Abstract
What role infectious agents play in the causation of psychotic disorders? To investigate this area, we have aimed to investigate the relationship between Toxoplasma gondii and psychotic disorders. A hospital-based cross-sectional study is designed. IgM and IgG antibodies to T. gondii in patients with psychotic disorders will be measured and presented in result. Seropositivity rates will be compared with first-degree relatives and healthy volunteers. Also, types of psychotic disorders and seropositivity rate will be compared. Here, we are presenting the study protocol with implications toward a brain-based diagnostic system and novel treatment approaches.
Keywords: Toxoplasma gondii, psychotic disorders, diagnostic system, seropositivity rate
1. INTRODUCTION
1.1. Background and Rationale
The role that infectious agents play in the aetiology of psychotic disorders is an area of interest. Among such candidates, Toxoplasma gondii becomes a prominent one. Evidences are emerging for this line of thinking [1]. Antibodies to T. gondii are more in patients with psychotic disorders. Some adults with toxoplasmosis exhibit psychotic symptoms. Epidemiological similarities are observed in toxoplasmosis and psychotic disorders. Antipsychotic agents inhibit T. gondii [2]. Toxoplasma raises dopamine levels in animals. Childhood exposure to cats is high in patients with psychotic disorders.
Abdollahian et al. [3] found more prevalence of T. gondii infection among schizophrenia patients compared to control in Iran. Chen et al. [4] found increased seropositivity of anti-Toxoplasma immunoglobulin G (IgG) and immunoglobulin M (IgM) not only with schizophrenia but also with bipolar disorder in China. By demonstrating elevated Toxoplasma exposure in recent onset psychosis, Yolken et al. [5] gave new insight to temporal relationship between exposure and disease onset.
The relationship of T. gondii and psychotic disorders has the potential to establish a brain-based diagnostic system in psychiatry and pave the way for novel therapeutic options with disease modifying effect.
2. OBJECTIVES
2.1. Specific Objectives
Measurement of IgM and IgG antibodies to T. gondii in patients with psychotic disorders.
Comparison of the seropositivity rate for anti-Toxoplasma IgG and IgM antibodies among patients with psychotic disorders with that of first-degree relatives (FDR) as well as healthy volunteers (HV).
Comparison of the types of psychotic disorders and seropositivity rate.
2.2. Hypotheses
A group of patients with psychotic disorders have serological evidence of Toxoplasma infection. There are certain characteristic clinical and demographic variables among patients with psychotic disorders who have serological evidence of Toxoplasma infection.
There might be a relationship between toxoplasmosis and the aetiology of schizophrenia, and an understanding of the pathogenesis of Toxoplasma infections in individuals with schizophrenia might lead to new approaches to the management of this disorder.
2.3. Design
The study will be a hospital-based cross-sectional study.
3. MATERIALS AND METHOD
3.1. Participants, Interventions, and Outcomes
3.1.1. Study setting
Department of Psychiatry and Department of Microbiology, Gauhati Medical College Hospital (GMCH), Guwahati, Assam, India.
3.2. Eligibility Criteria
3.2.1. Inclusion criteria for participants
Patients with psychosis as a defining feature (schizophrenia, acute and transient psychotic disorder, and delusional disorder) and psychosis as an associated symptom (mood disorder and substance use disorder).
3.2.2. Exclusion criteria for participants
Delirium, dementia, mental retardation, and neurological disorders that would affect cognitive performance including epilepsy, a history of encephalitis or head trauma, or any other reported disorder of the central nervous system.
3.2.3. Eligibility criteria for study centres
Patients with psychotic disorders attend for diagnosis and treatment, e.g. in Department of Psychiatry, GMCH.
IgG and IgM antibodies to T. gondii are measured, e.g. in Department of Microbiology, GMCH.
3.2.4. Eligibility criteria for who will perform
Competency in diagnosis and treatment of psychotic disorders, e.g. second, fourth, fifth, and seventh authors are psychiatrists.
