Abstract
Myocarditis following mRNA COVID-19 vaccination has recently been reported to health authorities in the United States and other countries. Cases predominately occur in young adult males within four days following the second dose of either the Moderna (mRNA-1273) or Pfizer-BioNTech (BNT162b2) vaccines. Although the number of cases reported have been small in comparison with the large number of people vaccinated, myocarditis may be a rare adverse reaction to the COVID-19 vaccination that is now only becoming apparent due to the widespread use of the vaccine. In this article, we present a case of a 20-year-old male with no prior medical history who presented to the emergency department (ED) with chest pain. He had received the BNT162b2 vaccine two days prior to his presentation to the ED. The patient had an elevated troponin at 89 ng/L which increased on repeat examination. His electrocardiogram showed diffuse concave ST segment elevations and a later MRI confirmed the diagnosis of myocarditis. Based on these findings, the patient was diagnosed with myocarditis. The patient had a previous infection with SARS-CoV-2 approximately two months prior to the onset of his symptoms, but since he had fully recovered before the time of his presentation to the ED, it is unlikely that the infection caused the myocarditis. To our knowledge, this is the first published case of myocarditis following BNT162b3 vaccination.
Keywords: COVID-19, Vaccination, Myocarditis
A 20-year-old male with no prior medical history presented to the emergency department (ED) with a chief complaint of midsternal chest pain that radiated to the left side. The pain started in the morning and remained while resting. The patient also complained of mild shortness of breath secondary to pain. Upon examination, pain worsened with sitting and improved while lying flat. The patient had received his second dose of the Pfizer-BioNTech (BNT 162b2) vaccination two days prior to the onset of chest pain. The patient denied history of venous thromboembolism or family history of cardiovascular disease. The patient had a history of tobacco use. Approximately two months prior to ED presentation, the patient tested positive for SARS-CoV-2 and recovered with no sequalae.
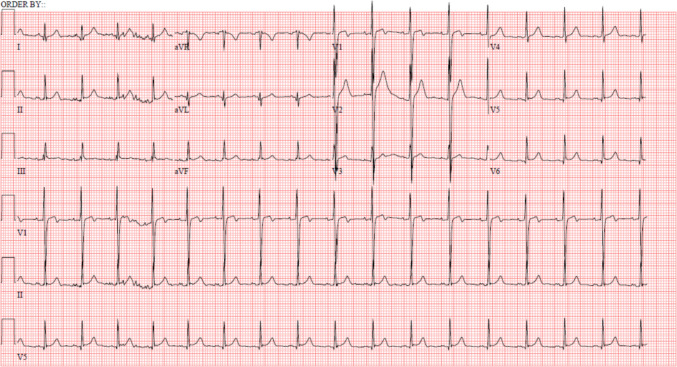
In the ED his initial troponin was 89 ng/L and increased to a maximum of 108 ng/L. The patient tested negative for SARS CoV-2 by PCR. Vital signs revealed blood pressure 121/54 mm/Hg, heart rate 113 beats per minute, temperature 98.4 °F orally, respirations 20 breaths per minute, SpO2 100% on room air. The patient's electrocardiogram showed diffuse concave ST segment elevations with PR depressions. (Fig. 1 ). Myocarditis was suspected and bedside ultrasound revealed a small pericardial effusion without evidence of tamponade, which supported the diagnosis. The patient was subsequently given a dose of colchicine 0.6 mg and then admitted to the hospital for further evaluation.
Fig. 1.
Note the somewhat diffuse concave ST elevations with PR depressions (V5-V6, II, aVF).
Inpatient echocardiogram showed left ventricular ejection fraction (LVEF) 59% with no other abnormalities. The patient underwent left heart catherization which was unremarkable. Cardiac computed tomography showed a coronary artery calcium score of zero and no pathology. Cardiac magnetic resonance imaging was positive for myocarditis. After his chest pain resolved, the patient was discharged with colchicine 0.6 mg for three months, metoprolol XL 12.5 mg daily for three months, and ibuprofen 600 mg three times daily for two weeks.
Myocarditis is most often caused by a viral infection; however, other causes include idiopathic, autoimmune, and hypersensitivity [1]. When there is an infectious etiology, patients typically present with flu-like symptoms in addition to chest pain [1]. Myocarditis is a potential complication of infection with COVID-19. Cardiac complications were first documented in Wuhan, China where 22–31% of COVID-19 patients admitted to the ICU developed myocarditis and 7% of COVID-19 deaths were secondary to myocarditis [2,3]. Pathologic mechanisms proposed for development of myocarditis following infection with COVID-19 include direct invasion of the myocardium, cytokine storm, or other hyperimmune activation that promotes inflammation [2].
