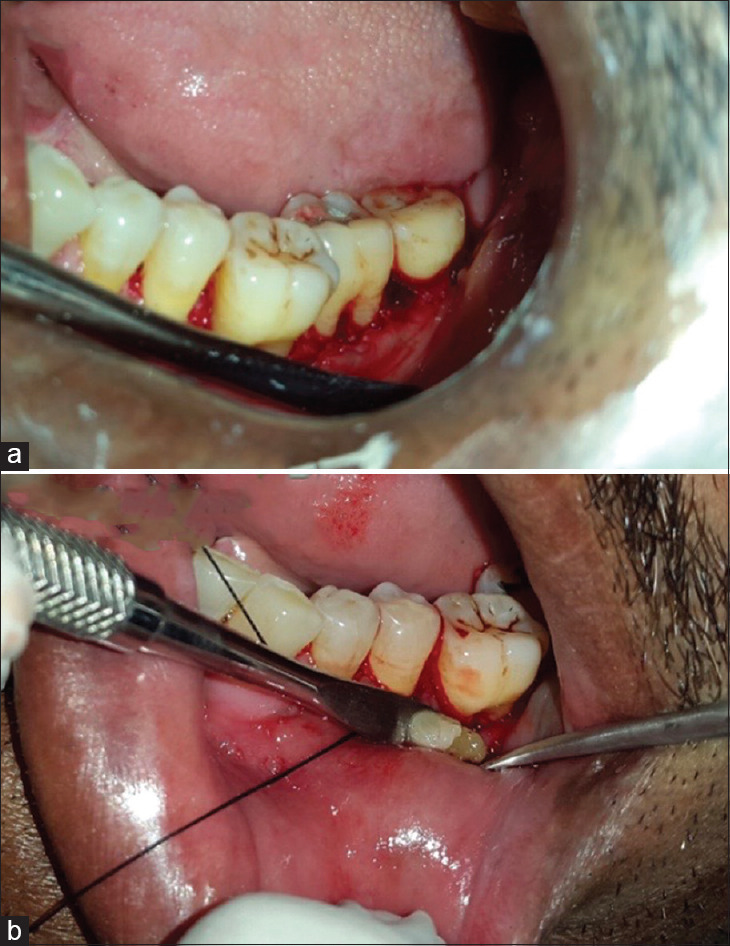
The selected sites were randomly assigned to Group A or Group B by tossing a coin, and the surgeries were performed by a single surgeon. Following adequate local anesthesia, crevicular incisions were placed and the defect site was exposed by the reflection of full-thickness mucoperiosteal flap. The three-walled defects in which all the three bony walls are present and the tooth constitutes the fourth wall were debrided of granulation tissue followed by thorough root planning and irrigation with normal saline. In Group A, the defect was filled with novabone putty [Figure 4]. In Group B, the defect was filled with PRF along with novabone putty [Figure 5]. The mucoperiosteal flaps were repositioned and secured in place using black braided (3-0) interrupted silk sutures to obtain primary closure of the interdental space and protected with a periodontal dressing [Figure 6].
Figure 4.
