Abstract
Research on traumatic events often emphasizes the importance of posttraumatic growth (PTG) and resilience, yet few studies have explored their trends and their relationship throughout the progression of traumatic events. This paper explores the longitudinal relationship between resilience and PTG, as well as the role of job burnout in this relationship, among frontline healthcare workers during the COVID‐19 pandemic, who have been exposed to high‐risk work environments over extraordinarily long workdays. In Study 1, 134 Chinese frontline healthcare workers completed a three‐wave survey (Time 1, Time 2, and Time 3) in February–May 2020. In Study 2, 401 frontline healthcare workers completed a cross‐sectional survey. The cross‐lagged analysis suggested that resilience at Time 1 positively predicted PTG at Time 2, which in turn positively predicted resilience at Time 3. PTG at Time 1 also positively predicted resilience at Time 2 (Study 1). However, job burnout was negatively related to both resilience and PTG; in particular, emotional exhaustion moderated the link between PTG and resilience (Study 2). Our findings support a cycle of reinforcement between resilience and PTG over time. The positive effect of PTG on resilience, however, is undermined by emotional exhaustion. Implications for future intervention research and workplace support are discussed.
Keywords: burnout, COVID‐19, healthcare worker, posttraumatic growth, resilience
INTRODUCTION
Declared a pandemic and Public Health Emergency of International Concern, the global outbreak of the novel coronavirus 2019 (COVID‐19) has changed daily life of all walks of life (Du et al., 2020). In addition to its widespread, indefinite influence on daily life, the pandemic has exposed individuals to a complex combination of stressors and blocked their access to protective factors such as social support (Gruber et al., 2020). During this highly stressful time, individuals are faced with a new reality dominated by fear of viral spread and contagion, and essential workers such as frontline medical professionals face significant health risks and stress. As medical professionals experience repeated exposure to stressful and traumatic events, the outbreak of COVID‐19 had a widespread effect on their psychological functioning.
The psychological impact of COVID‐19 among Chinese medical professionals
In China, the pandemic started hitting communities heavily in January 2020. To combat this potentially fatal coronavirus, many healthcare workers across China have been constantly on duty, aware that they put their own health at risk. Medical professionals treating COVID‐19 had to learn and explain to patients continuously updated treatment protocols, take on increased workloads beyond their limits, decide who should receive lifesaving treatment amidst limited resources, and experience the fear of contracting COVID‐19 and spreading it to their families.
In addition, healthcare providers were advised to self‐isolate away from family (Ellis, 2020), thereby limiting their access to social support and further increasing their risk of acute stress reactions (La Greca et al., 2010). Research on prior pandemic also demonstrated that healthcare providers may experience additional stigma and discrimination because of their heightened risk for disease transmission (Williams et al., 2011). Consequently, medical professionals experience constantly heightened psychological and physical stress (Bettinsoli et al., 2020; Walton et al., 2020).
In addition, the rapid increase in the number of cases overwhelmed the medical system and forced frontline healthcare workers to stay on duty nonstop. Compared with healthcare workers who engage in routine medical services, COVID‐19 frontline healthcare workers respond to more medical calls, more frequently witness severe illness and death, experience more intense shifts, and have less time to recharge and recover. As a possible response to work‐related stress, burnout is a notable issue for frontline healthcare workers and may detrimentally impact their psychological functioning.
Therefore, understanding the psychological functioning of medical professionals in the context of this public health crisis is key to the development of psychological interventions to alleviate their distress (Walton et al., 2020; Xiang et al., 2020). While many studies examining the psychological impact of previous pandemics among medical professionals focused on psychiatric conditions (Lancee et al., 2008; Lung et al., 2009), positive functioning such as resilience and posttraumatic growth (PTG) are important processes that receive less research attention (Kalaitzaki et al., 2020). Indeed, the COVID‐19 pandemic has engendered long‐term changes in people's daily lives and increased severity of stress, anxiety, and depression (Bao et al., 2020; Yu et al., 2020). Easily ignored is that even in the face of significant adverse life events, positive adjustment is possible (Chen & Bonanno, 2020).
Theory and hypothesis development
Resilience is often defined as the ability to adapt to, or bounce back from, extremely unfavorable circumstances (Carver, 1998). It may also refer to a system's capacity to “adapt successfully to significant challenges that threaten its function, viability, or development” (Masten, 2018, p. 12). Resilience is an important psychological asset that enables successful coping with stressful and traumatic life events and preserving well‐being in clinical settings (Ogińska‐Bulik & Zadworna‐Cieślak, 2018). Traditional perspectives framed resilience as a stable, trait‐like characteristic. More recently, resilience is recognized as a dynamic process that is influenced by lifelong interactions between internal and environmental resources (Laird et al., 2019). Common factors that contribute to resilience include individuals' internal capacities, such as problem‐solving skills, self‐regulation ability, hope, and a sense of meaning in life. Resilience is also linked to strong connections with external resources and supportive relationships (Masten, 2018).
A concept related to resilience is posttraumatic growth (PTG), which is manifested as improved self‐awareness, relationships, and appreciation of life developed from potentially traumatic events (Ogińska‐Bulik & Zadworna‐Cieślak, 2018; Tedeschi & Calhoun, 1996). As another psychological asset, PTG refers to positive psychological changes resulting from one's struggle with highly challenging life circumstances. Beyond the ability to resist negative impact of adversities, PTG transforms individual functioning to an even higher level than before (Tedeschi & Calhoun, 2004). Existing research shows that the development of PTG is a dynamic process (Tsai & Pietrzak, 2017). Various pathways may lead to PTG. For instance, by sharing their experiences with others, individuals may develop more intimate relationships and new narratives of their lives. By repeated cognitive processing of the traumatic experience, people may reconstruct their schema and goals (Tedeschi & Calhoun, 2004). Interestingly, Maercher and Zoellner (2004) proposed that PTG may have another self‐deceptive side (which is termed the Janus face model), in which people present illusory positivity through maladaptive coping strategies such as avoidance and denial. With this illusory positivity, trauma survivors overcompensate by developing unrealistic optimism about their future.
