Abstract
Objective:
Outcomes of extracorporeal cardiopulmonary resuscitation (ECPR) for out-of-hospital cardiac arrest (OHCA) are dependent on time to therapy initiation. We hypothesized that it would be feasible to select refractory OHCA patients for expedited transport (ET) based on real-time estimates of the 911 call to the emergency department (ED) arrival interval, and for emergency physicians to rapidly initiate ECPR in eligible patients.
Methods:
In a two-tiered emergency medical service with an ECPR-capable primary destination hospital, adults with refractory shockable or witnessed OHCA were randomized 4:1 to ET or standard care if the predicted 911 call to ED arrival interval was ≤30 min. The primary outcomes were the proportion of subjects with 911 call to ED arrival ≤30 min and ED arrival to ECPR flow ≤30 min.
Results:
Out of 151 OHCA 911 calls, 15 subjects (10%) were enrolled. Five of 12 subjects randomized to ET had an ED arrival time of ≤30 min (overall mean 32.5 ± 7.1), and 5 were eligible for and treated with ECPR. Three of 5 ECPR-treated subjects had flow initiated ≤30 min of ED arrival (overall mean 32.4 ±10.9). No subject in either group survived with a good neurological outcome.
Conclusions:
EROCA did not meet predefined feasibility outcomes for selecting OHCA patients for expedited transport and initiating ECPR in the ED. Additional research is needed to improve the accuracy of predicting the 911 to ED arrival interval, optimize patient selection, and reduce the ED arrival to ECPR flow interval.
Introduction
Background
An estimated 250,000 people are treated by EMS for out-of-hospital cardiac arrest (OHCA) each year in the United States.1 The modest improvement in survival rates over the past decade have been primarily attributed to better implementation of cardiopulmonary resuscitation (CPR), better advanced cardiac life support (ACLS) by emergency medical services (EMS), and better post-cardiac arrest care. However, no new therapies have been proven effective in more than a decade. The result is a plateau of overall survival with good neurologic function rates at less than 10% for EMS-treated OHCA.2 The limiting factor for the majority (68%) of OHCA patients is failure to achieve sustained return of spontaneous circulation (ROSC).3
Extracorporeal cardiopulmonary resuscitation (ECPR) using percutaneous veno-arterial extracorporeal membrane oxygenation (VA-ECMO) is emerging as a feasible and potentially effective resuscitation strategy for non-traumatic OHCA patients who fail standard therapy. A recent systematic review of non-randomized studies reported that ECPR after OHCA was associated with long-term favorable neurologic outcome with odds ratios ranging from 1.95–9.27.4 Despite the promise of this emerging therapy based on observational data, it is costly, highly resource intense and operationally difficult to implement. Randomized clinical trials will be required to definitively demonstrate its efficacy.
Yet there are many challenges to conducting a definitive multicenter clinical trial of ECPR for OHCA. These include an incomplete understanding of fundamental parameters such as how quickly after a patient’s collapse can systems of care initiate ECPR, and whether the 911 call to ECPR-flow interval can be reliably estimated in real time and used as an inclusion criteria. The Extracorporeal Resuscitation of Out-of-hospital Cardiac Arrest (EROCA) study is a multifaceted research effort that included a pilot randomized trial of expedited EMS transport to an ECPR-capable hospital emergency department (ED) to study these parameters.
Rationale
Currently available evidence suggests that initiation of ECPR within 60 minutes of OHCA onset is associated with better neurologic outcome.5 Many published case series of ECPR for OHCA initiate ECPR in the ED,5–14 while other programs initiate ECPR in the cardiac catheterization laboratory.15,16 In either model, the rationale is to optimize the potential for favorable neurologic outcome by minimizing the interval from cardiac arrest onset to initiation of ECPR. For the ED model, in addition to delivering patients to the ED as soon as possible, it is essential that the clinical team can reliably and rapidly initiate ECPR after ED arrival. In a recently published study of ED-initiated ECPR, the median time from intensivist-based ECPR team arrival to initiation of ECPR was 20 minutes [IQR 15–30 minutes].14 In our own simulation study, ECPR could be consistently initiated within 30 minutes of patient arrival by trained emergency physicians and nurses.17 The potential advantage of ED providers performing cannulation is that they are already present in ED, which could minimize delays waiting for ECPR teams to arrive. For this study, we set target intervals for our primary outcome at ≤30 minutes for 911 call to ED arrival goal and ≤30 minutes for ED arrival to ECPR initiation by an emergency medicine cannulation team, with the overall goal of achieving a ≤60 min 911 call to ECPR initiation.
Objectives
The study objectives were (1) to determine the proportion of patients with refractory OHCA randomized to expedited transport based on a real-time estimated 911-ED arrival interval of ≤30 minutes that actually arrive at an ECPR-capable ED within 30 min; and (2) to determine the proportion of ECPR-eligible patients in whom ECPR was initiated within 30 minutes of ED arrival by an emergency medicine cannulation team.
