Abstract
BACKGROUND
New York City (NYC) emerged as an epicenter of the COVID‐19 pandemic, and marginalized populations were affected at disproportionate rates. The authors sought to determine the impact of COVID‐19 on cancer treatment, anxiety, and financial distress among low‐income patients with gynecologic cancer during the peak of the NYC pandemic.
METHODS
Medicaid‐insured women who were receiving gynecologic oncology care at 2 affiliated centers were contacted by telephone interviews between March 15 and April 15, 2020. Demographics and clinical characteristics were obtained through self‐report and retrospective chart review. Financial toxicity, anxiety, and cancer worry were assessed using modified, validated surveys.
RESULTS
In total, 100 patients completed the telephone interview. The median age was 60 years (range, 19‐86 years), and 71% had an annual income <$40,000. A change in employment status and early stage cancer (stage I and II) were associated with an increase in financial distress (P < .001 and P = .008, respectively). Early stage cancer and telehealth participation were significantly associated with increased worry about future finances (P = .017 and P = .04, respectively). Lower annual income (<$40,000) was associated with increased cancer worry and anxiety compared with higher annual income (>$40,000; P = .036 and P = .017, respectively). When controlling for telehealth participation, income, primary language, and residence in a high COVID‐19 prevalence area, a delay in medical care resulted in a 4‐fold increased rate of anxiety (P = .023, 95% CI, 1.278‐14.50). Race was not significantly associated with increased financial distress, cancer worry, or anxiety.
CONCLUSIONS
Low socioeconomic status was the most common risk factor for increased financial distress, cancer worry, and anxiety. Interventions aimed at improving access to timely oncology care should be implemented during this ongoing pandemic.
Keywords: anxiety, cancer worry, financial toxicity, gynecologic oncology, health care disparity, Medicaid, mental health
Short abstract
Low socioeconomic status is the most common risk factor for increased financial distress, cancer worry, and anxiety among patients with Medicaid who are receiving gynecologic oncologic care during the coronavirus disease 2019 (COVID‐19) pandemic. Interventions aimed to improving access to timely oncology care for this population should be implemented during this ongoing pandemic.
Introduction
COVID‐19 spread rapidly to become a global pandemic, drastically transforming health care delivery. 1 Within the United States, New York City (NYC) emerged as an early epicenter of the pandemic. By April 2020, NYC had the highest number of COVID‐19 cases and deaths nationwide. 2 Data suggest that the pandemic has disproportionately affected many minority and marginalized populations throughout the United States. 3 , 4 , 5 , 6 , 7 NYC infection rates demonstrate that Hispanics and Blacks are twice as likely to die of COVID‐19 compared with Whites. 8 Preexisting disparities exist across gynecologic malignancies based on race, socioeconomic status, implicit and explicit biases, education, and biology. In the setting of the pandemic, inequities may further exacerbate both cancer morbidity and cancer mortality. 8
Studies suggest that patients with cancer may have increased COVID‐19 infection rates and COVID‐19–associated morbidity. 9 , 10 However, few studies have addressed socioeconomic status, financial burden, and mental health in this population. 11 , 12 Among patients with cancer, financial distress is common because of long‐term health expenses related to surgery, treatment, surveillance, and hospitalizations. 11 , 12 , 13 Financial distress subsequently can affect compliance with follow‐up during cancer care. 11 , 12 , 13 , 14 Circumstances related to job loss and the risk of COVID‐19 exposure as an essential worker may further exacerbate these concerns and affect cancer care. 8
To continue to safely care for oncology patients while still flattening the curve, national organizations have published guidelines on adapting oncology care to address the risks and benefits of time‐sensitive cancer treatments. 15 , 16 , 17 However, many underserved populations may face significant barriers to adhering to these guidelines. 8 , 13 We sought to determine the impact of COVID‐19 on cancer treatment, anxiety and financial distress among Medicaid‐insured (low‐income) gynecologic oncology patients receiving care at 2 affiliated medical centers during the peak of the pandemic in NYC.
Materials and Methods
A pilot descriptive survey with the intent of hypothesis generation was developed and used for telephone interviews during the peak of the COVID‐19 pandemic in NYC. This study was approved by the Institutional Review Board at 2 affiliated gynecologic oncology centers in NYC: an 862‐bed academic tertiary care and referral center in Manhattan and a 651‐bed community‐based tertiary care hospital in Brooklyn. Women were included if they had active Medicaid insurance; a diagnosis of gynecologic precancer, cancer, or cancer‐associated genetic mutation; and were treated by a gynecologic oncologist and/or radiation oncologist at 1 of the participating hospitals between April 1, 2019 and April 1, 2020. Patients were identified based on clinic schedules at each participating site between April 1, 2019 and April 1, 2020. Patients who died before March 15, 2020 were excluded from the study. In total, 158 eligible patients (n = 103, Manhattan site; n = 55, Brooklyn site) were contacted for a telephone interview between March 15, 2020 and April 15, 2020, and 100 responses were obtained (n = 76, Manhattan site; n = 24, Brooklyn site). Of the 58 patients who did not complete the survey, 14 declined, 1 had recently died, and 43 (n = 13, Manhattan site; n = 30, Brooklyn site) did not answer after ≥2 contact attempts.
