Abstract
To investigate the effect of core stability training on nonspecific low back pain (NSLBP) in nurses.
The data were collected retrospectively by reviewing the patient's medical records and pain questionnaires in our rehabilitation center. A total of 40 nurses with NSLBP were included and divided into observation group and control group. Each group were given routine health education for NSLBP. Core stability training was performed in observation group for 4 weeks. Surface electromyography (sEMG) evaluation of erector spine and multifidus muscle, pain Numeric Rating Scale (NRS) and Japanese Orthopaedic Association (JOA) scores were evaluated and analyzed before and 4 weeks after intervention.
There was no significant difference of NRS score and JOA score between two groups before intervention (P > .05, respectively). The NRS and JOA scores were significantly improved in both two groups after 4 weeks of intervention (P < .05, respectively). Moreover, the improvement of NRS and JOA scores in the observation group were better than those of the control group (P < .05, respectively). No significant difference of average electromyography (AEMG) or median frequency (MF) were noted between the healthy side and the affected side in both groups before or after intervention (P > .05, respectively). After 4 weeks of intervention, the AEMG of the healthy and the affected side of the two groups showed an improved trend without significant difference (P > .05, respectively). The MF of affected side was significantly higher 4 weeks after intervention than those before treatment in the observation and control group (P < .05, respectively).
Core stability training can alleviate pain, improve the fatigue resistance of the core muscles and the balance of the functions of bilateral multifidus muscles in nurses with NSLBP.
Keywords: core stability training, non-specific low back pain, nurses, surface electromyography
1. Introduction
Low back pain (LBP) is a group of pain syndrome characterized by pain in the lower back, lumbosacrum, sacroiliac, hip, often accompanied by leg pain, numbness and weakness. It mainly involves the lesions of lumbosacral muscles, fascia, ligaments, joints and intervertebral discs.[1,2] It affected 9.2% population worldwide and accounted for 11–12% disabled population.[3] Nonspecific LBP (NSLBP) is a general term for LBP, which cannot detect the exact histopathological changes and cannot identify its etiology through examination, which accounts for more than 85% of LBP.[4] It becomes a public health problem and a common disease in department of orthopaedics and rehabilitation. Psychosocial distress, poor coping skills, and high initial disability increase the risk for a prolonged disability course.[2] It is reported that nurses had higher incidence of NSLBP,[5–7] which not only seriously endangers the physical and mental health of nurses, but also affects the medical work, including high disability rate and high turnover rate.[8,9] Although one study showed that the onset age tends to be younger in nurses with the earliest age of 20 years,[10] the early diagnosis and treatment is still some difficult.
Core muscle stability training is widely used in the treatment of LBP in recent years.[11,12] It can strengthen the core muscle to maintain spinal stability, so as to relief pain. However, it was rare reported to be used in the NSLBP in nurses.
The purpose of this study is to evaluate the effect of core muscle stability training on NSLBP in nurses by measuring the surface electromyography (sEMG), pain Numeric Rating Scale (NRS) and Japanese Orthopaedic Association (JOA) LBP score.
2. Materials and methods
2.1. Subjects
This is a retrospective cohort study per protocol analysis. This study was supported by our Hospital Nursing Research Fund. It's the study for nurses’ occupational low back pain intervention. Patients meet strict inclusion/exclusion criteria were given routine health education, but core stability training were given on a voluntary basis from January 2016 to December 2017 in our rehabilitation center. We retrospectively collected the data after the study was finished. Two authors (Chao-Jun Zou and Fang Chao Wu) screened the records (stroke patients) from January 2016 to December 2017 in our rehabilitation center independently. Finally, a total of 40 nurses with NSLBP in our rehabilitation center were included. The diagnostic criteria of NSLBP was according to literature:[13,14]
-
1.
lumbar pain, pain locations below the scapular angle and above the hip with or without radiation pain of lower limbs, and NRS scores less than 5;
-
2.
no systemic diseases or specific positive imaging findings;
-
3.
psychological factors did not make pain enlarged or prolonged.
