Abstract
The effort to limit the spread of the coronavirus (COVID‐19) has relied heavily on the general public's compliance with health guidelines limiting social contact and mitigating risk when contact occurs. The aim of this study was to identify latent variables underlying adherence to COVID‐19 guidelines and to examine demographic and psychological predictors of adherence. A sample of US adults (N = 1,200) were surveyed in late April to mid‐May 2020. The factor structure of adherence was examined using exploratory factor analysis. Machine learning regression models using elastic net regularization were used to examine predictors of adherence. Two factors characterized adherence: avoidance and cleaning. Elastic net models identified differential demographic and psychological predictors of these two forms of adherence. Religious affiliation, denial coping, full‐time employment, substance use coping, and being 60 or older predicted lower avoidance adherence. Behavioral and mindfulness emotion regulation skills, agreeableness, and Democrat political affiliation predicted greater avoidance adherence. For cleaning adherence, interpersonal and behavioral emotion regulation skills and conscientiousness emerged as strong predictors of greater cleaning. Efforts to promote compliance with COVID‐19 health guidelines may benefit from distinguishing avoidance and cleaning adherence and considering predictors of each of these aspects of adherence.
Keywords: COVID‐19, health adherence, health behaviors, machine learning
INTRODUCTION
The novel coronavirus disease 2019 (COVID‐19) was declared a global pandemic by the World Health Organization on March 11, 2020 (Cucinotta & Vanelli, 2020). The first case was reported in the United States in early 2020, and infections have since spread across the country. Through testing, the United States has identified over 29 million COVID‐19 cases as of March 2021, with over 500,000 deaths (CDC COVID Data Tracker, Retrieved March 19, 2021). Public health officials have urged the general public to adhere to guidelines aimed at reducing transmission of the virus and the health consequences of infection, which include a risk of hospitalization and death.
On March 16, 2020, the White House and United States Centers for Disease Control and Prevention (CDC) put out initial guidelines for behavioral recommendations for individuals to slow the spread of COVID‐19 (CDC, 2020). These behaviors included the following: working from home when possible; avoiding social gatherings of 10 or more people; avoiding eating or drinking at bars, restaurants, and food courts; avoiding discretionary travel, shopping trips, and social visits; and practicing good hygiene. After initial suggestions to the contrary, wearing face coverings was recommended by the CDC for non‐healthcare professionals on April 3, 2020 (Chavez et al., 2020). While CDC guidelines were directed at everyone in the United States, regulation of COVID‐19 precautions varied by locality and across time. Perhaps because compliance with these guidelines entailed making substantial lifestyle changes, compliance with these guidelines has varied considerably (Kirzinger et al., 2020).
Predictors of adherence to COVID‐19 health guidelines
Understanding what predicts adherence to COVID‐19 health guidelines remains a public health priority. Researchers are in the early stages of identifying individual characteristics, which help to explain COVID‐19 adherence. To date, demographic characteristics, political affiliation, and risk for severe illness if infected have been identified as predictors. Women have consistently been found to be somewhat more adherent to COVID‐19 health guidelines compared with men (Clark et al., 2020; Czeisler et al., 2020; Nivette et al., 2021; Park et al., 2020; Pollak et al., 2020; Qeadan et al., 2020; Raude et al., 2020; Solomou & Constantinidou, 2020). Although the findings have been mixed, several studies have found age to be related to COVID‐19 health behaviors. Younger age has been associated with less (Solomou & Constantinidou, 2020) and greater (Steens et al., 2020) adherence in different studies. Another study failed to find a connection between age and COVID‐19 adherence (Clark et al., 2020). Political affiliation has also been tied to adherence, with evidence from geolocation data showing that residents of Republican (vs. Democratic) counties were less likely to comply with social distancing guidelines (Painter & Qiu, 2021). Finally, those as risk for severe illness (e.g. those with asthma, hypertension, or obesity) tend to report greater adherence (Qeadan et al., 2020).
Psychological vulnerability and the experience of mental health symptoms limit people's ability to function in a variety of ways, including successfully engaging in health behaviors. Research on other health behaviors has shown that mental health challenges such as anxiety and depression interfere with efforts to engage and persist with health behaviors (Hopko et al., 2017; Katon & Ciechanowski, 2002). On the other hand, those with greater health anxiety or worry might be expected to engage in health behaviors more fully. In fact, in one study, depressive symptoms were associated with lower COVID‐19 adherence, whereas anxiety was associated with greater COVID‐19 adherence (Solomou & Constantinidou, 2020). Mental health research has identified important vulnerability and resilience factors that have been found to be key to mental health and also extend to physical health and health‐promoting behaviors (Alloy & Riskind, 2006; Friedman, 2011). Many of these variables are likely to be important determinants of COVID‐19 adherence, though they largely have yet to be investigated.
To adhere fully to the health behaviors recommended by the CDC requires persistent planning and effort in the face of stressful circumstances and heightened emotions. Thus, there is reason to expect that individuals who utilize adaptive strategies to cope with stressful situations and are skilled at regulating their emotions to achieve their goals (Gross & Thompson, 2007) may be better equipped to fully adhere to COVID‐19 health guidelines. For example, maintaining disciplined cleaning behaviors and coordinating one's day‐to‐day activities while complying with social distancing and travel restrictions require strong coping skills and self‐control. Consistent with this view, Wolff et al. (2020) found that self‐control (i.e. the ability to control one's behavior to meet one's goals) was related to greater adherence to social distancing guidelines. Similarly, two studies have found that low perceived efficacy for following COVID‐19 guidelines was related to lower adherence (Chong et al., 2020; Pollak et al., 2020). Finally, Chong et al. (2020) also found avoidance‐based coping (i.e. strategies aimed at avoiding stressful situations, including self‐distraction, denial, substance use, behavioral disengagement, and self‐blaming) was associated with less adherence to COVID‐19 guidelines. Thus, theory and existing research suggests that coping processes and emotion regulation skills are likely related to COVID‐19 adherence, but it is not yet clear which specific skills and coping strategies promote various forms of adherence.
This study
The present study sought to examine demographic and psychological predictors of COVID‐19 adherence. We had two aims to achieve this overall goal. First, we planned to examine the factor structure of items assessing adherence to CDC‐recommended COVID‐19 health guidelines. Second, informed by evidence of adherence factors, we planned to examine demographic and psychological variables as predictors of adherence.