Methods
Trial design
EROCA was a parallel group, randomized clinical trial. The trial focused on the feasibility and reliability of randomizing OHCA patients to standard care (control) versus expedited transport to an ECPR-capable hospital (experimental) when the 911 call to ED arrival interval was estimated to be ≤30 minutes. It additionally evaluated the feasibility of emergency physicians initiating ECPR within 30 minutes of ED arrival. Participants were assigned to the experimental group in a 4:1 ratio relative to the control group. This ratio balanced learning about the feasibility of randomization with ensuring an adequate number of ECPR eligible patients. However, the eligible EMS transporting agencies expanded and the eligible ECMO devices changed over the course of the trial. The study protocol is available as Supplemental Material 1.
Setting
We conducted the trial in Ann Arbor, Michigan. Initially, only EMS patients located within the response zone of the City of Ann Arbor Fire Department were included. Ann Arbor has a population of 123,062 and a population density of 4,409/mi2.18 Due to lower than expected enrollment, the catchment area was expanded during the trial to several adjacent first responder agencies including Scio Township Fire Department (population 17,949, population density 525/mi2), Ann Arbor Township Fire Department (population 4,579, population density 271/mi2), and Saline Area Fire Department (population 9,363, population density 2,128/mi2). All participating Fire Departments were equipped with mechanical CPR devices (LUCAS-2 Physio-Control or Autopulse; Zoll, Chelmsford, MA). The ECPR-capable ED was in the Michigan Medicine/ University of Michigan Hospital.
Eligibility Criteria
The EROCA trial screened all adult OHCA patients within the catchment area of the participating first responding Fire Departments.
Inclusion Criteria
Present with OHCA, presumed non-traumatic etiology and requiring CPR
Age presumed or known to be 18 through 70 years old (prior to 71st birthday)
Predicted 911 call to arrival time at ECPR-capable ED interval predicted to be within 30 minutes.
Initial shockable rhythm (ventricular tachycardia or ventricular fibrillation) or witnessed arrest with pulseless electrical activity or asystole as presenting rhythm
Persistent cardiac arrest after initial manual paramedic cardiac rhythm analysis and shock if indicated.
Exclusion Criteria
Do Not Attempt Resuscitation or Do Not Intubate advanced directive
Pre-existing evidence of opting out of study
Prisoner
Pregnant (obvious or known)
ECPR-capable ED is not at the destination hospital as determined by EMS destination protocol
Legally authorized representative aware of study and refuses study participation at the scene
Eligibility for ECPR
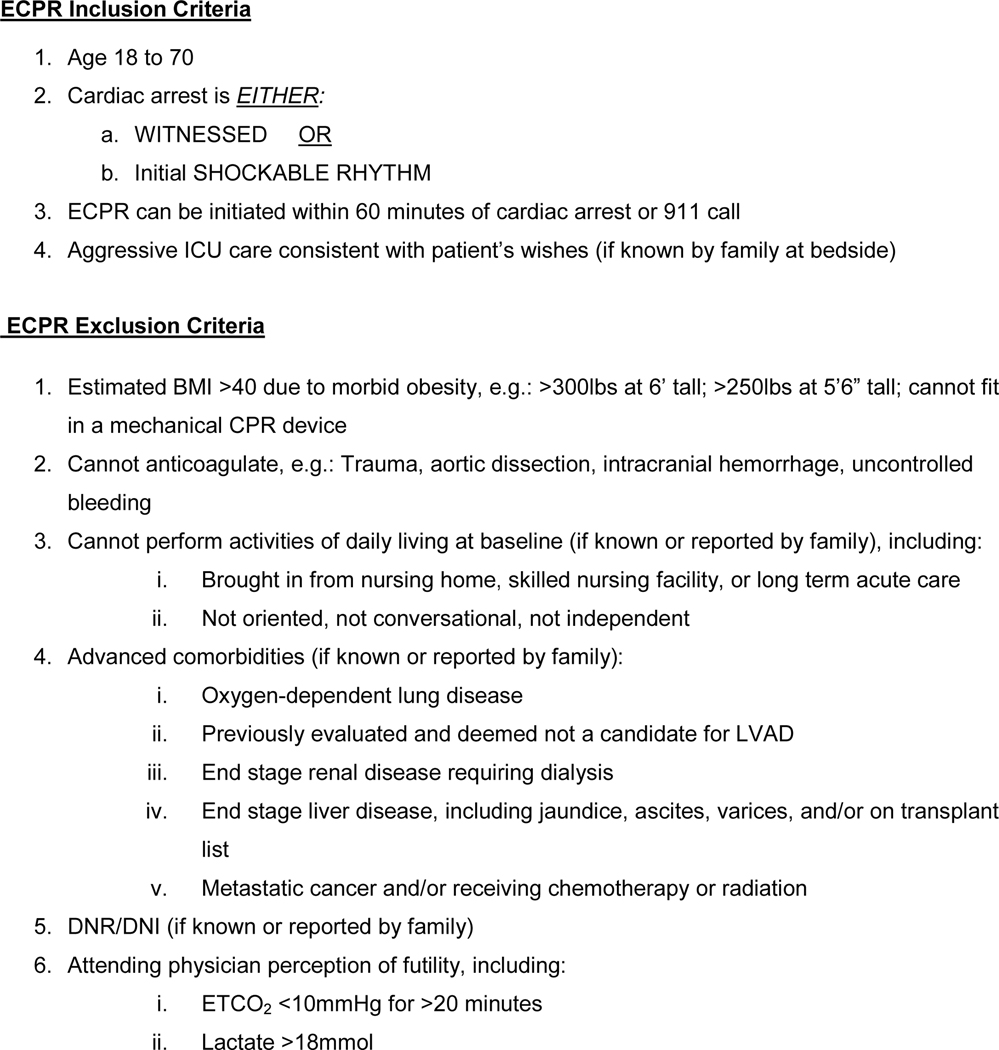
The ECPR-capable hospital had a written care guideline for all ED patients with refractory cardiac arrest with predefined eligibility criteria for initiating ECPR (Figure 1).