Telephone interviews were conducted by clinicians and research personnel using a standardized script with a total of 50 questions. Patients self‐reported demographic characteristics, including age, race/ethnicity, level of education, living location by zip code, marital status, number of children, number of roommates per household, and primary language. Patients were asked questions related to their current cancer treatment plan, delays in cancer‐related appointments and treatments, participation in and preferences for telemedicine, COVID‐19 symptoms, hospitalization because of COVID‐19, and access to testing for COVID‐19. Retrospective chart review was used to confirm clinical characteristics, including age, comorbidities, COVID‐19 status/testing, cancer diagnosis, cancer stage, cancer‐related appointments, treatments, delays, and use of telemedicine. Access to telehealth visits differed across sites, with the Manhattan site having access to video and telephone and the Brooklyn site with telephone only.
To screen for a broad range of outcomes, select questions from validated surveys were used to screen for financial toxicity, cancer worry, and anxiety in a brief telephone interview. Financial toxicity was assessed using a modified comprehensive score for financial toxicity (COST) patient‐reported outcome measure (PROM) survey that has been previously validated to assess financial toxicity in patients with cancer. 12 Four questions with the highest factor loading (ie, questions most significantly associated with outcomes) were selected from the 11‐point COST‐PROM tool and used in our survey instrument to be used as a screen for financial toxicity. 12 Patients were asked, “Do you feel financially stressed? Has COVID‐19 reduced your satisfaction with your current financial situation? Do you worry about future financial problems you may have as a result of COVID‐19? Are you frustrated that you cannot work or contribute as much as you normally do?” In addition, patients were asked about income level, employment status (pre–COVID‐19 and current), and levels of anxiety. Anxiety related to cancer diagnosis and generalized anxiety in the setting of the COVID‐19 pandemic were assessed using select questions from validated screening tools from the Cancer Worry Scale (CWS) 18 and the Generalized Anxiety Disorder‐7 (GAD‐7) survey. 19 , 20 The questions selected were framed to ask whether cancer worry and anxiety had increased since the start of the pandemic. To screen for cancer worry, 2 questions with high factor loading were selected from the 8‐question CWS. Patients were asked, “Do you feel that your cancer worry has increased since the pandemic started?” and “Do you worry about your cancer coming back?” A singular screening question for increased anxiety (“Over the past 2 weeks, how often have you felt more nervous, anxious, or on edge?”) was used to assess the need for further screening for anxiety by prompting completion of the full GAD‐7 survey. All patients were encouraged to complete the full GAD‐7 survey questions regardless of this initial screen because this single question has not been independently validated. Age was dichotomized based on existing data demonstrating that patients aged >65 years face greater morbidity in the setting of COVID‐19. 10 , 21 Comorbidities associated with increased COVID‐19 disease severity were documented (hypertension, obesity, chronic lung disease [including asthma], chronic obstructive pulmonary disease, and diabetes). 21
Statistical Analysis
Descriptive statistics were calculated using the numbers and percentages of patients for categorical variables and medians (ranges) for continuous variables. The distribution of continuous variables was tested for normality using the Shapiro‐Wilk normality test. Univariate tests were applied based on whether the variable of interest was distributed normally (ie, t test, analysis of variance) or not normally (ie, Mann‐Whitney U test, Kruskal‐Wallace test). Associations between categorical variables were evaluated using the χ2 test or the Fisher exact test, as appropriate, for category size. Self‐reported financial stress and worry about future financial problems were treated as binary variables based on the COST‐PROM tool and defined as yes or no responses to the questions, “Do you feel financially stressed?” and “Do you worry about future financial problems?” in the setting of the COVID‐19 pandemic. 12 Cancer worry and general anxiety responses were recorded based on a Likert scale as 0 (not at all), 1 (a little bit), 2 (somewhat), or 3 (very much). To facilitate the analysis because of the small sample size across responses, the decision was made to dichotomize findings into binary categories, in which the answers a little bit, somewhat, and very much were coded as increased worry/anxiety, and the answer not at all was coded as no increase in worry/anxiety.
Multivariable logistic regression analysis was explored to evaluate the independent effect of demographic and clinical variables of interest on financial toxicity and anxiety during the study period (ie, separate models for financial distress and anxiety). Anxiety was defined as a binary variable based on a screening question for increased anxiety (“Over the past 2 weeks, how often have you felt more nervous, anxious, or on edge?”), with the answer not at all (categorized as no and the answers a little bit, somewhat, and very much categorized as increased anxiety. 22 Financial distress was treated as a binary variable defined as yes or no responses to the question “Do you feel financially stressed?” Collinearity between predictors in the models was evaluated before formulation of the final multivariable models. Statistical significance was evaluated at the .05 α level, and 95% CIs were calculated to assess the precision of all obtained estimates. Because of the small sample size in this pilot study, all results are considered hypothesis‐generating and for exploratory purposes. Given the exploratory nature of the study, P values were not corrected for multiple comparisons or multiplicity of outcomes. Data were analyzed using the SPSS statistical software package (IBM SPSS Statistics for Windows, version 25.0; IBM Corporation) and R (version 3.6.1; R Foundation for Statistical Computing).