Patients with one of the following were excluded:
-
1.
NRS score was greater than 5;
-
2.
radioactive pain below knee joint or obvious organic lesions, such as lumbar disc herniation;
-
3.
pregnancy, systemic diseases, tumors, scoliosis and other known reason for LBP;
-
4.
complications with other lumbar diseases (e.g. congenital spinal stenosis, spondylolisthesis, spinal forward movement);
-
5.
with a history of lumbar fracture, trauma or lower extremity surgery;
-
6.
serviced in hospital less than 6 years or older than 60 years.
Calculation of the sample size was based on our previous pilot study, the effects of core stability training in low back pain. A difference in means of 2 points on the Numeric Rating Scale (NRS) score between the intervention and control group was considered as clinically relevant. If we applied a power of 80%, an alpha level of 5%, we had to include 40 patients.
These included nurses were divided into control group (n = 20) and observation group (n = 20). The control group included one male and 19 females aged 23 to 43 years, with a disease duration of 4 to 37 months. The observation group were all females aged from 26 to 40 years with a disease duration of 3 to 36 months. There was no significant difference in gender, age, and disease duration between two groups (P > .05, respectively).
This study was proved by the Ethical Committee of the Sir Run Run Shaw Hospital of Zhejiang University School of Medicine. All the participants provided written informed consent to participate in the study.
2.2. Assessment methods
sEMG, NRS[15] and JOA LBP score[16,17] were evaluated for all patients before and 4 weeks after treatment by one rehabilitation physician (T.W.). NRS score was investigated and assigned as following: 0, no pain; less than 3, mild tolerable pain; 4–6, tolerable pain, but affected sleep; 7–10, intense pain, intolerable. JOA LBP score was developed by Japan Orthopaedic Association including subjective symptoms, physical signs, activities of daily living and bladder function.
sEMG was performed in a quiet room with room temperature of 25°C. All subjects did not undergo any vigorous physical activity within 24 h. Five minutes of warm-up exercises such as proper stretching was performed before the experiment began. The sEMG signals of L3–4 erector spine muscle and L5-S1 multifidus muscle were recorded synchronously by Mega ME6000 T8 electromyograph (Finland Mega Company). The local skin of the lumbar dorsal muscles of the subjects was treated with alcohol degreasing before the electrodes were placed. The electrodes were placed in the fullest part of the erector spine muscle beside the L3 spinous process and the position of the multifidus muscle 2 cm beside the L5 spinous process. The recording electrodes were marked with a marker pen to be placed; the distance between the electrodes was 2 cm, parallel to the direction of the muscle fibers; and the reference electrodes were placed 3 cm outside the middle point of the recording electrodes. The original EMG waveforms recorded were analyzed by matching MegaWin 3.1 software. The original EMG signals of the subjects from the 5th to 35th second of the initial contraction for 30 s were analyzed. Average electromyography (AEMG) and median frequency (MF) were extracted for statistical analysis.
2.3. Intervention
Health education was performed for both 2 groups while core muscle stability training[18] was performed in the observation group only. Health education included enhance the awareness of occupational protection, avoid incorrect waist posture during working, weight control, regular exercise for low back pain at home, and wear waist brace if needed. Core muscle stability training for intervention group included:
-
1.
bridge exercise in supine position,
-
2.
back extension exercise in prone position,
-
3.
bridge exercise in lateral position,
-
4.
alternate arm and leg lifting in prone position,
-
5.
bridge exercise with swiss ball in supine position (see Fig. 1).
Figure 1.
