Abstract
Nursing home workers have been exposed to great physical and mental burdens during the COVID‐19 pandemic. Although this has generated high levels of exhaustion, it may also have contributed to feelings of professional satisfaction. The objective of this study was to explore the levels of satisfaction among nursing home workers during the COVID‐19 pandemic, as well as the role of job demands, resources and emotional experiences in explaining their levels of satisfaction. This cross‐sectional study was conducted in Spain between March and May 2020. Three hundred and thirty‐five nursing home workers participated. A quantitative analysis was conducted, as was a content analysis of the responses to an open‐ended question about the respondents' perceptions of job demands and resources during the crisis. The results showed that workers had very high levels of satisfaction. Social pressure from work, contact with death and suffering, and emotional exhaustion were negatively associated with satisfaction. Moreover, under conditions of extensive contact with suffering people and great fear of contagion, social support at work was shown to promote professional satisfaction. In conclusion, nursing home workers in Spain experienced high rates of satisfaction during the COVID‐19 crisis despite the high job demands, lack of job resources, fear of contagion and exhaustion. The main practical implication of this study is the importance of ensuring optimal working conditions in the nursing home sector in order to guarantee professional satisfaction, prevent burnout, reduce turnover and promote post‐crisis resilience.
Keywords: COVID‐19, emotional exhaustion, fear of contagion, nursing homes, professional satisfaction, social support at work
What is known about this topic
There is a high turnover rate in the nursing home and age‐care sector.
Job satisfaction is a strong indicator of resignation intentions. It is often associated with organisational variables (e.g., support at work) and psychosocial risks (e.g., burnout).
In the face of a crisis caused by an outbreak, professionals are exposed to greater physical and mental burdens, which could increase their intention to leave their position. However, studies that explore these issues in a nursing home context are limited.
What the paper adds
Professionals in nursing homes have been able to find professional satisfaction in the midst of the COVID‐19 crisis.
Experiencing professional satisfaction is not incompatible with the simultaneous experience of overwork, suffering, pressure, exhaustion, fear of contagion and anguish due to a lack of resources required to cope with the virus. Despite this situation, workers are satisfied with the work they are doing as professionals.
Social support at work is postulated as a relevant resource for maintaining satisfaction within the context of a crisis.
1. INTRODUCTION
On March 11, 2020, the World Health Organization (WHO) declared the SARS‐CoV‐2 outbreak to be a pandemic. In early March 2021, 116,166,652 cases and 2,582,528 deaths due to COVID‐19 (the disease caused by the SARS‐CoV‐2 virus) had been confirmed worldwide. Spain was one of the most affected countries, with around 3,142,358 confirmed cases and 70,501 deaths (WHO, 2020). In addition, a high number of health workers had become infected in hospitals, health centres and nursing homes (Spanish Coordination Centre for Health Alerts & Emergencies, 2020).
As shown in a synthesis study conducted by Pappa et al. (2020), frontline health workers have higher levels of perceived stress and symptoms of depression, anxiety and sleep problems due to work‐associated conditions, specifically excessive physical and mental burden and a lack of resources. A study of Spanish health personnel also reported feelings of pride, satisfaction in helping others and professional fulfilment (Luceño‐Moreno et al., 2020). Studying indicators of satisfaction among nursing home workers during the COVID‐19 crisis is relevant because satisfaction has been shown to be a good predictor of nursing home staff's intention to remain in their positions (Decker et al., 2009).
Nursing home employees have been greatly affected by the COVID‐19 crisis (Deusdad, 2020; Nyashanu et al., 2020). People who are over 60 years old and live in long‐term care residences are a high‐risk group (Spanish Coordination Centre for Health Alerts & Emergencies, 2020). In addition to their health and comorbidities, care home residents are in close contact with other residents, sharing common and private spaces. These spaces are also shared with health workers for whom, in some cases, close and direct contact is necessary to provide care. Moreover, during the COVID‐19 crisis, many residents were not transferred to hospitals despite their clinical complexity due to the lack of hospital space. This dramatically increased the care burden for nursing home workers (Deusdad, 2020).
Furthermore, at the beginning of the pandemic, nursing home workers did not have sufficient access to the equipment required to protect themselves and carry out their work safely (e.g., personal protective equipment [PPE], diagnostic tests), nor did they receive training to help them combat COVID‐19 (Fischer et al., 2020). Many nursing homes were not prepared to deal with a health crisis of this magnitude, and the system was already under strain prior to the pandemic due to reduced staff, precarious contracts, lack of medical equipment, low recognition and low wages (Rada, 2020). Some nursing home workers were even compelled to work in two residential areas due to financial need, which, in addition to increasing their workloads, increased the risk of contagion during the crisis (Armstrong et al., 2020).
Along with the physical overload, there was an emotional overload. Nursing home workers were exposed to very high levels of suffering and death and saw many residents with whom they had longstanding relationships die alone (Deusdad, 2020; Nyashanu et al., 2020). They were also subjected to social pressure by residents' families and health authorities (i.e., regional and community health departments), who implemented increased monitoring and control over the nursing facilities (Deusdad, 2020). This added to workers' feeling that their work was undervalued compared to that of hospital workers (Maben & Bridges, 2020).
Nursing home workers also experienced the fear of contagion and of infecting their loved ones first‐hand (Nyashanu et al., 2020). In some nursing homes, workers decided to isolate themselves as a preventive measure to stop the spread of the virus inside and outside the centre. This situation may have caused conflict between nursing home workers and their families. Findings from one report indicate that some healthcare workers felt guilty for being absent from their families (Huang et al., 2020). Furthermore, although important for preventing infection, containment measures have been found to increase worker's isolation, adversely affecting their cognitive, physical and emotional functioning (Webb, 2020) and exacerbating their emotional burden (Armitage & Nellums, 2020).
Recent studies have shown that today's healthcare workers present high levels of stress, emotional exhaustion, insomnia, depressive symptoms, anxiety and fear of contagion (Weilenmann et al., 2020). Some studies, however, have also pointed to the development of positive feelings amongst these workers as a result of coping with the crisis (Barello et al., 2020; Shechter et al., 2020). A recent study conducted by researchers from the Complutense University of Madrid found that 41% of 1,422 Spanish healthcare workers, mostly from the Community of Madrid (one of the areas most affected by the pandemic), showed high levels of emotional exhaustion (Luceño‐Moreno et al., 2020). At the same time, 81.9% of this sample reported feeling very fulfilled by their profession (Luceño‐Moreno et al., 2020).
