Abstract
Objectives
The aim of current systematic review and meta-analysis is to provide insight into the therapeutic efficacy of fecal microbiota transplantation (FMT) for the decolonization of antimicrobial-resistant (AMR) bacteria from the gut.
Methods
The protocol for this Systematic Review was prospectively registered with PROSPERO (CRD42020203634). Four databases (EMBASE, MEDLINE, SCOPUS, and WEB of SCIENCE) were consulted up until September 2020. A total of fourteen studies [in vivo (n = 2), case reports (n = 7), case series without control arm (n = 3), randomized clinical trials (RCT, n = 2)], were reviewed. Data were synthesized narratively for the case reports, along with a proportion meta-analysis for the case series studies (n = 102 subjects) without a control arm followed by another meta-analysis for case series studies with a defined control arm (n = 111 subjects) for their primary outcomes.
Results
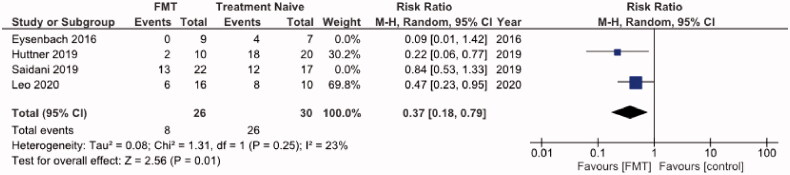
Overall, seven non-duplicate case reports (n = 9 participants) were narratively reviewed and found to have broad AMR remission events at the 1-month time point. Proportion meta-analysis of case series studies showed an overall 0.58 (95% CI: 0.42-0.74) AMR remission. Additionally, a significant difference in AMR remission was observed in FMT vs treatment naïve (RR = 0.44; 95% CI: 0.20-0.99) and moderate heterogeneity (I2=65%). A subgroup analysis of RCTs (n = 2) revealed FMT with further benefits of AMR remission with low statistical heterogeneity (RR = 0.37; 95% CI: 0.18-0.79; I2 =23%).
Conclusion
More rigorous RCTs with larger sample size and standardized protocols on FMTs for gut decolonization of AMR organisms are warranted.
KEY MESSAGE
Existing studies in this subject are limited and of low quality with moderate heterogeneity, and do not allow definitive conclusions to be drawn.
More rigorous RCTs with larger sample size and standardized protocols on FMTs for gut decolonization of AMR organisms are warranted.
Keywords: Faecal microbiota transplantation, antibiotic resistance, systematic review and meta-analysis, case study, case series study
Introduction
Currently, antimicrobial resistance (AMR) has been identified as one of the major threats to global health, food production, and economic development [1]. The US Centres for Disease Control and Prevention has estimated that each year, >2.8 M patients are infected with antibiotic-resistant (AR) bacteria and >35,000 dies of these infections. Also, nearly 223,900 people in the United States required hospital care for C. difficile and at least 12,800 people died in 2017 [2]. AMR is most often conferred through the expression of antimicrobial resistance genes that reduce a microbe’s susceptibility to the effects of antibiotics. AMR bacteria are stratified to, Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species, known to be “ESKAPE”, are responsible for the majority of hospital infections with higher mortality rates [3]. Data on AMR in Europe are reported by the European Antimicrobial Resistance Surveillance Network (EARS-Net) 2018 report, stated that more than half (58.3%) of the E. coli and third (37.2%) of K. pneumoniae isolates responsible for invasive diseases were resistant to at least one of the antimicrobial groups under regular surveillance (i.e. aminoglycosides, aminopenicillins, fluoroquinolones, third-generation cephalosporins, and carbapenems) [4].
The human gastrointestinal (GI) tract is colonized by different kinds of bacteria, archaea, fungus, and viruses, consensually termed as gut microbiota [5]. The intestinal microbiome of healthy patients often consists of well-balanced diversified microbiota members that predominantly belong to just four phyla—the Bacteroidetes, Firmicutes, Actinobacteria, and Proteobacteria and known to pose colonization resistance (CR) [6]. Gut microbiota can produce a variety of compounds that play key roles in the colon micro-ecology and host homeostasis. Delicate contemporary approaches to unravel the importance of the symbiosis of gut microbiota lead to its identification as a potential target of many chronic diseases ranging from gastrointestinal inflammatory and metabolic conditions to neurological, respiratory, and cardiovascular illnesses [7]. Apart from that, gut microbiota plays a beneficial role in maintaining human health via producing short-chain fatty acids (SCFA), vitamins and acting as a shield to protect the host from colonization by pathogenic bacteria [8].
However, under certain circumstances, the patient may develop a compromised microbiota by declining alpha-composition and it causes CR vulnerability and eventually leads to exogenous bacterial colonization. The deleterious effects of antibiotics on gut microbiota have been extensively studied [9,10]. Other than antibiotics, proton pump inhibitors (PPIs) are one of the most commonly prescribed drugs in western medicine [11], and they lead to a profound and prolonged reduction of gastric acid production. The association of PPIs and the risk of some enteric infections namely, Clostridium difficile, Campylobacter, Salmonella are well documented [12–14]. Importantly, antipsychotic drugs such as olanzapine [15], pimozide [16], fluphenazine [17], and flupenthixol dihydrochloride [18] were proven to pose in vitro antibacterial properties against a broad spectrum of bacteria alone and in combination with other antibiotics. A significant population of the community consumes these drugs and they may have disturbed gut microbiota composition, and consequently put their CR at risk. Hence, their intestinal microbiota dysbiosis provides favourable conditions for AMR bacteria to colonize and eventually act as a reservoir for horizontal resistant gene transfer [19,20]. Horizontal gene transfer has been documented as an important mechanism for the transfer and acquisition of antimicrobial resistance genes within and between gut bacterial species (Figure 1) [21–23].
Figure 1.
Concept illustration of colonization resistance due to alpha diversity of gut microbes and the effect of antimicrobials in destabilization of symbiotic stage. The disturbed gut microbiota could be colonized with AMRs and leads to dysbiosis. FMT is an alternative therapeutic modality to restore the alpha diversity by decolonizing AMRs.
Research on the bilateral relationship between gut microbiota and human health has been in the spotlight during the last decade. This has been mainly driven forward by improved next-generation sequencing (NGS) technologies [24] and novel proteomic [25] approaches, allowing the profiling of entire microbial communities with high efficacy and low cost.
The conservation effect of gut microbiota from AR has encouraged scientists to study faecal microbiota transplantation (FMT) to restore a healthy gut microbiome by eliminating AR colonization. The concept behind FMT is to directly alter the gut microbial composition of the recipient to establish the alpha-diversity [26]. This is achieved via the administration of a frozen, encapsulated or fresh solution of faecal matter from a donor into the intestinal tract of a recipient to confer a health benefit via altering the gut microbial composition [27]. The initial step of the process involves a thorough screening procedure to identify a suitable donor. This includes a questionnaire of the donors’ family health history, contemporary exposure to any medication and a series of laboratory tests to ensure there is no transmittable disease or pathogens [28]. According to the contemporary guidelines from the Infectious Diseases Society of America (IDSA) and the Society of Healthcare Epidemiology of America (SHEA), as well as the European Consensus Guidelines, FMT is recommended as a second-line treatment modality against recurrent C. difficile infection, due to over 90% efficacy in randomized control trials [26]. But the application of FMT for the decolonization of AMR microorganisms other than C. difficile is controverisal due to a limited number of reports [29–36].
The main objective of our review is to descriptively analyze the non-duplicate data and pool all published data to ascertain a conclusive statistical picture of the primary outcome, set as the decolonization of AMRs (except recurrent C. difficile) in adults (>18 years old) by FMT intervention at the 1-month time point. Secondary outcomes are to provide systematic descriptive analyses of case studies on decolonization of AMR via FMT, identifying adverse effects associated with FMT procedures, and outline key steps to be followed in future rigorous clinical trials.
Methods
Protocol development
We registered our review protocol (CRD42020203634) in the International Prospective Register of Systematic Reviews (PROSPERO) that is available at https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020203634. We adhered to the recommendations of the PRISMA-P 2015 statement in developing this protocol and conducting the review [37].
Search strategy
This global search was performed using four bibliographic databases, namely, EMBASE and MEDLINE through PubMed, SCOPUS, and WEB of SCIENCE. The following search terms were used: (“Faecal microbiota transplantation” OR “FMT” OR “bacteriotherapy” OR “gut microbiota transplantation” OR “fecal transplantation” OR “intestinal microbiota transfer”) AND (“intestinal antibiotic-resistant bacteria” OR “antibiotic-resistant bacteria” OR “intestinal antimicrobial resistance” OR “AMR”). The same search term was used in all databases to retrieve the data for this review. Apart from that, we have searched the following clinical trial registries; United States (www.clinicaltrials.org), Australia-New Zealand (www.anzctr.org.au) United Kingdom (www.isrctn.com), Germany (www.drks.de), and China (www.chictr.org.cn)
The final database update was carried out on 15 September 2020.
Eligibility criteria
Types of studies
This review included studies that investigated the effectiveness of FMT in eliminating AMR colonization confined to the gut. As a fact, FMT is an emerging therapy for the decolonization of AMR for intestinal carriage, hence the data on randomized clinical trials are scanty. Thus, we included different types of clinical trials including, cohort studies, case studies, case series studies, and case reports. Apart from clinical investigations, we also reviewed in vivo studies dealing with the same purpose. We excluded all the review articles, news, conference proceedings, editorials, and letters to the editor, expert opinions, or commentaries as they did not provide adequate information for review. Except for case series studies (used only for the meta-analysis), we also excluded studies (case reports) that were previously reviewed.
