Abstract
Purpose:
To qualitatively explore exercise barriers and facilitators experienced by rural female cancer survivors from the program interventionist and recipient perspective for the purpose of enhancing exercise program implementation and uptake in rural settings.
Methods:
A descriptive qualitative study design was utilized. Focus groups were conducted prior to implementation of an evidence-based exercise program by a rural non-research cancer clinical site. Nineteen rural female cancer survivors (mean age = 61.7 ± 10.9 years) and 11 potential interventionists (mean age = 42.3 ± 15.3 years) completed focus groups (stratified by participant role). Focus groups were audio recorded, transcribed, coded, and analyzed using inductive thematic analysis with NVivo 11.
Results:
Cancer survivors identified twelve barrier themes (cancer specific adverse effects, lack of support, lack of knowledge, perceived negative aspects of exercise, cost, lack of resources, motivation, inconvenience, lack of program flexibility, time, weather, safety) and eight facilitator themes (knowledge, ease of access, resources, awareness, cost, options, organized, fun) related to exercise. Interventionists identified seven barrier themes (cost, transportation, lack of cancer survivor and interventionist knowledge, fear, motivation, lack of support, lack of resources) and four facilitator themes (resources, support, knowledge, motivation). Narratives revealed differing role-specific perspectives on shared themes between survivors and interventionists as well as potential implementation strategies for enhancing exercise participation and exercise program uptake among rural female cancer survivors.
Conclusion:
Exploring multi-level stakeholder perspectives on cancer survivors’ exercise needs and related strategies yields important information for organizations to consider when implementing exercise programs in rural contexts.
Keywords: oncology, exercise, rural women, qualitative
Introduction
Across the cancer continuum, cancer survivors experience a range of symptoms and side effects that negatively impact their physical health, mental health, and overall well-being. Exercise is a therapeutic intervention capable of mitigating these effects, having been shown to reduce cancer survivors’ depressive symptoms and anxiety, and to improve physical functioning and quality of life [1–3]. Yet, a large portion of cancer survivors do not meet recommended exercise guidelines [4,5]. Rural cancer survivors are disproportionately affected, experiencing higher physical inactivity and mortality rates than their urban counterparts [6,7]. Furthermore, rural female cancer survivors are more likely to develop depression, anxiety, and report lower overall well-being than their urban peers [8,9]. Given this knowledge, it is clear that a large portion of cancer survivors are not receiving the benefits that exercise and evidence-based exercise programs can provide. To address this, recommendations have called for more collaborative, integrative, context-based approaches to exercise program design, implementation, and translation, especially as it relates to program settings and demographics [10]. Rural female cancer survivors could particularly benefit from these approaches as rural health inequities and settings pose additional challenges and considerations for effective delivery of exercise programs to this population [11–13].
Previous studies have aimed to quantitatively and qualitatively inform rural exercise program delivery through identification of barriers and facilitators to exercise from the perspective of the rural cancer survivor [14–16]. However, exercise program design and delivery are multi-faceted, often requiring the input and efforts of multiple stakeholders. As key stakeholders in the collaborative process, interventionists are often intimately familiar with program setting, demographics, and resources. However, few, if any, studies have qualitatively explored barriers and facilitators to exercise among rural cancer survivors from the perspective of individuals who may ultimately implement the program [14]. Including the perspective of potential interventionists in planning exercise programs for rural female cancer survivors may better inform future exercise program design and implementation strategies. Additionally, interventionist perspectives, when juxtaposed with cancer survivor perspectives, may provide additional contextual data that could further enhance understanding of previously reported exercise barriers and facilitators. Therefore, this study sought to examine exercise barriers and facilitators experienced by rural female cancer survivors through qualitative analysis of multiple stakeholder perspectives as a component of moving an evidence-based exercise program from an academic (research) to a rural community (non-research) setting.
Methods
Participants
Cancer survivors were women with a history of cancer (any type, stage, or time since diagnosis) at any time post-primary treatment who were able to participate in the planned exercise program (e.g., able to ambulate without assistance, denied contraindication to moderate intensity exercise, able to obtain physician clearance for exercise). We did not limit to a specific cancer type or time since primary treatment given the understanding that exercise programs implemented and translated in under-resourced rural settings would likely avoid participation limitations that would exacerbate the limited access already present and reduce the impact of the limited resources used. Interventionists were adults qualified to implement aspects of the program (i.e., fitness professionals, discussion group leaders, etc.). Additional inclusion criteria for cancer survivors and potential interventionists included age ≥18 years, English speaking, no history of dementia or organic brain syndrome, and intact hearing. Additionally, survivors and interventionists could not have a significant medical, psychological, or social characteristics that would hinder their ability to fully participate in or deliver the exercise program, respectively. All participants lived or worked in/or adjacent to the rural county in the Southeastern United States in which the planned program translation and implementation was to occur (i.e., Rural-Urban Continuum Code [RUCC] classification of 8 or 9) [17]. This designation indicates the county was classified as a completely rural or <2,500 urban population and either adjacent to a metro area (RUCC = 9) or not (RUCC =8). Survivor and interventionist recruitment activities included referrals from local rural cancer center leaders, staff, and project champion. Cancer survivors were also recruited using local news ads and letters sent to potential participants identified through an institutional cancer registry.