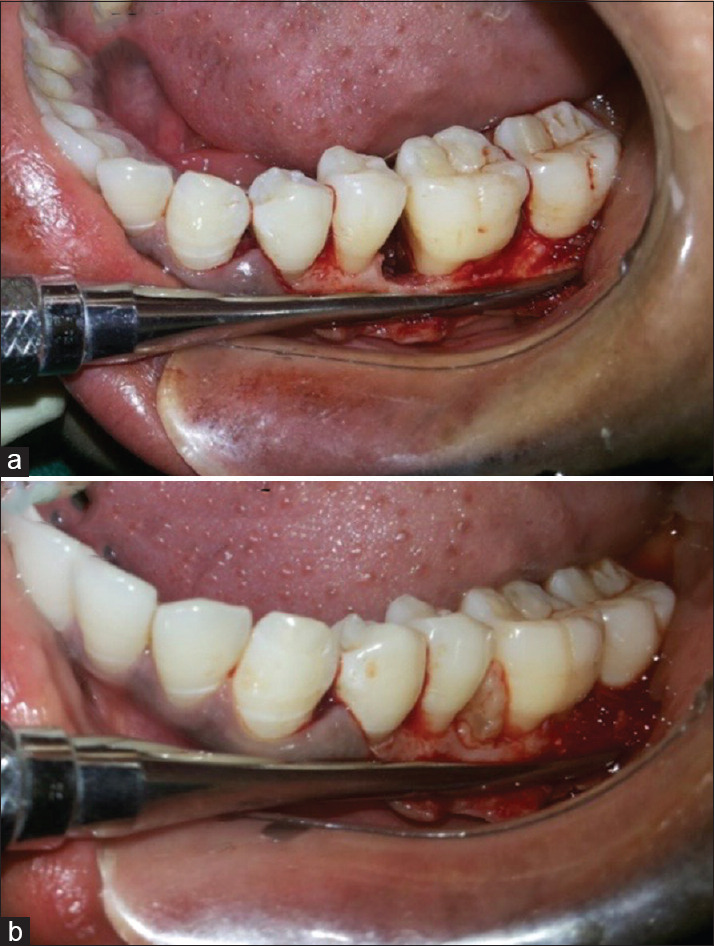
(a) Open flap debridement (Group A). (b) Placement of Novabone putty (Group A)
Figure 5.
(a) Open flap debridement (Group B). (b) Placement of Novabone putty with platelet rich fibrin (Group B)
Figure 6.
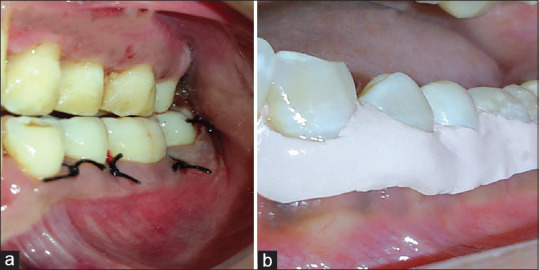
(a) Sutures given (b) periodontal dressing given
All postoperative instructions and medications were prescribed to each patient.
Postsurgical protocol
After 1 week following surgery, the dressing and sutures were removed, and surgical site was irrigated thoroughly with saline. At the end of 3 and 6 months posttherapy, patients were evaluated clinically and radiographically [Figures 7 and 8].
Figure 7.
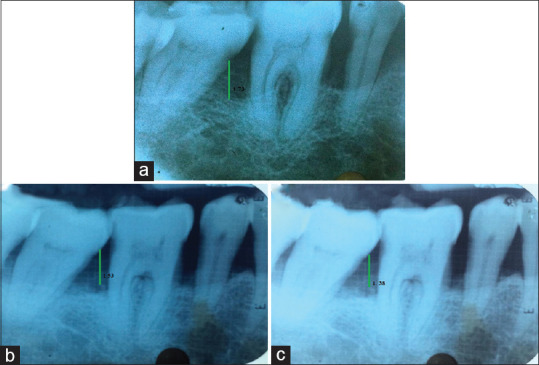
Radiographs of Group A (a) at baseline (b) at 3 months (c) at 6 months
Figure 8.
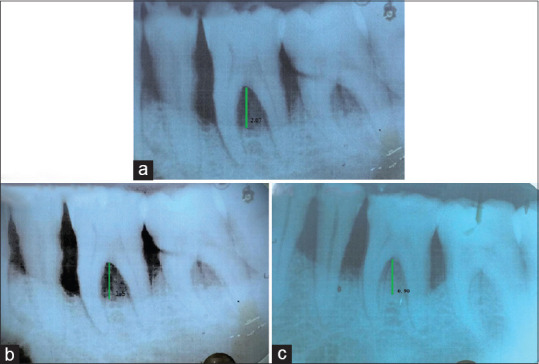
Radiographs of Group B (a) at baseline (b) at 3 months (c) at 6 months
Statistical analysis
The statistical analysis was performed with software SPSS 18 for windows. Student's t-test for the continuous variables and two-tailed Fisher's exact test or Chi-square test for categorical variables were used for analysis. The critical levels of significance of the results were considered at 0.05 levels, i.e., P < 0.05 was considered statistically significant.
Results
The purpose of this study was aimed to evaluate the regenerative properties of novabone putty with and without PRF in the treatment of human periodontal osseous defects.
