Abstract
1,259 premature infants at risk for ROP were evaluated. 29% were diagnosed with ROP and 39.4% had light fundus pigmentation (FP). Light FP had a higher association with ROP diagnosis and higher risk ROP features.
Introduction
Retinopathy of prematurity (ROP) is a complex disease driven by vascular abnormalities of the premature retina.1 Identifying diagnostic and prognostic variables for ROP is critical in preventing morbidity.2,3 Limited studies have suggested that retinal pigmentation plays a role in the development of ROP through the protective nature of intraocular melanin.4 We aim to explore the association between fundus pigmentation (FP) and ROP severity.
Materials and Methods
This study adhered to the Health Insurance Portability and Accountability Act of 1996, the tenets of the Declaration of Helsinki, was approved by the Institutional Review Board of the University of Miami, and obtained informed consent from all patients.
This consecutive retrospective case series included patients screened for ROP at Jackson Memorial Hospital Neonatal Intensive Care Unit (NICU). Eligible patients were those who met ROP screening criteria between October 2012 and June 2019. All included patients were evaluated by a single pediatric retinal physician. Exclusion criteria included >1500g BW and >32 weeks GA, and those transferred to our institution for higher level care.
Data Collection
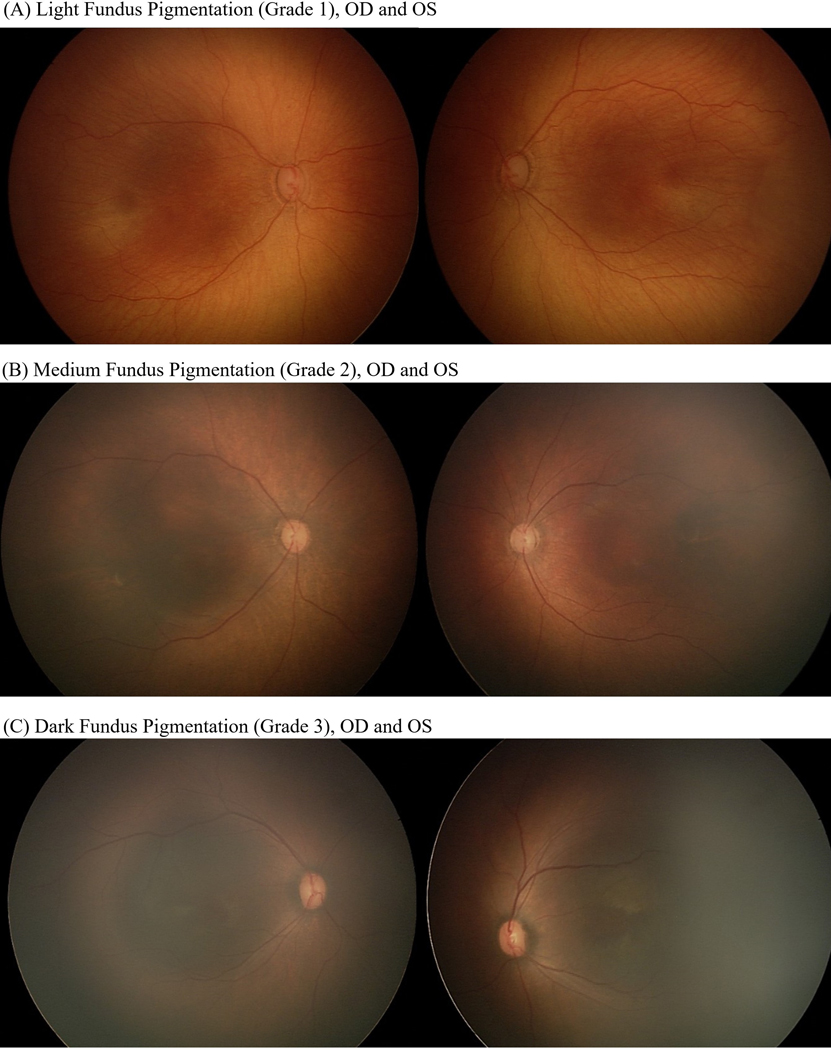
Demographic data collected included gender, birthweight (BW), gestational age (GA), and multiparity birth status. Dilated examinations were performed with standard dilation protocols and indirect ophthalmoscopy. Screening data included presence of ROP, zone, stage, plus disease, and level of FP, and was graded at the time of initial examination. FP was graded as follows: light as defined by presence of visible choroidal vessels in the macula, medium as defined by visible choroidal vessels outside the arcades, but not in the macula, and dark as defined by no visible choroidal vessels in the posterior pole and macula (see Figure 1, available at https://www.ophthalmologyretina.org/). Treatment threshold was in accordance with the Early Treatment for Retinopathy of Prematurity (ETROP) protocol.
