Abstract
Background:
Scapular assessment is important in examining overhead athletes, but there is inconsistency in scapular clinical assessment and its relation to pathology.
Purpose:
To determine the relationship between clinical scapular assessment and biomechanical scapula resting position, shoulder strength, and pitching shoulder kinematics and kinetics.
Study Design:
Descriptive laboratory study.
Methods:
Two clinicians performed scapular assessments and graded the scapula as presence or absence of scapular dyskinesis. Shoulder external rotation (ER) and internal rotation (IR) strength were collected. The 3-dimensional biomechanics of the scapula resting position (upward/downward rotation, IR/ER, and anterior/posterior tilt) were assessed while participants stood at rest, and pitching kinematics (maximum shoulder ER, shoulder abduction, shoulder horizontal abduction, shoulder rotation velocity) and kinetics (maximum shoulder distraction force) were assessed when participants pitched off the portable pitching mound that was engineered to meet major league specifications.
Results:
A total of 33 high school baseball pitchers (age, 16.3 ± 1.2 years; height, 184.0 ± 6.9 cm; weight, 76.8 ± 20.8 kg; hand dominance: left, 9 [27%]; right, 24 [73%]; pitch velocity, 34.7 ± 2.3 m/s) participated in this study. Of them, 15 participants had scapular dyskinesis, and 18 had normal scapulothoracic rhythm. No differences were observed for upward/downward rotation or anterior/posterior tilt, shoulder ER, shoulder abduction, or shoulder distraction force, based on the presence of scapular dyskinesis. Pitchers with scapular dyskinesis demonstrated significantly greater scapular resting IR position (effect size [ES], 0.80; 95% CI, 0.06 to 1.54; P = .020), greater nondominant shoulder ER to IR strength ratio (ES, 0.49; 95% CI, –0.02 to 1.00; P = .018), and decreased shoulder rotation velocity (ES, 14.66; 95% CI: 12.06 to 17.25; P = .016). Pitchers with greater anterior tilt demonstrated greater shoulder rotation velocity (r = –0.48; P = .006).
Conclusion:
Pitchers with scapular dyskinesis had greater scapular IR, greater nondominant shoulder ER to IR strength ratio, and reduced shoulder rotation velocity.
Clinical Relevance:
Scapular assessment may be more influenced by differential IR than upward rotation or anterior tilt. Scapular dyskinesis has no competitive performance advantage among amateur athletes. Greater understanding is needed to decipher the critical threshold between beneficial and maladaptive scapular movement patterns.
Keywords: baseball, scapular internal rotation, anterior tilt, shoulder rotation velocity
Previous studies in the literature have demonstrated high injury rates among baseball pitchers across all ages groups and skill levels. 14,32,34 In particular, upper extremity injuries account for 63% of all injuries among high school pitchers, 34 and shoulder injuries have the highest incidence, with 1.39 to 1.90 injuries per 1000 athlete-exposures. 3,18,33 Baseball shoulder injuries have been attributed to physiologic variables including decreased total range of motion 39 and shoulder strength. 7,42 Additionally, impaired scapular position and arthrokinematics may also play an underlying and integral role in development of these injuries. 4,19,28 As a result, clinicians have attempted to quantify scapular posture and arthrokinematics to more effectively address potential pitching shoulder injuries. 5,17,38
The scapulothoracic joint is the complex articulation between the surface of the thoracic cavity and the anterior surface of the scapula, and it confers a stable foundation for the glenohumeral joint during the pitching motion. 27,31 The scapula demonstrates 6 degrees of freedom and moves in 3 dimensions (ie, upward/downward rotation, internal/external rotation [IR/ER], and anterior/posterior tilt), providing dynamic shoulder alignment with the trunk during pitching. 16,24,27 The scapula also allows for fluid movement of other structures in the shoulder; for example, it upwardly rotates during shoulder abduction, providing sufficient subacromial space for rotator cuff contraction. 12,17 Without appropriate scapular alignment and arthrokinematics, impaired periscapular muscle function can ultimately contribute to the development of overuse shoulder pathology or secondary injury. 5,27 For instance, the literature has shown that individuals with subacromial impingement have decreased upward rotation of the scapula and increased anterior tilting compared with patients without impingement. 21 Alternatively, other studies have demonstrated that overhead athletes with impingement exhibit decreased protraction compared with healthy overhead athlete controls. 9
Clinical assessments of scapular function have been found to be of paramount importance in examining overhead athletes. 5,17 Historically, there have been inconsistencies in the methods for evaluating functional scapular motion clinically, and the fundamental role of aberrant scapular motion in the later development of shoulder pathology remains unclear. 27,38 Previous techniques for scrutinizing scapular position have been limited by poor reliability and dependence on 2-dimensional analysis. 30,38 In turn, scapular evaluation methods have evolved to using an overarching assessment for the presence of normal scapular arthrokinematics (eg, an absence of scapular dyskinesis) with or without 3-dimensional (3-D) biomechanical techniques, which have greater reliability. 27,31,38 Despite these changes, there is still controversy over what constitutes appropriate scapular posture and arthrokinematics in overhead athletes as they relate to athletic performance and overall shoulder health and to avoidance of secondary shoulder injury. 27,31 It has been theorized that scapular dyskinesis in overhead athletes encompasses asymmetrical posture and movement, with classic features of increased anterior tilt, internal rotation, and upward rotation. 5 Conversely, healthy overhead athletes have been found to predominantly display these same scapular positions, possibly suggesting that this is a necessary adaptation for high-level throwing performance. 27,31 However, based on the current literature, it remains uncertain whether these scapular adaptations contribute to shoulder velocity and force generation or just to an increased risk of structural pathology and possible shoulder injury. 31
While scapular dyskinesis has been observed to contribute to shoulder injury in some throwers, 27,28 few studies have investigated how dynamic scapular position relates to resting posture, shoulder strength, and pitching velocity and shoulder force generation. As such, the purpose of this study was to determine the relationship of clinical scapular assessment with biomechanical scapula resting position, shoulder strength, and pitching shoulder kinematics and kinetics. Our primary hypothesis was that the presence of clinically identified scapular dyskinesis would result in decreased shoulder strength, altered pitching shoulder kinematics, and increased shoulder distraction force. Our secondary hypothesis was that the scapular resting posture would be associated with baseball pitching shoulder kinematics and kinetics.
