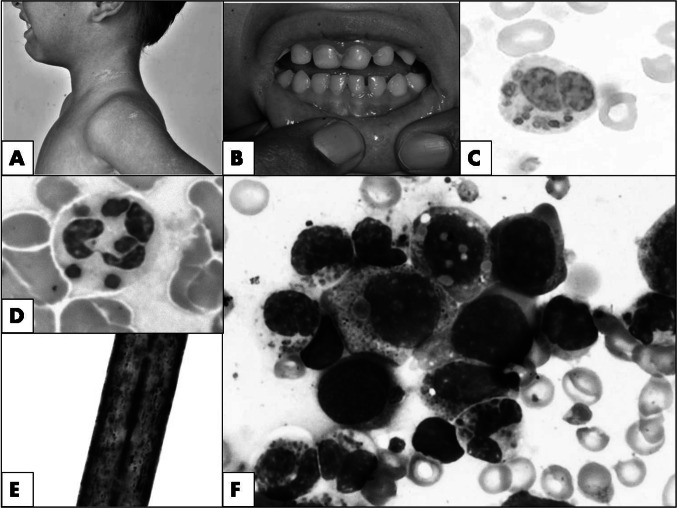
A 4-years-old boy presented with recurrent episodes of fever since 6 months of age associated with bilateral neck swellings, scalp abscesses and intermittent bilateral ear discharge requiring recurrent hospital admissions. On examination, he had microcephaly, diffuse skin hypopigmentation (Fig. 1a), silver-grey hair, pallor, periodontitis (Fig. 1b), generalized lymphadenopathy and hepatosplenomegaly. Investigations revealed hemoglobin of 70 g/L, platelet count 88 × 109/L, and total leukocyte count 6.7 × 109/L with an absolute neutrophil count of 0.873 × 109/L. Peripheral blood examination revealed discrete to multiple irregular large round-to-oval purple colored peroxidase positive intra-cytoplasmic inclusions (~ 1–2µ in diameter) in the neutrophils, lymphocytes and monocytes (Fig. 1c, d). Considering above findings, a diagnosis of Chédiak–Higashi syndrome (CHS) was considered. Hair-shaft microscopy revealed small regularly distributed clumps of melanin in the cortex (Fig. 1e). Bone marrow aspiration was done to identify the cause of cytopenia which showed similar granules in neutrophils and its precursors, monocytes and lymphocytes along with few haemophagocytic histiocytes (Fig. 1f). He was diagnosed as a case of CHS in accelerated phase and initiated on high-dose ascorbic acid (500 mg/day) with cotrimoxazole prophylaxis (60 mg/day). Genetic testing revealed mutation in LYST gene (c.10371delT), confirming the diagnosis of CHS.
Fig. 1.
a Child showing diffuse hypopigmentation of skin with intermittent areas of normal pigmentation; b showing periodontitis; c peripheral blood film with Chédiak–Higashi granules in a neutrophil (Leishman stain, ×1000); d strong myeloperoxidase positivity in the granules (Myeloperoxidase stain, ×1000). e polarizing light microscopy showing melanin clumps in a hair shaft (×400); f bone marrow aspirate smear showing coarse Chédiak–Higashi granules in the neutrophils, promyelocytes and myelocytes (May–Grünwald Giemsa stain, ×1000)
CHS shows characteristic clinical and laboratory findings [1, 2]. The present report emphasizes the importance of morphology in the era of molecular diagnosis especially imperative in resource limiting settings where genetic studies are not readily available. The index case could have been diagnosed earlier with a simple and careful peripheral smear examination instigating an earlier treatment which would have reduced the morbidities sustained.
Author’s Contribution
AS, AJ: concept and design of work; PS, AJ, RTI: analysis and Interpretation of data; AS, PS, RTI: drafted the work; NV, AR: critical revision of the article, approved final version of the article.
Funding
None.
Availability of Data and Materials
The patient data is available on request from the corresponding author.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics Approval
Departmental Review Board Approval was obtained for the study.
Human Participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. A detailed informed consent from the parents was taken for publication purposes.
Consent to Participate
Written informed consent was obtained.
Consent for Publication
Patients signed informed consent regarding publishing their data.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ankita Singh, Email: drankitakgmc123@gmail.com.
Ankur Kumar Jindal, Email: ankurjindal11@gmail.com.
Raviteja Indla, Email: raviteja733@gmail.com.
Praveen Sharma, Email: dr_praveen05@yahoo.co.in.
Neelam Varma, Email: varmaneelam@yahoo.com.
Amit Rawat, Email: rawatamit@yahoo.com, Email: amitrawat2002@rediffmail.com.
References
- 1.Rudramurthy P, Lokanatha H. Chediak–Higashi syndrome: a case series from Karnataka, India. Indian J Dermatol. 2015;60(5):524. doi: 10.4103/0019-5154.159662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carneiro IM, Rodrigues A, Pinho L, et al. Chediak–Higashi syndrome: lessons from a single-centre case series. Allergol Immunopathol (Madr) 2019;47(6):598–603. doi: 10.1016/j.aller.2019.04.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The patient data is available on request from the corresponding author.