Figure 1 –
Fundus pigmentation grading. Examples of fundus pigmentation grading to assess all screened patients with (A) representing examples of light (grade 1) fundus pigmentation, (B) medium (grade 2) fundus pigmentation, and (C) dark (grade 3) fundus pigmentation.
Statistical analysis
Explanatory variables were assessed with Pearson chi-square, Fisher exact, or exact chi-square tests (see Table 1). Univariate and multivariate, forward-stepwise logistic regressions were used to explore associations between explanatory variables and ROP and FP. All tests were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). A p-value ≤ 0.05 was considered statistically significant.
Table 1 –
Patient Demographics
| Fundus pigmentation | |||||||
|---|---|---|---|---|---|---|---|
| Light n = 496 (39.4%) | Medium/Dark n = 763 (60.6%) | Total n = 1259 | p-values (Light vs. Medium/Dark) | ||||
| Gender (female, %) | 236 | 48% | 342 | 45% | 578 | 46% | 0.25a |
| Patients with ROP (n, %) | 162 | 33% | 198 | 26% | 360 | 29% | 0.01a |
| Patients with Plus Disease (n, %) | 38 | 7.7% | 23 | 3.0% | 61 | 4.8% | 0.0002a |
| Multiparity Status (n, %) | 153 | 31% | 131 | 17% | 284 | 23% | <0.0001a |
| Birth Weight | |||||||
| Mean, std (grams) | 1195.4 | 451.7 | 1178.5 | 408.6 | 1185.1 | 426.0 | 0.7881b |
| Gestational Age | |||||||
| Mean, std (weeks) | 28.9 | 2.9 | 28.9 | 2.8 | 28.9 | 2.8 | 0.8214b |
Abbreviations: ROP = retinopathy of prematurity, std = standard deviation;
chi-square test,
independent-samples t-test
Results
A total of 1,259 infants were included in the study (table 1, available at https://www.ophthalmologyretina.org/). Of those, 39.4% (496) had light FP, 58.4% (735) had medium FP, and 2.2% (28) had dark FP. Patients with medium and dark FP were combined for analysis. Mean overall BW and GA were 1185.1g and 28.9w, respectively. There was no statistically significant difference in BW or GA between the two groups (light vs. medium/dark, p = 0.79 and 0.82, respectively). A total of 29% (360) of patients had ROP and 4.8% (61) of patients had plus disease. 23% (284) of patients were born in multiple births.
Associations with ROP
The following explanatory variables were significantly associated with ROP by univariate logistic regression: lighter FP (OR=1.38, p=0.010), presence of tunica vasculosa lentis (TVL) (OR =12.24, p<0.001), lower gestational age (OR=23.09, p<0.001), lower birthweight (OR=24.94, p <0.001), and singleton birth status (OR=0.72, p=0.035, see Table 2, available at https://www.ophthalmologyretina.org). By multivariate logistic regression, lower BW (p < 0.01), lower GA (p < 0.01), and light FP (p < 0.01) remained significantly associated with diagnosis of ROP, though multiparity did not (p = 0.30).