Methods
Study Design
After receiving institutional review board approval, we retrospectively analyzed data from reports generated as part of a pitching evaluation. A total of 33 high school baseball pitchers from regional high schools and baseball academies participated in a pitching evaluation at the Wake Forest Pitching Laboratory between June 2019 and August 2019. Inclusion criteria consisted of the following: adolescent baseball athletes from all competition levels, for whom pitcher was their primary or secondary position, and aged 14 to 19 years. Players were excluded if they reported pain during any testing; had undergone surgery in the past 12 months; or were not participating in all baseball-related training, practices, or games at the time of initial testing. As part of the pitching evaluation, all pitchers had a clinical scapular assessment and completed a 3-D biomechanical evaluation. Participants performed all clinical assessments before warm-up and biomechanical pitching assessment. All participants and their parents were informed of the risks and benefits of study participation, and participants and/or their parents gave oral and written assent and/or consent before study participation.
Scapular Assessment
Two clinicians, 1 who was an athletic trainer (J.S.) and 1 who was a physical therapist (G.S.B.), independently performed all scapular assessments. Participants were instructed to stand with their shirts off and feet together. They began the test with arms by their sides, arms straight, and shoulders in a neutral position. Participants were instructed to raise their arms at a 3-second count, with “thumbs up” as far as they could overhead. They performed 5 trials of shoulder elevation in the sagittal and scapular planes. The examiner observed the medial and superior scapular borders during rest and active elevation and scored normal scapular arthrokinematics, subtle scapular dyskinesis, and obvious scapular dyskinesis. Each scapula was evaluated independently for scapulohumeral rhythm, which has been found to have high reliability and validity. 23,37 For the purpose of analyses, clinical scapular assessment grading was then reduced to presence of scapular dyskinesis and normal scapular arthrokinematics, which has been previously determined to have higher sensitivity and positive predictive value in comparison with the 3-D scapular assessment method. 38
Shoulder Strength
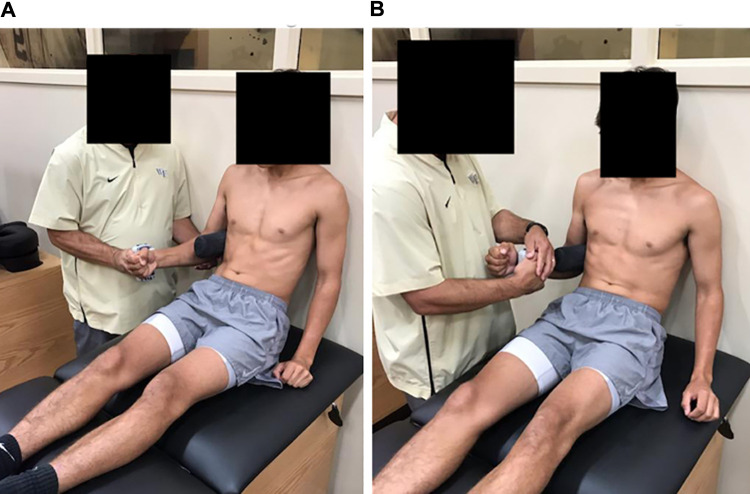
ER and IR shoulder strength was measured for dominant and nondominant arms. 13 A handheld dynamometer (Lafayette Manual Muscle Test System, Model 01165; Lafayette Instruments) was used in all testing. A handheld dynamometer has been observed to be valid and have excellent reliability in healthy adults and adolescent or high-level athletes. 6,22,26,35,36 A “make test” (as opposed to a “break test”) was used in the testing protocol because of the higher reliability of the “make test” when using a handheld dynamometer. 35 Participants sat upright on a treatment table with their backs against the wall for support. A rolled towel was placed under the arm against the axilla. Participants flexed the elbow to 90° with their wrist and hand in a neutral position (“thumbs up” position). 7 The handheld dynamometer was placed on the proximal dorsal wrist surface for ER and volar surface for IR (Figure 1). 13 Participants were instructed to maximally externally or internally rotate their arm at 0° of abduction while not abducting or adducting their shoulder. 7 Each test (ER and IR) was performed 3 times for each arm, with the results reported in newtons, and the mean was used for final analysis. 15 Variables included in the study were dominant and nondominant ER and IR shoulder strength, the ratio of dominant and nondominant ER to IR shoulder strength, and the difference between dominant and nondominant ER and IR shoulder strength. 7
Figure 1.