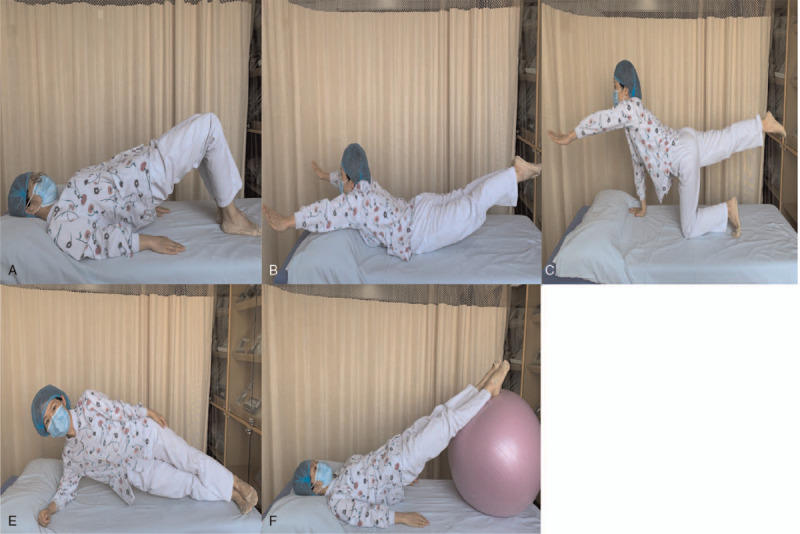
Examples of core stabilization exercises: (A). bridge exercise in supine position, (B). back extension exercise in prone position, (C). bridge exercise in lateral position, (D). alternate arm and leg lifting in prone position, (E). bridge exercise with swiss ball in supine position.
Exercises were designed 5 sets, from 8 to 10 repetitions and contractions from 5 s to 10 s. Rest intervals were set as 5 seconds between the sets and 2 mins between the exercises. Core stabilization exercise program was applied to the participants of the observation group for 5 days per week for 4 weeks with a total of 20 sessions. Each training session lasted for 45 mins, starting with a 10 mins warm up program and ending with a 5 mins cool down program.
2.4. Statistical analysis
SPSS17.0 statistical software was used for statistical analysis. Enumeration data were tested by Chi-square test, and the measurement data of normal distribution were expressed by mean ± SD. Independent sample t-test was used to measure the data between the two groups, and paired t-test was used to analyze the data before and after treatment. P < .05 by bilateral test was regarded as statistically significant.
3. Result
Two cases in the control group were loss to follow-up. There was no significant difference of NRS score and JOA LBP score between these two groups before intervention (P > .05, respectively). The NRS and JOA LBP score were significantly improved in both two groups after 4 weeks of intervention (P < .05, respectively). Moreover, the improved NRS and JOA LBP scores of the observation group were better than those of the control group (P < .05, respectively, Table 1).
Table 1.
NRS and JOA LBP scores in two groups pre- and post-intervention.
| Control group | Observation group | ||||||
| Baseline | After | P 1 | Baseline | After | P 1 | P 2 | |
| NRS score | 3.44 ± 1.14 | 2.50 ± 1.20 | t = 6.26 P = .00 | 3.33 ± 1.08 | 1.28 ± 0.89 | t = 9.99 P = .00 | t = 3.60 P = .00 |
| JOA score | 18.44 ± 1.65 | 20.67 ± 1.57 | t = -6.38 P = .00 | 18.72 ± 1.96 | 23.89 ± 2.05 | t = -9.39 P = .00 | t = -5.44 P = .00 |
The NRS and JOA LBP score were significantly improved in both two groups after 4 weeks of intervention (P < .05, respectively). Moreover, the improved NRS and JOA LBP scores of the observation group were better than those of the control group (P < .05, respectively). JOA = Japanese Orthopaedic Association, LBP = lower back pain, NRS = Numeric Rating Scale, P1 = P value compared within group, P2 = P value compared between two groups after therapy.