Table 2 –
Association of Risk Factors with Retinopathy of Prematurity
| Retinopathy of Prematurity | Fundus Pigmentation N (%)# | Lower Gestational Agec N (%) | Lower Birth Weightd N (%) | Tunica Vasculosa Lentis N (%) | Birth Status N (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Light | Medium/Dark | > 27 weeks | ≤ 27 weeks | >750 grams | ≤750 grams | Yes | No | Multiparous | Singleton | |
| Yes | 162 | 198 | 86 | 274 | 162 | 198 | 18 | 288 | 67 | 293 |
| 360 | (45%) | (55%) | (24%) | (76%) | (45%) | (55%) | (5%) | (80%) | (19%) | (81%) |
| No | 334 | 565 | 790 | 109 | 857 | 42 | 72 | 881 | 217 | 682 |
| 899 | (37%) | (63%) | (88%) | (12%) | (95%) | (5%) | (8%) | (98%) | (24%) | (76%) |
| Total | 496 | 763 | 876 | 383 | 1019 | 240 | 90 | 1169 | 284 | 975 |
| 1259 | (39%) | (61%) | (70%) | (30%) | (81%) | (19%) | (7%) | (93%) | (23%) | (77%) |
| Odds of ROP (OR [95% CI] p-value) | 1.38 [1.08–1.77] p = 0.01 | 23.1 [16.9–31.6] p <0.001 | 24.9 [17.2–36.2] p < 0.001 | 12.2 [7.2–20.9] p < 0.001 | 0.72 [0.53–0.98] p = 0.035 | |||||
All analyses performed with univariable logistic regression,
comparison of greater than to less than 27 weeks,
comparison of greater than to less than 750 grams,
percentages expressed respective to ROP groups;
Abbreviations: ROP = retinopathy of prematurity, OR = odds ratio, CI = confidence interval
Associations with Fundus Pigmentation
Regarding light FP, the following explanatory variables were significantly associated (see table 3): ROP (OR=1.38, p=0.01), plus disease (OR=4.01, p<0.01), multiparity birth status (OR=2.17, p<0.01), more posterior zone (OR=2.50, p<0.01), higher stage (OR=1.92, p<0.01), and treatment with intravitreal bevacizumab (IVB, OR=2.67, p<0.01). 68 patients (18.9%) in the study received IVB. Patients receiving IVB had greater odds of light FP (OR=2.67, p<0.01). No other significant associations were noted for treatment.
Table 3 –
Association of ROP Severity & Treatment with Light Fundus Pigmentation
| Fundus pigmentation | ROP Status N (%)# | Plus Disease N (%) | Zone Severity N (%) | Stage Severity N (%) | Treatment Type N (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Zone 1 | Zone 2 &3 | Stage 1 | Stage 2 | Stage 3 | IVB | Laser | |
| Light | 162 | 334 | 38 | 458 | 37 | 125 | 70 | 87 | 5 | 38 | 7 |
| 496 | (33%) | (67%) | (7.7%) | (92%) | (7.5%) | (25%) | (14%) | (18%) | (1.0%) | (7.7%) | (1.4%) |
| Medium/Dark | 198 | 565 | 23 | 740 | 25 | 169 | 99 | 86 | 13 | 23 | 8 |
| 763 | (26%) | (74%) | (3.0%) | (97%) | (3.3%) | (22%) | (13%) | (11%) | (1.7%) | (3.0%) | (1.0%) |
| Total | 360 | 899 | 61 | 1198 | 62 | 294 | 169 | 173 | 18 | 68 | 15 |
| 1259 | (29%) | (71%) | (4.8%) | (95%) | (4.9%) | (23%) | (13%) | (14%) | (1.4%) | (5.4%) | (1.2%) |
| Odds of ROP (OR [95% CI] p-value) | 1.38 [1.08–1.77] p = 0.01b | 4.01 [2.00–8.04] p > 0.01a | 2.50 [1.48–4.23] p > 0.01b | 1.22 [0.94–1.60] p = 0.14ǂ, b | 1.57 [1.08–2.3] p = 0.02a | 1.92 [1.27–2.9] p > 0.01a | * | 2.67 [1.57–4.54] p > 0.01b | * | ||
Zone 2 & 3 had reduced odds of light fundus pigmentation as compared to Zone 1 (OR 0.49, p = 0.01);
Associations for stage 3 severity and treatment with laser were not statistically significant; all analyses performed with logistic regression;
forward stepwise multivariable logistic regression
univariable logistic regression
percentages expressed respective to fundus pigmentation groups; Abbreviations: ROP = retinopathy of prematurity, OR = odds ratio, CI = confidence interval, IVB = intravitreal bevacizumab
Discussion
The current study was prompted by observations that light FP in ROP patients was consistently associated with more severe disease. Although few have directly studied fundus pigmentation, some investigators have found that darker skin pigmentation confers a lower risk of severe ROP.1,4,5 Our results confirm an association between light FP and the presence of ROP, plus disease, multiparous births, more posterior zone, higher stage, and treatment with IVB (table 3), independent of birthweight and gestational age.