Results
All patients who met the inclusion criteria (N = 158) were contacted for the telephone interview and 100 (63%) completed the interview. A health care proxy completed the interview for 4 patients. An interpreter was used to conduct 13 interviews in the patient's primary language. Fifty‐eight patients did not complete the survey (14 declined, 1 had recently died, and 43 did not answer after 2 contact attempts). Seventy‐six patient responses were obtained from the Manhattan site, and 24 were obtained from the Brooklyn site. The patient residences of the Manhattan site were diverse, with 21 (27%) residing in Manhattan, 16 (21%) residing in Brooklyn, 19 (25%) residing in Queens, 13 (17%) residing in the Bronx, 6 (8%) residing in the greater NYC area (Westchester, Suffolk County, Orange County NJ, upstate NY), and 1 (1%) residing in Staten Island. Twenty patients at the Brooklyn site lived primarily in Brooklyn (83%), 2 lived in Queens (8%), 1 lived in Manhattan (4%), and 1 lived in Staten Island (4%).
Demographic characteristics are reported in Table 1. The median patient age was 60 years (range, 19‐86 years). The most common primary languages were English (71%) and Spanish (13%). Self‐identified race included African American (36%), Hispanic (23%), non‐Hispanic White (17%), Asian (14%), and other (8%); 3 patients declined to answer. The majority of patients (71%) had an annual income <$40,000. Most patients reported completing some education: 28% completed grade school or some high school, 25% completed high school or obtained a General Equivalency Diploma, 23% completed some college or an associate degree, and 20% completed college or a graduate degree. Self‐reported marital status included single (39%), married (33%), divorced or separated (15%), in a relationship (4%), or widowed (9%). Sixty‐eight percent of patients had children, and 75% were living with others. Sixty‐nine percent of patients had at least 1 medical comorbidity, including hypertension (37.9%), obesity (17.9%), diabetes (14.5%), and chronic lung disease (8.3%). Most patients (94%) reported living in NYC and in areas with a high prevalence of COVID‐19 (74.4%) (Fig. 1).
TABLE 1.
Clinical and Demographic Characteristics of the Study Population
| Characteristic | No. of Patients (%) |
|---|---|
| Study Population, N = 100 | |
| Age: Median [range], y | 60 [19‐86] |
| <65 | 69 (69.0) |
| ≥65 | 31 (31.0) |
| Primary language | |
| English | 71 (71.0) |
| Spanish | 13 (13.0) |
| Cantonese/Mandarin/Korean | 7 (7.0) |
| Other | 9 (9.0) |
| Race a | |
| African American | 35 (36.1) |
| Asian | 14 (14.4) |
| Hispanic | 23 (23.7) |
| Non‐Hispanic White | 17 (17.5) |
| Other, including Native Hawaiian/Pacific Islander | 8 (8.3) |
| Income a | |
| <$21,000 | 36 (36.0) |
| $21,000‐$40,000 | 35 (35.0) |
| >$40,000 | 14 (14.0) |
| Education level a | |
| ≤GED or equivalent | 53 (53.0) |
| >GED or equivalent | 43 (43.0) |
| Marital status | |
| Single | 39 (39.0) |
| Married/in a relationship | 37 (37.0) |
| Divorced/separated | 15 (15.0) |
| Widowed | 9 (9.0) |
| Children | |
| Yes | 68 (68.0) |
| No | 32 (32.0) |
| Average no. of roommates per household [range] | 1.43 [0‐5] |
| Lives with others | 75 (75.0) |
| Lives alone | 25 (25.0) |
| Comorbidities b | |
| None | 31 (21.4) |
| Hypertension | 55 (37.9) |
| Obesity | 26 (17.9) |
| Chronic lung disease | 12 (8.3) |
| Diabetes | 21 (14.5) |
Abbreviation: GED, General Equivalency Diploma.
This variable indicates the subset of individuals who declined to respond to the question (race, n = 3; income, n = 15; education level, n = 4).
Patients who had more than 1 comorbidity were counted for each condition.
Figure 1.
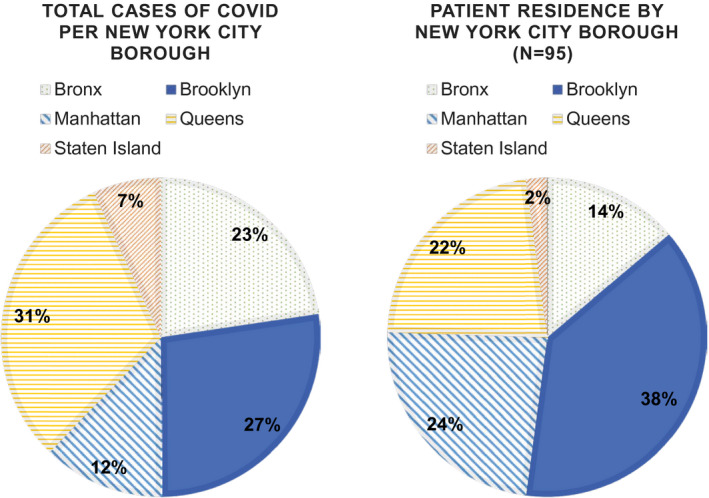
Residence of the patient population during the coronavirus disease 2019 (COVID‐19) pandemic is illustrated as of April 15, 2020. The illustrated population was limited to patients living in New York City boroughs. Only 5 patients resided in New York counties outside of the city.