Types of participants and eligible AMR bacteria
The adult population (>18 years) was included in the review. Studies with paediatric patients were excluded since their gut microbiome is in a dynamically developing stage and the study outcome could not be compared with the adults [38], and those who are carrying rather stable gut microbiome [39]. Patients who received antibiotics concurrently at the time the FMT were also excluded, due to its direct effect on the composition of the transplanting bacteria [40]. However, patients whose concomitant antibiotic therapy was discontinued at least 24 h before the FMT procedure were included.
AMRs involving viruses and fungi and AMR bacteria colonized outside the gut were also excluded. Furthermore, FMT on the patients who had recurrent or refractory C. difficile infections alone was also excluded from our review process, since there are other reviews solely focussed on the topic [41–43].
Types of interventions and outcome measures
The single-arm intervention trials were abundant in numbers in this review, but studies with control groups including placebo, antibiotics, or treatment-naive were also included, where necessary. Different FMT administration routes (upper and lower gastrointestinal routes) were considered including; caecum through colonoscopy, oral gavage, naso-duodenal tube and delivered via enema. The fresh, frozen or encapsulated samples were used in FMT along with related or unrelated donors, as well as, single or multiple FMTs were included in the review.
The primary outcome measured was the decolonization of AMR within 1 month (30 days) upon FMT with two consecutive negative results of rectum swabs or confirmed by PCR. However, the inter-study variation could be observed in the outcome for decolonization testing and are included in this review.
Assessment of risk of bias of eligibility criteria for the articles
This assessment was performed in several ways including, the use of https://www.covidence.org online platform. At the beginning, all the citations (from 4 databases) were uploaded to the software in “RIS” file format. A preliminary abstract screening was carried out by NR and AL for inclusion and the selected studies were subjected to scrutiny by full-text review by NR, AL, and PD to avoid the risk of bias. Any disparities were resolved upon the consultation of senior author MI.
Moreover, the selected studies were further verified by NR and PD, according to the Joanna Briggs Institution (JBI) standardized critical appraisal checklists for case series and case reports for the possibility of bias in its design, conduct, and analysis [44,45]. The completed JBI forms for the included studies were given in Supplementary information, Section 1. The studies with selection “No” for at least 3 questions in the appraisal form considered to pose a lack of integrity in the study design, hence excluded from data abstraction and reviewing.
Overall completeness and transparency of the included case reports were verified using CARE guidelines [46] and completed forms for the included studies are given in Supplementary information, Section 2. Similarly, PROCESS guidelines [47] were used to verify the quality and risk of bias of the case series studies (Supplementary information, Section 3). Quality of evidence for two randomized control trials and the remaining 3 case series studies were assessed following the GRADE recommendations [48] and completed on the GRADEpro online software (Supplementary information, Section 4).
Data abstraction
We developed a data abstraction spreadsheet using Excel version 2016 software (Microsoft Corporation, Redmond, Washington, USA). We conducted the data abstraction for the included full-text articles, and the data were independently assessed by two review authors. We extracted the following information: title, DOI number, type of study, acceptance or rejection of topic, type of faecal material, methods of infusion, characteristics or composition of stool, types of patients, the role of FMT on the antibiotic-resistant bacteria, mode of action, and side-effects with potential remarks.
Data synthesis
Two separate meta-analyses were carried out for the case series studies with and without control arms for their primary objective (percentage decolonization at the 1-month time point). However, in two studies [49,50], the decolonization rate was considered at the 35 to 48-day time point. The case reports were excluded from the meta-analysis, since the single data is not adequate to provide the estimation of effect size and for which, we have provided only a narrative synthesis [51].
The outcome for the case series studies is dichotomous with only two responses, such as AMR decolonization was successful or not. The meta-analysis for the case series studies without a control arm was analysed as proportions of decolonization [52,53] under the random-effects model using StatsDirect v3 statistical software. Analyses of the case series studies with the inclusion of a proper treatment naïve group were conducted via RevMan 5.4 using a random-effects model. For both meta-analyses, the combined effect was illustrated via creating a forest plot.
A statistically significant p-value was based on p < .05. Clinical and methodological heterogeneity across the included studies were expressed descriptively, while the statistical heterogeneity between the studies included for the two meta-analyses was expressed by using the I2 statistic, while I2 values interpreted as; low, moderate, and high levels of heterogeneity where, I2 < 50%, I2 50–75%, and I2 > 75%, respectively [54].
Results
Study selection
The search strategy from EMBASE and MEDLINE via PubMed, SCOPUS, and WEB of SCIENCE yielded one thousand five hundred and eighty-five (n = 1585) studies, none of the studies were retrieved from the grey literature. Upon removal of duplicates (n = 612), the title and abstracts of nine hundred and seventy-three (n = 973) studies were screened, and nine hundred and twenty-one (n = 921) studies did not meet the selection criteria. The full texts of the remaining fifty-two (n = 52) studies were assessed against the pre-defined inclusion and exclusion criteria, but thirty-eight (n = 38) studies did not meet the ultimate inclusion criteria. Additionally, the studies already included in previous literature reviews [38–40,50] were also excluded in abstracting data or review in detail. However, previously published case series studies were included in 2 meta-analyses to get an overall statistical conclusion on the effect of FMT on the decolonization of AMRs at the 1-month time point. Finally, fourteen (n = 14) studies were eligible for this detailed data abstraction and the broad discussion. The process of the selection of studies is summarized in a PRISMA flow diagram (Figure 2). Three reviewers, NR, AL, and PD, screened the studies for inclusion and exclusion in the systematic review and meta-analysis and all the review authors mutually agreed on the final set of articles to be included.
Figure 2.
Flowchart showing the systematic review process with the bibliometric assessment, including article attrition and study selection. Briefly, articles were filtered through an automated bibliographic database search using keywords.
Characteristics of included studies
The eligible articles had a publication date from September 2015 to September 2020. Out of fourteen studies, the majority are case reports or case studies (n = 7) followed by different types of case series (n = 5) and two (n = 2) in vivo studies involving mice models. Out of the five case series studies, two (n = 2) were carried out in multiple centres (Switzerland, Netherland, France, and Israel) [49,50], while the remaining (n = 3) are single-center studies [55–57]. Most of the case reports/studies (n = 5/7) were carried out in Europe; namely, Denmark (n = 2) [58,59], Poland (n = 2) [60,61], Netherland (n = 1) [62], and one study each in USA [63] and South Africa [64]. AMR colonization in the gut was varied among studies, particularly in CREs. Except in one case study where the gut was colonized by MDR Salmonella infantis, multiple MDR bacteria colonized participants across all other studies [63]. The clinical diagnostics of the subjects who underwent FMT across the case reports/studies included patients with; immunocompromised [61], diabetic [62], renal transplant [58], different types of leukemia [60,63] and critically ill with multiple organ failure [59,64]. We have observed an inter-study variability in using PPIs. None of the case studies/reports used PPIs in the pre-treatment step, except in Bilinki et al. [61]. This observation was in contrast to that in case-series studies, where PPIs (omeprazole and pentaprazole) were used in all studies as a pre-treatment in different time points, except in Leo et al. [49] Bowel cleansing was not conducted in any of the case studies/reports, but it has been applied in many case series studies [55–57]. Except in one case study [64], the FMTs in all included studies were procured from unrelated healthy donors. Among most case studies/reports (n = 5/7), fresh stool samples were used and diluted with sodium chloride solutions (saline). In contrast, FMT was applied as capsules from frozen stool samples (n = 3/5) with a dosage of 15 capsules/day for two consecutive days, in case series studies [49,50,55]. Among capsule-based FMTs, one study used 80% of glycerol instead of 10% in preparation of the capsule, to increase the stability [50].
Application of FMT in AMR decolonization in gut
In vivo models
The study characteristics of the two eligible in vivo studies are given in Table 1. FMT is effective in decolonizing various common resistant pathogens including, MDR P. aeruginosa, and concurrent colonization of vancomycin-resistant E. faecium and KPC [65,66]. Both included studies have shown that FMT significantly decreased the faecal load (in terms of CFU) of colonizing resistant bacteria when compared to those that did not receive FMT [65,66].
Table 1.
Characteristics of the in vivo studies eligible for the review.
| Mrazek et al. [65] | Caballero et al. [66] | |
|---|---|---|
| In vivo model | 8-weeks old female C57BL/6j mice | 6–8-week-old C57BL/6 female mice |
| MDR bacteria, resistant gene/pattern, load injected | MDR P. aeruginosa, sensitive to fosfomycin and colistin only, 109 CFU on 2 consecutive days |
E. faecium K. pneumoniae, Vancomycin and carbapenem resistant, 5 × 104 CFU by oral gavage |
| Confirmation of infection | Stool culture for CFU and 16 s rRNA analysis | Stool culture for CFU, 16 s rRNA analysis, Fluorescence in-situ hybridisation |
| FMT donor | 5 healthy human or 10 age and sex matched specific pathogen-free control mice | Untreated mice |
| FMT sample preparation | Dissolved in sterile PBS, aliquoted, and stored at − 80 °C. Immediately before FMT, individual faecal aliquots were thawed and pooled. | Faecal pellet/1 ml of PBS |
| FMT route and FMT dose | Oral gavage, 0.3 ml for 3 consecutive days | Oral gavage, 200 μl portion three doses |
| FMT efficacy | 4 log reduction of bacteria was observed at 1 W time point, irrespective of source of the donor | K. pneumoniae density in faecal pellets decreased within one day and became undetectable within 7 days in all mice |
A 2.5 and 4 log10 average CFU reduction was observed in MDR P. aeruginosa level in mice receiving FMT by murine donors and human donors, respectively, within 7 days post-FMT [65], implying donors of the same species can produce a stronger colonization resistance [65].
KPC was cleared more effectively than VRE in mice receiving FMT (100% and 60% clearance for K. pneumoniae and VRE, respectively) [66]. It may suggest there are different mechanisms of colonization resistance against VRE and K. pneumoniae, or K. pneumoniae is more susceptible to colonization resistance [66].
