Abstract
Nonfatal firearm assault incidents are more prevalent than gun homicides, however, little is understood about nonfatal firearm assault incidents due to a lack of accurate data in the United States. This is a descriptive study of all nonfatal firearm assault incidents identified through police and clinical records from 2007–2016 in Indianapolis, Indiana. Records were linked at the incident level to demonstrate the overlap and non-overlap of nonfatal firearm assault incidents in police and clinical records and describe differences in demographic characteristics of the victims. Incidents were matched within a 24-hour time window of the recorded date of the police incident. Data were analyzed in fall 2020. There were 3,797 nonfatal firearm assault incidents identified in police reports and 3,131 clinical encounters with an ICD 9/10 diagnosis-based nonfatal firearm-related injury. 62% (n=2,366) of nonfatal firearm assault incidents matched within 24 hours to a clinical encounter, 81% (n=1,905) had a firearm related ICD code: 40% (n=947) were coded as a firearm-related assault, 32% (n=754) were coded as a firearm-related accident; and 8.6% (n=198) were coded as undetermined, self-inflicted or law enforcement firearm-related. The other 20% (n=461) did not have an ICD firearm related diagnosis code. Results indicate most nonfatal firearm assault incidents overlap between police and clinical records systems, however, discrepancies between the systems exist. These findings also demonstrate an undercounting of nonfatal firearm assault incidents when relying on clinical data systems alone and more efforts are needed to link administrative police and clinical data in the study of nonfatal firearm assaults.
Firearm violence is a public health crisis in the United States. Nonfatal firearm assaults are estimated to be four times as prevalent as firearm homicides.1 Apart from a few key studies,1–5 little is known about nonfatal firearm assaults due to a dearth in research,6 a lack of accurate, timely, and available data in the United States.7,8 To address these issues, this study links police reports and incident-related clinical reports to examine nonfatal firearm assault incidents, as understanding the epidemiology of nonfatal firearm assault is critical to effectively identify and design prevention efforts.
The largest obstacle to advancing knowledge on nonfatal firearm assault is the lack of integrated data systems.7,8 In consequence, research on nonfatal firearm assaults has largely been conducted using data from single sources derived from clinical, public health, or police systems. National databases on firearm assaults collect data only on firearm related deaths, incompletely identify assault victims with gunshot wounds, or, in the case of CDC injury data, represent only a sample of emergency departments, and clinical and justice data are not integrated.1 Criminal justice databases such as the Federal Bureau of Investigation’s Uniform Crime Reports (UCR) use categories of Armed Robbery and Aggravated Assault-Gun to indicate a firearm was used but not that the victim suffered a gunshot wound. In the medical literature, researchers commonly use electronic health records (EHR) or trauma registry data to examine nonfatal firearm injuries. EHR data are known to underestimate injury prevalence due to limitations in coding;9 trauma registries miss nonfatal assault victims if injuries are too minor to require a trauma activation, or if the patient was cared for at a non-trauma center. From a public health perspective, these more minor events are still significant to consider, as less severe injury may still result in long-term physical, mental, and societal effects.10–12
Among firearm violence researchers, there has been a recent call to improve the infrastructure of firearms data at the local and national levels, specifically to determine the true prevalence of nonfatal firearm assault incidents. One potential avenue for creating more valid data on nonfatal assault incidents is by linking police and clinical administrative data.13 For instance, researchers in Philadelphia recently compared trends in firearm assault events over a 10-year period using both police records and trauma registry data.14 They found trauma registry data identified only half the number of firearm assaults identified in police records. Differences were also observed in victim demographics and injury trends across both data sets. These findings suggest combining police and clinical data may provide a more accurate picture of firearm assaults, event details, and injury severity. However, the Philadelphia study only examined aggregate numbers across both systems, limiting what we know about the true incident overlap of these two populations. Therefore, this study leverages linked administrative police reports and incident related clinical reports to examine the overlap and non-overlap of nonfatal firearm assault incidents and to describe differences in the demographic characteristics of the victims.
Methods
Study Setting and Sample
We conducted a descriptive study of all nonfatal firearm assault incidents identified through police records and one or more inpatient, outpatient or emergency department clinical encounters from 2007 through 2016 in Indianapolis, Indiana. We obtained these data in collaboration with the Indianapolis Metropolitan Police Department (IMPD) and the Regenstrief Institute’s Indiana Network for Patient Care (INPC). The IMPD records management system was used to pull incident reports and their corresponding UCR categories. IMPD is the largest police department in Marion County (Indianapolis metropolitan area), Indiana, covering over 90% of the county geographically. IMPD collects incident reports on all victimizations and crimes occur within their jurisdiction. Each police record includes incident case number, date of incident, location of incident, incident title (e.g., aggravated assault-gun or armed-robbery), person type (e.g., victim, suspect/offender, deceased, witness, involved, other), name, date of birth, age, race, sex, and narrative of the incident.
The INPC was developed over 30 years ago and has over 17 million patient-level medical records to inform both clinical care and research purposes.15 The INPC covers 90 hospitals within Indiana and seven of the emergency departments within Indianapolis and all within IMPD’s jurisdiction. Clinical records include patient demographics, encounter dates, and associated diagnoses codes at time of encounter. This project was approved by the Indiana University Institutional Review Board and data were analyzed in fall 2020.