Healthcare workers' feelings of gratification and fulfilment during this time of crisis could have been due to the knowledge that their work contributed to the greater good of the society and the residents they served (Santos et al., 2019). Healthcare workers generally have a strong inclination to help others. Their perceptions of the value of their work and how it can affect the lives of residents in this health crisis may, therefore, increase their levels of satisfaction, fulfilment and professional engagement (Santos et al., 2019). The availability of job resources (e.g., recognition, social support, positive feedback, learning opportunities) in demanding work contexts can contribute to the emergence of gratification and fulfilment of these feelings (Choi et al., 2012). Conversely, extreme job demands without job resources can lead to high job dissatisfaction, low professional fulfilment and low work engagement (Bishop et al., 2009).
To date, very few empirical studies have explored the demands, resources and emotional experiences of people working in nursing homes during the COVID‐19 pandemic (Daugherty & Arble, 2020; Nyashanu et al., 2020). Most studies have focused on health workers in intensive care units, health centres and specialised hospital units for COVID‐19. Furthermore, most studies have focused exclusively on investigating variables with negative emotional valence (e.g., exhaustion or traumatic stress), neglecting the possible positive emotional experiences that the crisis may have evoked among workers, such as the satisfaction of knowing that they are helping to overcome the health crisis (Shechter et al., 2020).
The objective of this study was, therefore, twofold. We explored the levels of satisfaction amongst nursing home workers amidst the COVID‐19 health crisis. We also examined select job demands (i.e., workload, social pressure from work, contact with death and suffering), resources (i.e., social support at work, human resources, PPE) and emotional experiences (i.e., fear of contagion, emotional exhaustion) as they relate to the satisfaction experienced by these workers.
The theoretical model that guided this research was the job demands and resources model (JD‐R model; Bakker & Demerouti, 2007), and specifically the ‘health impairment process’ that is initiated by job demands. According to this process, when workers are faced with prolonged, intense job demands (e.g., workload, time pressure) without the necessary resources to cope with them (e.g., job control, energy), they can experience high levels of stress and tension and become emotionally exhausted. If the situation continues, their health, job satisfaction and other well‐being indicators may deteriorate (Demerouti et al., 2000; McVicar, 2016). However, the presence of personal and job resources, besides having a direct effect on the motivation and satisfaction of the workers, can have a moderating effect on the impairment process initiated by job demands (Bakker & Demerouti, 2007).
2. METHODS
2.1. Sample and procedure
A total of 335 Spanish nursing home workers (269 women, 66 men), with an average age of 36.12 years (SD = 10.26) and 9.04 years of experience (SD = 8.11), participated in this study between March and May 2020. The main criterion for inclusion was working in a nursing home since the beginning of the pandemic. Two hundred and thirty‐seven of the workers had been in contact with COVID‐19 patients. Participants came from 43 Spanish provinces, with the highest percentages coming from Madrid (31%) and Barcelona (13.1%). As shown in Table 1, the final sample consisted of 183 professional staff (i.e., physicians, nurses, social workers, psychologists, occupational therapists, physiotherapists) and 135 support staff (i.e., nurse aides, geriatric assistants). Five centre managers also participated. Almost 75% of the participants lived with a partner, and 41% had at least one child.
TABLE 1.
Sociodemographic details of professional groups
| Categorical variables | Professional group | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Doctors | Nurses | Nurse Aides | Geriatric Assistants | Social Workers | Psychologist | Occupational Therapists | Physiotherapists | Center Management | Full sample | |
| n | 24 | 54 | 91 | 44 | 40 | 30 | 19 | 16 | 5 | 323/335 a |
| Gender | ||||||||||
| Male | 3 | 18 | 13 | 11 | 5 | 4 | 2 | 6 | 1 | 66 |
| Female | 21 | 36 | 78 | 33 | 35 | 26 | 17 | 10 | 4 | 269 |
| Relationship with a partner | ||||||||||
| With a relationship | 19 | 36 | 61 | 31 | 30 | 28 | 11 | 13 | 5 | 244 |
| Without a relationship | 5 | 18 | 30 | 13 | 10 | 2 | 8 | 3 | 0 | 91 |
| Contact with COVID‐19 patients | ||||||||||
| Yes | 22 | 47 | 61 | 29 | 21 | 20 | 14 | 13 | 3 | 237 |
| No | 2 | 7 | 29 | 15 | 19 | 10 | 5 | 3 | 2 | 96 |
| Quantitative variables | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) |
|---|---|---|---|---|---|---|---|---|---|---|
| Age | 44.2 (13.3) | 34.1 (9.1) | 37.7 (9.8) | 38.0 (12.0) | 31.9 (6.2) | 34.1 (7.1) | 29.2 (4.8) | 31.0 (6.5) | 44.6 (7.3) | 36.1 (10.2) |
| Years of experience in the field | 17.2 (13.94) | 10.3 (8.4) | 7.8 (6.17) | 9.9 (7.4) | 5.9 (4.3) | 8.0 (7.6) | 6.5 (5.0) | 8.3 (5.8) | 15.2 (7.0) | 9.0 (8.1) |
In this study, the statistical analyses were conducted with a sample of 335 workers, of which 323 reported their professions (12 missing values).
Approval from the ethics committee of the Universidad Autónoma de Madrid was obtained prior to initiating the study. Participants were recruited in two ways: (1) the researchers provided the electronic survey link to their professional contacts, who in turn distributed the link to their own contacts (snowballing); and (2) the researchers used LinkedIn and Twitter to contact healthcare workers and professionals whose public profiles indicated that they worked in nursing homes. All contacts received a digital link through which they could access the questionnaires hosted by Qualtrics online survey management. The researchers had no way of linking personal data from professional LinkedIn or Twitter profiles to the answers given in the surveys. The process was fully anonymised. Before completing the survey, individuals checked a box indicating that they agreed to participate in the research and provided their written informed consent.
2.2. Measures
The instructions given to the participants explicitly asked them to respond to the questionnaire by reflecting on their work during the COVID‐19 pandemic.
2.2.1. Sociodemographic and professional characteristics
Participants were asked to provide their sex, age, if they lived with a partner, number of children, province of origin, profession or work role, number of years of experience in the nursing home sector, and whether they were in contact with COVID‐19 cases at their workplace (yes/no).
2.2.2. Workload
The full workload subscale of the Secondary Traumatic Stress Questionnaire was used (Meda et al., 2012). It consisted of five items (e.g., ‘Sometimes, due to lack of time, decisions are made about the patient based on unclear criteria’). Responses ranged from 1 (‘strongly disagree’) to 4 (‘strongly agree’) on a Likert scale.