To achieve these aims, we collected data in the United States from a diverse adult sample between April 24 and May 21, 2020. During this period, most states were under stay‐at‐home orders, with several states experimenting with loosening restrictions and targeted re‐opening (Moreland et al., 2020). COVID‐19 testing was not widely available for the general public, and no vaccines or known treatments existed. With the rapid changes that came with the pandemic, research teams developed their own measures of COVID‐19 health behaviors to meet the needs of the moment. Several research groups in the United States assessed degree of adherence to the guidelines put forth by the CDC; however, assessment strategies varied. Although overall scores have most often been used, there have been some indications that adherence may be composed of more than one factor (see Solomou & Constantinidou, 2020). It is important to identify the factors that account for adherence to COVID‐19 health guidelines to inform efforts to identify predictors of adherence.
To examine predictors of adherence, we used elastic net regression to evaluate a set of 64 demographic and psychological factors. The set of predictors included demographic variables commonly assessed in health research, reflecting groups in which interventions may be aimed, as well as specific psychological characteristics, including emotion regulation skills and coping strategies, which may inform the types of interventions that may be successful in promoting adherence. There are several advantages of elastic net over standard multivariate regression approaches. Elastic net models perform both regularization by penalizing coefficient estimates and variable selection by shrinking the coefficients of irrelevant predictors to exactly zero, dropping them out of the model (Zou & Hastie, 2005). These procedures help to prevent overfitting (i.e. identifying sample specific relations that are unlikely to generalize to other samples). Furthermore, elastic net was developed to handle large predictor sets (such as when p > n) and high correlations among predictors. Consistent with recommendations for elastic net models, we used cross‐validation to select the best‐fitting model using a training dataset and then evaluated the selected model in a separate validation dataset. This sophisticated analytic approach will allow us to examine the importance of demographic factors and key psychological factors in explaining adherence to COVID‐19 health behaviors.
METHODS
Sample
A convenience sample of adults (N = 1,200) in the United States were recruited through Amazon Mechanical Turk (MTurk) to participate in an online study related to the COVID‐19 pandemic. To facilitate the collection of high‐quality data in MTurk, procedures were implemented in line with recommendations by Aguinis et al. (2020). Participants were required to have a strong record of providing quality responses (i.e. at least a 95% MTurk HIT approval rate) and pass multiple attention check items embedded throughout the online assessment. Other screening procedures were also utilized, such as age and location verification and blockage of suspicious or duplicate IP locations. Participants received $5 for completion of self‐report surveys. Study procedures were approved by an institutional review board at the Ohio State University. The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
The mean age of the sample was 37.7 years (SD = 11.5). Of all participants, 59.0% identified as male, 40.3% identified as female, and.5% identified as something else (e.g. gender fluid, non‐binary). The racial breakdown of the sample was as follows: 73.8% white, 16.3% black, 6.1% Asian, 2.3% more than race, 0.5% American Indian or Alaskan Native, and 0.1% Native Hawaiian or Pacific Islander. Approximately a fifth of the sample identified as Hispanic. Overall, the sample was relatively well educated, with 68.8% attaining at least a four‐year college degree. A large majority (78.6%) reported having full‐time employment prior to the start of the pandemic. At the time of the survey, 65.0% indicated they remained employed full‐time. Participants tended to be married (56.5%) and live with at least one other person (81.5%).
Measures
Demographic predictors
Participants reported the following demographic information used in analyses: age, sex, race, ethnicity, sexual orientation, education level, employment status, income level, marital status, number of children, number of people in household, political affiliation, religious affiliation, and perceived health status. Participants were asked whether they have ever been diagnosed with a mental health condition and whether they are currently receiving mental health treatment. Participants also reported on particular risk factors for COVID‐19, including whether they have a chronic health condition or are immunocompromised, or whether they are living in a household with someone who is 60 years of age or older or are at greater risk due to their physical health status. Participants reported the number of people they spoke to in the past week and the number of hours spent consuming pandemic‐related media in the past week. The Financial Chronic Stress Scale (FCSS; Lantz et al., 2005) was used to assess financial strain.
Psychological predictors
Participants completed psychological inventories assessing mental health, stress, coping, and personality. Symptoms of psychopathology were assessed with the following measures: generalized anxiety with the Generalized Anxiety Disorder Scale‐7 (GAD‐7; Spitzer et al., 2006); depressive symptoms with the Quick Inventory of Depressive Symptomatology‐Self‐Report (QIDS‐SR; Rush et al., 2003); and health anxiety with the Health Anxiety Inventory (HAI; Salkovskis et al., 2002). Loneliness was assessed with the UCLA Loneliness Scale (version 3; Russell, 1996) and rumination (i.e. brooding and reflection) with the Ruminative Response Scale (RRS; Treynor et al., 2003). To assess perceptions of stress, the Perceived Stress Scale was used (PSS; Cohen et al., 1983). Disproportionality of depressive reactions given one's life stress was assessed with the Proportionality of Depressive Reactions (PDR) measure (Pfeifer & Strunk, 2021). Attitudes toward pursuing one's goals were assessed with the Hope Scale (Snyder et al., 1991), which distinguishes agency and planning to accomplish goals. Negative attitudes about the future were assessed with the Hopelessness Scale (Beck et al., 1974). The Interpersonal Support Evaluation List‐Shortened Version (ISEL‐12; Cohen et al., 1985) measured appraisal support, belonging support, and tangible support. Coping strategies were assessed with the COPE Inventory (Carver et al., 1989), which assesses 15 coping strategies (e.g. active coping, behavioral disengagement, humor). Four emotion regulation skills (cognitive, behavioral, interpersonal, mindfulness) were measured with the Styles of Emotion Regulation Questionnaire (SERQ; Murphy et al., 2020). The big five personality traits of neuroticism, extraversion, openness to experience, conscientiousness, and agreeableness were measured with the NEO‐Five‐Factor Inventory 30‐Item Short Version (NEO‐FFI‐30; Körner et al., 2008). The Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989) assessed sleep quality, and the Trauma History Screen (Carlson et al., 2011) was used to approximate trauma history.
COVID‐19 guideline adherence
We created a 12‐item measure to assess the extent to which participants followed recommendations of the United States Centers for Disease Control and Prevention to slow the spread of COVID‐19. Participants rated their adherence in the past week on a Likert scale ranging from 0 (not at all) to 4 (always).
Data analysis
Preliminary analysis
Data were split into training (70%, n = 840) and test (30%, n = 360) datasets. Using the training dataset, an exploratory factor analysis (EFA) was conducted to determine the factor structure of the COVID‐19 guideline adherence measure. Examination of the scree plot and parallel analysis determined the number of factors to retain. A promax rotation method was used in the event of multiple factors.