The mean plaque index, gingival index, probing pocket depth, relative attachment level, and radiographic changes at baseline, 3 months, and 6 months are given in Table 1.
Table 1.
Comparison of mean index values between the groups at different time interval
| Index | Time period | Mean±SD |
t-test, P | |
|---|---|---|---|---|
| Group A | Group B | |||
| Plaque index | Baseline | 1.51±0.33 | 1.37±0.33 | 0.93, >0.05 |
| 3 months | 1.03±0.25 | 0.95±0.23 | 0.72, >0.05 | |
| 6 months | 0.90±0.21 | 0.84±0.20 | 0.63, >0.05 | |
| Change | 0.61±0.54 | 0.53±0.48 | 2.47, <0.05* | |
| Gingival Index | Baseline | 1.33±0.30 | 1.30±0.27 | 0.225, >0.05 |
| 3 months | 0.72±0.23 | 0.74±0.24 | 0.194, >0.05 | |
| 6 months | 0.86±0.20 | 0.85±0.17 | 0.102, >0.05 | |
| Change | 0.61±0.57 | 0.56±0.49 | 2.05, <0.05* | |
| Probing pocket depth | Baseline | 6.90±0.87 | 7.60±1.50 | 1.27, >0.05 |
| 3 months | 5.70±1.25 | 5.90±1.28 | 0.35, >0.05 | |
| 6 months | 5.40±0.51 | 5.00±0.94 | 1.18, >0.05 | |
| Change | 1.50±0.527 | 2.60±0.84 | 3.50, <0.05* | |
| Relative attachment level | Baseline | 12.60±2.27 | 11.30±3.05 | 1.08, >0.05 |
| 3 months | 11.40±2.67 | 9.80±2.44 | 1.40, >0.05 | |
| 6 months | 11.10±2.02 | 9.50±1.43 | 2.04, <0.05* | |
| Change | 1.50±0.84 | 1.80±0.52 | 2.11, <0.05* | |
| Radiographic depth of defect | Baseline | 6.10±0.76 | 6.23±0.66 | 0.39, >0.05 |
| 3 months | 5.12±0.61 | 5.11±0.75 | 0.02, >0.05 | |
| 6 months | 4.15±0.70 | 4.17±0.58 | 0.06, >0.05 | |
| Change | 1.95±0.46 | 2.05±0.57 | 0.64, >0.05 | |
*Significant. SD: Standard deviation
The mean plaque and gingival index values show statistically significant improvement in both groups [Table 1 and Graph 1].
Graph 1.
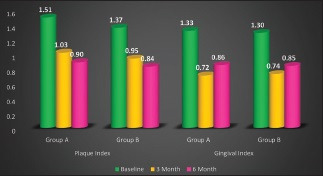
Plaque and gingival index values at different time intervals in both groups
There was a significant decrease in mean Probing pocket depth and relative attachment level in both Group A and B from baseline to 6 months and more decrease was observed in Group B as compared to Group A [Table 2 and Graph 2]. The radiographic depth of defect in both Group A and B shows a significant decrease from baseline to 6 months, but there were nonsignificant decrease in the radiographic defect in Group A as compared to Group B [Table 2 and Graph 2].
Table 2.
Comparison of mean index values between different time intervals within each group
| Index | Time period | Mean±SD |
P | ||
|---|---|---|---|---|---|
| Baseline | 3 months | 6 months | |||
| Plaque index | Group A | 1.51±0.33 | 1.03±0.25 | 0.90±0.21 | 0.01* |
| Group B | 1.37±0.33 | 0.95±0.23 | 0.84±0.20 | 0.01* | |
| Gingival index | Group A | 1.33±0.30 | 0.72±0.23 | 0.86±0.20 | 0.01* |
| Group B | 1.30±0.27 | 0.74±0.24 | 0.85±0.17 | 0.01* | |
| Probing pocket depth | Group A | 6.90±0.87 | 5.70±1.25 | 5.40±0.51 | 0.01* |
| Group B | 7.60±1.50 | 5.90±1.28 | 5.00±0.94 | 0.01* | |
| Relative attachment level | Group A | 12.60±2.27 | 11.40±2.67 | 11.10±2.02 | 0.01* |
| Group B | 11.30±3.05 | 9.80±2.44 | 9.50±1.43 | 0.01* | |
| Radiographic depth of defect | Group A | 6.10±0.76 | 5.12±0.61 | 4.15±0.70 | 0.01* |
| Group B | 6.23±0.66 | 5.11±0.75 | 4.17±0.58 | 0.01* | |
*ANOVA, significant. SD: Standard deviation
Graph 2.