2.2.3. Social pressure from work
Three of the five items from the social pressure subscale of the Secondary Traumatic Stress Questionnaire were used (e.g., ‘The most annoying thing is the reproaches of the patient's relatives’; Meda et al., 2012). The two items that were omitted were more relevant to individuals working in hospitals or emergency services than to those working in nursing homes (e.g., ‘I have difficulty caring for aggressors, drug addicts, drunkards’). The response scale ranged from 1 (‘strongly disagree’) to 4 (‘strongly agree’).
2.2.4. Contact with death and suffering
The full contact with death and suffering subscale, taken from the Nursing Burnout Scale, was used (NBS; Moreno‐Jiménez et al., 2000). It consisted of four items (e.g., ‘It hurts me that patients don't get family visits’). The response scale ranged from 1 (‘strongly disagree’) to 4 (‘strongly agree’).
2.2.5. Lack of material and human protection resources
The investigators developed two items for this research, one of which referred to a lack of material resources (i.e., ‘The lack of personal protective equipment against the virus distresses me’) and the other to a lack of human resources (i.e., ‘The lack of staff needed to care for patients distresses me’). Responses ranged from 1 (‘strongly disagree’) to 4 (‘strongly agree’).
2.2.6. Social support at work
Six of the nine items from the social support at work subscale, taken from the Job Content Questionnaire, were used (Escribà‐Agüir et al., 2001). The subscale assessed co‐worker support (e.g., ‘People I work with take a personal interest in me’) and supervisory support (e.g., ‘My supervisor is helpful in getting the job done’). As some items were very similar, only three items were selected for each dimension (those with the highest factorial weights in the original scale), which served to reduce the fatigue of the participants. Responses ranged from 1 (‘strongly disagree’) to 4 (‘strongly agree’).
2.2.7. Emotional exhaustion
The full emotional exhaustion subscale, taken from the Short Questionnaire of Burnout, was used (CBB; Moreno Jiménez et al., 1997). The three items (e.g., ‘I'm exhausted from my work’) use a response scale ranging from 1 (‘strongly disagree’) to 4 (‘strongly agree’).
2.2.8. Fear of contagion
The investigators also developed three items to assess fear of contagion: (1) ‘I am constantly thinking about the possibility of catching the virus’, (2) ‘I am afraid of spreading the virus to my loved ones or residents that I care for’, and (3) ‘I am afraid of being infected by the virus’. The response scale ranged from 1 (‘strongly disagree’) to 4 (‘strongly agree’).
2.2.9. Professional satisfaction
Three of the five items from the professional satisfaction subscale, taken from the Secondary Traumatic Stress Questionnaire, were used (e.g., ‘I feel satisfied to be able to help people’; Meda et al., 2012). The two omitted items were eliminated because they were similar to the three included items, which further reduced respondent burden. The response scale ranged from 1 (‘strongly disagree’) to 4 (‘strongly agree’).
2.2.10. Job demands and resources during the COVID‐19 crisis
We included an open‐ended question following the survey questions that sought to query workers' perceptions. It read: ‘If you wish to express anything relating to the demands or resources of your work during the COVID‐19 crisis, please do so below’. The written responses were also sent to the Qualtrics platform.
2.3. Analytical strategy
All survey data were analysed using IBM SPSS, v.26.0. Descriptive, correlation, Student's t‐test (independent sample) and hierarchical regression analyses were performed. The effect size of each variable was calculated with a semipartial correlation (sr). With regard to the criteria for interpreting the effect size of each correlation (r) and semipartial correlation (sr), the effect size was considered low if the value of r varied around 0.1, medium if r varied around 0.3, and large if r varied more than 0.5 (Cohen, 1988).
For a significant moderating effect, simple slope tests were performed to examine the pattern of the interaction. Visualisation was done using the online resource provided by www.jeremydawson.co.uk/slopes.htm. All variables were centred to reduce the problem of multicollinearity. The reliability of the scales was established using Cronbach's alpha and McDonald's omega indices (see Table 2). Student's t‐test for independent samples was conducted to analyse significant differences between the study variables based on the three nominal variables of this study: sex, relationship with a partner and contact with patients with COVID. Effect sizes for Student's t‐test were estimated with Cohen's d, for which values of 0.20, 0.50 and 0.80 were obtained, representing small, medium and large effects, respectively (Cohen, 1988).
TABLE 2.
Means, standard deviations, internal consistency indexes and bivariate correlations
| Variable | M | SD | ω | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 36.12 | 10.26 | ‐ | ‐ | ||||||||||
| 2. Number of children | 0.64 | 0.85 | ‐ | 0.61** | ‐ | |||||||||
| 3. Years of experience in the field | 9.04 | 8.11 | ‐ | 0.66** | 0.37** | ‐ | ||||||||
| 4. Workload | 3.11 | 0.44 | 0.64 | −0.06 | −0.08 | 0.02 | (0.61) | |||||||
| 5. Social pressure from work | 2.57 | 0.69 | 0.60 | −0.07 | −0.10 | −0.02 | 0.29** | (0.59) | ||||||
| 6. Contact with death and suffering | 3.40 | 0.53 | 0.78 | −0.01 | 0.04 | 0.01 | 0.25** | 0.18** | (0.77) | |||||
| 7. Fear of contagion | 2.75 | 0.73 | 0.77 | −0.11 | −0.01 | −0.01 | 0.19** | 0.25** | 0.29** | (0.75) | ||||
| 8. Emotional exhaustion | 2.39 | 0.93 | 0.82 | −0.13* | −0.16** | 0.00 | 0.13* | 0.29** | −0.03 | 0.19** | (0.81) | |||
| 9. Lack of material & human protection resources | 3.16 | 0.75 | 0.72 | 0.02 | 0.00 | 0.02 | 0.34** | 0.24** | 0.35** | 0.46** | 0.20** | (0.72) | ||
| 10. Social support at work | 2.86 | 0.65 | 0.87 | −0.07 | 0.00 | −0.07 | −0.09 | −0.07 | 0.13* | 0.01 | −0.38** | −0.14* | (0.87) | |
| 11. Professional satisfaction | 3.37 | 0.58 | 0.74 | −0.01 | −0.01 | −0.02 | −0.02 | −0.14* | 0.20** | −0.05 | −0.42** | −0.04 | 0.25** | (0.72) |
In all scales, the response range is between 1 and 4.
Cronbach's alphas appear in the diagonal between parentheses; ω = McDonald's omega.
p < 0.01
p < 0.05.