Except for the FMT donor, the mice model, colonization confirmation, and the route of FMT administration were quite similar in both studies (Table 1). However, the dosage of FMT and target MDR bacterial species vary among studies.
Case reports of FMT
The study characteristics of the seven case studies/reports included for the review are given in Table 2. In the case reports, the patients were mostly colonized with Enterobacteriaceae (Table 2). Besides, some other MDR pathogens were also confirmed such as; Candida albicans, Candida parapsilosis, Enterococcus faecalis, E. faecium, and S. infantis [58,60,62–64]. Except Ueckermann et al. [64], for the reaming studies, the colonization confirmation was achieved via rectal swab analysis
Table 2.
Characteristics of published case study/reports describing outcomes of FMT against AMR Decolonization.
| Biliński et al. [61] | Stalenhoef et al. [62] | Grosen et al. [58] | Soto et al. [64] | Biernat et al. [60] | Bahl et al. [59] | Ueckermann et al. [64] | ||
|---|---|---|---|---|---|---|---|---|
| Type of study | Case study | Case report | Case report | Case study | Case report | Case study | Case report | |
| Status | Immuno- compromised patient | Diabetic patient with recurrent UTIs | Recurrent UTI in first five months after Renal transplant recipient (RTX) | Patient 1 (P1): chronic lymphocytic leukaemia Patient 2 (P2); chronic arthropathy on rituximab |
P1: acute myeloid leukaemia P2: osteomyelofibrosis |
Multi organ failure along with severe recurrent CDI | Critically ill patient | |
| Age | 51 years | 34 years | 64 years | P1: 60 years P2: 48 years |
P1: 25 years P2: 32 years |
69 years | 60 years | |
| M/F | M | M | M | P1: M P2: F |
P1: M P2: M |
F | M | |
| Indication/colonization status and virulence genes |
K. pneumoniae NDM+ and E. coli ESBL |
MDR P.aeruginosa and MDR E. coli |
ESBL+ K. pneumoniae |
P1: MDR S. infantis P1: MDR S. infantis | P1: E. faecalis, C. albicans and ESBL + E. coli and K. pneumoniae P2: ESBL+ E. coli E. faecium GRE, C. albicans, C. parapsilosis, K. pneumonia etc. |
C. difficilli and KPC-producing, XDR K. pneumoniae | MDR K. pneumoniae Infection+ Candida parapsilosis | |
| Colonization confirmation | Rectal swab | Rectal swab | Stool sample | Stool sample | Stool sample | Stool sample | Blood cultures | |
| Biliński et al. [5,61] | Stalenhoef et al. [62] | Grosen et al. [58] | Soto et al. [63] | Biernat et al. [60] | Bahl et al. [59] | Ueckermann et al. [64] | ||
| Pre treatment | Antibiotic | penicillin V, co-trimoxazole | colistin intravenously (IV) for 2 weeks | vancomycin 125 mg orally four times per day | P1: Ertapenem and ciprofloxacin P2 azithromycin | NA | 12 days fidaxomicin | Amikacin, tigercylin and colistin for 14 days |
| PPI | Twice daily | NA | NA | NA | NA | NA | NA | |
| Bowel cleansing | Once before FMT | NA | NA | NA | NA | NA | NA | |
| Donor screening tests |
See Supplementary information, Section 5 | Multiple testing | screened for faecal and blood transmitted diseases | Questionnaire, blood sampling, and faecal sample analysis | NM | P1 and P2: Tested for active bacterial, viral, fungal, and parasitic infections | Screened according to a standard protocol | According to the European consensus statement |
| FMT | Donor Status of intervention Dilution |
Unrelated Fresh stool 100 g with 100 ml sterile physiological saline |
Unrelated Fresh stool 75 g processed 300 ml suspension of saline |
Unrelated Cryopreserved NM |
NM Frozen and encapsulated NA |
Unrelated Fresh stool 100 g of faeces in 150–250 ml physiological salt |
Unrelated Fresh stool 72 g of faeces in 500 ml of isotonic sodium chloride |
Wife Fresh stool 30 g of faeces diluted in 150 ml of 0.9% saline |
| Biliński et al. [61] | Stalenhoef et al. [62] | Grosen et al. [58] | Soto et al. [64] | Biernat et al. [60] | Bahl et al. [59] | Ueckermann et al. [64] | ||
| FMT | Dose | Single FMT | Single FMT | Single FMT and later dose of meropenem | P1:15 capsules on each of 2 successive days P2: First dose same as for P1 and the second dose was 15 capsules on each of 3 successive days | P1: three doses with 1 week gap for each P2: four doses with 1 week gap for each | Single FMT | Twice with a 2 week gap |
| Route | Naso-duodenal tube | Naso-duodenal tube | Nasojejunal tube | Oral | intranasal probe | colonoscope | Nasojejuneal tube | |
| Primary outcome | Rectal swabs collected on day 10 and 26 after FMT repeatedly did not show growth of either K. pneumoniae NDM + or E. coli ESBL+. | Negative for MDR P. aeruginosa, but failed to decolonize ESBL E. coli | E. coli and K. pneumoniae was not detected 4 and 8 month follow up testing | Both patients ultimately cleared symptomatic salmonella intestinal infection after a long course of a carbapenem and FMT. | P1: symptoms were completely resolved after the third FMT P2: antibiotic sensitive E. coli and Citrobacter freundii were detected | Resistance strains were negative at 1 week time point | Patient had no further episodes of sepsis, and blood cultures were repeatedly negative for any bacteria | |
| Adverse effects | Loose stool and abdominal pain | Loose stool for 3 days | diarrhoea | None | None | None | None | |
| Follow up time | 1 month | 3 months | 12 months | P1: 4 months P2: 2 months | 7 months | 203 days | 6 weeks |
It is apparent from Table 2 that most of the AMR strains with different resistant mechanisms were susceptible to the FMT at the 1-month time point [58,59,61,63,64]. However, Stalenhoef et al. [62], reported that the patient who received single FMT failed to decolonize ESBL + E. coli resistant to carbapenems, gentamicin, piperacillin/tazobactam, and colistin, respectively but eradicated MDR P. aeruginosa successfully during the 3 months follow-up period. Similarly, Biernat et al. [60], reported that patient-1 has completely resolved the symptoms after having three consecutive doses of FMT with a 1-week interval and decolonized all the pathogens. On the contrary, the patient-2 of the same study who received four doses of FMT with a 1-week gap failed to decolonize multidrug-resistant E. coli, and Citrobacter freundii.
Though most of the studies did not mention on side effects, some patients complained of having loose stool [61,62], abdominal cramps, anorexia, and diarrhoea (Table 2) [61].
Case series studies
The characteristics of the case series studies (studies not discussed elsewhere) included in this review are given in Table 3 [49,50,55–57]. So far only two [49,50] randomized control trial results have been reported (Table 3). For statistical interpretation, we have divided case series studies into 2 cohorts including the case series, with and without a control arm. Additionally, we have pooled the results of all reported case series studies published so far [29–36], including the studies previously discussed elsewhere [42,43,53], to obtain a larger sample set for analysis for the FMT intervention.
Table 3.
Characteristics of case-series studies (non-duplicate) with and without control arm included for the review.
| Bar-Yoseph et al. [55] | Davido et al. [57] | Huttner et al. [50] | Leo et al. [49] | Saidani et al. [56] | ||
|---|---|---|---|---|---|---|
| Type and place of study | Prospective cohort study, Israel | Pilot prospective monocenter study, France | Multicenter randomized superiority trial, Switzerland, Netherlands, France and Israel | Multicenter randomized clinical trial, Switzerland, Netherlands, France and Israel | A single-center case-control retrospective study | |
| Subjects details | Age range | 21.8–81.3 years | 50–80 years | 23–89 years | 18–64 years | 22–88 years |
| Participants No: | 15 | 08 | 22 | 16 | 10 | |
| Male (M): Female (F) | 10:5 | 5:3 | 10:12 | 8:8 | 8:2 | |
| Indication/colonization status |
K. pneumoniae- KPCa and OXA-48 E. coli- ESBL+b, NDMc, OXA-48, E. cloacae- KPC, E. hormechai- KPC, K. oxytoca- KPC, S. marcescens- KPC C. freundii- KPC |
Cd, Van-A/Van-B |
E. coli – ESBL+, OXA and NDM, K. pneumoniae- ESBL+, E. cloacae- ESBL+, C. freundii- ESBL+, |
ESBL-E and CPE |
K. pneumoniae-OXA-48 and NDM-1, E. coli – OXA-48, E. cloacae-– OXA-48, S. marcescens- OXA-48, A. baumanii- OXA-24, C. freundii- OXA-48, C. koseri- OXA-48 |
|
| Colonization confirmation | Cell cultures and PCRe from 5 samples of rectal swab in the last 6 months | PCR method to determine Van-A/Van-B from the samples taken from a rectal swab | Stool culture | Rectal swab was taken and species identification was done through MOLDI-TOFf resistance patterns via and ABSTsg and RT-PCRsh. | ||
| Pre treatment | Antibiotic | NAi | NA | colistin sulphate and neomycin sulphate tablets for 5 days | Colistin/neomycin | Based upon the type of resistance strain, colistin, and aminoglycosides (amikacin or gentamicin) or sulfadiazine/fusidic acid |
| PPIj | PPI given prior to pre-FMT fasting | PPI given 2 days prior to FMT | Omeprazole 20 mg at the evening of 1 day prior to FMT and the morning of the FMT procedure | NA | Pantoprazole 40 mg twice a day since from 2 days before to FMT | |
| Bowel cleansing | 12 h fasting | Bowel lavage 1 day prior to FMT | NA | NA | First and second bowel wash in 5 days and 1 day before, respectively to the FMT | |
| Donor screening tests |
See Supplementary information, Section 5 | Screened for infectious, metabolic and immune diseases | Done according to the French Agency for the Safety of health Products | According to the 2014 French guidance document for use of FMT in clinical trialsk. | According to the 2014 French guidance document for use of FMT in clinical trials. | NMl |
| FMT | Donor | Unrelated | Unrelated (n = 2) |
Unrelated | Unrelated (n = 7) |
Unrelated |
| Status of intervention sample | frozen faecal capsules | Frozen sample (−80 oC) |
Faecal capsules made up with 80% of glycerol | oral capsules and nasogastric tube | Aseptically prepared sample | |
| Dilution | NA | 1–5 ml of saline per 1 g of faeces | 40 g of stool in 80 ml to prepare the capsules | 40 g of stool in 80 ml of saline | 50 g of stool diluted in 0.9% NaCl 300–400 ml | |
| Dose | 15 capsules/day for 2 days | Five 50 cc syringes | 15 capsules in two consecutive days | 15 capsules in two consecutive days in 2 centres and 80 ml of FMT preparation on a single day in remaining centres | 50g/300 ml in single or double dose | |
| Route | Oral gavage | Nasoduodenal tube | Nasogastric administration | Nasogastric tube | Nasogastric tube or gastrostomy tube | |
| Primary outcome at 1 month time point | CPEm decolonization rate > 50% | VRE decolonization rate was > 50% at one-month time point and it was 87.5% at 3 months. | 40.9% decolonization rate was achieved at 1-month time point | Enterobacteriaceae was lower compared to baseline but without statistical significance | 80% decolonization rate was observed at 1-month time point | |
| Adverse effects | None | None | 90% of the patients in the intervention group have at least 1 adverse event and 4 patients had severe adverse events | None | None | |
| Follow up time | 6 months | 3 months | 7 months | 7 months | 6 months |
aK. pneumoniae carbapenemase; bExtended spectrum β-lactamase; cNew-Delhi metallo-β-lactamase; dVancomycin-resistant Enterococcus; epolymer chain reaction; fMatrix-assisted laser desorption/ionization; gantibiotic sensitivity testing; hReal-time PCRs; iNot applicable; jproton pump inhibitor; khttps://ansm.sante.fr/var/ansm_site/storage/original/application/5e5e01018303790194275ded0e02353c.pdf; lNot mentioned; mcarbapenemase-producing Enterobacteriaceae.