Figure 1 – ECPR Eligibility Criteria.
Identification of participants
The EMS central dispatchers identified potential cardiac arrest patients based on the reason for call from 911. If the potential cardiac arrest occurred within the response boundaries of a participating first responding Fire Department, the dispatcher would complete a pre-assignment computer application that would return a transport strategy of either expedited transport or standard care. The computer application used real-time web-based information from Google Maps Application Programing Interface regarding traffic and distance from location of arrest to the ambulance bay of ECPR-capable hospital.
Consent
Patients were enrolled under the exception from informed consent process. Enrollment occurred at the time of randomization by the prehospital providers at the scene of the OHCA. The study team conducted community consultation and public disclosure in each participating community. The study team approached a legally authorized representative and obtained consent to continue data collection and outcome assessment when the patient survived to hospitalization. The study team provided notification to a legally authorized representative if the patient did not survive to hospital admission or if the team was unable to contact them prior to the death.
Interventions
EROCA compared two treatment strategies for refractory OHCA: continued standard care in the field (control) versus expedited transport with ongoing mechanical CPR to a hospital capable of initiating ECPR in the ED (experimental). ECPR is defined as percutaneous VA-ECMO initiated during cardiac arrest. The standard care EMS cardiac arrest protocol is provided as Supplemental Material 2. For the expedited transport group, interventions required prior to initiating transport included the insertion of an advanced airway, establishment of intravenous or intraosseous access, and initiation of mechanical CPR. If the patient were to re-arrest during transport, the EMS providers were instructed to deliver shocks and medications during transport rather than stopping to deliver these interventions until ROSC. There was no time limit to provide on-scene resuscitation prior to transport. The standard protocols were otherwise not modified for the expedited transport group.
Randomization
A website available to the Huron Valley Ambulance 911 Medical Dispatch Center was used to randomize subjects. Randomization occurred in blocks of 5 using an urn method. The randomization ratio was 4:1 favoring the expedited transport group; this was intended to establish the feasibility of the randomization process, while providing more opportunities to provide ECPR as compared to 1:1 allocation. In situations where the dispatcher used the website and gave a treatment group assignment, but the patient was not enrolled/randomized in the study because they did not meet inclusion/exclusion criteria at the scene, that treatment group assignment was returned to the urn.
Outcomes
Primary endpoints
Proportion of patients with a 911 call or prehospital witnessed first cardiac arrest (qualifying OHCA event) to ED arrival interval of ≤30 minutes. We selected this primary endpoint because the goal of the study was to demonstrate the feasibility and reliability of transporting patients with refractory OHCA to an ECPR-capable ED within a predefined interval based on real time estimates.
Proportion of ECPR-eligible patients with an ED arrival to ECPR initiation interval of ≤30 minutes. We chose this time interval because the estimated therapeutic window for OHCA ECPR is 60 minutes, and our simulation studies support the feasibility of emergency physicians initiating ECPR within this interval.
Safety endpoints
Hemorrhage requiring blood transfusion, pneumothorax requiring thoracostomy, hemopericardium requiring pericardiocentesis.
Hemorrhage requiring blood transfusion (greater than 4 units packed red blood cells per incident), vessel damage requiring vascular procedure or leading to occlusion, venous/arterial thromboembolism, stroke, renal failure, and infection. Other safety endpoints included all components of composite safety endpoints along with splenic and/or liver injury.
