Abstract
Background:
Depressive symptoms predict hospitalization and mortality in adults with cardiac disease. Resilience, defined as a dynamic process of positively responding to adversity, could protect against depressive symptoms in cardiac disease. No systematic review has been conducted on the relationship between these variables in this population.
Objective:
The aim of this review was to explore the association between psychological resilience and depressive symptoms in adults with cardiac disease.
Methods:
Seven databases (PubMed, Embase, CINAHL, PsycInfo, Web of Science, SCOPUS and Cochrane) were searched from inception to December 2019 using the search terms “cardiac disease,” “depressive symptoms,” “depression,” and “resilience”. Inclusion criteria dictated that studies reported original research on the association between resilience and depressive symptoms in adults with a cardiac disease broadly defined. Quality ratings were performed by two independent raters.
Results:
We identified 13 studies for final review. Study sample sizes ranged from 30 to 1022 participants, average age ranged from 52 to 72 years, and all studies had majority male participants (64% to 100%). Resilience and depressive symptoms were inversely related in 10 of 13 studies. The three studies with poor quality sampling techniques or significant loss to follow-up found no relationship.
Conclusions:
Resilience appears to protect against depression in adults with cardiac disease. Gaps in the literature include poor understanding of the direction of causality. Methods of promoting resilience need to be identified and studied.
Keywords: cardiovascular diseases, heart failure, coronary artery disease, depression, resilience
Background and significance:
Depressive symptoms are common in adults with cardiac disease. In patients with heart failure (HF), depressive symptoms affect up to 79% of people.1 Similarly, severe depressive symptoms are estimated to affect 30% of patients with coronary heart disease (CHD).2 These prevalence figures are striking in comparison to the general adult population, where 13.7% of the adult population ≥65 years of age suffer from severe depressive symptoms.3
A recent meta-analysis of risk factors for depression following acute coronary syndrome identified major risk factors were a history of depressive disorder, current anti-depressive therapy, being a widow, a housewife, and having a history of HF.4 Others also have found that women with CHD experience more depressive symptoms than men.5 Patients with HF or CHD and severe depressive symptoms have two-fold risk of secondary events and mortality.6, 7 Even sub-diagnostic depressive symptoms predict increased risk of mortality in patients with many types of cardiac disease, including CHD8, 9 and atrial fibrillation.10, 11
Depressive symptoms rarely improve spontaneously over time. Only half of patients with significant depressive symptoms achieve relief of these symptoms within 5 years.12 This is important to note, as 60% to 80% of CHD patients with elevated depressive symptoms are at increased risk of an acute cardiac event.2, 9 Relief of depressive symptoms could be a potentially modifiable factor for the reduction of acute cardiac events.
To combat the negative effects of depressive symptoms in patients with cardiac disease, psychological and pharmacological treatments are used to treat depressive symptoms. The two mainstay treatments are cognitive behavioral therapy (CBT) and selective serotonin reuptake inhibitors (SSRIs).13–15 However, mortality and recurrent cardiac events are not always reduced with these treatments.13 Only mild improvements have been seen in depressive symptoms following CBT in patients with CHD and HF.16, 17
While SSRIs have been shown to improve depressive symptoms in cardiac patients, they have negative consequences, including interactions with essential medications for cardiac patients18 and potential for ventricular damage.19 As a result, SSRIs are thought to potentially increase risk of mortality and acute cardiac events.20, 21 The American College of Cardiology currently recommends careful consideration of the potential benefits and risks in each individual patient.22
Strategies are needed to augment the current symptom management options available. One potential avenue of intervention is in psychological resilience. Resilience has been defined as a dynamic process,23 the “homeostatic return” to prior functioning following an adverse event (serious stress or trauma, physical or psychological),24, 25 and positive adaptation due to personal characteristics and environmental circumstances.26 For the purpose of our analysis, resilience is defined as a “dynamic process of maintaining positive adaptation in the face of adversity.”23 This classic definition has previously been adopted for research on the effects of chronic illness.27 Resilience has been described in many different populations, including those with chronic illness.28–30 We currently know little about the components of resilience, but social support is the most commonly proposed modifiable component of resilience.27, 31–33 At this point, the consensus is that psychological resilience can be cultivated and as such may serve as a potential avenue for intervention in depressive symptoms.
As consequences of depressive symptoms in cardiac diseases are severe, protective factors are important to identify.34, 35 Previously, three systematic reviews have been conducted on resilience in chronic illness but none in cardiac disease specifically.36–38 In order to examine whether resilience can be an avenue of intervention for depressive symptoms in cardiac disease, a clear understanding of the relationship must be established. Thus, the aim of this systematic review was to answer the following question: What is the association between psychological resilience and depressive symptoms in adults with cardiac disease? Cardiac disease was specified as those conditions that directly affect the heart tissue, such as HF or CHD. These diseases pose an increased risk of mortality with even sub-diagnostic levels of depressive symptoms and therefore, were the focus of our analysis.
Methods:
A systematic review was conducted to answer the research question.39 Inclusion criteria specified studies that included adult patients with cardiac disease (≥18 years old) and measured both depressive symptoms and psychological resilience. Exclusion criteria specified patients with vascular disease that does not affect heart tissue directly, articles not written in English, analysis that aggregated cardiac disease with other illnesses, conference abstracts, non-peer-reviewed articles, and studies that measured biological resilience rather than psychological resilience. Biological resilience is defined as “the capacity to maintain adequate function and structure at molecular and cellular levels by adapting to changing to specific challenges.”40 For this analysis, we were more interested in the phenomenon of psychological resilience, which has potential to influence behavior. As such, we excluded studies on biological resilience. Members of our team are fluent in English only; therefore, we excluded studies not written in English.
In consultation with a biomedical librarian, we used the following terms to identify the sample of articles: “cardiac disease,” “depression,” “depressive symptoms,” and “resilience” to search PubMed, Embase, CINAHL, PsycInfo, Web of Science, SCOPUS and Cochrane from inception to December 2019. Search formulae for each database are provided in Supplemental Table 1.
Following the search, duplicates were removed (See Figure 1). Titles and abstracts were then reviewed for eligibility. Full text review was conducted on eligible studies. Citations of all eligible studies were hand searched to make sure that relevant articles were not inadvertently missed.
Figure 1.