As for sEMG performed for erector muscle of spine and multifidus muscle, AEMG in the affected side was lower than these in the healthy group without significant difference in both groups before or after intervention (P > .05, respectively). After 4 weeks of intervention, the AEMG of the healthy side and the affected side of the two groups showed a trend of improvement, but there was no significant difference between two sides(P > .05, respectively). AEMG of affected side of the erector muscle of spine and multifidus muscles in both two groups after 4 weeks intervention was significantly higher than those before treatment (P < .05, respectively, as showed in Table 2).
Table 2.
AEMG in two groups pre- and post-intervention (μV).
| Control group | Observation group | ||||||
| Baseline | After | P 1 | Baseline | After | P1 | P2 | |
| Erector spine muscle | |||||||
| Healthy side | 97.44 ± 13.03 | 109.50 ± 12.24 | t = -8.79 P = .00 | 98.22 ± 12.43 | 117.39 ± 12.02 | t = -12.20 P = .00 | t = -2.01 P = .05 |
| Affected side | 84.39 ± 11.27 | 93.33 ± 10.00 | t = -12.20 P = .00 | 85.39 ± 12.60 | 101.06 ± 11.44 | t = -14.77 P = .00 | t = -2.22 P = .03 |
| Polyfidus muscle | |||||||
| Healthy side | 79.22 ± 9.97 | 89.06 ± 9.33 | t = -27.02 P = .00 | 80.28 ± 10.71 | 92.56 ± 10.41 | t = -11.14 P = .00 | t = -1.09 P = .28 |
| Affected side | 70.89 ± 8.48 | 79.28 ± 7.89 | t = -8.52 P = .00 | 72.00 ± 10.34 | 88.67 ± 10.60 | t = -22.90 P = .00 | t = -3.10 P = .00 |
AEMG in the affected side was lower than these in the healthy group but without significant difference in both groups pre- and post-intervention (P > .05, respectively). After 4 weeks of intervention, the AEMG of the healthy side and the affected side of the two groups showed a trend of improvement, but there was still no significant difference between two sides(P > .05, respectively). AEMG of affected side of the erector muscle of spine and multifidus muscles in both two groups after 4 weeks intervention was significantly higher than those before treatment (P < .05, respectively).
P1 = P value compared within group, P2 = P value compared between two groups after therapy.
The MF in the affected side was lower than these in the healthy group without significant difference in the two groups before intervention (P > .05, respectively). The MF of affected side of the erector muscle of spine and multifidus muscles in the observation group after 4 weeks intervention was significantly higher than those before treatment both in the observation and control group (P < .05, respectively). Moreover, the MF data in the affected side was showed a consistent trend with the healthy side in the observation group after 4 weeks intervention (Table 3).
Table 3.
MF between two groups pre- and post-intervention (Hz).
| Control group | Observation group | ||||||
| Baseline | After | P1 | Baseline | After | P1 | P2 | |
| Erector spine muscle | |||||||
| Healthy side | 78.44 ± 12.03 | 86.50 ± 11.25 | t = -7.55 P = .00 | 79.22 ± 12.33 | 94.39 ± 12.01 | t = -11.21 P = .00 | t = -2.09 P = .04 |
| Affected side | 75.39 ± 12.27 | 85.83 ± 11.01 | t = -11.08 P = .00 | 75.39 ± 12.61 | 92.06 ± 13.44 | t = -13.77 P = .00 | t = -1.56 P = .13 |
| Polyfidus muscle | |||||||
| Healthy side | 84.23 ± 16.97 | 94.06 ± 9.33 | t = -26.01 P = .00 | 90.22 ± 11.71 | 103.56 ± 10.41 | t = -13.15 P = .00 | t = -2.96 P = .01 |
| Affected side | 80.89 ± 8.48 | 89.28 ± 7.79 | t = -8.52 P = .00 | 84.00 ± 15.34 | 101.74 ± 12.60 | t = -21.91 P = .00 | t = -3.67 P = .01 |
The MF of affected side of the erector muscle of spine and multifidus muscles in the observation group after 4 weeks intervention was significantly higher than those before treatment both in the observation and control group (P < .05, respectively). P1 = P value compared within group, P2 = P value compared between two groups after therapy.