Primary outcome (decolonization of AMRs) for the case series studies without a control arm
Including the two-case series studies [55,57] listed in Table 3, nine studies were included for the meta-analysis [29,32–36]. The proportion of decolonization shows that FMT was successful in decolonizing antibiotic-resistant bacteria from the gut of participants in 55.9% (n = 57/102) of the cases [0.58 95% confidence interval (CI) 0.42–0.74], and presented in a forest plot (Figure 3).
Figure 3.
Forest plot, meta-analysis of proportions for decolonization success at 1 month.
Primary outcome (decolonization of AMRs) for the case series studies with a control arm
All 111 participants were included in the intention-to-treat analysis of the primary outcome, of whom 57 received FMT and 54 received no treatment. Significantly, more patients receiving donor FMT achieved clinical remission at the 1-month time point compared with those receiving control interventions, with a pooled RR of not achieving remission of 0.44 (95% CI: 0. 20–0.99) (p = .03) with an I2 = 65% (forest plot, Figure 4). The pooled rate of clinical remission in all 4 trials was 63.2% (n = 36/57) in the group receiving donor FMT and 22.2% (n = 12/54) in those receiving control interventions. Statistical assessment for publication bias was not performed because only 4 included trials were inadequate for funnel plots or regression-based assessments. Altogether, the forest plots obtained from the meta-analysis (Figures 3 and 4) point towards favouring FMT as an alternative treatment modality for the decolonization of AMR bacteria in the gut.
Figure 4.
Forest plot of all case series studies reporting AMR remission at 1 month time point.
Assessment of heterogeneity
Given moderate heterogeneity (I2 = 65%), the moderate 95% CI (0.2–0.99), and the relatively small number of trials, we performed subgroup analyses for the randomized clinical trials [51,52] to explore possible explanations for the inconsistency (Figure 5). It is apparent from Figure 5 that among rigorous randomized clinical trials, FMT was associated with decolonization of AMR bacteria, with a low heterogeneity (RR 0.37; 95% CI 0.18–0.79; I2 = 23%) encouraging more randomized clinical trials in the field to ascertain a better understanding of FMT intervention.
Figure 5.
Forest plot of sub group analysis of randomized clinical trials for AMR remission at 1 month time point.
Figure 6.
Important steps to be followed in future rigorous randomized clinical trials.
Apart from the lack of a rigorous experimental setting, other reasons also contributed to the overall moderate heterogeneity. We observed clinical heterogeneity among studies with the type of colonizing AMR bacteria (Gram-negative and Gram-positive bacteria), and their diverse resistance mechanisms including; OXA-48, OXA-24, KPC, ESBL, NDM-1, and Van A. Overall, the male patient ratio is higher than female, except in Huttner et al. [50], where there more female participants and an equal ratio was obtained in Leo et al. (Table 3) [49]. The inter-study variability of the patient preparation was also significant, such as pre-antibiotic treatment [49,50,56], use of PPIs (omeprazole or pantoprazole) before FMT [50,55–57], bowel lavage [56,57] or 12 h fasting (Table 3) [55].
Regarding the intervention of FMT, the method of sample preparation was somewhat identical. In all cases, the donors were unrelated and the intervention was in the form of capsules, except in two studies where the samples were aseptically prepared in saline and administered (Table 3) [56,57]. In most studies FMT was administered twice for each subject and on consecutive days [49,50,55,56].
FMT susceptible AMRs and their decolonization time points
The time frame achieved for the decolonization with respect to their resistance mechanism was also analysed as percentage decolonization at 1, 2, and 4 weeks (1 month) after FMT, and the results are presented in Table 4. The decolonization rates were within 33.3-100% at the one-month time point (Table 4) with the highest (100%) decolonization rate for AMRs in Enterobacter hormechai (n = 1), Klebsiella oxytoca (n = 1), Citrobacter freundi (n = 3), Acinetobacter baumanii (n = 1), and Citrobacter koseri (n = 1) (Table 4) and the lowest against Serratia marcescens with KPC (n = 2) (Table 4). However, it is worth noting that the sample size is inadequate to draw a robust conclusion for the effectiveness of FMT against these strains.
Table 4.
Decolonization of different pathogens according to their resistance mechanisms at different time points.
| AMRs | Resistance mechanism | Decolonization (1 W) |
Decolonization (2 W) |
Decolonization (1 M) |
% decolonization bacteria of the bacteria at 1 M time point | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ndeca | ntotb | %Decc | ndec | ntot | %Dec | ndec | ntot | %Dec | |||
| K. pneumoniae | OXA-48 | 4 | 11 | 36.3 | 7 | 11 | 63.6 | 8 | 11 | 72.7 | 69.5 |
| KPCd | 1 | 3 | 33.3 | 1 | 3 | 33.3 | 1 | 3 | 33.3 | ||
| ESBLe | NMf | 7 | NAg | NM | 7 | NA | 6 | 7 | 85.7 | ||
| NDM-1h | 1 | 2 | 50.0 | 1 | 2 | 50.0 | 1 | 2 | 50.0 | ||
| E. coli | NDM | NA | 3 | NA | 1 | 3 | 33.3 | 1 | 3 | 33.3 | 52.6 |
| OXA/OXA-48 | 1 | 5 | 20.0 | 2 | 5 | 40.0 | 4 | 5 | 80.0 | ||
| ESBL | NM | 11 | NA | NM | 11 | NA | 5 | 11 | 45.5 | ||
| E. hormechai | KPC | NM | 1 | NA | 1 | 1 | 100.0 | 1 | 1 | 100.0 | 100 |
| E. cloacae | KPC | NM | 2 | NA | 0 | 2 | 0.0 | 1 | 2 | 50.0 | 75 |
| OXA-48 | 1 | 1 | 100 | 1 | 1 | 100 | 1 | 1 | 100.0 | ||
| ESBL | NM | 1 | NA | NM | 1 | NA | 1 | 1 | 100.0 | ||
| K. oxytoca | KPC | NM | 1 | NA | 0 | 1 | 0.0 | 1 | 1 | 100.0 | 100 |
| S. marcescens | KPC | NM | 2 | NA | 1 | 2 | 50.0 | 0 | 2 | 0.0 | 33.3 |
| OXA-48 | 0 | 1 | 0.0 | NM | 1 | NA | 1 | 1 | 100.0 | ||
| C. freundii | KPC | NM | 1 | NA | 0 | 1 | 0.0 | 1 | 1 | 100.0 | 100 |
| OXA-48 | 1 | 1 | 100.0 | 1 | 1 | 100.0 | 1 | 1 | 100.0 | ||
| NDM-1 | NM | 1 | NA | NM | 1 | NA | 1 | 1 | 100.0 | ||
| A. baumanii | OXA-24 | 1 | 1 | 100.0 | 1 | 1 | 100.0 | 1 | 1 | 100.0 | 100 |
| C. koseri | OXA-48 | 1 | 1 | 100.0 | 1 | 1 | 100.0 | 1 | 1 | 100.0 | 100 |
| VREi | Van-A | NM | 8 | NA | NM | 8 | NA | 5 | 8 | 62.5 | 62.5 |
aNumber of decolonizations; btotal number; cpercentage decolonization; dKlebsiella pneumoniae carbapenemase; eextended spectrum β-lactamase producing; fnot mentioned; gnot applicable; hNew Delhi metallo-β-lactamase-1; ivancomycin-resistant enterococci.