Exploratory Endpoints
We measured the modified Rankin Scale (mRS) and Cerebral Performance Category (CPC) at hospital discharge and 90 days. Good neurologic outcome was predefined as 90-day mRS ≤3 or CPC ≤2. We also assessed patient reported outcomes using the Neuro-QOL battery and cognitive functioning using the NIH-Toolbox.
Sample Size
This was a pilot trial, designed to demonstrate feasibility in preparation for a larger trial that will be powered to detect effect on patient outcomes. As such, the primary endpoints targeted process measures. The expedited transport protocol would thus have been considered acceptable if ≥ 80% (20/24) patients arrived at the ED ≤30 minutes. Similarly the ED ECPR initiation time would have been considered acceptable if the ED arrival to ECPR initiation interval was ≤30 minutes in 80% or more of patients eligible for ECPR. Planned enrollment was 30 patients with 24 enrolled in the expedited transport group (experimental) and 6 enrolled in the standard care group (control).
Trial registration and ethical approvals
The EROCA trial was registered as NCT03065647 on ClinicalTrals.gov, granted an Investigational Device Exemption from the Food and Drug Administration (FDA) (G160263 IDE), and was approved by the University of Michigan Institutional Review Board as application HUM00117553.
Participants
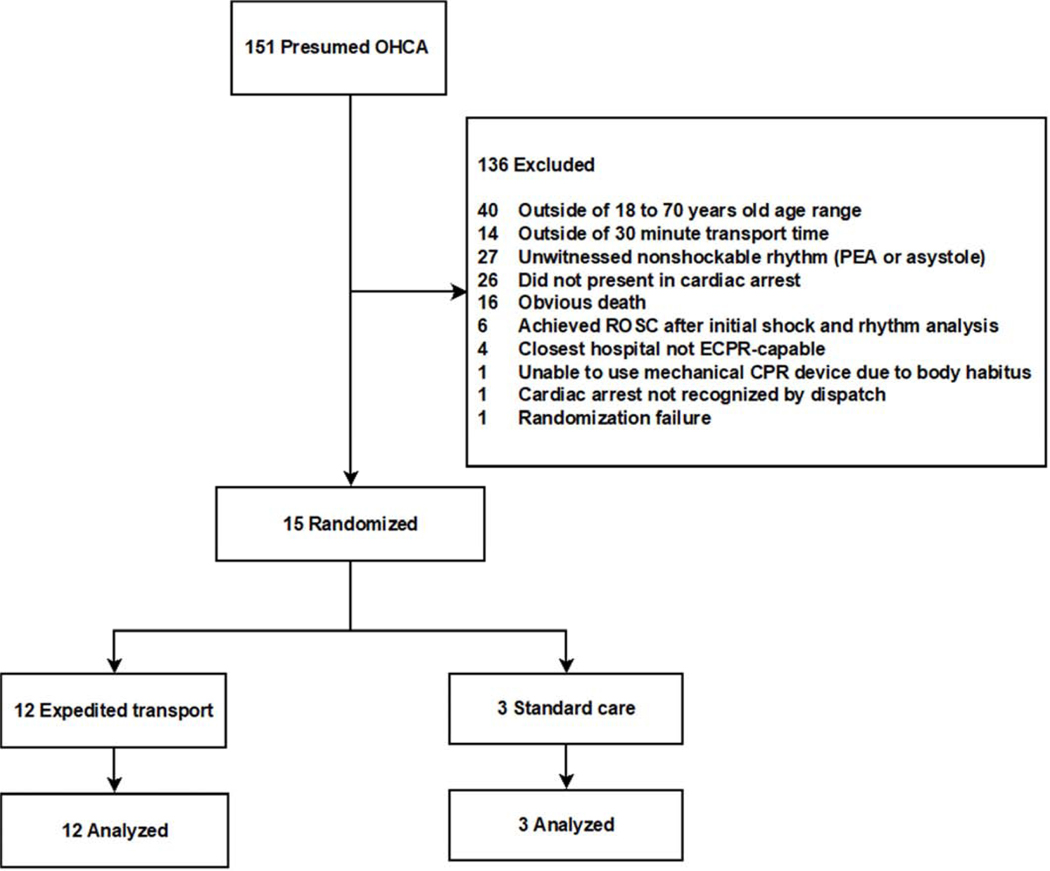
During the study period, 151 OHCA patients met initial pre-screening criteria and 15 were randomized (Figure 2). Randomization was turned off during 3% of the overall study period, primarily due to the unavailability of qualified ECPR cannulators. During that time, there were 5 OHCA 911 calls. Two out of these 5 OHCA patients had a shockable rhythm and were within the predicted time to ED arrival. Two were ineligible based on being asystole and unwitnessed, and one was outside the predicted time to ED arrival.
Figure 2 – CONSORT Diagram.