Shoulder testing for (A) external rotation strength and (B) internal rotation strength.
Biomechanical Analysis
3-D motion data were collected using the 40 reflective marker set required for PitchTrak (Motion Analysis Corporation) and a 16-camera motion analysis system (Motion Analysis Corporation). Motion data were collected at 250 Hz. Before pitching, a static trial was collected with players standing in a neutral position facing the home plate, with their feet a shoulder-width apart and their arms down by their sides. While standing in this position, scapular landmarks were palpated, and markers were placed on the trigonum spinae and inferior angle of each scapula (Figure 2). A lumbosacral marker was placed at L5 for spatial reference. This enabled the calculation of scapula resting position during the static trial with the addition of the marker on the acromion process. Participants then pitched off of the Perfect Mound (Porta-Pro Mounds Inc), which was engineered to meet major league specification. Pitchers were allowed to wear their cleats. Ball velocity was recorded using a Trackman device (Trackman).
Figure 2.

Resting scapular position with marker placement.
Each pitcher went through an individualized pregame 15-minute warm-up period, which consisted of throwing to 36 m. After the warm-up, each pitcher pitched 4 fastballs, 4 breaking balls, and 4 changeups to a catcher receiving throws at a regulation distance (18.4 m). Only the fastball data were analyzed for this study. Each individual fastball was analyzed separately. Data were processed and kinematic variables were calculated using Visual3D (C-Motion, Inc). Pitching models were defined using the PitchTrak model, and segment coordinate systems were defined according to International Society of Biomechanics recommendations. 1,41 Scapulothoracic angles were calculated to represent scapula resting position. Because PitchTrak uses the scapular markers to build trunk coordinate systems, a modified trunk coordinate system was used for scapulothoracic calculations: vertical axis from the midpoint between the sacral marker and the midpoint between the anterior superior iliac spine markers to the midpoint between the acromion markers, transverse axis perpendicular to the plane defined by the 2 vertical axis points and the clavicle marker, and anterior axis mutually perpendicular. The scapular coordinate system was created as a slight modification of International Society of Biomechanics recommendations: the acromion process was substituted for the acromial angle. 41 Angles were calculated using a helical approach 40 and resolved onto anatomic axes to avoid any singularities associated with Euler sequences. Anatomic axes were defined as follows: upward/downward rotation occurs about the X axis, IR/ER occurs about the Y axis, and anterior/posterior tilt occurs about the Z axis. The absolute value of rotation about the Y axis was used to enable comparison of left and right scapulae. Variables extracted from the pitching reports included resting scapular position (X, Y, and Z position), maximum shoulder ER, maximum shoulder abduction, maximum shoulder horizontal abduction, maximum shoulder rotation velocity, and maximum shoulder distraction force. Shoulder distraction force was normalized by body weight.
Statistical Analysis
We performed an a priori analysis using a β of 0.80 and an α of .05 that determined a sample size of 15 was necessary to observe a moderate correlation of 0.30 between presence of scapular dyskinesis and scapular kinematics. 8 All range of motion and velocity averages are reported as degree or degree/s ± SD unless otherwise stated. Before analyses, data were evaluated for normality. Data were observed to have a nonnormal distribution for scapula resting position, shoulder strength, and shoulder kinematic and kinetic data. Data transformations were then attempted for postural, strength, and kinematic data without success. Mann-Whitney U tests were performed to analyze the difference between presence of scapular dyskinesis and normal scapular arthrokinematics for scapula resting position, shoulder strength, and shoulder pitching kinematics and kinetics (P < .05). If a statistically significant difference was found between presence of scapular dyskinesis and normal scapular arthrokinematics clinical assessments, Cohen d effect size (ES) calculations were performed. A series of nonparametric Spearman rho correlations were then performed to investigate the relationship between scapula resting position and shoulder pitching kinematics and kinetics (P < .05). All analyses were performed using R Version 3.5.1 (R Core Team).
Results
Data from 33 high school pitchers (mean ± SD age, 16.3 ± 1.2 years; height, 184.0 ± 6.9 cm; weight, 76.8 ± 20.8 kg; hand dominance: left, 9 [27%]; right, 24 [73%]; pitch velocity, 34.7 ± 2.3 m/s) were included in this study. A total of 15 participants (primary pitcher, n = 10; secondary pitcher, n = 5; left-handed, n = 6; right-handed, n = 9) were graded as having scapular dyskinesis (obvious scapular dyskinesis, n = 5; subtle scapular dyskinesis, n = 10), and 18 were graded as having normal scapular arthrokinematics. Table 1 demonstrates measured scapula resting positions, and Table 2 demonstrates shoulder strength and shoulder pitching kinematics.
Table 1.
