Abstract
For many low-income Medicare beneficiaries, Medicaid provides important supplemental insurance that covers out-of-pocket costs and additional benefits. We examine whether Medicaid participation by low-income adults age 65 and up increased as a result of Medicaid expansions to working-age adults under the Affordable Care Act (ACA). Previous literature documents so-called “welcome mat” effects in other populations but has not explicitly studied older persons dually eligible for Medicare and Medicaid. We extend this literature by estimating models of Medicaid participation among persons age 65 and up using American Community Survey data from 2010 to 2017 and state variation in ACA Medicaid expansions. We find that Medicaid expansions to working-age adults increased Medicaid participation among low-income older adults by 1.8 percentage points (4.4 percent). We also find evidence of an “on-ramp” effect; that is, low-income Medicare beneficiaries residing in expansion states who were young enough to gain coverage under the 2014 ACA Medicaid expansions before aging into Medicare were 4 percentage points (9.5 percent) more likely to have dual Medicaid coverage relative to similar individuals who either turned 65 before the 2014 expansions or resided in non-expansion states. This on-ramp effect is an important mechanism behind welcome mat effects among some older adults.
1. INTRODUCTION
A major component of the Affordable Care Act (ACA) is the expansion of Medicaid coverage to adults ages 19 to 64 with incomes up to 138 percent of the federal poverty guidelines (FPG). Made optional to states by the U.S. Supreme Court’s 2012 decision, Medicaid expansions have been adopted by 36 states and the District of Columbia as of November 2018 (KFF, 2018). In addition to having direct consequences for the targeted population, Medicaid expansions have the potential to generate indirect effects known as “welcome mat” effects, which occur when persons previously eligible for Medicaid, but not enrolled, sign up following coverage expansions to other populations. As summarized by Gruber and Sommers (2019), prior studies suggest that the ACA’s Medicaid expansions significantly increased Medicaid participation by both children and working-age adults who were previously eligible (e.g., Hudson & Moriya, 2017; Frean, Gruber, & Sommers, 2017).
Though not widely studied, the ACA’s Medicaid expansions could also trigger welcome mat effects for previously eligible but unenrolled adults age 65 and older. While nearly all adults age 65 and over are covered by Medicare, Medicare entails substantial out-of-pocket costs and does not cover certain categories of benefits. For eligible low-income persons, Medicaid fills these gaps by covering premiums, cost-sharing, and additional benefits, such as home and community-based services, dental, or vision. Yet, a persistent issue has been low Medicaid participation by eligible low-income older adults. Our focus is on whether the ACA’s Medicaid expansions to working-age adults impacted Medicaid participation for these older Medicare beneficiaries, perhaps due to spillover effects from enrollment assistance and eligibility information intended for newly-eligible working-age persons.
If welcome mat effects occur for older low-income adults, this could have important implications for federal and state governments as well as individual enrollees. Studies from the pre-ACA era suggest that at least half of those eligible for both Medicare and Medicaid do not enroll in Medicaid (Pezzin & Kasper, 2002; Ungaro & Federman, 2009), which is consistent with older Americans’ low take-up of means-tested federal programs in general (Coe & Wu, 2014). Further, dual-eligible adults enrolled in both Medicare and Medicaid have more serious health problems than the average beneficiary and account for disproportionately higher shares of Medicare and Medicaid spending (Jacobson, Neuman, & Damico, 2012). The combination of low baseline Medicaid participation rates and high per capita spending means that welcome mat effects could trigger large increases in federally-financed healthcare spending and state Medicaid spending in particular. While the federal government currently pays for more than 90 percent of the ACA’s Medicaid expansions to working-age adults, it pays about 60 percent of Medicaid program costs for enrollees age 65 and up. Beyond these fiscal considerations, Medicaid’s broader coverage and reduced cost-sharing may alleviate financial barriers to access or adherence to high-quality care, potentially improving health outcomes among low-income seniors (Tamblyn et al., 2001; Trivedi, Moloo, & Mor, 2010).
Welcome mat effects among previously-eligible children and adults have been attributed to general increases in program awareness resulting from expanded outreach and enrollment assistance. While these mechanisms may apply to older adults too, another possibility is that Medicaid expansions to the working-age population provide adults in their early 60s with firsthand experience with Medicaid, which in turn contributes to higher rates of Medicaid participation once they turn age 65. This phenomenon, which we deem the “on-ramp” effect, is unique to older adults and has not been examined in any prior work. The on-ramp effect has potential implications for health and healthcare spending as well; if low-income older adults age into Medicare with fewer untreated chronic conditions, this could reduce spending by Medicare or Medicaid in the long run.
Our study contributes to the literature on Medicaid participation in several ways. It is one of a few studies to examine whether state Medicaid expansions to working-age adults increase Medicaid participation by older low-income Medicare beneficiaries, and it is the first study to investigate the on-ramp effect among individuals who become newly-eligible for Medicaid under the ACA’s expansions before aging into Medicare. The only published study on welcome mat effects in older adults examined smaller, state-level expansions in the 2000s (Mclnerney, Mellor, & Sabik, 2017); in contrast, the present study focuses on the ACA’s Medicaid expansions, which led an estimated 10 million newly-eligible persons to enroll in Medicaid (CBO, 2016). We use data from the 2010 to 2017 American Community Survey (ACS) to study a sample of roughly 350,000 respondents who are age 65 and older and on Medicare. Further, we use state-specific Medicaid income eligibility criteria to more precisely identify those older adults likely to be eligible for Medicaid. To identify welcome mat and on-ramp effects, we use plausibly exogenous variation in state decisions to expand Medicaid to working-age adults under the ACA, and we test our identifying assumptions with pre-trend comparisons and event study specifications.
To preview our results, we find evidence of both welcome mat and on-ramp effects. Specifically, older low-income Medicare beneficiaries residing in states that expanded Medicaid under the ACA were 1.8 percentage points more likely to enroll in Medicaid after the expansion. Given that the Medicaid participation rate was 40.8 percent in the pre-period, the welcome mat effect represents a 4.4 percent increase in take-up. Notably, the welcome mat effect is larger when we exclude individuals who received Supplemental Security Income (SSI), who are automatically enrolled in Medicaid in 35 states. This suggests that the increased Medicaid participation we estimate occurred among seniors who had to apply for Medicaid directly, and is not driven solely by persons whose enrollment would have been administratively facilitated by the SSI program. We also find evidence that the on-ramp effect described above contributes to the increase in Medicaid enrollment. Medicare beneficiaries exposed to the ACA Medicaid expansions as working-age adults in their early 60s were four percentage points (or 9.5 percent) more likely to participate in Medicaid relative to similar individuals who either turned 65 before the 2014 expansions or resided in non-expansion states. Thus, the on-ramp effect is an important mechanism behind welcome mat effects for some older adults.
2. BACKGROUND AND RELATED LITERATURE
We first provide a brief summary of Medicaid benefits and eligibility rules for persons age 65 and up and enrolled in Medicare. For this group, as well as for some disabled persons under age 65, Medicare Part A covers inpatient hospital stays, skilled nursing facility care, hospice care and some home healthcare, while Medicare Part B covers physician services and hospital outpatient care, as well as laboratory, imaging, durable medical equipment, and other outpatient services. Nearly all persons age 65 and up have coverage for Part A and B services through either traditional Medicare or a private Medicare Advantage plan. Traditional Medicare requires beneficiary out-of-pocket spending through monthly Part B premiums (and in some cases Part A premiums) and significant Part A and B cost-sharing (deductibles, coinsurance, and copays). Further, traditional Medicare does not provide coverage for certain types of health services, such as dental, vision, and long-term care benefits, including home and community-based services (HCBS). Estimates suggest that, on average, Medicare pays for about half of all healthcare costs for those enrolled (Lind, 2012).
Both of these coverage gaps in traditional Medicare can be filled by full Medicaid coverage for persons who qualify.1 First, Medicaid pays Medicare premiums and cost sharing for those dually enrolled in both programs. These payments are not trivial: Medicaid spends $1,339 per person on annual Medicare premiums for enrollees age 65 and older, which is nearly half of annual per capita Medicaid spending on children, and one-third of annual per capita Medicaid spending on non-elderly, non-disabled adults (MACPAC, 2018). Second, Medicaid provides coverage for many services that Medicare does not, including long-term care and (in many states) dental and vision benefits.
Adults age 65 and older who live in the community can be eligible for full Medicaid coverage through several pathways. Seventy percent of older dual enrollees are eligible because their incomes and assets fall below state-specific eligibility thresholds (MedPAC and MACPAC, 2018). In 2015, 23 states set eligibility levels for Medicaid equal to SSI eligibility criteria; for a single adult, this requires income to be below 75 percent of the FPG and assets to be below $2,000. Eleven states (called 209(b) states) have the option of using more restrictive criteria, and the remaining 17 states use more generous criteria. Older adults with income and/or assets above their state’s eligibility criteria may be eligible for full Medicaid through optional Medically Needy programs or Home and Community Based Services (HCBS) waivers in some states.
Prior studies show that Medicaid participation by older adults is low. Some estimates suggest that the Medicaid enrollment rate is under 50 percent among community-dwelling Medicare beneficiaries age 65 and older with household incomes at or below 100 percent FPG (Pezzin & Kasper, 2002), and only 27 percent among low-income older adults without employer-sponsored health insurance or Medigap insurance (Ungaro & Federman, 2009). Low take-up rates in other social programs have been explained by the presence of administrative hurdles in the application process that increase the implicit cost of enrollment (Currie, 2004; Remler & Glied, 2003) or by the possibility that program benefits are not salient to individuals (e.g., Bhargava & Manoli, 2015). These explanations may extend to older adults. In terms of administrative hurdles, older applicants for Medicaid must demonstrate that they meet both the income and asset requirements, and this age group did not benefit from the ACA’s adoption of the simpler Modified Adjusted Gross Income (MAGI) criteria used for younger, non-disabled applicants. Further, some applicants must submit a separate application to the state Medicaid or human services office.2,3 Furthermore, older adults who have Medicare but are unaware of its coverage gaps may perceive the benefits of Medicaid participation to be low.
Prior work also shows that Medicaid participation by older adults is linked to changes in Medicaid eligibility rules and/or benefits. Ungaro & Federman (2009) found that persons in states with liberalized Medicaid eligibility rules (rules that exclude certain income or asset amounts when making eligibility determinations) were more likely to enroll in Medicaid. Pezzin & Kasper (2002) and Gardner & Gilleskie (2012) found that persons in states with more generous coverage for HCBS were more likely to enroll in Medicaid. Examining the effects of state Medicaid expansions in the 2000s, McInerney, Mellor, & Sabik (2017) found some evidence that low-income older adults were more likely to be enrolled in Medicaid in states with more generous Medicaid eligibility for adults ages 20 to 64 years old.
Our work adds to the prior literature on both Medicaid participation by older adults and welcome mat effects from Medicaid expansions. The welcome mat literature finds that state Medicaid expansions in the 1990s and 2000s increased Medicaid enrollment by already-eligible children (Aizer & Grogger, 2003; Dubay & Kenney, 2003; Hamersma, Kim, & Timpe, 2019; Kenney, Long, & Luque, 2010) and reports similar increases in children’s Medicaid coverage following the ACA’s Medicaid expansions (Sommers et al., 2016; Hudson & Moriya, 2017). Prior studies also document welcome mat effects for working-age adults in response to Massachusetts’ 2006 reforms (Sonier, Boudreaux, & Blewitt, 2013), the early ACA expansions that took place in 2010 in some states (Sommers, Kenney, & Epstein, 2014, Sommers et al., 2016), and the 2014 ACA Medicaid expansions (Frean, Gruber, & Sommers, 2017).
Welcome mat effects among older adults may be smaller than those observed among previously-eligible children and working-age adults. One reason that expansions to working-age adults have spillover benefits for children is that enrolling parents complete the same Medicaid application required to enroll a child. This type of intra-family spillover is not present for older adults since the Medicaid application procedures for older adults differ from those for working-age adults. In addition, welcome mat effects observed for working-age adults under the ACA arose partly from the individual mandate, which imposed a cost on uninsured persons who did not obtain coverage.4 This cost did not apply to persons enrolled in Medicare, who already met the mandate’s coverage requirements.
Alternatively, welcome mat effects for older adults may be larger. This could arise in part because Medicaid participation rates are lower for eligible older adults than for eligible children and working-age adults. Specifically, estimates of Medicaid participation rates range from 27 to 50 percent for older adults, compared to 87 percent for children (Kenney, Anderson, & Lynch, 2013) and 52 percent for working-age adults (Davidoff, Yemane, & Adams, 2005). Moreover, larger welcome mat effects could arise because of our hypothesized on-ramp effect (which occurs when older adults who were young enough to benefit from the ACA Medicaid expansions as working-age adults become more likely to participate in Medicaid as dual eligibles after age 65). Our analysis of Health and Retirement Study (HRS) longitudinal data suggests that there is substantial continuity in Medicaid enrollment before and after participants turn age 65: 73 percent of adults who were enrolled in Medicaid at ages 63 or 64 were also enrolled at ages 65 or 66.5 Thus, factors that increase Medicaid participation before an individual turns 65 could potentially increase Medicaid participation after age 65, contributing to welcome mat effects in this age group.6
3. DATA AND METHODS
We use data from the Integrated Public Use Microdata Series (IPUMS) American Community Survey (ACS) annual files from 2010 through 2017 (Ruggles et al., 2019). The ACS is an ongoing mandatory federal survey that collects data on demographic, social, and economic characteristics of the U.S. population. Given its large sample size (nearly 3 million persons in each year), the ACS is recommended by the Census Bureau for state- and local-level analysis of insurance coverage (Smith & Medalia, 2014).
To construct our main sample, we start with ACS respondents age 65 and over, who number about 4.5 million persons across our study period.7 We then exclude non-citizens (about 2.6 percent of respondents age 65 and up) and persons residing in group quarters since nursing home residents face very different circumstances regarding Medicaid enrollment than the community-dwellers who are the focus of our analysis (another 5.5 percent of the sample). Finally, we exclude persons not enrolled in Medicare (another 2.7 percent of the sample). The remaining sample consists of 3.99 million ACS respondents.
We next use Medicaid eligibility rules in each state to identify persons who would be income-eligible for full Medicaid in their state.8 We first identify whether the state uses SSI or optional poverty coverage criteria or is a 209(b) state; we then apply the corresponding income criteria. In SSI states, eligibility is set by the Social Security Administration; in our study period, eligibility is based on having income at or below approximately 75 percent FPG for individuals or 83 percent FPG for couples (Watts, Cornachione, & Musumeci, 2016). In 209(b) states, Medicaid eligibility criteria can be restricted to income thresholds below that of SSI (SSA POMS SI 01715.010, n.d.). In states that use optional coverage provisions, Medicaid eligibility is extended to older adults with incomes over the SSI threshold and up to 100 percent FPG (Watts, Cornachione, & Musumeci, 2016).9
To apply these criteria to ACS respondents, we use published data on states’ SSI, 209(b), and optional income eligibility criteria (Watts, Cornachione, & Musumeci, 2016); see Appendix Table 1. We use eligibility criteria from a single year, 2015, to keep the composition of the sample respondents consistent in each state throughout the analysis (Bruen, Wiener, & Thomas, 2003; KFF, 2010).10 These data report the state’s income cutoff for determining Medicaid eligibility as a share of the federal poverty level, for individuals and couples separately. For example, California uses an income cutoff equal to 100 percent FPG for both individuals and couples, while Wisconsin uses a cutoff of 83 percent FPG for individuals and 93 percent FPG for couples. We compare the state cutoff to each respondent’s poverty measure; the poverty measure reports family income for the respondent as a percentage of the federal poverty guideline based on each respondent’s detailed income and family structure information (SHADAC, 2013).11 We follow SHADAC (2013) procedures for constructing this measure from the IPUMS ACS.12 In comparing each respondent’s poverty measure to the state eligibility criteria, we use the respondent’s marital status to apply either the individual or couple eligibility cutoff. After applying these criteria to all ACS respondents, we select only those respondents who would be eligible for Medicaid based on their state’s criteria and their own income/marital status. After applying these restrictions, our sample consists of 347,781 ACS respondents age 65 and up, on Medicare, not living in group quarters, and eligible for Medicaid based on the pathways to full Medicaid described above.