The cancer characteristics among our cohort are reported in Table 2. Cancer types of participants included uterine (47%), ovary/peritoneum/fallopian tube (22%), cervix (15%), and vulva/vagina (9%). Two percent of patients had metastatic cancer from a nongynecologic primary, and 9% were undergoing treatment or surgery for a cancer‐associated genetic mutation (Table 2). Among the patients who had cancer, 48% had early stage (I or II) cancer, and 32% had late stage (III or IV) cancer. Thirty‐six percent of patients were in active oncologic treatment. Active treatments included chemotherapy (10%), radiation therapy (7%), surgery (9%), targeted therapy with a PARP inhibitor or immunotherapy (9%), and other hormone and topical therapy (12%).
TABLE 2.
Cancer Treatment During Coronavirus Disease 2019 for Underserved Patients
| Characteristic | Study Population: No. of Patients (%) |
|---|---|
| Cancer type a | |
| Ovarian/peritoneal/Mullerian | 22 (21.2) |
| Uterine | 47 (45.2) |
| Cervical | 15 (14.4) |
| Vulvar/vaginal | 9 (8.7) |
| Other | 11 (10.6) |
| Stage | |
| Early: I‐II | 48 (40.0) |
| Late: III‐IV | 32 (32.0) |
| Precancerous | 20 (20.0) |
| Active disease during the time of COVID‐19 | |
| Yes | 36 (36.0) |
| No | 64 (64.0) |
| Type of treatment during COVID‐19 b | |
| Chemotherapy | 10 (16.7) |
| Radiation | 7 (11.7) |
| Surgery | 9 (15.0) |
| Targeted therapy: PARP inhibitor, immunotherapy | 9 (15.0) |
| Other | 12 (20.0) |
| Treatment delay | 13 (21.7) |
| Treatment delay by type | |
| Chemotherapy | 3 (23.1) |
| Radiation | 1 (7.7) |
| Surgery | 9 (69.2) |
| Self‐reported reason for delay | |
| Patient preference | 1 (7.1) |
| Medical team decision | 13 (92.8) |
| Appointment delay | |
| Oncology clinic | 36 (53.7) |
| Imaging | 15 (22.4) |
| Bloodwork | 16 (23.9) |
| Patients tested for COVID‐19 | |
| Positive | 3 (42.9) |
| Negative | 4 (57.1) |
| Reason for COVID‐19 test | |
| Symptomatic | 1 (14.3) |
| Asymptomatic/hospital admission | 6 (85.7) |
| Know someone with COVID‐19 c | |
| Yes | 20 (47.6) |
| No | 22 (52.4) |
| Know someone who died from COVID‐19 c | |
| Yes | 9 (21.4) |
| No | 33 (78.6) |
Abbreviation: COVID‐19, coronavirus disease 2019.
Patients who had 2 primary gynecologic cancers were counted for each individual cancer.
Several patients received more than 1 form of therapy simultaneously.
The denominator was N = 42 for this variable.
Of those who were receiving treatment at the time of the pandemic, 16 patients self‐reported treatment delays, and 13 patients had a documented delay, including: 9 surgery delays, 3 chemotherapy delays, and 1 radiation delay. Among the patients who had documented delays, 93% reported that the decision to delay treatment was made by the medical team, and 7% reported that the delay was because of patient preference. By the end of the study period (April 15, 2020), only 2 of 13 patients (15%) had been rescheduled for treatment. Appointment delays among all patients included oncology clinic appointments (36%), imaging appointments (15%), and bloodwork (16%). Seven patients were tested for COVID‐19 at the time of interview completion. Of these 7 tested patients, 3 (42.8%) tested positive and 4 (57.1%) tested negative; however, these finding may have been skewed by the small sample size of only 7 patients who were tested for COVID‐19. Of 42 patients who were asked the questions, “Do you know someone with COVID‐19?” and “Do you know someone who died from COVID‐19?,” 48% knew someone with COVID‐19, and 21% knew someone who had died from COVID‐19.
Thirty‐five percent of patients used telehealth visits (19 telephone visits, 14 video visits, and 2 visits using both telephone and video). Seventy‐two percent of patients expressed interest in using telehealth platforms to receive care: 26% expressed interest in telephone visits only, 14% expressed interest in video visits, and 60% expressed interest in both methods.
Before the start of the pandemic, 31% patients reported being employed. Twenty‐one percent had a change in employment status because of the pandemic. When screened for financial toxicity, 50% of patients reported that they felt more financial stress since the start of the pandemic, and 54% reported that they worry about future financial problems because of the pandemic. Forty‐nine percent of patients expressed increased anxiety about cancer since the start of the pandemic, and 83% expressed feeling increased generalized anxiety. Of the 77% of patients who completed the GAD‐7, 39% had minimal symptom severity (GAD score, <5), 42% had mild symptom severity (GAD score, 5‐9), 17% had moderate symptom severity (GAD score, 10‐14), and 3% had severe symptoms (GAD score, >15). Twenty percent of patients reported access to a therapist or psychiatrist. Among the 71 patients without access to a therapist or psychiatrist, 20% expressed interest in seeing a mental health professional.