Competency in measurement of IgG and IgM antibodies to T. gondii, e.g. first, third, and fifth authors are microbiologists.
3.2.5. Outcomes
Demography of participants. Clinical information of patients. IgM and IgG antibodies to T. gondii.
3.2.6. Participant timeline
One-year.
3.3. Sample Size
The sample size is calculated taking the prevalence to be estimated at 60% that gives the maximum sample size, with 95% levels of confidence and 20% bound on error of estimation. Taking this prevalence and stated permissible level of error, the sample size for the study is calculated using the formula
where n = required sample size, p = 0.6, q = 0.4, d = 20%.
Considering a 20% attrition rate, the sample size is 65 + 13 = 78.
3.4. Recruitment
Laboratory technician attending the individuals for collection of blood sample, without the individuals having to go to the laboratory is a strategy to improve adherence and procedure for monitoring adherence.
3.5. Data Collection, Management, and Analysis
3.5.1. Data collection methods
After written consent by the participant and her family, demographic and clinical information as well as 5 ml of blood samples will be taken from patients with psychotic disorders, first-degree relatives (FDR), and healthy volunteers (HV). The samples will be centrifuged for 5 minutes at 3,500 rpm; separated, quantitated, and stored at −20°C until later analysis. The serum obtained will be screened for IgM and IgG anti-Toxoplasma antibodies using the Enzyme Linked Fluorescent Assay (ELFA) in the mini VIDAS system (BioMérieux).The samples will be processed according to manufacturer’s instruction. The diagnoses of the patients with psychotic disorders will be made according to the criteria of the tenth revision of the World Health Organizatioin’s International Statistical Classification of Diseases and Related Health Problems (ICD-10) [6].