Record Linkage Procedures
Deterministic and probabilistic matching linked individuals from IMPD’s records management system to individuals with one or more INPC clinical records, by using identifiers including first name, middle name, last name, sex, race, date of birth, social security number, ZIP code, and street address number. Individuals were matched using the following procedures. First, deterministic algorithms were applied using different combinations of identifiers to establish exact and conservative matches. Next, several probabilistic algorithms were employed based on prior linkage studies.16–20 A probabilistic algorithm defines the probability a specific pair is a true match.16–19 Three strategies were used to refine the probabilistic linkage process: (1) phonetic transformations were created using “Soundex” and New York Statewide Immunization Information System (NYSIIS) methods to help match misspelled names: (2) names with possible nicknames and known aliases were matched: (3) possibly switched last, first, and middle names, as well as mismatched day and month of birth, and (4) iteratively refined the algorithms to a desired level of performance, by using alternative strategies such as weighing by name frequency. Three research team members independently reviewed each of the probabilistic matching algorithms and determined a match threshold score for each algorithm. The most conservative of match scores was chosen to select true matches (pairs with scores greater than or equal to that threshold).
Cohort Definition
The outcome of interest is nonfatal firearm assault incidents. Nonfatal firearm assault incidents were defined by two criteria: (1) the incident had to meet the criteria of an aggravated assault according to Federal Bureau of Investigation Uniform Crime Reporting (UCR) standards, and (2) an individual had to have a penetrating injury caused directly by a firearm.21,22 Self-inflicted, unintentional, accidental, and police involved shootings were excluded. Only victims identified in the police report were included in this study. We gathered all IMPD UCR events for armed robbery and aggravated assault-gun within Indianapolis between 2007 and 2016. To ensure the incident involved a penetrating gunshot wound victim, all UCR narratives were queried, coded with multiple sets of key words: (1) “person shot,” “gunshot wound,” “gsw,” “people shot,” “shots fired,”; (2) “firearm,” “gun,” “bullet,” “armed”; and/or (3) “hospital,” “transported,” and then reviewed,1 and verified by querying clinical records for an ICD gun-assault code to confirm a gunshot injury. Given mandatory reporting laws that require hospitals to report all gunshot wounds to law enforcement;23 our population of nonfatal firearm assaults should be inclusive for all nonfatal firearm assault incidents treated at a hospital or reported to police within IMPD jurisdiction.
Police Incident and Clinical Encounter Date Match
We matched incidents by date to identify the same police incident with the corresponding clinical encounter between 2007–2016. We considered an incident a match on two criteria: 1) victim unique identifier, as previously described above and 2) police date and clinical encounter data were within 24 hours of each other (e.g., exact date match). Given the possible delays in police incident reporting, or hospital reporting a gunshot wound to the police, we also searched a 48-hour window outside the initial 24 hours (e.g., exact date +/- 1) (Figure 1)..
Fig. 1.
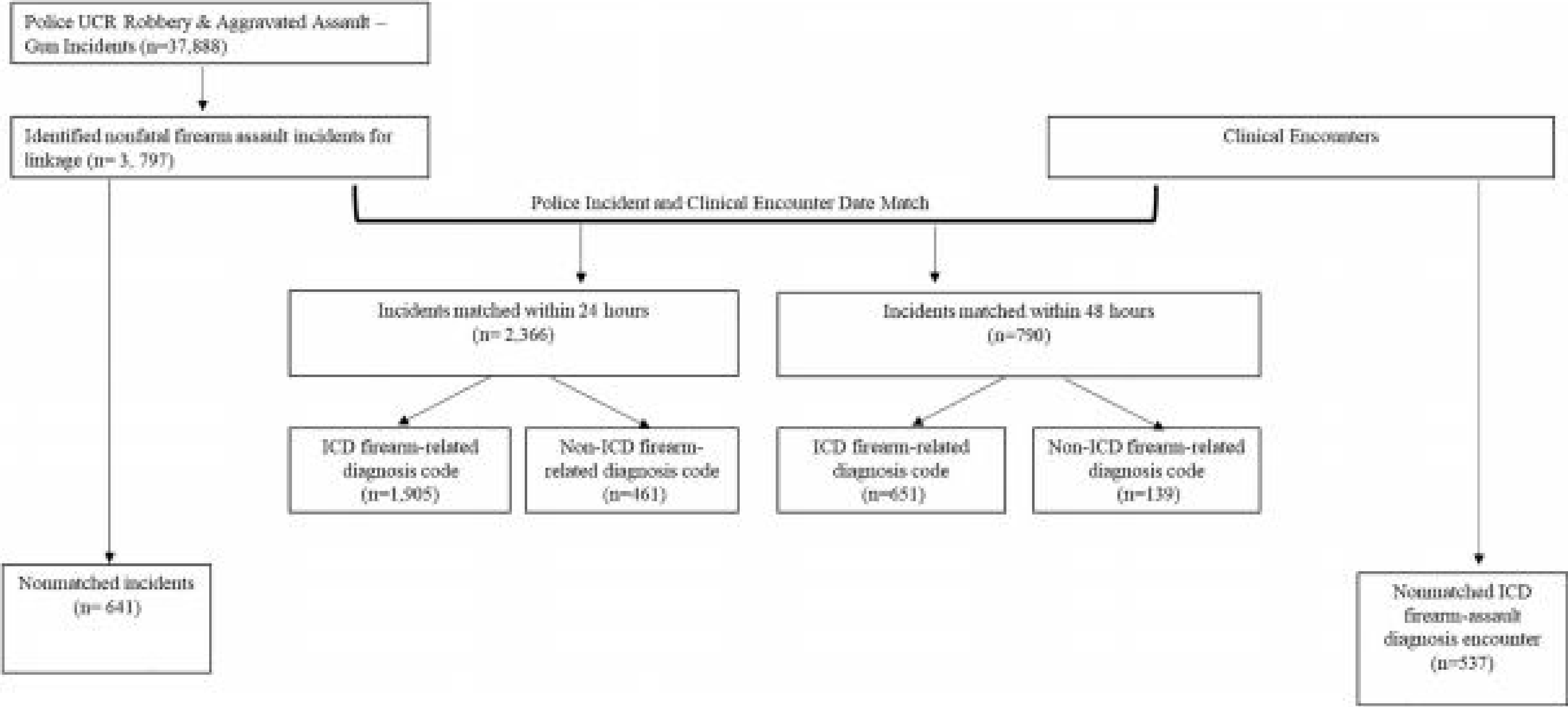
Study flow diagram.
ICD Diagnoses Code Classification