As two important aspects of positive functioning after trauma, the relationship between PTG and resilience remains under debate. Early research suggested that individuals with more resilience may not experience PTG, since the stressful or traumatic events may have little impact on resilient individuals (Tedeschi & Calhoun, 1996). However, recent studies on the association between resilience and PTG have yielded mixed results. Findings suggest that their relationship may be positive (Jeon et al., 2017), curvilinear (Kaye‐Tzadok & Davidson‐Arad, 2016), or nonsignificant (Ogińska‐Bulik & Zadworna‐Cieślak, 2018). The reason for these mixed findings may be the cross‐sectional design that was widely adopted in previous studies, whereas the relationship between resilience and PTG is possibly dynamic and changes over time. Even though PTG is unrelated to resilience at certain points in time, it may still facilitate the development of resilience over time.
In addition to resilience and PTG, burnout is an important consideration when studying medical professionals' psychological functioning. Burnout is often described as a three‐dimensional syndrome that is characterized by emotional exhaustion, depersonalization, and lack of personal accomplishment (Cohen‐Katz et al., 2005). Burnout is closely associated with physical and emotional symptoms, poor interpersonal relationships, and high turnover (Hetzel‐Riggin et al., 2020). Although burnout is likely a chronic state that one may experience after a relatively long period of work, the experience of vigor, dedication, and absorption during work is also possible (Leiter & Maslach, 2017; Sonnentag, 2017). In the context of COVID‐19, medical professionals may experience burnout a few months after repeated exposure to high‐intensity and emotionally provocative work. In particular, as they are repeatedly exposed to potentially traumatic events such as witnessing severe illness and death, emotional exhaustion is highly likely. Even so, they may still find meaning in their work and experience posttraumatic growth. Whereas posttraumatic growth may facilitate the development of resilience, burnout may hinder the maintenance of resilience.
Research gaps
While existing studies of resilience and PTG mostly adopt a cross‐sectional design, longitudinal studies will more accurately capture the dynamic changes in their relationship over time. Existing longitudinal studies provided some initial evidence of the dynamic link between resilience and PTG. Resilience was found to directly (Bensimon, 2012; Yu et al., 2013) or indirectly (Ogińska‐Bulik & Zadworna‐Cieślak, 2018) promote the development of positive growth among individuals who experienced stressful or potentially traumatic events. Yet to our knowledge, no study thus far has explored the reverse direction of this relationship: PTG may also benefit the maintenance and improvement of resilience over time.
In addition, considering the context in which people achieve PTG is necessary. For frontline healthcare workers amidst COVID‐19, burnout is an important factor that may compromise their PTG. Although recent research showed that lower levels of burnout were associated with higher PTG and resilience (Taku, 2014), no study to date has examined the role of burnout in the relationship between PTG and resilience.
The COVID‐19 pandemic provides a unique context and opportunity to examine the presentation, development, and evolvement of PTG and resilience over time. As medical professionals continue to function at an intense level during this public health crisis, resilience serves as an important psychological process during the pandemic and in its aftermath (Chen & Bonanno, 2020). As resilience and PTG facilitate health and well‐being under stress (Kalaitzaki et al., 2020), understanding how resilience and PTG change over the course of a pandemic will yield critical insights into the process of psychological adjustment among medical professionals, which will lead to interventions that benefit this high‐risk population in both the current and future public health crises.
The current investigation
In this research, we examine the bidirectional relationship between PTG and resilience over time and, in addition, examine the moderating effect of job burnout in this relationship a few months into the outbreak of COVID‐19. Two studies were conducted. In the first study, we measured PTG and resilience among frontline healthcare workers over three timepoints in 2020. Using a longitudinal design, we examine whether PTG and resilience mutually reinforce each other over time. Our hypothesis is that greater PTG leads to greater resilience, which in turn leads to greater PTG.
In the second study, we asked frontline healthcare workers about their burnout after a few months into the outbreak of COVID‐19 when burnout is most likely to occur. Using a cross‐sectional design with a larger sample, we examined the moderating role of burnout in relation to PTG and resilience. Our hypothesis is that the extent to which medical staff resilience and PTG benefit each other depends on individual level of burnout. The combination of studies 1 and 2 aims to better understand the relationship among PTG, burnout, and resilience, while generating insights into how to maintain resilience among frontline healthcare workers in highly demanding work environments.
STUDY 1
Methods
Participants and procedure
Participants were recruited from the only COVID‐19‐designated hospital in Shenzhen, China. The corresponding author obtained permission from the president of the hospital. Frontline healthcare workers were recruited with the help of hospital authorities. To be eligible for participation, the majority of participants' work had to be related to COVID‐19.
Participants completed three waves of survey in spring 2020, shortly after the epidemic started in China. The first assessment took place on February 17–19, 2020 (Time 1). This period could be considered the peak of the pandemic in China, when healthcare workers were facing tremendous workloads and pressure. A month later (March 17–19; Time 2), we conducted the second survey. At this stage, although COVID‐19 was relatively under control in China, the outbreak worldwide and increasing cases in cross‐border populations made disease control increasingly difficult. Thus, tensions among healthcare workers continued to be high. Two months later (May 23 to 25; Time 3), a third survey was conducted. At this stage, the pandemic had basically been brought under effective control in China; Chinese healthcare workers' main duties had gradually returned to the pre‐pandemic norm and no longer focused on treating COVID‐19 patients. This may be a time for Chinese frontline healthcare workers to recover from this collectively traumatic period.
All data were collected through self‐reported questionnaires using the hospital online office system. To avoid null values, all items were set as required. All participants provided informed consent. During the Time 1 assessment, 492 frontline healthcare workers completed the survey, among whom 251 completed the survey at Time 1 and Time 2, and 205 completed Time 1 and Time 3. Participants' identification numbers were used to match them across the three time stamps, and the final sample size that completed all three surveys was 134.