Relevant care and interventions for which the patients with psychotic disorders have attended Department of Psychiatry, GMCH are permitted to continue concomitantly. Participant/guardian request and worsening disease leading to clinically uncooperative state are criteria for discontinuing.
3.5.2. Statistical methods
Data will be analysed by descriptive (frequency and percentage) and inferential (Fisher’s exact and chi-square tests) statistics using Statistical Package for the Social Sciences (SPSS) and InStat GraphPad.
4. RESULT
Fig. 1. schematically represents the study procedure. Participants would constitute of patients, FDR, and HV. Their demography and clinical data would be collected. Sex and locality would be the demography while clinical data would be the antibodies to T. gondii.
Fig. 1.
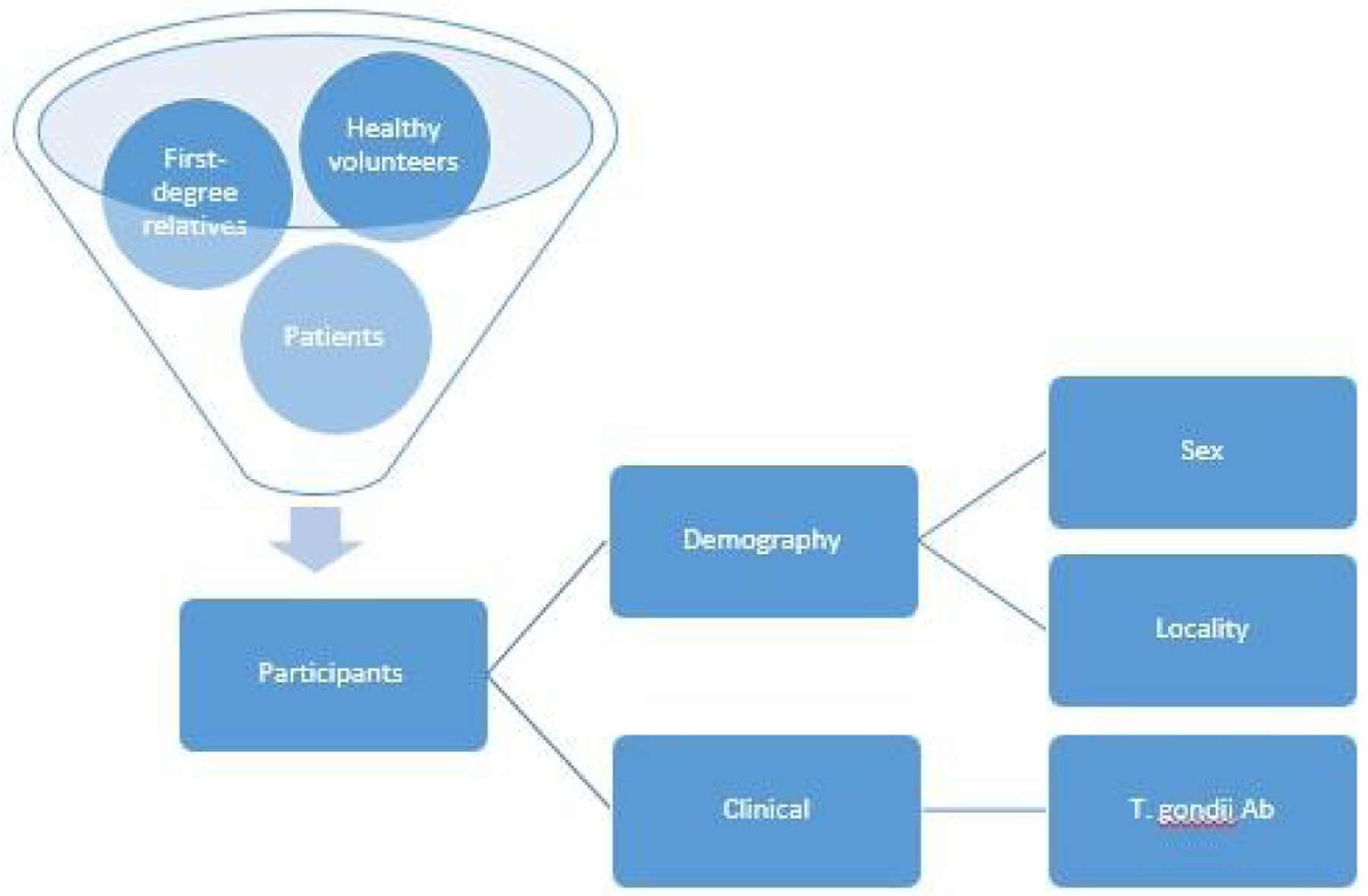
Schematic diagram. T. gondii Ab: Antibodies to Toxoplasma gondii
Table 1 will show characteristics of the sample. Characteristics would include sex, locality, diagnosis, participant distribution, IgM and IgG status.
Table 1.
Characteristics of the sample
| Characteristics | N | % |
|---|---|---|
| Sex | ||
| Women | x | x |
| Men | x | x |
| Locality | ||
| Rural | x | x |
| Urban | x | x |
| Diagnosis | ||
| F1 | x | x |
| F2 | x | x |
| F3 | x | x |
| Participant distribution | ||
| Patient | x | x |
| First-degree relative | x | x |
| Healthy volunteer | x | x |
| IgM status | ||
| Negative | x | x |
| Positive | x | x |
| Equivocal | x | x |
| IgG status | ||
| Negative | x | x |
| Positive | x | x |
| Equivocal | x | x |
F1: Mental and behavioural disorders due to psychoactive substance use, F2: Schizophrenia, schizotypal and delusional disorders, F3: Mood [affective] disorders
Tables 2 and 3 will show seroprevalence of anti-T. gondii antibodies in different participants. The Ig status can be positive, negative, or equivocal.
Table 2.