Estimation Strategy
To test for a welcome mat effect among low-income older adults, we estimate difference-in-differences (DD) models of Medicaid participation as shown in equation (1):
| (1) |
The dependent variable (Yist) is a binary indicator of Medicaid participation based on whether ACS respondent i in state s and year t had health insurance coverage through Medicaid or other governmental insurance for persons with low incomes/disability at the time of the survey. The term Postt*Expansions is equal to one for sample respondents living in expansion states in the year of the expansion or later, and zero otherwise. In our time period, 32 states, including the District of Columbia, expanded Medicaid between 2014 and 2017, as shown in Appendix Table 2.13 A positive and significant estimate of γ would provide evidence of a welcome mat effect. Given that the ACA Medicaid expansions did not impact Medicaid eligibility for senior Medicare beneficiaries, any associated increase in participation is due to indirect effects of that policy.
We control for various exogenous factors that may affect Medicaid participation (represented by Xist) including age fixed effects, the respondent’s sex, race, ethnicity, educational attainment, and whether the respondent is a naturalized citizen. We include state fixed effects (λs) to capture time-invariant unobserved differences across states, and we include year fixed effects (τt) to capture changes over time that are common to all states. We report standard errors clustered by state, and we weight observations using the ACS person weights provided by the Census Bureau. In addition to the DD model shown in equation (1), we also test for welcome mat effects using an event study, which allows us to test the common trends assumption behind the DD approach. Further, we examine the sensitivity of our main results to the addition of various model controls and to changes in the sample.
We next test for evidence of an on-ramp effect, or evidence of increased Medicaid participation by low-income Medicare beneficiaries in expansion states who were young enough to gain Medicaid coverage under the ACA as working-age adults (relative to similar individuals who either turned 65 before the expansions or resided in non-expansion states). We test this with a difference-in-difference-in-differences (DDD) model and by focusing on the 2014 expansions. Treatment status is defined as being surveyed at least one year post-expansion (i.e., 2015, 2016 or 2017), residing in an expansion state, and being age 65 at the time of the survey. Importantly, adults who were age 65 when they were surveyed between 2015 and 2017 would have been 62 to 64 years old at the time of the 2014 Medicaid expansions, and thus would have been exposed to the Medicaid expansion as working-age adults. In contrast, adults who were age 68 and up between 2015 and 2017 would have been at least 65 when the 2014 expansions took place, and were too old to gain coverage under the Medicaid expansion.14 Our DDD strategy essentially compares DD estimates (where the treatment is residing in an expansion state, and post is defined as one year after the 2014 Medicaid expansion) across two groups: 1) persons age 65 at the time of the survey, and 2) persons age 68 and over at the time of the survey.
Formally, we estimate equation (2):
| (2) |
As in equation (1), the dependent variable is a binary indicator of Medicaid participation at the time of the survey, though equation (2) also incorporates variation in age such that (Yigst) indicates Medicaid participation for respondent i in age group g who resides in state s in year t, and Expansions is an indicator for residing in an expansion state. Post 2015t is equal to one in 2015, 2016, and 2017 (and 0 in 2014 and earlier), and Age 65 in Year of Surveyg is equal to one for respondents who are age 65 at the time of the survey (and zero if over 65). A positive and statistically significant estimate of β1 would provide evidence of an “on-ramp effect.” The DDD approach controls for permanent differences across expansion versus non-expansion states in Medicaid enrollment of 65 year-olds (captured by β2) and secular trends in Medicaid participation among 65 year-olds common to both expansion and non-expansion states (captured by β3), and allows us to identify changes in Medicaid enrollment over and above any ACA expansion-induced changes in Medicaid participation that are common to all older adults (captured by β4).
The DDD model differs in several other ways from our DD model in equation (1). As noted, we define the post period as starting in 2015, since it is the first year we can observe an on-ramp effect among 65 year-olds. In 2014, 65 year-olds would not have qualified for the ACA’s Medicaid expansions as working-age adults. We also focus only on the Medicaid expansions that occurred in 2014 and exclude respondents residing in states that expanded Medicaid in later years in our sample. This allows us to test for on-ramp effects with three years of data after the Medicaid expansion. Because of this sample restriction it is not possible to quantify the contribution of the on-ramp effect to the effect we estimate in equation (1). Instead we investigate the relative contribution of the on-ramp effect indirectly, by estimating our DD specification in equation (1) only for those persons who are age 70 and older and would not be subject to the potential on-ramp effect.
Another difference is that we estimate equation (2) for a subset of respondents based on age. First, we exclude 66 and 67 year-olds because their exposure to Medicaid expansion is imprecisely measured. For example, 66 year-olds in 2015 were already 65 in 2014, and too old to qualify for expanded Medicaid coverage for working-age adults, while 66 year-olds in 2016 were 64 in 2014, and would have qualified. Second, we limit the comparison group to persons ages 68 and 69. As we show in Appendix Table 4, the mean observable traits of 65 year-olds are very comparable to those of 68 and 69 year-olds, which suggests that these two age groups are likely similar in terms of unobservable traits such as health risks or comorbidities. In a sensitivity analysis, we also report results including older respondents in the comparison group.
4. RESULTS
A. Welcome Mat Effect Estimates
Table 1 describes the main sample used to estimate equation (1); we report means separately for respondents in expansion and non-expansion states surveyed before and after the expansion and include means for the equation (1) controls and for other controls used in robustness checks. Across all subgroups, a majority of respondents are female, non-Hispanic white, and have a high school degree or more. In the pre-period, respondents in expansion and non-expansion states are similar in terms of reported cognitive difficulties (difficulties learning, remembering, concentrating, or making decisions), physical difficulties (difficulties walking, climbing stairs, reaching, lifting, or carrying), independent living difficulties (difficulties performing tasks outside the home, such as shopping), self-care difficulties (difficulties with tasks inside the home, such as bathing and dressing), and difficulties with vision and hearing. In the pre-period, between seven and eight percent of respondents own non-housing assets.15 Compared to those in non-expansion states, respondents in expansion states are more likely to be naturalized citizens and are more highly educated. The average Medicaid participation rate in the pre-period is 1.5 percentage points higher in states that expanded Medicaid (40.8 percent) than in states that did not (39.3 percent).
Table 1.
Descriptive statistics, welcome mat effect analysis, 2010-2017 ACS, ages 65+.
| Expansion States | Non-Expansion States | ||||
|---|---|---|---|---|---|
| Pre | Post | Pre | Post | DD | |
| Medicaid participation at time of survey | 0.408 | 0.417 | 0.393 | 0.377 | 0.026*** |
| Female | 0.69 | 0.67 | 0.69 | 0.68 | −0.004 |
| Age | 76.2 | 75.8 | 76.0 | 75.6 | −0.038 |
| White | 0.58 | 0.55 | 0.58 | 0.56 | −0.008 |
| Black | 0.13 | 0.12 | 0.21 | 0.21 | −0.009*** |
| Hispanic | 0.14 | 0.16 | 0.16 | 0.17 | 0.007** |
| Other race | 0.14 | 0.16 | 0.05 | 0.06 | 0.010*** |
| Naturalized citizen | 0.27 | 0.31 | 0.17 | 0.19 | 0.017*** |
| Less than high school | 0.38 | 0.34 | 0.43 | 0.36 | 0.023*** |
| High school degree | 0.34 | 0.33 | 0.33 | 0.34 | −0.023*** |
| Some college | 0.17 | 0.19 | 0.16 | 0.18 | −0.004 |
| College or more | 0.11 | 0.14 | 0.09 | 0.11 | 0.005* |
| Income ($10,000, 2017) | 3.21 | 3.45 | 2.52 | 2.74 | 0.016 |
| Income as % FPG | 59.6 | 55.9 | 55.8 | 52.0 | 0.070 |
| Single elig. (% FPG) | 93.0 | 92.7 | 86.3 | 85.8 | 0.130 |
| Couple elig. (% FPG) | 95.4 | 95.2 | 89.0 | 88.7 | 0.164*** |
| Employed | 0.02 | 0.02 | 0.02 | 0.03 | −0.003** |
| Married | 0.26 | 0.28 | 0.26 | 0.27 | 0.008** |
| Widowed | 0.40 | 0.36 | 0.42 | 0.38 | 0.001 |
| Separated or divorced | 0.23 | 0.24 | 0.24 | 0.26 | −0.007 |
| Never married | 0.10 | 0.11 | 0.09 | 0.09 | −0.002 |
| Cognitive difficulty | 0.17 | 0.16 | 0.18 | 0.16 | 0.005 |
| Ambulatory difficulty | 0.36 | 0.34 | 0.37 | 0.34 | 0.018*** |
| Independent living difficulty | 0.28 | 0.27 | 0.28 | 0.25 | 0.013*** |
| Self-care difficulty | 0.15 | 0.15 | 0.16 | 0.14 | 0.016*** |
| Vision difficulty | 0.11 | 0.10 | 0.12 | 0.11 | 0.001 |
| Hearing difficulty | 0.17 | 0.17 | 0.18 | 0.17 | 0.012*** |
| Any non-housing assets | 0.08 | 0.09 | 0.07 | 0.08 | −0.004* |
| Receive SSI | 0.17 | 0.17 | 0.12 | 0.12 | 0.0001 |
| State unemployment rate | 8.82 | 5.41 | 8.26 | 4.99 | −0.140*** |
| Share of state Medicare enrollees in Med. Adv. | 0.29 | 0.32 | 0.24 | 0.31 | −0.033*** |
| N | 104,080 | 111,721 | 61,740 | 70,240 | 347,781 |
Notes: Sample weights are used in the calculation of means. The sample consists of respondents to the 2010-17 ACS who are 65 or older and income-eligible for Medicaid according to the criteria in their state of residence. In expansion states, Post=1 beginning the year of the expansion; in non-expansion states, Post=1 beginning in 2014. Statistically significant unadjusted DD differences are indicated by
for the .01 level,
for the .05 level, and
for the .10 level.
We use the main sample described in Table 1 to estimate both unadjusted and adjusted DD estimates of the overall welcome mat effect. We calculate the unadjusted DD estimate using the mean Medicaid participation rates reported in Table 1. This yields a statistically significant welcome mat effect of 2.6 percentage points, or 6.4 percent, of pre-expansion Medicaid participation rates in expansion states. We report the adjusted DD estimate obtained from estimating equation (1) in Table 2, column (1). Adjusting for covariates yields a positive and statistically significant welcome mat effect of 1.8 percentage points, or 4.4 percent, of pre-expansion Medicaid participation rates in expansion states. Coefficient estimates for the covariates in this model are reported in Appendix Table 3.
Table 2.
Welcome mat effect estimates, baseline DD specification with alternate controls.
Linear probability model (DV=Medicaid participation)
| Baseline specification | State and year fixed effects only | Baseline + disability | Baseline + own home | Baseline + any non-housing assets | Baseline + SSI receipt | Baseline + other potentially endogenous variables | Baseline + all | |
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| Expansion x Post | 0.018*** | 0.021*** | 0.015*** | 0.019*** | 0.017*** | 0.020*** | 0.021*** | 0.018*** |
| (0.006) | (0.006) | (0.005) | (0.006) | (0.006) | (0.005) | (0.008) | (0.005) | |
| Ambulatory diff. | 0.093*** | 0.033*** | ||||||
| (0.003) | (0.004) | |||||||
| Cognitive diff. | 0.053*** | 0.017*** | ||||||
| (0.004) | (0.003) | |||||||
| Ind. living diff. | 0.082*** | 0.030*** | ||||||
| (0.008) | (0.004) | |||||||
| Self-care diff. | 0.043*** | 0.029*** | ||||||
| (0.009) | (0.004) | |||||||
| Vision diff. | 0.038*** | 0.017*** | ||||||
| (0.004) | (0.004) | |||||||
| Hearing diff. | 0.007** | 0.000 | ||||||
| (0.003) | (0.003) | |||||||
| Own home | −0.206*** | −0.124*** | ||||||
| (0.010) | (0.006) | |||||||
| Any non-housing assets | −0.169*** | −0.093*** | ||||||
| (0.013) | (0.004) | |||||||
| Receives SSI | 0.600*** | 0.532*** | ||||||
| (0.018) | (0.020) | |||||||
| Employed | −0.126*** | −0.032*** | ||||||
| (0.008) | (0.005) | |||||||
| Married | −0.200*** | −0.100*** | ||||||
| (0.007) | (0.005) | |||||||
| Widowed | −0.114*** | −0.058*** | ||||||
| (0.008) | (0.005) | |||||||
| Separated/divorced | −0.015*** | 0.001 | ||||||
| (0.005) | (0.005) | |||||||
| Income ($10K, 2017) | −0.00002*** | −0.000003 | ||||||
| (0.000005) | (0.00003) | |||||||
| State unemp. rate | 0.003 | −0.000 | ||||||
| (0.003) | (0.002) | |||||||
| Share of state Medicare enrollees in Med. Adv. | 0.042 | −0.059 | ||||||
| (0.099) | (0.066) | |||||||
| Observations | 347,781 | 347,781 | 347,781 | 347,781 | 347,781 | 347,781 | 347,781 | 347,781 |
| Implied effect size | 4.4% | 5.1% | 3.7% | 4.7% | 4.2% | 4.9% | 5.1% | 4.4% |
| , Pre, exp | 0.408 | 0.408 | 0.408 | 0.408 | 0.408 | 0.408 | 0.408 | 0.408 |
Notes: The sample consists of respondents to the 2010-17 ACS who are age 65 or older and income-eligible for Medicaid according to the criteria in their state of residence. The baseline specification includes controls for black race, other race, Hispanic ethnicity, female, naturalized citizenship status, and education (high school diploma, some college, and college degree or more), age fixed effects, state fixed effects, and year fixed effects. Sample weights are used in model estimation. Standard errors clustered by state are reported in parentheses. Statistical significance is indicated by
for the .01 level,
for the .05 level and
for the .10 level.