Scapula Resting Position a
| Scapula resting position, deg b | Dominant Scapula | Nondominant Scapula | Difference |
|---|---|---|---|
| Upward/downward rotation (X) | 18.27 ± 4.83 | 17.71 ± 5.81 | 0.56 ± 3.59 |
| Internal/external rotation (Y) | 137.93 ± 5.14 | 139.57 ± 6.80 | –1.64 ± 7.22 |
| Anterior/posterior tilt (Z) | 0.63 ± 9.84 | –4.26 ± 9.51 | 4.89 ± 9.23 |
a Data are reported as mean ± SD.
bX position = upward rotation is positive; Y position = internal rotation is positive; Z position = anterior tilt is negative.
Table 2.
Shoulder Strength and Kinematics During Pitching a
| Mean ± SD | |
|---|---|
| ER shoulder strength, N | |
| Dominant ER | 101.9 ± 22.7 |
| Nondominant ER | 98.3 ± 30.0 |
| Dominant vs nondominant | 3.6 ± 21.6 |
| IR shoulder strength, N | |
| Dominant IR | 135.7 ± 37.1 |
| Nondominant IR | 136.7 ± 42.6 |
| Dominant vs nondominant | –1.0 ± 19.6 |
| Dominant ER:IR ratio, % | 78.2 ± 17.1 |
| Nondominant ER:IR ratio, % | 73.5 ± 19.0 |
| Pitching shoulder kinematics | |
| Maximum shoulder ER, deg | 175.98 ± 6.82 |
| Maximum shoulder abduction, deg | 92.55 ± 16.13 |
| Maximum horizontal shoulder abduction, deg | –41.82 ± 15.52 |
| Maximum shoulder rotation velocity, deg/s | 4830 ± 466 |
| Maximum shoulder distraction force, % BW | 132.59 ± 23.29 |
a BW, body weight; ER, external rotation; IR, internal rotation.
Pitchers with scapular dyskinesis demonstrated significantly greater dominant scapula resting IR (Y) (P = .020; ES, 0.80; 95% CI, 0.06 to 1.54), a greater difference between dominant and nondominant scapula resting IR (P = .011; ES: –0.43; (95% CI, –0.92 to 0.07), greater nondominant shoulder ER to IR strength ratio (P = .018; ES: 0.49; 95% CI, –0.02 to 1.00), and decreased maximum shoulder rotation velocity (P = .016; ES: 14.66; 95% CI, 12.06 to 17.25) compared with pitchers with normal scapular arthrokinematics (Table 3).
Table 3.
Differences Between Presence of Scapular Dyskinesis or Normal Scapular Arthrokinematics Clinical Assessments a
| Presence of Scapular Dyskinesis | Normal Scapular Arthrokinematics | P Value | |
|---|---|---|---|
| Scapula resting position b | |||
| Dominant upward/downward rotation (X), deg | 19.88 ± 4.11 | 16.92 ± 5.07 | .135 |
| Dominant IR/ER (Y), deg | 140.03 ± 5.02 | 136.19 ± 4.68 | .020 |
| Dominant anterior/posterior tilt (Z), deg | 4.09 ± 7.57 | –2.25 ± 10.75 | .079 |
| Dominant vs nondominant upward/downward rotation (X), deg | 0.78 ± 0.38 | 0.38 ± 3.77 | .630 |
| Dominant vs nondominant IR/ER (Y), deg | 1.95 ± 5.33 | –4.63 ± 7.33 | .011 |
| Dominant vs nondominant anterior/posterior tilt (Z), deg | 5.89 ± 10.07 | 4.07 ± 8.68 | .464 |
| ER shoulder strength, N | |||
| Dominant | 99.9 ± 27.1 | 103.6 ± 18.8 | .792 |
| Nondominant | 100.5 ± 20.1 | 96.3 ± 32.3 | .464 |
| Dominant vs nondominant | –0.6 ± 13.2 | 7.3 ± 26.8 | .533 |
| IR shoulder strength, N | |||
| Dominant | 131.3 ± 41.7 | 139.4 ± 33.6 | .911 |
| Nondominant | 126.6 ± 42.5 | 145.2 ± 41.9 | .219 |
| Dominant vs nondominant | 4.7 ± 20.0 | –5.8 ± 18.5 | .206 |
| Dominant ER:IR ratio, % | 79.8 ± 21.0 | 76.8 ± 13.3 | .999 |
| Nondominant ER:IR ratio, % | 81.3 ± 12.8 | 66.5 ± 21.2 | .018 |
| Dominant (pitching) shoulder kinematics | |||
| Maximum shoulder ER, deg | 176.38 ± 5.10 | 175.67 ± 8.04 | .837 |
| Maximum shoulder abduction, deg | 90.39 ± 7.29 | 94.35 ± 15.37 | .492 |
| Maximum horizontal shoulder abduction, deg | –48.63 ± 17.15 | –36.16 ± 11.67 | .060 |
| Maximum shoulder rotation velocity, deg/s | 4630 ± 398 | 4999 ± 461 | .016 |
| Maximum shoulder distraction force, % BW | 124.40 ± 24.9 | 137.00 ± 19.7 | .156 |
a Data are reported as mean ± SD. Statistically significant (P < .05) differences are in bold. BW, body weight; ER, external rotation; IR, internal rotation.
bX position = upward rotation is positive; Y position = internal rotation is positive; Z position = anterior tilt is negative.