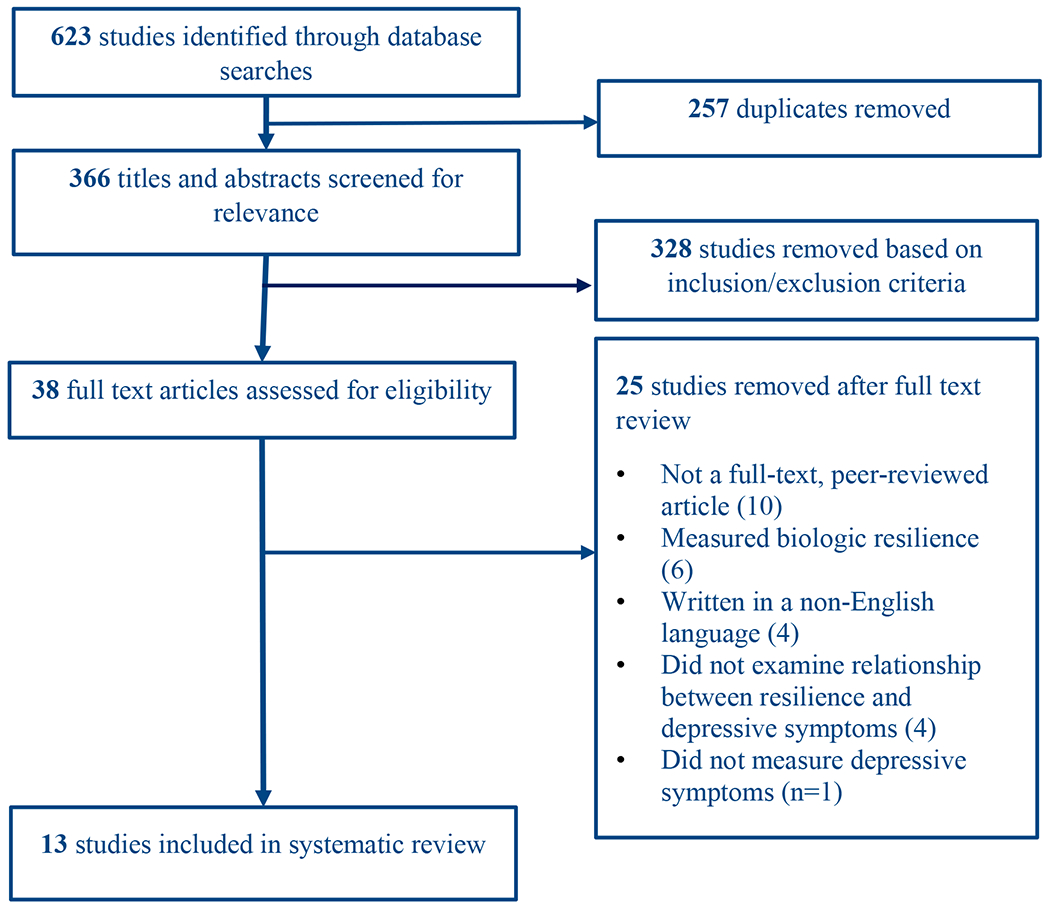
PRISMA diagram of study selection process.
Initial database search identified 623 studies. Duplicates were then removed, leaving 366 titles and abstracts for initial screening. Full text review was conducted on 38 articles. In total, 13 studies were included in the systematic review.
Of the 623 articles identified, 257 duplicates were removed. Title and abstract review were then conducted on the remaining 366 studies. Of those, 38 studies fit the inclusion and exclusion criteria but 25 were excluded during full text review. Thirteen studies remained for final analysis (see Figure 1).
Procedure.
Once studies were selected for final inclusion, we abstracted information and then rated quality, as described below. Most studies on psychological resilience and depressive symptoms are observational.41 Despite the utility of observational studies in the health fields, many recommendations are borrowed from reviews of randomized controlled trials and many provide conflicting recommendations on inclusion of different study designs and the use of quality scales to assess the risk of bias.39 To accommodate our question, we abstracted information using the Meta-Analysis of Observational Studies in Epidemiology (MOOSE) method.42 However, due to variations in reported data, our systematic review does not include a meta-analysis of our findings. The data abstracted from eligible studies included study design; objective/aims, hypothesis; patient sample size and eligibility criteria; variables, instruments and measurement frequency; methodology and analysis approach; main findings; and study limitations.
The quality of selected studies was graded using the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies provided by the National Heart, Lung and Blood Institute.43 Fourteen questions relevant to observational study design guided the rating process. These included questions such as “was the research question or objective in this paper clearly stated?” and “was the participation rate of eligible persons at least 50%?” From these, an overall quality rating can be made for each individual study (i.e. poor, fair or good). Two raters (A.K. and A.M.) independently graded the quality of each of the 13 selected articles using Covidence systematic review software. This software allows independent quality grading and comparison between the two graders. Initial inter-rater reliability was 0.69. The two raters met in person to compare differences in quality grading. Differences were commonly due to one reviewer or the other missing a detail in the full-text analysis. Inter-rater agreement after discussion reached 0.92.
All data from the article abstraction process was summarized in a table. Using this format, data were compared across studies to assess for common themes. These themes were synthesized into general patterns of results.
Results:
Study characteristics:
The 13 studies were conducted in a variety of places, including Australia (n=2), Austria (n=1), Brazil (n=1), China (n=1), England (n=1), India (n=1), the Netherlands (n=1), Palestine (n=2), Taiwan (n=2), and the United States (n=1). Six studies were conducted with acutely ill patients admitted to the hospital. Three studies were longitudinal.44–46 All three of the longitudinal studies examined patients just prior to or following coronary intervention and then again, several months later. Studies looked at a variety of cardiac diseases, with the majority of the samples having CHD. Six studies looked specifically at patients with CHD. Two examined patients with HF.47, 48 Four studies included patients with “cardiac diagnoses”, which included CHD, HF, atrial fibrillation, and/or arrythmia.49–52 One study examined patients who were admitted to a cardiac rehabilitation program with a cardiac diagnosis.53
Sample characteristics:
Study sample sizes ranged from 30 to 1022 participants. Average age ranged from a low of 52 to a high of 72 years. All studies had majority male participants (64% to 100%). None of the studies reported ethnicity rates. Four studies reported rates of marriage or partnership (72% to 91%). Six studies reported educational level of participants. Of these, rate of high school education or above ranged from 41% to 96%. Sample characteristics for each study are detailed in Supplementary Table 2.
