Neighborhood Level Data is a Crucial Resource in Informing Vaccine Delivery
For many people around the world, the arrival of COVID-19 vaccines marks the beginning of the end of the current pandemic. However, in order for things to “return to normal,” public health officials face the challenge of distributing vaccines to billions of people around the world. One of the groups at increased risk for COVID-19 is older adults, as an overwhelming amount of evidence suggests that “age itself is the most significant risk factor for severe [cases of] COVID-19 and its adverse health outcomes” [1]. Thus, when vaccinations first became available to the public, this age group was prioritized in the Centers for Disease Control and Prevention’s (CDC) vaccine rollout recommendations [2].
On the national, state, and county level, there are many data reporting tools that can inform and coordinate COVID-19 vaccine distribution. The CDC’s Social Vulnerability Index (SVI) uses sociodemographic variables to calculate a social vulnerability rank for each census tract, which can help officials identify and assist communities most susceptible to public health emergencies [3]. Surgo Ventures’ COVID-19 Community Vulnerability Index builds upon SVI data by incorporating COVID-specific themes such as population density, access to testing, and nearby hospital capacity [4]. The company’s recent COVID-19 Vaccine Coverage Index applies the same model to identify and analyze areas at risk of poor vaccine coverage [5]. The University of Pittsburgh’s VaxMap 2.0 identifies county-level access to potential vaccine distribution centers and highlights areas where populations may have lower access to facilities that administer COVID-19 vaccines [6].
While these tools help public health officials identify areas at risk for COVID-19 and low vaccine uptake, they do not display available resources or specific sociodemographic descriptors on the neighborhood level. Such information is the true driver behind equitable vaccine distribution as differences in socioeconomic status and neighborhood resources can affect one’s health outcomes [7, 8]. In New York City, these differences are on display when one looks at COVID-19 vaccination rates by borough. As of April 29, the percentage of fully vaccinated older adults in Manhattan was 70% among adults 65–74, 67% among adults 75–84, and 54% among adults older than 85. In Brooklyn, meanwhile, the percentage of fully vaccinated older adults was much lower across all three age groups: 52%, 47%, and 35%, respectively [9]. The higher rates of vaccination in Manhattan can be partially explained by two sociodemographic indicators that are strong predictors of health outcomes: poverty and education status [10]. Adults 65+ living in Manhattan have, on average, lower rates of individuals living in poverty (18.0%) and more people with higher levels of education (18.4% have at least bachelor’s degree) than those living in Brooklyn (22.6% live in poverty, 11.8% have at least bachelor’s degree) [11, 12].
How Tools Like IMAGE:NYC Leverage Data to Address Vaccine Distribution Challenges
Unlike national or state level data, local data that combines sociodemographic descriptors with geospatial mapping provides a more nuanced picture of existing communities. One example of such a resource is IMAGE:NYC, an interactive map created by The New York Academy of Medicine (NYAM) in partnership with the City University of New York. As an open-source map of the city’s aging population, IMAGE:NYC provides its users with a visualization of local data while also displaying overlays of services and resources relevant to adults age 65+ [13]. By utilizing tools such as IMAGE:NYC, public health practitioners can better understand the communities they work in and adapt vaccine distribution efforts as needed.
Bridging the Digital Divide
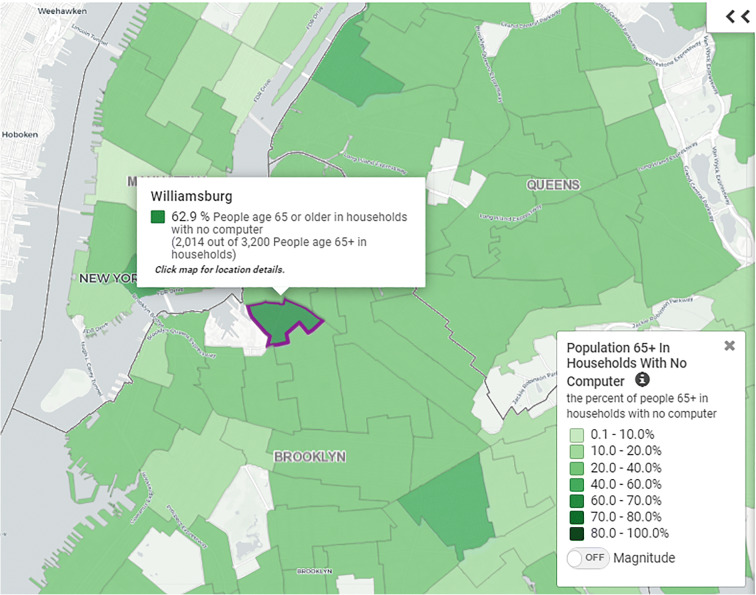
Older adults are typically less fluent with computers and/or internet services than their younger counterparts. In NYC’s vaccine rollout efforts, most public health announcements and education materials are first posted online. The easiest way for individuals to secure an early vaccination appointment is to use the city’s online Vaccine Finder to locate a preferred distribution center [14]. For older adults lacking internet access, the only option is to make appointments by phone, where they are often put on hold for hours [15]. According to the 2015–2019 American Community Survey, about 23.5% of adults 65+ living in NYC have no access to a computer. When broken down by neighborhood tabulation area (NTA), places like Williamsburg (62.9%), East Harlem North (47.1%), and Chinatown (43.4%) begin to stand out with even higher percentages [11].
