Abstract
Objectives: To investigate telemedicine adoption, emergency department avoidance, and related characteristics of patients with chronic obstructive pulmonary disease (COPD) with and without exacerbations since the coronavirus 2019 (COVID-19) pandemic began.
Methods: We conducted the second of a series of online surveys via SurveyMonkey.com of people with COPD between May 1, 2020 and May 31, 2020. Frequency, percentage, and Fisher’s exact test (2-sided) were calculated using SPSS version 26.
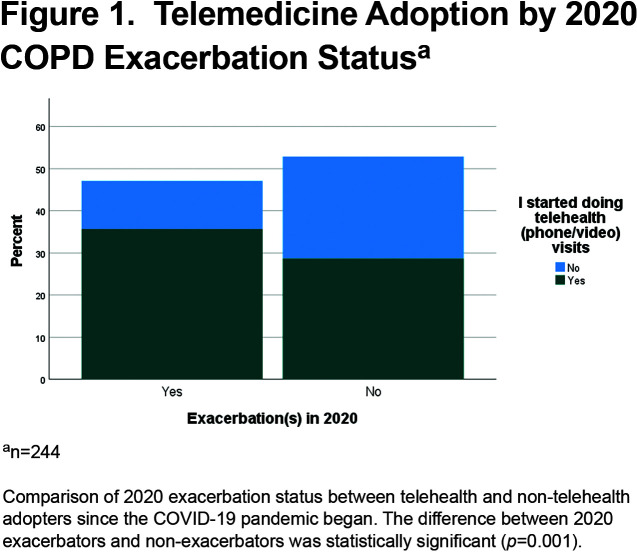
Results: More than half of respondents (157, 64%), indicated that they started using telemedicine in 2020. A total of 47% of respondents reported having had at least 1 exacerbation since January 1, 2020. Respondents who had at least 1 exacerbation in 2020 were more likely to start using telemedicine in 2020 than respondents who did not report any exacerbation in 2020 (75.7% versus 54.3%, p < 0.001). Respondents reporting a 2020 exacerbation indicated having a significantly higher avoidance of emergency health care since the pandemic began (27.8%) as compared to those who did not have an exacerbation in 2020 (10.1%), p < 0.001.
Conclusions: In response to social distancing and other COVID-19 precautions, people with COPD are avoiding traditional, in-person health care environments and turning to telemedicine to prevent and manage exacerbations. Further investigation is needed to identify best practices in and barriers to telemedicine in this population.
Keywords: copd, exacerbations, COVID-19, telemedicine, telehealth
Introduction
Individuals with chronic obstructive pulmonary disease (COPD) are at high risk of morbidity and mortality from coronavirus 2019 (COVID-19),1 but they are also at a risk of mortality and poor outcomes with high rates of health care resource utilization if their COPD exacerbations are untreated as recommended.2,3 Telemedicine has potential as an effective tool for prevention and management of exacerbations in individuals with COPD.4 Telemedicine also allows for monitoring of patients during the vulnerable period following a hospitalized COPD exacerbation.2 In-home digital health apps, such as the COPD Foundation Pocket Consultant Guide, can be used to improve self-management and prevent untreated COPD exacerbations.5 Improved tools for telehealth-administered pulmonary rehabilitation are comparable to in-person pulmonary rehabilitation programs.6 However, COPD telehealth care is not standardized with few well-designed intervention trials. Aiming to assess the impact of COVID-19 on individuals with COPD and related chronic lung conditions, the COPD Foundation conducted 2 online community surveys which informed ongoing community webinars and programs.7
Methods
Survey 1 (S1) was administered between March 29 and April 13, 2020. Qualitative analysis of open-ended responses to S1 informed the questions administered in Survey 2 (S2), administered between April 26 and May 31, 2020. Survey 3 (S3) was administered between August 14 and September 15, 2020. S1 respondents with COPD expressed extreme fear and anxiety about leaving the house for any reason, including health care-related visits, due to fear of being infected with COVID-19. As many health care providers in highly COVID-19-affected areas cancelled in-person visits, either by their own decision or through state and local policy requirements, we were concerned about avoidance of preventive care and treatment for exacerbations by individuals with COPD, resulting in poor outcomes. Hence, in S2 we added the following questions to explore the use of health care and telemedicine in individuals experiencing COPD exacerbations:
“Which of the following ways has COVID-19 affected your interactions with health care providers?” including the choices, “I started doing telehealth (phone/video) visits” and, “I started avoiding the emergency department for situations that I would have gone to the emergency department before COVID-19.”