The data obtained through the open‐ended question were analysed following content analysis procedures (Graneheim & Lundman, 2004). In particular, a conceptual analysis was carried out to determine the existence and frequency of concepts in a text (Wilson, 2016). The answers to the open‐ended question were separated from the answers to the quantitative survey to prevent the researchers from being influenced by the results of the scales and questionnaires. To identify themes, an inductive approach was used. As a first step, one of the authors created a list of initial codes from the data. Each code identified a situation or factor that appeared relevant to the topic. Then a codebook was created. The first author and two additional authors used the codebook to guide their independent work coding the data. Discrepancies between authors regarding the coded data were discussed and resolved through consensus during research team sessions. The authors then grouped the different codes into broader categories with similar content, and these categories were grouped into themes.
3. RESULTS
3.1. Descriptive statistics and correlations
Table 2 shows the means, standard deviations, correlations and internal consistency indices for all variables. The means obtained from the Likert scales were moderately high to very high. The high averages of workload (M = 3.11), contact with death and suffering (M = 3.40), lack of material and human resources (M = 3.16) and professional satisfaction (M = 3.37) stood out. An analysis of the three items comprising professional satisfaction (see Table 3) revealed that 98.2% of the participants agreed or totally agreed with the item ‘I feel satisfied to be able to help people’ (M = 3.74, range 1–4).
TABLE 3.
Frequencies, percentages and means for the items referring to Professional satisfaction
| Items | Totally disagree | Disagree | Agree | Totally agree | M | SD |
|---|---|---|---|---|---|---|
| 1. I feel satisfied to be able to help people | 4 (1.2%) | 2 (0.6%) | 70 (20.9%) | 259 (77.3%) | 3.74 | 0.525 |
| 2. I feel satisfied when I get home at the end of the working day | 13 (3.9%) | 57 (17%) | 142 (42.4%) | 123 (36.7%) | 3.12 | 0.825 |
| 3. The satisfaction I get from my work gives me energy to continue working on it | 10 (3%) | 46 (13.7) | 124 (37%) | 155 (46.3%) | 3.27 | 0.807 |
The response range is between 1 and 4.
The Student's t‐test reflected significant differences between women (M = 3.44; SD = 0.51) and men (M = 3.27; SD = 0.56) for the questions about contact with death and suffering (t = −2.30, p < 0.05, d = 0.30). Moreover, the same test revealed significant differences in workload (t = −2.74, p < 0.01, d = 0.30) between workers exposed to COVID patients (M = 3.15; SD = 0.41) versus unexposed workers (M = 3.01; SD = 0.49), and for the emotional exhaustion variable (t = −2.19, p < 0.05, d = 0.26), for which workers exposed to COVID patients had a higher mean than unexposed workers (M = 2.46 and M = 2.21, respectively).
Regarding the correlation analysis, social pressure from work and emotional exhaustion were significantly and negatively related to professional satisfaction (r = −0.14, p < 0.05; r = −0.42, p < 0.01; respectively), while contact with death and suffering and social support at work were positively related to professional satisfaction (r = 0.20, p < 0.01; r = 0.25, p < 0.01, respectively).
3.2. Hierarchical regression analysis
Table 4 shows the results of the regression analysis used to explain the variance attributable to professional satisfaction. The first model that controlled for sociodemographic variables was not statistically significant (F 6,282 = 0.287, p > 0.05). When the three work‐stressor variables were introduced into the second model, 7.9% of the variances was explained (F 9,279 = 2.89, p < 0.01). Two of the stressor variables, social pressure from work (β = −0.18, p < 0.01, sr = −0.16) and contact with death and suffering (β = 0.25, p < 0.001, sr = 0.24), demonstrated statistical significance.
TABLE 4.
Regression analysis for professional satisfaction
| Criterion | Professional satisfaction | ||||
|---|---|---|---|---|---|
| Standardised regression coefficients | |||||
| Predictors | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 |
| Gender | 0.038 | 0.048 | 0.062 | 0.058 | 0.028 |
| Age | 0.028 | 0.013 | 0.087 | 0.074 | 0.056 |
| Relationship with a partner | −0.047 | −0.023 | −0.022 | −0.020 | −0.035 |
| Number of children | −0.020 | 0.023 | 0.068 | 0.068 | 0.072 |
| Years of experience in the field | −0.009 | −0.006 | −0.053 | −0.049 | −0.011 |
| Contact with COVID patients | 0.052 | 0.061 | 0.004 | 0.007 | 0.010 |
| Workload | −0.035 | −0.007 | 0.001 | 0.046 | |
| Social pressure from work | −0.183** | −0.059 | −0.060 | −0.041 | |
| Contact with death and suffering | 0.253*** | 0.210*** | 0.206*** | 0.131* | |
| Fear of contagion | −0.008 | −0.001 | −0.016 | ||
| Emotional exhaustion | −0.429*** | −0.401*** | −0.449*** | ||
| Lack of MHPR | −0.023 | 0.008 | |||
| Social support at work | 0.053 | 0.009 | |||
| Workload x Lack of MHPR | −0.069 | ||||
| Workload x Social support at work | −0.081 | ||||
| Social pressure from work x Lack of MHPR | −0.043 | ||||
| Social pressure from work x Social support at work | −0.113 | ||||
| Contact with death and suffering X Lack of MHPR | −0.033 | ||||
| Contact with death and suffering X Social support at work | 0.160* | ||||
| Fear of contagion x Lack of MHPR | −0.041 | ||||
| Fear of contagion x Social support at work | 0.131* | ||||
| Emotional exhaustion x Lack of MHPR | 0.070 | ||||
| Emotional exhaustion x Social support at work | 0.073 | ||||
| R 2 | 0.006 | 0.085 | 0.239 | 0.241 | 0.307 |
| ΔR 2 | 0.079*** | 0.153*** | 0.003 | 0.066** | |
Gender was coded as 0 = male 1 = female; Relationship with a partner was coded as 0 = no 1 = yes; and contact with patients with COVID was coded as 0 = no 1= yes.
Abbreviation: MHPR, Material and Human Protection Resources.
p < 0.001
p < 0.01
p < 0.05.
When emotional experiences of fear of contagion and emotional exhaustion were introduced (see Model 3 in Table 4), the model also was statistically significant (F 11,277 = 7.88, p < 0.001), explaining 15.3% of the variance (p < 0.001). However, only emotional exhaustion contributed to an explanation of professional satisfaction (β = −0.42, p < 0.001, sr = −0.38). When job resources were introduced in Model 4, the model remained statistically significant (F 13,275 = 9.48, p < 0.001), although only 0.3% of the variance was explained—a non‐significant increase (p > 0.05).