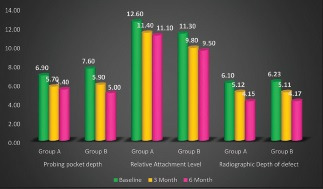
Different index values at different time intervals in both groups
Discussion
The main objective of periodontal therapy is to control periodontal infection and regenerate lost periodontal structures. It is challenging to achieve complete regeneration of periodontium after various periodontal treatment modalities because of variations in the healing abilities of periodontal tissues.[6] The present study evaluates the clinical efficacy of novabone putty in combination with PRF in the treatment of human intrabony periodontal defects and shows statistically significant improvement in clinical and radiographic parameters.
Bioactive glasses are alloplastic materials and are claimed to act by osteoconduction and/or osteopromotion.[7] Bioglass particulate exhibits enhanced new bone formation many times faster than hydroxyapatite.[8] Novabone putty being an osteoconductive bioactive material that can be used for grafting osseous defects, is a premixed composite of bioactive calcium phosphosilicate particulate matter. There were superior results found when comparing bioactive glass with hydroxyapatite with respect to bone and cementum formation.[9] Novabone putty was also found to be more effective in retarding epithelial downgrowth when compared to the hydroxyapatite group.[10] Novabone putty being an osteoconductive bioactive material that can be used for grafting osseous defects, is a premixed composite of bioactive calcium phosphosilicate particulate matter.
Bioactive glass is shown to be hemostatic, anti-inflammatory, and anti-microbial. Bioactive glass putty form has been shown to be hemostatic, decreasing clotting time in lab tests by 25% when compared to controls. This is due to the development of a positive surface charge that forms on the Bioglass after implantation and release of calcium ions during material dissolution. Calcium ions are needed during several steps in intrinsic and extrinsic clotting pathways and therefore are also required in the maturation of the fibrin network formed during clotting. There is continued physical presence of the bioglass particles, which stabilizes the formed clot and encourages more rapid site vascularization and provides an active scaffold for bone regeneration.[9]
The inflammatory response in host tissue can reduce local pH to 5.5 or lower due to the release of various enzymes in the process of phagocytosis. This acidic pH damages the surrounding tissues and has an impact to prolong the healing process. Since bioactive glass leaches out cations into the surrounding tissues, it negates the acidic pH hence, decreases the inflammation.[8]
PRF represents a new step in the platelet gel therapeutic concept with simplified processing without any artificial biochemical modification. Choukroun's PRF, is a platelet concentrate of the second generation, which consists of a mature union of cytokines, structural glycoproteins, and glycanic chains embedded within an extensive polymerized fibrin network.[5]
The PRF production protocol aims to accumulate platelets and released cytokines in a fibrin clot. Although platelets and leukocyte cytokines play a crucial part in the biology of this biomaterial, the fibrin matrix supporting them certainly constitutes the main determining portion responsible for the real therapeutic benefit of PRF.[5]
In this study, clinical parameters were compared and an attempt was also made to compare the results radiographically. The clinical parameters were measured at the baseline, 3, and 6 months follow-up period. The clinical assessment included soft tissue as well as hard tissue parameters.
Comparison of the arithmetic determination in this study with those reported in other similar studies is difficult due to the lack of data reported and/or lack of specific explanations regarding measurement calculations. There was a statistically significant reduction in the Plaque and gingival Scores from baseline to 3 and 6 months in both the groups. Probing pocket depth measurements are of prime importance in evaluating the success of periodontal therapy as it directly relates to the ability of the patient to maintain adequate plaque control. Statistically significant reduction in the probing depths was observed in both the groups. Observations indicate that Group A demonstrated less reduction in the probing depths as compared to Group B at 6 months interval, but it was statistically significant with t value 3.50.