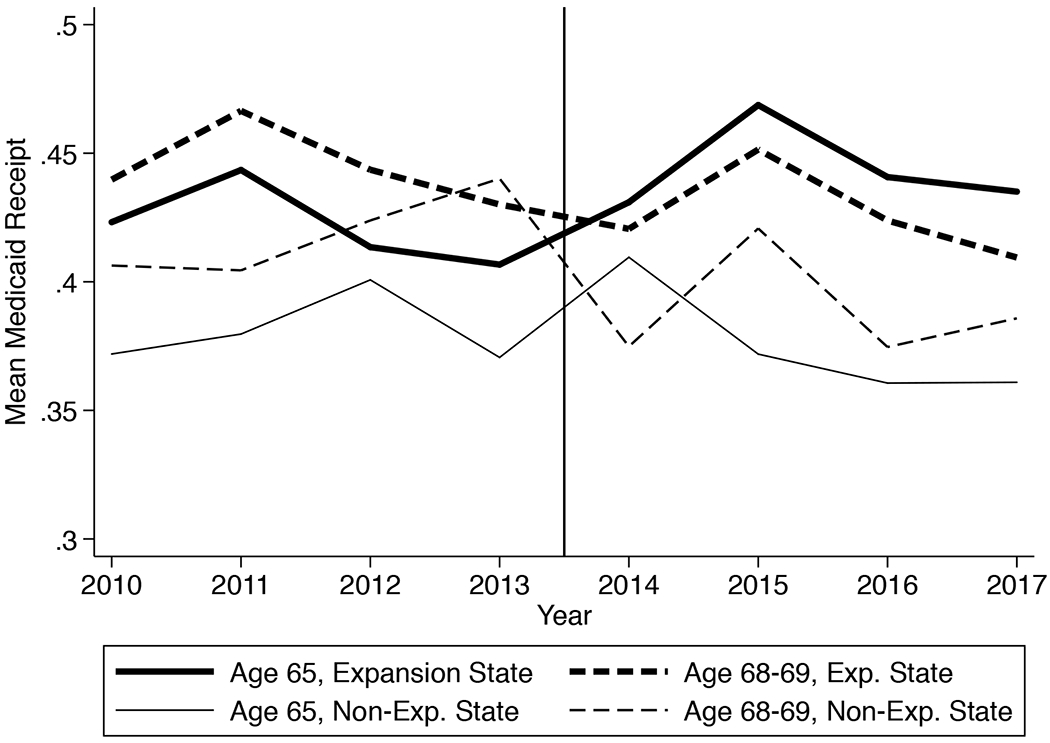
To examine support for the parallel trends assumption underlying the DD analysis, we plot mean Medicaid participation among respondents in each year for expansion and non-expansion states separately. Figure 1 shows that mean Medicaid participation is about 1.5 percentage points higher in expansion than non-expansion states in the first year of our study period, and this difference is persistent across the pre-expansion period, which supports the parallel trends assumption. By 2017, mean Medicaid participation is 3.9 percentage points higher for respondents living in expansion states than those in non-expansion states.
Figure 1.
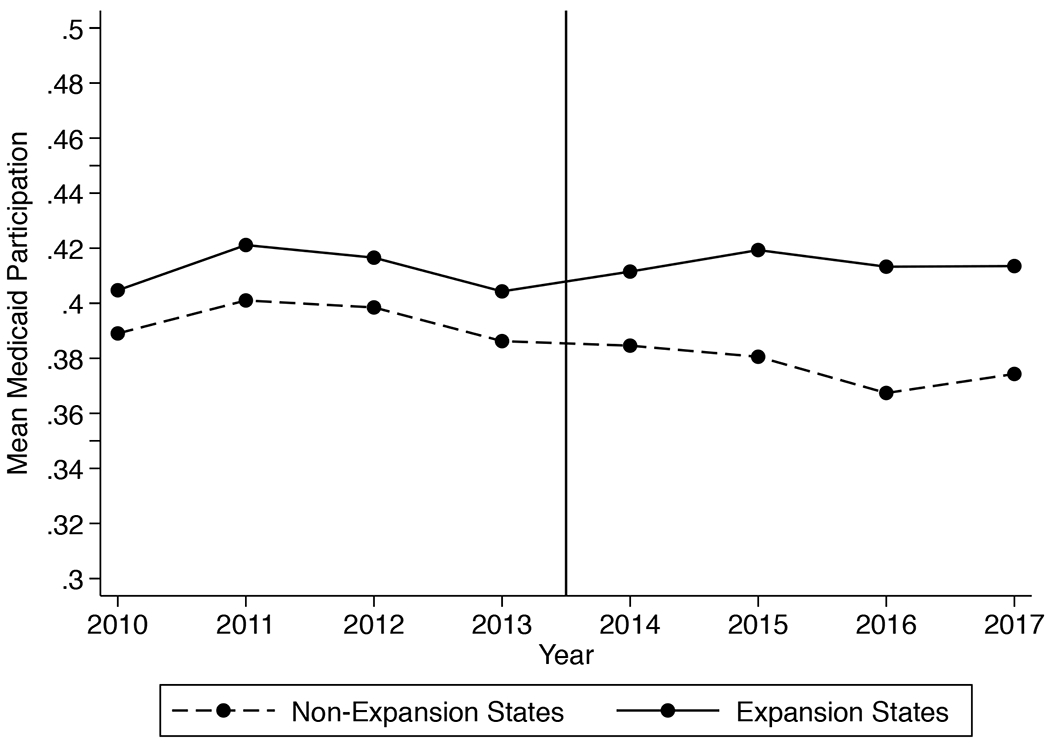
Trends in Medicaid Enrollment Among Low-Income Older Adults Age 65+.
Notes: Sample weights are used in the calculation of means.
For additional support of the parallel trends assumption, we estimate an event study specification using a comparison group. In this model, we replace the term “Post * Expansion” in equation (1) with a full set of indicator variables representing each year, relative to the expansion year, interacted with the Expansion indicator variable; non-expansion states are coded as zero in all years. We omit the indicator variable for the year prior to expansion in the state. Figure 2A plots the coefficients of these interaction terms and their confidence intervals and again shows the absence of a differential pre-expansion trend between expansion and non-expansion state respondents. The coefficient estimates in the years prior to expansion are close to zero (ranging from 0.0008 to 0.0043) and are not statistically significant individually or as a group (the p-value from an F-test of joint significance is 0.965). In contrast, residents of expansion states are more likely to be enrolled in Medicaid in the year of the expansion and the years following the expansion. Expansion state respondents are 1.5 percentage points more likely to be on Medicaid in the year of the expansion (p=0.084), 2.7 percentage points more likely to be on Medicaid two years post-expansion, and 1.6 percentage points more likely to be on Medicaid three years post-expansion (p=0.052). We also estimate this same event study specification using a sample that is a balanced panel in event time (that is, a sample that excludes states that expanded Medicaid in 2015 or 2016). Figure 2B plots the coefficient estimates and their confidence intervals. The main results are the same. There is no evidence of a differential pre-trend between expansion and non-expansion state respondents, and compared to those in non-expansion states, older adults in expansion states are significantly more likely to be enrolled in Medicaid after the expansion.
Figure 2A.
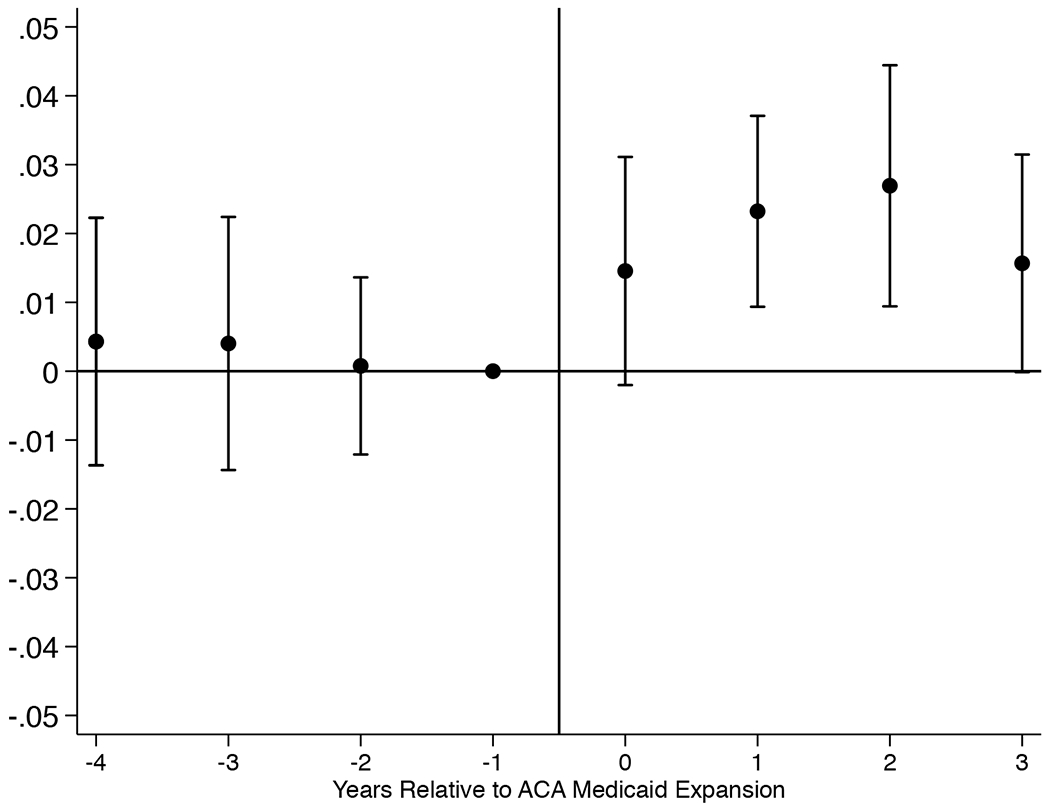
Event Study Estimates, Full Sample.
Notes: Coefficients from an event study specification are reported along with 95% confidence intervals that account for within-state clustering. Each coefficient estimate reflects the interaction of an indicator for state adoption of the Medicaid expansion with an indicator for years relative to the Medicaid expansion, estimated from a linear probability model of Medicaid participation. The model controls for the other explanatory variables included in the baseline model in Table 2, plus state fixed effects and year fixed effects. Standard errors are clustered by state. Expansion x 1 Year Pre Expansion is the omitted category.
Figure 2B.
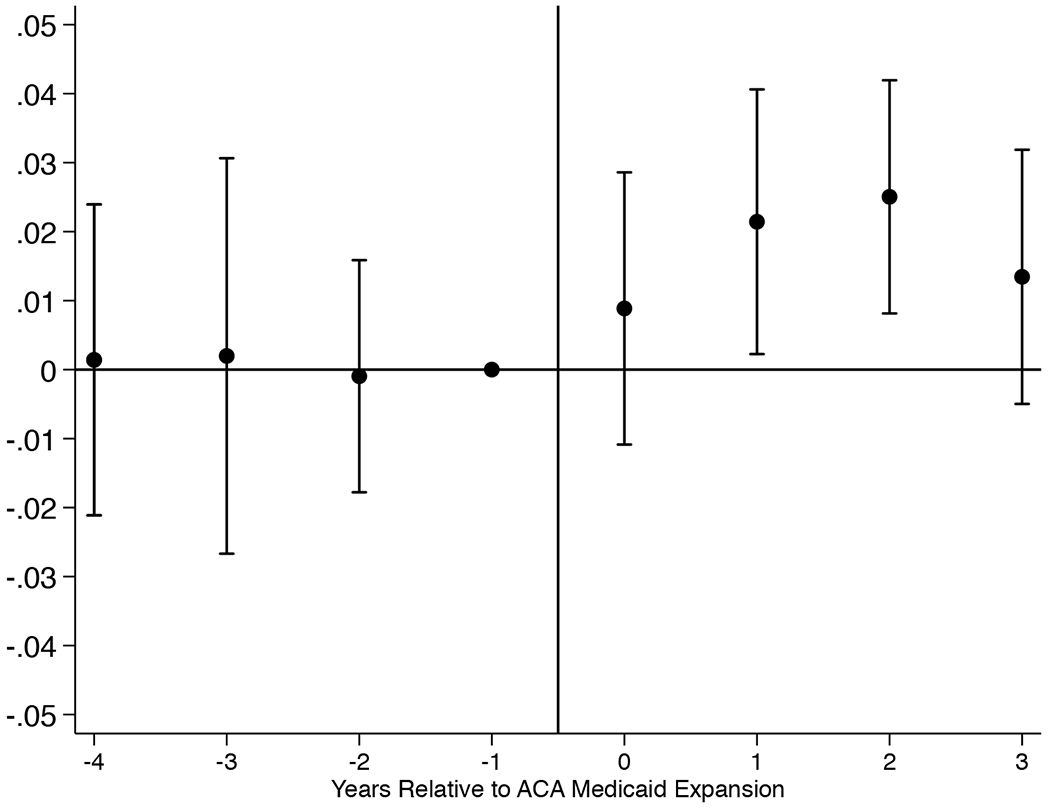
Event Study Estimates, Excluding States that Expanded Medicaid in 2015, 2016, or 2017.
Notes: Coefficients from an event study specification are reported along with 95% confidence intervals that account for within-state clustering. Each coefficient estimate reflects the interaction of an indicator for state adoption of the Medicaid expansion with an indicator for years relative to the Medicaid expansion, estimated from a linear probability model of Medicaid participation. The model controls for all the other explanatory variables included in the baseline model in Table 2, plus state fixed effects and year fixed effects. Expansion x 1 Year Pre Expansion is the omitted category.
B. Tests of the Robustness of the Welcome Mat Effect
In additional columns of Table 2, we report tests of the robustness of the welcome mat effect to changes in the controls. In column (2), we omit all respondent traits and include only state and year fixed effects. In column (3), we include the controls from the baseline model and also add controls for respondent disabilities. In columns (4) through (6), we add controls for home ownership, non-housing asset ownership, and SSI receipt, respectively. We excluded these controls from the main model because they are potentially endogenous; for example, some individuals could strategically reduce their assets in order to gain eligibility for Medicaid. In column (7) we add controls for marital status, income, employment status, the state unemployment rate and the state Medicare Advantage penetration rate.16 In column (8), we add all of the preceding controls from columns (3) through (7). Across the board, these changes to the controls have little effect on the estimated welcome mat effect; the DD estimates are always positive and statistically significant, and are similar in size to the baseline estimate in column (1).17
Table 3 reports the results of additional robustness checks. In column (1) we show that the DD estimate from unweighted data is very similar to the baseline estimate shown in Table 2. In column (2) of Table 3, we confirm that the DD estimate is robust to excluding SSI recipients, which is important since Medicaid enrollment is automatic for SSI recipients residing in 1634 states. The DD estimate from this exercise suggests a slightly larger welcome mat effect of 2.4 percentage points which corresponds to an 8.1 percent increase in Medicaid receipt. Given the limited asset data in the ACS, our main sample may include persons whose asset levels exceed the typical $2,000 or $3,000 limit for Medicaid eligibility. For this reason, column (3) of Table 3 excludes ACS respondents who have any non-housing assets (i.e., they report some business, farm, interest, dividend, or rental income).18 This check leads us to drop 9.4 percent of our low-income sample, and the DD welcome mat estimate is robust to this exclusion as well. Our main sample consists of ACS respondents who are income-eligible for Medicaid based on state-specific criteria. To ensure that the effects we observe in the main sample are not driven by heterogeneous responses across different income levels, we alternatively select low-income respondents uniformly across all states. In column (4) of Table 3, we include older adults with incomes up to 100 percent FPG in every state, even those where the SSI/209(b)/poverty-Medicaid income eligibility threshold is lower (e.g., 75 percent FPG), and in column (5), we include older adults with incomes up to 150 percent FPG. In both of these checks, the DD estimates are positive and statistically significant.19
Table 3.