Given all incidents matched within the 24 and 48-hours are considered assaults per the police data, we sought to classify incidents by ICD diagnoses codes to determine misclassification within the clinical data. Using ICD-9 and ICD-10 diagnosis codes, we identified records coded as firearm assault (E965, X93, X94, X95.8–9), firearm accidental/unintentional (E922, W32, W33, W34.00, W34.09, W34.10, W34.19), firearm undetermined (E985, E979.4, E991, Y22, Y23, Y24.8–9, Y36.41, Y36.42, Y36.43), firearm self-inflicted (E955, X72, X73, X74.8–9), or firearm-law enforcement (E970, Y35.0). A text search for keywords, “gunshot,” “firearm,” “gsw,” “open wound,” “injury,” “trauma,” “open fracture,” “assault,” “shot,” and “gun shot”24 in the diagnoses text field was performed and manually reviewed to classify incidents not coded or classified as a firearm related incident in the clinical data. Records without any indication of firearm-related injury were coded as non-firearm encounters. For incidents with more than one ICD firearm-related codes, we prioritized codes to create mutually exclusive categories as follows: 1) firearm-related assault, 2) firearm-related unintentional/accidental, 3) other firearm-related, or 4) non-firearm related ICD code, to examine the frequency of firearm related ICD code by specific category, as well as non-firearm coded encounters.
Sensitivity Analysis
To resolve incidents in the IMPD data not matching to a clinical encounter within 24 or 48 hours (n=641) of the IMPD event, all INPC encounters were searched within 20 days before and after the IMPD date to locate any delayed reports; 131 additional incidents were located within +/- 20 days of the police event date. These encounters were classified into three categories: (1) labeled with an ICD related gun code, (2) labeled as “open wound,” “trauma,” or “injury,” and (3) labeled with other non-trauma related ICD codes (e.g., asthma, pregnancy test). Police narratives were reviewed to determine if medical attention was refused. Finally, all ED encounters from the date of the police incident were searched for ICD-firearm codes as well as any injury or trauma, given some victims may not present with identifying information; we then matched on race, sex, age, date, and time. INPC encounters were coded with an ICD firearm assault diagnosis code that did not match to police records and may indicate incidents outside IMPD’s jurisdiction, patients who transferred from out of county, or incidents missing from police data.
Results
From 2007 to 2016, 3,797 (comprised by 3,608 unique victims, 120 persons with more than one incident, and 249 incidents with multiple victims) nonfatal firearm assault incidents were identified in police reports (Table 1). Within the clinical records, there were 3,131 ICD firearm-related clinical encounters. Annual rates of nonfatal firearm assault incidents were consistently lower when based on clinical data with an ICD firearm-related code (ranging from 26.7 – 51.3 per 100,000 from 2007–2016) and even lower when based on an ICD firearm-assault code (ranging from 12.5 – 32.6 per 100,000), compared to police-reports (33.3 to 55.8 per 100,000 population)(Figure 2).
Table 1 –
Multiple Victim Incidents and Repeat Victim Incidents involved in Nonfatal
| Number of incidents with multiple victims | ||
| # of victims per incident | # of incidents | Total # of incidents (N=3,797) |
| 1 | 3,218 | 3,218 |
| 2 | 206 | 412 |
| 3 | 24 | 72 |
| 4 | 7 | 28 |
| 5 | 8 | 40 |
| 6 | 1 | 6 |
| 7 | 3 | 21 |
| Number of repeat victims per incidents | ||
| # of victims | # of incidents | Total # of incidents (N=3,797) |
| 3,548 | 1 | 3,548 |
| 111 | 2 | 222 |
| 9 | 3 | 27 |
Firearm Assault Incidents, Indianapolis, Indiana, 2007 – 2016
Fig. 2.