Univariate analysis was performed to identify factors associated with financial stress and anxiety. Increased financial stress was associated with employment status change (P < .001) and low‐stage cancer (P = .008) (Table 3). Worry about future financial problems was associated with early stage cancer (P = .017) and telehealth participation (P = .04) (Table 3). When assessing anxiety levels, lower annual income, defined as <$40,000, was the most significant variable associated with both increased cancer worry and generalized anxiety (P = .03 and P = .005, respectively) (Table 4). Delays in cancer treatment were significantly associated with increased generalized anxiety (P = .018). Access to therapy was associated with self‐reported increased anxiety (P = .05) (Table 4). This finding was reinforced in patients who had clinically significant anxiety, as defined by a GAD score >10, which was associated with both access to therapy and interest in therapy (P = .006 and P < .001, respectively). Primary language, living with roommates, education level, having children, residence by COVID‐19 prevalence, active treatment, comorbidities, and interest in therapy were not associated with an increase in cancer worry or anxiety.
TABLE 3.
Factors Associated With Financial Toxicity
| Factor | No. of Patients (%) | P | |
|---|---|---|---|
| Yes | No | ||
| Self‐reported financial stress a , b | |||
| Age, y | .520 | ||
| <65 | 37 (54.4) | 31 (45.6) | |
| >65 | 13 (44.8) | 16 (55.2) | |
| Income c | .450 | ||
| <$21,000 | 22 (62.9) | 13 (37.1) | |
| $21,000‐$40,000 | 17 (48.6) | 18 (51.4) | |
| ≥$40,000 | 7 (50.0) | 7 (50.0) | |
| Employment status change | <.001 d | ||
| Yes | 18 (90.0) | 2 (10.0) | |
| No | 32 (41.6) | 45 (58.4) | |
| Roommates | .952 | ||
| Yes | 13 (54.2) | 11 (45.8) | |
| No | 37 (50.7) | 36 (49.3) | |
| Children | .987 | ||
| Yes | 34 (50.7) | 33 (49.3) | |
| No | 16 (53.3) | 14 (46.7) | |
| Patient residence e | .718 | ||
| High COVID‐19 prevalence | 35 (50.7) | 34 (49.3) | |
| Low COVID‐19 prevalence | 10 (43.5) | 13 (56.5) | |
| Cancer stage | .008 d | ||
| Low: I‐II | 42 (60.9) | 27 (39.1) | |
| High: III‐IV | 8 (28.6) | 20 (71.4% | |
| Active treatment | .880 | ||
| Yes | 9 (47.4) | 10 (52.6) | |
| No | 41 (52.6) | 37 (47.4) | |
| Telehealth participation | .657 | ||
| Yes | 17 (47.2) | 19 (52.8) | |
| No | 33 (54.1) | 28 (45.9) | |
| Worry about future financial problems f , g | |||
| Age, y | .308 | ||
| <65 | 41 (60.3) | 27 (39.7) | |
| >65 | 13 (46.4) | 15 (53.6) | |
| Income c | .618 | ||
| <$21,000 | 20 (57.1) | 15 (42.9) | |
| $21,000‐$40,000 | 20 (57.1) | 15 (42.9) | |
| ≥$40,000 | 6 (42.9) | 8 (57.1) | |
| Employment status change | .254 | ||
| Yes | 14 (70.0) | 6 (30.0) | |
| No | 40 (52.6) | 36 (47.4) | |
| Roommates | .786 | ||
| Yes | 14 (60.9) | 9 (39.1) | |
| No | 40 (54.8) | 33 (45.2) | |
| Children | .153 | ||
| Yes | 34 (50.7) | 33 (49.3) | |
| No | 20 (69.0) | 9 (31.0) | |
| Patient residence h | >.99 | ||
| High COVID‐19 prevalence | 39 (56.5) | 30 (43.5) | |
| Low COVID‐19 prevalence | 12 (54.5) | 10 (45.5) | |
| Cancer stage | .017 d | ||
| Low: I‐II | 44 (64.7) | 24 (35.3) | |
| High: III‐IV | 10 (35.7) | 18 (64.3) | |
| Active treatment | >.99 | ||
| Yes | 11 (57.9) | 8 (42.1) | |
| No | 43 (55.8) | 34 (44.2) | |
| Telehealth participation | .04 d | ||
| Yes | 25 (71.4) | 10 (28.6) | |
| No | 29 (47.5) | 32 (52.5) | |
Abbreviation: COVID‐19, coronavirus disease 2019.
Financial toxicity was based on the binary measure (yes/no): “Do you feel financially stressed?”
Three of 100 patients declined to report financial stress.
Thirteen of 97 patients declined to report income.
This P value indicates a significant difference.
Of the patients who reported financial stress, 5 of 97 lived outside of New York City.
Financial toxicity was based on the binary measure (yes/no): “Do you worry about future financial problems as a result of COVID‐19?”
Four of 100 patients declined to report worry about future financial problems.
Of the patients who reported worry about future financial problems, 5 of 96 lived outside of New York City.
TABLE 4.