Data preprocessing
Predictor variables were screened for near‐zero variance. Categorical predictor variables were dummy coded for analysis. Data had low levels of missingness (all scores <4%). Since elastic net models require complete data, data were imputed using the R package missForest, which is a random forest‐based approach of multiple imputation (Stekhoven, 2013). This approach generates a single set of imputed values by averaging over multiple regression trees. It is a nonparametric method that can handle datasets with multiple types of data and has been shown to outperform some other commonly used imputation methods (Stekhoven & Buhlmann, 2012). Following multiple imputation, numerical predictor variables were standardised (M = 0, SD = 1) in line with elastic net model requirements (Zou & Hastie, 2005). Outcome variables were centered (M = 0) for ease of interpretation. Imputation, standardisation, and centering were performed separately for training and test datasets to preserve data independence. See Methods Supplement (Appendix S1) for more information on variable preprocessing.
Primary analysis
Elastic net regularized regression (Zou & Hastie, 2005) was used to develop models of each of two forms of adherence. Elastic net combines ridge regression and LASSO regression penalties to shrink coefficient estimates and select relevant predictors from a large predictor set. Analyses were conducted in R using the caret (Kuhn, 2020) and glmnet (Friedman et al., 2010) packages. A 10‐fold cross‐validation repeated 100 times was applied to the training dataset to determine the best‐fitting model across a series of hyperparameters (i.e. the alpha and lambda values that corresponded to the lowest root mean squared error (RMSE)). Coefficients were obtained for the best‐fitting model. Coefficient estimates reflect the relationship of each predictor with adherence (with each predictor standardised so that 1 unit reflects 1 SD), while also modeling the effects of the other covariates. Using only the predictor variables identified in the training dataset, the parameters of the best‐fitting model were used to predict test dataset outcomes. Predicted outcome values were compared against the actual values in the test dataset to determine the model's predictive accuracy, as measured by the predicted coefficient of determination (R2 ).
RESULTS
Exploratory factor analysis
The EFA identified a two‐factor solution given evaluation of the scree plot and parallel analysis. The second and third eigenvalues from the observed data were 1.47 and 0.93 compared with 1.15 and 1.11 from the simulated data. Retaining two factors, five items loaded onto the first factor and four items loaded onto the second factor. One item loaded weakly onto the first factor (i.e. standardised regression coefficients less than 0.4; item 5), and two items exhibited low factor loadings and poor simple structure (i.e. loading similarly onto both factors; items 7, 12); therefore, these three items were not included in subsequent analyses. 1 Using the remaining items, two adherence subscale scores were created, which appeared to reflect avoidance and cleaning dimensions of adherence. Item loadings are presented in Table 1 along with subscale descriptive statistics in the full sample. Cronbach's alphas were.82 for the avoidance subscale and.78 for the cleaning subscale.
TABLE 1.
Behavioral health adherence outcome measure
| Avoidance Factor (M = 17.26, SD = 3.35) | Cleaning Factor (M = 12.71, SD = 3.12) | Unloaded Items |
|---|---|---|
| 6. I stay home as much as possible (M = 3.43, SD = 0.84). | 1. I wash my hands often, using soap and water for at least 20 seconds (M = 3.35, SD = 0.93). | 5. I carry out work or school activities from home to the maximum degree possible (M = 3.02, SD = 1.26). |
| 8. I avoid all social gatherings (M = 3.44, SD = 0.89). | 2. After being in public places, I always wash my hands or use hand sanitizer (M = 3.45, SD = 0.87). | 7. I maintain a social distance of 6 feet or more from others (M = 3.33, SD = 0.87). |
| 9. I avoid social gatherings of 10 or more people (M = 3.53, SD = 0.85). | 3. I disinfect commonly used items and surfaces frequently (M = 2.86, SD = 1.17). | 12. I wear a facemask whenever social distancing might be difficult (M = 3.10, SD = 1.24). |
| 10. I avoid eating or drinking at bars, restaurants, and food courts (M = 3.51, SD = 0.90). | 4. I avoid touching my eyes, nose, and mouth whenever I might have had contact with something that could be contaminated (M = 3.04, SD = 1.03). | |
| 11. I do not take discretionary trips (for travel, shopping, or social visits) (M = 3.30, SD = 0.98). |
Participants received the following instructions: “Please indicate to what extent you have practiced the following behaviors in the past week.” Items were rated on a 5‐point Likert scale with the following response options: 0 (not at all), 1 (sometimes), 2 (usually), 3 (most of the time), 4 (always). Avoidance (range 0–20) and cleaning (range 0–16) factors were used in analyses.
Among the full sample, average item‐level response corresponded to a rating of adhering “most of the time” in the past week (item means ranged from 2.86 to 3.53). The avoidance and cleaning subscales were positively correlated (r = .48, p < .0001). Wearing a facemask was equally correlated with avoidance (r = .37, p < .0001) and cleaning (r = .37, p < .0001) subscales.
Model of avoidance adherence
Table 2 provides descriptive statistics for all predictor variables in the full sample. Using the training dataset, a model including 39 of the 64 predictors was selected as the best model for predicting avoidance (hyperparameters: alpha = 0.1, lambda = 0.54). The model corresponded to a RMSE of 2.75 and predicted 31.2% of the variance in the training dataset. Figure 1 presents model predictors ranked by absolute regression coefficient (i.e. absolute value of the beta weights). To highlight predictors with numerically larger standardised coefficients (<−0.25), religious affiliation, greater denial coping, full‐time employment, substance use coping, and being age of 60 or older emerged as predictors of less avoidance adherence. Predictors of greater adherence (with standardised coefficients >0.25) were behavioral emotion regulation skills, agreeableness, mindfulness emotion regulation skills, and Democrat political affiliation. The model explained 31.1% of the variance in outcome in the test dataset.
TABLE 2.