Recruitment
Recruitment occurred between May 1, 2017 and March 5, 2020. The study investigators proposed ending the trial early to the Data and Safety Monitoring Board (DSMB) prior to achieving intended accrual. This was due to slower than anticipated recruitment, FDA-mandated pause after enrollment of initial 15 subjects pending approval for additional enrollment on March 5, 2020, and institutionally-mandated pause in clinical research operations on March 14, 2020, due to the COVID-19 pandemic. The DSMB agreed to end the trial early on April 22, 2020.
Results
Baseline Data
The overall cohort (n=15) was 67% male and 80% Caucasian with a mean age of 62. The initial cardiac rhythm was shockable in 53% (n=8). Additional characteristics of the overall cohort, standard care, and expedited transport groups are available in Table 1. We report this trial in accordance with the CONSORT extension for Pilot and Feasibility Trial (Supplemental Material 3).
Table 1 -.
Characteristics of subjects by group.
| Cardiac Arrest Characteristics | Overall (n=15) | Standard Care (n=3) | Expedited Transport (n=12) |
|---|---|---|---|
| Age (mean ± SD years) | 62 ± 7 | 61 ± 3 | 62 ± 8 |
| Sex (n, %) | |||
| Female | 5 (33) | 1 (33) | 4 (33) |
| Male | 10 (67) | 2 (67) | 8 (67) |
| Race (n, %) | |||
| Caucasian | 12 (80) | 3 (100) | 9 (75) |
| African American | 1 (7) | 0 | 1 (8) |
| Unknown/Declined | 2 (13) | 0 | 2 (17) |
| Asian | 0 | 0 | 0 |
| American Indian/Alaskan Native | 0 | 0 | 0 |
| Native Hawaiian/Pacific Islander | 0 | 0 | 0 |
| Bystander CPR (n, %) | 10 (67) | 3 (100) | 7 (58) |
| Cardiac arrest location (n, %) | |||
| Home | 12 (80) | 2 (67) | 10 (83) |
| Public location | 3 (20) | 1 (33) | 2 (17) |
| Initial cardiac rhythm (n, %) | |||
| Ventricular fibrillation | 8 (53) | 3 (100) | 5 (42) |
| Witnessed PEA | 4 (27) | 0 | 4 (33) |
| Witnessed asystole | 3 (20) | 0 | 3 (25) |
SD = standard deviation, CPR = cardiopulmonary resuscitation, PEA = pulseless electrical activity
Outcomes
For primary endpoint 1, 5 out of 12 participants or 42% (95% CI 19–68%) in the expedited transport group had a 911 call to ED arrival interval of ≤30 minutes. For primary endpoint 2 in the subset eligible for ECPR, 3 out of 5 participants or 60% (95% CI 23–88%) had an ED arrival to ECPR initiation interval of ≤30 minutes. Table 2 compares the estimated and actual subintervals for each patient in the expedited transport group including 911 call to scene arrival by paramedics, paramedic scene time, and transport time. These sub-interval results demonstrate that our model systematically underestimated paramedic scene time and overestimated transport times.
Table 2 -.
Expedited transport time intervals.
| Individual subject data by ECPR use | 911 Call to scene arrival interval (min) | Scene arrival to scene departure interval (min) | Scene departure to ED arrival interval (min) | 911 Call to ED arrival interval (min) | ED arrival to ECPR flow interval (min) | 911 Call to ECPR flow interval (min) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predicted* | Observed | Predicted* | Observed | Predicted# | Observed | Predicted | Observed | Predicted | Observed | Predicted | Observed | |
| ECPR | 5 | 8 | 8 | 7 | 12 | 7 | 25 | 22 | 30 | 34 | 60 | 56 |
| 5 | 12 | 8 | 19 | 15 | 8 | 28 | 39 | 30 | 21 | 60 | 60 | |
| 5 | 6 | 8 | 29 | 15 | 8 | 28 | 43 | 30 | 30 | 60 | 73 | |
| 5 | 3 | 8 | 15 | 13 | 5 | 26 | 23 | 30 | 27 | 60 | 50 | |
| 5 | 8 | 8 | 28 | 5 | 6 | 18 | 42 | 30 | 50 | 60 | 92 | |
| No ECPR | 5 | 11 | 8 | 19 | 16 | 7 | 29 | 37 | ||||
| 5 | 6 | 8 | 15 | 12 | 7 | 25 | 28 | |||||
| 5 | 4 | 8 | 26 | 11 | 2 | 24 | 32 | |||||
| 5 | 5 | 8 | 14 | 17 | 11 | 30 | 30 | |||||
| 5 | 7 | 8 | 22 | 8 | 4 | 21 | 33 | |||||
| 5 | 5 | 8 | 12 | 12 | 8 | 25 | 25 | |||||
| 5 | 6 | 8 | 23 | 12 | 7 | 25 | 36 | |||||
| Mean ± SD (min) | 5 | 6.8 ± 2.7 | 8 | 19.1±6.8 | 12.3±3.3 | 6.7 ± 2.3 | 25.3±3.3 | 32.5 ± 7.1 | 30 | 32.4 ± 10.9 | 60 | 66.2 ± 16.7 |
| Proportion ≤ target | 0.42 | 0.08 | 0.92 | 0.42 | 0.40 | 0.60 | ||||||
| Mean Δ from predicted (min) | 1.8 ± 2.7 | 11.1 ± 6.8 | −5.7 ± 2.7 | 7.2 ± 8.1 | 2.4 ± 10.9 | 6.2 ± 16.7 | ||||||
ED = Emergency department. ECPR = Extracorporeal cardiopulmonary resuscitation. SD = Standard deviation.