Police and clinical nonfatal firearm assault incident rates per 100,000 population, Indianapolis, Indiana, 2007–2016.
Of the 3,797 nonfatal assault incidents identified in the police reports, 62% (n=2,366) were matched to a corresponding clinical encounter within 24 hours (i.e., exact date match). An additional 21% (n=790) of nonfatal firearm assault incidents were matched within 48 hours (i.e., exact date +/- 1) of the initial police reported date. There were 641 nonfatal firearm assault incidents identified in the police data that did not match within the 24 or 48 hours of a corresponding clinical encounter and an additional 537 nonfatal firearm assault incidents were identified within the clinical records but did not match to a corresponding police incident (Figure 3).
Fig. 3.

Overlap and non-overlap of nonfatal firearm assault incidents in police and clinical data*, Indianapolis, Indiana, 2007–2016. *overLap displays overLap of both 24 h (n=2,366)and the next 43 h (n=790).
Of the 641 nonfatal firearm assault incidents that did not match between police and clinical data within 24 or 48 hours, 57 refused medical attention and/or emergency medical services transport and 131 clinical encounters were identified within 40 days of the police event date. Of the 131 with a clinical encounter within 40 days, 33 had an ICD firearm-related code at that time, 37 had a trauma or injury related code, and 61 had ICD codes that could not necessarily be attributed to a firearm (e.g., asthma or pregnancy test), however, these clinical encounters are not considered the same incident identified within the police records given the large time window.
Police records (76.1% vs. 17.8%) and matched police-clinical records had higher proportions of Black victims (77.2% vs. 19.3%) compared to White victims. Firearm assault incidents only identified in clinical data had higher proportions of White victims (41.3% vs. 19.8%) compared to Black victims. Sex and age of victims were similar across match groups. Most non-matched cases involved Black, male victims, between 20–24 years of age (Table 2). Of the 2,366 nonfatal firearm assault incidents matched within 24 hours to a clinical encounter, 81% (n=1,905) had a firearm-related ICD code: 40% (n=947) had a firearm-related assault code; 32% (n=754) were coded as firearm-related accidental code; and 8.6% (n=198) were coded as undetermined, self-inflicted or law enforcement firearm-related. The other 20% (n=461) were coded with ICD diagnosis codes for open wounds, trauma, assault, or injuries; however, they did not indicate that a firearm was used or the intent of injury. E-codes were only included in 1.6% (n=61) of encounters (Appendix Table A). Across ICD firearm-related diagnoses codes, observed victim demographics were similar (Appendix Table B).
Table 2 –
Characteristics of police and clinical nonfatal firearm assaults by match group, Indianapolis, IN, 2007 – 2016
| Overall police records | Clinical Firearm-related code records | Police-Clinical records matched within 24 hours | Police-Clinical records matched within 48 hours | Police-Clinical records matched w/ in +/− 20 days | Police record not matched to clinical records | Refused medical care at scene | Clinical record Only | |
|---|---|---|---|---|---|---|---|---|
| N=3,797 | N=3,131 | n=2,366 | n=790 | n = 131 | n = 453 | n=57 | n=537 | |
| Race | ||||||||
| Black | 2,890 (76.1) | 2,141 (68.4) | 1,826 (77.2) | 636 (80.5) | 111 (84.7) | 308 (67.9) | 9 (15.7) | 103 (19.8) |
| White | 676 (17.8) | 695 (22.2) | 456 (19.3) | 126 (15.9) | 17 (13.0) | 73 (16.1) | 4 (7.02) | 222 (41.3) |
| Other | 155 (4.1) | 108 (3.45) | 79 (3.34) | 28 (3.54) | 3 (2.29) | 45 (10.0) | 0 (0.00) | 29 (5.40) |
| Unknown | 76 (2.0) | 187 (5.97) | 5 (0.21) | 0 (0.00) | 0 (0.00) | 27 (5.96) | 44 (77.2) | 183 (34.1) |
| Sex | ||||||||
| Male | 3,210 (84.5) | 2,685 (85.8) | 2,033 (86.0) | 698 (88.4) | 108 (82.4) | 360 (79.5) | 11 (19.3) | 445 (82.9) |
| Female | 516 (13.5) | 446 (14.2) | 333 (14.0) | 92 (11.7) | 23 (17.6) | 66 (14.6) | 2 (3.51) | 92 (17.1) |
| Unknown | 71 (1.87) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 27 (5.96) | 44 (77.2) | 0 (0.00) |
| Age Groups | ||||||||
| <15 | 51 (1.34) | 60 (1.92) | 26 (1.10) | 11 (1.39) | 1 (0.76) | 13 (2.90) | 0 (0.00) | 28 (5.21) |
| 15–19 | 318 (8.40) | 334 (10.7) | 213 (9.00) | 62 (7.85) | 8 (6.11) | 34 (7.51) | 1 (1.75) | 86 (16.0) |
| 20–24 | 855 (22.5) | 692 (22.1) | 537 (22.7) | 180 (22.8) | 39 (29.7) | 96 (21.2) | 3 (5.26) | 85 (15.8) |
| 25–29 | 692 (18.2) | 557 (17.8) | 451 (19.1) | 147 (18.6) | 23 (17.6) | 70 (15.5) | 1 (1.75) | 80 (14.9) |
| 30–34 | 540 (14.2) | 419 (13.4) | 346 (14.6) | 113 (14.3) | 16 (12.2) | 62 (13.7) | 3 (5.36) | 43 (8.01) |
| 35–39 | 365 (9.61) | 301 (9.61) | 235 (9.93) | 83 (10.5) | 11 (8.40) | 36 (7.96) | 0 (0.00) | 42 (7.82) |