Descriptive statistics (N = 1200)
| Predictor variable | Mean (SD) or N (%) |
|---|---|
| Age | 37.67 (11.50) |
| Sex—male | 720 (60.00%) |
| Sexual minority | 963 (80.25%) |
| Race—white | 897 (74.75%) |
| Hispanic ethnicity | 250 (20.83%) |
| Education | |
| Less than high school | 10 (0.83%) |
| High school or equivalent | 97 (8.08%) |
| Some college/2‐year degree | 265 (22.08%) |
| 4‐year degree | 601 (50.08%) |
| Some graduate school or graduate degree | 227 (18.92%) |
| Religious | 831 (69.25%) |
| Political Party Affiliation (variables were Republican and Democrat) | |
| Republican | 427 (35.58%) |
| Democrat | 524 (43.67%) |
| Independent | 249 (20.75%) |
| Immunocompromised—self | 232 (19.33%) |
| Immunocompromised—other in household | 305 (25.42%) |
| 60 or older—self | 65 (5.42%) |
| 60 or older—other in household | 305 (25.42%) |
| Full‐time employment | 825 (68.75%) |
| Married or living with a partner | 798 (66.50%) |
| Any previous psychological diagnosis | 383 (31.92%) |
| Current mental health treatment | 189 (15.75%) |
| Time spent consuming media (hours/week) | 5.03 (4.15) |
| Number of people spoken to (past week) | 5.46 (3.86) |
| Number of people in household | 1.97 (1.31) |
| Number of children | 1.01 (0.99) |
| Number of types of traumatic events | 2.92 (2.83) |
| Income | |
| <$25,000 | 41 (3.42%) |
| $25,000–$34,999 | 116 (9.67%) |
| $35,000–$49,999 | 217 (18.08%) |
| $50,000–$74,999 | 321 (26.75%) |
| $75,000–$99,999 | 233 (19.42%) |
| $100,000–$149,999 | 142 (11.83%) |
| $150,000 or more | 130 (10.83%) |
| Perceived health status | 3.77 (0.96) |
| Financial strain (FCSS) | 0.22 (2.36) |
| Generalized anxiety (GAD−7) | 8.83 (6.37) |
| Depressive symptoms (QIDS‐SR) | 8.30 (5.45) |
| Health anxiety (HAI) | 16.14 (9.67) |
| Perceived stress (PSS) | 17.51 (7.63) |
| Agency (AHS) | 23.95 (5.58) |
| Planning to accomplish goals (AHS) | 24.38 (4.93) |
| Hopelessness (Hopelessness Scale) | 6.44 (5.38) |
| Appraisal support (ISEL−12) | 11.91 (3.08) |
| Belonging support (ISEL−12) | 11.37 (3.04) |
| Tangible support (ISEL−12) | 11.58 (2.92) |
| Openness (NEO‐FFI−30) | 12.45 (3.50) |
| Conscientiousness (NEO‐FFI−30) | 16.28 (4.05) |
| Extraversion (NEO‐FFI−30) | 13.22 (4.06) |
| Agreeableness (NEO‐FFI−30) | 14.17 (4.37) |
| Neuroticism (NEO‐FFI−30) | 11.35 (5.39) |
| Loneliness (UCLA Loneliness Scale) | 44.71 (13.20) |
| Brooding (RRS) | 11.72 (4.33) |
| Reflection (RRS) | 12.44 (4.24) |
| Behavioral emotion regulation skill (SERQ) | 3.88 (0.62) |
| Cognitive emotion regulation skill (SERQ) | 3.76 (0.59) |
| Interpersonal emotion regulation skill (SERQ) | 3.66 (0.64) |
| Mindfulness emotion regulation skill (SERQ) | 3.96 (0.60) |
| Positive reinterpretation and growth (COPE Inventory) | 12.09 (2.88) |
| Mental disengagement (COPE Inventory) | 10.41 (2.71) |
| Focus on and venting of emotions (COPE Inventory) | 10.22 (3.12) |
| Use of instrumental social support (COPE Inventory) | 11.19 (3.17) |
| Active coping (COPE Inventory) | 12.18 (2.55) |
| Denial coping (COPE Inventory) | 7.99 (3.87) |
| Religious coping (COPE Inventory) | 9.83 (4.56) |
| Humor coping (COPE Inventory) | 10.15 (3.59) |
| Behavioral disengagement (COPE Inventory) | 8.50 (3.70) |
| Restraint coping (COPE Inventory) | 11.07 (2.61) |
| Use of emotional social support (COPE Inventory) | 10.94 (3.39) |
| Substance use coping (COPE Inventory) | 7.94 (4.01) |
| Acceptance coping (COPE Inventory) | 11.91 (2.57) |
| Suppression of competing activities (COPE Inventory) | 11.01 (2.49) |
| Planning coping (COPE Inventory) | 12.45 (2.66) |
| Sleep quality (PSQI) | 7.68 (4.30) |
FIGURE 1.
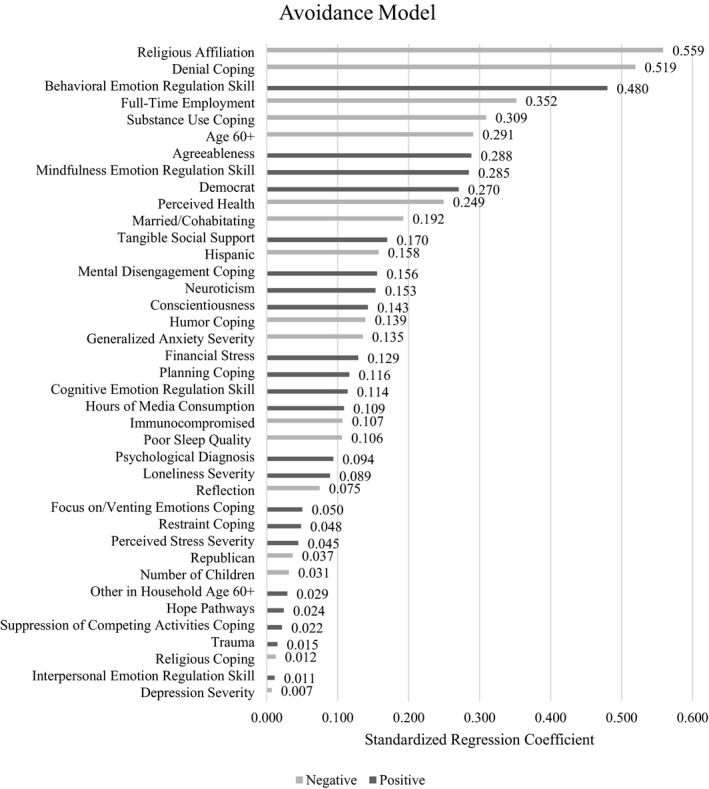
Predictors of Avoidance Adherence. Note. Predictors dropped from the model (i.e. coefficient regularized to zero) not included in figure
Model of cleaning adherence
Again using the training dataset, a model including 28 of the 64 predictors was selected as the best model for predicting cleaning (hyperparameters: alpha = 0.2, lambda = 0.46). The model corresponded to a RMSE of 2.85 and predicted 19.1% of the variance in the training set. Figure 2 presents model predictors ranked by absolute regression coefficient (i.e. absolute value of the beta weights). Predictors of greater cleaning adherence with numerically larger standardised coefficients (>0.25) were as follows: interpersonal emotion regulation skills, behavioral emotion regulation skills, and conscientiousness. Currently receiving mental health treatment predicted lower cleaning adherence. The model explained 15.7% of the variance in outcome for the test dataset.
FIGURE 2.