Focus Group Procedure
Focus groups were conducted at or near a rural community hospital in which the planned program was to take place. Focus groups were comprised exclusively of interventionists (2 groups) or rural female cancer survivors (3 groups). Each participant completed one focus group based on their respective role. Focus group guides were developed and iteratively revised following established guidelines by a coauthor experienced in focus group design and qualitative data in conjunction with other investigators [18,19]. Participants completed a demographic survey before initiating the focus group. A trained research staff member used the focus group guide (including, but not limited to, questions and prompts) to facilitate focus group discussions with a secondary staff member present to take notes to clarify any segments of the recordings that were difficult to hear. Cancer survivors were asked their general thoughts regarding exercise and tasked specifically about the availability of exercise promoting resources, health and exercise information of greatest interest, and concerns related to exercise for cancer survivors in their area.
The program being prepared for implementation was then described to cancer survivors (12-week program; 12 supervised exercise sessions with an exercise specialist during the first six weeks that are gradually tapered to unsupervised and more home-based exercise; follow-up exercise counseling every two weeks during the unsupervised exercise weeks; six discussion group sessions; goal of 150 weekly minutes of exercise) [20]. Cancer survivors were then asked about their general thoughts regarding participation in the exercise program including potential concerns, reasons for participation, and how the program could work best for cancer survivors in their area. Interventionists were asked to identify things they perceived as promoting or discouraging exercise in cancer survivors in their area (note: most interventionists were aware of the planned program aspects). Focus group sessions were audio recorded and transcribed verbatim.
Data Analyses
Qualitative data was managed and analyzed using NVivo 11, a qualitative data analysis software system. Two research staff trained in qualitative analysis established a codebook based on initial transcript readings and coding of focus group transcripts. A directed, inductive content analysis approach [21] was utilized to code themes within 2 broad categories, barriers and facilitators. Coding was iteratively discussed, and Kappa coefficients were calculated utilizing NVivo 11, resulting in inter-coder agreements of 0.70 (cancer survivor data) and 0.74 (interventionist data). Relative frequency of themes was calculated separately for cancer survivors and interventionists. A post hoc decision was made by researchers to analyze and report potential exercise program strategies identified by participants within barrier and facilitator themes. Participant characteristics were gathered from demographic surveys and are presented using descriptive statistics that were obtained through the use of SAS software (version 9.4; SAS institute, Cary, NC).
Results
Participants
A total of 19 female cancer survivors participated in focus groups. Cancer survivor participants had a mean age of 61.7 ± 10.9 years and were a mean of 33.2 ± 21.5 months from their cancer diagnosis. A total of eleven potential interventionists participated in focus groups. Nine interventionists were female and two were male. The average age of interventionists was 42.3 ± 15.3 years. Further participant characteristics can be found in Table 1.
Table 1.
Interventionists and Rural Female Cancer Survivor Characteristics
| Variable | Interventionists (n=11) |
Cancer survivors (n=19) |
|---|---|---|
| Age (years) [mean ± SD] | 42.3 ±15.3 | 61.7 ± 10.9 |
| Ethnicity [no. (%)] | ||
| Non-Hispanic/Latino | 11 (100) | 19 (100) |
| Race [no. (%)] | ||
| White/Caucasian | 11 (100) | 16 (84.2) |
| African-American | 0 (0) | 3 (15.8) |
| Gender [no. (%)] | ||
| Female | 9 (81.8) | 19 (100) |
| Male | 2 (18.2) | 0 (0) |
| Education [no. (%)] | ||
| ≤ 12 years | 1 (9.1) | 5 (26.3) |
| > 12 years | 10 (90.9) | 14 (73.7) |
| Annual Household Income [no. (%)]a | ||
| < $20,000 | 1 (9.1) | 4 (25.0) |
| $20,000 to <$50,000 | 2 (18.2) | 4 (25.0) |
| ≥ $50,000 | 8 (72.7) | 8 (50.0) |
| Employed (yes) [no. (%)] | --- | 7 (36.8) |
| Marital Status [no. (%)] | ||
| Married/living with significant other | 9 (81.8) | 13 (68.4) |
| Other | 2 (18.2) | 6 (31.6) |
| Cancer Type [no. (%)] | --- | |
| Breast | 10 (52.6) | |
| Ovarian | 2 (10.5) | |
| Uterine | 2 (10.5) | |
| Bladder | 2 (10.5) | |
| Lung | 2 (10.5) | |
| Melanoma | 1 (5.3) | |
| Months since cancer diagnosis [mean ± SD] | --- | 33.2 ± 21.5 |
| History of chemotherapy (yes) [no. (%)] | --- | 14 (73.7) |
| History of Radiation (yes) [no. (%)] | --- | 12 (63.2) |
| Smoker [no. (%)] | --- | |
| Never | 16 (84.2) | |
| Ex-smoker | 3 (15.8) | |
| Current smoker | 0 (0) | |
| Alcohol (yes) [no. (%)] | --- | 8 (42.1) |
| Distance from home to planned program implementation site (miles) [mean + SD] | 22.7 ± 18.7 | 19.8 ± 18.2 |
| Works at planned implementation site | 7 (70.0) (n=10) |
--- |
The 3 cancer survivors who did not provide this information were excluded from the statistical analysis of this variable.