The mean age of participants was 35.41 ± 8.09 years, and the sample included 40 doctors, 44 nurses, 13 medical technicians, 5 medical researchers, and 32 administrators. Furthermore, 95 participants were female. Of the participants, 21 had a junior college or below degree, 75 had a college degree, and 38 had a master's or above degree.
Measures
Posttraumatic growth
A modified version of the Posttraumatic Growth Inventory (PTGI; Wang et al., 2011) was administered to measure frontline healthcare workers' posttraumatic growth. The original PTGI was developed by Tedeschi and Calhoun (1996) to assess positive changes after traumatic events. The modified version contains 20 items, with one item deleted from the original scale. The scale exhibited good internal consistency in our study (Cronbach's alpha was .82 at Time 1, .92 at Time 2, and .80 at Time 3) and good fit indices in our confirmative factor analysis (χ 2/df = 1.55, CFI = 0.99, TLI = 0.98, SRMR = 0.021, RMSEA = 0.064 at Time 1; χ 2/df = 2.47, CFI = 0.98, TLI = 0.95, SRMR = 0.037, RMSEA = 0.105 at Time 2; χ 2/df = 2.32, CFI = 0.99, TLI = 0.97, SRMR = 0.017, RMSEA = 0.099 at Time 3). Participants rated their agreement with each item using a scale ranging from 1 (totally disagree) to 5 (totally agree). We used the average score of all items, with higher scores indicating higher posttraumatic growth.
Resilience
The Chinese version (Yu & Zhang, 2007) of the Ego‐Resilience Scale (ERS) was used to measure resilience. The ERS was developed by Block and Kreman (1996) and included 14 items, and the Chinese version exhibited good internal consistency in our study (Cronbach's alpha was .79 at Time 1, .78 at Time 2, and .85 at Time 3) and good fit indices in our confirmative factor analysis (χ 2/df = 2.32, CFI = 0.95, TLI = 0.96, SRMR = 0.052, RMSEA = 0.073 at Time 1; χ 2/df = 2.13, CFI = 0.93, TLI = 0.97, SRMR = 0.046, RMSEA = 0.068 at Time 2; χ 2/df = 2.54, CFI = 0.98, TLI = 0.97, SRMR = 0.055, RMSEA = 0.071 at Time 3). Respondents specified their agreement with each item using a scale ranging from 1 (totally disagree) to 5 (totally agree). We used the average score of all items, with higher scores indicating higher resilience.
Statistical analysis
SPSS version 22.0 and Mplus version 7.0 were used for data analysis. First, an independent‐samples t test and a chi‐square test were used to test for attrition effects. A repeated‐measures ANOVA was then conducted to test the differences in resilience and PTG at different timepoints. Third, descriptive statistical analysis and Pearson's correlation analysis were performed for the key variables using SPSS. Finally, cross‐lagged analysis was conducted using Mplus, with maximum‐likelihood robust (MLR) estimation.
Results
Attrition analysis
To test for attrition effects, we compared participants who completed all three waves of data with those who dropped out after Time 1 and Time 2. Attrition analysis results indicated that there were no significant differences in age [t(490) = −1.52, p > .05], gender [χ 2(1) = 0.03, p > .05], education level [χ 2(3) = 4.14, p > .05], marital status [χ 2(2) = 5.68, p > .05], resilience [t(490) = −1.08, p > .05], and PTG [t(490) = −1.34, p > .05].
Descriptive statistics
Table 1 shows the means, standard deviations of the main variables, and their correlations. On average, participants showed an increase in PTG from Time 1 (M = 3.43 on a scale of 1–5, SD = 0.66) to Time 2 (M = 3.92, SD = 0.70), and a decrease in Time 3 (M = 2.90, SD = 0.64). Meanwhile, their resilience slightly decreased from Time 1 (M = 3.65 on a scale of 1–5, SD = 0.80) to Time 2 (M = 3.54, SD = 0.67) and Time 3 (M = 3.44, SD = 0.76). The PTG scores at Time 1, Time 2, and Time 3 showed positive correlations with each other, as did resilience scores at Time 1, Time 2, and Time 3. Additionally, PTG at Time 1 and Time 2 showed positive correlations with resilience across three timepoints, and PTG at Time 3 was positively correlated with resilience at Time 2.
TABLE 1.
Means, standard deviations, and correlations of variables in Study 1
| Variables | M ± SD | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|---|
| 1. PTG at Time 1 | 3.43 ± 0.66 | 1 | |||||
| 2. PTG at Time 2 | 3.92 ± 0.70 | .49* | 1 | ||||
| 3. PTG at Time 3 | 2.90 ± 0.64 | .47* | .24* | 1 | |||
| 4. Resilience at Time 1 | 3.65 ± 0.80 | .44* | .49* | .06 | 1 | ||
| 5. Resilience at Time 2 | 3.54 ± 0.67 | .36* | .58* | .18* | .39* | 1 | |
| 6. Resilience at Time 3 | 3.44 ± 0.76 | .21* | .41* | .07 | .53* | .35* | 1 |
p < .05, **p < .01.
Mean differences among variables over time
The repeated‐measures ANOVA revealed that there were significant differences in resilience at Time 1, Time 2, and Time 3 [W = 0.99, χ 2(2) = 1.60, p = .45; F(2) = 4.26, p < .05], and in PTG at Time 1, Time 2, and Time 3 [W = 0.92, χ 2(2) = 10.90, p < .01; F(2) = 131.56, p < .01]. The results of the LSD multiple comparison showed that there were significant differences between resilience at Time 1 and resilience at Time 3, PTG at Time 1 and PTG at Time 2, and PTG at Time 2 and PTG at Time 3. There was no significant difference in resilience between Time 1 and Time 2, or between Time 2 and Time 3.