The interaction terms were introduced in Model 5, which was also significant, explaining 6.6% of the variance (p < 0.01). Specifically, the interactions between contact with death and suffering and social support at work (β = 0.16, p < 0.05, sr = 0.12), and fear of contagion and social support at work (β = 0.13, p < 0.05, sr = 0.11), were significant. Figure 1 shows that the relationship between contact with death and suffering and professional satisfaction was statistically significant and increased only for the high levels of social support at work (slope gradient = 0.492, t = 3.31, p < 0.001), but not for the low levels (slope gradient = −0.066, t = −0.538, p > 0.05). That is to say, professionals with high levels of social support at work regarding their exposure to patient and family suffering experienced more professional satisfaction than those with low levels of support.
FIGURE 1.
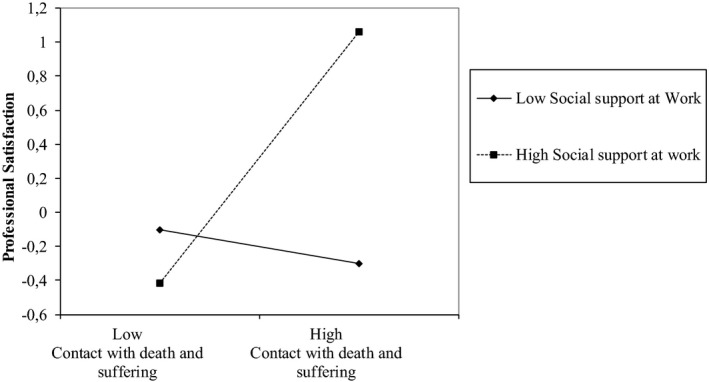
Interaction effects of Contact with death & suffering and Social support at work in predicting Professional satisfaction
Figure 2, however, shows how the relationship between fear of contagion and professional satisfaction interacted in a statistically significant and increasing manner with high levels of social support at work (slope gradient = 0.275, t = 1.96, p < 0.05) and with low levels of support (slope gradient = −0.190, t = −2.005, p < 0.05). So, workers with high levels of social support regarding their fear of contagion experienced more professional satisfaction than workers with low levels of support. The greater the fear of contagion among workers who received little social support, the lower their professional satisfaction. All the variables introduced in the last model (step 5) explained a total variance of 30.7% for professional satisfaction.
FIGURE 2.
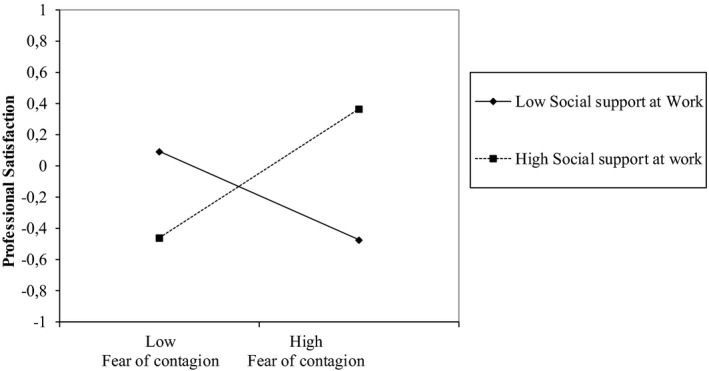
Interaction effects of Fear of contagion and Social support at work in predicting Professional satisfaction
3.3. Content analyses
One hundred and twenty‐one participants (36.1%) responded to the open‐ended question about job demands and resources during the COVID‐19 crisis. Of these, 31% were nurse aides, 20% were nurses, 10% were doctors, 7% were social workers and the rest were ‘other professionals’, such as psychologists and physiotherapists. The content analysis of the responses revealed two themes regarding the perceptions and difficulties of nursing home staff during the COVID‐19 pandemic: (a) inadequate working conditions and lack of resources, and (b) impact and consequences of the COVID‐19 crisis.
Regarding the first theme, the absence of resources was one of the most frequent sources of distress reported by the professionals. On many occasions, the workers reported an absence of material resources, such as PPE, that would enable them to fulfil their caregiving duties safely. In addition, their distress was exacerbated by ongoing negative working conditions, such as poor salaries and high turnover rates.
The second theme relates to the physical and mental consequences experienced by the professionals. Although the majority reported negative experiences derived from their work during the COVID‐19 crisis (e.g., depression, ambivalence, being infected with COVID‐19), some reported positive feelings (e.g., a sense of fulfilment, pride). The results of meaning units, codes and frequencies, subthemes, and themes from the content analysis of answers to the open‐ended question are shown in Table 5.
TABLE 5.
Meaning units, codes and frequencies, and subthemes and themes from the content analysis of answers to the open question
| Theme | Subtheme | Code (number of reports) | Examples |
|---|---|---|---|
| Inadequate working conditions and lack of resources | Lack of resources to deal with the virus | Lack of tests (28) |
“We work blindly, not knowing whether we are sentencing our residents to death through lack of resources and materials” “We have not been given enough protective equipment” “We work without protection; only with will” |
| Lack of PPE (65) | |||
| Lack of staff (19) | |||
| Lack of support | Lack of institutional support (25) |
“In this work we are totally abandoned, without protective equipment or anyone who controls what is going on” “I have felt supported by my coworkers, but not by the manager or by the political institutions” “I feel that the work we do in the residences is not valued, since the news only shows the negative side—the numbers of dead and the residences that are overwhelmed” |
|
| Lack of recognition (17) | |||
| Inadequate organisational management of COVID−19 crisis | Inadequate organisation (21) |
“We suffer from] scarce materials and we have not been instructed how to use EPP correctly; therefore, we are forced to improvise” “The mismanagement of prevention and organisation (testing prior to entry of new personnel or personnel who have had contact with COVID−19, is becoming a serious problem” |
|
| Insufficient information and/or training (10) | |||
| Failure of prevention (14) | |||
| Lack of action protocols (9) | |||
| Excessive job demands | Work overload (14) |
“Double shifts and work outside normal hours, because you never finish and are not even rewarded with a thank you” “There is a lack of empathy from family members in general” |
|
| Increased working hours (4) | |||
| Difficulties with residents’ families (4) | |||
| Previous working conditions | Lack of adequate staff (6) |
“Since it is a job that requires a lot of effort and dedication … the salary should be increased, especially in nursing homes, which do not pay more than 900 euros” “COVID‐19 has been the trigger that has exposed the deficiencies of the system” |
|
| Low wage (6) | |||
| Job instability (4) | |||
| Coping with lack of resources | Recycle PPE (9) | “We have faced the virus with minimal resources, we have recycled the masks for up to six days because we do not have any more, we have protected ourselves with garbage bags against COVID patients with serious pathologies, cough, secretions …” | |
| Making own PPE (5) | |||
| Asking for PPE donations (3) | |||
| Impact and consequences of COVID−19 crisis | Negative physical and psychological consequences | Staff infection (11) |
“Although I feel satisfied with my profession, I also feel helpless for not being able to carry out my duties effectively due to lack of resources. The measures are applied too late and people die” “It is heartbreaking, and I feel guilty for not being able to remain calm and do more to save the life of my patient and the peace of mind of her children and grandchildren” “Anguish … seeing the neglect and total dehumanisation due to lack of hands … I couldn't stand it and I had to ask for unpaid leave, despite the dilemma that, as a nurse, that involved: abandon even more of those people or end up being more devastated than I already I was” |
| Fear of contagion (5) | |||
| Concerns about future consequences (4) | |||
| Concerns about care received by residents (21) | |||
| Suffering due to residents' deaths (11) | |||
| Depressive feelings (5) | |||
| Anxious feelings (5) | |||
| Ambivalent feelings (8) | |||
| Frustration/feelings of impotence (11) | |||
| Exhaustion (4) | |||
| Positive psychological consequences | Gratitude (7) | “The majority of the team has responded with humanity and professionalism, which I am proud of” | |
| Professional fulfillment (2) | |||
| Sense of pride (3) |
4. DISCUSSION
The main objective of this study was to explore the professional satisfaction of nursing home workers in Spain who faced the health crisis caused by COVID‐19. We also explored the role of certain job demands, resources and emotional experiences and the relationship between these aspects and professional satisfaction.