Cancer Survivor Barriers
Rural female cancer survivors felt several factors impeded their participation in exercise and exercise programs. Analysis revealed twelve barrier themes: cancer specific adverse effects, lack of knowledge, lack of support, perceived negative aspects of exercise (e.g., intimidation, pain, futility), cost related to exercise (especially within the context of the financial hardships caused by cancer), lack of resources (e.g., exercise professionals with expertise related to cancer-specific exercise, physical location), lack of motivation to exercise, inconvenient (related to time and travel distance required), lack of program flexibility (with regard to timing and location), lack of time, weather, and safety (e.g., access to medical services, trained professionals nearby). Relative frequency is represented in Figure 1 as percent of coded text. For practical reasons, we provide more detail for the three most referenced barrier-related themes. See online resource 1 for detail and illustrative quotes for remaining themes.
Fig. 1.
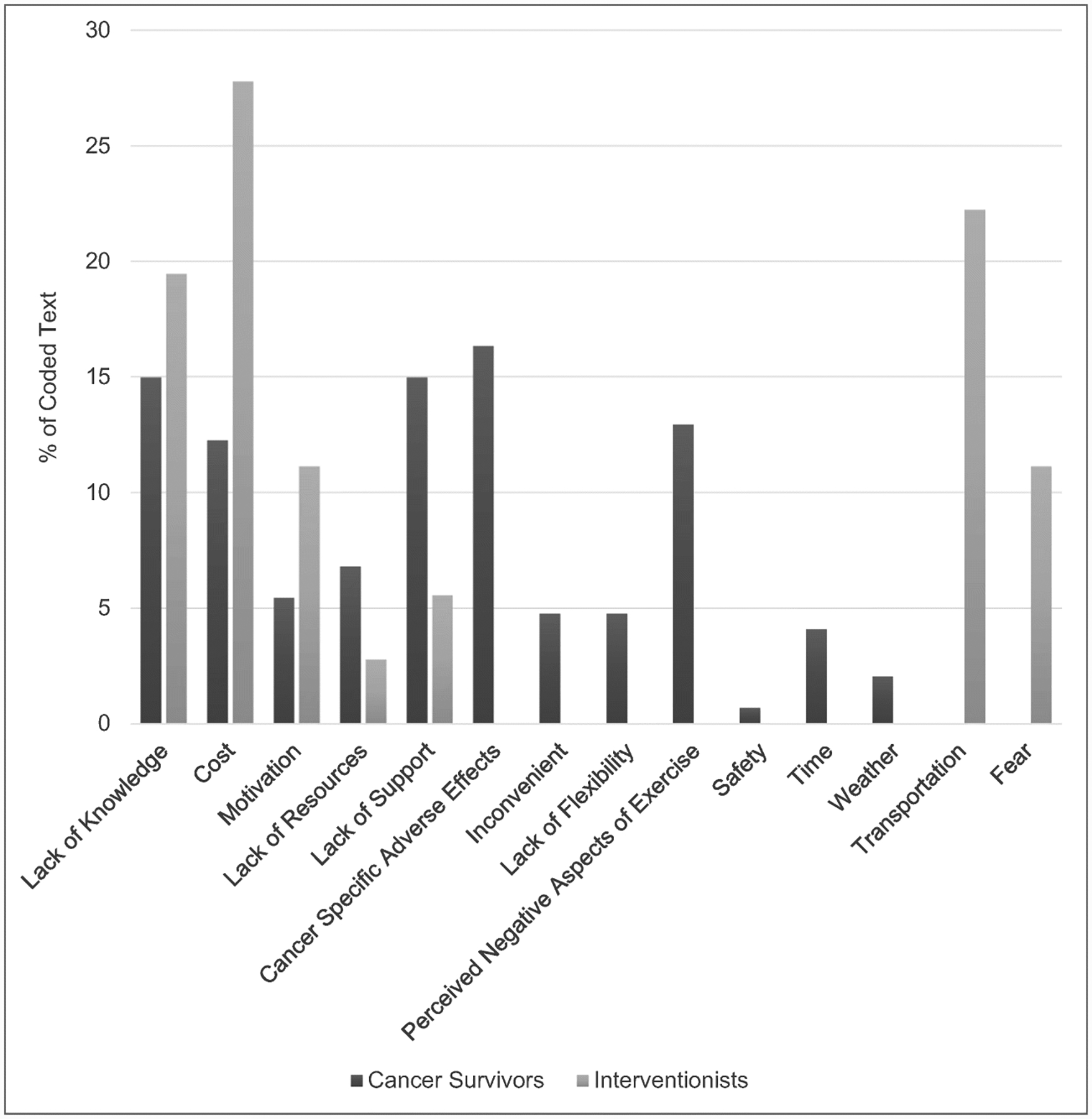
Barriers identified during cancer survivor and interventionist focus groups: Percent of coded text attributed to each barrier
Cancer Specific Adverse Effects
Both physical and psychological cancer specific adverse effects were identified by cancer survivors as barriers to exercise. These side effects included loss of balance, fatigue, decreased strength, and “brain fog” among others. Additionally, survivors referenced the unmet expectation of returning to their pre-treatment physical fitness level and trouble coping with their exercise limitations after treatment.