Cross‐lagged analysis
Considering that demographic variables may have an impact on the study variables, we used SPSS to analyze the correlation between demographic variables and the study variables before carrying out cross‐lagged analysis. The results showed that the correlations between occupation and resilience at Time 1 and Time 3 were significant and the correlations between education level and resilience at Time 1 and Time 3 were also significant. The correlations between the remaining variables were not significant.
A structural equation model was used to explore the relationship between resilience and PTG. With each item of the Chinese version of the ERS as the observed variable of resilience, the latent variable of resilience was established. With each item of PTGI as the observed variable of PTG, the latent variable of PTG was established. We then constructed the cross‐lagged model of resilience and PTG (Figure 1). As occupation and education levels were correlated with resilience, we added occupation and education level into the cross‐lagged model as control variables.
FIGURE 1.
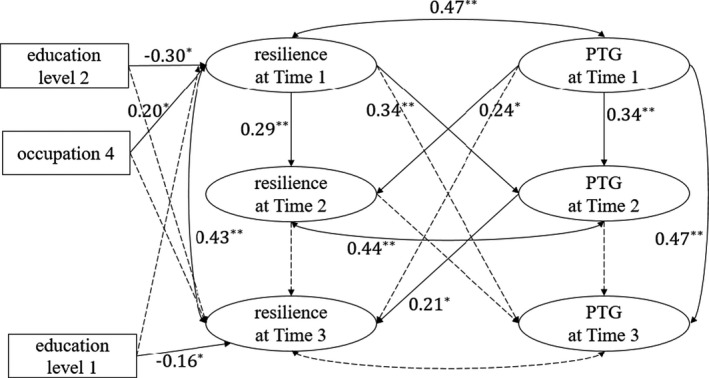
Cross‐lagged model testing the relationship between resilience and PTG. Note. Path coefficients are standardised. Education level 1, education level 2, and occupation 1 were dummy variables. Among the three educational levels, using “junior college or below” as the benchmark, two dummy variables were generated: “education level 1” (college) and “education level 2” (“master's degree or above”). Among the five occupation categories, using “doctor” as the benchmark, four dummy variables were generated: “occupation 1” (nurse), “occupation 2” (medical technician), “occupation 3” (medical researcher), and “occupation 4” (administrator). * p < .05, **p < .01
The result showed acceptable model fit: χ 2/df = 1.09; RMSEA = 0.026; CFI = 0.990; TLI = 0.983; SRMR = 0.042. There was a significant, positive association between resilience and PTG at Time 1 and Time 2, but not at Time 3. Specifically, resilience at Time 1 positively predicted PTG at Time 2, which in turn positively predicted resilience at Time 3. Additionally, PTG at Time 1 positively predicted resilience at Time 2. The R 2‐values for resilience at Time 2, PTG at Time 2, resilience at Time 3, and PTG at Time 3 were .20, .33, .37, and .22, respectively. This indicates that the predictors explained 20 per cent, 33 per cent, 37 per cent, and 22 per cent of the variance in resilience at Time 2, PTG at Time 2, resilience at Time 3, and PTG at Time 3, respectively.
Study 1 summary
The repeated‐measures ANOVA showed that PTG scores across timepoints were as follows: score at Time 2 > score at Time 1 > score at Time 3. Resilience at Time 3 was significantly lower than resilience at Time 1. Moreover, the cross‐lagged analysis indicated that resilience at Time 1 was beneficial to the development of PTG at Time 2, which then benefited resilience at Time 3. The results also revealed that resilience was significantly related to PTG at Time 1 and Time 2. However, no significant association was found between resilience and PTG at Time 3.
STUDY 2
Methods
Participants and procedure
The Study 2 participants were also from the only COVID‐19 hospital in Shenzhen. Aiming to recruit a larger sample, a cross‐sectional survey was conducted between May 23 and 25, 2020, and 401 completed responses were collected. The mean age of participants was 35.45 ± 8.78 years, and 290 participants were female. The sample included 114 doctors, 172 nurses, 44 medical technicians, 14 medical researchers, and 57 administrators. Furthermore, of the participants, 78 had a junior college or below degree, 218 had a college degree, and 105 had a master's or above degree.
Measures
The scales used to measure posttraumatic growth and resilience were the same as those used in Study 1. In Study 2, their Cronbach's alphas were .85 and .81, respectively.
Job Burnout
The Chinese Maslach Burnout Inventory (CMBI; Li & Wu, 2005) was used to measure frontline healthcare workers' burnout. It was revised according to the Maslach Burnout Inventory—General Survey (MBI‐GS; Schaufeli et al., 1996). The CMBI included three dimensions: emotional exhaustion (7 items), depersonalization (7 items), and personal accomplishment (7 items). Participants' ratings used a 5‐point Likert response format (1 = “never”; 5 = “always”). We used the average score of all items (the dimension of personal accomplishment was reverse‐coded), and higher scores indicated higher job burnout. Cronbach's alphas of the whole scale and the three dimensions in our study were .73, .83, .84, and .71, respectively.
Statistical analysis
All statistical analyses were performed using SPSS version 22.0. First, we conducted a common method deviation test. Descriptive analyses and Pearson's correlation analyses were then performed for key variables. Following Hayes's (2013) guideline, the SPSS PROCESS macro was used to test whether job burnout moderated the relationship between PTG and resilience. In the SPSS PROCESS, the interaction effect is automatically calculated by the software, which also produces the proportion of the variance explained by the moderating effect of emotional exhaustion (indicated by the R‐squared increase due to interaction).
Results
Common method analysis
The Harman single‐factor test was used to identify common method deviation. The results showed that three factors with characteristic roots greater than 1 were extracted. The variation rate of the first factor was less than 40 per cent (at 36.93%), indicating that the common method deviation in this study was not significant.