“Since January 1, 2020, have you had exacerbations or flare-ups of your COPD that required ANY of the following: use of oral steroids or antibiotics, a visit to the emergency room, or hospitalization?”
“What do you feel would help you cope during this COVID-19 pandemic?” which included the response choice “Assistance with technology, video calls, and/or social media.”
S3 was considerably shorter than the first 2 surveys and included new questions about telehealth utilization; the results of S3 informed our programming and outreach and confirmed some of the findings of S2. Surveys were conducted using SurveyMonkey.com and received an exemption determination from the Western Institutional Review Board before recruitment began. We recruited respondents through the COPD Foundation’s COPD360 network, including the online communities for COPD (COPD360social)8 and bronchiectasis and nontuberculous mycobacterial lung disease (BronchandNTM360social),9 e-newsletters, Twitter, and Facebook. COPD Foundation partners, the NTM Info and Research organization and the Pulmonary Education and Research Foundation, also assisted in recruitment.This report focuses on respondents with COPD in the United States who answered S2 questions on telemedicine and exacerbation history (n=244 out of 508 total respondents). Overall summaries of surveys were reported on the COPD Foundation website.4 Frequency, percentages, and Fisher’s exact test (2-sided) were calculated using SPSS version 26.
Results
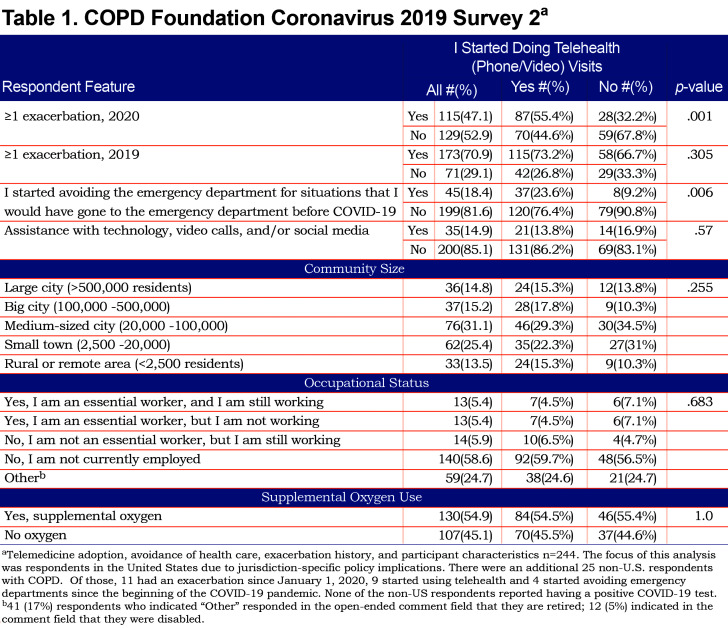
Respondents to S2 represent a variety of communities, with 31% residing in medium-sized cities. More than half of the respondents (59%) are not currently employed, but 5% are essential workers and were still working at the time of the survey. Among those respondents who categorized their employment status as “other,” 17% wrote in “retired” while 5% wrote in “disabled.” A total of 55% of the sample reported the use of supplemental oxygen (See Table 1). Almost all (97%) of respondents to S2 reported being on respiratory medication for their COPD and 78% reported that they had “avoided leaving the house” since the beginning of the pandemic. More than half of respondents (157, 64%), indicated that they started using telemedicine in 2020. A total of 47% of respondents reported having had at least 1 exacerbation since January 1, 2020. Respondents who had at least 1 exacerbation in 2020 were more likely to start using telemedicine in 2020 than respondents who did not report any exacerbation in 2020 (75.7% versus 54.3%, p < 0.001, Figure 1). Respondents reporting a 2020 exacerbation indicated having a significantly higher avoidance of emergency health care since the pandemic began (27.8%) as compared to those who did not have an exacerbation in 2020 (10.1%), p < 0.001. There was no statistically significant difference in adoption of telemedicine based on size of city or town of residence, employment status, or supplemental oxygen use (Table 1). One respondent (non-exacerbator) tested positive for COVID-19 and reported initiating telehealth in 2020. A total of 15% of all respondents indicated that they would like assistance with using technology, video calls, and/or social media. While not statistically significant, we noted that respondents who had exacerbations in 2020 were more likely to report that they needed assistance with technology (19.5%) as compared to respondents who did not have an exacerbation (10.7%), p=0.07.