Measurement characteristics:
Resilience.
Five different scales were used to measure resilience. Details on validity and reliability of each resilience scale are provided in Table 1. Five studies used the Wagnild and Young Resilience Scale (WYRS), either 13-, 14- or 25-item versions,47–49, 51, 52, 54 first established from a qualitative study of 24 women who had adapted successfully following a major adverse event.55 From their narratives, five interrelated components were identified that constitute resilience: equanimity, perseverance, self-reliance, meaningfulness, and existential aloneness.55 One study used the Sense of Coherence Scale as a measure of resilience.50 Three studies used the Connor Davidson Resilience Scale (CD-RISC). Two studies used the Dispositional Resilience Scale.45, 46 One study used the Brief Resilience Scale.53 All resilience scales reflected the person’s ability to “bounce back.”41
Table 1.
Resilience measures used by each study.
| Measurement | Citations | Reliability | Convergent Validity | Scoring | Levels of resilience | Item example |
|---|---|---|---|---|---|---|
| Wagnild and Young Resilience Scale (13-, 14- or 25-item version) | • Kunschitz et al.54 • H. Allabadi et al.49 • Hala Allabadi et al.51 • Chang et al.,47 • J.C. Liu et al.48 • Barreto et al.52 |
Cronbach’s α 0.8965 | r = 0.75 with CD-RISC65 | Sum of score on 25 items, 7-point Likert scale from 1 (strongly disagree) to 7 (strongly agree) | 25-115 = low resilience 116-160 = moderate resilience 161-175 = high resilience |
“When I am in a difficult situation, I can usually find my way out of it” |
| Sense of Coherence Scale | • Toukhsati et al.50 | Cronbach’s α 0.70-0.9266 | r = 0.714 with CD-RISC67 | Sum of score on 13 items, 7-point Likert scale | Score ranges between 13 and 91 points, no cut-offs provided | “When something unpleasant happened in the past your tendency was: (from ‘to eat yourself up about it’ to ‘to say, “ok that’s that, I have to live with it” and go on’)” |
| Dispositional Resilience Scale | • van Montfort et al.46 • Thornton & Hallas45 |
Cronbach’s α 0.8268 | Convergent validity not tested with other resilience scales.68 | Sum of score on 15 items, 4-point Likert scale from 0 (not true at all) to 3 (completely true) | Score ranges from 0 to 60, no cut-offs provided | “How things go in my life depends on my own actions” |
| Brief Resilience Scale | • Smith et al.53 | Cronbach’s α 0.91 | r = 0.59 with CD-RISC53 | Average of score on 5 items (3 items reverse-scored), 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree) | 1-2.99 = low resilience 3-4.3 = moderate resilience 4.31-6 = high resilience |
“I tend to bounce back quickly after hard times” |
| Connor Davidson Resilience Scale | • Liu et al.69 • Edward et al.44 • Kumar, Awasthi, & Shankar63 |
Cronbach’s α 0.92 | r = 0.75 with WYRS65 | Sum of score on 25 items, 5-point Likert scale from 0 (not at all) to 4 (almost always) | 0-73 = Low resilience 74-91 = moderate resilience 91-100 = high resilience |
“I adapt when changes occur” |
Column labels for the table were chosen based on a previous systematic review on resilience measures.41 BDI=Beck Depression Inventory, CD-RISC=Connor Davidson Resilience Scale, CDS=Cardiac Depression Scale, DRS-15=Dispositional Resilience Scale, HADS-D=Hospital Anxiety and Depression Scale (Depression Subscale), PHQ-9=Patient Health Questionnaire
Depressive Symptoms.
Six different measures of depressive symptoms were used (Table 2). Three studies used the Beck Depression Inventory (BDI),45, 47, 48 which was developed in 1961 to improve assessment of psychotherapy for depression56 and has since become the gold standard in assessing depressive symptoms.57 In patients with medical disorders, the mean score is generally higher than those without medical disorders due to somatic symptoms that co-occur with other illnesses.58 Several have suggested that depressive symptom severity with BDI-II would be biased in patients with medical disorders due to somatic symptoms.58, 59 However, BDI allows clinicians to assess improvements over time due to psychotherapy and allows researchers to assess for depressive symptoms in patients with “sub-diagnostic” depressive symptoms who do not qualify for a diagnosis of major depressive disorder.59
Table 2.
Depressive symptom measures used by each study.
| Measurement | Citations | Reliability | Convergent Validity | Scoring | Severity of symptoms | Recall period | Item Example |
|---|---|---|---|---|---|---|---|
| Cardiac depression scale | • H. Allabadi et al.49 • Toukhsati et al.50 • Hala Allabadi et al.51 |
Cronbach’s α 0.9060 | r = 0.73 with BDI60 | Sum of score on 26 items, 7-point Likert scale from 1 (strongly disagree) to 7 (strongly agree) | ≥80 indicates depressive symptoms | Last several days | “I can’t be bothered doing anything much” |
| Beck Depression Inventory | • Chang et al.47 • J.C. Liu et al.48 • Thornton & Hallas45 |
Cronbach’s α 0.8970 | r = 0.73 with Zung Self-Rating Depression Scale71 | Sum of score on 21 items, 3-point Likert scale from 0 (not at all) to 3 (extreme form of each symptom) | 0–13 = no symptoms, 14–19 = mild symptoms, 20–28 = moderate symptoms, and 29–63 = severe symptoms | Last two weeks | “I don’t get real satisfaction out of anything anymore” |
| Patient Health Questionnaire – 9 | • Van Montfort et al.46 • Kunschitz et al.54 • Edward et al.44 |
Cronbach’s α 0.8372 | r = 0.87 with BDI73 | Sum of score on 9 items, 4-point Likert scale from 0 (not at all) to 3 (nearly every day) | 1–4 = no symptoms, 5–9 = mild symptoms, 10–14 = moderate symptoms, 15–19 = moderately severe symptoms, and 20–27 = severe symptoms | Last two weeks | “Over the last 2 weeks, how often have you been bothered by little interest or pleasure in doing things?” |
| Zung Self-Rating Depression Scale | • Liu et al.69 | Cronbach’s α 0.8874 | r = 0.73 with BDI71 | 20 items, 4-point Likert scale from 0 (none or little of the time) to 3 (most or all the time) with a several items reverse-scored | 0-50=no symptoms, 50-59=mild symptoms, 60-69=moderate symptoms, 70 and above=severe symptoms | Last two weeks | “I still enjoy the things I used to do” |
| Hospital Anxiety and Depression Scale (Depression Subscale) | • Barreto et al.52 • Smith et al.53 |
Cronbach’s α 0.67-0.9062 | r = 0.62-0.73 with BDI62 | Sum of score on 7 items, 4-point Likert scale from 0 to 3 with several items reverse-scored | 0–7 = no symptoms, 8–10 = mild symptoms, 11–15 = moderate symptoms, and ≥16 = severe symptoms | Last week | “I still enjoy the things I used to enjoy” |
| General Health Questionnaire (Depression Subscale) | • Kumar et al.63 | Cronbach’s α 0.8675 | r = 0.67 with BDI75 | Sum of 12 items, 4-point Likert scale from 0 (no more than usual) to 3 (much more than usual) | 0-36 with higher scores indicating worse severity | Last week | “Have you been feeling unhappy or depressed?” |
BDI=Beck Depression Inventory, CD-RISC=Connor Davidson Resilience Scale, CDS=Cardiac Depression Scale, DRS-15=Dispositional Resilience Scale, HADS-D=Hospital Anxiety and Depression Scale (Depression Subscale), PHQ-9=Patient Health Questionnaire 9.