| 40–44 | 250 (6.58) | 213 (6.80) | 168 (7.10) | 51 (6.46) | 9 (6.87) | 20 (4.42) | 2 (3.51) | 42 (7.82) |
| 45–54 | 367 (9.67) | 291 (9.29) | 230 (9.72) | 83 (10.5) | 14 (10.7) | 38 (8.39) | 2 (3.51) | 48 (8.94) |
| 55+ | 259 (6.82) | 251 (8.02) | 160 (6.76) | 60 (7.59) | 10 (7.63) | 28 (6.18) | 1 (1.75) | 74 (13.8) |
| Unknown | 100 (2.63) | 13 (0.42) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 56 (12.4) | 44 (77.2) | 9 (1.68) |
Discussion
Using linked administrative police report and incident related clinical reports, our analysis demonstrated most nonfatal firearm assault incidents overlapped between the police and clinical data, however, there was a proportion of non-overlapped cases within each dataset. Clinical data identify less than half of nonfatal firearm assault incidents, as indicated by those not appropriately coded as such but with overlapping records with the police report data. Most incidents did indicate a firearm code, however, there was a notable number of incidents that did not receive any firearm-related ICD code. These incidents would be left out of any analysis collected through electronic health records and other injury surveillance systems derived from hospital data had these records not been confirmed as nonfatal firearm assaults through police data. This finding confirms the underreporting of nonfatal firearm assaults within clinical data systems.13
Our findings aligned with prior research14,25 and indicate police data may provide a more complete record of nonfatal firearm assault incidents compared to clinical data, and linking police and clinical data is important to improve our understanding of nonfatal firearm assault incidents due to the underreporting of firearm assaults in clinical records. Prior research has linked clinical and police data at the individual level to examine firearm violence; however, police data has largely been used to only study firearm related offending and clinical data have defined victimization.2,3,26 Criminologists have long utilized police records to study homicides and more recently nonfatal assaults.1,21,27,28 Police records include the incident location, which is often missing from clinical records,29 the relationship between the victim and the suspect, the incident’s motive,1,21,30 as well as incidents with minor injuries that do not require medical attention, as were found in this study. Police data allow for a more contextual understanding of the nonfatal shooting assault incidents.31 For instance, nonfatal firearm assault incidents spatially cluster on a small number of streets,28,32 and drug involved assaults have the highest risk of fatality.1 Understanding the spatial patterns and other incident details may be important for designing prevention efforts.
Police data, however, have also been found to underrepresent nonfatal firearm assaults when compared to clinical data.33,34 The results from this study partially support this finding, in that a number of firearm assault incidents were found in the clinical data that could not be matched to police records. Criminologists often refer to the underreporting of crime to police as the “dark figure of crime”35 and attribute, largely, the lack of willingness to report a crime to the police to mistrust in the police.36 Given the majority of states have mandatory reporting laws,23 that require medical professionals to contact police when a person presents for care with a gunshot wound, police data should document each nonfatal firearm assault incidents; however, the unmatched nonfatal assault incidents identified in our study through clinical data does not fully support this notion, and is consistent with others’ work that have linked police and clinical data.25 There are a number of plausible explanations for these unmatched records. A police report is generated but may not reflect the correct victim information or the correct date of the incident, as many victims are uncooperative with police.21 As for clinical records, in high volume emergency departments minor gunshot wound injuries may go unreported to police, simply get overlooked during busy shifts, or the physician’s focus is on treatment and not incident circumstances.37 Prior research has also noted a victim’s unwillingness to give accurate contact information to healthcare workers,38,39 due to mistrust of healthcare providers from a history of racism within the healthcare system,38,40 as well as perceived blurred lines between medical professionals and police.38,39 Victims of violence often view the police as helpful when providing safety and information immediately following a violent injury; however, questioning by police can feel stressful, and disrespectful, and can impede medical care at the time of injury.39,41 Our study cannot account for these factors, but they may temper our findings.