Factors Associated With Anxiety
| Factor | No. of Patients (%) | P | |
|---|---|---|---|
| Yes | No | ||
| Self‐reported increased worry about cancer a , b | |||
| Age, y | .931 | ||
| <65 | 31 (50.0) | 31 (50.0) | |
| >65 | 13 (46.4) | 15 (53.6) | |
| Income c | .036 d | ||
| <$21,000 | 20 (62.5) | 12 (37.5) | |
| $21,000‐$40,000 | 17 (53.1) | 15 (46.9) | |
| ≥$40,000 | 3 (21.4) | 11 (78.6) | |
| Children | .434 | ||
| Yes | 33 (52.4) | 30 (47.6) | |
| No | 11 (40.7) | 16 (59.3) | |
| Patient residence e | .597 | ||
| High COVID‐19 prevalence | 33 (50.0) | 33 (50.0) | |
| Low COVID‐19 prevalence | 8 (40.0) | 12 (60.0) | |
| Cancer stage | .573 | ||
| Low: I‐II | 33 (51.6) | 31 (48.4) | |
| High: III‐IV | 11 (42.3) | 15 (57.7) | |
| Active treatment | .712 | ||
| Yes | 10 (55.6) | 8 (44.4) | |
| No | 34 (47.2) | 38 (52.8) | |
| Any delay in cancer care: Treatment, appointments | .092 | ||
| Yes | 26 (59.1) | 18 (40.9) | |
| No | 18 (39.1) | 28 (60.9) | |
| Access to therapy f | .685 | ||
| Yes | 8 (42.1) | 11 (57.9) | |
| No | 34 (50.7) | 33 (49.3) | |
| Interest in therapy g | >.99 | ||
| Yes | 7 (50.2) | 7 (50.0) | |
| No | 27 (50.9) | 26 (41.9) | |
| Self‐reported increase in anxiety h , i | |||
| Age, y | .79 | ||
| <65 | 43 (66.2) | 22 (33.8) | |
| >65 | 17 (60.7) | 11 (39.3) | |
| Income j | .005 d | ||
| <$21,000 | 28 (84.8) | 5 (15.2) | |
| $21,000‐$40,000 | 20 (58.8) | 14 (41.2) | |
| ≥$40,000 | 5 (38.5) | 8 (61.5) | |
| Children | .661 | ||
| Yes | 44 (66.7) | 22 (33.3) | |
| No | 16 (59.3) | 11 (40.7) | |
| Patient residence k | .286 | ||
| High COVID‐19 prevalence | 41 (60.3) | 27 (39.7) | |
| Low COVID‐19 prevalence | 16 (76.2) | 5 (23.8) | |
| Cancer stage | >.99 | ||
| Low: I‐II | 44 (64.7) | 24 (35.3) | |
| High: III‐IV | 16 (64.0) | 9 (36.0) | |
| Active treatment | >.99 | ||
| Yes | 12 (66.7) | 6 (33.3) | |
| No | 48 (64.0) | 27 (36.0) | |
| Any delay in cancer care: Treatment, clinic appointments | .018 d | ||
| Yes | 35 (77.8) | 10 (22.2) | |
| No | 25 (52.1) | 23 (47.9) | |
| Access to therapy l | .051 d | ||
| Yes | 17 (85.0) | 3 (15.0) | |
| No | 40 (58.0) | 29 (42.0) | |
| Interest in therapy m | .401 | ||
| Yes | 10 (71.4) | 4 (28.6) | |
| No | 30 (54.5) | 25 (45.5) | |
Abbreviation: COVID‐19, coronavirus disease 2019.
Cancer worry was categorized as binary: no (not at all) or yes (a little bit, somewhat, very much).
Ten of 100 patients declined to report worry about cancer.
Twelve of 90 patients declined to report income.
This P value indicates a significant difference.
Of the patients who reported a level of worry about cancer, 4 of 90 lived outside of New York City.
Of the patients who reported a level of worry about cancer, 4 of 90 declined to report access to therapy.
All 67 patients who reported no access to a therapist were asked about interest in therapy.
Screening for an increase in generalized anxiety was categorized as binary: no (not at all) or yes (a little bit, somewhat, very much).
Seven of 100 patients declined to report worry about cancer.
Thirteen of 93 patients declined to report income.
Of the patients who reported general anxiety levels, 4 of 93 lived outside of New York City.
Of the patients who reported general anxiety levels, 4 of 93 declined to report access to therapy.
All 69 patients who reported no access to a therapist were asked about interest in therapy.
Multivariable logistic regression analysis was used to evaluate factors predictive of anxiety and financial stress. After controlling for change in employment, education, income, and residence in an area with high COVID‐19 prevalence, the odds of experiencing anxiety increased 4‐fold when patients had any delay in oncology care (P = .023; 95% CI, 1.278‐14.950). Higher annual income, defined as >$40,000, decreased the odds of experiencing anxiety by a factor of 0.04 (P = .001; 95% CI, 0.004‐0.238) (see Supporting Table 1). The odds of experiencing financial stress decreased by a factor of 0.353 in patients who had advanced‐stage cancer compared with those who had early stage cancer after controlling for these same factors (P = .063; nonsignificant trend favoring a decrease in financial distress with higher cancer stage) (see Supporting Table 2).