The algorithm used fixed predictions for time from the 911 call until advanced life support providers arrived on scene (5 minutes) and for scene time (8 minutes).
Transport time from scene to hospital was estimated using a call to the Google Maps API to get estimated vehicular drive time.
Seven out of 12 patients in the expedited transport group were not ECPR candidates based on ED criteria. The reasons for their ineligibility included not consistent with goals of care, contraindication to anticoagulation, advanced cancer on chemotherapy, ROSC achieved in the ED, BMI > 40, attending physician’s perception of futility, and ECPR could not be initiated within 60 minutes of 911 call. The one patient in the expedited transport group that achieved ROSC prior to ECPR died during hospitalization due to post-cardiac arrest brain injury.
The 5 patients that were ECPR eligible were all cannulated and had CPR flow initiated (Table 3). Three survived to hospital admission. Of the two that did not survive to hospital admission, one developed hemorrhagic shock from internal bleeding and the family declined operative intervention, and the other had inadequate ECPR flow despite appropriate cannula placement confirmed by autopsy. Of the 3 patients admitted to the hospital, two died from post-cardiac arrest brain injury (one of which met brain death criteria), and the third patient died from multiorgan failure despite initially recovering ability to follow commands.
Table 3 -.
Characteristics and clinical outcomes of subjects with ECPR
| Initial Rhythm | Witnessed | Bystander CPR | 911 call to ECPR flow interval (min) | ECPR Duration (hours) | Cause of Death |
|---|---|---|---|---|---|
| PEA | Yes | Yes | 56 | 92.2 | Post-cardiac arrest brain injury |
| PEA | Yes | Yes | 60 | 6.7 | Hemorrhagic shock |
| Asystole | Yes | No | 73 | <1 | Sudden cardiac death |
| VF | Yes | Yes | 50 | 112.8 | Multi-organ failure |
| VF | Yes | No | 92 | 27 | Brain death |
ECPR = Extracorporeal cardiopulmonary resuscitation, VF = Ventricular fibrillation, PEA = Pulseless electrical activity, ROSC = return of spontaneous circulation, ED = Emergency Department
The time intervals for the standard care group are reported in Supplemental Material 4. All 3 standard care patients had a shockable rhythm (Table 1). None had a 911 call to ED arrival time interval of less than 30 minutes, and none received ECPR. One standard care patient survived to hospital discharge and had a 90-day mRS of 5 and 90-day CPC of 3. Neuro-QOL battery and cognitive functioning using the NIH-Toolbox could not be performed due to patient condition.
Harms
There were no unanticipated complications during the study. There were 3 protocol deviations. Three subjects with an unwitnessed non-shockable rhythm were transported to the ED with mechanical CPR in progress. One of these subjects was originally reported as witnessed and subsequently determined to be unwitnessed. These patients were excluded from the study as they did not meet inclusion criteria.
Limitations
Main limitation of this study is the small sample size due to lower than expected recruitment. This gave us less information to evaluate the precision of the estimates of 911 call to ED arrival interval, and the feasibility of consistently achieving an ED arrival to ECPR interval ≤30 minutes. With only 5 patients in the expedited transport group treated with ECPR, we also have an inadequate sample size to inform the impact of ECPR on OHCA patient outcomes given the 95% confidence interval of a 0/5 survival rate is 0%−43%. It is also notable that only 3 patients had ECPR initiated within 60 minutes of the 911 call and only 2 patients treated with ECPR had an initial shockable rhythm. Most other OHCA ECPR case series and ongoing clinical trials15,19–21 only include patients with an initial shockable rhythm. Furthermore, this study was not powered to examine the safety of expedited transport versus standard resuscitation in the field. However, the rate of ROSC (2/3) in the standard care group suggests that there is equipoise for randomization in future trials. Expedited transport for ECPR may result in higher or lower rates of survival.
Generalizability of our findings is limited due to performance at a single site. The population density (4,408.9/mi2), median age (27.5 years), and traffic patterns of our primary catchment area could be significantly different from other systems performing ECPR for OHCA. In addition, the ED personnel available to participate in initiating ECPR at our large academic medical center could differ significantly from other academic and non-academic EDs.