“I kept feeling like it should be better now. I should be back to myself by now… but I just don’t feel like that energy is coming back.”
Lack of Knowledge
Lack of knowledge encompassed a wide array of knowledge types including exercise, technology competency, and knowledge of local resources. Cancer survivors identified a dearth of survivor and fitness professional knowledge regarding cancer survivor specific exercise. They also cited a lack of education by healthcare teams regarding survivorship, including post-treatment exercise. Survivors noted a perceived expectation by healthcare teams that they would utilize technology to obtain exercise information independently. Technologic competency and anxiety associated with finding unwanted or incorrect information regarding their disease online were indicated as barriers to this approach. Cancer survivors also discussed the isolation characteristic of rural areas contributing to inadequate survivor knowledge of local resources.
“We tend to be kind of isolated there…So getting the information would be something we would need to think about.”
Lack of Support
Cancer survivors perceived a lack of support regarding participation in exercise from their friends, family, and medical teams. They highlighted a lack of understanding among loved ones regarding post-treatment physical limitations, a lack of exercise focused guidance and support from medical teams post-treatment, and absence of accessible survivor support groups.
“you know, my girlfriends are like ‘uh, XXX, you used to have so much energy’… hello, I had cancer. You know, I have to keep reminding her.”
Cancer Survivor Facilitators
Analysis revealed eight themes regarding facilitators to participation in exercise and exercise programs among rural cancer survivors. These themes included knowledge, ease of access, resources, awareness (e.g., advertising exercise program through media outlets, end of treatment exercise discussions with medical team), cost, options (e.g., range of exercise offerings based on fitness level, multiple time options), organized (e.g., small groups, instructors), and fun. Relative frequency is represented in Figure 2 as percent of coded text. The three most commonly referenced themes are presented below. See online resource 1 for descriptions of remaining themes and illustrative quotes.
Fig. 2.
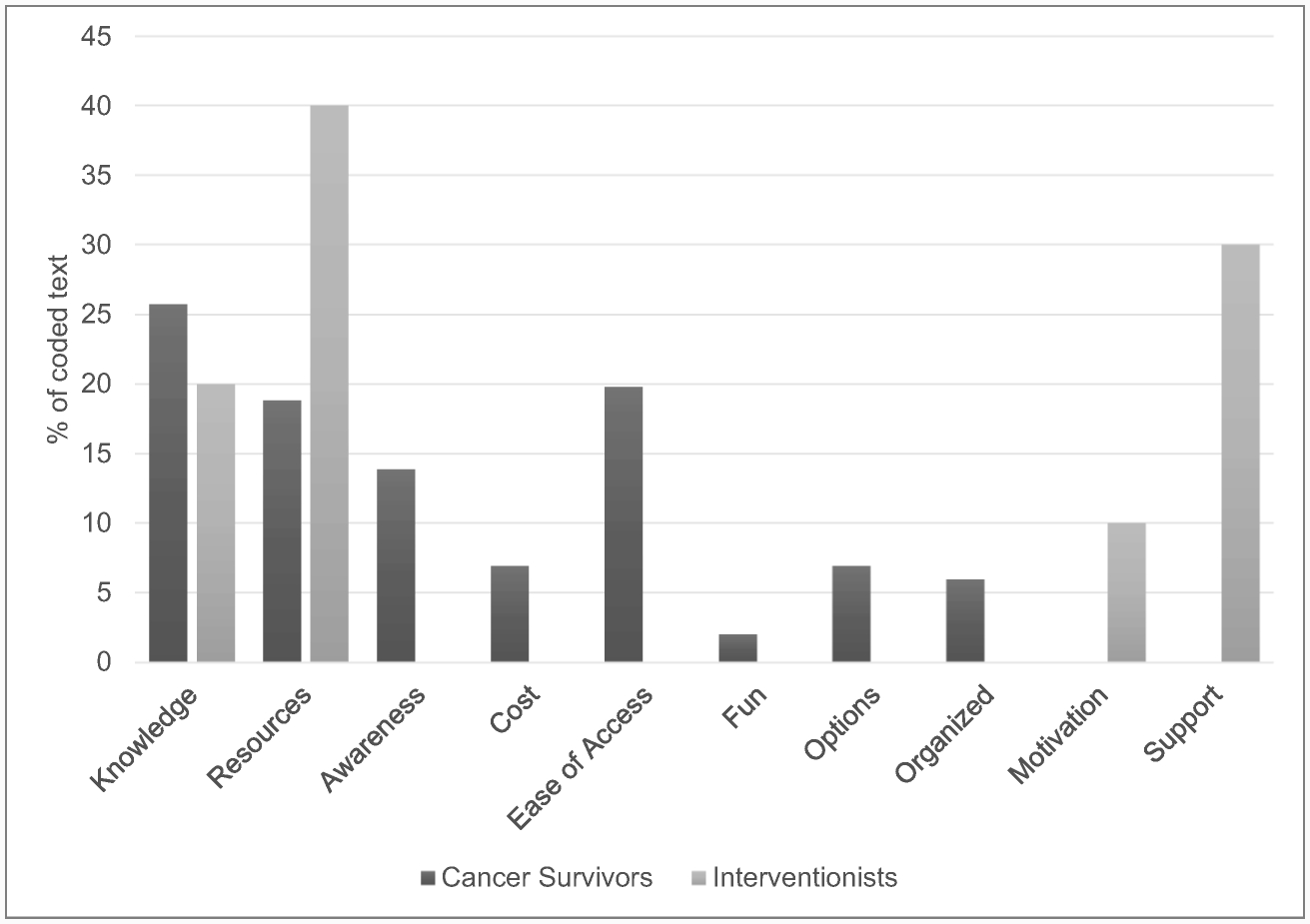
Facilitators identified during cancer survivor and interventionist focus groups: Percent of coded text attributed to each facilitator.
Knowledge
Knowledge was the most frequently referenced facilitator. This theme encompassed a wide array of knowledge types (e.g., information on cancer survivor specific diet and exercise, benefits of exercise for cancer survivors, mental health information, survivors’ personal experiences) as adding value to the exercise program for survivors.
“if you bring it on up and let them know that this can happen and you can… and people have survived cancer.”
Ease of Access
Cancer survivors noted ease of access to facilities, organized activities, supervision, medical professionals in case of injury, and home-based workout plans as exercise facilitators.
“Convenience, it’s right at home…I just had a lot of great luck with the apps.”
Resources
Safe, local exercise facilities in addition to experienced exercise program leadership, such as exercise trainers, were identified as resources facilitating exercise among cancer survivors.
“two churches in the area have indoor walking tracks. So, instead of getting your religion, you are getting your exercise and physical too.”