Ongoing and completed clinical trials not published
We have extended our background search on different clinical trial registries and found that twenty-two (n = 22) more clinical trials have already been registered to investigate AMR decolonization of the gut via FMT. In that, twelve (n = 12), three (n = 3), six (n = 6), and one (n = 1) studies are randomized, non-randomized, interventional and observational clinical trials, respectively (Table 5). Out of the 12 randomized clinical trials, two studies were (n = 2/12) already completed, but results have not been published. A summary of all the clinical trials is given in Table 5.
Table 5.
Characteristics of ongoing clinical trials.
| Trial no./title | Primary outcome | Secondary outcome | Participants/age | Type of study (type/mask) | Country | Status |
|---|---|---|---|---|---|---|
| NCT02472600/Eradication of Antibiotic-resistant Bacteria Through Antibiotics and Faecal Bacteriotherapy (R-GNOSIS WP3) | Intestinal carriage of ESBL-E/CRE 35 to 48 days after randomization | adverse event, Comparison of the global microbiota composition and diversity | 39/adults | Randomized/parallel open label | Switzerland | Active 02/2017 to 03/2018 |
| NCT02922816/FMT for MDRO Colonization After Infection in Renal Transplant Recipients (PREMIX) | The safety and feasibility of using FMT in adult participants with Target MDRO colonization after infection, Change in Target MDRO Growth | Not mentioned | 20/Adults | Randomized/parallel open label | USA | Active 12/2016 to 06/2021 |
| NCT03061097/Autologous Faecal Microbiota Transplantation to Prevent Antibiotic Resistant Bacteria Colonization | Number of participants with NIH Grade ≥2 adverse events at Day 7 after randomization. | Number of patients with clearance of ARB among patients colonized at Day 28 | 7/Adults | Randomized/single open label | USA | Active 07/2017 to 06/2019 |
| NCT03063437/A Trial of Encapsulated Faecal Microbiota for Vancomycin Resistant Enterococcus Decolonization | Percentage of Participants With VRE Decolonization | Percentage of Participants With VRE Infection, VRE Decolonization Among Immunocompromised Patients | 9/Adults | Randomized/parallel assignment, quadraple | USA | Completed 06/2020 |
| NCT03643887/Trial of Faecal Microbiota Transplant (FMT) for VRE and CRE Patients | Compare incidence of VRE/CRE decolonization between FMT Capsule | VRE/CRE infection at Day 3, Day 10, and Week 4 following randomization. | 90/Adults | Randomized/double blind | USA | Active 09/2022 to 09/2025 |
| NCT03802461/Effectiveness of Faecal Flora Alteration for Eradication of CPE Colonization | Incidence of CPE colonization in FMT arm vs control arm at 3 months | Incidence of CPE decolonization in FMT-treatment and non-treatment groups at 1, 6 and 12 months, Number of patients with all-cause mortality at 30 days post-randomization | 40/Adults | Randomized/parallel open label | Canada | Recruiting 03/2019 to 12/2020 |
| NCT04146337/Faecal Microbiota Transplantation for CPE | Number of participants achieving CRE eradication at 28 days | Number of participants who died by 28-day and 6-month, Number of participants with CRE bacteraemia and any bacteraemia, Adverse events | 60/Adults | Randomized/parallel open label | Israel | Recruiting 10/2020 to 06/2022 |
| NCT04181112/Faecal Transplant for MDRO Decolonization | The elimination of the target MDR organism | Compare proportions, type and timing of adverse events post-FMT, Proportions and timing of recolonization over 180 days | 90/Adults | Randomized/parallel open label | Canada | Recruiting 11/2019 to 11/2023 |
| NCT04188743/Decolonization of Gram-negative MDRO With Donor Microbiota (FMT) | Number of participants with decolonization success/failure | Side effects, Treatment effect on microbial community | 150/Adults | Randomized/quadraple | Belgium | Recruiting 12/2019 to 12/2023 |
| NCT04431934/Efficacy of a Probiotic or FMT on the Eradication of Rectal MDR Gram-negative Bacilli (MDR-GNB) Carriage (PROFTMDECOL) (PROFTMDECOL) | Proportion of patients with digestive decolonization rate defined as negative rectal swab (RS) for the target MDR-GNB (ESBL-producing K. pneumoniae, CPE and MDR/XDR P. aeruginosa) at the end of study (60 ± 7 days after the randomization) | Any changes with baseline after 1 week, 1 year | 437/Adults | Randomized/parallel open label | Spain | Active/Not recruiting 06/2020 to 07/2023 |
| NCT03061097/Autologous FMT to Prevent AMR Bacteria Colonization (RACE) | Number of Participants With Adverse Events (NIH Grade ≥2) at Day 7 After Randomization | Number of patients with clearance of ARB among patients colonized at Day 28 by PCR assay | 33/Adults | Randomized/parallel multiple | Not mentioned | Completed 12/2020 |
| ACTRN12617000561381/Gastrointestinal eradication of MDR Gram negative bacteria by FMT | Relative abundance of Gram-negative pathogenic organisms in the stool microbial community as assessed by next generation sequencing 1 year of post FMT | Number of episodes of infection, as assessed by positive culture of clinical specimen (not faeces) for resistant Gram-negative organism with same resistance mechanism | Not mentioned/Adults | Randomized/Double blind | Australia | Recruiting not mentioned |
| NCT02592343/A Prospective Trial of Lyophilised Faecal Microbiota Transplantation for Recurrent C. difficile Infection | Efficacy of lyophilised FMT for treatment of recurrent C. difficile infection | Evaluate treatment failure rate as defined by persistence of diarrhoea and a positive C. difficile toxin assay | 100/Adults | Non-randomized/single open label | Canada | Completed 01/2020 |
| NCT03050515/FMT for the treatment of recurrent urinary tract infections | Change in frequency of culture proven urinary tract infections following faecal transplant | Change in the gut microbiome following faecal transplantation measured via 16 s sequencing of stool samples | 12/Adults | Non-randomized/single open label | USA | Completed 02/2020 |
| NCT02543866/FMT as a Strategy to Eradicate Resistant Organisms | Incidence, severity, and relatedness of solicited, unsolicited, and serious adverse events | Proportion of subjects free from ESC-R intestinal colonization and recurrent ESC-R infections 2 days, 2 weeks, 4 weeks, 8 weeks, 6 months, and 12 months post-FMT | 20/Adults | Non-randomized/single open label | USA | Recruiting 02/2017 to 02/2024 to |
| NCT02312986/FMT for MDR organism reversal | Safety of FMT in patients with recurrent MDRO infections | Proportion of subjects free from recurrent MDRO infections 30 days, 6 months, and 12 months post-FMT. | 20/adults | Interventional/single open label | USA | Active 05/2015 to 06/2020 |
| NCT02816437/FMT for MDRO Colonization in Solid Organ Transplant (FMT) | Number of participants with adverse events | Rate of MDRO decolonization, rate of recurrent MDRO infection | Not mentioned/Adults | Interventional/single open label | USA | Recruiting 07/2016 to 09/2022 |
| NCT03029078/FMT, a Hope to eradicate colonization of patient harbouring XDR bacteria? | Negative result of the rectal swab performed, free from CRE or GRE | Study with a universal super donor in order to improve efficacy | 50/Adults | Interventional/single open label | France | Active 11/2014 to 01/2024 |
| NCT03167398/FMT for eradication of CRE | 3 consecutive negative rectal samples for CRE after 1 month of trial | Not mentioned | 15/Adults | Interventional/single open label | Israel | Completed 01/2020 |
| NCT03479710/FMT for CRE/VRE | Absence of intestinal colonization of CRE/VRE | Incidence, severity and relatedness of adverse events, changes in intestinal microbiota | 40/Adults | Interventional Parallel open label | Hong Kong | Recruiting 02/2018 to 12/2019 |
| NCT03367910/FMT for MDRO UTI | FMT safety: adverse events during and after FMT | Risk of recurrent UTI post-FMT will be evaluated | 60/Adults | Interventional/single open label | USA | Active 02/2018 to 06/2021 |
| NCT04583098/The Effect of FMT on the decolonization of MDR Organisms | successful decolonization of CPE or VRE in the gut within 3 months | Not mentioned | 100/Adults | Observation/Prospective cohort | Korea | Active 03/2019 to 03/2022 |
Discussion
According to the contemporary guidelines from the Infectious Diseases Society of America (IDSA) and the Society of Healthcare Epidemiology of America (SHEA), as well as the European Consensus Guidelines, FMT is recommended as a second-line treatment modality against recurrent C. difficile infection, due to over 90% efficacy in randomized control trials [6]. Our analysis in this study points towards support of decolonization of ESKAPE pathogens with FMT intervention (Table 6). However, RCTs and sample sizes are still limited, and in addition, lack of standardized protocol and their demonstration of improvement in clinical endpoints has been inconsistent. Therefore, RCTs involving larger sample size and consensus on standardized protocols are warranted.
Table 6.
Decolonization status of ESKAPE pathogens of the included clinical studies.
| Study | ESKAPE pathogen/s | Decolonization status |
|
|---|---|---|---|
| Yes | NO | ||
| Biliński et al. [61] | K. pneumoniae NDM+ and E. coli ESBL | * | |
| Stalenhoef et al. [62] | MDR P. aeruginosa and MDR E. coli | PAa | ** ECb |
| Grosen et al. [58] | ESBL+ K. pneumoniae | ||
| Soto et al. [64] | None | ||
| Biernat et al. [60] | ESBL + E. coli and K. pneumoniae, E. faecium GRE | ECc | |
| Bahl et al. [59] | KPC-producing XDR K. pneumoniae | ||
| Ueckermann et al. [64] | MDR K. pneumoniae | ||
| Bar-Yoseph et al. [55] | K. pneumoniae- KPCa and OXA-48 E. coli- ESBL+b, NDMc, OXA-48 | ||
| Davido et al. [57] | VRE | ||
| Huttner et al. [50] | E. coli – ESBL+, OXA and NDM, K. pneumoniae- ESBL | ||
| Leo et al. [49] | ESBL-E.coli and CPE | EC | |
| Saidani et al. [56] | K. pneumoniae-oxa-48 and NDM-1, E. coli – OXA-48, A. baumanii- OXA-24, E. cloacae-– OXA-48 | ||
aP. aeruginosa; bESBL E.coli was eradicated but drug sensitive E.coli detected upon FMT; cRemission rate was not significant compared to control.