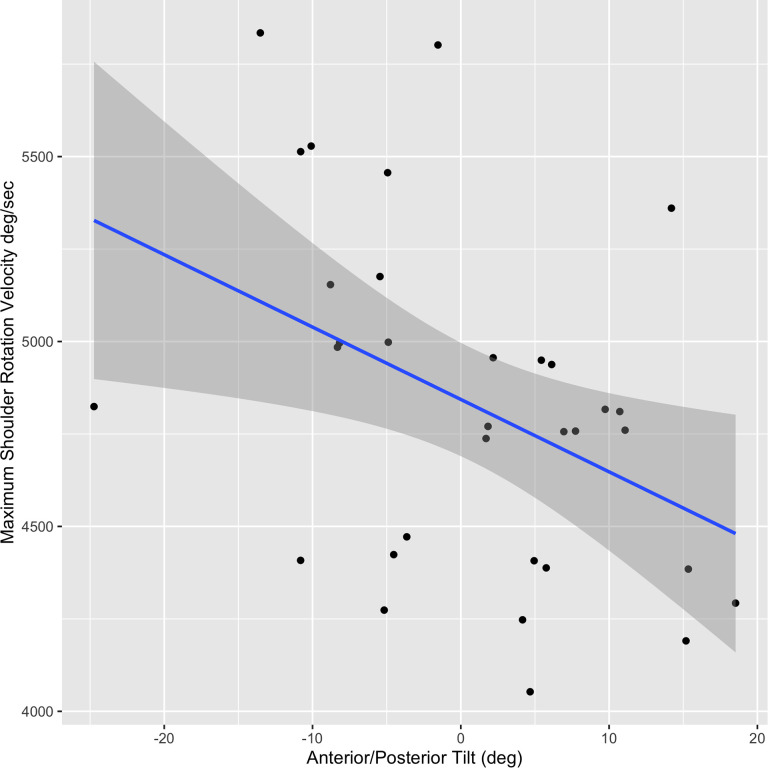
There was a statistically significant moderate association between pitchers with greater dominant anterior tilt demonstrating greater maximum shoulder rotation velocity (r = –0.48, P = .006) (Figure 3). However, no other correlations were significant (Table 4).
Figure 3.
Relationship between scapular anterior/posterior tilt and maximum pitching shoulder rotation velocity.
Table 4.
Relationship Between Scapula Resting Position and Pitching Shoulder Kinematics a
| Dominant (Pitching) Shoulder b | Difference, Dominant vs Nondominant b | ||||||
|---|---|---|---|---|---|---|---|
| X Position | Y Position | Z Position | X Position | Y Position | Z Position | ||
| Maximum shoulder ER | 0.007 | –0.157 | 0.228 | –0.144 | –0.209 | 0.314 | |
| P value | .969 | .39 | .209 | .43 | .249 | .081 | |
| Maximum shoulder abduction | 0.086 | –0.045 | –0.145 | –0.097 | –0.261 | 0.222 | |
| P value | .633 | .806 | .422 | .59 | .143 | .21 | |
| Maximum shoulder horizontal abduction | 0.194 | –0.264 | –0.218 | –0.076 | –0.265 | 0.168 | |
| P value | .278 | .138 | .223 | .674 | .136 | .35 | |
| Maximum shoulder rotation velocity | 0.016 | –0.0832 | –0.475 | –0.017 | –0.327 | 0.013 | |
| P value | .928 | .644 | .006 | .924 | .063 | .945 | |
| Maximum shoulder distraction force | –0.173 | –0.064 | –0.312 | –0.219 | –0.258 | 0.065 | |
| P value | .344 | .727 | .082 | .228 | .154 | .725 | |
a Statistically significant correlations are in bold. ER, external rotation.
bX position = upward/downward rotation; Y position = internal/external rotation; Z position = anterior/posterior tilt.
Discussion
The principal findings of the current study were that pitchers with clinically identified scapular dyskinesis had greater postural scapular IR compared with pitchers with normal scapular arthrokinematics. Furthermore, pitchers with clinically identified scapular dyskinesis had greater nondominant shoulder ER to IR strength ratio and reduced shoulder rotation velocity in comparison with pitchers with clinically identified normal scapular arthrokinematics. Last, those with greater scapular anterior tilt had greater shoulder rotation velocity in comparison with pitchers with posterior tilt. These findings may translate clinically, as previous studies have demonstrated that scapular dyskinesis is a risk factor for shoulder injury and pathology in overhead athletes. 5,9
Pitchers with clinically identified scapular dyskinesis had greater postural scapular IR in comparison with pitchers who had clinically determined normal scapular arthrokinematics. Greater scapular IR is associated with increased medial border prominence on physical examination, and this has been associated with a muscle imbalance between the upper trapezius and serratus anterior activity, 21 particularly in overhead throwing athletes with shoulder injuries. 9 Some authors have proposed this as a maladaptive pattern stemming from the unique repetitive demands from overhand throwing. 10 In the current study, while greater scapular IR was prominent throughout the dyskinesis group, the scapular posture for all pitchers (scapular dyskinesis and normal scapular arthrokinematics) exhibited comparable upward rotation and neutral anterior/posterior tilt. Furthermore, while not statistically different, pitchers determined to have normal scapular arthrokinematics displayed greater anterior tilt, which has been hypothesized in previous literature to be a sign of scapular dyskinesis. 5,17 These findings suggest that scapular assessment may be more influenced by differential IR than by upward rotation or anterior tilt. For example, during scapular visual inspection, increased medial border prominence is perceived to be in a “dropped” position, potentially giving more weight to this scapula resting position. 27 Determining the influence of different scapular postural dimensions could assist in more effectively identifying subtle scapular dyskinesis.