Interventionist Barriers
Interventionists identified seven themes as barriers to participation in exercise and exercise programs for rural cancer survivors. These themes included cost, transportation, lack of survivor and interventionist knowledge, fear (e.g., fear resulting from cancer “scare,” perceived inability to complete exercises), lack of motivation (decreased motivation to exercise after formal program completion), lack of support (e.g., medical team support, loss of fitness group support post-program) and lack of resources (e.g., athletic clothing, sidewalks). Relative frequency is represented in Figure 1 as percent of coded text. The three most commonly referenced themes are detailed here. Remaining themes and their respective illustrative quotes are detailed in online resource 1.
Cost
Cost was the most frequently mentioned barrier among interventionists. Interventionists cited participant costs such as childcare, transportation, membership fees, and athletic attire as components of the cost barrier. A need for strategies aimed at reducing the costs of participation for cancer survivors was also discussed.
“if they wanted to have a gym membership afterwards, which is a monthly fee, it would be very difficult and very challenging if they are already concerned about fuel.”
Transportation
Interventionists highlighted the added transportation burden that rural cancer survivors faced in getting to exercise programs or facilities. Rural cancer survivors’ access to public transportation is limited and survivors are often responsible for finding and paying for transportation.
“They rely on someone to take them to appointments or to, if they were going to exercise, they would have to have someone drop them off and pick them up and it is not very convenient.”
Lack of Knowledge
Interventionists identified lack of exercise knowledge among cancer survivors as a major barrier. They attributed this to inadequate survivorship education by cancer survivors’ medical teams. Interventionists also discussed their own lack of knowledge regarding exercising with cancer survivors, especially as it relates to individual types of cancers.
“I know there is a lot more that can be determined, because with all the different kinds of cancers that are out there, you know, it’s hard to find a good starting point and it has to be very individualized…”
Interventionist Facilitators
Resources, support, knowledge, and motivation (e.g., verbal follow-up from program leadership, accountability within fitness groups) were identified as facilitators to exercise participation in rural cancer survivors. Relative frequency is represented in Figure 2 as percent of coded text. The resource, support, and knowledge themes are detailed below. See online resource 1 for motivation theme details and an illustrative quote.
Resources
Resources was the most referenced facilitator by interventionists. They highlighted the need for community exercise events and centrally located medical and non-medical exercise facilities. They also referenced partnerships between medical and fitness professionals as a further resource that could prove beneficial in promoting exercise participation.
“several of the churches in town have indoor walking tracks that people go to exercise as well and we are also located right on the lake so lots of people enjoy going down to the lake and swimming or using hiking trails and biking…”
Support
Interventionists cited support as a facilitator, highlighting cancer survivor support groups and community support through transportation options and community sponsored exercise events.