By identifying these neighborhoods, public health officials can understand which areas require additional assistance. Local health departments can partner with organizations such as religious institutions, senior centers, and libraries to distribute educational materials and inform older adults on vaccine education and safety. Encouraging healthcare providers, social workers, and other community members to assist older patients with online registration can improve vaccination rates in neighborhoods with low technological access or literacy [Fig. 1].
Fig. 1.
The map key on IMAGE:NYC allows users to quickly identify NTAs where computer access is limited. Here, we can see that the majority of older adults living in Williamsburg, Brooklyn, do not have access to a computer [11]
Ensuring Accessibility
Mobility is another major concern as older adults (and anyone with a physical disability) may be unable to leave their home or commute to a vaccination site without assistance. Those who cannot rely on friends or family members may find vaccine sites inaccessible due to transportation difficulties or location. In the past decade, various studies have linked living alone in later life to increased vulnerability for social isolation, loneliness, and mobility problems [16–18]. In New York City, about half of adults 65+ live alone with NTA specific rates ranging from 73% in Hudson Yards-Chelsea-Flatiron-Union Square to 22.5% in South Ozone Park [11]. These individuals represent a significant portion of the aging population that may have difficulty traveling to designated vaccine centers on their own.
In recent weeks, there has been much progress improving vaccine accessibility among mobility-restricted individuals. FDA emergency use authorization of the Johnson & Johnson COVID-19 vaccine, a one dose vaccine that does not require intense refrigeration, has allowed NYC to offer in-home vaccine services to qualifying New Yorkers [19, 20]. However, further improvements can be made if vaccine distribution efforts are driven by local data. Demographic mapping can inform vaccine distributors where high concentrations of homebound adults are located, and visualization tools like IMAGE:NYC can further direct distribution efforts. In addition, by combining the framework of existing resources with data such as the ones mentioned above, vehicles similar to the COVID-19 Testing Mobile Units can offer vaccines and increase the pace of in-home vaccine services [21].
Adapting Public Health Messages to Different Communities
In cities as diverse as New York, historical, cultural, and language barriers must be considered with every public health issue, including vaccine distribution. Communities of color, with populations at higher risk of getting sick and dying from COVID-19, have faced historic and ongoing racism and discrimination in the medical system [22]. Studies show that concerns and/or distrust of the health care system are often identified as some of the biggest barriers to vaccine uptake [23]. Language barriers may also prevent individuals from accepting the COVID-19 vaccination. If information and resources are not accessible to people from different linguistic backgrounds, they will not be able to make fully informed decisions on whether or not to be vaccinated.
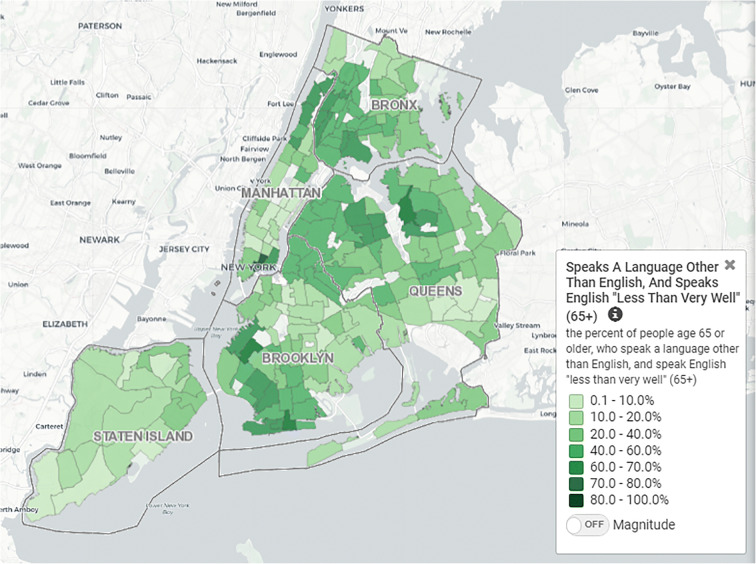
To adapt public health messages for diverse communities, local data can inform effective solutions. Recent census surveys show that a third of adults 65+ in NYC speak English “less than very well.” More than half of the older adults living in NTAs such as Flushing (73.5%), Brighton Beach (76.4%), and Washington Heights South (66.6%) have difficulty communicating in English [11]. By identifying these neighborhoods, the NYC Department of Health and Mental Hygiene can determine which areas require vaccine information and outreach in multiple languages. Furthermore, by including healthcare providers from diverse ethnic and racial backgrounds and local community institutions in the vaccine campaign process, the health department can ensure that its messaging is culturally appropriate for the intended audience(s) (Fig. 2).