Welcome mat effect estimates, robustness checks.
Linear probability model (DV=Medicaid participation)
| Unweighted | Drop SSI recipients | Drop respondents with any non-housing assets | All ACS respondents with income <= 100% FPG | All ACS respondents with income <= 150% FPG | |
|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | |
| Expansion x Post | 0.016*** | 0.024*** | 0.019*** | 0.015** | 0.012** |
| (0.005) | (0.006) | (0.006) | (0.006) | (0.005) | |
| , Pre, exp. | 0.396 | 0.297 | 0.431 | 0.423 | 0.325 |
| Implied effect size | 4.0% | 8.1% | 4.4% | 3.5% | 3.7% |
| N | 347,781 | 298,462 | 314,967 | 452,929 | 961,734 |
| Drop states that had coverage for childless adults in the pre period | Drop early expansion states | Drop states with mid-year expansions | Keep treatment states with lowest pre-period dual enrollment | Drop states that expanded Medicaid in 2015, 2016, or 2017 | |
| (6) | (7) | (8) | (9) | (10) | |
| Expansion x Post | 0.014** | 0.019** | 0.020*** | 0.010 | 0.017** |
| (0.005) | (0.008) | (0.006) | (0.007) | (0.006) | |
| , Pre, exp. | 0.394 | 0.378 | 0.413 | 0.251 | 0.420 |
| Implied effect size | 3.6% | 5.0% | 4.8% | 4.0% | 4.0% |
| N | 314,219 | 261,488 | 317,054 | 148,039 | 316,994 |
Notes: All samples consist of respondents to the 2010-17 ACS who are age 65 or older. In columns (4) and (5), the samples are defined from all ACS respondents who reside in the community and meet the income restrictions shown. The samples in columns (1)-(3) and (6)-(10) are defined from the baseline sample, which further restricts the sample to include only those who are income-eligible for Medicaid according to the criteria in their state of residence. Column (6) excludes respondents in the District of Columbia, Delaware, Massachusetts, New York, and Vermont because these states had coverage for childless adults prior to 2014 (as in Miller and Wherry, 2017 and Ghosh et al., 2019). Column (7) excludes respondents in California, Connecticut, the District of Columbia, Massachusetts, Minnesota, New Jersey, and Washington because these states enacted expansions early (as in Frean et al., 2017). Column (8) excludes respondents in Michigan, New Hampshire, Indiana, Louisiana, and Alaska. In column (9), the treatment group is comprised of residents of Alaska, Colorado, Connecticut, Delaware, Iowa, Montana, New Hampshire, North Dakota, and Ohio. Column (10) excludes residents of the states that expanded Medicaid after 2014 (but before 2017): Pennsylvania, Indiana, Alaska, Montana, and Louisiana. All models also include the controls reported in the baseline specification shown in Table 2, column 1. Sample weights are used (except in column 1). Standard errors clustered by state are reported in parentheses. Statistical significance is indicated by
for the .01 level,
for the .05 level and
for the .10 level.
Columns (6) through (10) of Table 3 report the robustness of the estimated welcome mat effect to changes in the states included in the sample. In column (6), we exclude states that provided Medicaid coverage to childless adults with incomes up to 100 percent FPG or higher during the years 2010 through 2013 (DC, Delaware, Massachusetts, New York, and Vermont), as in Miller & Wherry (2017) and Ghosh, Simon, & Sommers (2019). In column (7), we exclude states that had early (albeit small in some cases) Medicaid expansions (California, Connecticut, DC, Massachusetts, Minnesota, New Jersey and Washington), as in Frean, Gruber, & Sommers (2017). In column (8), we exclude states that had mid-year expansions (Michigan, New Hampshire, Indiana, Louisiana, and Alaska), as in Courtemanche et al. (2017). In column (9), we limit the treatment group to respondents from expansion states with the lowest Medicaid coverage rates among older adults prior to 2014 (similar to Simon, Soni, & Cawley, 2017). In these states (Alaska, Colorado, Connecticut, Delaware, Iowa, Montana, New Hampshire, North Dakota, and Ohio), Medicaid participation rates were below 29 percent. In column (10), we limit the treatment group to respondents from states that expanded Medicaid in 2014 only; this allows for a longer horizon over which to observe welcome mat effects. In all but one instance, the DD estimate of the welcome mat effect is positive and statistically significant, and similar in size to our baseline estimate.
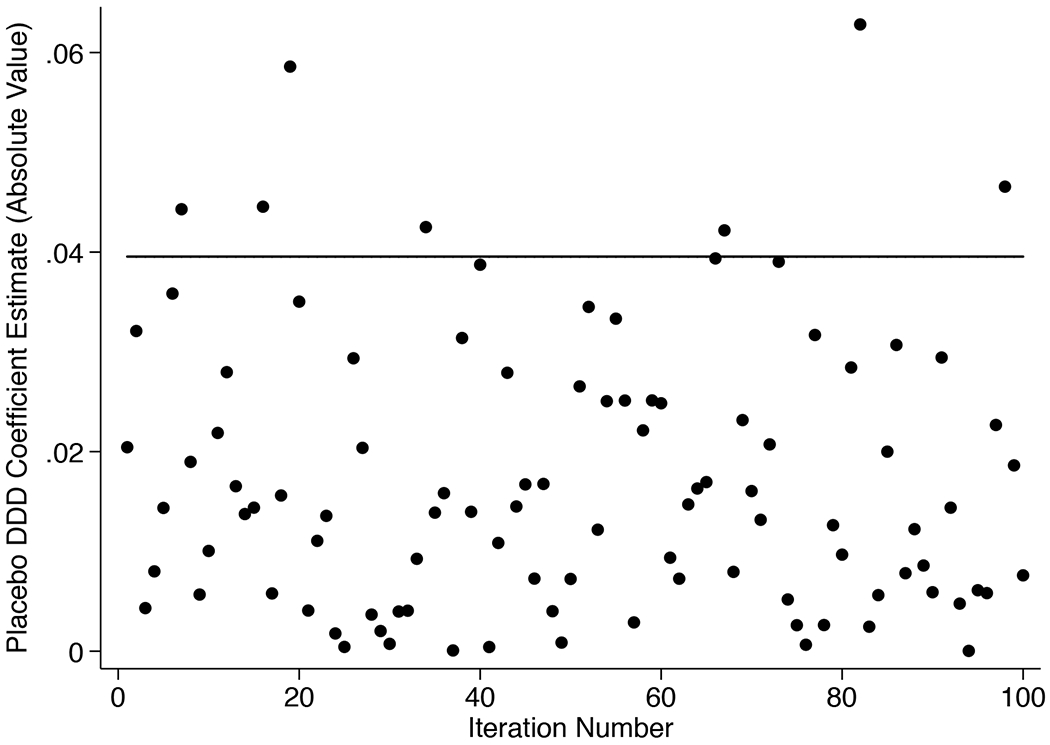
Finally, we conducted three additional checks on our DD welcome mat estimates. We estimated a leave-one-out analysis, in which we estimated the main specification repeatedly, leaving each of the treatment states out of the analysis one at a time. The results of this exercise are reported in Appendix Figure 1A, which plots the 32 DD estimates and their confidence intervals. All of these DD estimates are positive and statistically significant at the 5 percent level, and our baseline coefficient always falls within the 95 percent confidence interval. We also conducted a placebo analysis by assigning treatment status to 27 states at random (to reflect the 27 states that expanded Medicaid in 2014) and then estimating equation (1) where Post equals one beginning in 2014 (we exclude the late-adopting states in this exercise). We did the random assignment 100 times, and we report the estimated placebo DD coefficients in Appendix Figure 2A. Each point represents the absolute value of a placebo DD estimate from a different iteration, and together these placebo estimates approximate the distribution of treatment effects under the null hypothesis that the ACA Medicaid expansions had no effect on older adults’ Medicaid participation (Bertrand, Duflo, & Mullainathan, 2004; Kaestner, 2016). In 11 iterations the absolute value of placebo DD is larger than the welcome effect estimate from our baseline specification; therefore, the p-value from randomization inference is 0.11, which exceeds the 10% threshold. We do note, however, that in eight of the 11 iterations, the placebo DD is negative. Lastly, to bolster confidence that our results are not driven by differential trends, we used the 2010 through 2013 data to estimate state-specific trends in Medicaid participation over time, and then used each state’s coefficient estimate of the trend term to de-trend our dependent variable. We then estimated equation (1) using the de-trended outcome and omitting year fixed effects. The DD estimate from this exercise is 0.016 (similar to our baseline estimate of 0.018) although the standard error increases and the estimate is no longer statistically significant (results available upon request). Thus, our baseline welcome mat effect estimate is generally supported by these additional tests.20
C. Do Welcome Mat Effects Represent Crowd-Out?
Our baseline DD estimate suggests that the ACA’s Medicaid expansions increased the likelihood that an eligible older adult enrolled in Medicaid by 1.8 percentage points. It is possible that this increased Medicaid coverage represents newly obtained supplemental coverage to Medicare, but it may represent changes in the type of supplemental coverage that Medicare beneficiaries have. As an example of the latter scenario, an individual may drop private coverage through a retiree plan and subsequently enroll in Medicaid, in which case the newly-gained Medicaid coverage results from the crowd-out of private coverage. To test this, we use equation (1) to model two alternate outcomes: first, we define a dependent variable equal to one if the respondent has private insurance coverage and no Medicaid coverage (zero otherwise), and second, we define a dependent variable equal to one if the respondent has Medicare coverage alone (zero otherwise). Table 4 reports the results (with column 1 reporting our baseline DD for comparison). Column 2 shows that the welcome mat effect does not arise from the crowd-out of private coverage. Column 3 shows that the increased Medicaid participation under the welcome mat represents a gain in supplemental coverage (or a decrease in having Medicare-only coverage). This is consistent with prior work that has found that the ACA Medicaid expansion did not crowd out private insurance among younger age groups (e.g., Frean et al., 2017 and Kaestner et al., 2017).
Table 4.
Effects on private coverage and Medicare-only coverage.
| Dependent Variable | |||
|---|---|---|---|
| Medicaid coverage | Private supplemental insurance coverage | Medicare coverage only | |
| (1) | (2) | (3) | |
| Expansion x Post | 0.018*** | −0.002 | −0.016*** |
| (0.006) | (0.005) | (0.005) | |
| Observations | 347,781 | 347,781 | 347,781 |
| , Pre, exp | 0.408 | 0.278 | 0.300 |
Notes: The sample consists of respondents to the 2010-17 ACS who are age 65 or older and income-eligible for Medicaid according to the criteria in their state of residence. In column (2), the dependent variable equals one if the respondent has private supplemental insurance coverage (and no Medicaid), and in column (3), the dependent variable equals one if the respondent has no supplemental insurance coverage of any type. The regressions include controls for black race, other race, Hispanic ethnicity, female, naturalized citizenship status, and education (high school diploma, some college, and college degree or more), age fixed effects, state fixed effects, and year fixed effects. Sample weights are used in model estimation. Standard errors clustered by state are reported in parentheses. Statistical significance is indicated by
for the .01 level,
for the .05 level and
for the .10 level.
D. Are Welcome Mat Effects Explained by an On-Ramp Effect?
We next examine whether a so-called “on-ramp to Medicaid” can explain increases in Medicaid participation among older adults. Before we formally model this, we first consider some suggestive evidence for an on-ramp effect.
For our hypothesized on-ramp effect to take place, it must be the case that adults in their early 60s living in expansion states experienced a bump in their Medicaid participation following the ACA’s Medicaid expansion. We examine this in Figure 3, which reports mean Medicaid participation rates among ACS respondents who were age 63 or 64 at the time of the survey and had income below their state’s 2015 cutoff for Medicaid through the SSI/209(b)/optional poverty eligibility pathways (shown in Appendix Table 1). Since the state cutoffs are at or below 100 percent FPG, all of these adults also have income below the cutoff for the ACA Medicaid expansions (138 percent FPG). We exclude respondents in states that expanded Medicaid in 2015 or later so that 2014 reflects the first year of the expansion for all observations. Figure 3 shows that between 2010 and 2013, mean Medicaid participation was approximately 30 percent in non-expansion states and roughly 37 percent in states that expanded Medicaid in 2014. In 2014, there was no change in mean Medicaid participation in the non-expansion states, but in expansion states, Medicaid participation among 63 and 64 year-olds increased by 10 percentage points to 47 percent. This suggests that the expansions increased participation by working-age adults approaching age 65, providing them with the firsthand experience with Medicaid that contributes to our hypothesized on-ramp effect.
Figure 3.
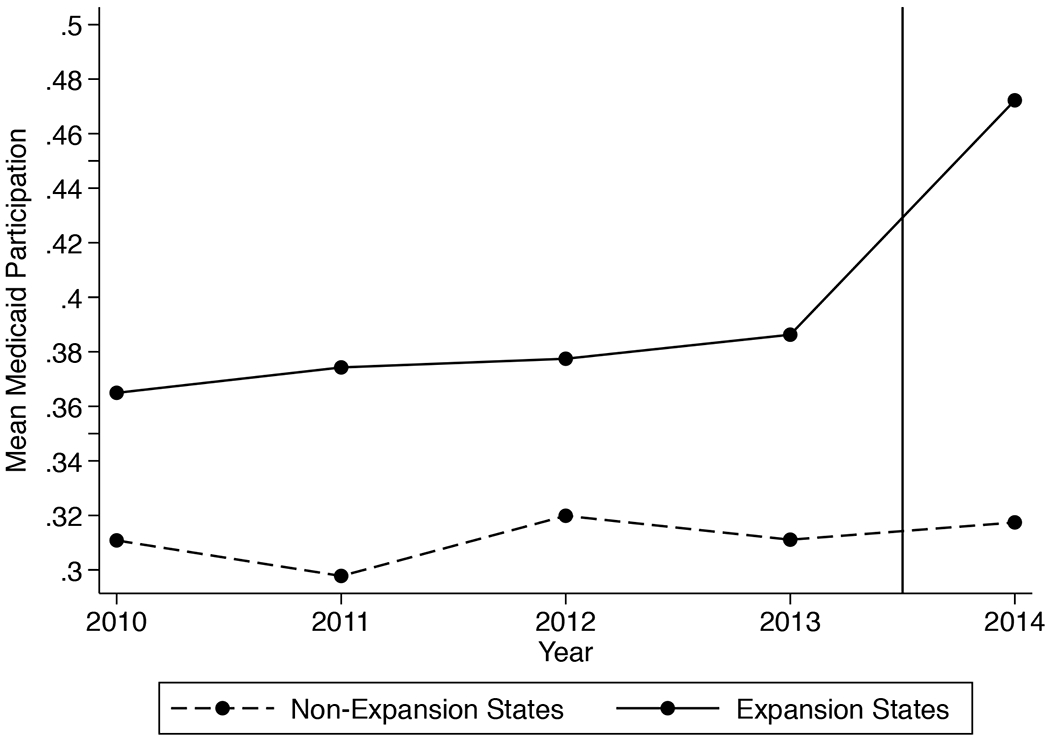
Trends in Medicaid Enrollment Among Low-Income Adults Age 63-64 by State of Residence (Excludes States that Expanded Medicaid in 2015, 2016, or 2017).