Overall, our results indicate most nonfatal firearm assault incidents overlap between both the police and clinical systems within 24 hours. There were notable differences across both systems, which indicates that no single data set completely captures nonfatal firearm assaults.14,25 Partnerships between police and clinical systems have improved surveillance of non-firearm injury data, such as road traffic injuries.42 Police-public health partnerships can improve data collection,34,43,44 can better direct policies and initiatives, and can improve response efforts through combined teams, such as crisis intervention teams for individuals suffering from mental illness.43 There have been a number of initiatives focused on violence over the years,42 but the Cardiff Violence Prevention Program is the only partnership which has evaluated the cost-benefit ratios and the success in reducing violent injuries.42,45 Although only aggregated data from both police and ED data systems have been used thus far, the Cardiff model demonstrates ED nurses can be a valid source for additional screening in identifying firearm assault injuries.42,45,46
Additionally, these findings support prior work which suggests additional efforts to link administrative data across disciplines are needed13,26,34 at both the local and federal level to better inform prevention efforts. This study was feasible only due to the longstanding research partnership with the local police department47 and the robust clinical data available at the individual level through the Regenstrief Institute’s INPC data. Such efforts at the local level can inform local prevention initiatives, however, accurate and integrated data on nonfatal shooting assault incidents should be collected and available at the federal level. For instance, as of 2021 the FBI is no longer collecting UCR data from police agencies and is transitioning to the National Incident-Based Reporting Systems (NIBRS). This transition period may be an opportunity to improve police reporting of nonfatal firearm assault incidents by including a category that indicates a gunshot wound injury at the federal level. This more complete capture of nonfatal firearm assaults at the national level would allow for more opportunities to link to other national level health data and more accurately examine correlates of nonfatal firearm assaults.
Limitations
Our results should be considered with several limitations in mind. With mandatory reporting laws, all nonfatal firearm assault incidents should be included in police records, but victims who have minor wounds may not seek medical treatment or may not contact the police and therefore would be missing from our study. We examined data from only one metropolitan area, so our findings may not be generalizable. We did not examine the incident location, but this is a clear direction for future research, as incident location can influence transportation type, linkage to trauma care, and contribute to mortality rates. Although we have population data on clinical encounters within INPC, some records may still be missing or unmatched because of inaccurate or incomplete data, and the data do not capture encounters outside the INPC system. For instance, among the 453 non-matched incidents; we identified 94 ED encounters with an ICD firearm-related code and matching race, sex, and age of police defined victim and an additional 385 ED encounters within 24 hours of the police incident with a trauma/injury related ICD code. These potential incidents, however, could not be matched based on our criteria. We were not able to account for injury severity which may influence hospital staff ICD coding, incident motive, injury location or length of hospital stay but these are clear directions for future research. Future research could involve techniques such as natural language processing (NLP) in both the police and clinical data to better classify records automatically.48,49 NLP has proven successful with electronic health records in other health outcome studies,50,51 more recently in identifying nonfatal firearm incident locations from medical records,29 and could help establish a gold standard in nonfatal firearm assault incident reporting across systems. Integration of additional data sources such as trauma registries, emergency management services, and death records may further improve surveillance of nonfatal firearm assault incidents.25,26,31
Our study demonstrates overlap and non-overlap between police and clinical data systems does exist and illustrates the benefit of linking administrative police and clinical data in the study of nonfatal firearm assault incidents, however, more research is needed to further implement standardization and linkage at both the local and federal level. Partnerships between healthcare systems and police are needed, both of which have the potential to enhance such data collection, data quality,13 and better inform community responses to sources of firearm morbidity.
Supplementary Material
Highlights.
Overlap and non-overlap exists between police and clinical data regarding nonfatal firearm assault incidents
Most nonfatal firearm assaults overlap within 48 hours of shooting incident
Clinical data alone identifies less than half of nonfatal firearm assault incidents
ACKNOWLEDGEMENTS
Thank you to the Indianapolis Metropolitan Police Department for their assistant in data acquisition. This study was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number F32HD101211 (PI: Lauren A. Magee), National Institute of Health (R01AI114435-01, PI: Sarah E. Wiehe) and Agency for Healthcare Research and Quality (R01HS023318-01,PI: Sarah E. Wiehe). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Health, Agency for Healthcare Research and Quality or the Indianapolis Metropolitan Police Department.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICTS OF INTEREST
The authors report that they have no conflicts of interest.
HUMAN PARTICIPANT PROTECTION
This study was approved by Indiana University institutional review board.
Key findings: Our study demonstrates overlap and non-overlap between police and clinical data systems do exist and illustrate the benefit of linking administrative police and clinical data in the study of nonfatal firearm assault incidents.