Fig. 2.
Various neighborhoods throughout the city have a significant portion of older adults struggle with English [11]
Using Geospatial Tools to Display Public Health Data—Examples Outside NYC
In recent years, the rise of geospatial tools exhibiting neighborhood level data has been observed throughout the United States as more professionals realize its importance in addressing public health issues. Developed in 2018, California’s Healthy Places Index (HPI) aggregates community characteristics and “non-health” policies into a HPI score for each census tract throughout the state. In addition to sociodemographic indicators such as household income and education levels, HPI also displays data on commuter patterns, supermarket access, and air pollution [24]. The Baltimore City Health Department offers a map gallery with many resources specific to the city’s health needs including locations offering the flu vaccine, pharmacies carrying naloxone nasal spray and public schools with mental health/substance abuse programs [25]. More recently, Rutgers, The State University of New Jersey, is collaborating with local government leaders to develop their own age-friendly mapping tool for Bergen and Somerset counties. An adaptation of IMAGE:NYC, this tool will display concentrations of older adult subgroups with similar sociodemographic characteristics, as well as the geospatial positions of community-based assets [26].
The Importance of Data-Driven Public Health Solutions
While systemic inequities within the American health system have been worsening for years, the COVID-19 pandemic has shed light on problems that can no longer be ignored [27]. The disproportionate rates of COVID-19-related hospitalizations and deaths experienced in lower income neighborhoods, among people of color, and those with limited English proficiency, make it clear that changes are necessary. In order to address the health inequities that are related to an individual’s neighborhood, solutions driven by local data must be utilized by public health practitioners. By effectively disseminating and visualizing information, neighborhood level geospatial data will continue to aid the public health field in striving toward a greater and more equitable health system.
Footnotes
Yuxiao Lei graduated with a B.A. in Community & Global Public Health from the University of Michigan, School of Public Health.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chen Y, Klein SL, Garibaldi BT, et al. Aging in COVID-19: vulnerability, immunity and intervention. Ageing Res Rev. 2021;65 10.1016/j.arr.2020.101205. [DOI] [PMC free article] [PubMed]
- 2.Centers for Disease Control and Prevention. CDC’s COVID-19 vaccine rollout recommendations. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations.html. Published 2021. Accessed Mar 15, 2021.
- 3.Agency for Toxic Substances and Disease Registry. At A Glance: CDC/ATSDR Social Vulnerability Index. Centers for Disease Control & Prevention. https://www.atsdr.cdc.gov/placeandhealth/svi/at-a-glance_svi.html. Published 2021. Accessed Apr 29, 2021.
- 4.Surgo Ventures. Vulnerable Communities and COVID-19: The Damage Done, and the Way Forward. https://precisionforcovid.org/ccvi. Published 2021. Accessed Apr 29, 2021.
- 5.Surgo Ventures (2021) The U.S. COVID-19 Vaccine CoverageIndex: Leaving No Community Behind in the COVID-19 VaccineRollout. http://precisionforcovid.org/cva. Published 2021. Accessed Apr 29, 2021.
- 6.University of Pittsburgh School of Pharmacy, West Health. VaxMap: a county-level map of potential COVID-19 vaccine locations. West Health. https://www.westhealth.org/resource/vaxmap-potential-covid-19-vaccine-locations/. Published 2021. Accessed May 12, 2021.
- 7.Ducharme J, Wolfson E. Your ZIP code might determine how long you live—and the Difference Could Be Decades. Time. https://time.com/5608268/zip-code-health/. Published 2019. Accessed Mar 16, 2021.
- 8.New York City Department of Health and Mental Hygiene. Community Health Profiles. New York City Department of Health and Mental Hygiene. https://a816-health.nyc.gov/hdi/profiles/. Published 2020. Accessed Mar 16, 2021.
- 9.New York City Health. COVID-19: data on vaccines. City of New York. https://www1.nyc.gov/site/doh/covid/covid-19-data-vaccines.page. Published 2021. Accessed 29 Apr 2021.