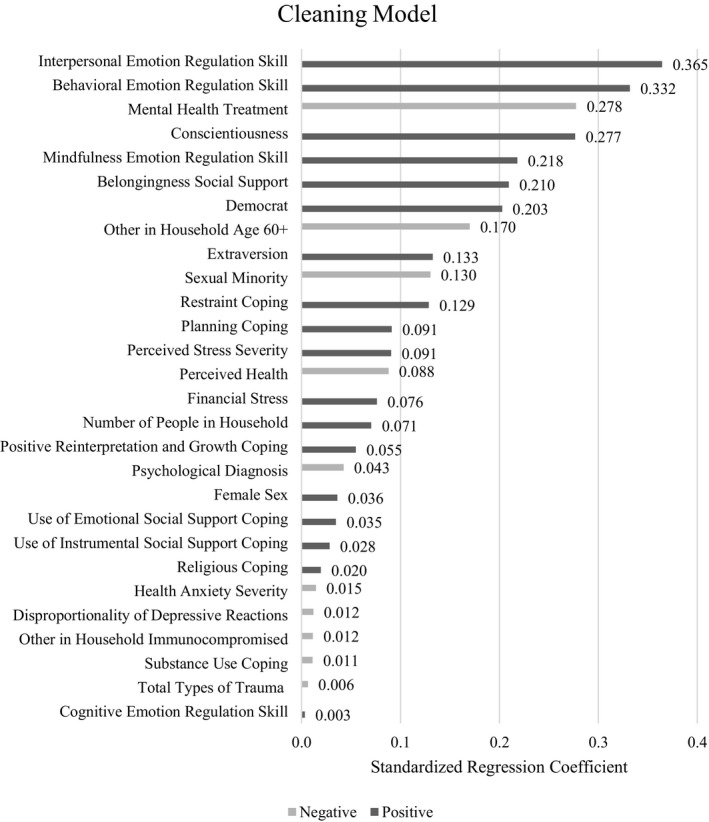
Predictors of Cleaning Adherence. Note. Predictors dropped from the model (i.e. coefficient regularized to zero) not included in figure
DISCUSSION
We were able to predict adherence to behaviors intended to slow the spread of COVID‐19 in the United States using a machine learning approach and elastic net regularized linear regression. Analyses suggested adherence was best characterized by two factors: avoidance and cleaning. These factors align with a recently reported principal component analysis that identified two very similar components of adherence, consisting of social distancing and cleaning behaviors (Solomou & Constantinidou, 2020). In the present study, demographic and psychological characteristics predicted adherence to avoidance behaviors somewhat more strongly than cleaning behaviors, with each model accounting for 31.1% and 15.7% of the variance in the test dataset, respectively. These values are comparable to variance accounted for in a recent study that examined several domains of predictors of COVID‐19 adherence (Raude et al., 2020). The elastic net models also identified substantially different predictors of avoidance and cleaning adherence. Only 16 predictors were included in both the avoidance and cleaning models, and only one predictor with a regression coefficient over 0.25 was common to both models: behavioral emotion regulation skill, which was related to greater adherence in both models. The differential predictive accuracy and differences in the predictors identified provide further evidence of the importance of distinguishing between avoidance and cleaning adherence.
Predictors of avoidance
Among the top predictors of avoidance adherence were denial and substance use coping, which are considered avoidant coping strategies associated with a variety of negative psychological outcomes (Litman, 2006). Those who tend to use denial as a coping strategy may underestimate COVID‐19 risks and therefore more often make social contacts in ways contrary to guidelines. This result appears compatible with studies, which have found a connection between adherence and knowledge about COVID‐19, perceptions of COVID‐19 risk, and belief in the efficacy of public health measures (Al Hasan et al., 2020; de Bruin & Bennett, 2020; Clark et al., 2020). Our finding regarding denial coping may be related to the previously reported association between COVID‐19 skepticism and less engagement in COVID‐19 health behaviors (Latkin et al., 2021). The present study also found that those who tend to use drugs or alcohol when they experience stress reported lower avoidance adherence. Lower adherence among substance users may be due to the social nature of activities such as drinking, which are discordant with avoidance recommendations, lower inhibitions, or emotion regulation difficulties, which contribute to both substance use and reduced adherence behavior. These results align with Chong et al. (2020) who found that avoidance‐based coping was associated with less adherence in Hong Kong.
Next, we turn to demographic characteristics and factors that would place one at risk for serious illness if infected. Participants affiliated with a religion reported less avoidance adherence. It may be that religiously affiliated participants valued attendance at religious services (or other social events) highly enough to take additional risks. Ours is the first study to our knowledge to find a connection between religious affiliation and adherence to COVID‐19 social distancing measures. Future research is needed to explore this connection. Full‐time employment also predicted lower avoidance adherence, perhaps reflecting these participants’ work responsibilities keeping them from distancing more extensively and also leading them to feel more comfortable socializing in other contexts (as most adherence items are not specific to social distancing at work). At least one other study has found that employed individuals were less likely to adhere to avoidance recommendations (Czeisler et al., 2020). We also found that identifying as a Democrat was associated with greater adherence to avoidance behaviors, in line with previous findings (Painter & Qiu, 2021).
More favorable self‐reported health was associated with lower avoidance adherence. This finding is in line with previous research reporting lower adherence behaviors among those who perceived their risk of adverse outcomes related to COVID‐19 to be low (de Bruin & Bennet, 2020; Chong et al., 2020; Clark et al., 2020; Pollak et al., 2020). On the other hand, advanced age is a risk factor for adverse outcomes of COVID‐19. Despite this risk, we found that those aged 60 or older were less likely to adhere to avoidance guidelines than those below age 60. As previously noted, research on adherence across age groups has been quite mixed, though most studies finding a relationship between age and adherence have found relatively higher adherence among the oldest age cohorts (Clark et al., 2020; Czeisler et al., 2020; Latkin et al., 2021; Park et al., 2020; Qeadan et al., 2020; Solomou & Constantinidou, 2020; Steens et al., 2020). Our own visual examination of the unadjusted association between avoidance adherence and age suggested that this adherence appeared to be higher among older participants, but only among those at the higher end of our older age group (i.e. age 68 – 79). Caution with regard to our finding for older age is also warranted because we had representation of older adults (5.4%) that was lower than the minimum recommended (20%; Cohen et al., 2020).
Finally, behavioral and mindfulness skills were identified as predictors of avoidance adherence. The finding for behavioral emotion regulation skills is particularly interesting as this was among the strongest predictors of both avoidance and cleaning adherence. These skills reflect the ability to stay on track with plans, suggesting that the ability to follow through with plans is important to following through with guidelines. Mindfulness, which partly reflects acting with intention and awareness of one's underlying motivations, appears to reflect a complementary skill that aids in compliance. Participants tended to report relatively high levels of use of each of these skills, indicating that they use them “often” on average. Other research groups have found that related constructs such as self‐efficacy (Chong et al., 2020), self‐control (Nivette et al., 2021; Wolff et al., 2020), and perceived behavioral control (Raude et al., 2020) were related to COVID‐19 behavioral health adherence. Finally, consistent with Clark et al. (2020), those who were more agreeable reported greater adherence to avoidance recommendations (though agreeableness was not identified as a predictor of cleaning adherence).