“We see every day, if you can get a group together to do something exercise wise, you have that accountability, you have that support for each other no matter what you’ve gone through.”
Knowledge
Interventionists discussed knowledge of the exercise program among cancer survivors and healthcare providers as a facilitator of program engagement and recruitment. They indicated cancer survivor knowledge of the program and its benefits, emphasizing survivors’ regaining some level of physical functioning or lifestyle prior to their cancer diagnosis, as a facilitator. Interventionists also mentioned educating physicians on the program in order to gain their support. One interventionist highlighted the importance of gaining buy-in from local primary care physicians as cancer survivors often return to these physicians after their primary cancer care.
“our patients are going to do what their doctor says and that’s just what they do…It’s not just centered around the oncologist, it’s really about your primary and the internist in the area as well. Getting them on board.”
Insight into Identified Strategies
In analyzing the data, researchers noted that focus group participants identified strategies for addressing exercise barriers and facilitators. In regard to cancer specific adverse effects, participants emphasized training interventionists on appropriate exercises for survivors based on their cancer type and symptoms. To facilitate awareness, ease of access, and knowledge among cancer survivors, post-treatment exercise discussions, use of accessible, free technology like smartphone applications, and inclusion of mental health components, such as anxiety and depression counseling groups, within exercise programs were suggested, respectively. Obtaining funding from external agencies and patient scholarships were also suggested to address cost and financial resource limitations. In addressing lack of flexibility and travel inconvenience barriers, one cancer survivor indicated a desire for programs to prepare survivors to exercise independent of the program implementation site. Local newspaper articles were also proposed as a more effective form of facilitating exercise program awareness than newspaper ads. Finally, framing exercise as a component of a patient care plan was suggested to increase exercise participation among rural cancer survivors.
Discussion
Our qualitative data is best discussed within the perspective of population-based quantitative studies in rural cancer survivor populations [15, 16, 22, 23, 24, 25]. These larger cohort studies have identified that greater physical activity is associated with better quality of life (including but not limited to physical functioning) [22], fewer perceived exercise barriers, greater confidence in overcoming these barriers [23], and more exercise facilitators (e.g., resources) [15]. Having identified the presence and importance of exercise barriers and facilitators, these studies also acknowledge a need to better understand these barriers and facilitators in more detail [24], a need addressed by the contextual exploration reported here.
To exemplify, several barrier themes have been reported in population-based survey studies (e.g., cost, fatigue, lack of interest or motivational issues, etc.) [14, 16, 24, 25]. However, our contextual exploration indicates that reducing cost goes beyond providing a free exercise program since cancer survivors may not be able to afford childcare or appropriate clothing due to the financial burden of a cancer diagnosis and its treatment. Targeting fatigue as a barrier should consider both physical fatigue and the detrimental psychological impact of unmet survivor expectations regarding fatigue post-treatment. Similarly, our data suggest survivors’ lack of interest or motivational issues may stem from multiple factors such as physical limitations (e.g., fatigue, “getting winded”, etc.), inability to exercise in their preferred setting (e.g., not on a treadmill, outdoors), perceived futility of exercise in cancer recurrence prevention, and other personal factors (e.g., loss of loved ones).
With regard to facilitators, prior quantitative studies have suggested offering a variety of programming options and consider alternative methods of offering these options in resource-limited rural settings [15, 16]. Our study supports and further informs these findings with survivors describing a desire for exercise options that accommodate different physical functioning abilities and identifying alternative exercise locations (e.g., churches) for facilitating these options in rural communities. Prior studies have also proposed the use of technology-based strategies (smartphone applications, internet, electronic mail) for delivering exercise programming to survivors [16, 24]. Data described here revealed one survivor viewed the use of certain technologies such as guided exercise smartphone applications as beneficial when inexpensive. However, survivors had reservations regarding independent internet usage to acquire exercise knowledge given concerns about technology competency and reliability of the cancer-related information.
Also related to facilitating exercise, previous quantitative surveys have reported wide variability in exercise program preferences among cancer survivors yet underlying reasons for preference differences have not been elucidated [25]. In our study, survivors describe intimidation in gym settings and embarrassment at being “shown up” by others which suggests preferences may be indicators of underlying factors that should be considered in program design. This is important because a majority of rural cancer survivors have indicated a preference to be physically active at a community fitness center [16] and targeting potential intimidation and embarrassment may optimize this resource. Additionally, some survivors preferred home-based exercise or programming at community centers that prepared them to exercise independently at home, a nuance not previously detected in quantitative survey studies.
This study is unique in its inclusion of interventionist perspectives which, to our knowledge, has not been done previously. Interventionists identified implementation barriers and facilitators not mentioned by survivors (e.g., interventionist lack of knowledge regarding how to individualize regimens for specific cancer types, garnering physician buy-in outside of the oncology team, etc.). Notably, interventionists and survivors often offered differing viewpoints on the same barriers and facilitators (e.g., interventionists predominantly focused on long term maintenance when discussing motivation barrier while cancer survivors focused on initial engagement). Hence, multi-level input provided additional detail relevant to addressing barriers and enhancing facilitators of exercise in rural cancer survivors.