Discussion
In this study, we evaluated the feasibility of using a real-time estimate of the 911 call to ED arrival interval to determine eligibility for expedited transport of refractory OHCA patients to an ECPR-capable ED. However, the accuracy of our methodology was less than our desired goal of 80% of patients arriving within the estimated interval. Table 2 illustrates that our fixed 5-minute estimate of 911 call to paramedic arrival time, based on historical averages, was relatively close to the overall mean of 6.9 minutes. However, there were two cases in which arrival time was > 10 minutes.
Identifying the causes of variability in 911 call to ED arrival time and incorporating them into the algorithm could improve the accuracy of the overall estimate. Our fixed scene time estimate of 8 minutes, which was based on expedited transport simulations by first responders and paramedics in our system, underestimated the average scene time by 11.7 minutes. Moreover, the variability of the scene time, ranging from 7 to 29 minutes, suggests that using a fixed time interval will severely limit the accuracy of the overall estimate. The sources of this variability are likely to be multifactorial and require additional investigation. If causes of variability can be identified that can also be known at the time the estimate is performed, these could be built into the algorithm to improve accuracy. Finally, the estimated transport time based on Google Maps consistently overestimated transport time by an average of 5.7 minutes. Based on these results, a modified algorithm would be improved by accounting for this systematic overestimation in predicted transport times.
A lower than expected number of patients were eligible for prehospital enrollment and ECPR in this study. In our model, the majority of patients in the expedited transport group were not eligible for ECPR. This is in part due to the fact that we did not expect paramedics in the field to accurately identify many of the exclusion criteria for ECPR, and some exclusion criteria developed during or after transport. Although there is the potential to more precisely select patients for expedited transport, any future study or clinical implementation of an expedited transport protocol will likely include a significant number of patients transported who are ultimately not ECPR candidates.
The accurate prediction of potential eligible subjects will be important for future studies. Reasons for prehospital exclusion not accounted for in our pre-trial estimates included early ROSC (n=6), unable to use mechanical CPR (n=1), cardiac arrest not recognized by dispatch (n=1), and randomization failure (n=1). The reasons that 7 of 12 patients in the expedited transport group were not eligible for ECPR would have been difficult to predict based on historical data. Given our small sample size, the external validity of this point estimate is limited.
We also evaluated the feasibility of trained emergency physicians initiating ECPR in the ED for refractory OHCA patients. However, only 3 out of 5 patients achieved the goal of initiating ECPR within 30 minutes, which fell short of our benchmark targeting 80% of cases. Despite the fact that emergency physicians trained in ECPR cannulation participated in quarterly simulations to maintain skills, the low incidence of study cases could have limited the ability to optimize ED arrival to ECPR flow times.
Conclusion
EROCA did not meet predefined feasibility outcomes for selecting OHCA patients for expedited transport and initiating ECPR in the ED. The majority of subjects transported did not meet eligibility criteria for ECPR. These results provide important insight into the feasibility of ECPR clinical trials and clinical practice based on selected target intervals. Additional research is needed to improve the accuracy of predicting the 911 to ED arrival interval, optimize patient selection, and reduce the ED arrival to ECPR flow interval.
Supplementary Material
Acknowledgements
The authors would like to acknowledge Fire Departments of the City of Ann Arbor, Scio Township, Ann Arbor Township, and Saline Area, Huron Valley Ambulance paramedics and dispatchers, the Washtenaw/Livingston Medical Control Authority, and Michigan Medicine Adult Emergency Department nurses and physicians for their assistance with this study. The authors would also like to acknowledge the regulatory support from the Michigan Institute for Clinical and Health Research IND/IDE Investigator Assistance Program. LUCAS mechanical CPR devices were provided to the Ann Arbor Fire Department by Jolife AB/Stryker (Lund, Sweden) for the duration of this study.
Funding and Support
This study was supported by a grant from the National Heart Lung and Blood Institute (R34 HL130738) and the National Center for Advancing Translational Sciences (UL1 TR002240). CHH was supported by a research grant K12HL133304–01 from the National Institutes of Health.
Grant: This study was supported by a grant from the National Heart Lung and Blood Institute (R34 HL130738) and the National Center for Advancing Translational Sciences (UL1 TR002240). CHH was supported by a research grant K12HL133304–01 from the National Institutes of Health.
Footnotes
Conflicts of interest: RWN reports equipment support for laboratory research from Physio-Control.