*Green colour highlighted box represents as decolonization status “yes”.
**Red colour highlighted box represents as decolonization status “No”.
The human gut contains up to 3.8 × 1013 bacteria that represent around 55% of stool mass [67]. Therefore, selecting a healthy donor without an intact gut microbial composition plays an important role. Similarly, the direct correlation between the effectiveness of the FMT with the pre-bowel preparation of the receptor is an equally important component for successful transplantation. Based on the studies included in this review, it is considered that an optimised FMT protocol should include: (i) rigorous donor screening procedures including, not having taken antibiotics, immunosuppressants, chemotherapy, and PPIs in recent <3 months [50,68], (ii) decontamination of nasopharyngeal colonized sites prior to FMT [56] (iii) ≥5 days prolonged treatment with high dose of appropriate antibiotic/s regimen to reduce the diversity of gut microflora and discontinue 48 h prior to prime the gut for FMT [49,50,56,58,59,61,62] (iv) two bowel cleansing regimens (one before antibiotic treatment and the other before FMT) [56] or at least (one day before FMT) [57,61] to cleanse the intestinal residues (v) adhere to strict post-FMT decolonization measures (isolation, disinfect the environment and remove catheters or other non-essential medical parts connected) and follow up (at least 3–6 months) with regular stool testing to confirm the sustainable decolonization (Figure 6).
It is worth notice that several studies [50,55–57,61] have used PPIs just before FMT, in view of protecting the transplanting microbiota from gastric acids. However, its evidence for the benefit as a pre-treatment for FMT is controversial [69], since it has been reported that PPIs are associated with an increased risk of CDI [70] and other enteric infections [71]. Also, they can alter the gut microbiota by expanding the Enterococcus and Streptococcus genera and increasing other bacterial genes associated with epithelial invasion [72,73]. Furthermore, a meta-analysis from Hong et al. [74] proved there was no statistically significant benefit from the routine use of pre-treatment with PPIs in the FMT protocol compared to no PPI-used protocols.
Even though the mechanistic studies are scanty to reveal the exact mechanism of action of FMT towards decolonization of drug-resistant bacteria, some important observations made during the studies help to speculate that FMT may have a strain-specific mechanism of action apart from general criteria like; bile-salt metabolism, GI luminal pH, and competition for resources.
Caballero et al. [66] conducted an FMT on mice co-colonized with VRE and K. pneumoniae those who are residing in the same region of the GI tract (lower GI tract). Unlike in most closely related species [75–78], these two strains did not show colonization resistance to each other due to nutrient competition. This may be attributed generally to their different metabolic requirements as well as their ability to switch nutrient precursors in the presence of competing strains [66]. However, investigators specifically observed that the antibiotic pre-treated control group demonstrated a thickening of the mucus layer by K. pneumoniae compared to VRE, indicating their high permeability towards the mucus layer, during the weak expression of host antimicrobial molecules such as RegIIIγ upon pre-antibiotic treatment [79]. This mucus infiltration, consequently increased K. pneumoniae translocation to mesenteric lymph nodes (mLNs) relative to VRE. Co-colonization and K. pneumoniae eventually increased VRE translocation too, via opening up the barrier towards mLNs. Now, the more diverse microbiota in FMT can largely colonize the intestine, while the K. pneumoniae and VRE are translocated towards mLNs and the complete eradication was observed in both pathogens upon FMT, which means their translocation is continuous and no replication is taking place within mLNs. Even though the exact mechanism is yet to be identified, previous studies have speculated that [80,81] cells within the colonic lamina propria, including CD103+ and CX3CR1+ dendritic cells, are believed to capture K. pneumoniae and carry them to mLNs.
In another in vivo study [65], mice were colonized to mimic two clinical conditions like the status of depleted gut microbiota and humanised mice, challenged with a high load of MDR P. aeruginosa (1 × 109 CFU/g of faeces). In both cases, up to a 4-log10 reduction of MDR P. aeruginosa was observed upon single FMT and in a humanised model, a significant depletion of MDR carrier rate (>50%) was also observed with murine FMT at the 1-week time point. According to quantitative analysis byqRT-PCR with group-specific 16S rRNA, there was a decrease of Enterobacteria, Enterococci, Bacteroides/Prevotella species, and Clostridia, whereas the numbers of Lactobacilli, Bifidobacteria, and mouse intestinal Bacteroides were higher in the faeces derived post-FMT as compared to the pre-FMT status. Therefore, investigators hypothesised the mechanism behind the reduction of MDR P. aeruginosa burden was due to the higher loads of Lactobacilli and Bifidobacteria and for their pronounced production of bacteriocins and short chain fatty acids [82,83].
In a case study [59] of a 69 year-old woman referred with severe recurrent CDI and complicated by intestinal co-colonization with KPC-producing bacteria, XDR K. pneumoniae was successfully decolonized by a single FMT treatment. Interestingly, 16S rRNA amplicon profiling revealed Enterobacterales constituted 18% of the microbiota before FMT and subsequently dropped to lower levels after the FMT by increasing butyrate-producing Faecalibacterium prausnitzii. This species has been associated with treatment success and a mechanism for butyrate-induced reduction of intestinal inflammation and bacterial translocation of the C. difficile pathogen [84]. A similar observation was also made by Billinski et al. [60], where VRE decolonization was observed in a case study of an immunocompromised male patient (51 years). On the same note, the mechanism behind this decolonization was explained previously through in vivo mice model [85], in that the eradication may be associated with direct inhibition of VRE by a single component of healthy gut microbiota belonging to Barnesiella species. However, extensive studies with long-term follow-ups are warranted to determine the stability of this effect.
By using 16S rRNA metagenome sequencing, a substantial increment of Bifidobacterium bifidum was noted at post-FMT of a case series study conducted to decolonize CPE [55]. This species was shown to possess anti-Enterobacteriaceae effects [86] and anti-lysozyme activity [87], decrease biofilm formation [88], and modulate virulence gene expression [89] alone and with the combination of lactitol and Lactobacillus acidophilus to reduced OXA-48-producing Enterobacteriaceae [90]. These might explain the mechanism of action of B. bifidum in the decolonization of CPE in the gut.
Tavoukjian [53], have included 5 case series studies alone and according to the meta-analysis, a higher remission rate upon FMT was observed against P. aeruginosa while the lowest was against K. pneumoniae with NDM-1 and ESBL-producing strains, at the 1-month time point. These findings are in line with the analysis outcome of our systematic review, and with a comparatively lower decolonization rate for E. coli with NDM-1 (33.3%) and ESBL (45.5%) and K. pneumoniae with KPC (33.3%) (Table 4). The literature review by Amrane and Lagier [43], similarly and qualitatively, updated the recent literature.
The application of FMT for the decolonization of MDR bacteria is still in the early stage of development. Most of the eligible studies are not randomized control trials, except Huttner et al. [50] and Leo et al. [49] The effect of FMT alone is still undefined, whether the role of antibiotics and PPIs prior to FMT or other forms of priming was essential, and the possibility of spontaneous decolonization might also play a role. Therefore, further rigorous randomized control trials with the inclusion of suitable control arms are warranted to establish the therapeutic efficacy of FMT.
Conclusion
In summary, there are limited existing studies which are generally of low quality with moderate heterogeneity, and do not allow definitive conclusions to be drawn. More rigorous RCTs with larger sample size and standardized protocols on FMTs for gut decolonization of AMR organisms are warranted.
Glossary
Abbreviations
- AMR
antimicrobial resistant
- AR
antibiotic resistant
- CDI
Clostridioides difficile infection
- CFU
colony forming unit
- CI
confidence interval
- CR
colonization resistant
- EARS
European Antimicrobial Resistance Surveillance Network
- ESBL
extended spectrum β-lactamase
- FMT
faecal microbiota transplantation
- GI
gastrointestinal
- IDSA
Infectious Diseases Society of America
- JBI
Joanna Briggs Institution
- KPC
Klebsiella pneumoniae carbapenemase
- MDR
multidrug-resistant
- mLNs
mesenteric lymph nodes
- NDM
New Delhi metallo-β- lactamase
- NGS
next generation sequencing
- PPIs
proton pump inhibitors
- RCT
randomized clinical trials
- RR
risk ratio
- RT-PCR
real-time polymer chain reaction
- SCFA
short chain fatty acids
- SHEA
Society of Healthcare Epidemiology of America
- US
United States
- VRE
vancomycin-resistant enterococcus
- XDR
Extensively drug-resistant
Funding Statement
The study was partially funded by a seed fund for gut microbiota research provided by the Faculty of Medicine, The Chinese University of Hong Kong and from the Health and Medical Research Fund (Project number 18170082, PI: MI), Food and Health Bureau of the Hong Kong Special Administrative Region, People’s Republic of China. The funding bodies did not involve in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Disclosure statement
The authors report no financial or personal conflicts of interest.