Discussion
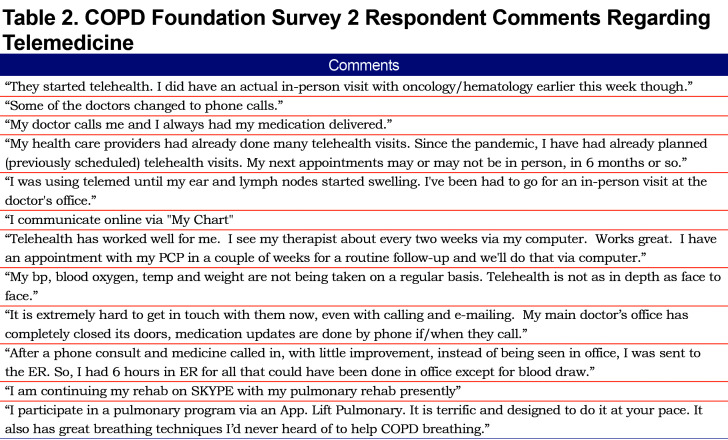
Our data demonstrate that the most vulnerable members of the COPD community are turning to telemedicine for the management of their condition during COVID-19. Some S2 respondents commented that they were already using telemedicine prior to COVID-19 (Table 2), so we do not assume that if they did not respond that they started telemedicine since the pandemic began that they are not using telemedicine. Acknowledging this limitation of S2, we asked respondents about prior use of telehealth in S3. We found that all 6 of the respondents who reported using telehealth exclusively before the pandemic continued to use telehealth exclusively after the pandemic. For those who had only in-person appointments before the pandemic, 44 (49%) of exacerbators versus 28 (34%) of non-exacerbators reported using at least some telehealth visits (p=0.046). Because S3 was conducted later in the pandemic (August 2020 versus May 2020), it is possible that part of this mix is due to the fact that some health care facilities had reopened and participants were no longer forced to postpone essential, in-person services such as spirometry.
While we are pleased to observe that a high percentage of our survey respondents seem to be following general COPD treatment10 and COVID-19 prevention guidelines7 (based on medication use and social distancing responses), we are concerned about the inconsistency of telehealth approaches reported in open-ended comments. We remain concerned about the quality, consistency, technological accessibility, and affordability of the telemedicine options available to the COPD community at large and accelerating the development of better digital tools remains a key focus of the COPD Foundation. A potential limitation of our study is the fact that respondents to our online surveys are likely a subset of the population more inclined to use the internet and telemedicine while our mission is to meet the needs of the entire COPD community. In addition, based on the number of respondents reporting supplemental oxygen use, exacerbations, and that they are not working or retired, our sample may skew toward older and/or severely ill participants. This is also true in S3, in which 52% of respondents had experienced at least 1 exacerbation since January 1, 2020. We did not collect data on age or other demographic characteristics, so it was impossible to control for confounders. However, even if the adoption of telehealth is due to age and severity of illness, we do not feel that this changes the conclusion that there needs to be improved access to telehealth for all members of the COPD community, especially the elderly and more severe cases.
COPD is the fourth leading cause of death in the United States and in 2017, there were nearly 1 million emergency department visits and 5.7 million physician office visits with emphysema or COPD as the primary diagnosis.11 The Centers for Disease Control and Prevention recognizes telemedicine as a promising public health tool in part because of its potential to improve health care access to medically underserved populations.12 However, it is imperative to include the patient perspective in the design of these programs to avoid the risk of creating new disparities in communities that lack the hardware, internet access, and skills to fully participate in telemedicine. Additionally, given the fact that 51% of COPD-related medical costs are borne by Medicare, and outside of the current public health emergency, telehealth services in patients’ homes are not reimbursed, future efforts will be needed to inform policy changes required to allow the full benefits of telehealth chronic disease management services to be realized.13
Abbreviations
Abbreviations: chronic obstructive pulmonary disease, COPD; coronavirus 2019, COVID-19; survey1, S1; survey 2, S2; survey 3, S3
Funding Statement
This study/survey was supported by COVID-19 research grants from AstraZeneca, GlaxoSmithKline, Teva, Mylan, and Pfizer. The funders had no role in: (1) conception, design, or conduct of the surveys; (2) collection, management, analysis, interpretation, or presentation of the data; or (3) preparation, review, or approval of the manuscript.