Our results showed that workers reported very high levels of workload pressure, contact with death and suffering, and a lack of material and human resources. Women were more affected than men by contact with death and suffering. In addition, workers exhibited moderately high levels of social pressure from work, fear of contagion and emotional exhaustion. These findings are in line with work experiences found in the emerging literature related to the COVID‐19 pandemic (Huang et al., 2020; Lu et al., 2020; Nyashanu et al., 2020). Overload and exhaustion were especially high among workers who had contact with COVID‐19 patients.
The survey results also revealed very high levels of professional satisfaction among nursing home workers during the COVID‐19 crisis, especially in terms of being able to help people. Staff perceptions of the value, impact and contribution of their work to society and the residents of the nursing homes during the COVID‐19 crisis have been shown to contribute to high levels of professional satisfaction despite the negative circumstances and working conditions (Santos et al., 2019; Shechter et al., 2020). Moderately high levels of social support at work were also observed, a finding consistent with another report on workers who took a collective approach to the COVID‐19 crisis and helped each other through difficult times (Weilenmann et al., 2020).
The possibility that workers may simultaneously develop feelings and experiences of overload, emotional exhaustion, support and professional satisfaction while under great physical and mental burden was consistent with the findings of recent studies, which observed that facing a crisis can also generate experiences of professional fulfilment and motivation (Barello et al., 2020; Brooks et al., 2018; Luceño‐Moreno et al., 2020). Some of these findings were also corroborated by the answers that participants in the present study gave to the open‐ended question about job demands and available resources during the health emergency. Data from the quantitative analysis and the content analysis converged, especially regarding perceptions of lack of resources, exposure to high degrees of suffering, fear of contagion and social pressure from work.
An important finding is that, according to the quantitative analysis, lack of material and human resources had no effect on professional satisfaction. This paradox could be explained by the fact that the dissatisfaction felt by workers regarding the lack of material and human resources was directed more toward the work organisation and the political management of the crisis. The acquisition and provision of resources typically depended on management by regional and national governments, and workers knew this. Professional satisfaction remained high, however, because it was related more to the workers' value and role in helping others.
The analysis also revealed that as workers experienced more social pressure in their jobs and as their emotional exhaustion increased, they became less satisfied with their jobs. In terms of social pressure, these results may indicate workers' dissatisfaction with the fact that they are sometimes assigned responsibilities that they are not equipped to deal with, their interventions and professionalism are questioned, and they are reproached by families for not providing sufficient care to their loved ones (Abrahamson et al., 2009; Deusdad, 2020). Emotional exhaustion could generate professional dissatisfaction if workers perceive that they are giving far more than they are receiving during this crisis (Van Bogaert et al., 2010).
Another interesting result revealed by the analysis was that contact with death and suffering was positively associated with professional satisfaction. An analysis of the content of the items allowed us to infer a tentative explanation for this finding. It is possible that nursing home workers achieved more professional satisfaction by viewing themselves as essential mediators in meeting the emotional needs of their patients and their families and helping them deal with confinement, loneliness and even death. In this way, workers and professionals may have had an opportunity to develop their full human potential through their caregiving roles in situations where residents were not able to receive visits from their families. At the same time, they witnessed residents' suffering due to isolation from their loved ones and accompanied them through illness and death. This explanation is congruent with previous studies on how, in healthcare professions, emotional demands can be associated with positive indicators of work motivation, especially when healthcare workers have the emotional competence to face the demands (Blanco‐Donoso et al., 2015; Slocum‐Gori et al., 2013). Similarly, the association could reflect experiences of ‘compassion satisfaction’, which stems from the emotional rewards of caring for others in a healthcare context (Slocum‐Gori et al., 2013).
Finally, the results showed that workers with more social support at work experienced higher levels of professional satisfaction under demanding work conditions, such as those involving high degrees of contact with death and suffering and high levels of fear of contagion. This aligns with other studies that found that workers who worked in a positive work climate and who received support from their organisations, including supervisors and colleagues, experienced high levels of job satisfaction (Bishop et al., 2009; Choi et al., 2012). Social support at work helps people achieve work goals (i.e., the instrumental value of support) and protects them from the negative consequences of stressful work experiences (i.e., the emotional value of support; Van de Ven et al., 2013).
This study has some limitations. First, this research used a cross‐sectional design. Second, the open question only asked workers about factors relating to their job demands and resources; it did not explicitly focus on aspects related to professional satisfaction. Third, only a few items and two subscales with low Cronbach's alpha indices (workload [α = 0.61] and social pressure from work [α = 0.59]) were used to assess the study variables. This calls for caution in interpreting the results relating to these variables. However, some authors consider these indices to be acceptable for scales that have not previously been used for a specific population and comprise a small number of items (Clark & Watson, 1995).
Finally, another limitation is the sampling technique used in this study (i.e., the snowball technique). Since this was not random sampling, some biases may have occurred. In this regard, future research should improve the sampling technique and method of recruitment to avoid these possible biases. In the future, it would also be interesting to carry out longitudinal studies of mixed design with a greater focus on the investigation of positive emotional experiences, such as professional satisfaction, work meaning and post‐traumatic growth.