Notes: Sample weights are used in the calculation of means.
Other suggestive evidence for the on-ramp effect comes from evidence that welcome mat effects are present, if not stronger, for younger older adults. We examine this in Table 5. Column (1) reports the baseline DD estimate of the welcome mat effect for comparison. Columns (2) and (3) split the sample into ACS respondents aged 65 through 69, and those age 70 and older. Because all persons age 70 and older during our study period were at least age 65 in the years the Medicaid expansions took place, none of them were eligible for the ACA’s Medicaid expansions to working-age adults. We find that the welcome effect estimate is larger for 65 through 69 year-olds than it is for persons aged 70 and older. Further, as shown in column (4), the welcome effect estimate is somewhat larger for persons age 65, who in the years 2015 through 2017 were all young enough to have been eligible for expansion Medicaid coverage. Although the confidence intervals are such that we cannot rule out similarly-sized effects across these age groups, the relative sizes of the point estimates are consistent with the hypothesized on-ramp effect.
Table 5.
Welcome mat effect estimates, by age group.
Linear probability model (DV=Medicaid participation)
| Baseline | Age 65-69 | Age 70+ | Age 65 only | |
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Expansion x Post | 0.018*** | 0.024*** | 0.016** | 0.027** |
| (0.006) | (0.008) | (0.006) | (0.013) | |
| Observations | 347,781 | 93,194 | 254,587 | 22,292 |
| , Pre, exp | 0.408 | 0.425 | 0.402 | 0.420 |
Notes: The sample consists of respondents to the 2010-17 ACS who are income-eligible for Medicaid according to the criteria in their state of residence. The baseline sample consists of all persons age 65 and up. All models also include the controls reported in the baseline specification shown in Table 2, column 1. Columns (2)-(4) restrict to age groups listed. Sample weights are used in estimation. Standard errors clustered by state are reported in parentheses. Statistical significance is indicated by
for the .01 level,
for the .05 level and
for the .10 level.
Additionally, we examine Medicaid participation rates over time for the treated age group (65 year-olds) separately in expansion and non-expansion states, and we do the same for the comparison age group (68 and 69 year-olds). As shown in Figure 4, we find that in most years, Medicaid participation rates are higher in expansion states than non-expansion states for both age groups, and prior to 2014, Medicaid participation is higher among 68 and 69 year-olds than among 65 year-olds across both sets of states. In 2014, 65 year-olds in both sets of states are more likely to be enrolled in Medicaid than 68 and 69 year-olds, but by 2015, the 65 year-olds are more likely than the older group to be enrolled in Medicaid in expansion states and continue to be so over time, whereas the opposite trend occurs in non-expansion states.
Figure 4.
Mean Medicaid Participation by Year, Expansion State Residence, and Age Among Low-Income Adults Ages 65, 68, and 69, Excluding States that Expanded Medicaid in 2015, 2016, or 2017.
Notes: Sample weights are used in the calculation of means. The sample consists of respondents to the 2010-17 ACS who are age 65, 68, or 69 and income-eligible for Medicaid according to the criteria in their state of residence. Residents of states that expanded Medicaid in 2015, 2016, or 2017 are excluded.
To formally test for an on-ramp effect, we estimate equation (2) to test whether increases in Medicaid participation over time in expansion states relative to non-expansion states are larger for respondents who were age 65 at the time of the survey (and thus were age-eligible for ACA Medicaid expansions in 2014) than those just over age 65. Table 6 reports the results. Column (1) reports results from our main specification, which uses persons ages 68 and 69 at the time of the survey as the comparison group for the 65 year-olds. The DDD estimate is marginally significant (p=0.054) and suggests there is a four percentage point (or 9.5 percent) increase in Medicaid participation for those expansion state residents who were young enough to participate in the ACA Medicaid expansions as working-age adults. Column (2) shows that the DDD estimate is somewhat smaller when we expand the comparison group to include older respondents (age 68 through 79 at the survey), at a statistically significant 3.3 percentage points (or 7.8 percent).
Table 6.
On-ramp effect estimates, 2010-17 ACS, adults ages 65+.
Linear probability model (DV=Medicaid participation)
| Comparison group age 68-69 in year of survey | Comparison group age 68-79 in year of survey | |
|---|---|---|
| (1) | (2) | |
| Age 65 in Year of Survey x Expansion x Post 2015 | 0.040* | 0.033** |
| (0.020) | (0.013) | |
| Implied effect size (Pre pd. Mean for 65 year olds=0.422) | 9.5% | 7.8% |
| N | 51,314 | 179,392 |
Notes: The sample consists of respondents to the 2010-17 ACS who are income-eligible for Medicaid according to the criteria in their state of residence and do not reside in a state that expanded Medicaid in 2015, 2016, or 2017. In column (1), the sample is restricted to adults ages 65, 68, and 69. In column (2), the sample is restricted to adults ages 65, 68-79. Models include interaction terms representing Post 2015 x Age 65, Expansion x Age 65, and Post 2015 x Expansion, plus controls for black race, other race, Hispanic ethnicity, female, naturalized citizenship status, and education (high school diploma, some college, and college degree or more), age fixed effects, state fixed effects, and year fixed effects. Standard errors clustered by state are reported in parentheses. Sample weights are used. Statistical significance is indicated by
for the .01 level,
for the .05 level and
for the .10 level.
Table 7 shows that the DDD estimate from our main specification is robust to the same types of specification changes we used to test our DD estimate of the welcome mat effect. For ease of comparison, column (1) reports the main DDD results. In specifications that either limit the controls to state and year fixed effects, or add the controls included in our main specification as well as controls for respondent disabilities, asset ownership, SSI receipt, and other traits, the DDD estimate ranges from 3.6 to 4.2 percentage points and remains statistically significant at either the five percent or 10 percent level. We also report the coefficient estimates on the three cross-product terms in Table 7. The coefficient estimate for the interaction of Post 2015 and Expansion is not statistically significant, though as discussed earlier, this is not directly comparable to the estimates of the overall welcome mat effect. All but one specification shows that permanent differences in Medicaid participation among 65 year-olds in expansion states relative to non-expansion states are not statistically significant, and there is no evidence of a secular change in Medicaid participation for 65 year-olds across all states timed with the ACA’s Medicaid expansion.
Table 7.
On-ramp effect estimates, baseline DDD specification with alternate controls.
Linear probability model (DV=Medicaid participation)
| Baseline specification | State and year fixed effects only | Baseline + disability | Baseline + own home | Baseline + any non-housing assets | Baseline + SSI receipt | Baseline + other potentially endogenous variables | Baseline + all | |
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| Age 65 x Post 2015 x Expansion | 0.040* | 0.042** | 0.041** | 0.036* | 0.040** | 0.041** | 0.039* | 0.039** |
| (0.020) | (0.020) | (0.019) | (0.019) | (0.019) | (0.018) | (0.021) | (0.017) | |
| Post 2015 x Expansion | 0.002 | 0.004 | 0.001 | 0.006 | 0.001 | 0.008 | 0.005 | 0.003 |
| (0.014) | (0.014) | (0.013) | (0.013) | (0.013) | (0.013) | (0.014) | (0.012) | |
| Expansion x Age 65 | 0.007 | 0.010 | 0.008 | 0.010 | 0.007 | 0.015 | 0.011 | 0.018* |
| (0.014) | (0.015) | (0.013) | (0.013) | (0.013) | (0.010) | (0.013) | (0.009) | |
| Post 2015 x Age 65 | −0.008 | −0.004 | −0.010 | −0.002 | −0.007 | −0.012 | −0.011 | −0.010 |
| (0.016) | (0.015) | (0.016) | (0.015) | (0.014) | (0.014) | (0.017) | (0.013) | |
| Ambulatory diff. | 0.135*** | 0.057*** | ||||||
| (0.009) | (0.008) | |||||||
| Cognitive diff. | 0.128*** | 0.057*** | ||||||
| (0.011) | (0.007) | |||||||
| Ind. living diff. | 0.098*** | 0.038*** | ||||||
| (0.011) | (0.010) | |||||||
| Self-care diff. | 0.041*** | 0.033*** | ||||||
| (0.009) | (0.009) | |||||||
| Vision diff. | 0.037*** | 0.010 | ||||||
| (0.011) | (0.011) | |||||||
| Hearing diff. | −0.003 | −0.008 | ||||||
| (0.008) | (0.009) | |||||||
| Own home | −0.231*** | −0.133*** | ||||||
| (0.012) | (0.009) | |||||||
| Any non-housing assets | −0.182*** | −0.089*** | ||||||
| (0.011) | (0.008) | |||||||
| Receives SSI | 0.597*** | 0.504*** | ||||||
| (0.023) | (0.026) | |||||||
| Employed | −0.137*** | −0.032*** | ||||||
| (0.008) | (0.009) | |||||||
| Married | −0.217*** | −0.114*** | ||||||
| (0.012) | (0.014) | |||||||
| Widowed | −0.117*** | −0.068*** | ||||||
| (0.015) | (0.012) | |||||||
| Separated/Divorced | −0.023** | −0.009 | ||||||
| (0.011) | (0.008) | |||||||
| Income ($10K, 2017) | −0.000*** | −0.000 | ||||||
| (0.000) | (0.000) | |||||||
| State unemp. rate | 0.001 | −0.005 | ||||||
| (0.004) | (0.004) | |||||||
| Share of state Medicare enrollees in Med. Adv. | 0.085 | −0.081 | ||||||
| (0.143) | (0.111) | |||||||
| Observations | 51,314 | 51,314 | 51,314 | 51,314 | 51,314 | 51,314 | 51,314 | 51,314 |
| DV mean | 0.422 | 0.422 | 0.422 | 0.422 | 0.422 | 0.422 | 0.422 | 0.422 |
Notes: The sample consists of respondents to the 2010-17 ACS who are age 65, 68, or 69, are income-eligible for Medicaid according to the criteria in their state of residence, and do not reside in a state that expanded Medicaid in 2015, 2016, or 2017. The baseline specification includes controls for black race, other race, Hispanic ethnicity, female, naturalized citizenship status, and education (high school diploma, some college, and college degree or more), age fixed effects, state fixed effects, and year fixed effects. Sample weights are used in model estimation. Standard errors clustered by state are reported in parentheses. Statistical significance is indicated by
for the .01 level,
for the .05 level and
for the .10 level.
In Table 8, we report the sensitivity of the on-ramp effect to weighting or sample construction; in general, the coefficient estimates are robust. The DDD coefficient estimate is smallest in size and fails to achieve statistical significance in the unweighted results presented in column (1). The DDD estimate is largest (7.3 percentage points, or a 25 percent increase) when only the expansion states with the lowest pre-period rate of Medicaid participation are included in the treatment group.21
Table 8.
On-ramp effect estimates, robustness checks.
Linear probability model (DV=Medicaid participation)
| Unweighted | Drop SSI recipients | Drop respondents with any assets | All ACS respondents with income <= 100% FPG | All ACS respondents with income <= 150% FPG | |
|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | |
| Age 65 x Post 2015 x Expansion | 0.013 | 0.054** | 0.047** | 0.034 | 0.042*** |
| (0.019) | (0.021) | (0.020) | (0.023) | (0.014) | |
| , Pre, exp. | 0.417 | 0.319 | 0.441 | 0.438 | 0.372 |
| Implied effect size | 3.1% | 16.9% | 10.7% | 7.8% | 11.3% |
| N | 51,314 | 43,900 | 46,818 | 66,662 | 128,164 |
| Drop states that had coverage for childless adults in the pre period | Drop early expansion states | Drop states with mid-year expansions | Keep treatment states with lowest pre-period dual enrollment | ||
| (6) | (7) | (8) | (9) | ||
| Age 65 x Post 2015 x Expansion | 0.028 | 0.053** | 0.040* | 0.073** | |
| (0.018) | (0.024) | (0.021) | (0.034) | ||
| , Pre, exp. | 0.411 | 0.425 | 0.432 | 0.290 | |
| Implied effect size | 6.8% | 12.5% | 9.3% | 25.2% | |
| N | 46,038 | 38,015 | 48,122 | 23,994 | |
Notes: All samples consist of respondents to the 2010-17 ACS who are age 65 or age 68-69 and residing in states other than those that had Medicaid expansions in 2015-2017 (i.e., other than Pennsylvania, Indiana, Alaska, Montana, and Louisiana). In columns (4) and (5), the samples are defined from all ACS respondents who reside in the community and meet the income restrictions shown. The samples in columns (1)-(3) and (6)-(9) are defined from the baseline sample, which further restricts the sample to include only those who are income-eligible for Medicaid according to the criteria in their state of residence. Column (6) excludes respondents in the District of Columbia, Delaware, Massachusetts, New York, and Vermont because these states had coverage for childless adults prior to 2014 (as in Miller and Wherry, 2017 and Ghosh et al., 2019). Column (7) excludes respondents in California, Connecticut, the District of Columbia, Massachusetts, Minnesota, New Jersey, and Washington (as in Frean et al., 2017). Column (8) excludes respondents in Michigan, New Hampshire, Indiana, Louisiana, and Alaska. In column (9), the treatment group is comprised of residents of Alaska, Colorado, Connecticut, Delaware, Iowa, Montana, New Hampshire, North Dakota, and Ohio. All models also include the controls reported in the baseline specification shown in Table 7, column 1. Sample weights are used (except in column 1). Standard errors clustered by state are reported in parentheses. Statistical significance is indicated by
for the .01 level,
for the .05 level and
for the .10 level.
As we did for the welcome mat analysis, we conducted three additional checks on our DDD on-ramp effect estimates. The results of the leave-one-out exercise are reported in Appendix Figure 1B. In most cases, the DDD estimate is similar in size to our baseline DDD estimate, and in every case the DDD estimate falls within the 95 percent confidence interval of our baseline estimate. From the 27 iterations, seven estimates are statistically significant at the five percent level and 18 estimates are significant at the ten percent level. We fail to achieve statistical significance at the 10 percent level when we omit either of the two largest states (CA or NY).22 The results of the placebo analysis are shown in Appendix Figure 2B. In seven iterations, the absolute value of the placebo DDD estimate is greater than the on-ramp effect estimate from our baseline specification. Thus, the p-value from randomization inference is 0.07. Lastly, we similarly estimated equation (2) using the state-specific de-trended outcome. The DDD estimate from this exercise is 0.046 and is statistically significant (p-value<0.05). Taken as a whole, these results are generally supportive of our DDD estimates of the on-ramp effect.23
5. DISCUSSION
We examine whether the expansion of Medicaid to working-age adults increased Medicaid participation by older low-income Medicare enrollees. Our results provide evidence of a welcome mat effect; namely, older low-income Medicare beneficiaries residing in states that expanded Medicaid under the ACA were 1.8 percentage points more likely to enroll in Medicaid after the expansion. We also find evidence that the welcome mat effect is due in part to an on-ramp effect whereby older adults who were young enough to benefit from ACA Medicaid expansions were more likely to be dually enrolled in both Medicare and Medicaid when they were 65 years old than similar individuals who turned 65 before the 2014 expansions or resided in non-expansion states. The potential for welcome mat effects among low-income seniors has been overlooked in previous literature, including studies that use adults over age 65 as a control group or falsification test when estimating the impact of the ACA on working-age adults (Simon, Soni, & Cawley, 2017; Khantana, Bhatla, & Nathan, 2019; Hu et al., 2018).