The remaining five depression scales used in the studies in this analysis also can be used as continuous measurements, with higher scores indicating increased severity of depressive symptoms.60–62 Three studies used the Cardiac Depression Scale.49–51 Three studies used the Patient Health Questionnaire.44, 46, 54 One study used the Zung Self-Rating Depression Scale,48 two studies used the Hospital Anxiety and Depression Scale,52, 53 and one study used the General Health Questionnaire (depression subscale).63
Quality grading:
All studies had an explicit research question, purpose or aim stated. All specified a population that was clearly defined. Three studies had poor quality sampling or high attrition.44, 45, 63 Thornton et al. analyzed 30 patients out of 180 available.45 The rationale for the reduced sample was based on anxiety and depressive symptom scores.45 Details were not provided on the participant selection process. Therefore, it was not clear whether inclusion and exclusion criteria were pre-specified or uniformly applied. Few of the investigators justified their study sample size due to the observational nature of the research. Of the three studies that were longitudinal, two of them lost >20% of their original sample.44, 45 The third longitudinal study did not specify attrition.46
All 13 studies measured predictor and outcome variables consistently across participants. Whether or not assessors were blinded to the level of resilience or depressive symptoms in participants was unclear; none of the studies explicitly addressed blinding. Nine studies statistically accounted for confounding variables. One study was conducted in India and used the CD-RISC.63 This measure has been validated for use in adolescents or young adults in India. However, the scale was used in adults and not translated to Hindi; it was used in English for this study.64 No information was provided on the languages spoken by the participants. Overall, 8 studies were good quality, 3 were fair, and 2 were poor.
Association between resilience and depressive symptoms:
Ten studies found a negative association between resilience and depressive symptoms. These negative associations included correlation coefficients between resilience and depressive symptoms that ranged from -0.87 to -0.33 (all p<0.05), decreased odds of depressive symptoms in participants with high resilience (OR 0.42-0.48, all p<0.05), and significantly lower average resilience scores (measured by the Wagnild and Young Resilience Scale) in patients with severe depressive symptoms (138.5±14.5 vs. 144.9±14.9, p=0.029). Three studies found non-significant relationships between resilience and depressive symptoms.44, 45, 63 These three studies were kept in the review but the results were given less weight due to their lower-quality ratings. Results of each study are detailed in Table 3.
Table 3:
Description of the Characteristics of Each Study Included in the Review
| Author, year (Country) | Study Design | Sample | If longitudinal, follow-up periods | Measurements (Resilience, depressive symptoms) | Results | Quality grading and key issues |
|---|---|---|---|---|---|---|
| H. Allabadi et al., 2019 (Palestine) | Prospective, observational, cross-sectional | Cardiac inpatients | N/A | WYRS, CDS (moderate depressive symptoms with score ≥ 90, severe ≥ 100) | Decreased odds of depressive symptoms for moderately high and high resilience (OR 0.48 and 0.42, respectively, all p < 0.05) | Good |
| Hala Allabadi et al., 2019 (Palestine) | Prospective, observational, cross-sectional | Cardiac inpatients | N/A | WYRS, CDS | Men with depressive symptoms had significantly higher levels of resilience compared to females with depressive symptoms (men vs. women with high resilience, 8.9% vs. 5.1%) | Good |
| Barreto et al., 2017 (Brazil) | Prospective, observational, cross-sectional | Cardiac inpatients | N/A | WYRS, HADS-D, scores > 8 | Lower resilience in patients who had depressive symptom score > 8 (patients with moderate depressive symptoms vs. those with low depressive symptoms, 138.5±14.5 vs. 144.914.9, p=0.029) | Fair Key issues: (1) vague inclusion and exclusion criteria |
| Chang, Wu, Chiang & Tsai, 2017 (Taiwan) | Prospective, observational, cross-sectional | HF outpatients | N/A | WYRS (Chinese version), BDI (Chinese version) | Higher levels of resilience were significantly associated with lower levels of depressive symptoms (r=−0.51, p ˂ 0.001). Additionally, resilience significantly moderated the direct effects of depressive symptoms on self-care maintenance (B=0.02, SE=0.01, p<0.01). | Good |
|
Edward et al., 2016 (Australia) |
Prospective, observational cohort, longitudinal | Cardiac outpatients following PCI | 6- and 12-months following PCI | CD-RISC, PHQ-9 | At 6 months s/p PCI, PHQ-9 and CD-RISC were inversely correlated (r = -0.331, p=0.018). In a multiple model with PHQ-9 as an outcome, CD-RISC was not a statistically significant predictor. At 12 months following PCI, CD-RISC was not significantly different (83.3 vs 80.6), although PHQ-9 scores were significantly different (13.9 vs. 4.97). | Fair Key issues: (1) loss of follow-up to baseline |
| Kuman, Awasthi, & Shankar, 2019 (India) | Prospective, observational, cross-sectional | Inpatients with CAD | N/A | CD-RISC, General Health Questionnaire – Depression Subscale | Non-significant correlation between resilience and depressive symptoms (r=−0.023, p>0.05) | Poor Key issues: (1) unclear participation rate of eligible participants, (2) exclusion of women |
| Kunschitz, Friedrich, Schoppl, Maitz, & Sipotz, 2017 (Austria) | Prospective, observational, cross-sectional | Inpatients with CAD | N/A | WYRS, PHQ-9 | Cluster analysis found a four-group solution. Cluster 1 was significantly higher in depressive symptoms and lower in resilience scores compared to Cluster 4 (all p<0.008). These clusters were determined based on illness perception. | Good |