4.1. Practical implications
It is essential to increase job resources for workers and professionals working in nursing homes. Increased staffing, specialised infection training, more diagnostic tests, and more human and material protective resources would help prevent overload and exhaustion and reduce the fear of contagion. It is also very important to support and encourage collective coping regarding shared stressors (e.g., a pandemic) by increasing levels of institutional, organisational and team support. As Deusdad (2020) points out, it is not enough for workers to be willing to face a crisis; structural changes are needed. We cannot continue to expect satisfied workers to do their jobs effectively if health, social and labour organisations do not improve their working conditions. If these issues are not addressed, turnover rates in the nursing home sector could increase greatly after the crisis, with highly negative consequences for the system should new infection outbreaks occur.
Finally, high levels of professional satisfaction indicated that nursing home workers and professionals felt proud of their work and the role they played during the crisis, assisting vulnerable people faced with adversity. It would be interesting to work with them on the positive aspects of their work, such as its purpose, meaning and social value, as well as on the development of their resilience and personal growth under adverse conditions once this health crisis has passed.
5. CONCLUSION
Workers in nursing homes in Spain were able to find professional satisfaction with their work in the midst of the COVID‐19 crisis. Professional satisfaction helped to compensate for their simultaneous experiences of overload, contact with suffering, pressure, exhaustion, fear of contagion, distress due to a lack of human resources and protection to face the virus. Social support at work was postulated as a relevant and vital resource for maintaining professional satisfaction in crisis contexts.
CONFLICTS OF INTEREST
The authors declare that there is no conflict of interest.
ACKNOWLEDGEMENTS
The authors appreciate the invaluable participation of all professionals in this study in times of crisis.
Blanco‐Donoso LM, Moreno‐Jiménez J, Gallego‐Alberto L, Amutio A, Moreno‐Jiménez B, Garrosa E. Satisfied as professionals, but also exhausted and worried!!: The role of job demands, resources and emotional experiences of Spanish nursing home workers during the COVID‐19 pandemic. Health Soc Care Community. 2022;30:e148–e160. 10.1111/hsc.13422
Funding information
This work was supported by I+D+I National Project of Ministerio de Ciencia e Innovación (PID2019‐106368GB‐I00) AEI/10.13039/501100011033.
DATA AVAILABILITY STATEMENT
Data available on request from the authors.
REFERENCES
- Abrahamson, K. , Jill Suitor, J. , & Pillemer, K. (2009). Conflict between nursing home staff and residents' families: Does it increase burnout? Journal of Aging and Health, 21(6), 895–912. 10.1177/0898264309340695 [DOI] [PubMed] [Google Scholar]
- Armitage, R. , & Nellums, L. B. (2020). COVID‐19 and the consequences of isolating the elderly. The Lancet Public Health, 5(5), e256. 10.1016/S2468-2667(20)30061-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong, P. , Armstrong, H. , Choiniere, J. , Lowndes, R. , & Struthers, J. (2020). Re‐imagining long‐term residential care in the COVID‐19 crisis. Canadian Centre for Policy Alternatives. [Google Scholar]
- Bakker, A. B. , & Demerouti, E. (2007). The job demands‐resources model: State of the art. Journal of Managerial Psychology, 22(3), 309–328. 10.1108/02683940710733115 [DOI] [Google Scholar]
- Barello, S. , Palamenghi, L. , & Graffigna, G. (2020). Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID‐19 pandemic. Psychiatry Research, 290, 113129. 10.1016/j.psychres.2020.113129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop, C. E. , Squillace, M. R. , Meagher, J. , Anderson, W. L. , & Wiener, J. M. (2009). Nursing home work practices and nursing assistants' job satisfaction. The Gerontologist, 49(5), 611–622. 10.1093/geront/gnp040 [DOI] [PubMed] [Google Scholar]
- Blanco‐Donoso, L. M. , Demerouti, E. , Hernández, E. G. , Moreno‐Jimenez, B. , & Cobo, I. C. (2015). Positive benefits of caring on nurses' motivation and well‐being: A diary study about the role of emotional regulation abilities at work. International Journal of Nursing Studies, 52(4), 804–816. 10.1016/j.ijnurstu.2015.01.002 [DOI] [PubMed] [Google Scholar]
- Brooks, S. K. , Dunn, R. , Amlôt, R. , Greenberg, N. , & Rubin, G. J. (2018). Training and post–disaster interventions for the psychological impacts on disaster–exposed employees: A systematic review. Journal of Mental Health, 1–25, 10.1080/09638237.2018.1437610 [DOI] [PubMed] [Google Scholar]
- Choi, J. , Flynn, L. , & Aiken, L. H. (2012). Nursing practice environment and registered nurses' job satisfaction in nursing homes. The Gerontologist, 52(4), 484–492. 10.1093/geront/gnr101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark, L. A. , & Watson, D. (1995). Constructing validity: Basic issues in objective scale development. Psychological Assessment, 7, 309–319. 10.1037/1040-3590.7.3.309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Erlbaum. 10.4324/9780203771587 [DOI] [Google Scholar]
- Daugherty, A. M. , & Arble, E. P. (2020). Prevalence of mental health symptoms in residential healthcare workers in Michigan during the COVID‐19 pandemic. Psychiatry Research, 291, 113266. 10.1016/j.psychres.2020.113266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker, F. H. , Harris‐Kojetin, L. D. , & Bercovitz, A. (2009). Intrinsic job satisfaction, overall satisfaction, and intention to leave the job among nursing assistants in nursing homes. The Gerontologist, 49(5), 596–610. 10.1093/geront/gnp051 [DOI] [PubMed] [Google Scholar]
- Demerouti, E. , Bakker, A. B. , Nachreiner, F. , & Schaufeli, W. B. (2000). A model of burnout and life satisfaction amongst nurses. Journal of Advanced Nursing, 32, 454–464. 10.1046/j.1365-2648.2000.01496.x [DOI] [PubMed] [Google Scholar]
- Deusdad, B. (2020). COVID–19 and care homes and nursing homes crisis in Spain: Ageism and scarcity of resources. Research on Ageing and Social Policy, 8(2). 10.17583/rasp.2020.5598 [DOI] [Google Scholar]
- Escribà‐Agüir, V. , Pons, R. M. , & Reus, E. F. (2001). Validation of the Job Content Questionnaire in hospital nursing staff. Gaceta Sanitaria, 15(2), 142–149. 10.1016/S0213-9111(01)71533-6 [DOI] [PubMed] [Google Scholar]