Our estimate of the welcome mat effect among older adults is similar to estimated welcome mat effects among already-eligible children and working-aged adults. Welcome mat effects for other populations following the ACA Medicaid expansions range from 2.6 to 4.6 percentage points (Hudson & Moriya, 2017; Sommers, Kenney, & Epstein, 2014; Sommers et al., 2016; and Frean, Gruber, & Sommers 2017). This similarity is notable given that older adults without Medicaid are not uninsured—they have Medicare insurance—and they are not impacted by the individual mandate or by intra-family spillover benefits.
Some limitations of the ACS data are worth noting. Although we apply state-specific income eligibility criteria, we are unable to compare asset levels of ACS respondents to state asset limits. To partly address this, we identify whether respondents have asset-related income from investments or businesses. We find that 90.5 percent of low-income older Medicare enrollees report no income in these categories, and that our results are robust to checks that exclude respondents who have these types of asset-related income.
Additionally, in restricting our sample to respondents eligible for Medicaid, we focus on the SSI/209(b)/poverty pathways and do not capture eligibility through optional Medically Needy programs or HCBS waivers. This largely reflects data limitations. The ACS does not contain the information on medical expenses needed to impute medically needy eligibility. Rules regarding functional eligibility criteria for HCBS pathways are determined by individual states and are not readily available, and ACS data may be inadequate for measuring functional eligibility even if all states’ criteria were available. That said, our study improves upon previous studies of Medicaid participation by older adults that use uniform thresholds, such as having income at or below 100 percent FPG, to define the analytic sample (Pezzin & Kasper, 2002; Ungaro & Federman, 2009; Mclnerney, Mellor, & Sabik, 2017). The three pathways that we identify represent 70 percent of full Medicaid participants among older adults 65 and up (MedPAC and MacPAC, 2018). An additional limitation is that we define Medicaid coverage using self-reports from ACS respondents, which are subject to misreporting (see, e.g., Boudreaux et al., 2015; Mellor, McInerney, & Sabik, 2019).
A novel contribution of our work is that we identify a new mechanism that contributes to the welcome mat effect among older adults—the on-ramp to Medicaid, whereby individuals who were exposed to Medicaid expansions before they turned 65 are more likely to be dually enrolled in Medicare and Medicaid by age 65 than similar individuals who either turned 65 before the 2014 expansions or resided in non-expansion states. To the best of our knowledge, this type of effect has not been documented elsewhere. By definition, the on-ramp effect contributes to welcome mat effects for younger seniors – those who were in their early 60s during the time of the ACA’s Medicaid expansions. Other results suggest that the on-ramp effect is not the only mechanism behind welcome mat effects for seniors as a whole. In particular, our age subgroup analysis shows evidence of sizeable welcome mat effects in the population age 70 and up, none of whom would have qualified for expanded Medicaid for working-age adults under the ACA in our time period (Table 5). Likewise, the 95 percent confidence interval of our coefficient estimate of the interaction of Post 2015 and Expansion includes large positive values (Table 7).
For this reason, future work that examines other potential mechanisms behind the welcome mat effect would be worthwhile. While beyond the scope of our current analysis, we expect that having household members, family members, or other close social ties exposed to ACA Medicaid expansions could influence seniors’ participation in Medicaid. Further, providers may play a role in facilitating Medicaid coverage for eligible low-income seniors, and ACA Medicaid expansions may have increased their awareness of or ability to assist with Medicaid enrollment for duals. Understanding these mechanisms will inform policymakers regarding strategies to effectively increase Medicaid participation among older Medicare enrollees. Another direction for future work is to study the on-ramp effect using longitudinal data, which will enable policymakers to identify which individuals are most likely to continue to enroll in Medicaid after turning 65.
Finally, the welcome mat effects identified in this analysis may yield important protective effects for the older adults now dually enrolled in Medicare, in the form of improved healthcare access, health outcomes, and financial well-being. For example, older adults dually enrolled in Medicare and Medicaid spend a smaller share of their income on out-of-pocket medical costs than older adults with retiree health insurance, Medigap coverage, or no supplemental insurance (McInerney, Rutledge, & King, 2017; Neuman et al., 2007). A more complete accounting of the benefits of Medicaid participation for low-income older adults does not yet exist, suggesting that this is an important area for future research.
Acknowledgments
This research was supported by R01 HS025422 from the Agency for Healthcare Research and Quality (AHRQ). We are grateful for excellent research assistance from Noelle Cornelio, Miranda McKelvey Chavez, Grace McCormack, Venkatesh Ramamoorthy, and Vivian Kim. We thank Eric Roberts and participants at the joint Harvard/BU/MIT health economics seminar, the Tufts University brown bag, the 2016 American Society for Health Economists meeting, the 2016 Association for Public Policy Analysis and Management annual conference, and the 2016 National Tax Association meeting for helpful comments.
Appendix Figure 1A.
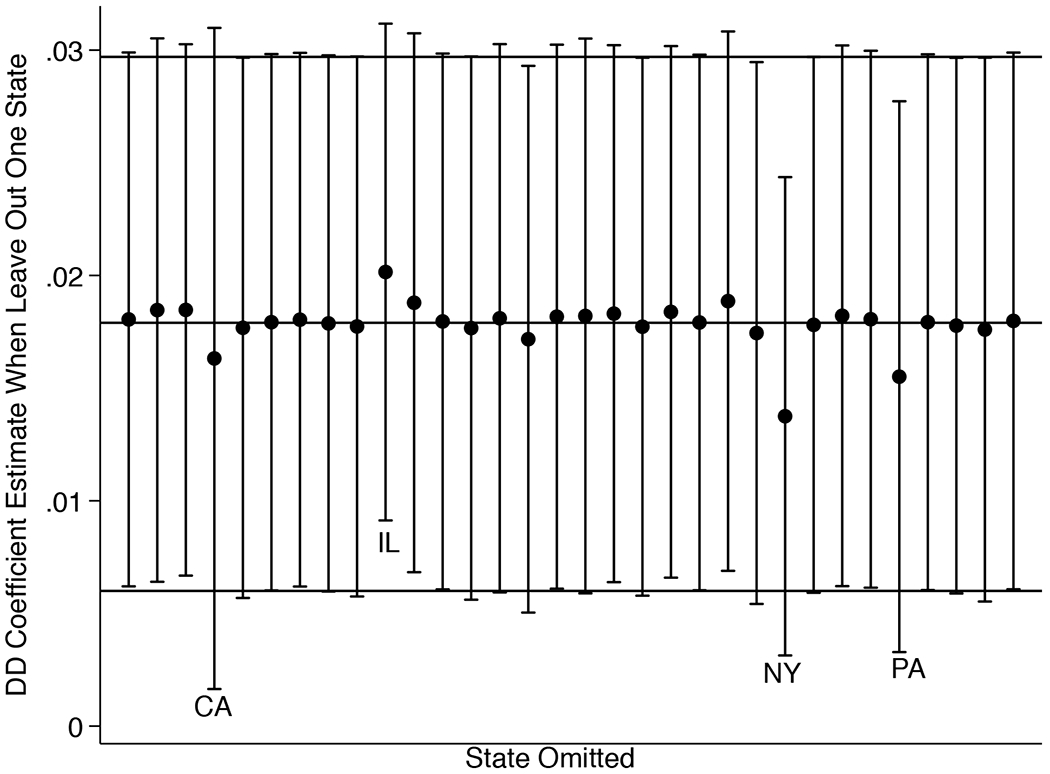
DD Coefficient Estimates, Leaving Out One State.
Appendix Figure 1B.
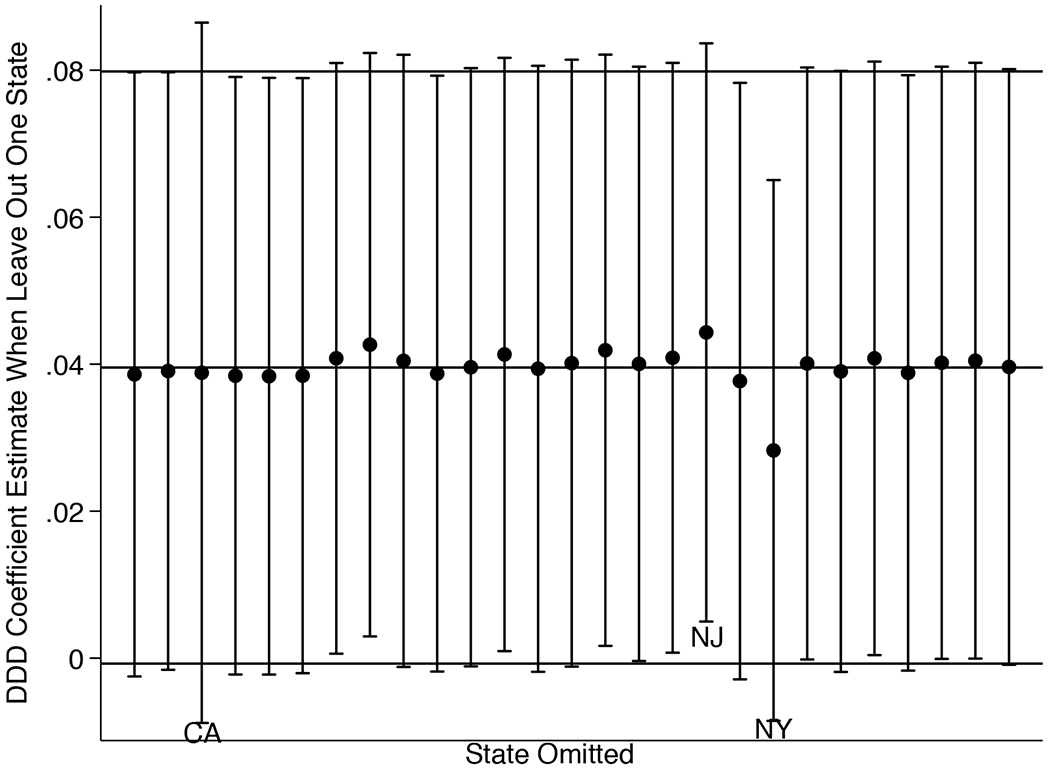
DDD Coefficient Estimates, Leaving Out One State.
Notes: The figures report the coefficient estimate and 95% confidence interval when we singly leave out each treatment state. In Figure 1A, we singly leave out each of the 32 states that expanded Medicaid between 2014 and 2017. The horizontal line at 0.018 represents our baseline DD estimate, and the horizontal lines at 0.006 and 0.0297 represent the 95% confidence interval around our baseline DD estimate. In Figure 1B, we singly leave out each of the 27 states that expanded Medicaid in the year 2014. The horizontal line at 0.040 represents our baseline DDD estimate, and the horizontal lines at −0.001 and 0.080 represent the 95% confidence interval.
Appendix Figure 2A.
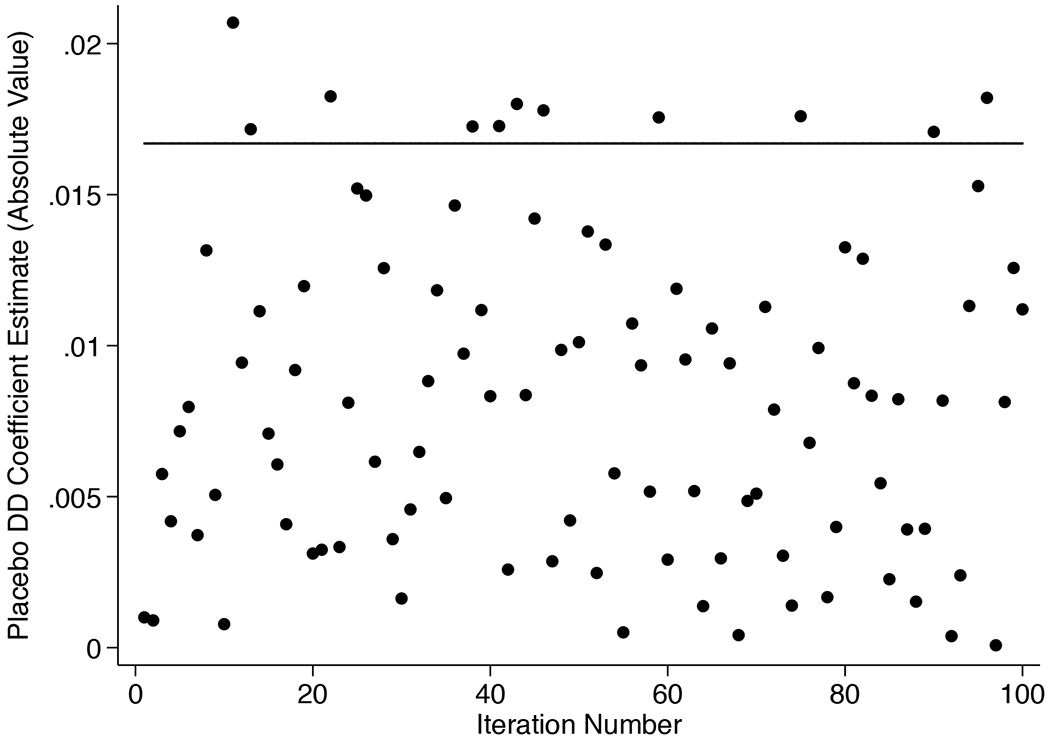
DD Placebo Analysis Results.
Appendix Figure 2B.
DDD Placebo Analysis Results.
Notes: The sample used to construct these estimates excludes states that adopted the ACA Medicaid expansions in 2015-17. Each point in these figures is the absolute value of a placebo estimate where we randomly select 27 states to be the treatment states (to reflect the 27 states that expanded Medicaid in 2014) and estimate the placebo coefficient on placebo treat x post 2014 (for Figure 2A) and placebo treat xpost 2015 x age 65 (for Figure 2B). We estimate 100 placebo regressions and the p-value from randomization inference is the fraction of times for which the absolute value of the placebo estimate exceeds the baseline estimate. In each figure, the horizontal line reflects the baseline estimate of 0.017 for the DD results (for the sample that excludes residents of states that adopted Medicaid in 2015-2017) and 0.040 for the DDD results. For the DD results, the p-value is 0.11, and for the DDD results, the p-value is 0.07.
Appendix Table 1.