Descriptive and correlation analyses
Table 2 shows the means of burnout, PTG, and resilience, and correlations among these key measures. On a scale of 1–5, participant scored 2.94 on PTG on average (SD = 0.74), 3.48 on resilience (SD = 0.81), and 2.56 on burnout (SD = 0.66). With respect to the specific dimensions of burnout, emotional exhaustion scored the highest (M = 2.89, SD = 0.96), followed by personal accomplishment (reverse‐coded, M = 2.47, SD = 0.83) and depersonalization (M = 2.33, SD = 0.98). As hypothesised, burnout was negatively associated with both PTG and resilience.
TABLE 2.
Means, standard deviations, and correlations of variables in Study 2
| Variable | Mean ± SD | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|---|
| 1. PTG | 2.94 ± 0.74 | 1 | |||||
| 2. Resilience | 3.48 ± 0.81 | .31* | 1 | ||||
| 3. Burnout | 2.56 ± 0.66 | −.11* | −.32* | 1 | |||
| 4. Emotional exhaustion | 2.89 ± 0.96 | .08 | −.20* | .81* | 1 | ||
| 5. Depersonalization | 2.33 ± 0.98 | .06 | −.24* | .85* | .67* | 1 | |
| 6. Personal accomplishment | 2.47 ± 0.83 | −.42* | −.25* | .46* | .02 | .09 | 1 |
p < .05, **p < .01.
Moderation effect of job burnout
The SPSS PROCESS macro (model 1) was used to test the moderating role of job burnout. The results showed that overall job burnout had no significant moderating effect on the relationship between PTG and resilience. Among the three dimensions of job burnout, depersonalization and personal accomplishment showed no significant moderating effect; however, emotional exhaustion played a moderating role (Table 3).
TABLE 3.
Moderation effect of emotional exhaustion
| Predictor | Responding variable | |||
|---|---|---|---|---|
| Resilience | ||||
| Coeff. | SE | p | 95%CI | |
| PTG | 0.04 | .14 | .746 | −0.22, 0.31 |
| Emotional exhaustion (EE) | −0.53 | .14 | <.001 | −0.81, −0.25 |
| PTG * EE | 0.11 | .04 | .013 | 0.02, 0.20 |
| Constant | 3.96 | .43 | <.001 | 3.11, 4.81 |
| R 2 = .162, F (3,397) = 25.63, p < .001 | ||||
| ΔR 2 = .013, F (1,397) = 15.42, p = .013 | ||||
A follow‐up analysis was performed to probe the conditional effects of PTG on resilience at two levels of emotional exhaustion (i.e. 1 SD below the average, representing low exhaustion, and 1 SD above the average, representing high exhaustion). Results showed a stronger relationship between PTG and resilience (B = .47, p < .001, 95% CI [0.34, 0.60]) among participants with high exhaustion, compared with those with low exhaustion (B = 0.26, p < .001, 95% CI [0.12, 0.39]), which indicates that the association between PTG and resilience was more prominent among those with high emotional exhaustion. This moderation is illustrated in Figure 2.
FIGURE 2.
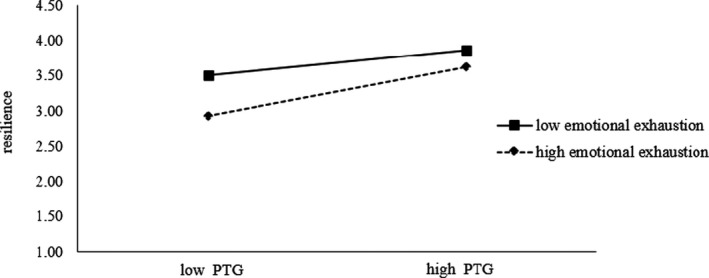
Resilience by PTG at different levels of emotional exhaustion
Study 2 summary
The results of Study 2 demonstrated that job burnout was negatively related to resilience and PTG. Furthermore, the results of the moderation model showed that the emotional exhaustion factor of job burnout moderated the link between PTG and resilience. PTG had a stronger association with resilience among healthcare workers with higher levels of emotional exhaustion.
GENERAL DISCUSSION
The results of Study 1 revealed that resilience had a positive association with PTG, both at Time 1 and at Time 2. However, resilience was not significantly related to PTG at Time 3. Notably, unlike previous studies, resilience and PTG did not increase over time throughout our study. In general, the higher the resilience, the more likely the PTG will be developed. Since resilience could alleviate the negative effects brought by traumatic events (Bonanno et al., 2004), when individuals face lower stress (such as at Time 3 when COVID‐19 was relatively under control in China), resilience may serve merely as a buffer, protecting individuals from adverse events and exerting minimal effect on PTG, whereas under high stress (such as at Time 1 and Time 2), resilience may contribute significantly to PTG.
The repeated‐measures ANOVA showed that PTG scores rose first and then fell. According to the Janus face model (Maercher & Zoellner, 2004), PTG has both constructive and illusory aspects. In related research on positive illusions, Taylor and his colleagues found that when confronted with threatening events, people often had a slight distortion of their positive perceptions (self‐aggrandizement), an exaggerated sense of personal control, and unrealistic optimism (Taylor, 1983; Taylor & Armor, 1996; Taylor et al., 2000). Therefore, we speculate that the increased PTG at Time 2 may be an indicator of increased participant optimism. As it became clear that the pandemic situation was not under control, however, frontline healthcare workers' optimism faded, hence the decline in PTG at Time 3.
Although compared with baseline (Time 1), participants' resilience declined significantly at Time 3, their resilience at Time 2 was not significantly different from Time 1 or Time 3. This seems to indicate that resilience did not change substantially over time, which may be related to the timepoints when the study was conducted. The three waves of data collection were undertaken within 6 months, shortly after the COVID‐19 outbreak in China. This short period may not be enough time for resilience to change.
Consistent with previous research findings that resilience can lead to PTG after traumatic events, our cross‐lagged analysis indicated that people with higher levels of resilience at Time 1 developed greater PTG at Time 2. During traumatic experiences, resilience may help people understand the value of life, find new meaning, determine their life priorities, and achieve spiritual well‐being (Üzar‐Özçetin & Hiçdurmaz, 2019).