4. Discussion
NSLBP, a common type of LBP, affects the daily life of affected nurses.[8–10] It may be due to the fatigue of the paravertebral muscles, which maintain the stability of the spine, especially in the lumbar spine. These muscles need to maintain contraction for a long time to ensure the stability of the spine and the movement of the trunk. Long time standing or abnormal signature may worsen these fatigue of muscle fibers. Till now, therapy for NSLBP are very limited, including rest in hard mattress, physical therapy (e.g. hot compress), and appropriate analgesics. Previous studies showed that the effect of treatments for mild NSLBP was better than severe patients, which implied that early diagnosis and early intervention are very important. Traditional diagnosis of NSLBP mainly relies on self-report, physical examination, scale evaluation, CT and MRI imaging, and traditional electromyography. Recently, sEMG technology provides the possibility for early detection of slight neuromuscular dysfunction and observation of curative effect. sEMG is a technique for quantitative and qualitative analysis of neuromuscular function by placing skin surface electrodes on muscle surface to collect EMG signals during muscle activity (isotonic, isometric and isokinetic).[19]
Our results showed that the pain degree and scale scores were improved after 4 weeks even just accepting education. This suggested that excessive lumbar fatigue and long-term fixed posture may be the important causes of NSLBP in nurses, and rest and good posture maintenance are effective to improve NSPBL. The efficacy of exercise therapy in alleviating NSLBP has been widely recognized.[20] In our study, we noted that nurses accepted core muscle stability training improved significantly than these accepted rehabilitation educations only. Core muscle stability training is widely used in the treatment of LBP in recent years,[11,12] but rare for NSLBP in nurse. It was regarded that core muscle stability training may strengthen the lumbar paraspinal muscles (e.g. erector spine muscle, multifidus muscle), maintain spinal stability, and so to relief the pain.[11,21] Hence, core muscle stability training can effectively improve the symptoms of NSLBP, which is worthy of further promotion in clinical practice.
Our results also showed that MF of lumbar paraspinal muscles in the observation group were significantly improved after 4 weeks training. Moreover, the MF and AEMG were increased and much similar with the healthy side after 4 weeks training. These suggested that core muscle stability training increase the muscle fatigue resistance and the balance of muscle recruitment in the affected and healthy side of the lumbar spine. The results suggest that core stability training can effectively improve the fatigue resistance of paravertebral muscles in patients with LBP, thereby restoring spinal stability and alleviating the onset of NSLBP symptoms.[22]
Therefore, according to the results of this study, we speculate that the important factor of pain in NSLBP patients is the decrease of fatigue resistance of paravertebral muscles, and core stability training can effectively recruit muscle contraction, thereby restoring the stability and symmetry of the spine. As our study is 4 weeks only, further long-term follow-up studies are necessary to investigate the long-term efficacy.
Some limitations should be addressed as well. First, this is a retrospective study. Both patients and physiatrists were not blind to the therapy, thus the possibility of selection bias and placebo effect should be considered in the interpretation of our results. Second, our population consisted of working-age LBP patients, whose results may not correlate with other age groups, such as older adults LBP conditions. The LBP in working-age population may remit spontaneously. Third, although 40 patients were included, this study included a relatively small sample. In the future, multicenter studies with RCT and a long-term follow-up period should be performed to explore the core stability training effects on the fatigue resistance of the core muscles and the balance of the functions of bilateral multifidus muscles in patients with NSLBP.
In summary, our results show that core stability training can alleviate the symptoms, improve the fatigue resistance of the core muscles and the balance of the functions of bilateral multifidus muscles in patients with NSLBP. Long-term follow-up studies are necessary to investigate the long-term efficacy.
Acknowledgments
We thank all the members of our research team. The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Author contributions
Conceptualization: Chao-Jun Zou, Tao Wu.