Predictors of cleaning
Compared with avoidance adherence, this model showed more limited prediction of cleaning adherence (predicted R2 = .16), with fewer predictors emerging. Interpersonal and behavioral emotion regulation skills and conscientiousness were the strongest predictors of greater cleaning. Those high in interpersonal skills tend to have strong social connections and actively nurture social relationships. Such participants might be adherent to cleaning procedures to protect others, but be less inclined to adhere in ways that conflict with social connections. The relation between conscientiousness and cleaning is understandable, as trait conscientiousness involves neatness and self‐discipline (Costa et al., 1991). The relation of conscientiousness to avoidance adherence was much weaker.
Prior research has found women to be somewhat more adherent to COVID‐19 guidelines than men. Female sex emerged as a predictor of greater adherence in the cleaning model, but sex was not selected as a predictor of avoidance adherence. A final predictor of cleaning adherence that merits comment is current mental health treatment; those receiving mental health services reported lower cleaning adherence. It is possible that those receiving mental health services were experiencing greater mental health problems that impeded their ability to engage in recommended cleaning behaviors. While few variables assessing psychopathology emerged as important predictors in the cleaning model, those that were selected (e.g. psychological diagnosis, health anxiety) were associated with lower cleaning. No mental health variables emerged as strong predictors in the avoidance model.
Limitations
A few limitations merit comment. First, the adherence outcome variable was based on self‐report. As a result, responses may have been influenced by participants’ desire to respond in a manner they believe to be socially desirable. However, efforts to ensure responses would remain confidential hopefully helped participants respond honestly. Future research is needed to evaluate the psychometric properties of this COVID‐19 adherence measure. Second, categorical predictor variables with small numbers of participants in specific categories were collapsed to ensure sufficient representation in each category (e.g. racial group categories were recoded to white/non‐white). Differences across these groups may merit further evaluation. Third, analyses were based on cross‐sectional data. Furthermore, this investigation focused on predictors of adherence in the early stages of the pandemic in the United States. Both adherence and predictors of adherence may vary over time, a possibility that we plan to investigate with subsequent longitudinal data.
CONCLUSION
Findings of this study suggest two distinct factors underlying adherence to COVID‐19 guidelines: one that reflects limiting or avoiding social contact and one that reflects cleaning activities. Elastic net models identified markedly distinct sets of predictors of these two forms of adherence. However, emotion regulation skills emerged as particularly important predictors of greater adherence in both models. The connection between behavioral control and COVID‐19 adherence has also been identified by other researcher teams (Chong et al., 2020; Raude et al., 2020; Wolff et al., 2020). This is a promising finding because emotion regulation skills can be learned. One of the goals of cognitive behavioral therapy, for example, is to teach emotion regulation skills and help clients implement these skills in their lives. Interventions aimed at promoting emotion regulation skills to improve mental health functioning may also improve adherence to COVID‐19 health behaviors. Interventions that emphasize being action‐oriented and taking concrete steps to plan and follow through with avoidance and cleaning behaviors may promote adherence to COVID‐19 guidelines. Future research on promoting adherence should examine the impact of behavioral skill interventions, such as goal setting, breaking tasks into small steps, behavior tracking, and identifying and addressing implementation barriers.
Other identified predictors provide important clues about the kinds of interventions that might successfully reach those showing low levels of adherence. As denial coping emerged as a top predictor of lower avoidance behaviors, including social distancing, campaigns may benefit from efforts to combat COVID‐19 denial and strategically correct misinformation about the virus and public safety measures (Pennycook et al., 2020). Relevant demographic predictors point to groups, which may be important targets for COVID‐19 adherence interventions. For example, our results raise the possibility that interventions could be geared toward religious communities. Taken together, efforts to promote compliance with COVID‐19 health guidelines may benefit from distinguishing avoidance and cleaning behaviors. Demographic and psychological predictors of each of these aspects of adherence may inform how and for whom targeted intervention strategies be implemented. Future research is needed to experimentally test interventions to promote COVID‐19 adherence that are informed by the relationships identified in naturalistic studies.
CONFLICT OF INTEREST
No conflict of interest has been declared by the authors.
ETHICAL APPROVAL
Study procedures were approved by an institutional review board at the Ohio State University. Participants provided informed consent.
Supporting information
Supinfo
Bailey B, Whelen ML, Strunk DR. Adhering to COVID‐19 health guidelines: Examining demographic and psychological predictors of adherence. Appl Psychol Health Well‐Being. 2021;13:968–985. 10.1111/aphw.12284
ENDNOTE
An additional EFA was conducted to explore whether results based on the training dataset (n = 840) would hold when using the full sample (n = 1200). Findings remained the same.
Contributor Information
Brooklynn Bailey, Email: bailey.1451@osu.edu.