Resilience leading to PTG is not the only story here. Our findings also capture a dynamic interaction between resilience and PTG among COVID‐19 frontline healthcare workers. Over time, people who developed higher PTG at Time 1 showed greater resilience at Time 2, and PTG at Time 2 continued to lead to enhanced resilience at Time 3. Thus, our hypothesis that resilience and PTG promote each other over time is well supported. Some researchers (Hobfoll et al., 2007) proposed that PTG is an active adaptation that helps individuals grow and build a more resilient self by preventing individuals from sinking into apathy following trauma. Tedeschi and Calhoun (1996) also considered PTG involving several stages, including initial growth, coping success, and further growth.
Based on our findings, the process through which individuals continue to grow after trauma is a virtuous cycle. While previous research suggests that resilience facilitates PTG, our study suggests that PTG in turn also promotes resilience. These two factors positively influence each other over time, prompting individuals to continuously achieve positive functioning during and after adverse experiences. Our speculation is that when people experience PTG, they will gain more internal capacities that boost their resilience, such as enhanced self‐efficacy and cognitive flexibility. With enhanced self‐efficacy, people may develop an increased sense of control, which strengthens their confidence when coping with adversity. With enhanced cognitive flexibility, people may see adverse experiences from new perspectives, with more cognitive space to learn from such experiences and develop active coping skills. These potential mechanisms between PTG and resilience warrant further investigation. Future trauma‐focused interventions may also focus on promoting these internal capacities to help clients achieve sustainable PTG and resilience over time.
Furthermore, our second study suggests that in addition to stress coping, burnout reduction is an important method to enhance resilience (Sotile et al., 2019). In their efforts to prevent the infection of family members and others, frontline healthcare workers suffered from boredom, exhaustion, and loneliness, along with the pressure of administering intensive medical treatment (Walton et al., 2020), which has made medical staff burnout a common phenomenon in this pandemic (Restauri & Sheridan, 2020). Our findings suggest that burnout is negatively related to resilience and PTG. In particular, emotional exhaustion (a key component of burnout) moderates the link between PTG and resilience. Under high levels of emotional exhaustion, PTG plays a stronger protective role in maintaining resilience. Under low levels of emotional exhaustion, the association between PTG and resilience is less pronounced but still significant. These findings suggest that the positive association between PTG and resilience is more evident under situations in which individuals experience a higher emotional burnout. This provides an informative addition to existing literature that the relationship between PTG and resilience may be more nuanced as they are suspectable to other environmental and psychological contexts. Capturing the context in which PTG and resilience are measured is critical to better illustrate their association.
From the perspective of preventive intervention, these findings suggest that resilience promotion programs that target posttraumatic growth are more likely to benefit those that are experiencing more severe emotional burnout. With adequate support in building resilience, such as developing effective coping strategies and fostering new perspectives on adverse experiences, those who face higher work‐related emotional distress may benefit more from such support and achieve further growth over time. In addition, measuring burnout carries the potential to identify medical professionals who are suitable for resilience promotion programs, which will in turn improve their psychological functioning in the aftermath of public health crises.
This study has several limitations. First, the self‐reported surveys may have bias (e.g. social desirability bias), even though we encouraged participants to answer survey questions truthfully. Although self‐reported measures seem to be the best approach to capture individuals' internal states such as personal growth, future studies may supplement such measures with other assessment methods, including peer report and stress biomarkers. Also, although our first study adopted a longitudinal design and controlled for demographic variables in the analyses, there can be other confounders affecting participants' resilience and PTG, such as other life events during the survey period and the ever‐changing COVID‐19 situation. While our survey was limited by its brevity, future studies may consider controlling for more factors if participants' time allows. Future studies may also use a mixed‐methods design to explore how individual resilience and PTG reinforce each other, and how burnout affects resilience, through in‐depth interviews. However, given that such studies require more of their participants' time, it may not be appropriate to use these methods until after the pandemic.
Second, all three waves of data collection were carried out within 6 months of the COVID‐19 outbreak in China. Given that resilience and PTG of frontline healthcare workers may further evolve over time, it is necessary to conduct a continuous follow‐up investigation among the frontline healthcare workers in the future. We also had a relatively low response rate after three timepoints, and those who withdrew from the study may be those with higher distress. Although our attrition analysis did not show a significant difference, this decreasing response rate is noteworthy. Despite these limitations, this study provides valuable information for gauging the positive psychological functioning of frontline healthcare workers. By focusing on resilience and posttraumatic growth, our findings offer important practice implications for maintaining, and potentially enhancing, medical staff well‐being during and after the pandemic.
CONFLICT OF INTEREST
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ETHICS STATEMENTS
This study was approved through the Institutional Review Board of the Department of Psychology (Ref: 202004), Tsinghua University, and research meets the ethical guidelines, including adherence to the legal requirements of the study country.
Lyu Y, Yu Y, Chen S, Lu S, Ni S. Positive functioning at work during COVID‐19: Posttraumatic growth, resilience, and emotional exhaustion in Chinese frontline healthcare workers. Appl Psychol Health Well‐Being. 2021;13:871–886. 10.1111/aphw.12276
Yizhi Lyu and Yongju Yu contributed equally to this work.
Funding information
This study was funded by the Tsinghua SIGS Overseas Research Cooperation Foundation (Grant No. HW2020004), the National Philosophy and Social Sciences Foundation of China (Grant No. 20AZD085), the Guangdong Natural Science Foundation (Grant No. 2020A1515010949), and the Interdisciplinary Research Project of Graduate School of Shenzhen of Tsinghua University (JC2017005)
Contributor Information
Shuang Lu, Email: shuanglu@hku.hk.
Shiguang Ni, Email: ni.shiguang@sz.tsinghua.edu.cn.