Pitchers with scapular dyskinesis exhibited greater nondominant shoulder ER to IR strength ratio than did pitchers with normal scapular arthrokinematics. Furthermore, the reported strength ratios ranging from 67% to 81% were similar to those reported for high school and collegiate baseball pitchers. 2,25,29 While pitchers with scapular dyskinesis demonstrated a greater nondominant shoulder ER to IR strength ratio than did pitchers with normal scapular arthrokinematics, the dominant shoulder strength ratio was similar between scapular groups. Overall, there were little shoulder strength differences between pitchers with scapular dyskinesis and normal scapular arthrokinematics, indicating the lack of a power advantage. These data suggest that other outside factors may have a more prominent role in the development of scapular dyskinesis and abnormal scapular rhythm, including starting upper quarter posture and periscapular muscle timing. 5
Pitchers with scapular dyskinesis had reduced maximum shoulder rotation velocity versus pitchers with normal scapular arthrokinematics. Importantly, shoulder rotation velocity has been found to be integral to pitching velocity and a key determinant of performance. 11 Periscapular muscle imbalance and improper scapular arthrokinematics timing are proposed factors relating to dyskinesis. 5,17 For example, during the pitching motion, the scapula provides 3-D dynamic stability to the shoulder. 27,31 Periscapular muscle imbalances can contribute to decreased force production and muscle timing. 9 Thus, these muscle imbalances could potentially lead to impaired scapulothoracic alignment and/or timing with the shoulder during pitching, potentially decreasing shoulder rotation velocity.
Pitchers with increased scapular anterior tilt at rest had greater shoulder rotation velocity in comparison with pitchers with posteriorly tilted resting scapula. Anterior tilt has been proposed to be a fundamental feature of dyskinesis. 5,17 However, it has been hypothesized that overhead athletes require specific scapular adaptations to throw at a high level. 27 Greater scapular anterior tilt has been associated with increased levator scapulae and upper trapezius muscle activity. 20 During the pitching motion, the trapezius and levator scapulae had high muscle activity during the cocking and acceleration phases, 10 and this may be required to produce high shoulder rotation velocity. Despite these scapular adaptations, repeated throwing exposure may predispose the athlete to greater injury risk. 27 Increased anterior tilt has been related to decreased glenohumeral IR and subacromial impingement in overhead athletes, 4 demonstrating that there is an adaption threshold between performance and increased injury risk in overhead athletes. Furthermore, there is a need to understand if resting scapular anterior tilt persists during pitching, especially during the cocking and acceleration phases. 10 Elucidating the association between scapula resting and dynamic position can improve clinicians’ understanding of the necessity of targeted clinical interventions on a throwing athlete’s scapular postural position.
Scapular dyskinesis in throwing athletes has been associated with shoulder pathology, particularly internal impingement, articular-sided rotator cuff injury, and biceps-superior labral complex disease. 27,28 Static postural and dynamic scapular biomechanical analyses have been conducted in overhead athletes, 27,31 but these evaluations have not been assessed throughout the throwing motion. There is a need to more thoroughly investigate throwing dynamic scapular motion to further elucidate the interplay among the trunk, scapula, and shoulder. These data can assist in better understanding of throwing injury mechanisms. Furthermore, more research is required to understand the threshold between positive and maladaptive scapular adaptation in throwers.
Strengths and Potential Limitations
The strengths of the current study are that experienced baseball-specific clinicians were involved in performing scapular assessment. Additionally, all pitchers’ scapulae were assessed through both clinical and biomechanical examination. Participants underwent assessments of shoulder strength and 3-D analysis of their pitching motion, giving a multidimensional investigation of the relationship between clinical scapular assessment and shoulder strength and scapula resting position. However, only scapula resting position was biomechanically analyzed, without dynamic scapular analysis, decreasing the generalizability of these findings. Each pitch type (ie, fastball, curveball, changeup) was pitched in a specific order, potentially creating an order effect. Only fastballs were analyzed, with other pitch types potentially having slight differences in kinematic variables. There was a potential for selection bias, as only regional high school pitchers were included in this study. Only shoulder ER and IR strengths were assessed at 0° of abduction, without testing the entire rotator cuff or periscapular musculature. Scapular posture and arthrokinematics are influenced by the shoulder and periscapular musculature, decreasing the clinical applicability of these findings. Other scapular assessments are available, such as the lateral scapular slide test. Using only 1 method of scapular assessment decreased the clinical generalizability of these results. There was some skin movement between the reflective markers and the anatomic landmarks that the markers were signifying, potentially decreasing the precision of these findings. However, this limitation was potentially minimized by placing markers directly on bony landmarks. There was a potential for type 2 error due to combining the scapular dyskinesis groups, decreasing the precision of these findings. There was a potential for confounding variables such as previous injury history and chronicity of scapular dyskinesis that increased the potential bias in these results. Only high school pitchers participated in this study, potentially decreasing the generalizability of these findings to higher levels of competition. Last, no clinical injury data were available for this sample. Future prospective longitudinal studies are needed to understand how these scapular assessments relate to pitching arm injuries.