Daniel R. Strunk, Email: strunk.20@osu.edu.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Aguinis, H. , Villamor, I. , & Ramani, R. S. (2020). MTurk research: Review and recommendations. Journal of Management, 47(4), 823–837. https://doi.org/10.1177%2F0149206320969787 [Google Scholar]
- Al‐Hasan, A. , Yim, D. , & Khuntia, J. (2020). Citizens’ adherence to COVID‐19 mitigation recommendations by the government: A 3‐country comparative evaluation using web‐based cross‐sectional survey data. Journal of Medical Internet Research, 22(8), e20634. 10.1016/j.jiph.2020.05.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alloy, L. B. , & Riskind, J. H. (2006). Cognitive vulnerability to emotional disorders. Routledge. [Google Scholar]
- Beck, A. T. , Weissman, A. , Lester, D. , & Trexler, L. (1974). The measurement of pessimism: The hopelessness scale. Journal of Consulting and Clinical Psychology, 42, 861–865. 10.1037/h0037562 [DOI] [PubMed] [Google Scholar]
- Buysse, D. J. , Reynolds, C. F. 3rd , Monk, T. H. , Berman, S. R. , & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28, 193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- Carlson, E. B. , Smith, S. R. , Palmieri, P. A. , Dalenberg, C. , Ruzek, J. I. , Kimerling, R. , Burling, T. A. , & Spain, D. A. (2011). Development and validation of a brief self‐report measure of trauma exposure: The Trauma History Screen. Psychological Assessment, 23, 463–477. 10.1037/a0022294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver, C. S. , Scheier, M. F. , & Weintraub, J. K. (1989). Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology, 56, 267–283. 10.1037/0022-3514.56.2.267 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2020). How to protect yourself and others. Retrieved November 2, 2020, from https://www.cdc.gov/coronavirus/2019‐ncov/prevent‐getting‐sick/prevention.html [Google Scholar]
- Centers for Disease Control and Prevention . (2021). Coronavirus disease 2019 (COVID‐19) in the U.S. Retrieved March 19 2021, from https://covid.cdc.gov/covid‐data‐tracker [Google Scholar]
- Chavez, N. , Andone, D. , & Maxouris, C. (2020). CDC recommends Americans wear face masks voluntarily in public but some officials say they felt “pressured” to draft new guidelines. CNN. https://www.cnn.com/2020/04/03/health/us‐coronavirus‐friday/index.html [Google Scholar]
- Chong, Y. Y. , Chien, W. T. , Cheng, H. Y. , Chow, K. M. , Kassianos, A. P. , Karekla, M. , & Gloster, A. (2020). The role of illness perceptions, coping, and self‐efficacy on adherence to precautionary measures for COVID‐19. International Journal of Environmental Research and Public Health, 17, 6540. 10.3390/ijerph17186540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark, C. , Davila, A. , Regis, M. , & Kraus, S. (2020). Predictors of COVID‐19 voluntary compliance behaviors: An international investigation. Global Transitions, 2, 76–82. 10.1016/j.glt.2020.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, S. , Kamarck, T. , & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Cohen, S. , Mermelstein, R. , Kamarck, T. , & Hoberman, H. M. (1985). Measuring the functional components of social support. In Sarason I. G. & Sarason B. R. (Eds.), Social support: Theory, research and applications (pp. 73–94). Martinus Nijhoff Publishers. [Google Scholar]
- Cohen, Z. D. , Kim, T. T. , Van, H. L. , Dekker, J. J. , & Driessen, E. (2020). A demonstration of a multi‐method variable selection approach for treatment selection: Recommending cognitive–behavioral versus psychodynamic therapy for mild to moderate adult depression. Psychotherapy Research, 30, 137–150. 10.1080/10503307.2018.1563312 [DOI] [PubMed] [Google Scholar]
- Costa, P. T. Jr , McCrae, R. R. , & Dye, D. A. (1991). Facet scales for agreeableness and conscientiousness: A revision of the NEO Personality Inventory. Personality and Individual Differences, 12, 887–898. 10.1016/0191-8869(91)90177-D [DOI] [Google Scholar]
- Cucinotta, D. , & Vanelli, M. (2020). WHO declares COVID‐19 a pandemic. Acta bio‐medica: Atenei Parmensis, 91, 157–160. 10.23750/abm.v91i1.9397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czeisler, M. É. , Tynan, M. A. , Howard, M. E. , Honeycutt, S. , Fulmer, E. B. , Kidder, D. P. , Robbins, R. , Barger, L. K. , Facer‐Childs, E. R. , Baldwin, G. , Rajaratnam, S. M. W. , & Czeisler, C. A. (2020). Public attitudes, behaviors, and beliefs related to covid‐19, stay‐at‐home orders, nonessential business closures, and public health guidance ‐ United States, New York City, and Los Angeles, May 5–12, 2020. Morbidity and Mortality Weekly Report, 69, 751–758. 10.15585/mmwr.mm6924e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bruin, W. B. , & Bennett, D. (2020). Relationships between initial COVID‐19 risk perceptions and protective health behaviors: A national survey. American Journal of Preventive Medicine, 59, 157–167. 10.1016/j.amepre.2020.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman, H. S. (Ed.) (2011). The Oxford handbook of health psychology. Oxford University. [Google Scholar]
- Friedman, J. , Hastie, T. , & Tibshirani, R. (2010). Regularization paths for generalized linear models via coordinate descent. Journal of Statistical Software, 33, 1–22. 10.18637/jss.v033.i01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross, J. J. , & Thompson, R. A. (2007). Emotion regulation: Conceptual foundations. In Gross J. J. (Ed.), Handbook of emotion regulation (pp. 3–24). [Google Scholar]
- Hopko, D. R. , Mclndoo, C. C. , & File, A. A. (2017). Depressive syndromes and medical comorbidities. In DeRubeis R. J. & Strunk D. R. (Eds.), The oxford handbook of mood disorders. Oxford University. 10.1093/oxfordhb/9780199973965.013.30 [DOI] [Google Scholar]
- Katon, W. , & Ciechanowski, P. (2002). Impact of major depression on chronic medical illness. Journal of Psychosomatic Research, 53(4), 859–863. 10.1016/S0022-3999(02)00313-6 [DOI] [PubMed] [Google Scholar]
- Kirzinger, A. , Kearney, A. , Hamel, L. , & Brodie, M. (2020). KFF health tracking poll‐early April 2020: The impact of coronavirus on life in America. The Henry J. Kaiser Family Foundation. [Google Scholar]
- Körner, A. , Geyer, M. , Roth, M. , Drapeau, M. , Schmutzer, G. , Albani, C. , & Brähler, E. (2008). Personality assessment with the NEO‐five‐factor inventory: the 30‐item‐short‐version (NEO‐FFI‐30). Psychotherapie, Psychosomatik, Medizinische Psychologie, 58, 238–245. 10.1055/s-2007-986199 [DOI] [PubMed] [Google Scholar]
- Kuhn, M. (2020). caret: Classification and Regression Training. R package version 6.0‐86.