References
- 1.Hipple NK, Magee L. The difference between living and dying: victim characteristics and motive among nonfatal shootings and gun homicides. Violence Vict. 2017;32(6):977–997. [DOI] [PubMed] [Google Scholar]
- 2.Mills BM, Nurius PS, Matsueda RL, Rivara FP, Rowhani-Rahbar A. Prior arrest, substance use, mental disorder, and intent-specific firearm injury. Am J Prev Med. 2018;55(3):298–307. [DOI] [PubMed] [Google Scholar]
- 3.Rowhani-Rahbar A, Zatzick D, Wang J, et al. Firearm-related hospitalization and risk for subsequent violent injury, death, or crime perpetration: a cohort study. Ann Intern Med. 2015;162(7):492–500. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham RM, Carter PM, Ranney M, et al. Violent reinjury and mortality among youth seeking emergency department care for assault-related injury: a 2-year prospective cohort study. JAMA Pediatr. 2015;169(1):63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ranney M, Karb R, Ehrlich P, et al. What are the long-term consequences of youth exposure to firearm injury, and how do we prevent them? A scoping review. J Behav Med. 2019;42(4):724–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kellermann AL, Rivara FP. Silencing the science on gun research. JAMA. 2013;309(6):549–550. [DOI] [PubMed] [Google Scholar]
- 7.Wellford CF, Pepper JV, Petrie CV. Firearms and violence: A critical review. Committee to Improve Research Information and Data on Firearms. In: Washington, DC: The National Academies Press; 2005. [Google Scholar]
- 8.NORC. The State of Firearms Data in 2019. University of Chicago; 2019. [Google Scholar]
- 9.Hink AB, Bonne S, Levy M, et al. Firearm injury research and epidemiology: A review of the data, their limitations, and how trauma centers can improve firearm injury research. Journal of trauma and acute care surgery. 2019;87(3):678–689. [DOI] [PubMed] [Google Scholar]
- 10.Fagan J, Wilkinson DL. Guns, youth violence, and social identity in inner cities. Crime and justice. 1998;24:105–188. [Google Scholar]
- 11.Baumer E, Horney J, Felson R, Lauritsen JL. Neighborhood disadvantage and the nature of violence. Criminology. 2003;41(1):39–72. [Google Scholar]
- 12.Lauritsen JL, White NA. Putting violence in its place: The influence of race, ethnicity, gender, and place on the risk for violence. Criminology & Public Policy. 2001;1(1):37–60. [Google Scholar]
- 13.Wardell CA R; Barber C; Cook P; Culhane D; Cunningham R; Dalton E; Jenkins R; Joyce N; Mueller-Smith M; Muhammad F; Potok N; Webster D; Wintemute G A Blueprint for a U.S. Firearms Data Infrastructure. NORC: University of Chicago;2020. [Google Scholar]
- 14.Kaufman E, Holena DN, Yang WP, et al. Firearm assault in Philadelphia, 2005–2014: a comparison of police and trauma registry data. Trauma surgery & acute care open. 2019;4(1):e000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Biondich PG, Grannis SJ. The Indiana network for patient care: an integrated clinical information system informed by over thirty years of experience. J Public Health Manag Pract. 2004;10:S81–S86. [PubMed] [Google Scholar]
- 16.Grannis SJ, Overhage JM, Hui S, McDonald CJ. Analysis of a probabilistic record linkage technique without human review. AMIA Annu Symp Proc. 2003:259–263. [PMC free article] [PubMed] [Google Scholar]
- 17.Grannis SJ, Overhage JM, McDonald C. Real world performance of approximate string comparators for use in patient matching. Stud Health Technol Inform. 2004;107(Pt 1):43–47. [PubMed] [Google Scholar]
- 18.Grannis SJ, Overhage JM, McDonald CJ. Analysis of identifier performance using a deterministic linkage algorithm. Proc AMIA Symp. 2002:305–309. [PMC free article] [PubMed] [Google Scholar]
- 19.Grannis SJ, Stevens KC, Merriwether R. Leveraging health information exchange to support public health situational awareness: the indiana experience. Online J Public Health Inform. 2010;2(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Magee LA, Fortenberry JD, Rosenman M, Aalsma MC, Gharbi S, Wiehe SE. Two-year prevalence rates of mental health and substance use disorder diagnoses among repeat arrestees. Health & Justice. 2021;9(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hipple NK, Garrity KT, Huebner BM, Magee L. Understanding Victim Cooperation in Cases of Nonfatal Gun Assaults. Criminal Justice and Behavior. 2019;46(12):1793–1811. [Google Scholar]
- 22.Beaman V, Annest JL, Mercy JA, Kresnow M-j, Pollock DA. Lethality of firearm-related injuries in the United States population. Ann Emerg Med. 2000;35(3):258–266. [DOI] [PubMed] [Google Scholar]
- 23.Gupta M. Mandatory reporting laws and the emergency physician. Ann Emerg Med. 2007;49(3):369–376. [DOI] [PubMed] [Google Scholar]
- 24.Fahimi J, Larimer E, Hamud-Ahmed W, et al. Long-term mortality of patients surviving firearm violence. Inj Prev. 2016;22(2):129–134. [DOI] [PubMed] [Google Scholar]
- 25.Post LA, Balsen Z, Spano R, Vaca FE. Bolstering gun injury surveillance accuracy using capture– recapture methods. J Behav Med. 2019;42(4):674–680. [DOI] [PubMed] [Google Scholar]
- 26.Sumner SA, Maenner MJ, Socias CM, et al. Sentinel events preceding youth firearm violence: An investigation of administrative data in Delaware. Am J Prev Med. 2016;51(5):647–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hipple NK, Huebner BM, Lentz TS, McGarrell EF, O’Brien M. The Case for Studying Criminal Nonfatal Shootings: Evidence from Four Midwest Cities. Justice Evaluation Journal. 2019:1–20. [Google Scholar]
- 28.Braga AA, Papachristos AV, Hureau DM. The Concentration and Stability of Gun Violence at Micro Places in Boston, 1980–2008. Journal of Quantitative Criminology. 2009;26(1):33–53. [Google Scholar]
- 29.Parker ST. Estimating nonfatal gunshot injury locations with natural language processing and machine learning models. JAMA network open. 2020;3(10):e2020664–e2020664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grommon E, Rydberg J. Elaborating the Correlates of Firearm Injury Severity: Combining Criminological and Public Health Concerns. Victims & Offenders. 2014;10(3):318–340. [Google Scholar]
- 31.Kaufman EJ, Wiebe DJ, Xiong RA, Morrison CN, Seamon MJ, Delgado MK. Epidemiologic trends in fatal and nonfatal firearm injuries in the US, 2009–2017. JAMA internal medicine. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Magee L, Fortenberry D, Tu W, Wiehe SE. The Role of Social and Physical Disorder in Community Variation in Unsolved Homicides. Under Review. 2020.