Conclusion
Pitchers with identifiable scapular dyskinesis had greater scapular IR, greater nondominant shoulder ER to IR strength ratio, and reduced shoulder rotation velocity in comparison with pitchers with normal scapular arthrokinematics. Clinical scapular assessment was more influenced by IR than upward rotation or anterior tilt when determining scapular dyskinesis. Scapular dyskinesis provided no competitive performance advantage among amateur athletes, but these differences could identify potential injury risk and lower maximum shoulder velocity. Future studies with a prospective follow-up of this cohort are needed. Greater understanding is needed to decipher the threshold between positive and maladaptive scapular adaption in throwers.
Footnotes
Final revision submitted September 14, 2020; accepted November 11, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: B.R.W. has received research support from Arthrex and Encore Medical; educational support from Medwest, Smith & Nephew, and Arthrex; honoraria from Vericel; and hospitality payments from Wright Medical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Wake Forest University (study No. IRB00060712).
References
- 1. Aguinaldo AL, Buttermore J, Chambers H. Effects of upper trunk rotation on shoulder joint torque among baseball pitchers of various levels. J Appl Biomech. 2007;23(1):42–51. [DOI] [PubMed] [Google Scholar]
- 2. Alderink GJ, Kuck DJ. Isokinetic shoulder strength of high school and college-aged pitchers. J Orthop Sports Phys Ther. 1986;7(4):163–172. [DOI] [PubMed] [Google Scholar]
- 3. Bonza JE, Fields SK, Yard EE, Comstock RD. Shoulder injuries among United States high school athletes during the 2005-2006 and 2006-2007 school years. J Athl Train. 2009;44(1):76–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Borich MR, Bright JM, Lorello DJ, Cieminski CJ, Buisman T, Ludewig PM. Scapular angular positioning at end range internal rotation in cases of glenohumeral internal rotation deficit. J Orthop Sports Phys Ther. 2006;36(12):926–934. [DOI] [PubMed] [Google Scholar]
- 5. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology part I. Pathoanatomy and biomechanics. Arthroscopy. 2003;19(4):404–420. [DOI] [PubMed] [Google Scholar]
- 6. Byl NN, Richards S, Asturias J. Intrarater and interrater reliability of strength measurements of the biceps and deltoid using a hand held dynamometer. J Orthop Sports Phys Ther. 1988;9(12):395–398. [DOI] [PubMed] [Google Scholar]
- 7. Byram IR, Bushnell BD, Dugger K, Charron K, Harrell FE, Jr, Noonan TJ. Preseason shoulder strength measurements in professional baseball pitchers: identifying players at risk for injury. Am J Sports Med. 2010;38(7):1375–1382. [DOI] [PubMed] [Google Scholar]
- 8. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Revised edition. Routledge; 2013. [Google Scholar]
- 9. Cools AM, Witvrouw EE, Mahieu NN, Danneels LA. Isokinetic scapular muscle performance in overhead athletes with and without impingement symptoms. J Athl Train. 2005;40(2):104. [PMC free article] [PubMed] [Google Scholar]
- 10. DiGiovine NM, Jobe FW, Pink M, Perry J. An electromyographic analysis of the upper extremity in pitching. J Shoulder Elbow Surg. 1992;1(1):15–25. [DOI] [PubMed] [Google Scholar]
- 11. Dillman C. Valgus extension overload in baseball pitching. Med Sci Sports Exerc. 1991;23:S153. [Google Scholar]
- 12. Fleisig GS, Barrentine SW, Zheng N, Escamilla RF, Andrews JR. Kinematic and kinetic comparison of baseball pitching among various levels of development. J Biomech. 1999;32(12):1371–1375. [DOI] [PubMed] [Google Scholar]
- 13. Garrison JC, Johnston C, Conway JE. Baseball players with ulnar collateral ligament tears demonstrate decreased rotator cuff strength compared to healthy controls. Int J Sports Phys Ther. 2015;10(4):476–481. [PMC free article] [PubMed] [Google Scholar]
- 14. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 15. Horsley I, Herrington L, Hoyle R, Prescott E, Bellamy N. Do changes in hand grip strength correlate with shoulder rotator cuff function? Shoulder Elbow. 2016;8(2):124–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Karduna AR, McClure PW, Michener LA, Sennett B. Dynamic measurements of three-dimensional scapular kinematics: a validation study. J Biomech Eng. 2001;123(2):184–190. [DOI] [PubMed] [Google Scholar]
- 17. Kibler WB, Uhl TL, Maddux JW, Brooks PV, Zeller B, McMullen J. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elbow Surg. 2002;11(6):550–556. [DOI] [PubMed] [Google Scholar]
- 18. Krajnik S, Fogarty KJ, Yard EE, Comstock RD. Shoulder injuries in US high school baseball and softball athletes, 2005-2008. Pediatrics. 2010;125(3):497–501. [DOI] [PubMed] [Google Scholar]
- 19. Laudner KG, Moline MT, Meister K. The relationship between forward scapular posture and posterior shoulder tightness among baseball players. Am J Sports Med. 2010;38(10):2106–2112. [DOI] [PubMed] [Google Scholar]