References
- 1.World Health Organization [Internet]. Antimicrobial resistance: global report on surveillance. Geneva (Switzerland): WHO; 2014. [cited 2020 Dec 23]. Available from: https://eur03.safelinks.protection.outlook.com
- 2.Centers for Disease Control and Prevention [Internet]. Antibiotic resistance threats in the United States. Atlanata (GA): CDC; 2019. [cited 2020 Dec 23]. Available from: https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf
- 3.Rice LB. Federal funding for the study of antimicrobial resistance in nosocomial pathogens: no ESKAPE. J Infect Dis. 2008;197:1079–1081. [DOI] [PubMed] [Google Scholar]
- 4.European Centre for Disease Prevention and Control [Internet]. European antimicrobial resistance Surveillance Network (EARS-Net). Stockholm city (Sweden); 2020. [cited 2020 Dec 23]. Available from: www.ecdc.europa.eu/en/about-us/partnerships-and-networks/disease-and-laboratory-networks/ears-net
- 5.Ducarmon QR, Zwittink RD, Hornung BVH, et al. Gut microbiota and colonization resistance against bacterial enteric infection. Microbiol Mol Biol Rev. 2019;83(3):1–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim S, Covington A, Pamer EG.. The intestinal microbiota: antibiotics, colonization resistance, and enteric pathogens. Immunol Rev. 2017;279:90–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Durack J, Lynch SV.. The gut microbiome: relationships with disease and opportunities for therapy. J Exp Med. 2019;216:20–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sommer F, Bäckhed F.. The gut microbiota-masters of host development and physiology. Nat Rev Microbiol. 2013;11:227–238. [DOI] [PubMed] [Google Scholar]
- 9.Keeney KM, Yurist-Doutsch S, Arrieta MC, et al. Effects of antibiotics on human microbiota and subsequent disease. Annu Rev Microbiol. 2014;68:217–235. [DOI] [PubMed] [Google Scholar]
- 10.Simone Becattini YT. Antibiotic-induced changes in the intestinal microbiota and disease. Trends Mol Med. 2017;22:458–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Forgacs I, Loganayagam A.. Overprescribing proton pump inhibitors. BMJ. 2008;336:2–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wei L, Ratnayake L, Phillips G, et al. Acid-suppression medications and bacterial gastroenteritis: a population-based cohort study. Br J Clin Pharmacol. 2017;83:1298–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hafiz RA, Wong C, Paynter S, et al. The risk of community-acquired enteric infection in proton pump inhibitor therapy: systematic review and meta-analysis. Ann Pharmacother. 2018;52(7):613–622. [DOI] [PubMed] [Google Scholar]
- 14.Bavishi C, DuPont HL.. Systematic review: the use of proton pump inhibitors and increased susceptibility to enteric infection. Aliment Pharmacol Ther. 2011;34:1269–1281. [DOI] [PubMed] [Google Scholar]
- 15.Morgan AP, Crowley JJ, Nonneman RJ, et al. The antipsychotic olanzapine interacts with the gut microbiome to cause weight gain in mouse. PLoS One. 2014;9(12):e115225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lieberman LA, Higgins DE.. A small-molecule screen identifies the antipsychotic drug pimozide as an inhibitor of Listeria monocytogenes infection. Antimicrob Agents Chemother. 2009;53:756–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dastidar SG, Chaudhury A, Annadurai S, et al. In vitro and in vivo antimicrobial action of fluphenazine. J Chemother. 1995;7(3):201–206. [DOI] [PubMed] [Google Scholar]
- 18.Jeyaseeli L, Dasgupta A, Dastidar SG, et al. Evidence of significant synergism between antibiotics and the antipsychotic, antimicrobial drug flupenthixol. Eur J Clin Microbiol Infect Dis. 2012;31(6):1243–1250. [DOI] [PubMed] [Google Scholar]
- 19.D’Costa VM, McGrann KM, Hughes DW, et al. Sampling the antibiotic resistome. Science (80-). 2006;311(5759):374–377. [DOI] [PubMed] [Google Scholar]
- 20.Wright GD. The antibiotic resistome: the nexus of chemical and genetic diversity. Nat Rev Microbiol. 2007;5:175–186. [DOI] [PubMed] [Google Scholar]
- 21.Liu L, Chen X, Skogerbø G, et al. The human microbiome: a hot spot of microbial horizontal gene transfer. Genomics. 2012;100:265–270. [DOI] [PubMed] [Google Scholar]
- 22.Huddleston JR. Horizontal gene transfer in the human gastrointestinal tract: potential spread of antibiotic resistance genes. Infect Drug Resist. 2014;7:167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lerner A, Matthias T, Aminov R.. Potential effects of horizontal gene exchange in the human gut. Front Immunol. 2017;8:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Panek M, Čipčić Paljetak H, Barešić A, et al. Methodology challenges in studying human gut microbiota-Effects of collection, storage, DNA extraction and next generation sequencing technologies. Sci Rep. 2018;8(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Petriz BA, Franco OL.. Metaproteomics as a complementary approach to gut microbiota in health and disease. Front Chem. 2017;5:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim KO, Gluck M.. Fecal microbiota transplantation: an update on clinical practice. Cli Endos. 2019;52:137–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bakken J, Borody T, Brandt L, et al. Treating Clostridium difficile infection with fecal microbiota transplantation. Clin Gastro Hepa. 2011;9:1044–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gupta S, Allen-Vercoe E, Petrof EO.. Fecal microbiota transplantation: in perspective. Therap Adv Gastroenterol. 2016;9:229–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Battipaglia G, Malard F, Rubio MT, et al. Fecal microbiota transplantation before or after allogeneic hematopoietic transplantation in patients with hematologic malignancies carrying multidrug-resistance bacteria. Haematologica. 2019;104:1682–1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dubberke ER, Mullane KM, Gerding DN, et al. Clearance of vancomycin-resistant Enterococcus concomitant with administration of a microbiota-based drug targeted at recurrent Clostridium difficile infection. Open Forum Infect Dis. 2016;3:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eysenbach L, Allegretti JR, Aroniadis O, et al. Clearance of vancomycin-resistant Enterococcus colonization with fecal microbiota transplantation among patients with recurrent Clostridium difficile infection. Open Forum Infect Dis. 2016;3(1):2119. [Google Scholar]
- 32.Lombardo MJ, Vulic M, Ohsumi T, et al. Vancomycin-resistant enterococcal iters diminish among patients with recurrent Clostridium difficile infection after administration of SER-109, a novel microbiome agent. Open Forum Infect Dis. 2015;2(1):757. [Google Scholar]
- 33.Bilinski J, Grzesiowski P, Sorensen N, et al. Fecal microbiota transplantation in patients with blood disorders inhibits gut colonization with antibiotic-resistant bacteria: results of a prospective, single-center study. Clin Infect Dis. 2017;65(3):364–370. [DOI] [PubMed] [Google Scholar]
- 34.Singh R, De Groot PF, Geerlings SE, et al. Fecal microbiota transplantation against intestinal colonization by extended spectrum beta-lactamase producing Enterobacteriaceae: a proof of principle study ISRCTN48328635 ISRCTN. BMC Res Notes. 2018;11(1):4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dinh A, Fessi H, Duran C, et al. Clearance of carbapenem-resistant Enterobacteriaceae vs vancomycin-resistant enterococci carriage after faecal microbiota transplant: a prospective comparative study. J Hosp Infect. 2018;99:481–486. [DOI] [PubMed] [Google Scholar]
- 36.Davido B, Batista R, Michelon H, et al. Is faecal microbiota transplantation an option to eradicate highly drug-resistant enteric bacteria carriage? J Hosp Infect. 2017;95:433–437. [DOI] [PubMed] [Google Scholar]
- 37.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015 statement. Syst Rev. 2015;4:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Odamaki T, Kato K, Sugahara H, et al. Age-related changes in gut microbiota composition from newborn to centenarian: a cross-sectional study. BMC Microbiol. 2016;16(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Agans R, Rigsbee L, Kenche H, et al. Distal gut microbiota of adolescent children is different from that of adults. FEMS Microbiol Ecol. 2011;77:404–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Le Bastard Q, Ward T, Sidiropoulos D, et al. Fecal microbiota transplantation reverses antibiotic and chemotherapy-induced gut dysbiosis in mice. Sci Rep. 2018;8(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lai CY, Sung J, Cheng F, et al. Systematic review with meta-analysis: review of donor features, procedures and outcomes in 168 clinical studies of faecal microbiota transplantation. Aliment Pharmacol Ther. 2019;49(4):354–363. [DOI] [PubMed] [Google Scholar]
- 42.Woodworth MH, Hayden MK, Young VB, et al. The role of fecal microbiota transplantation in reducing intestinal colonization with antibiotic-resistant organisms: the current landscape and future directions. Open Forum Infect Dis. 2019;6:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Amrane S, Lagier JC.. Fecal microbiota transplantation for antibiotic resistant bacteria decolonization. Hum Microbiome J. 2020;16:100071. [Google Scholar]
- 44.Moola S, Munn Z, Tufanaru C, et al. Systematic reviews of etiology and risk. In: Aromataris E, Munn Z, editors. Joanna Briggs institute reviewer’s manual. Adelaide (Australia): The Joanna Briggs Institute; 2017. [Google Scholar]
- 45.Aromataris E, Munn Z.. Joanna Briggs institute reviewer’s manual. Adelaide (Australia): The Joanna Briggs Institute; 2017. [Google Scholar]
- 46.Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. Forsch Komplementarmed. 2013;20:385–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Agha RA, Fowler AJ, Rajmohan S, et al. Preferred reporting of case series in surgery; the PROCESS guidelines. Int J Surg. 2016;36:319–323. [DOI] [PubMed] [Google Scholar]
- 48.Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–406. [DOI] [PubMed] [Google Scholar]