- 33.Kellermann AL, Rivara FP, Lee RK, et al. Injuries due to firearms in three cities. N Engl J Med. 1996;335(19):1438–1444. [DOI] [PubMed] [Google Scholar]
- 34.Wu DT, Moore JC, Bowen DA, et al. Proportion of violent injuries unreported to law enforcement. JAMA internal medicine. 2019;179(1):111–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Biderman AD, Reiss AJ Jr. On exploring the" dark figure" of crime. The Annals of the American Academy of Political and Social Science. 1967;374(1):1–15. [Google Scholar]
- 36.Kirk DS, Matsuda M. Legal cynicism, collective efficacy, and the ecology of arrest. Criminology. 2011;49(2):443–472. [Google Scholar]
- 37.Richardson JB Jr., St Vil C, Cooper C. Who Shot Ya? How Emergency Departments Can Collect Reliable Police Shooting Data. J Urban Health. 2016;93 Suppl 1:8–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liebschutz J, Schwartz S, Hoyte J, et al. A chasm between injury and care: experiences of black male victims of violence. J Trauma. 2010;69(6):1372–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jacoby SF, Richmond TS, Holena DN, Kaufman EJ. A safe haven for the injured? Urban trauma care at the intersection of healthcare, law enforcement, and race. Soc Sci Med. 2018;199:115–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee C, Ayers SL, Kronenfeld JJ. The association between perceived provider discrimination, health care utilization, and health status in racial and ethnic minorities. Ethn Dis. 2009;19(3):330. [PMC free article] [PubMed] [Google Scholar]
- 41.Patton D, Sodhi A, Affinati S, Lee J, Crandall M. Post-discharge needs of victims of gun violence in Chicago: A qualitative study. Journal of interpersonal violence. 2019;34(1):135–155. [DOI] [PubMed] [Google Scholar]
- 42.Jacoby SF, Kollar LMM, Ridgeway G, Sumner SA. Health system and law enforcement synergies for injury surveillance, control and prevention: a scoping review. Inj Prev. 2018;24(4):305–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shepherd JP, Sumner SA. Policing and public health—strategies for collaboration. JAMA. 2017;317(15):1525–1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marshall WA, Egger ME, Pike A, et al. Recidivism rates following firearm injury as determined by a collaborative hospital and law enforcement database. Journal of trauma and acute care surgery. 2020;89(2):371–376. [DOI] [PubMed] [Google Scholar]
- 45.Kollar LMM, Sumner SA, Bartholow B, et al. Building capacity for injury prevention: a process evaluation of a replication of the Cardiff Violence Prevention Programme in the Southeastern USA. Inj Prev. 2020;26(3):221–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Florence C, Shepherd J, Brennan I, Simon T. Effectiveness of anonymised information sharing and use in health service, police, and local government partnership for preventing violence related injury: experimental study and time series analysis. BMJ. 2011;342:d3313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wiehe SE, Rosenman MB, Chartash D, et al. A Solutions-Based Approach to Building Data-Sharing Partnerships. eGEMs. 2018;6(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ballesteros MF, Sumner SA, Law R, Wolkin A, Jones C. Advancing injury and violence prevention through data science. Journal of Safety Research. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Johnson JR, Miller A, Khan L, Thuraisingham B. Extracting semantic information structures from free text law enforcement data. Paper presented at: 2012 IEEE International Conference on Intelligence and Security Informatics 2012.
- 50.Mendonça EA, Haas J, Shagina L, Larson E, Friedman C. Extracting information on pneumonia in infants using natural language processing of radiology reports. J Biomed Inform. 2005;38(4):314–321. [DOI] [PubMed] [Google Scholar]
- 51.Mulyana S, Hartati S, Wardoyo R. A Processing Model Using Natural Language Processing (NLP) For Narrative Text Of Medical Record For Producing Symptoms Of Mental Disorders. Paper presented at: 2019 Fourth International Conference on Informatics and Computing (ICIC) 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