DATA AVAILABILITY STATEMENT
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
REFERENCES
- Bao, Y. , Sun, Y. , Meng, S. , Shi, J. , & Lu, L. (2020). 2019‐nCoV epidemic: Address mental health care to empower society. Lancet, 395(10224), 37–38. 10.1016/S0140-6736(20)30309-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bensimon, M. (2012). Elaboration on the association between trauma, PTSD and posttraumatic growth: The role of trait resilience. Personality and Individual Differences, 52(7), 782–787. 10.1016/j.paid.2012.01.011 [DOI] [Google Scholar]
- Bettinsoli, M. L. , Di Riso, D. , Napier, J. L. , Moretti, L. , Bettinsoli, P. , Delmedico, M. , Piazzolla, A. , & Moretti, B. (2020). Mental health conditions of Italian healthcare professionals during the COVID‐19 disease outbreak. Applied Psychology Health and Well‐Being, 12(4), 1054–1073. 10.1111/aphw.12239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block, J. , & Kreman, A. M. (1996). IQ and Ego‐resiliency: Conceptual and empirical connections and separateness. Journal of Personality and Social Psychology, 70(2), 349–361. [DOI] [PubMed] [Google Scholar]
- Bonanno, G. A. , Wortman, C. B. & Nesse, R. M. (2004). Prospective patterns of resilience and maladjustment during widowhood. Psychology and Aging, 19(2), 260–271. [DOI] [PubMed] [Google Scholar]
- Carver, C. S. (1998). Resilience and thriving: Issues, models, and linkages. Journal of Social Issues, 54(2), 245–266. [Google Scholar]
- Chen, S. , & Bonanno, G. A. (2020). Psychological adjustment during the global outbreak of COVID‐19: A resilience perspective. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S51–S54. 10.1037/tra0000685 [DOI] [PubMed] [Google Scholar]
- Cohen‐Katz, J. , Wiley, S. D. , Capuano, T. , Baker, D. M. , & Shapiro, S. (2005). The effects of mindfulness‐based stress reduction on nurse stress and burnout, part II: A quantitative and qualitative study. Holistic Nursing Practice, 19(1), 26–35. 10.1097/00004650-200501000-00008 [DOI] [PubMed] [Google Scholar]
- Du, H. , Yang, J. , King, R. B. , Yang, L. , & Chi, P. (2020). COVID‐19 increases online searches for emotional and health‐related terms. Applied Psychology: Health and Well‐Being, 12(4), 1039–1053. 10.1111/aphw.12237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis, E. G. (2020). How health care workers avoid bringing COVID‐19 home. https://www.wired.com/story/coronavirus‐covid‐19‐health‐care‐workers‐families/ [Google Scholar]
- Gruber, J. , Prinstein, M. J. , Clark, L. A. , Rottenberg, J. , Abramowitz, J. S. , Albano, A. M. , & Weinstock, L. M. (2020). Mental health and clinical psychological science in the time of COVID‐19: Challenges, opportunities, and a call to action. American Psychologist. Advance online publication. 10.1037/amp0000707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression‐based approach. The Guilford Press. [Google Scholar]
- Hetzel‐Riggin, M. D. , Swords, B. A. , Tuang, H. L. , Deck, J. M. , & Spurgeon, N. S. (2020). Work engagement and resiliency impact the relationship between nursing stress and burnout. Psychological Reports, 123, 1835–1853. 10.1177/0033294119876076 [DOI] [PubMed] [Google Scholar]
- Hobfoll, S. E. , Hall, B. J. , Canetti‐Nisim, D. , Galea, S. , Johnson, R. J. , & Palmieri, P. A. (2007). Refining our understanding of traumatic growth in the face of terrorism: Moving from meaning cognitions to doing what is meaningful. Applied Psychology, 56(3), 345–366. [Google Scholar]
- Jeon, G. , Park, S. , & Bernstein, K. S. (2017). Socio‐demographic and psychological correlates of posttraumatic growth among Korean Americans with a history of traumatic life experiences. Archives of Psychiatric Nursing, 31(3), 256–262. 10.1016/j.apnu.2016.12.002 [DOI] [PubMed] [Google Scholar]
- Kalaitzaki, A. E. , Tamiolaki, A. , & Rovithis, M. (2020). The healthcare professionals amidst COVID‐19 pandemic: A perspective of resilience and posttraumatic growth. Asian Journal of Psychiatry, 52, 102172. 10.1016/j.ajp.2020.102172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaye‐Tzadok, A. , & Davidson‐Arad, B. (2016). Posttraumatic growth among women survivors of childhood sexual abuse: Its relation to cognitive strategies, posttraumatic symptoms, and resilience. Psychological Trauma: Theory, Research, Practice, and Policy, 8(5), 550–558. 10.1037/tra0000103 [DOI] [PubMed] [Google Scholar]
- La Greca, A. M. , Silverman, W. K. , Lai, B. , & Jaccard, J. (2010). Hurricane‐related exposure experiences and stressors, other life events, and social support: Concurrent and prospective impact on children's persistent posttraumatic stress symptoms. Journal of Consulting and Clinical Psychology, 78, 794–805. 10.1037/a0020775 [DOI] [PubMed] [Google Scholar]
- Laird, K. T. , Krause, B. , Funes, C. , & Lavretsky, H. (2019). Psychobiological factors of resilience and depression in late life. Translational Psychiatry, 9(1), 88. 10.1038/s41398-019-0424-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancee, W. J. , Maunder, R. G. , Goldbloom, D. S. , & the Coauthors for the Impact of SARS Study (2008). Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatric Services, 59, 91–95. 10.1176/ps.2008.59.1.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leiter, M. P. , & Maslach, C. (2017). Burnout and engagement: Contributions to a new vision. Burnout Research, 5, 55–57. 10.1016/j.burn.2017.04.003 [DOI] [Google Scholar]