- Fischer, F. , Raiber, L. , Boscher, C. , & Winter, M. H. J. (2020). COVID‐19 and the elderly: Who cares? Frontiers in Public Health, 8, 151. 10.3389/fpubh.2020.00151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graneheim, U. H. , & Lundman, B. (2004). Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today, 24(2), 105–112. 10.1016/j.nedt.2003.10.001 [DOI] [PubMed] [Google Scholar]
- Huang, L. , Lei, W. , Xu, F. , Liu, H. , & Yu, L. (2020). Emotional responses and coping strategies in nurses and nursing students during Covid‐19 outbreak: A comparative study. PLoS One, 15(8), e0237303. 10.1371/journal.pone.0237303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu, W. , Wang, H. , Lin, Y. , & Li, L. (2020). Psychological status of medical workforce during the COVID‐19 pandemic: A cross‐sectional study. Psychiatry Research, 288, 112936. 10.1016/j.psychres.2020.112936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luceño‐Moreno, L. , Talavera‐Velasco, B. , García‐Albuerne, Y. , & Martín‐García, J. (2020). Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID‐19 Pandemic. International Journal of Environmental Research and Public Health, 17(15), 5514. 10.3390/ijerph17155514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maben, J. , & Bridges, J. (2020). Covid‐19: Supporting nurses' psychological and mental health. Journal of Clinical Nursing, 29(15‐16), 2742–2750. 10.1111/jocn.15307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McVicar, A. (2016). Scoping the common antecedents of job stress and job satisfaction for nurses (2000–2013) using the job demands‐resources model of stress. Journal of Nursing Management, 24(2), E112–E136. 10.1111/jonm.12326 [DOI] [PubMed] [Google Scholar]
- Meda, R. , Moreno‐Jiménez, B. , Palomera, A. , Arias, E. , & Vargas, R. (2012). La Evaluación del Estrés Traumático Secundario: Estudio Comparado en Bomberos y Paramédicos de los Servicios de Emergencia de Guadalajara, México [Secondary Traumatic Stress Assesment. Comparative Study of Firemen and Paramedics in Emergency Services]. Terapia Psicológica, 30(2), 31–41. 10.4067/S0718-48082012000200003 [DOI] [Google Scholar]
- Moreno Jiménez, B. , Bustos Rodríguez, R. , Matallana Álvarez, A. , & Miralles Caballero, T. (1997). La evaluación del burnout. Problemas y alternativas. El CCB como evaluación de los elementos del proceso [The burnout assessment. Problems and alternatives. The CBB as an assessment of the elements of the process]. Journal of Work and Organizational Psychology, 13(2), 185–207. [Google Scholar]
- Moreno‐Jiménez, B. , Garrosa, E. , & González‐Gutiérrez, J. L. (2000). Desgaste profesional sanitario de enfermería. Validación factorial del CDPE [Nursing burnout. Development and factorial validation of the CDPE]. Archivos De Prevención De Riesgos Laborales, 3(1), 18–28. [Google Scholar]
- Nyashanu, M. , Pfende, F. , & Ekpenyong, M. S. (2020). Triggers of mental health problems among frontline healthcare workers during the COVID‐19 pandemic in private care homes and domiciliary care agencies: Lived experiences of care workers in the Midlands region, UK. Health & Social Care in the Community, 1–7. 10.1111/hsc.13204 [DOI] [PubMed] [Google Scholar]
- Pappa, S. , Ntella, V. , Giannakas, T. , Giannakoulis, V. G. , Papoutsi, E. , & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID‐19 pandemic: A systematic review and meta‐analysis. Brain, Behavior, and Immunity, 88, 901–907. 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rada, A. (2020). Covid‐19: The precarious position of Spain's nursing homes. BMJ, 369, 1–3. 10.1136/bmj.m1554 [DOI] [PubMed] [Google Scholar]
- Santos, A. , Chambel, M. J. , & Castanheira, F. (2019). Well–being among hospital nurses: A cross–sectional study of the contributions of relational job characteristics. International Journal of Nursing Studies, 105, 103438. 10.1016/j.ijnurstu.2019.103438 [DOI] [PubMed] [Google Scholar]
- Shechter, A. , Diaz, F. , Moise, N. , Anstey, D. E. , Ye, S. , Agarwal, S. , Birk, J. L. , Brodie, D. , Cannone, D. E. , Chang, B. , Claassen, J. , Cornelius, T. , Derby, L. , Dong, M. , Givens, R. C. , Hochman, B. , Homma, S. , Kronish, I. M. , Lee, S. A. J. , … Abdalla, M. (2020). Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID‐19 pandemic. General Hospital Psychiatry, 66, 1–8. 10.1016/j.genhosppsych.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slocum‐Gori, S. , Hemsworth, D. , Chan, W. W. , Carson, A. , & Kazanjian, A. (2013). Understanding compassion satisfaction, compassion fatigue and burnout: A survey of the hospice palliative care workforce. Palliative Medicine, 27(2), 172–178. 10.1177/0269216311431311 [DOI] [PubMed] [Google Scholar]
- Spanish Coordination Centre for Health Alerts and Emergencies . (2020). Scientific‐technical information: Coronavirus disease, COVID‐19. Update, May 18, 2020. Spanish Ministry of Health. Retrieved from https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov–China/documentos/ITCoronavirus.pdf [Google Scholar]
- Van Bogaert, P. , Clarke, S. , Roelant, E. , Meulemans, H. , & Van de Heyning, P. (2010). Impacts of unit‐level nurse practice environment and burnout on nurse‐reported outcomes: A multilevel modelling approach. Journal of Clinical Nursing, 19(11–12), 1664–1674. 10.1111/j.1365-2702.2009.03128.x [DOI] [PubMed] [Google Scholar]
- Van de Ven, B. , van den Tooren, M. , & Vlerick, P. (2013). Emotional job resources and emotional support seeking as moderators of the relation between emotional job demands and emotional exhaustion: A two‐wave panel study. Journal of Occupational Health Psychology, 18(1), 1–8. 10.1037/a0030656 [DOI] [PubMed] [Google Scholar]
- Webb, L. (2020). Covid‐19 lockdown: A perfect storm for older people's mental health. Journal of Psychiatric and Mental Health Nursing, 28, 300. 10.1111/jpm.12644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weilenmann, S. , Ernst, J. , Petry, H. , Sazpinar, O. , Pfaltz, M. C. , Gehrke, S. , Spiller, T. R. (2020). Health care workers mental health during the first weeks of the SARS‐CoV‐2 pandemic in Switzerland: A cross‐sectional study. medRxiv, 10.1101/2020.05.04.20088625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO , World Health Organization. (2020). Coronavirus disease 2019 (COVID–19): Weekly Epidemiological Update, 9 March 2020. World Health Organization. Retrieved from https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20210309_weekly_epi_update_30.pdf?sfvrsn=4e7da248_8&download=true [Google Scholar]
- Wilson, V. (2016). Research methods: Content analysis. Evidence Based Library and Information Practice, 11(1(S)), 41–43. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request from the authors.