References
- 1.Alqahtani JS,Oyelade T,Aldhahir AM,et al. Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: a rapid systematic review and meta-analysis. PLoS One. 2020;15(5):1-13. doi: https://doi.org/10.1371/journal.pone.0233147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Donner CF,Raskin J,ZuWallack R,et al. Incorporating telemedicine into the integrated care of the COPD patient a summary of an interdisciplinary workshop held in Stresa, Italy, 7-8 September 2017. Respir Med. 2018;143:91-102. doi: https://doi.org/10.1016/j.rmed.2018.09.003 [DOI] [PubMed] [Google Scholar]
- 3.Dransfield MT,Kunisaki KM,Strand MJ,et al. Acute exacerbations and lung function loss in smokers with and without chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2017;195(3):324-30. doi: https://doi.org/10.1164/rccm.201605-1014OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cordova FC,Ciccolella D,Grabianowski C,et al. A telemedicine-based intervention reduces the frequency and severity of COPD exacerbation symptoms: a randomized, controlled trial. Telemed e-Health. 2016;22(2):114-122. doi: https://doi.org/10.1089/tmj.2015.0035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomashow B,Crapo JD,Drummond MB,et al. Introducing the new COPD pocket consultant guide app: can a digital approach improve care? A statement of the COPD foundation. Chronic Obstr Pulm Dis. 2019;6(3):210-220. doi: https://doi.org/10.15326/jcopdf.6.3.2018.0167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stickland MK,Jourdain T,Wong EY,Rodgers WM,Jendzjowsky NG,MacDonald GF. Using telehealth technology to deliver pulmonary rehabilitation to patients with chronic obstructive pulmonary disease. Can Respir J. 2011;18:216-220. doi: https://doi.org/10.1155/2011/640865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.COPD Foundation. Coronavirus information for the COPD community. COPD Foundation website. Published 2020. Updated March 2021. Accessed August 8, 2020. https://www.copdfoundation.org/Learn-More/I-am-a-Person-with-COPD/Coronavirus-Information.aspx [Google Scholar]
- 8.COPD Foundation. COPD360social activity feed. COPD Foundation website. Accessed August 2020. https://www.copdfoundation.org/COPD360social/Community/Activity-Feed.aspx [Google Scholar]
- 9.Bronchiectasis and NTM Initiative. BronchandNTM360 social activity feed. Bronch and NTM Initiative website. Accessed August 2020. https://www.bronchiectasisandntminitiative.org/ [Google Scholar]
- 10.COPD Foundation. NEW! Our free COPD pocket consultant guide app track for people with COPD and their families!. COPD Foundation website. Published July 30, 2020. Accessed August 15, 2020. https://www.copdfoundation.org/Learn-More/The-COPD-Pocket-Consultant-Guide/Patient-Caregiver-Track.aspx [Google Scholar]
- 11.Centers for Disease Control and Prevention (CDC). Chronic obstructive pulmonary disease (COPD) includes: chronic bronchitis and emphysema. U.S.data.CDC website. Updated March 1, 2021. Accessed July 31, 2020. https://www.cdc.gov/nchs/fastats/copd.htm [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC). Telehealth and telemedicine. CDC website. Updated July 8, 2020. Accessed July 31, 2020. https://www.cdc.gov/phlp/publications/topic/telehealth.html [Google Scholar]
- 13.Ford ES,Murphy LB,Khavjou O,Giles WH,Holt JB. Total and state-specific medical and absenteeism costs of COPD among adults aged ≥18 years in the United States for 2010 and projections through 2020. Chest. 2020;147(1):31-45. doi: https://doi.org/10.1378/chest.14-0972 [DOI] [PubMed] [Google Scholar]