- Li, Y. , & Wu, M. H. (2005). Developing the Job Burnout Inventory. Psychological Science, 28(2), 454–457 (in Chinese). [Google Scholar]
- Lung, F. W. , Lu, Y. C. , Chang, Y. Y. , & Shu, B. C. (2009). Mental symptoms in different health professionals during the SARS attack: A follow‐up study. Psychiatric Quarterly, 80, 107–116. 10.1007/s11126-009-9095-5 [DOI] [PubMed] [Google Scholar]
- Maercher, A. , & Zoellner, T. (2004). The Janus face of self‐perceived growth: Toward a two‐component model of posttraumatic growth. Psychological Inquiry, 15(1), 41–48. 10.2307/20447200 [DOI] [Google Scholar]
- Masten, A. S. (2018). Resilience theory and research on children and families: Past, present, and promise. Journal of Family Theory & Review, 10, 12–31. 10.1111/jftr.12255 [DOI] [Google Scholar]
- Ogińska‐Bulik, N. , & Zadworna‐Cieślak, M. (2018). The role of resiliency and coping strategies in occurrence of positive changes in medical rescue workers. International Emergency Nursing, 39, 40–45. 10.1016/j.ienj.2018.02.004 [DOI] [PubMed] [Google Scholar]
- Restauri, N. , & Sheridan, A. D. (2020). Burnout and posttraumatic stress disorder in the coronavirus disease 2019 (COVID‐19) pandemic: Intersection, impact, and interventions. Journal of the American College of Radiology, 17, 921–926. 10.1016/j.jacr.2020.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaufeli, W. B. , Leiter, M. P. , & Maslach, C. (1996). Maslach Burnout Inventory General Survey (MBI‐GS). In Maslach C. et al (Eds.), Maslach Burnout Inventory manual (3rd ed.). Consulting Psychologists Press. [Google Scholar]
- Sonnentag, S. (2017). A task‐level perspective on work engagement: A new approach that helps to differentiate the concepts of engagement and burnout. Burnout Research, 5, 12–20. 10.1016/j.burn.2017.04.001 [DOI] [Google Scholar]
- Sotile, W. M. , Fallon, R. S. , & Simonds, G. R. (2019). Moving from physician burnout to resilience. Clinical Obstetrics and Gynecology, 62(3), 480–490. 10.1097/GRF.0000000000000444 [DOI] [PubMed] [Google Scholar]
- Taku, K. (2014). Relationships among perceived psychological growth, resilience and burnout in physicians. Personality and Individual Differences, 59, 120–123. 10.1016/j.paid.2013.11.003 [DOI] [Google Scholar]
- Taylor, S. E. (1983). Adjustment to threatening events: A theory of cognitive adaptation. American Psychologist, 38, 1161–1173. [Google Scholar]
- Taylor, S. E. , & Armor, D. A. (1996). Positive illusions and coping with adversity. Journal of Personality, 64, 873–898. [DOI] [PubMed] [Google Scholar]
- Taylor, S. E. , Kemeny, M. E. , Reed, G. M. , Bower, J. E. , & Gruenewald, T. L. (2000). Psychological resources, positive illusions, and health. American Psychologist, 55, 99–109. [DOI] [PubMed] [Google Scholar]
- Tedeschi, R. G. , & Calhoun, L. G. (1996). The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. 10.1007/BF02103658 [DOI] [PubMed] [Google Scholar]
- Tedeschi, R. G. , & Calhoun, L. G. (2004). Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry, 15(1), 1–18. [Google Scholar]
- Tsai, J. , & Pietrzak, R. H. (2017). Trajectories of posttraumatic growth among US military veterans: A 4‐year nationally representative, prospective cohort study. Acta Psychiatrica Scandinavica, 136(5), 483–492. 10.1111/acps.12800 [DOI] [PubMed] [Google Scholar]
- Üzar‐Özçetin, Y. S. , & Hiçdurmaz, D. (2019). Effects of an empowerment program on resilience and posttraumatic growth levels of cancer survivors. Cancer Nursing, 42(6), E1–E13. 10.1097/NCC.0000000000000644 [DOI] [PubMed] [Google Scholar]
- Walton, M. , Murray, E. , & Christian, M. D. (2020). Mental health care for medical staff and affiliated healthcare workers during the COVID‐19 pandemic. European Heart Journal: Acute Cardiovascular Care, 9(3), 241–247. 10.1177/2048872620922795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, J. , Chen, Y. , & Wang, Y. B. (2011). Revision of the Posttraumatic Growth Inventory and testing its reliability and validity. Journal of Nursing Science, 26(14), 26–28 (in Chinese). [Google Scholar]
- Williams, J. , Gonzalez‐Medina, D. , & Le, Q. (2011). Infectious diseases and social stigma. Applied Technologies and Innovations, 4, 58–70. 10.15208/ati.2011.7 [DOI] [Google Scholar]
- Xiang, Y.‐T. , Yang, Y. , Li, W. , Zhang, L. , Zhang, Q. , Cheung, T. , & Ng, C. H. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry, 7(3), 228–229. 10.1016/S2215-0366(20)30046-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu, X. , & Zhang, J. X. (2007). A comparison between the Chinese version of ego‐resiliency scale and connor‐davidson resilience scale. Psychological Science, 30(5), 1169–1171 (in Chinese). [Google Scholar]
- Yu, Y. , Peng, L. , Chen, L. , Long, L. , He, W. , Li, M. , & Wang, T. (2013). Resilience and social support promote posttraumatic growth of women with infertility: The mediating role of positive coping. Psychiatry Research, 215(2), 401–405. 10.1016/j.psychres.2013.10.032 [DOI] [PubMed] [Google Scholar]
- Yu, Y. , Yu, Y. , & Li, B. (2020). Effects of mindfulness and meaning in life on psychological distress in Chinese university students during the COVID‐19 epidemic: A chained mediation model. Asian Journal of Psychiatry, 53, 102211. 10.1016/j.ajp.2020.102211 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