| J.C. Liu, Chang, Wu, & Tsai, 2015 (Taiwan) | Prospective, observational, cross-sectional | Outpatients with HF | N/A | WYRS (Chinese version), BDI | Depressive symptoms were significantly associated with resilience (α=−1.468, p<0.001). Resilience did not significantly mediate the relationship between depressive symptoms and physical health status (measured by Medical Outcome Studies 36-item Short Form). | Good |
| Liu et al., 2018 (China) | Prospective, observational, cross-sectional | Inpatients with CAD | N/A | CD-RISC, Zung Self-Rating Depression Scale | Depressive symptoms and resilience were significantly associated (r=−0.869, p<0.01) | Good |
| Smith et al., 2008 (United States) | Prospective, observational, cross-sectional (longitudinal for 3 months but assessed BRS only at baseline) | Outpatients attending cardiac rehabilitation | N/A | BRS, HADS-D | Depressive symptoms negatively correlated with resilience (r=−0.50, p<0.01). Partial correlation between depressive symptoms and resilience (r=−0.37, p<0.01) where health-related outcomes were controlling for other predictors. | Good |
| Thornton & Hallas, 1999 (England) | Prospective, observational cohort, longitudinal | Outpatients s/p AMI | 4 weeks and 18mos following AMI | DRS, HADS-D | No significant contribution in regression analysis (p>0.05) | Poor Key issues: (1) unclear selection of participants, (2) reduction in sample size without clear justification, (3) did not collect data on resilience at follow-up |
| Toukshati et al., 2017 (Australia) | Prospective, observational, cross-sectional | Cardiac outpatients | N/A | SOC, CDS | Resilience negatively associated with depressive symptoms (r=−0.79, p<0.001). In particular, the hopelessness component showed a high degree of correlation with resilience (r=−0.73, p<0.001). In linear regression, 65% of the variance in depressive symptoms was explained by resilience factors. Resilience was a stronger predictor of affective depressive symptoms (e.g. anhedonia, mood, hopelessness) than it was of somatic depressive symptoms (e.g. sleep disturbance). | Good |
| van Montfort, Kupper, Widdershoven, & Denollet, 2018 (The Netherlands) | Prospective, observational cohort, longitudinal | Outpatients following PCI | Baseline (pre-PCI), 1wk-, 1mo-, 6mos, 1yr and 2yrs following PCI | DRS-15, PHQ-9 | Resilience levels were lower in the group with significantly higher depressive symptoms (identified via step-3 latent class analysis) | Fair Key issue: significant loss of follow-up |
Results of the analyzed studies. CHD=Coronary heart disease, PCI=percutaneous coronary intervention, AMI=acute myocardial infarction, HF= heart failure, CD-RISC=Connor Davidson Resilience Scale, PHQ-9=Patient Health Questionnaire 9, DRS-15=Dispositional Resilience Scale, BDI=Beck Depression Inventory, HADS-D= Hospital Anxiety and Depression Scale (Depression Subscale), CDS=Cardiac Depression Scale
Additional Findings:
One study found a mediated relationship between depressive symptoms, self-care confidence and self-care maintenance, with resilience serving as a moderator between these variables (B=0.02, SE=0.01, p<0.01).47 When high resilience was present, depressive symptoms did not lead to poor self-care maintenance. The negative relationship between depressive symptoms and self-care maintenance was reversed in the presence of high resilience due to its effect on self-care confidence.
Two studies examined physical health status in the relationship between depressive symptoms and resilience. Liu et al. (2015) found that resilience did not significantly mediate the relationship between depressive symptoms and physical health status (measured by Medical Outcome Studies 36-item Short Form).48 In another study, resilience was a stronger predictor of affective depressive symptoms (anhedonia, mood, hopelessness) than it was of somatic depressive symptoms (sleep disturbance).50
Discussion:
The question driving this systematic review was “what is the association between psychological resilience and depressive symptoms in cardiac patients?” Most studies reviewed reported an inverse relationship between resilience and depressive symptoms, consistent with our hypothesis that psychological resilience can protect against depressive symptoms. Only three studies found no relationship between resilience and depressive symptoms44, 45, 63 and two of these studies had poor quality ratings.45, 63 Together, these results support but do not confirm our hypothesis because the studies were all cross-sectional. It is possible that resilience built up through social support or another mechanism can protect patients from severe depressive symptoms. Longitudinal studies testing modifiable components of resilience are needed before we can conclude that resilience is sufficient to protect against depressive symptom severity in patients with cardiac disease. Overall, based on these results, we are moderately confident that resilience is associated with reduced depressive symptoms in cardiac patients.
In the study by Chang et al.,47 the relationship between resilience and depressive symptoms was connected to self-care maintenance. The concept of self-care maintenance embodies patients’ daily care of their disease. Examples of self-care maintenance include taking daily medications, getting sufficient sleep and regular exercise. Chang et al. found that the even in the presence of depressive symptoms people with high resilience scores can maintain their self-care maintenance due to the effect of resilience on self-care confidence.47 Patients who have cultivated high levels of resilience may be better able to care for themselves even when experiencing increases in depressive symptoms.
In the two studies that examined the influence of resilience on the relationship between depressive symptoms and physical health, resilience was not protective. Depressive symptoms have been shown to negatively affect physical symptom burden in patients with chronic illness.47 Resilience could be a factor that improves physical symptom burden through its effect on depressive symptoms. Additional research on the interplay between physical health and symptoms, depressive symptoms and resilience is warranted. Components of resilience are unknown and are important to examine in future research.