- Lantz, P. M. , House, J. S. , Mero, R. P. , & Williams, D. R. (2005). Stress, life events, and socioeconomic disparities in health: Results from the Americans’ Changing Lives Study. Journal of Health and Social Behavior, 46, 274–288. 10.1177/002214650504600305 [DOI] [PubMed] [Google Scholar]
- Latkin, C. A. , Dayton, L. , Moran, M. , Strickland, J. C. , & Collins, K. (2021). Behavioral and psychosocial factors associated with COVID‐19 skepticism in the United States. Current Psychology, 1–9. 10.1007/s12144-020-01211-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litman, J. A. (2006). The COPE inventory: Dimensionality and relationships with approach‐and avoidance‐motives and positive and negative traits. Personality and Individual Differences, 41, 273–284. 10.1016/j.paid.2005.11.032 [DOI] [Google Scholar]
- Moreland, A. , Herlihy, C. , Tynan, M. A. , Sunshine, G. , McCord, R. F. , Hilton, C. , Poovey, J. , Werner, A. K. , Jones, C. D. , Fulmer, E. B. , Gundlapalli, A. V. , Strosnider, H. , Potvien, A. , García, M. C. , Honeycutt, S. , Baldwin, G. , Clodfelter, C. , Howard‐Williams, M. , Jeong, G. I. , … Popoola, A. (2020). Timing of state and territorial COVID‐19 stay‐at‐home orders and changes in population movement—United States, March 1–May 31, 2020. Morbidity and Mortality Weekly Report, 69(35), 1198–1203. 10.15585/mmwr.mm6935a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy, S. T. , Cheavens, J. S. , & Strunk, D. R. (2020). Overcoming a poor early response with cognitive behavioral therapy skills. Cognitive Therapy and Research, 44, 1177–1185. 10.1007/s10608-020-10140-1 [DOI] [Google Scholar]
- Nivette, A. , Ribeaud, D. , Murray, A. , Steinhoff, A. , Bechtiger, L. , Hepp, U. , Shanahan, L. , & Eisner, M. (2021). Non‐compliance with COVID‐19‐related public health measures among young adults in Switzerland: Insights from a longitudinal cohort study. Social Science & Medicine, 268, 10.1016/j.socscimed.2020.113370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Painter, M. , & Qiu, T. (2021). Political beliefs affect compliance with government mandates. Journal of Economic Behavior & Organization, 185, 688–701. 10.2139/ssrn.3569098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, C. L. , Russell, B. S. , Fendrich, M. , Finkelstein‐Fox, L. , Hutchison, M. , & Becker, J. (2020). Americans’ COVID‐19 stress, coping, and adherence to CDC guidelines. Journal of General Internal Medicine, 35, 2296–2303. 10.1007/s11606-020-05898-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennycook, G. , McPhetres, J. , Zhang, Y. , Lu, J. G. , & Rand, D. G. (2020). Fighting COVID‐19 misinformation on social media: Experimental evidence for a scalable accuracy‐nudge intervention. Psychological Science, 31, 770–780. 10.1177/0956797620939054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeifer, B. J. , & Strunk, D. R. (2021). Assessing the disproportionality of depressive reactions to life stress [Manuscript submitted for publication]. Department of Psychology, The Ohio State University. [DOI] [PubMed] [Google Scholar]
- Pollak, Y. , Dayan, H. , Shoham, R. , & Berger, I. (2020). Predictors of non‐adherence to public health instructions during the COVID‐19 pandemic. Psychiatry and Clinical Neurosciences, 11, 602–604. 10.1111/pcn.13122 [DOI] [PubMed] [Google Scholar]
- Qeadan, F. , Akofua Mensah, N. , Tingey, B. , Bern, R. , Rees, T. , Talboys, S. , Singh, T. P. , Lacey, S. , & Shoaf, K. (2020). What protective health measures are Americans taking in response to COVID‐19? Results from the COVID Impact Survey. International Journal of Environmental Research and Public Health, 17(17), 6295. 10.3390/ijerph17176295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raude, J. , Lecrique, J. M. , Lasbeur, L. , Leon, C. , Guignard, R. , Roscoät, E. D. , & Arwidson, P. (2020). Determinants of preventive behaviors in response to the COVID‐19 pandemic in France: Comparing the sociocultural, psychosocial and social cognitive explanations. Frontiers in Psychology, 11, 584500. 10.3389/fpsyg.2020.584500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush, A. J. , Trivedi, M. H. , Ibrahim, H. M. , Carmody, T. J. , Arnow, B. , Klein, D. N. , Markowitz, J. C. , Ninan, P. T. , Kornstein, S. , Manber, R. , Thase, M. , Kocsis, J. H. , & Keller, M. B. (2003). The 16‐item Quick Inventory of Depressive Symptomatology (QIDS) Clinician Rating (QIDS‐C) and Self‐Report (QIDS‐SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54, 573–583. 10.1016/S0006-3223(02)01866-8 [DOI] [PubMed] [Google Scholar]
- Russell, D. (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment, 66, 20–40. 10.1207/s15327752jpa6601_2 [DOI] [PubMed] [Google Scholar]
- Salkovskis, P. M. , Rimes, K. A. , Warwick, H. M. C. , & Clark, D. M. (2002). The Health Anxiety Inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine, 32, 843–853. 10.1017/s0033291702005822 [DOI] [PubMed] [Google Scholar]
- Snyder, C. R. , Harris, C. , Anderson, J. R. , Holleran, S. A. , Irving, L. M. , Sigmon, S. T. , Yoshinobu, L. , Gibb, J. , Langelle, C. , & Harney, P. (1991). The will and the ways: development and validation of an individual‐differences measure of hope. Journal of Personality and Social Psychology, 60, 570–585. 10.1037/0022-3514.60.4.570 [DOI] [PubMed] [Google Scholar]
- Solomou, I. , & Constantinidou, F. (2020). Prevalence and predictors of anxiety and depression symptoms during the COVID‐19 pandemic and compliance with precautionary measures: Age and sex matter. International Journal of Environmental Research and Public Health, 17(14), 4924. 10.3390/ijerph17144924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer, R. L. , Kroenke, K. , Williams, J. B. W. , & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD‐7. Archives of Internal Medicine, 166, 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Steens, A. , De Blasio, B. F. , Veneti, L. , Gimma, A. , Edmunds, W. J. , Van Zandvoort, K. , Jarvis, C. I. , Forland, F. , & Robberstad, B. (2020). Poor self‐reported adherence to COVID‐19‐related quarantine/isolation requests, Norway, April to July 2020. Eurosurveillance, 25(37), 2001607. 10.2807/1560-7917.ES.2020.25.37.2001607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stekhoven, D. J. (2013). missForest: Nonparametric Missing Value Imputation using Random Forest. R package version 1.4.
- Stekhoven, D. J. , & Bühlmann, P. (2012). MissForest—non‐parametric missing value imputation for mixed‐type data. Bioinformatics, 28, 112–118. 10.1093/bioinformatics/btr597 [DOI] [PubMed] [Google Scholar]
- Treynor, W. , Gonzalez, R. , & Nolen‐Hoeksema, S. (2003). Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research, 27, 247–259. 10.1023/A:1023910315561 [DOI] [Google Scholar]
- Wolff, W. , Martarelli, C. S. , Schüler, J. , & Bieleke, M. (2020). High boredom proneness and low trait self‐control impair adherence to social distancing guidelines during the COVID‐19 pandemic. International Journal of Environmental Research and Public Health, 17, 5420. 10.3390/ijerph17155420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou, H. , & Hastie, T. (2005). Regularization and variable selection via the elastic net. Journal of the Royal Statistical Society: Series B (Statistical Methodology), 67, 301–320. 10.1111/j.1467-9868.2005.00503 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supinfo
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