The data reported here have several implications and suggest areas for future application and research. Similar to other studies [14], narratives pointed towards a need for reframing the cancer survivorship dialogue between medical professionals, patients, and their families to include a greater emphasis on exercise as a component of survivorship. This could potentially include education on post-treatment physical limitations and education of both survivors and interventionists on how to safely incorporate cancer-specific exercise into survivors’ routines. The lack of medical team support cited by participants further indicates the need for training regarding exercise and its benefits for cancer survivors for all medical professionals (nutritionists, physicians, nurses, therapists, etc.) that work with cancer patients during their primary treatment in order to facilitate these dialogues. Additionally, rural cancer survivors indicated differing preferences in desired travel time and exercise environment (independent home-based, support group, supervised, etc.) suggesting the need for more customization within exercise program design. Given cancer survivors’ perceived value of mental, emotional, and spiritual resources, more holistic approaches may also prove beneficial. Additional important points for consideration in exercise program delivery are collaboration with primary care physicians, available resources in rural communities, and the patient populations’ relationship with technology in regard to how program information is provided.
Our broad inclusion criteria, albeit appropriate for a rural setting, introduced heterogeneity with regard to cancer type and time since treatment which may have influenced study results. In contrast, the inclusion criteria that were used limit generalizability of results beyond cancer survivors who are capable of transportation to the rural program site, live in the rural Southeastern United States, and are female. Furthermore, the majority of cancer survivor focus group participants were breast cancer survivors and data shared here may not be as widely applicable to individuals who have survived cancer types not represented. Although this study did not use large population-based surveys and is limited by its small sample size, the congruence between the major themes discussed here and prior published literature support the relevance of our findings. Also, our qualitative data has expanded our understanding of known barriers and suggested facilitators/strategies in rural female cancer survivors, a historically underserved population. Larger, studies that employ a mixed methods approach (e.g., population-based surveys, subsample qualitative interviews, and possibly physical performance assessments) are needed to better understand the impact of the barriers, facilitators, and strategies discussed here on rural female cancer survivors at large.
Conclusion
This study provides valuable insight into the factors that play a role in decisions to participate in exercise and exercise programs in an understudied and underserved population (rural female cancer survivors). The insights into survivor perspectives regarding previously identified barriers and strategies shared here can inform future program design and implementation strategies targeting the needs of rural cancer survivors. Also, narratives reinforced the value of gaining multi-level stakeholder perspectives regarding implementation of exercise programs in rural contexts. Further research evaluating the effectiveness of survivor and interventionist identified strategies can support the implementation of evidence-based exercise programs and, in so doing, reduce health disparities in this population.
Supplementary Material
Online Resource 1 Description of additional barrier and facilitator themes with illustrative quotes
Acknowledgments:
This work was supported by the National Institutes of Health (R21CA182601, R25CA76023, 5R25MH080916, 3U01 HL133994-02S1, UL1 TR002345, and R01HG009351).
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflicts of interest/Competing interests: All authors declare they have no conflicts of interest.
Ethics Approval: All study procedures involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its amendments or comparable ethical standards. The proposal was approved by the UAB Institutional Review Boards for Human Use.
Consent to participate: Informed consent was obtained from all participants included in the study.
Consent to publish: Informed consent was obtained from all participants included in the study.
Availability of data and material: Data and materials available upon request from the corresponding author.
Code availability: Code available upon request from the corresponding author.