Seroprevalence of anti-Toxoplasma gondii IgM antibodies in different participants
| Participants | IgM status | |||||
|---|---|---|---|---|---|---|
| IgM negative | IgM positive | IgM equivocal | ||||
| N | % | N | % | N | % | |
| Patient | x | x | x | x | x | x |
| FDR | x | x | x | x | x | x |
| HV | x | x | x | x | x | x |
| Total | x | x | x | x | x | x |
FDR: First-degree relative, HV: Healthy volunteer
Table 3.
Seroprevalence of anti-Toxoplasma gondii IgG antibodies in different participants
| Participants | IgG status | |||||
|---|---|---|---|---|---|---|
| IgG negative | IgG positive | IgG equivocal | ||||
| N | % | N | % | N | % | |
| Patient | x | x | x | x | X | x |
| FDR | x | x | x | x | X | x |
| HV | x | x | x | x | X | x |
| Total | x | x | x | x | X | x |
FDR: First-degree relative, HV: Healthy volunteer
Tables 4 and 5 will show seroprevalence of anti-T. gondii antibodies in different groups. Diagnosis would be according to ICD-10:[6] F1 standing for mental and behavioural disorders due to psychoactive substance use, F2 standing for schizophrenia, schizotypal and delusional disorder, and F3 standing for mood [affective] disorders.
Table 4.
Seroprevalence of anti-Toxoplasma gondii IgM antibodies in different groups
| Groups | IgM positive | IgM negative | IgM equivocal | Total | ||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| F1 | x | x | x | x | x | x | x | x |
| F2 | x | x | x | x | x | x | x | x |
| F3 | x | x | x | x | x | x | x | x |
| None* | x | x | x | x | x | x | x | x |
| Total | x | x | x | x | x | x | x | x |
The ‘None’ group constitutes of first-degree relatives (FDR) and healthy volunteers (HV). F1: Mental and behavioural disorders due to psychoactive substance use, F2: Schizophrenia, schizotypal and delusional disorders, F3: Mood [affective] disorders
Table 5.
Seroprevalence of anti-Toxoplasma gondii IgG antibodies in different groups
| Groups | IgG positive | IgG negative | IgG equivocal | Total | ||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| F1 | x | x | x | x | x | x | x | x |
| F2 | x | x | x | x | x | x | x | x |
| F3 | x | x | x | x | x | x | x | x |
| None* | x | x | x | x | x | x | x | x |
| Total | x | x | x | x | x | x | x | x |
The ‘None’ group constitutes of first-degree relatives (FDR) and healthy volunteers (HV). F1: Mental and behavioural disorders due to psychoactive substance use, F2: Schizophrenia, schizotypal and delusional disorders, F3: Mood [affective] disorders
5. DISCUSSION
We have presented here the study protocol of the investigation of the relationship between Toxoplasma gondii and psychotic disorders with implications toward a brain-based diagnostic system and novel treatment approaches.
This line of investigation is not restricted to psychosis among adults. Researchers have explored this subject in different neuropsychiatric disorders as well as in the young population. Abd El-Aal et al. [7] found “significant associations between T. gondii seropositivity of epilepsy and depression groups where youth and adults had the highest sero-T. gondii infection especially male in rural areas with low social class”. Among children and adolescents, Yalın Sapmaz et al. [8] found higher T.gondii IgG seropositivity in depression, especially with suicidality. But, exploring suicidality among adolescents and T. gondii infection, Sari and Kara [9] found no significant differences between the patient and the control groups.
6. CONCLUSION
This study protocol outlines how the investigation of the relationship between Toxoplasma gondii and psychotic disorders is planned that has implications toward a brain-based diagnostic system and novel treatment approaches.
Footnotes
ETHICS AND DISSEMINATION
Consent: Authors will obtain informed consent from participants and authorized surrogates.
Ethical approval: The study proposal was approved by the Institutional Ethics Committee of GMCH (No. MC/02/2015/19, Date: 06/04/2015).
Confidentiality: Personal information about participants will be coded in order to protect confidentiality.