- 20. Laudner KG, Myers JB, Pasquale MR, Bradley JP, Lephart SM. Scapular dysfunction in throwers with pathologic internal impingement. J Orthop Sports Phys Ther. 2006;36(7):485–494. [DOI] [PubMed] [Google Scholar]
- 21. Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80(3):276–291. [PubMed] [Google Scholar]
- 22. Magnusson SP, Gleim GW, Nicholas JA. Subject variability of shoulder abduction strength testing. Am J Sports Med. 1990;18(4):349–353. [DOI] [PubMed] [Google Scholar]
- 23. McClure P, Tate AR, Kareha S, Irwin D, Zlupko E. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009;44(2):160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McClure PW, Michener LA, Sennett BJ, Karduna AR. Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg 2001;10(3):269–277. [DOI] [PubMed] [Google Scholar]
- 25. Mikesky AE, Edwards JE, Wigglesworth JK, Kunkel S. Eccentric and concentric strength of the shoulder and arm musculature in collegiate baseball pitchers. Am J Sports Med. 1995;23(5):638–642. [DOI] [PubMed] [Google Scholar]
- 26. Moller M, Attermann J, Myklebust G, et al. The inter- and intrarater reliability and agreement for field-based assessment of scapular control, shoulder range of motion, and shoulder isometric strength in elite adolescent athletes. Phys Ther Sport. 2018;32:212–220. [DOI] [PubMed] [Google Scholar]
- 27. Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 2006;34(3):385–391. [DOI] [PubMed] [Google Scholar]
- 28. Myers JB, Oyama S, Hibberd EE. Scapular dysfunction in high school baseball players sustaining throwing-related upper extremity injury: a prospective study. J Shoulder Elbow Surg. 2013;22(9):1154–1159. [DOI] [PubMed] [Google Scholar]
- 29. Newsham KR, Keith CS, Saunders JE, Goffinett AS. Isokinetic profile of baseball pitchers’ internal/external rotation 180, 300, 450 degrees.s-1. Med Sci Sports Exerc. 1998;30(10):1489–1495. [DOI] [PubMed] [Google Scholar]
- 30. Odom CJ, Taylor AB, Hurd CE, Denegar CR. Measurement of scapular asymmetry and assessment of shoulder dysfunction using the lateral scapular slide test: a reliability and validity study. Phys Ther. 2001;81(2):799–809. [DOI] [PubMed] [Google Scholar]
- 31. Oyama S, Myers JB, Wassinger CA, Daniel Ricci R, Lephart SM. Asymmetric resting scapular posture in healthy overhead athletes. J Athl Train. 2008;43(6):565–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Posner M, Cameron KL, Wolf JM, Belmont PJ, Jr, Owens BD. Epidemiology of Major League Baseball injuries. Am J Sports Med. 2011;39(8):1676–1680. [DOI] [PubMed] [Google Scholar]
- 33. Saper MG, Pierpoint LA, Liu W, Comstock RD, Polousky JD, Andrews JR. Epidemiology of shoulder and elbow injuries among United States high school baseball players: school years 2005-2006 through 2014-2015. Am J Sports Med. 2018;46(1):37–43. [DOI] [PubMed] [Google Scholar]
- 34. Shanley E, Rauh MJ, Michener LA, Ellenbecker TS. Incidence of overall and upper extremity injuries in high school baseball and softball players. Med Sci Sports Exerc. 2010;42(5):471–471. [Google Scholar]
- 35. Stratford PW, Balsor BE. A comparison of make and break tests using a hand-held dynamometer and the Kin-Com. J Orthop Sports Phys Ther. 1994;19(1):28–32. [DOI] [PubMed] [Google Scholar]
- 36. Sullivan SJ, Chesley A, Hebert G, McFaull S, Scullion D. The validity and reliability of hand-held dynamometry in assessing isometric external rotator performance. J Orthop Sports Phys Ther. 1988;10(6):213–217. [DOI] [PubMed] [Google Scholar]
- 37. Tate AR, McClure P, Kareha S, Irwin D, Barbe MF. A clinical method for identifying scapular dyskinesis, part 2: validity. J Athl Train. 2009;44(2):165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Uhl TL, Kibler WB, Gecewich B, Tripp BL. Evaluation of clinical assessment methods for scapular dyskinesis. Arthroscopy. 2009;25(11):1240–1248. [DOI] [PubMed] [Google Scholar]
- 39. Wilk KE, Macrina LC, Fleisig GS, et al. Deficits in glenohumeral passive range of motion increase risk of elbow injury in professional baseball pitchers: a prospective study. Am J Sports Med. 2014;42(9):2075–2081. [DOI] [PubMed] [Google Scholar]
- 40. Woltring H, Huiskes R, De Lange A, Veldpaus F. Finite centroid and helical axis estimation from noisy landmark measurements in the study of human joint kinematics. J Biomech. 1985;18(5):379–389. [DOI] [PubMed] [Google Scholar]
- 41. Wu G, Van der Helm FC, Veeger HD, et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion—part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38(5):981–992. [DOI] [PubMed] [Google Scholar]
- 42. Yong N, Park JH, Lee DY, Yu JH, Kim JS, Hong JH. Shoulder strength ratio between baseball players and general population. J Eng Appl Sci. 2018;13(2, special issue):3092–3096. [Google Scholar]