The association between ROP and light FP may be explained by the regulation of reactive oxygen species (ROS) of the retina and choroid.6 Melanin pigments are a protective antioxidant for the retinal milieu through the mechanism of removing ROS during stress and phototoxicity.4,6 Therefore, the antioxidative effects of melanin may reduce the progression of ROP in stressful environments (such as the premature retina). Studies of diseases of the retina, RPE, and choroid, such as AMD, have found similar associations.7
This pathophysiology may also explain the stronger association of light FP with more severe disease and therefore treatment with IVB as well (table 3). As such, the presence of light FP can be used as a risk stratification indicator in premature infants and may raise clinical suspicion or prompt closer observation during the ROP screening process.
Our study also found that ROP was strongly associated with lower birth GA, lower BW, as well as presence of TVL, which have been established by previous authors.1,2 Surprisingly, in our regression model, the presence of singleton births had a higher association with ROP, although previous authors have found mixed associations with singleton vs. multiparous births.3 While lower BW and GA are known risk factors for ROP,1 regression analysis did not find these significantly associated with fundus pigmentation in our study.
Many prediction models have been developed to ease the burden of ROP screening and improve detection of high-risk patients.2 Our study has shown that FP is objective and generalizable, since all screenings require fundus evaluations and can be interpreted separately from race or skin pigmentation. As ophthalmologists increase their adoption of telemedicine and remote screening, we may wish to consider FP as a variable for prediction models and risk stratification.2
Limitations of our study include its retrospective nature. Changes in screening guidelines may have allowed some variability in the BW and GA of ROP infants across time. Some subjectivity of fundus pigmentation grading was likely present in the study.
Conclusion
In summary, the present study confirms the hypothesis that ROP and more aggressive features of ROP are associated with patients with light FP. In the future, validation of fundus pigmentation as a clinical and algorithmic predictor for ROP may help advance ophthalmological care in premature infants.
Acknowledgments
Financial Support: The research was supported in part by the National Eye Institute Center Core Grant (P30EY014801), an unrestricted grant from the Research to Prevent Blindness, Inc., New York, NY to the Department of Ophthalmology, University of Miami Miller School of Medicine, and the Heed Ophthalmic Foundation.
Meeting presentations: Accepted for poster presentation at the American Academy of Ophthalmology Annual Meeting 2020
Abbreviations:
- ROP
retinopathy of prematurity
- FP
fundus pigmentation
- BW
birthweight
- GA
gestational age
- NICU
neonatal intensive care unit
- IVB
intravitreal bevacizumab
Footnotes
Conflict of Interest: No conflicting relationship exists for any author
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Palmer EA, Flynn JT, Hardy RJ, et al. Incidence and early course of retinopathy of prematurity. The Cryotherapy for Retinopathy of Prematurity Cooperative Group. Ophthalmology. 1991;98(11):1628–1640. [DOI] [PubMed] [Google Scholar]
- 2.Hutchinson AK, Melia M, Yang MB, VanderVeen DK, Wilson LB, Lambert SR. Clinical Models and Algorithms for the Prediction of Retinopathy of Prematurity: A Report by the American Academy of Ophthalmology. Ophthalmology. 2016;123(4):804–816. [DOI] [PubMed] [Google Scholar]
- 3.Ludwig CA, Greven MA, Moshfeghi DM. Predictors of treatment-warranted retinopathy of prematurity in the SUNDROP cohort: influence of photographic features. Graefes Arch Clin Exp Ophthalmol. 2017;255(10):1935–1946. [DOI] [PubMed] [Google Scholar]
- 4.Monos T, Rosen SD, Karplus M, Yassur Y. Fundus pigmentation in retinopathy of prematurity. Pediatrics. 1996;97(3):343–348. [PubMed] [Google Scholar]
- 5.Saunders RA, Donahue ML, Christmann LM, et al. Racial variation in retinopathy of prematurity. The Cryotherapy for Retinopathy of Prematurity Cooperative Group. Arch Ophthalmol. 1997;115(5):604–608. [DOI] [PubMed] [Google Scholar]
- 6.Katz ML, Robison WG Jr., Autoxidative damage to the retina: potential role in retinopathy of prematurity. Birth Defects Orig Artic Ser. 1988;24(1):237–248. [PubMed] [Google Scholar]
- 7.Dieguez HH, Gonzalez Fleitas MF, Aranda ML, et al. Melatonin protects the retina from experimental nonexudative age-related macular degeneration in mice. J Pineal Res. 2020;68(4):e12643. [DOI] [PubMed] [Google Scholar]