Myocarditis has also been reported following live viral vaccinations, most notably the smallpox vaccine. From the early 1950s until 2003, six cases of cardiac complications following smallpox vaccination were reported in the United States [4]. A campaign to vaccinate U.S. military personnel against smallpox with the DryVax vaccine between 2002 and 2003 resulted in 67 cases of myocarditis or pericarditis out of the 540,824 personnel vaccinated [5]. Due to concern for cardiac complications following smallpox vaccination, a study was conducted to evaluate risk of myocarditis and pericarditis in live viral vaccinations [4]. Of the 416,629 vaccinated adults studied, only one case of pericarditis and zero cases of myocarditis were identified following vaccination [4]. The authors concluded there was no increased risk of myopericarditis following live viral vaccination [4].
There have been several cases of myocarditis following mRNA COVID-19 vaccination reported to authorities in the United States and Israel [6,7]. The U.S. Department of Defense (DoD) reported 14 military personnel were diagnosed with myocarditis following vaccination with either Moderna (mRNA-1273) or Pfizer-BioNTech COVID-19 vaccines [6]. The majority of cases received the mRNA-1273 vaccine, and most instances of myocarditis appeared following the second vaccination. With 2.7 million military personnel vaccinated, the rate of myocarditis in this population was 0.52 per 100,000 individuals [6]. The Israeli Ministry of Health reported 62 cases of myocarditis following mRNA COVID-19 vaccination [7]. Most cases occurred after the second dose and the prevalence of myocarditis was higher in men under 30 years old (1 per 20,000 in males aged 16–30 vs. 1 per 100,000 in the general population) [7].
The Advisory Committee on Immunization Practices (ACIP) COVID-19 Vaccine Safety Technical (VaST) session on May 17, 2021 reviewed presentations on myocarditis following mRNA vaccines from representatives of the DoD, the Vaccine Adverse Event Reporting System (VAERS), the Vaccine Safety Datalink, and the Veteran's Administration [8]. They concluded cases predominately occurred in adolescents and young adult males following the second dose and within four days after vaccination [8]. Although the Centers for Disease Control and Prevention claims reports of myocarditis cases following COVID-19 vaccination are within the expected baseline number, the members of VaST recommended that information should be provided to clinicians about the potential relationship between myocarditis and COVID-19 vaccination [8].
Despite news reports as well as a few cases reported to VAERS, only one case report of myocarditis following COVID-19 vaccination has been published to date [9]. That report detailed a case of myocarditis that developed four days after receiving a second dose of the mRNA-1273 vaccine in a 24-year-old male with no prior history of cardiovascular disease [9]. While our case demonstrates a clear temporal association of vaccine-related myocarditis and other potential causes of myocarditis are unlikely, a true cause-and-effect relationship could not be established nor determined. We hope this case provides emergency medicine physicians additional information on evaluating potential post COVID-19 vaccination myocarditis.
COI statement
The authors have no conflicts of interest.
Prior presentations
None
Funding sources/disclosures
None
Author contribution statement
AY conceived the case report. AY contributed to the medical management of the patient in the
emergency department. ELS drafted the manuscript, and all authors contributed substantially to its revision. AY takes responsibility for the paper as a whole.
References
- 1.Imazio M., Cecchi E., Demichelis B., et al. Myopericarditis versus viral or idiopathic acute pericarditis. Heart Br Card Soc. 2008;94(4):498–501. doi: 10.1136/hrt.2006.104067. [DOI] [PubMed] [Google Scholar]
- 2.Ma L., Song K., Huang Y. Coronavirus Disease-2019 (COVID-19) and cardiovascular complications. J Cardiothorac Vasc Anesth. 2021;35(6):1860–1865. doi: 10.1053/j.jvca.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuntz J., Crane B., Weinmann S., Naleway A.L. Myocarditis and pericarditis are rare following live viral vaccinations in adults. Vaccine. 2018;36(12):1524–1527. doi: 10.1016/j.vaccine.2018.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eckart R.E., Love S.S., Atwood J.E., Arness M.K., Cassimatis D.C., Campbell C.L., et al. Incidence and follow-up of inflammatory cardiac complications after smallpox vaccination. J Am Coll Cardiol. 2004;44(1):201–205. doi: 10.1016/j.jacc.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 6.Lee BY. Are rare cases of myocarditis linked to Pfizer, Moderna Covid-19 vaccines? https://www.forbes.com/sites/brucelee/2021/04/27/are-rare-cases-of-myocarditis-linked-to-pfizer-moderna-covid-19-vaccines/?sh=1b774c3d7442. April 27, 2021. Accessed May 25, 2021.
- 7.Staff T Israel said probing link between Pfizer shot and heart problem in men under 30. April 23, 2021. https://www.timesofisrael.com/israel-said-probing-link-between-pfizer-shot-and-heart-problem-in-men-under-30/ Accessed May 25, 2021.
- 8.Centers for Disease Control and Prevention COVID-19 VaST work group technical report. May 17, 2021. https://www.cdc.gov/vaccines/acip/work-groups-vast/technical-report-2021-05-17.html Accessed May 25, 2021.
- 9.Albert E., Aurigemma G., Saucedo J., Gerson D.S. Myocarditis following COVID-19 vaccination. Radiol Case Rep. May 18, 2021 doi: 10.1016/j.radcr.2021.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]