Discussion
To our knowledge, this is the first study to evaluate and identify factors associated with the financial and emotional impact of the COVID‐19 pandemic on patients with gynecologic cancer who have Medicaid insurance. NYC Medicaid is a program for low‐income individuals whose annual household incomes and/or resources are below set guidelines. To qualify for NYC Medicaid, patients must have high medical bills and low income (ie, for a family of 4, annual income <$36,156). 23 In our study, most patients lived in boroughs that were disproportionately affected by COVID‐19 and had an annual income <$40,000. These patients receiving gynecologic oncology care experienced significantly increased financial distress during the pandemic, which was further exacerbated by lower income bracket, early cancer stage, and a change in employment status. In addition, patients in the lowest income brackets who experienced delays in cancer care reported significantly increased cancer worry and anxiety.
Public health emergencies, such as the current COVID‐19 pandemic, affect the health, safety, and well‐being of individuals and lead to ubiquitous emotional distress. 24 It is reported that populations with preexisting medical conditions are at increased risk for adverse psychosocial outcomes. 24 In our study, Medicaid patients with cancer in the lowest income bracket (annual household income <$21,000) experienced significantly increased levels of cancer worry and anxiety. Within this group, 69% had medical comorbidities identified that were considered a high risk for COVID‐19 disease severity, which may account for additional stress identified in this population. Furthermore, access to or interest in therapy was significantly associated with GAD scores >10 (P = .006 and P < .001, respectively). This is an important finding because the GAD‐7 scale has been shown to highly correlate with anxiety and its degree of severity. GAD scores >10 correlate with the highest anxiety levels and are an appropriate clinical marker for referral to therapy. 20 , 22 In addition, we found that the odds of having anxiety increases 4‐fold when patients experienced any delay in their cancer care (odds ratio, 4.089; P = .023), even when controlling for changes in employment status, education, income level, and residence in an area with high COVID‐19 prevalence. These findings demonstrate the importance of timely cancer care and its impact on cancer worry and generalized anxiety. Asking about social determinants of health may reveal factors that could exacerbate treatment delays and help facilitate an individualized approach to cancer treatment. 8
As COVID‐19 cases rise and reach critical levels in other major states, patients with low income will continue to be affected. Patients in lower income brackets often have less financial stability and limited job flexibility with regard to working from home. 25 , 26 Changes in employment status and early stage cancer were significantly associated with an increase in financial distress (P < .001 and P = .008, respectively), even after controlling for factors that include changes in employment, education, and income and residence in an area with high COVID‐19 prevalence. Although it may be surprising that early stage cancer was associated with an increase in financial distress compared with late‐stage cancer, this may be explained in part by increasing coverage of health care expenses by Medicaid for patients with higher medical bills. 23 These results suggest that patients who have early stage cancer may have increased concerns for financial planning, morbidity, and accumulating treatment costs in the future compared with those who have advanced disease and may have more costs covered and a limited lifespan. 14 Patients who have cancer already face a higher rate of bankruptcy because of high medical costs and may struggle to prioritize cancer care and treatments over other costs of daily living because of increased financial distress during the pandemic, especially compared with those who have a more limited lifespan. 11 , 12 , 13 , 14 Telehealth visits were an emerging technology during the study period, and the use of telehealth appeared to play a role in financial distress, with 71% of patients reporting increased future financial worry compared with those who did not use telehealth (P = .04). As cancer care facilities continue to build their telemedicine infrastructure, incorporating questions around financial toxicity will be crucial because finances can affect care.
Despite the racial disparities in COVID‐19 morbidity and mortality, we observed that race alone was not significantly associated with increased financial distress, increased worry about cancer, or anxiety in our study population. Socioeconomic status, not race, appeared to be the most significant factor in our cohort. Reasons for this finding may be related to the inherent diversity of the NYC population, in whom higher incomes help to close the gaps in health care inequities and in cancer care. 11 , 27 This finding is supported by a recent study conducted in racially diverse Florida demonstrating that, for women with epithelial ovarian cancer, after adjusting for all covariates (including race/ethnicity), women living in more marginalized neighborhoods had an increased hazard of death. 28
The current study has several limitations. This was a descriptive, hypothesis‐generating pilot study that relied on a 1‐time interview based on patient self‐report. Without a baseline pre–COVID‐19 interview, there is concern for recall bias. To account for this, a retrospective review of medical records was also performed to confirm findings when possible. To screen for a broad range of outcomes, validated surveys, such as the COST‐PROM survey, the CWS, and the GAD‐7, were modified and abbreviated for use in a time‐limited, 50‐question telephone interview. Because these validated tools were modified for ease of application in a telephone interview setting, the results reported in this study may be different compared with results from use of the complete validated surveys when screening for financial toxicity, cancer worry, and anxiety. Our goal was to broadly survey potential negative outcomes of the COVID‐19 pandemic on cancer care in a hypothesis‐generating study, and further research using complete validated tools in a larger sample size will be required to confirm findings from this study. Despite the modification of these validated surveys, other studies that have examined financial toxicity and cancer worry report findings similar to ours. 13 , 29 In addition, because this study was conducted among patients with Medicaid insurance who were receiving gynecologic oncology care, it is unclear whether these results could be applied to the general cancer population or among those who have private insurance. Although there are limited studies examining the effect of the COVID‐19 pandemic on cancer survivors and financial toxicity, cancer worry, and anxiety, studies in head and neck cancer and ovarian cancer among patients with both private and public insurance have revealed similar findings. 13 , 29
The ongoing COVID‐19 pandemic has highlighted existing inequities in health care, and consideration of alternative methods to achieve health equity are pertinent. Increased screening for anxiety and financial toxicity in this population is essential, as is a restructuring of practices to minimize delays in care while maintaining appropriate social distancing and safe practices for both providers and patients. Oncology providers should consider implementing screening tools to address social health determinants that may cause delays in or create barriers to care in already vulnerable patients. These include screening for changes in employment status and food security as well as providing transportation assistance for those who may otherwise rely on public transit. Finally, providing additional support and treatment options to the most financially vulnerable patients during this time is important because they appear to experience significantly increased cancer worry and anxiety compared with those patients in higher income brackets.