Meetings: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Flipbook. Accessed October 1, 2020. https://mycares.net/sitepages/uploads/2020/2019_flipbook/index.html?page=1
- 2.Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation. 2018;137(12):e67–e492. [DOI] [PubMed] [Google Scholar]
- 3.CARES Summary Report Demographic and Survival Characteristics of OHCA. https://mycares.net/sitepages/uploads/2020/2013-2019%20NonTraumatic%20National%20Summary%20Report.pdf [Google Scholar]
- 4.Holmberg MJ, Geri G, Wiberg S, et al. Extracorporeal cardiopulmonary resuscitation for cardiac arrest: A systematic review. Resuscitation. 2018;131:91–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagao K, Kikushima K, Watanabe K, et al. Early induction of hypothermia during cardiac arrest improves neurological outcomes in patients with out-of-hospital cardiac arrest who undergo emergency cardiopulmonary bypass and percutaneous coronary intervention. Circ J. 2010;74(1):77–85. [DOI] [PubMed] [Google Scholar]
- 6.Chen Y-S, Lin J-W, Yu H-Y, et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet. 2008;372(9638):554–561. [DOI] [PubMed] [Google Scholar]
- 7.Kagawa E. Extracorporeal cardiopulmonary resuscitation for adult cardiac arrest patients. World Journal of Critical Care Medicine. 2012;1(2):46. doi: 10.5492/wjccm.v1.i2.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nagao K, Hayashi N, Kanmatsuse K, et al. Cardiopulmonary cerebral resuscitation using emergency cardiopulmonary bypass, coronary reperfusion therapy and mild hypothermia in patients with cardiac arrest outside the hospital. J Am Coll Cardiol. 2000;36(3):776–783. [DOI] [PubMed] [Google Scholar]
- 9.Le Guen M, Nicolas-Robin A, Carreira S, et al. Extracorporeal life support following out-of-hospital refractory cardiac arrest. Crit Care. 2011;15(1):R29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sakamoto T, Asai Y, Nagao K, et al. Extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest. Resuscitation. 2010;81(2):S62. doi: 10.1016/j.resuscitation.2010.09.258 [DOI] [PubMed] [Google Scholar]
- 11.Lamhaut L, Jouffroy R, Kalpodjian A, et al. Successful treatment of refractory cardiac arrest by emergency physicians using pre-hospital ECLS. Resuscitation. 2012;83(8):e177–e178. [DOI] [PubMed] [Google Scholar]
- 12.Johnson NJ, Acker M, Hsu CH, et al. Extracorporeal life support as rescue strategy for out-of-hospital and emergency department cardiac arrest. Resuscitation. 2014;85(11):1527–1532. [DOI] [PubMed] [Google Scholar]
- 13.Sakamoto T, Morimura N, Nagao K, et al. Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with out-of-hospital cardiac arrest: a prospective observational study. Resuscitation. 2014;85(6):762–768. [DOI] [PubMed] [Google Scholar]
- 14.Stub D, Bernard S, Pellegrino V, et al. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial). Resuscitation. 2015;86:88–94. [DOI] [PubMed] [Google Scholar]
- 15.Bartos JA, Grunau B, Carlson C, et al. Improved Survival With Extracorporeal Cardiopulmonary Resuscitation Despite Progressive Metabolic Derangement Associated With Prolonged Resuscitation. Circulation. 2020;141(11):877–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boudoulas KD, Whitson BA, Keseg DP, et al. Extracorporeal Cardiopulmonary Resuscitation (ECPR) for Out-of-Hospital Cardiac Arrest due to Pulseless Ventricular Tachycardia/Fibrillation. J Interv Cardiol. 2020;2020:6939315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whitmore SP, Gunnerson KJ, Haft JW, et al. Simulation training enables emergency medicine providers to rapidly and safely initiate extracorporeal cardiopulmonary resuscitation (ECPR) in a simulated cardiac arrest scenario. Resuscitation. 2019;138:68–73. [DOI] [PubMed] [Google Scholar]
- 18.Arbor Ann, Population Michigan 2020. (Demographics, Maps, Graphs). Accessed October 1, 2020. https://worldpopulationreview.com/us-cities/ann-arbor-mi-population [Google Scholar]
- 19.Haas NL, Coute RA, Hsu CH, Cranford JA, Neumar RW. Descriptive analysis of extracorporeal cardiopulmonary resuscitation following out-of-hospital cardiac arrest-An ELSO registry study. Resuscitation. 2017;119:56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tonna JE, Selzman CH, Girotra S, et al. Patient and Institutional Characteristics Influence the Decision to Use Extracorporeal Cardiopulmonary Resuscitation for In-Hospital Cardiac Arrest. J Am Heart Assoc. 2020;9(9):e015522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grunau B, Reynolds J, Scheuermeyer F, et al. Relationship between Time-to-ROSC and Survival in Outof-hospital Cardiac Arrest ECPR Candidates: When is the Best Time to Consider Transport to Hospital? Prehospital Emergency Care. 2016;20(5):615–622. doi: 10.3109/10903127.2016.1149652 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.