State Medicaid eligibility limits for duals through SSI/209(b)/poverty pathways (% FPG).
| State | Single | Couple | State | Single | Couple |
|---|---|---|---|---|---|
| Alabama | 75% | 83% | Missouria | 87% | 87% |
| Alaska | 75% | 83% | Montana | 75% | 83% |
| Arizona | 100% | 100% | Nebraska | 100% | 100% |
| Arkansas | 80% | 80% | Nevada | 75% | 83% |
| California | 100% | 100% | New Hampshire3 | 76% | 83% |
| Colorado | 75% | 83% | New Jersey | 100% | 100% |
| Connecticuta,b | 53% | 52% | New Mexico | 75% | 83% |
| Delaware | 75% | 83% | New York | 84% | 91% |
| DC | 100% | 100% | North Carolina | 100% | 100% |
| Florida | 88% | 88% | North Dakotaa | 75% | 83% |
| Georgia | 75% | 83% | Ohioa | 66% | 83% |
| Hawaiia | 100% | 100% | Oklahomaa | 92% | 91% |
| Idaho | 78% | 83% | Oregon | 75% | 83% |
| Illinoisa | 100% | 100% | Pennsylvania | 100% | 100% |
| Indianaa | 100% | 100% | Rhode Island | 100% | 100% |
| Iowa | 75% | 83% | South Carolina | 100% | 100% |
| Kansas | 75% | 83% | South Dakota | 75% | 83% |
| Kentucky | 75% | 83% | Tennessee | 75% | 83% |
| Louisiana | 75% | 83% | Texas | 75% | 83% |
| Maine | 100% | 100% | Utah | 100% | 100% |
| Maryland | 75% | 83% | Vermont | 75% | 83% |
| Massachusetts | 100% | 100% | Virginiaa | 80% | 80% |
| Michigan | 100% | 100% | Washington | 75% | 83% |
| Minnesotaa | 100% | 100% | West Virginia | 75% | 83% |
| Mississippi | 75% | 83% | Wisconsin | 83% | 93% |
| Wyoming | 75% | 83% |
These eleven states are 209(b) states that may have more restrictive criteria than SSI.
Connecticut has different eligibility thresholds for the counties near New York City and the remainder of the state. The counties near New York City have higher eligibility thresholds. In this table, we present the more conservative thresholds used in the rest of the state.
Source: Watts, M.O., E. Cornachione, and M. Musumeci. 2016. “Medicaid Financial Eligibility for Older adults and People with Disabilities in 2015.” Kaiser Family Foundation. Appendix Table 2.
We computed the % FPG for singles and couples from the reported monthly income limit and the 2015 federal poverty guidelines. In 2015, the poverty guidelines correspond to $981 per month for a household of one and $1,328 per month for two-person households in the contiguous states and DC (Available at: https://aspe.hhs.gov/2015-poverty-guidelines; viewed March 15, 2018). In Alaska, Medicaid eligibility is governed by SSA guidelines for SSI eligibility, so 75% FPG corresponds to the poverty guidelines in the contiguous states. In Hawaii, a 209(b) state, the % FPG is computed based on the higher Hawaii poverty guidelines.
Appendix Table 2.
Expansion and non-expansion states through 2017.
| Expansion States | Expansion Date | Non-Expansion States |
|---|---|---|
| Alaska | 9/2015 | Alabama |
| Arizona | 1/2014 | Florida |
| Arkansas | 1/2014 | Georgia |
| California | 1/2014 | Idaho |
| Colorado | 1/2014 | Kansas |
| Connecticut | 1/2014 | Maine |
| Delaware | 1/2014 | Mississippi |
| District of Columbia | 1/2014 | Missouri |
| Hawaii | 1/2014 | Nebraska |
| Illinois | 1/2014 | North Carolina |
| Indiana | 2/2015 | Oklahoma |
| Iowa | 1/2014 | South Carolina |
| Kentucky | 1/2014 | South Dakota |
| Louisiana | 7/2016 | Tennessee |
| Maryland | 1/2014 | Texas |
| Massachusetts | 1/2014 | Utah |
| Michigan | 4/2014 | Virginia |
| Minnesota | 1/2014 | Wisconsin |
| Montana | 1/2016 | Wyoming |
| Nevada | 1/2014 | |
| New Hampshire | 8/2014 | |
| New Jersey | 1/2014 | |
| New Mexico | 1/2014 | |
| New York | 1/2014 | |
| North Dakota | 1/2014 | |
| Ohio | 1/2014 | |
| Oregon | 1/2014 | |
| Pennsylvania | 1/2015 | |
| Rhode Island | 1/2014 | |
| Vermont | 1/2014 | |
| Washington | 1/2014 | |
| West Virginia | 1/2014 |
Source: Kaiser Family Foundation. 2018. “Status of State Action on the Medicaid Expansion.” Available at: https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D; viewed March 9, 2018.
Appendix Table 3.
Coefficient estimates of explanatory variables in linear probability models of Medicaid participation.
| Welcome Mat Effect | On-Ramp Effect | ||
|---|---|---|---|
| Expansion x Post | 0.018*** | Age 65 x Post 2015 x Expansion | 0.040* |
| (0.006) | (0.020) | ||
| Expansion x Post 2015 | 0.002 | ||
| (0.014) | |||
| Expansion x Age 65 | 0.007 | ||
| (0.014) | |||
| Post 2015 x Age 65 | −0.008 | ||
| (0.016) | |||
| Female | 0.034*** | Female | 0.043*** |
| (0.003) | (0.006) | ||
| Black | 0.146*** | Black | 0.123*** |
| (0.007) | (0.010) | ||
| Hispanic | 0.126*** | Hispanic | 0.092** |
| (0.039) | (0.040) | ||
| Other race | 0.114*** | Other race | 0.076*** |
| (0.014) | (0.018) | ||
| Naturalized citizen | 0.143*** | Naturalized citizen | 0.046** |
| (0.014) | (0.018) | ||
| High school | −0.138*** | High school | −0.155*** |
| (0.005) | (0.011) | ||
| Some college | −0.147*** | Some college | −0.174*** |
| (0.006) | (0.011) | ||
| College or more | −0.171*** | College or more | −0.253*** |
| (0.011) | (0.011) | ||
| Observations | 347,781 | Observations | 51,314 |
Notes: Each regression also includes age fixed effects, state fixed effects, and year fixed effects. Standard errors clustered by state are in parentheses. Sample weights are used. Statistical significance is indicated by
for the .01 level,
for the .05 level and
for the .10 level.
Appendix Table 4.
Descriptive statistics for alternative on-ramp comparison cohorts.
| Age at time of survey: | 65 | 68-69 | 68-79 | 68-89 | 68-99 |
|---|---|---|---|---|---|
| Medicaid | 0.42 | 0.44* | 0.43 | 0.42 | 0.42 |
| Female | 0.62 | 0.64** | 0.67*** | 0.69*** | 0.70*** |
| White | 0.54 | 0.52* | 0.52*** | 0.55 | 0.55 |
| Black | 0.15 | 0.14 | 0.13*** | 0.12*** | 0.12*** |
| Hispanic | 0.17 | 0.18 | 0.17 | 0.16* | 0.16** |
| Other race | 0.13 | 0.16*** | 0.17*** | 0.17*** | 0.17*** |
| Naturalized citizen | 0.25 | 0.30*** | 0.34*** | 0.33*** | 0.33*** |
| Employed | 0.07 | 0.04*** | 0.02*** | 0.02*** | 0.02*** |
| Married | 0.30 | 0.31 | 0.31 | 0.28*** | 0.26*** |
| Widowed | 0.19 | 0.23*** | 0.32*** | 0.41*** | 0.44*** |
| Separated or divorced | 0.35 | 0.34* | 0.26*** | 0.22*** | 0.21*** |
| Never married | 0.16 | 0.13*** | 0.11*** | 0.09*** | 0.09*** |
| Less than high school | 0.30 | 0.34*** | 0.38*** | 0.39*** | 0.39*** |
| High school degree | 0.31 | 0.31 | 0.31 | 0.32 | 0.32 |
| Some college | 0.24 | 0.22*** | 0.18*** | 0.17*** | 0.16*** |
| College or more | 0.15 | 0.13** | 0.13*** | 0.12*** | 0.12*** |
| Income ($10,000, 2017) | 2.85 | 3.04* | 3.42*** | 3.51*** | 3.53*** |
| Income as % FPG | 53.3 | 59.7*** | 59.5*** | 59.4*** | 59.3*** |
| Single elig. (% FPG) | 91.8 | 92.5*** | 92.7** | 92.7** | 92.7*** |
| Couple elig. (% FPG) | 94.6 | 95.1*** | 95.2*** | 95.2*** | 95.2*** |
| Cognitive difficulty | 0.11 | 0.12 | 0.13*** | 0.16*** | 0.18*** |
| Ambulatory difficulty | 0.26 | 0.27 | 0.30*** | 0.35*** | 0.37*** |
| Independent living difficulty | 0.16 | 0.17* | 0.21*** | 0.28*** | 0.31*** |
| Self-care difficulty | 0.09 | 0.10 | 0.12*** | 0.15*** | 0.17*** |
| Vision difficulty | 0.08 | 0.07 | 0.09** | 0.11*** | 0.12*** |
| Hearing difficulty | 0.08 | 0.09** | 0.13*** | 0.17*** | 0.19*** |
| Has any non-housing assets | 0.08 | 0.07* | 0.07** | 0.08 | 0.08 |
| Receive SSI | 0.16 | 0.18** | 0.18*** | 0.18*** | 0.18*** |
| Share in Med. Adv. | 0.29 | 0.29 | 0.29 | 0.29 | 0.29 |
| N | 6,697 | 10,032 | 53,866 | 84,316 | 91,275 |
Notes: The samples consist of respondents to the 2010-14 ACS who are age 65 or older, are income-eligible for Medicaid according to the criteria in their state of residence, and reside in a state that expanded Medicaid in 2014. Statistically significant differences between 65 year-olds and each of the potential comparison cohorts are indicated by
for the .01 level,
for the .05 level, and
for the .01 level.
Appendix Table 5.
Effects on Medicaid coverage and Medicare coverage.
(Sample includes non-Medicare enrollees)
| Baseline: Sample restricted to Medicare enrollees | Sample expanded to include non-Medicare enrollees | |
|---|---|---|
| (1) | (2) | |
| Panel A: DD Estimates | ||
| Expansion x Post | 0.018*** | 0.019*** |
| (0.006) | (0.006) | |
| Observations | 347,781 | 362,127 |
| , Pre, exp | 0.408 | 0.391 |
| Panel B: DDD Estimates | ||
| Age 65 x Post 2015 x Expansion | 0.040* | 0.045** |
| (0.020) | (0.020) | |
| Expansion x Post 2015 | 0.002 | 0.004 |
| (0.014) | (0.013) | |
| Expansion x Age 65 | 0.007 | 0.001 |
| (0.014) | (0.014) | |
| Post 2015 x Age 65 | −0.008 | −0.007 |
| (0.016) | (0.016) | |
| Observations | 51,314 | 54,559 |
| , Pre, exp | 0.422 | 0.404 |
Notes: The sample consists of respondents to the 2010-17 ACS who are age 65 or older and income-eligible for Medicaid according to the criteria in their state of residence. In column (1), the sample is restricted to respondents who are enrolled in Medicare. In column (2), the sample includes respondents who are not enrolled in Medicare. The regressions include controls for black race, other race, Hispanic ethnicity, female, naturalized citizenship status, and education (high school diploma, some college, and college degree or more), age fixed effects, state fixed effects, and year fixed effects. Sample weights are used in model estimation. Standard errors clustered by state are reported in parentheses. Statistical significance is indicated by
for the .01 level,
for the .05 level and
for the .10 level.
Footnotes
Persons age 65 and older who do not qualify for full Medicaid through their state plan’s mandatory/optional eligibility pathways may be able to obtain assistance with Medicare cost-sharing through Medicare Savings Programs (MSPs) such as the Qualified Medicare Beneficiary (QMB) Program, the Specified Low-Income Medicare Beneficiary (SLMB) Program, and the Qualifying Individual (QI) Program, depending on their incomes and other resources. Persons enrolled in these MSPs are said to have partial Medicaid coverage, since MSPs cover some mix of Medicare premiums and cost-sharing, but do not provide additional benefits. Partial Medicaid coverage is not the focus of our analysis.
Persons age 65 and older who are income-eligible for Supplemental Security Income (SSI) are automatically enrolled in Medicaid in the 35 “1634 states.” That is, the applicant completes one application with the Social Security Administration for Medicaid and SSI. Applicants who are income eligible for full Medicaid in a 1634 state but have income too high to qualify for SSI benefits must file a separate application to the state Medicaid or human services office. In the remaining states, those who are income-eligible for SSI submit a separate application to the state Medicaid or human services office (SSA POMS SI 01730.005, n.d.).
Although the Social Security Administration sends letters to Social Security recipients who appear to be income-eligible but do not participate in Medicare Savings Programs (partial Medicaid) or the low-income subsidy for Part D, we know of no outreach for individuals who are eligible but not enrolled in full Medicaid.
Other mechanisms through which the welcome mat effect may operate (e.g., increased program awareness or increased assistance with enrollment) could impact all previously-eligible groups (including low-income older adults) in similar ways.
This rate is calculated from waves 8 through 12 of the HRS data. We first selected respondents who were enrolled in Medicaid at ages 63 and 64 and then computed the fraction who were enrolled in Medicaid in the subsequent wave when the respondent was age 65 or 66.
This continuity in coverage may reflect outreach from state Medicaid offices. Centers for Medicare and Medicaid Services (CMS) training materials suggest that as Medicaid enrollees approach age 65, their continued eligibility for Medicaid is reevaluated, and this may include outreach to the insured under age 65 (CMS, 2018).
We exclude Medicare beneficiaries under age 65 who qualify due to disability and represent about 17 percent of all Medicare beneficiaries (KFF, 2017) because patterns of Medicaid enrollment appear very different for this group (Cubanski, Neuman, & Damico, 2016). For example, about 14 percent of Medicare beneficiaries age 65 and up are enrolled in Medicaid, while 49 percent of Medicare beneficiaries under age 65 are enrolled in Medicaid (MedPAC and MACPAC, 2018).
The ACS does not capture asset balances. In a robustness check, we exclude respondents who appear to hold assets because they report receipt of income from a business or farm or interest, dividend, or rental income. With the Health and Retirement Study, which has detailed information on income sources and asset holdings of older adults, we examined what share of adults meeting the income criteria also meet the asset criteria. Using eligibility for SSI, which describes Medicaid eligibility in 23 states in the year 2015 and is uniform across the U.S., we confirmed that among older adults who meet the income criteria for SSI, 75 to 80 percent also meet the SSI asset criteria.
In 209(b) states, individuals can become eligible for Medicaid if their income falls below the 209(b) threshold or if their income after a “spend down” (i.e., income with medical expenses deducted) falls under the 209(b) limit. Since we do not observe medical expenses in the ACS data, we can only identify those residents of 209(b) states who are income-eligible, not those who are eligible after the spend-down process. In the pre-ACA period, there were 11 209(b) states. Three of these 209(b) states subsequently changed authorization leaving only eight 209(b) states by the end of 2017.
Only one state, Indiana, changed the income eligibility threshold for older adults during our study period, and our results are robust to excluding Indiana from the analysis.
The IPUMS ACS measure of total personal income (INCTOT) includes wages, salaries, nonfarm profit (or loss) from self-employment, farm profit, interest, dividends, rental income, Social Security and/or Railroad Retirement payments, SSI income, other public assistance, retirement, survivor, or disability benefits received from companies and unions, regular income from annuities and IRA or KEOGH retirement plans, and VA disability compensation.
Because Medicaid eligibility for adults age 65 and older is determined based on a “household of one” or a couple only, we adapt the SHADAC code to consider only income reported by the respondent or spouse.