Data curation: Chao-Jun Zou, Yang-Zhen Li.
Formal analysis: Chao-Jun Zou, Fang Chao Wu, Yang-Zhen Li.
Funding acquisition: Chao-Jun Zou.
Investigation: Fang Chao Wu, Yang-Zhen Li.
Methodology: Fang Chao Wu, Tao Wu.
Project administration: Fang Chao Wu, Hong Ying Pan, Tao Wu.
Resources: Fang Chao Wu, Jian Hua Li.
Software: Fang Chao Wu.
Supervision: Jian Hua Li, Hong Ying Pan, Tao Wu.
Validation: Jian Hua Li, Tao Wu.
Visualization: Hong Ying Pan.
Writing – original draft: Chao-Jun Zou, Tao Wu.
Footnotes
Abbreviations: AEMG = Average electromyography, JOA = Japanese Orthopaedic Association, LBP = Low back pain, MF = Median frequency, NSLBP = Nonspecific low back pain, NRS = Numeric Rating Scale, sEMG = Surface electromyography.
How to cite this article: Zou CJ, Li JH, Wu FC, Li YZ, Pan HY, Wu T. The effects of core stability training in nurses with nonspecific low back pain. Medicine. 2021;100:25(e26357).
This study was supported by Sir Run Run Shaw Hospital Nursing Research Fund (No.2015∗∗HL) and the Healthy and Family Planning Commission of Zhejiang Province, China (No. 2020385370).
The authors have no conflicts of interest to declare.
The datasets generated during and/or analyzed during the current study are publicly available; All data generated or analyzed during this study are included in this published article [and its supplementary information files]. The datasets generated during and/or analyzed during the present study are not publicly available, but are available from the corresponding author on reasonable request.
References
- [1].Tavee JO, Levin KH. Low back pain. Continuum (Minneap Minn) 2017;467–86. DOI: 10.1212/CON.0000000000000449. [DOI] [PubMed] [Google Scholar]
- [2].Golob AL, Wipf JE. Low back pain. Med Clin North Am 2014;98:405–28. DOI: 10.1016/j.mcna.2014.01.003. [DOI] [PubMed] [Google Scholar]
- [3].Waterman BR, Belmont PJ, Jr, Schoenfeld AJ. Low back pain in the United States: incidence and risk factors for presentation in the emergency setting. Spine J 2012;12:63–70. DOI: 10.1016/j.spinee.2011.09.002. [DOI] [PubMed] [Google Scholar]
- [4].Machado LA, Kamper SJ, Herbert RD, Maher CG, McAuley JH. Analgesic effects of treatments for non-specific low back pain: a meta-analysis of placebo-controlled randomized trials. Rheumatology (Oxford) 2009;48:520–7. DOI: 10.1093/rheumatology/ken470. [DOI] [PubMed] [Google Scholar]
- [5].O’Connell NE, Cook CE, Wand BM, Ward SP. Clinical guidelines for low back pain: a critical review of consensus and inconsistencies across three major guidelines. Best Pract Res Clin Rheumatol 2016;30:968–80. DOI: 10.1016/j.berh.2017.05.001. [DOI] [PubMed] [Google Scholar]
- [6].Delitto A, George SZ, Van Dillen L, et al. Low back pain. J Orthop Sports Phys Ther 2012;42:A1–57. DOI: 10.2519/jospt.2012.42.4.A1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Deyo RA, Dworkin SF, Amtmann D, et al. Report of the NIH Task Force on research standards for chronic low back pain. Phys Ther 2015;95:e1–18. DOI: 10.2522/ptj.2015.95.2.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kamioka H, Okuizumi H, Okada S, et al. Effectiveness of intervention for low back pain in female caregivers in nursing homes: a pilot trial based on multicenter randomization. Environ Health Prev Med 2011;16:97–105. DOI: 10.1007/s12199-010-0170-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Sundstrup E, Seeberg KGV, Bengtsen E, et al. A systematic review of workplace interventions to rehabilitate musculoskeletal disorders among employees with physical demanding work. J Occup Rehabil 2020;30:588–612. DOI: 10.1007/s10926-020-09879-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Pakbaz M, Hosseini MA, Aemmi SZ, Gholami S. Effectiveness of the back school program on the low back pain and functional disability of Iranian nurse. J Exerc Rehabil 2019;15:134–8. DOI: 10.12965/jer.1836542.