Limitations:
There are several limitations of this analysis. First, no consistency existed in measurement of depressive symptoms or resilience between the studies. Six different measures of depressive symptoms and five different measures of resilience were used, which limited our ability to compare results. The three longitudinal studies were all poor in quality, so the directly of causality between resilience and depressive symptoms remains unclear. Statistical procedures used in the primary studies rarely accounted for confounding variables; simple bivariate correlations were calculated in several studies. No studies examined the mechanism of action between resilience and depressive symptoms. We also limited our search to studies published in English only; this may have excluded eligible studies with additional data related to the research question. Inter-rater agreement was not addressed at the level of title and abstract review.
Conclusion:
Overall, high resilience appears to be associated with lower levels of depressive symptoms in cardiac patients. Resilience could be a potential avenue for intervention. However, the relationship between depressive symptoms, resilience and associated variables over time is not well understood in patients with cardiac disorders. Additional research into this phenomenon is needed. Patients with depressive symptoms have reduced quality of life and increased hospitalization and mortality risk. A clear understanding of resilience and its components may aid in the development of depressive symptom management strategies.
Supplementary Material
Footnotes
Conflicts of interest: None to report.
Contributor Information
Amy Ketcham, School of Nursing, University of Pennsylvania, Philadelphia, PA.
Austin Matus, School of Nursing, University of Pennsylvania, Philadelphia, PA.
Barbara Riegel, School of Nursing, University of Pennsylvania, Philadelphia, PA.
References
- 1.Sokoreli I, De Vries J, Pauws S, Steyerberg E. Depression and anxiety as predictors of mortality among heart failure patients: systematic review and meta-analysis. Heart failure reviews. 2016;21(1):49–63. [DOI] [PubMed] [Google Scholar]
- 2.Carney RM, Freedland KE. Depression and coronary heart disease. Nature Reviews Cardiology. 2017;14(3):145. [DOI] [PubMed] [Google Scholar]
- 3.Laborde-Lahoz P, El-Gabalawy R, Kinley J, Kirwin PD, Sareen J, Pietrzak RH. Subsyndromal depression among older adults in the USA: prevalence, comorbidity, and risk for new-onset psychiatric disorders in late life. International Journal of Geriatric Psychiatry. 2015;30(7):677–685. [DOI] [PubMed] [Google Scholar]
- 4.Yuan MZ, Fang Q, Liu GW, Zhou M, Wu JM, Pu CY. Risk Factors for Post-Acute Coronary Syndrome Depression: A Meta-analysis of Observational Studies. J Cardiovasc Nurs. Jan/Feb 2019;34(1):60–70. doi: 10.1097/JCN.0000000000000520 [DOI] [PubMed] [Google Scholar]
- 5.Buckland S, Pozehl B, Yates B. Depressive Symptoms in Women With Coronary Heart Disease. Journal of Cardiovascular Nursing. 2019;34(1):52–59. doi: 10.1097/JCN.0000000000000533 [DOI] [PubMed] [Google Scholar]
- 6.Meijer A, Conradi HJ, Bos EH, Thombs BD, van Melle JP, de Jonge P. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis of 25 years of research. General hospital psychiatry. 2011;33(3):203. [DOI] [PubMed] [Google Scholar]
- 7.Fan H, Yu W, Zhang Q, et al. Depression after heart failure and risk of cardiovascular and all-cause mortality: a meta-analysis. Preventive medicine. 2014;63:36–42. [DOI] [PubMed] [Google Scholar]
- 8.Connerney I, Sloan RP, Shapiro PA, Bagiella E, Seckman C. Depression is associated with increased mortality 10 years after coronary artery bypass surgery. Psychosomatic medicine. 2010;72(9):874–881. [DOI] [PubMed] [Google Scholar]
- 9.Kim J-M, Stewart R, Kang H-J, et al. Long-term cardiac outcomes of depression screening, diagnosis and treatment in patients with acute coronary syndrome: the DEPACS study. Psychological Medicine. 2020:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wändell P, Carlsson AC, Gasevic D, Wahlström L, Sundquist J, Sundquist K. Depression or anxiety and all-cause mortality in adults with atrial fibrillation–a cohort study in Swedish primary care. Annals of medicine. 2016;48(1-2):59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rafanelli C, Milaneschi Y, Roncuzzi R. Minor depression as a short-term risk factor in outpatients with congestive heart failure. Psychosomatics. 2009;50(5):493–499. [DOI] [PubMed] [Google Scholar]
- 12.Meyer ML, Lin F-C, Jaensch A, et al. Multi-state models of transitions in depression and anxiety symptom severity and cardiovascular events in patients with coronary heart disease. PloS one. 2019;14(3):e0213334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen RA, Gunstad J. Neuropsychology and cardiovascular disease. Oxford University Press, USA; 2010. [Google Scholar]
- 14.Riba M, Wulsin L, Rubenfire M, Ravindranath D. Psychiatry and heart disease: the mind, brain, and heart. John Wiley & Sons; 2012. [Google Scholar]
- 15.Burga MM. Intervention research on therapies that aim to treat depression and cardiovascular. Cardiovascular Implications of Stress and Depression. 2019:61. [Google Scholar]
- 16.Dickens C, Cherrington A, Adeyemi I, et al. Characteristics of psychological interventions that improve depression in people with coronary heart disease: a systematic review and meta-regression. Psychosomatic medicine. 2013;75(2):211–221. [DOI] [PubMed] [Google Scholar]
- 17.Jeyanantham K, Kotecha D, Thanki D, Dekker R, Lane DA. Effects of cognitive behavioural therapy for depression in heart failure patients: a systematic review and meta-analysis. Heart failure reviews. 2017;22(6):731–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pizzi C, Rutjes AWS, Costa GM, Fontana F, Mezzetti A, Manzoli L. Meta-analysis of selective serotonin reuptake inhibitors in patients with depression and coronary heart disease. The American journal of cardiology. 2011;107(7):972–979. [DOI] [PubMed] [Google Scholar]
- 19.Frey A, Saxon V-M, Popp S, et al. Early citalopram treatment increases mortality due to left ventricular rupture in mice after myocardial infarction. Journal of molecular and cellular cardiology. 2016;98:28–36. [DOI] [PubMed] [Google Scholar]