References
- 1.Campbell KL, Winters-Stone KM, Wiskemann J, et al. (2019) Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc. 51(11):2375–2390. 10.1249/mss.0000000000002116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spence RR, Heesch KC, Brown WJ (2010) Exercise and cancer rehabilitation: a systematic review. Cancer Treat Rev. 36(2):185–194. 10.1016/j.ctrv.2009.11.003 [DOI] [PubMed] [Google Scholar]
- 3.Speck RM, Courneya KS, Mâsse LC, Duval S, Schmitz KH (2010) An update of controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. J Cancer Surviv. 4(2):87–100. 10.1007/s11764-009-0110-5 [DOI] [PubMed] [Google Scholar]
- 4.Troeschel AN, Leach CR, Shuval K, Stein KD, Patel AV (2018) Physical Activity in Cancer Survivors During “Re-Entry” Following Cancer Treatment. Prev Chronic Dis. 15:170277. 10.5888/pcd15.170277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blanchard CM, Courneya KS, Stein K (2008) Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: results from the American Cancer Society’s SCS-II. J Clin Oncol. 26(13):2198–204. 10.1200/JCO.2007.14.6217 [DOI] [PubMed] [Google Scholar]
- 6.Weaver KE, Palmer N, Lu L, Case LD, Geiger AM (2013) Rural-urban differences in health behaviors and implications for health status among US cancer survivors. Cancer Causes Control. 24(8):1481–1490. 10.1007/s10552-013-0225-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh GK, Williams SD, Siahpush M, Mulhollen A (2011) Socioeconomic, rural-urban, and racial inequalities in US cancer mortality: part I—all cancers and lung cancer and part II—colorectal, prostate, breast, and cervical cancers. J Cancer Epidemiol. 2011:107497. 10.1155/2011/107497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reid-Arndt SA, Cox CR (2010) Does Rurality Affect Quality of Life Following Treatment for Breast Cancer? The Journal of Rural Health. 26(4):402–405. 10.1111/j.1748-0361.2010.00295.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burris JL, Andrykowski M (2010) Disparities in mental health between rural and nonrural cancer survivors: a preliminary study. Psycho-Oncology. 19(6):637–645. 10.1002/pon.1600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Phillips SM, Alfano CM, Perna FM, Glasgow RE (2014) Accelerating Translation of Physical Activity and Cancer Survivorship Research into Practice: Recommendations for a More Integrated and Collaborative Approach. Cancer Epidemiol Biomarkers Prev. 23(5):687–699. 10.1158/1055-9965.EPI-13-1355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cadmus-Bertram LA, Gorzelitz JS, Dorn DC, Malecki KMC (2020) Understanding the physical activity needs and interests of inactive and active rural women: a cross-sectional study of barriers, opportunities, and intervention preferences. J Behav Med. 43(4):638–647. 10.1007/s10865-019-00070-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seguin R, Connor L, Nelson M, LaCroix A, Eldridge G (2014) Understanding barriers and facilitators to healthy eating and active living in rural communities. J Nutr Metab. 2014(2):146502. 10.1155/2014/146502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olsen JM (2013) An integrative review of literature on the determinants of physical activity among rural women. Public Health Nurs. 30(4):288–311. 10.1111/phn.12023 [DOI] [PubMed] [Google Scholar]
- 14.Clifford BK, Mizrahi D, Sandler CX, et al. (2018) Barriers and facilitators of exercise experienced by cancer survivors: a mixed methods systematic review. Support Care Cancer. 26(3):685–700. 10.1007/s00520-017-3964-5 [DOI] [PubMed] [Google Scholar]
- 15.Rogers LQ, Markwell SJ, Courneya KS, McAuley E, Verhulst S (2009) Exercise preference patterns, resources, and environment among rural breast cancer survivors. J Rural Health. 25(4):388–391. 10.1111/j.1748-0361.2009.00249.x [DOI] [PubMed] [Google Scholar]
- 16.Vallance J, Lavallee C, Culos-Reed NS, Trudeau M (2013) Rural and small town breast cancer survivors’ preferences for physical activity. Int. J. Behav. Med 20(4):522–528. 10.1007/s12529-012-9264-z [DOI] [PubMed] [Google Scholar]
- 17.Economic Research Service (2013) Rural-Urban Continuum Codes. United States Department of Agriculture https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx. Accessed 5 July 2019.
- 18.Krueger RA, Casey MA (2015) Focus groups : a practical guide for applied research. 5th ed. Sage Publications, Thousand Oaks, CA [Google Scholar]
- 19.Morgan DL (1997) Focus groups as qualitative research. 2nd ed. Qualitative research methods series, vol 16. Sage Publications, Thousand Oaks, CA. [Google Scholar]
- 20.Rogers LQ, McAuley E, Anton PM, Courneya KS, Vicari S, Hopkins-Price P, Verhulst S, Mocharnuk R, Hoelzer K (2012) Better exercise adherence after treatment for cancer (BEAT Cancer) study: rationale, design, and methods. Contemp Clin Trials. 33(1):124–37. 10.1016/j.cct.2011.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krippendorff K (2003) Content analysis: an introduction to its methodology. 2nd ed. Sage Publications, Newbury Park, CA [Google Scholar]
- 22.Milne HM, Gordon S, Guilfoyle A, Wallman KE, Courneya KS. (2007) Association between physical activity and quality of life among Western Australian breast cancer survivors. Psychooncology. 16(12):1059–68. 10.1002/pon.1211 [DOI] [PubMed] [Google Scholar]
- 23.Olson EA, Mullen SP, Rogers LQ, Courneya KS, Verhulst S, McAuley E. (2014) Meeting physical activity guidelines in rural breast cancer survivors. Am J Health Behav. 38(6):890–9. 10.5993/ajhb.38.6.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vallance JK, Lavallee CM, Culos-Reed NS et al. (2012) Physical activity is associated with clinically important differences in health-related quality of life among rural and small-town breast cancer survivors. Support Care Cancer. 20:1079–1087. 10.1007/s00520-011-1188-7 [DOI] [PubMed] [Google Scholar]
- 25.Rogers LQ, Markwell SJ, Verhulst S, McAuley E, Courneya KS. (2009) Rural breast cancer survivors: exercise preferences and their determinants. Psycho-Oncology. 18(4):412–21. 10.1002/pon.1497 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Resource 1 Description of additional barrier and facilitator themes with illustrative quotes