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Aluko A, DeSouza L, Peacock J. The effect of core stability exercises on variations in acceleration of trunk movement, pain, and disability during an episode of acute nonspecific low back pain: a pilot clinical trial. Manipulative Physiol Ther 2013;36:497–504. DOI: 10.1016/j.jmpt.2012.12.012. [DOI] [PubMed] [Google Scholar]
- [12].Coulombe BJ, Games KE, Neil ER, Eberman LE. Core stability exercise versus general exercise for chronic low back pain. J Athl Train 2017;52:71–2. DOI: 10.4085/1062-6050-51.11.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K. Interobserver and intraobserver reliability of the Japanese Orthopaedic Association scoring system for evaluation of cervical compression myelopathy. Spine (Phila Pa 1976) 2001;26:1890–4. DOI: 10.1097/00007632-200109010-00014. [DOI] [PubMed] [Google Scholar]
- [14].Lee T, Kim YH, Sung PS. A comparison of pain level and entropy changes following core stability exercise intervention. Med Sci Monit 2011;17:CR362–8. DOI: 10.12659/msm.881846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Yao M, Li ZJ, Zhu S, et al. Simplified Chinese version of the Japanese Orthopaedic Association back pain evaluation questionnaire: cross-cultural adaptation, reliability, and validity for patients with low back pain. Spine (Phila Pa 1976) 2018;43:E357–64. DOI: 10.1097/BRS.0000000000002424. [DOI] [PubMed] [Google Scholar]
- [16].Chiarotto A, Maxwell LJ, Ostelo RW, Boers M, Tugwell P, Terwee CB. Measurement properties of Visual Analogue Scale, Numeric Rating Scale, and Pain Severity Subscale of the brief pain inventory in patients with low back pain: a systematic review. J Pain 2019;20:245–63. DOI: 10.1016/j.jpain.2018.07.009. [DOI] [PubMed] [Google Scholar]
- [17].Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976) 2005;30:1331–4. DOI:10.1097/01.brs.0000164099.92112.29. [DOI] [PubMed] [Google Scholar]
- [18].Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non-specific low back pain. Lancet 2012;379:482–91. DOI: 10.1016/S0140-6736(11)60610-7. [DOI] [PubMed] [Google Scholar]
- [19].Norwood JT, Anderson GS, Gaetz MB, Twist PW. Electromyographic activity of the trunk stabilizers during stable and unstable bench press. J Strength Cond Res 2007;21:343–7. DOI: 10.1519/R-17435.1. [DOI] [PubMed] [Google Scholar]
- [20].Macedo LG, Maher CG, Latimer J, McAuley JH. Motor control exercise for persistent, nonspecific low back pain: a systematic review. Phys Ther 2009;89:09–25. DOI: 10.2522/ptj.20080103. [DOI] [PubMed] [Google Scholar]
- [21].Wang XQ, Zheng JJ, Yu ZW, et al. A meta-analysis of core stability exercise versus general exercise for chronic low back pain. PLoS One 2012;7:e52082.DOI: 10.1371/journal.pone.0052082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Haruyama K, Kawakami M, Otsuka T. Effect of core stability training on trunk function, standing balance, and mobility in stroke patients. Neurorehabil Neural Repair 2017;31:240–9. DOI: 10.1177/1545968316675431. [DOI] [PubMed] [Google Scholar]