- 20.Nezafati MH, Eshraghi A, Vojdanparast M, Abtahi S, Nezafati P. Selective serotonin reuptake inhibitors and cardiovascular events: A systematic review. Journal of research in medical sciences: the official journal of Isfahan University of Medical Sciences. 2016;21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iasella CJ, Kreider MS, Huang L, Coons JC, Stevenson JM. Effect of Selective Serotonin Reuptake Inhibitors on Cardiovascular Outcomes After Percutaneous Coronary Intervention: A Retrospective Cohort Study. Clinical drug investigation. 2019:1–9. [DOI] [PubMed] [Google Scholar]
- 22.Jha MK, Qamar A, Vaduganathan M, Charney DS, Murrough JW. Screening and management of depression in patients with cardiovascular disease: JACC state-of-the-art review. Journal of the American College of Cardiology. 2019;73(14):1827–1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Luthar SS, Cicchetti D, Becker B. Research on resilience: Response to commentaries. Child development. 2000;71(3):573–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carver CS. Resilience and thriving: Issues, models, and linkages. Journal of social issues. 1998;54(2):245–266. [Google Scholar]
- 25.Lee S-Y, Tung H-H, Peng L-N, Chen L-K, Hsu C-I, Huang Y-L. Resilience among older cardiovascular disease patients with probable sarcopenia. Archives of gerontology and geriatrics. 2020;86:103939. [DOI] [PubMed] [Google Scholar]
- 26.Fonagy P, Steele M, Steele H, Higgitt A, Target M. The Emanuel Miller memorial lecture 1992 the theory and practice of resilience. Journal of child psychology and psychiatry. 1994;35(2):231–257. [DOI] [PubMed] [Google Scholar]
- 27.Resnick B, Gwyther L, Roberto KA. Resilience in aging. Springer; 2011. [Google Scholar]
- 28.Trivedi RB, Bosworth HB, Jackson GL. Resilience in chronic illness. Resilience in aging. Springer; 2011:181–197. [Google Scholar]
- 29.Yu X, Zhang J. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Social Behavior and Personality: an international journal. 2007;35(1):19–30. [Google Scholar]
- 30.Fujikawa M, Lee E-J, Chan F, Catalano D, Hunter C, Bengston K. The Connor-Davidson Resilience Scale as a Positive Psychology Measure for People With Spinal Cord Injuries. Rehabilitation Research, Policy & Education. 2013;27(3) [Google Scholar]
- 31.Dong X, Li G, Liu C, et al. The mediating role of resilience in the relationship between social support and posttraumatic growth among colorectal cancer survivors with permanent intestinal ostomies: A structural equation model analysis. European Journal of Oncology Nursing. 2017;29:47–52. [DOI] [PubMed] [Google Scholar]
- 32.Wu M, Yang Y, Zhang D, et al. Association between social support and health-related quality of life among Chinese rural elders in nursing homes: the mediating role of resilience. Quality of Life Research. 2018;27(3):783–792. [DOI] [PubMed] [Google Scholar]
- 33.Chang P-J, Yarnal C. The effect of social support on resilience growth among women in the Red Hat Society. The Journal of Positive Psychology. 2018;13(1):92–99. [Google Scholar]
- 34.Jiang W, Kuchibhatla M, Clary GL, et al. Relationship between depressive symptoms and long-term mortality in patients with heart failure. American heart journal. 2007;154(1):102–108. [DOI] [PubMed] [Google Scholar]
- 35.Gathright EC, Goldstein CM, Josephson RA, Hughes JW. Depression increases the risk of mortality in patients with heart failure: a meta-analysis. Journal of psychosomatic research. 2017;94:82–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stewart DE, Yuen T. A Systematic Review of Resilience in the Physically Ill. Psychosomatics. May-Jun 2011;52(3):199–209. doi: 10.1016/j.psym.2011.01.036 [DOI] [PubMed] [Google Scholar]
- 37.Gheshlagh RG, Sayehmiri K, Ebadi A, Dalvandi A, Dalvand S, Tabrizi KN. Resilience of patients with chronic physical diseases: A systematic review and meta-analysis. Iranian Red Crescent Medical Journal. 2016;18(7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cal SF, Sá LRd, Glustak ME, Santiago MB. Resilience in chronic diseases: A systematic review. Cogent Psychology. 2015;2(1):1024928. [Google Scholar]
- 39.Mueller M, D’Addario M, Egger M, et al. Methods to systematically review and meta-analyse observational studies: a systematic scoping review of recommendations. journal article. May 21 2018;18(1):44. doi: 10.1186/s12874-018-0495-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Franco OH, Karnik K, Osborne G, Ordovas JM, Catt M, van der Ouderaa F. Changing course in ageing research: the healthy ageing phenotype. Maturitas. 2009;63(1):13–19. [DOI] [PubMed] [Google Scholar]
- 41.Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health and quality of life outcomes. 2011;9(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Jama. 2000;283(15):2008–2012. [DOI] [PubMed] [Google Scholar]
- 43.National Heart L, and Blood Institute. Study Quality Assessment Tools. National Institutes of Health. Accessed December 4, 2019. https://www-nhlbi-nih-gov.proxy.library.upenn.edu/health-topics/study-quality-assessment-tools [Google Scholar]
- 44.Edward KL, Stephenson J, Giandinoto JA, et al. An Australian longitudinal pilot study examining health determinants of cardiac outcomes 12 months post percutaneous coronary intervention. Bmc Cardiovascular Disorders. Feb 2016;1631. doi: 10.1186/s12872-016-0203-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Thornton EW, Hallas C. Affective status following myocardial infarction can predict long term heart rate variability and blood pressure reactivity. British Journal of Health Psychology. 1999;4(3):231–245. [Google Scholar]
- 46.van Montfort E, Kupper N, Widdershoven J, Denollet J. Person-centered analysis of psychological traits to explain heterogeneity in patient-reported outcomes of coronary artery disease– the THORESCI study. Article. Journal of Affective Disorders. 2018;236:14–22. doi: 10.1016/j.jad.2018.04.072 [DOI] [PubMed] [Google Scholar]
- 47.Chang L-Y, Wu S-Y, Chiang C-E, Tsai P-S. Depression and self-care maintenance in patients with heart failure: A moderated mediation model of self-care confidence and resilience. European Journal of Cardiovascular Nursing. 2017;16(5):435–443. [DOI] [PubMed] [Google Scholar]