- 49.Leo S, Lazarevic V, Girard M, et al. Metagenomic characterization of gut microbiota of carriers of extended-spectrum beta-lactamase or carbapenemase-producing Enterobacteriaceae following treatment with oral antibiotics and fecal microbiota transplantation: results from a multicenter randomized trial. Microorganisms. 2020;8(6):941–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Huttner BD, de Lastours V, Wassenberg M, et al. A 5-day course of oral antibiotics followed by faecal transplantation to eradicate carriage of multidrug-resistant Enterobacteriaceae: a randomized clinical trial. Clin Microbiol Infect. 2019;25:830–838. [DOI] [PubMed] [Google Scholar]
- 51.Murad MH, Sultan S, Haffar S, et al. Methodological quality and synthesis of case series and case reports. Evid Based Med. 2018;23:60–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.El Dib R, Nascimento Junior P, Kapoor AA.. alternative approach to deal with the absence of clinical trials. A proportional meta-analysis of case series studies. Acta Cir Bras. 2013;28:870–876. [DOI] [PubMed] [Google Scholar]
- 53.Tavoukjian V. Faecal microbiota transplantation for the decolonization of antibiotic-resistant bacteria in the gut: a systematic review and meta-analysis. J Hosp Infect. 2019;102:174–188. [DOI] [PubMed] [Google Scholar]
- 54.Deeks JJ, Higgins JP, Altman DG.. Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, et al., editors. Cochrane handbook for systematic reviews of interventions. Oxford (UK): The Cochrane Collaboration; 2008. p. 243–296. [Google Scholar]
- 55.Bar-Yoseph H, Carasso S, Shklar S, et al. Oral capsulized fecal microbiota transplantation for eradication of carbapenemase-producing Enterobacteriaceae colonization with a metagenomic perspective. Clin Infect Dis. 2020;737:1–10. [DOI] [PubMed] [Google Scholar]
- 56.Saïdani N, Lagier JC, Cassir N, et al. Faecal microbiota transplantation shortens the colonization period and allows re-entry of patients carrying carbapenamase-producing bacteria into medical care facilities. Int J Antimicrob Agents. 2019;53:355–361. [DOI] [PubMed] [Google Scholar]
- 57.Davido B, Batista R, Fessi H, et al. Fecal microbiota transplantation to eradicate vancomycin-resistant enterococci colonization in case of an outbreak. Med Mal Infect. 2019;49:214–218. [DOI] [PubMed] [Google Scholar]
- 58.Grosen AK, Povlsen JV, Lemming LE, et al. Faecal microbiota transplantation eradicated extended-spectrum beta-lactamase-producing klebsiella pneumoniae from a renal transplant recipient with recurrent urinary tract infections. Case Reports Nephrol Dial. 2019;9:102–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bahl MI, Jørgensen SMD, Skriver AH, et al. Faecal microbiota transplantation for eradication of co-infection with Clostridioides difficile and extensively drug-resistant KPC-producing Klebsiella pneumoniae. Scand J Gastroenterol. 2020;55:626–630. [DOI] [PubMed] [Google Scholar]
- 60.Biernat MM, Urbaniak-Kujda D, Dybko J, et al. Fecal microbiota transplantation in the treatment of intestinal steroid-resistant graft-versus-host disease: two case reports and a review of the literature. J Int Med Res. 2020;48(6):030006052092569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Biliński J, Grzesiowski P, Muszyński J, et al. Fecal microbiota transplantation inhibits multidrug-resistant gut pathogens: preliminary report performed in an immunocompromised host. Arch Immunol Ther Exp. 2016;64:255–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stalenhoef JE, Terveer EM, Knetsch CW, et al. Fecal microbiota transfer for multidrug-resistant gram-negatives: a clinical success combined with microbiological failure. Open Forum Infect Dis. 2017;4:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Torres SM, Hammond S, Elshaboury RH, et al. Recurrent relatively resistant Salmonella infantis infection in 2 immunocompromised hosts cleared with prolonged antibiotics and fecal microbiota transplantation. Open Forum Infect Dis. 2019;6:2–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ueckermann V, Hoosien E, De Villiers N, et al. Fecal microbial transplantation for the treatment of persistent multidrug-resistant Klebsiella pneumoniae infection in a critically ill patient. Case Rep Infect Dis Clostridium difficile 2020;2020:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mrazek K, Bereswill S, Heimesaat MM.. Fecal microbiota transplantation decreases intestinal loads of multi-drug resistant Pseudomonas aeruginosa in murine carriers. Eur J Microbiol Immunol. 2019;9:14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Caballero S, Carter R, Ke X, et al. Distinct but spatially overlapping intestinal niches for vancomycin-resistant Enterococcus faecium and carbapenem-resistant Klebsiella pneumoniae. PLoS Pathog. 2015;11(9):e1005132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Stephen M, Cummings JH.. The microbial contribution to human faecal mass. J Med Microbiol Clostridium difficile 1980;13:45–56. DOI: [DOI] [PubMed] [Google Scholar]
- 68.Cammarota G, Ianiro G, Gasbarrini A.. Faecal microbiota transplantation in clinical practice. Gut. 2018;67:196–197. [DOI] [PubMed] [Google Scholar]
- 69.Wong SH, Yu J.. Proton-pump inhibitor use before fecal microbiota transplant: a wonder drug, a necessary evil, or a needless prescription? J Gastroenterol Hepatol. 2020;35:913–914. [DOI] [PubMed] [Google Scholar]
- 70.McDonald EG, Milligan J, Frenette C, et al. Continuous proton pump inhibitor therapy and the associated risk of recurrent Clostridium difficile infection. JAMA Intern Med. 2015;175:784–791. [DOI] [PubMed] [Google Scholar]
- 71.Vilcu AM, Sabatte L, Blanchon T, et al. Association between acute gastroenteritis and continuous use of proton pump inhibitors during winter periods of highest circulation of enteric viruses. JAMA Netw Open. 2019;2:e1916205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Freedberg DE, Toussaint NC, Chen SP, et al. Proton Pump inhibitors alter specific taxa in the human gastrointestinal microbiome: a crossover trial. Gastroenterology. 2015;149:883–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jackson MA, Goodrich JK, Maxan ME, et al. Proton pump inhibitors alter the composition of the gut microbiota. Gut. 2016;65:749–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hong AS, Yu WY, Hong JM, et al. Proton pump inhibitor in upper gastrointestinal fecal microbiota transplant: a systematic review and analysis. J Gastroenterol Hepatol. 2020;35:932–940. [DOI] [PubMed] [Google Scholar]
- 75.Kamada N, Kim Y-G, Sham HP, et al. Regulated virulence controls the ability of a pathogen to compete with the gut microbiota. Science. 2012;336(6086):1325–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lee SM, Donaldson GP, Mikulski Z, et al. Bacterial colonization factors control specificity and stability of the gut microbiota. Nature. 2013;501:426–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lam LH, Monack DM.. Intraspecies competition for niches in the distal gut dictate transmission during persistent Salmonella infection. PLoS Pathog. 2014;10(12):e1004527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Meador JP, Caldwell ME, Cohen PS, et al. Escherichia coli pathotypes occupy distinct niches in the mouse intestine. Infect Immun. 2014;82:1931–1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Brandl K, Plitas G, Mihu CN, et al. Vancomycin-resistant enterococci exploit antibiotic-induced innate immune deficits. Nature. 2008;455:804–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Farache J, Koren I, Milo I, et al. Luminal bacteria recruit CD103+ dendritic cells into the intestinal epithelium to sample bacterial antigens for presentation. Immunity. 2013;38:581–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Diehl GE, Longman RS, Zhang J, et al. Microbiota restrict trafficking of bacteria to mesenteric lymph nodes by CX3CR1hi cells. Nature. 2013;494:116–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Corr SC, Li Y, Riedel CU, et al. Bacteriocin production as a mechanism for the antiinfective activity of Lactobacillus salivarius UCC118. Proc Natl Acad Sci USA Clostridium difficile 2007;104:7617–7621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wong JMW, De Souza R, Kendall CWC, et al. Colonic health: fermentation and short chain fatty acids. J Clin Gastroenterol. 2006;40:235–243. [DOI] [PubMed] [Google Scholar]
- 84.Fachi JL, Felipe JdS, Pral LP, et al. Butyrate protects mice from Clostridium difficile-induced colitis through an HIF-1-dependent mechanism. Cell Rep. 2019;27:750–761. [DOI] [PubMed] [Google Scholar]
- 85.Ubeda C, Bucci V, Caballero S, et al. Intestinal microbiota containing Barnesiella species cures vancomycin-resistant Enterococcus faecium colonization. Infect Immun. 2013;81:965–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.De Oliveira CP, Da Silva JA, De Siqueira JP.. Nature of the antimicrobial activity of Lactobacillus casei Bifidobacterium bifidum and Bifidobacterium animalis against foodborne pathogenic and spoilage microorganisms. Nat Prod Res. 2015;29:2133–2136. [DOI] [PubMed] [Google Scholar]
- 87.Valyshev AV, Elagina NN, Kirillov VA, et al. Effect of Bifidobacteria on the anti-lysozyme activity of enterobacteria. Zh Mikrobiol Epidemiol Immunobiol. 2000;4:77–79. [PubMed] [Google Scholar]
- 88.Smith AR, Macfarlane GT, Reynolds N, et al. Effect of a synbiotic on microbial community structure in a continuous culture model of the gastric microbiota in enteral nutrition patients. FEMS Microbiol Ecol. 2012;80:135–145. [DOI] [PubMed] [Google Scholar]
- 89.Bondue P, Crèvecoeur S, Brose F, et al. Cell-free spent media obtained from Bifidobacterium bifidum and Bifidobacterium crudilactis grown in media supplemented with 3’-sialyllactose modulate virulence gene expression in Escherichia coli O157: H7 and Salmonella typhimurium. Front Microbiol. 2016;7:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ramos-Ramos JC, Lázaro-Perona F, Arribas JR, et al. Proof-of-concept trial of the combination of lactitol with Bifidobacterium bifidum and Lactobacillus acidophilus for the eradication of intestinal OXA-48-producing Enterobacteriaceae. Gut Pathog. 2020;12(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]