Specifically, of the states in our sample, the following states expanded Medicaid to working age adults: 1) in 2014: AZ, AR, CA, CO, CT, DE, DC, HI, IL, IA, KY, MD, MA, MI, MN, NV, NH, NJ, NM, NY, ND, OH, OR, RI, VT, WA, and WV; 2) in 2015: AK, IN and PA; and 3) in 2016: LA and MT.
We omit adults who are 66 and 67 years old from the analysis for reasons described in detail below.
We measure ownership of non-housing assets using two income measures: 1) investment income, which measures pre-tax money received/lost such as income from an estate or trust, interest, dividends, royalties, and rents received and 2) business income, which measures self-employment income from a business. Respondents with any positive amounts of investment or business income are coded as having any non-housing assets.
We obtain annual state level data on the unemployment rate from the Local Area Unemployment Statistics program at the Bureau of Labor Statistics (https://www.bls.gov/lau/, viewed November 21, 2019) and on the Medicare Advantage penetration rate from the Kaiser Family Foundation (https://www.kff.org/data-collection/medicare-health-and-prescription-drug-plans/, viewed November 21, 2019).
The coefficients on these additional controls often have the expected signs: individuals with disabilities and those on SSI are more likely to participate in Medicaid, whereas older adults who either own a home or have other assets are less likely to participate in Medicaid.
The ACS does not solicit the value of the underlying assets.
We also test whether the DD estimate is robust to restricting the sample to single adults. This is relevant since Medicaid eligibility determination is more complex for couples, especially those needing long term care services (Musumeci and O’Malley Watts, 2019). We find a DD coefficient estimate of 0.023 (p<0.01).
In Appendix Table 5, we show that our DD estimate is also robust to including respondents not enrolled in Medicare. Thus, we find evidence of a welcome mat effect even if the welcome mat effect encourages new enrollment in both Medicare and Medicaid. Our baseline estimate focuses on respondents who are enrolled in Medicare because we are interested in dual enrollment, and for the dually enrolled, Medicare pays first and Medicaid is the payer of last resort.
Similar to the DD estimate, the DDD estimate is robust to restricting the sample to single adults. Among single adults, the DDD coefficient estimate is 0.061 (p<0.05).
When we omit California, the p-value is 0.108, and when we omit New York, the p-value is 0.129.
As with our DD estimates, in Appendix Table 5 we show that our DDD estimates are robust to including respondents not enrolled in Medicare in the sample.
REFERENCES
- Aizer A & Grogger J (2003). Parental Medicaid expansions and health insurance coverage. National Bureau of Economic Research Working Paper No. 9907. Cambridge MA: NBER. [Google Scholar]
- Bertrand M, Duflo E, & Mullainathan S (2004). How much should we trust differences-in-differences estimates? Quarterly Journal of Economics, 119, 249–275. [Google Scholar]
- Bhargava S & Manoli D (2015). Psychological Frictions and the Incomplete Take-Up of Social Benefits: Evidence from an IRS Field Experiment. American Economic Review, 105, 3489–3529. [Google Scholar]
- Boudreaux MH, Call KT, Turner J, Fried B, & O’Hara B (2015). Measurement error in public health insurance reporting in the American Community Survey: Evidence from record linkage. Health Services Research, 50, 1973–1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruen BK, Wiener JM, & Thomas S (2003). Medicaid eligibility policy for aged, blind, and disabled beneficiaries. AARP Public Policy Institute report #2003-14. Retrieved March 20, 2018, from https://www.aarp.org/health/medicare-insurance/info-2003/aresearch-import-575-2003-14.html. [Google Scholar]
- CBO (Congressional Budget Office). (2016). Federal subsidies for health insurance coverage for people under age 65: 2016 to 2026. Retrieved March 5, 2018, from https://www.cbo.gov/sites/default/files/114th-congress-2015-2016/reports/51385-healthinsurancebaselineonecol.pdf.
- CMS (Centers for Medicare and Medicaid Services). (2018). Complex case scenarios preventing gaps in health care coverage mini-series: Transitioning from Medicaid coverage to other health care coverage. (Slide 12). Retrieved June 5, 2019, from https://marketplace.cms.gov/technical-assistance-resources/transitioning-from-medicaid.pdf.
- Coe NB & Wu AY (2014). What impact does social security have on the use of public assistance programs among the elderly? Center for Retirement Research at Boston College Working Paper. CRR WP 2014–5. [Google Scholar]
- Courtemanche CH, Marton J, Ukert B, Yelowitz A & Zapata D (2017). Early impacts of the Affordable Care Act on health insurance coverage in Medicaid expansion and non-expansion states.” Journal of Policy Analysis and Management, 36, 178–210. [DOI] [PubMed] [Google Scholar]
- Cubanski J, Neuman T & Damico A (2016). Medicare’s role for people under age 65 with disabilities. Kaiser Family Foundation Issue Brief. Retrieved March 5, 2018, from https://www.kff.org/medicare/issue-brief/medicares-role-for-people-under-age-65-with-disabilities/. [Google Scholar]
- Currie JA (2004). The take up of social benefits. NBER Working Paper No. 10488. [Google Scholar]
- Davidoff A, Yemane A & Adams E (2005). Health coverage for low-income adults: Eligibility and enrollment in Medicaid and state programs, 2002. Kaiser Family Foundation Issue Brief. Retrieved December 13, 2018, from https://kaiserfamilyfoundation.files.wordpress.com/2013/01/health-coverage-for-low-income-adults-eligibility-and-enrollment-in-medicaid-and-state-programs-2002-policy-brief.pdf. [Google Scholar]
- Dubay L & Kenney G (2003). Expanding public health insurance to parents: Effects on children’s coverage under Medicaid. Health Services Research, 38, 1283–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frean M, Gruber J & Sommers B (2017). Premium subsidies, the mandate, and Medicaid expansion: Coverage effects of the Affordable Care Act. Journal of Health Economics, 53, 72–86. [DOI] [PubMed] [Google Scholar]
- Gardner L, & Gilleskie D (2012). The effects of state Medicaid policies on the dynamic savings patterns and Medicaid enrollment of the elderly. The Journal of Human Resources, 47, 1082–1127. [Google Scholar]
- Ghosh A, Simon K & Sommers BD (2019). The effect of health insurance on prescription drug use among low-income adults: Evidence from recent Medicaid expansions. Journal of Health Economics, 63, 64–80. [DOI] [PubMed] [Google Scholar]
- Gruber J and Sommers BD. (2019) The Affordable Care Act’s Effects on Patients, Providers, and the Economy: What We’ve Learned So Far. Journal of Policy Analysis and Management, 38(4): 1028–1052. [Google Scholar]
- Hamersma S, Kim M & Timpe B (2019). The effect of parental Medicaid expansions on children’s health insurance coverage. Contemporary Economic Policy, 37, 297–311. [Google Scholar]
- Hu L, Kaestner R Mazumder B, Miller S & Wong A (2018). The effect of the Affordable Care Act Medicaid expansions on financial wellbeing. Journal of Public Economics, 163, 99–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson J & Moriya A (2017). Medicaid expansion for adults had measurable “Welcome Mat” effects on their children. Health Affairs, 36, 1643–1651. [DOI] [PubMed] [Google Scholar]
- Jacobson G, Neuman T, & Damico A (2012). Medicare’s role for dual eligibles. Issue Brief. April 2012. Retrieved March 5, 2018, from http://kaiserfamilyfoundation.files.wordpress.com/2013/01/8138-02.pdf.
- Kaestner R (2016). Did Massachusetts health care reform lower mortality? No according to randomization inference.” Statistics and Public Policy, 3, 1–6. [Google Scholar]
- Kaestner R, Garrett B, Chen J, Gangopadhyaya A, and Fleming C. (2017) Effects of ACA Medicaid Expansions on Health Insurance Coverage and Labor Supply. Journal of Policy Analysis and Management. 36(3): 608–642. [DOI] [PubMed] [Google Scholar]
- Kenney GM, Anderson N & Lynch V (2013). Medicaid/CHIP participation rates among children: An update. The Urban Institute. [Google Scholar]
- Kenney GM, Long SK, & Luque A (2010). Health reform in Massachusetts cut the uninsurance rate among children in half. Health Affairs, 29, 1242–1247. [DOI] [PubMed] [Google Scholar]
- KFF (Kaiser Family Foundation). (2010). Medicaid financial eligibility: primary pathways for the elderly and people with disabilities. Retrieved March 5, 2018, from http://kff.org/medicaid/issue-brief/medicaid-financial-eligibility-primary-pathways-for-the-elderly-and-people-with-disabilities/.
- KFF (Kaiser Family Foundation). (2017). An overview of Medicare. Retrieved March 5, 2018, from https://www.kff.org/medicare/issue-brief/an-overview-of-medicare/.
- KFF (Kaiser Family Foundation). (2018) Status of State Action on the Medicaid Expansion Decision. Retrieved March 5, 2018, from http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/.
- Khantana SAM, Bhatla A & Nathan AS (2019) Association of Medicaid expansion with cardiovascular mortality. JAMA Cardiology, 4, 671–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lind KD (2012). Setting the record straight about Medicare. Washington, DC: AARP Public Policy Institute. Retrieved March 5, 2018, from http://www.aarp.org/content/dam/aarp/research/public_policy_institute/health/Setting-the-Record-Straight-about-Medicare-fact-sheet-AARP-ppi-health.pdf. [Google Scholar]
- MACPAC (Medicaid and CHIP Payment and Access Commission). (2018). MACStats: Medicaid and CHIP data book. Exhibit 19: Medicaid benefit spending per full-year equivalent enrollee by eligibility group and service category, FY 2013. Retrieved July 12, 2019, from https://www.macpac.gov/wp-content/uploads/2018/12/December-2018-MACStats-Data-Book.pdf.
- McInerney M, Mellor JM, & Sabik L (2017). The effects of state Medicaid expansions for working-age adults on senior Medicare beneficiaries. American Economic Journal: Economic Policy, 9, 408–438. [Google Scholar]
- McInerney M, Rutledge MS & King SE (2017). How much does out-of-pocket medical spending eat away at retirement income? Boston College Center for Retirement Research Working Paper (CRR WP 2017-13). [Google Scholar]
- MedPAC (Medicare Payment Advisory Commissions) and MACPAC (Medicaid and CHIP Payment and Access Commission). (2018). Beneficiaries dually eligible for Medicare and Medicaid. Retrieved March 5, 2018, from http://Medpac.Gov/Docs/Default-Source/Data-Book/Jan18_Medpac_Macpac_Dualsdatabook_Sec.Pdf?Sfvrsn=0.
- Mellor JM, McInerney M, & Sabik LM (2019). Misclassification of Medicaid Participation by Dual Eligibles: Evidence from the Medicare Current Beneficiary Survey. Medical Care Research and Review, forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller S and Wherry L (2017). Health and Access to Care during the first 2 years of the ACA Medicaid expansions. New England Journal of Medicine, 376, 947–956. [DOI] [PubMed] [Google Scholar]
- Musumeci M, Chidambaram P, & Watts MO (2019). Potential changes to Medicaid long-term care spousal impoverishment rules: States’ plans and implications for community integration.” Retrieved May 29, 2019, from https://www.kff.org/report-section/potential-changes-to-medicaid-long-term-care-spousal-impoverishment-rules-states-plans-and-implications-for-community-integration-issue-brief/.
- Neuman P, Cubanski J, Desmond KA & Rice TH (2007). How much “Skin in the Game” do Medicare beneficiaries have? The increasing financial burden of health care spending, 1997-2003. Health Affairs, 26, 1692–1701. [DOI] [PubMed] [Google Scholar]
- Pezzin LE & Kasper JD (2002). Medicaid enrollment among elderly Medicare beneficiaries: individual determinants, effects of state policy, and impact on service use. Health Services Research, 37, 827–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remler DK & Glied SA (2003). What other programs can teach us: Increasing participation in health insurance programs. American Journal of Public Health, 93, 67–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggles S, Flood S, Goeken R, Grover J, Meyer E, Pacas J, & Sobek M (2019) Integrated Public Use Microdata Series: Version 9.0 [dataset]. Minneapolis: University of Minnesota, 2019. [Google Scholar]
- SHADAC (State Health Access Data Assistance Center). (2013). Using SHAD AC Health Insurance Unit (HIU) and Federal Poverty Guideline (FPG) microdata variables. Retrieved November 7, 2018, from http://www.shadac.org/publications/using-shadac-health-insurance-unit-hiu-and-federal-poverty-guideline-fpg-microdata.
- Simon K, Soni A & Cawley J (2017). The impact of health insurance on preventive care and health behaviors: Evidence from the first two years of the ACA Medicaid expansions. Journal of Policy Analysis and Management, 36, 390–417. [DOI] [PubMed] [Google Scholar]
- Smith JC & Medalia C (2014). U.S. Census Bureau, Current Population Reports, P60–250, health insurance coverage in the United States: 2013, U.S. Government Printing Office, Washington, DC. Retrieved May 13, 2020, from http://www.census.gov/content/dam/Census/library/publications/2014/demo/p60-250.pdf. [Google Scholar]
- Sommers BD, Kenney GM & Epstein AM (2014). New evidence on the Affordable Care Act: Coverage impacts of early Medicaid expansions. Health Affairs, 33, 78–87. [DOI] [PubMed] [Google Scholar]
- Sommers BD, Chua KP, Kenney GM, Long SK, & McMorrow S (2016). California’s early coverage expansion under the Affordable Care Act: A county-level analysis. Health Services Research, 51, 825–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonier J, Boudreaux MH, & Blewitt LA (2013). Medicaid “Welcome-Mat” effect of Affordable Care Act implementation could be substantial. Health Affairs, 32, 1319–1325. [DOI] [PubMed] [Google Scholar]
- SSA (Social Security Administration). (n.d.). Program Operations Manual System (POMS). SI 01715.010 Medicaid and the Supplemental Security Income (SSI) program. Retrieved March 5, 2018, from http://policy.ssa.gov/poms.nsf/lnx/0501715010.
- SSA (Social Security Administration). (n.d.). Program Operations Manual System (POMS). SI 01730.005 Social Security Administration/state agreements under Section 1634. Retrieved December 17, 2018, from https://secure.ssa.gov/poms.nsf/lnx/0501730005.
- Tamblyn R, Rejean L, Hanley JA, Abrahamowicz M, Scott S, Mayo N, … Mallet L (2001). Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA, 285, 421–429. [DOI] [PubMed] [Google Scholar]
- Trivedi AN, Moloo H & Mor V (2010). Increased ambulatory care copayments and hospitalizations among the elderly. New England Journal of Medicine, 362, 320–328. [DOI] [PubMed] [Google Scholar]
- Ungaro R and Federman AD (2009). Restrictiveness of eligibility determination and Medicaid enrollment. Journal of Aging and Social Policy, 21, 338–351. [DOI] [PubMed] [Google Scholar]
- Watts MO, Cornachione E, & Musumeci M (2016). Medicaid financial eligibility for seniors and people with disabilities in 2015. Retrieved March 5, 2018, from http://kff.org/report-section/medicaid-financial-eligibility-for-seniors-and-people-with-disabilities-in-2015-report/.