- 48.Liu J-C, Chang L-Y, Wu S-Y, Tsai P-S. Resilience mediates the relationship between depression and psychological health status in patients with heart failure: a cross-sectional study. International journal of nursing studies. 2015;52(12):1846–1853. [DOI] [PubMed] [Google Scholar]
- 49.Allabadi H, Alkaiyat A, Alkhayyat A, et al. Depression and anxiety symptoms in cardiac patients: a cross-sectional hospital-based study in a Palestinian population. Article. BMC public health. 2019;19(1):232. doi: 10.1186/s12889-019-6561-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Toukshati SR, Jovanovic A, Dehghani S, Tran T, Tran A, Hare DL. Low psychological resilience is associated with depression in patients with cardiovascular disease. Article. European Journal of Cardiovascular Nursing. 2017;16(1):64–69. doi: 10.1177/1474515116640412 [DOI] [PubMed] [Google Scholar]
- 51.Allabadi H, Probst-Hensch N, Alkaiyat A, et al. Mediators of gender effects on depression among cardiovascular disease patients in Palestine. BMC psychiatry. 2019;19(1):284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barreto FJN, Garcia FD, Prado PHT, et al. Childhood trauma and factors associated with depression among inpatients with cardiovascular disease. World Journal of Psychiatry. Jun 2017;7(2):106–113. doi: 10.5498/wjp.v7.i2.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. International journal of behavioral medicine. 2008;15(3):194–200. [DOI] [PubMed] [Google Scholar]
- 54.Kunschitz E, Friedrich O, Schoppl C, Maitz J, Sipotz J. Illness perception patterns in patients with Coronary Artery Disease. Psychology Health & Medicine. 2017;22(8):940–946. doi: 10.1080/13548506.2016.1271439 [DOI] [PubMed] [Google Scholar]
- 55.Wagnild G, Young H. Development and psychometric. Journal of nursing measurement. 1993;1(2):165–17847. [PubMed] [Google Scholar]
- 56.Beck AT, Ward C, Mendelson M, Mock J, Erbaugh J. Beck depression inventory (BDI). Arch Gen Psychiatry. 1961;4(6):561–571. [DOI] [PubMed] [Google Scholar]
- 57.Nelson CJ, Cho C, Berk AR, Holland J, Roth AJ. Are gold standard depression measures appropriate for use in geriatric cancer patients? A systematic evaluation of self-report depression instruments used with geriatric, cancer, and geriatric cancer samples. Journal of Clinical Oncology. 2010;28(2):348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Freedland KE, Steinmeyer BC, Carney RM, Rubin EH, Rich MW. Use of the PROMIS® Depression scale and the Beck Depression Inventory in patients with heart failure. Health Psychology. 2019;38(5):369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Knaster P, Estlander A-M, Karlsson H, Kaprio J, Kalso E. Diagnosing depression in chronic pain patients: DSM-IV major depressive disorder vs. Beck Depression Inventory (BDI). PloS one. 2016;11(3):e0151982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hare DL, Davis CR. Cardiac Depression Scale: validation of a new depression scale for cardiac patients. Journal of psychosomatic research. 1996;40(4):379–386. [DOI] [PubMed] [Google Scholar]
- 61.Pressler SJ, Subramanian U, Perkins SM, et al. Measuring depressive symptoms in heart failure: Validity and reliability of the Patient Health Questionnaire–8. American Journal of Critical Care. 2011;20(2):146–152. [DOI] [PubMed] [Google Scholar]
- 62.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. Journal of psychosomatic research. 2002;52(2):69–77. [DOI] [PubMed] [Google Scholar]
- 63.Kuman S, Awasthi P, Shankar O. Religious beliefs, patient-doctor interaction and resilience as predictors for treatment decisions and health outcomes of heart patients. Mental Health Religion & Culture. Apr 2019;22(4):423–436. doi: 10.1080/13674676.2019.1620190 [DOI] [Google Scholar]
- 64.Kumar S, Awasthi P, Shankar O. Religious beliefs, patient-doctor interaction and resilience as predictors for treatment decisions and health outcomes of heart patients. Mental Health Religion & Culture. doi: 10.1080/13674676.2019.1620190 [DOI] [Google Scholar]
- 65.Cohen MZ, Kupzyk KA, Holley LM, Katzman RM. Measuring resilience in two generations: psychometric properties of available instruments. Journal of Nursing Measurement. 2017;25(2):332–352. [DOI] [PubMed] [Google Scholar]
- 66.Eriksson M, Lindström B. Validity of Antonovsky’s sense of coherence scale: a systematic review. Journal of Epidemiology & Community Health. 2005;59(6):460–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gupta K Role of Resilience & Sense of Coherence in Subjective Improvement of Psychiatric Patients. Department of Humanities and Social Sciences, Indian Institute of Technology; …; 2015. [Google Scholar]
- 68.Bartone PT. A short hardiness scale. 1995. [Google Scholar]
- 69.Liu N, Liu SH, Yu N, et al. Correlations among Psychological Resilience, Self-Efficacy, and Negative Emotion in Acute Myocardial Infarction Patients after Percutaneous Coronary Intervention. Frontiers in Psychiatry. Jan 2018;91. doi: 10.3389/fpsyt.2018.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Low GD, Hubley AM. Screening for depression after cardiac events using the Beck Depression Inventory-II and the Geriatric Depression Scale. Social Indicators Research. 2007;82(3):527. [Google Scholar]
- 71.Davies B, Burrows G, Poynton C. A comparative study of four depression rating scales. Australian & New Zealand Journal of Psychiatry. 1975;9(1):21–24. [DOI] [PubMed] [Google Scholar]
- 72.Hammash MH, Hall LA, Lennie TA, et al. Psychometrics of the PHQ-9 as a measure of depressive symptoms in patients with heart failure. European Journal of Cardiovascular Nursing. 2013;12(5):446–453. [DOI] [PubMed] [Google Scholar]
- 73.Rogers WH, Adler DA, Bungay KM, Wilson IB. Depression screening instruments made good severity measures in a cross-sectional analysis. Journal of clinical epidemiology. 2005;58(4):370–377. [DOI] [PubMed] [Google Scholar]
- 74.Gabrys JB, Peters K. Reliability, discriminant and predictive validity of the Zung Self-Rating Depression Scale. Psychological Reports. 1985;57(3_suppl):1091–1096. [DOI] [PubMed] [Google Scholar]
- 75.Aalto A-M, Elovainio M, Kivimäki M, Uutela A, Pirkola S. The Beck Depression Inventory and General Health Questionnaire as measures of depression in the general population: a validation study using the Composite International Diagnostic Interview as the gold standard. Psychiatry research. 2012;197(1-2):163–171. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