Declaration of interests: India-US Fogarty Training in Chronic Non-Communicable Disorders and Diseases Across Lifespan Grant #1D43TW009120 (SS Bhandari, Fellow; LB Cottler, PI).
Access to data: Along with the principal investigator (first author) and the co-investigator (second author), the funding agency (SSUHS) will have access to the final dataset.
Ancillary care: Any harm resulting from the interview for collection of demographic and clinical information as well as during the collection of blood samples will be addressed appropriately through mental and physical treatment and management as deemed necessary.
Dissemination policy: Not only participants and healthcare professionals but also the public and other relevant groups can access results from investigators and sponsor through publication [10].
Publisher's Disclaimer: DISCLAIMER
Publisher's Disclaimer: The products used for this research are commonly and predominantly use products in our area of research and country. There is absolutely no conflict of interest between the authors and producers of the products because we do not intend to use these products as an avenue for any litigation but for the advancement of knowledge. Also, the research was not funded by the producing company rather it was funded by personal efforts of the authors.
COMPETING INTERESTS
Authors have declared that no competing interests exist.
REFERENCES
- 1.Yolken RH, Dickerson FB, Fuller Torrey E. Toxoplasma and schizophrenia. Parasite Immunol. 2009;31(11):706–15. DOI: 10.1111/j.1365-3024.2009.01131.x. [DOI] [PubMed] [Google Scholar]
- 2.Jones-Brando L, Torrey EF, Yolken R. Drugs used in the treatment of schizophrenia and bipolar disorder inhibit the replication of Toxoplasma gondii. Schizophr Res. 2003;62(3):237–44. DOI: 10.1016/s0920-9964(02)00357-2. [DOI] [PubMed] [Google Scholar]
- 3.Abdollahian E, Shafiei R, Mokhber N, Kalantar K, Fata A. Seroepidemiological study of Toxoplasma gondii infection among psychiatric patients in Mashhad, Northeast of Iran. Iran J Parasitol. 2017;12(1):117–22. [PMC free article] [PubMed] [Google Scholar]
- 4.Chen X, Chen B, Hou X, Zheng C, Yang X, Ke J, et al. Association between Toxoplasma gondii infection and psychiatric disorders in Zhejiang, Southeastern China. Acta Trop. 2019;192:82–6. DOI: 10.1016/j.actatropica. 2019.02.001. Epub 2019 Feb 4. [DOI] [PubMed] [Google Scholar]
- 5.Yolken R, Torrey EF, Dickerson F. Evidence of increased exposure to Toxoplasma gondii in individuals with recent onset psychosis but not with established schizophrenia. PLoS Negl Trop Dis. 2017;11(11):e0006040. DOI: 10.1371/journal.pntd.0006040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992. [Google Scholar]
- 7.Abd El-Aal NF, Saber M, Fawzy N, Ashour WR. Sero-prevalence of anti-Toxoplasma gondii antibodies among patients with neuropsychiatric disorders: epilepsy and depression. J Egypt Soc Parasitol. 2016;46(3):729–36. [PubMed] [Google Scholar]
- 8.Yalın Sapmaz Ş, Şen S, Özkan Y, Kandemir H. Relationship between Toxoplasma gondii seropositivity and depression in children and adolescents. Psychiatry Res. 2019;278:263–7. DOI: 10.1016/j.psychres.2019.06.031. Epub 2019 Jun 20. [DOI] [PubMed] [Google Scholar]
- 9.Sari SA, Kara A. Association of suicide attempt with seroprevalence of Toxoplasma gondii in adolescents. J Nerv Ment Dis. 2019;207(12):1025–30. DOI: 10.1097/NMD.0000000000001046. [DOI] [PubMed] [Google Scholar]
- 10.Equator Network. SPIRIT 2013 Statement: Defining standard protocol items for clinical trials; 2021. Accessed 29 March 2021. Available: https://www.equator-network.org/reporting-guidelines/spirit-2013-statement-defining-stand