- 10.Office of Disease Prevention and Health Promotion. Social Determinants of Health - Healthy People 2030. U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. https://health.gov/healthypeople/objectives-and-data/social-determinants-health. Published 2020. Accessed Apr 14, 2021.
- 11.New York Academy of Medicine. Use the Map – IMAGENYC. http://imagenyc.nyam.org/map/. Published 2021. Accessed Apr 4, 2021.
- 12.The Mayor’s Office for Economic Opportunity. Poverty in NYC - Data Tool. https://www1.nyc.gov/site/opportunity/poverty-in-nyc/data-tool.page. Published 2018. Accessed Apr 10, 2021.
- 13.New York Academy of Medicine. About IMAGE:NYC. http://imagenyc.nyam.org/about/. Published 2021. Accessed Apr 4, 2021.
- 14.New York City. NYC COVID-19 Vaccine Finder. 2020. https://vaccinefinder.nyc.gov/. Accessed Mar 23, 2021.
- 15.Otterman S. The red tape facing older people who want the Covid-19 vaccine. The New York Times. https://www.nytimes.com/2021/01/14/nyregion/covid-vaccine-older-people-senior-citizens.html. Published 2021. Accessed Mar 18, 2021.
- 16.Haslbeck JW, McCorkle R, Schaeffer D. Chronic illness: self-management while living alone in later life. Res Aging. 2012;34(5):507–547. doi: 10.1177/0164027511429808. [DOI] [Google Scholar]
- 17.Bergland A, Engedal K. Living Arrangements, Social Networks, Health, Mobility, and Balance of Older Women. Phys Occup Ther Geriatr. 2011;29(2):90–101. doi: 10.3109/02703181.2010.541987. [DOI] [Google Scholar]
- 18.Shaw BA, Fors S, Fritzell J, Lennartsoon C, Agahi N. Who lives alone during old age? Trends in the social and functional disadvantages of Sweden’s solitary living older adults. Res Aging. 2018;40(9):815–838. doi: 10.1177/0164027517747120. [DOI] [PubMed] [Google Scholar]
- 19.U.S. Food and Drug Administration. FDA issues emergency use authorization for third COVID-19 vaccine. FDA News Release. https://www.fda.gov/news-events/press-announcements/fda-issues-emergency-use-authorization-third-covid-19-vaccine. Published 2021. Accessed Mar 19, 2021.
- 20.New York City Department of Health and Mental Hygiene. COVID-19 vaccine distribution frequently asked questions. New York City Department of Health and Mental Hygiene. https://www1.nyc.gov/site/mopd/resources/covid-19-vaccine-distribution-frequently-asked-questions.page. Published 2021. Accessed Mar 19, 2021.
- 21.New York City Health & Hospitals. NYC Test & Trace Corps Announces New Covid Testing Mobile Units | NYC Health + Hospitals. New York City Health & Hospitals. https://www.nychealthandhospitals.org/pressrelease/nyc-test-trace-corps-announces-new-covid-testing-mobile-units/. Published 2020. Accessed Mar 24, 2021.
- 22.Centers for Disease Control & Prevention. Health equity considerations and racial and ethnic minority groups. Centers for Disease Control & Prevention. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html. Published 2021. Accessed April 4, 2021.
- 23.Artiga S, Kates J. Addressing racial equity in vaccine distribution. Kaiser Family Foundation. https://www.kff.org/racial-equity-and-health-policy/issue-brief/addressing-racial-equity-vaccine-distribution/. Published 2020. Accessed March 24, 2021.
- 24.Public Health Alliance of Southern California. California Healthy Places Index Map. California Department of Public Health. https://map.healthyplacesindex.org/. Published 2018. Accessed May 9, 2021.
- 25.Baltimore City Health Department. Maps Gallery. Baltimore City Health Department. http://gis.baltimorecity.gov/healthmaps/. Published 2020. Accessed May 9, 2021.
- 26.Rugers Community Design for Health & Wellness. Developing an interactive county mapping tool to advance age-friendly policies, programs, and planning in New Jersey. Rutgers, The State University of New Jersey. https://communitydesign.rutgers.edu/developing-an-interactive-county-mapping-tool-to-advance-age-friendly-policies-programs-and-planning-in-new-jersey/. Published 2021. Accessed May 15, 2021.
- 27.Odlum M, Moise N, Kronish IM, Broadwell P, Alcántara C, Davis NJ, Cheung YKK, Perotte A, Yoon S. Trends in poor health indicators among Black and Hispanic middle-aged and older adults in the United States, 1999-2018. JAMA Open Netw. 2020;3(11):e2025134. doi: 10.1001/jamanetworkopen.2020.25134. [DOI] [PMC free article] [PubMed] [Google Scholar]