The study demonstrated a statistically significant increased gain in the attachment levels in both groups. This gain in relative attachment level from baseline to 6 months postoperatively was more for Group B as compared to Group A after 6 months. The comparable attachment gain in Group A could be attributed to the formation of the long junctional epithelium instead of increased bone fill and tissue repair, as seen in Group B.
Measurement of bone fill: comparative analysis of mean change in defect fill for both the groups were done, which revealed mean defect depth for Group A at baseline was 6.109 ± 0.768, which reduce to 5.125 ± 0.615 (16.11%) at 3 months and to 4.158 ± 0.701 (31.94%) at 6 months with t value of 5.93 after 6 months and for Group B, the mean defect depth at baseline was 6.234 ± 0.661 which reduced to 5.117 ± 0.758 (17.9%) at 3 months and 4.174 ± 0.582 (33.1%) at 6 months with t value of 7.39 after 6 months. The percentage change from baseline to 6 months was found to be 31.94% in Group A and 33.1% in Group B, which indicates that no statistically significant difference amongst the groups.
Overall the results indicated that novabone putty along with PRF produced a more favorable relative attachment level gain and reduction in probing pocket depth and no statistically significant increased bone fill when compared with putty alone.
In view of the limitations, lack of standardization of the radiograph technique as it is very difficult to repeat the radiographs in the same three-dimensional unit but best efforts were made to repeat the radiographs in the same manner with the use of grids; also there was small sample size in the study.
Conclusion
This study was aimed at evaluating the efficacy of Novabone Putty with and without PRF as a bone graft material in the treatment of interproximal vertical defects.
Overall the results indicated that novabone putty along with PRF produced a more favorable relative attachment level gain and reduction in probing pocket depth and no statistically significant increased bone fill when compared with novabone putty alone.
This study was an attempt to evaluate the regenerative properties of novabone putty along with PRF. Due to the small sample size, further larger scale randomized control trials are required to clinically imply the results in a more generalized population.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.American Academy of Periodontology, editor. Glossary of Periodontal Terms. American Academy of Periodontology. 2001 [Google Scholar]
- 2.Hanes PJ. Bone replacement grafts for the treatment of periodontal intrabony defects. Oral Maxillofac Surg Clin North Am. 2007;19:499–512,VI. doi: 10.1016/j.coms.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Lovelace TB, Mellonig JT, Meffert RM, Jones AA, Nummikoski PV, Cochran DL. Clinical evaluation of bioactive glass in the treatment of periodontal osseous defects in humans. J Periodontol. 1998;69:1027–35. doi: 10.1902/jop.1998.69.9.1027. [DOI] [PubMed] [Google Scholar]
- 4.Howell TH, Fiorellini JP, Paquette DW, Offenbacher S, Giannobile WV, Lynch SE. A phase I/II clinical trial to evaluate a combination of recombinant human platelet-derived growth factor-BB and recombinant human insulin-like growth factor-I in patients with periodontal disease. J Periodontol. 1997;68:1186–93. doi: 10.1902/jop.1997.68.12.1186. [DOI] [PubMed] [Google Scholar]
- 5.Dohan DM, choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part I: Technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e37–44. doi: 10.1016/j.tripleo.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 6.Wang HL, Greenwell H. Surgical periodontal therapy. Periodontol 2000. 2001;25:89–99. doi: 10.1034/j.1600-0757.2001.22250107.x. [DOI] [PubMed] [Google Scholar]
- 7.Zhong JP, LaTorre GP, Hench LL. Bioceramics. Pergamon: Elsevier; 1994. The kinetics of bioactive ceramics part VII: Binding of collagen to hydroxyapatite and bioactive glass; pp. 61–6. [Google Scholar]
- 8.Hench LL. Bioceramics. Pergamon: Elsevier; 1994. Bioactive ceramics: Theory and clinical applications; pp. 3–14. [Google Scholar]
- 9.Ali S, Farooq I, Iqbal K. A review of the effect of various ions on the properties and the clinical applications of novel bioactive glasses in medicine and dentistry. Saudi Dent J. 2014;26:1–5. doi: 10.1016/j.sdentj.2013.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yukna RA. Synthetic bone grafts in periodontics. Periodontol 2000. 1993;1:92–9. [PubMed] [Google Scholar]