Funding Support
Paul J. Christos and Charlene Thomas were supported in part by a grant from the Clinical and Translational Science Center at Weill Cornell Medical College (1‐UL1‐TR002384‐01).
Conflict of Interest Disclosures
Kevin Holcomb reports personal fees from Johnson & Johnson and research support from Fujirebio Diagnostics, outside the submitted work. The remaining authors made no disclosures.
Author Contributions
All authors made substantial contributions to the conception or design of the work or to the acquisition, analysis, or interpretation of data for the work and to the drafting of the work or its critical revision for important intellectual content; have given final approval of the version to be published; and have agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Supporting information
Supplementary Material
Chen YS, Zhou ZN, Glynn SM, Frey MK, Balogun OD, Kanis M, Holcomb K, Gorelick C, Thomas C, Christos PJ, Chapman‐Davis E. Financial toxicity, mental health, and gynecologic cancer treatment: The effect of the COVID‐19 pandemic among low‐income women in New York City. Cancer. 2021. 10.1002/cncr.33537
References
- 1. Mahase E. Covid‐19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ. 2020;368:m1036. doi: 10.1136/bmj.m1036 [DOI] [PubMed] [Google Scholar]
- 2. New York City Health . COVID‐19: Data. Accessed April 15, 2020. https://www1.nyc.gov/site/doh/covid/covid‐19‐data.page
- 3. Mansoor S. Data Suggests Many New York City Neighborhoods Hardest Hit by COVID‐19 Are Also Low‐Income Areas. Time. April 5, 2020. Accessed April 15, 2020. https://time.com/5815820/data‐new‐york‐low‐income‐neighborhoods‐coronavirus/ [Google Scholar]
- 4. Mauger C, MacDonald C. Michigan's COVID‐19 cases, deaths hit blacks disproportionately. The Detroit News. April 2, 2020. Accessed April 15, 2020. https://www.detroitnews.com/story/news/local/michigan/2020/04/02/michigans‐covid‐19‐deaths‐hit‐417‐cases‐exceed‐10‐700/5113221002/ [Google Scholar]
- 5. Stark C, Rice G. Coronavirus hitting black residents in Kansas City hardest. The Kansas City Star. April 7, 2020. Accessed April 15, 2020. https://www.kansascity.com/news/coronavirus/article241824321.html [Google Scholar]
- 6. Garcia M. Chelsea, city of the working Latino immigrant, emerges as a COVID‐19 hotspot. The Boston Globe. April 7, 2020. Accessed April 15, 2020. https://www.bostonglobe.com/2020/04/07/opinion/chelsea‐city‐working‐latino‐immigrant‐emerges‐covid‐19‐hotspot/ [Google Scholar]
- 7. New York City Health . Age adjusted rate of fatal lab confirmed COVID‐19 cases per 100,000 by race/ethnicity group as of April 6, 2020. Accessed April 15, 2020. https://www1.nyc.gov/assets/doh/downloads/pdf/imm/covid‐19‐deaths‐race‐ethnicity‐04082020‐1.pdf
- 8. Farley JH, Hines J, Lee NK, et al. Promoting health equity in the era of COVID‐19. Gynecol Oncol. 2020;158:25‐31. doi: 10.1016/j.ygyno.2020.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yu J, Ouyang W, Chua MLK, Xie C. SARS‐CoV‐2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol. 2020;6:1108‐1110. doi: 10.1001/jamaoncol.2020.0980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Liang W, Guan W, Chen R, et al. Cancer patients in SARS‐CoV‐2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335‐337. doi: 10.1016/S1470-2045(20)30096-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zheng Z, Han X, Guy GP, et al. Do cancer survivors change their prescription drug use for financial reasons? Findings from a nationally representative sample in the United States. Cancer. 2017;123:1453‐1463. doi: 10.1002/cncr.30560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. De Souza JA, Yap BJ, Hlubocky FJ, et al. The development of a financial toxicity patient‐reported outcome in cancer: the COST measure. Cancer. 2014;120:3245‐3253. doi: 10.1002/cncr.28814 [DOI] [PubMed] [Google Scholar]
- 13. Baddour K, Kudrick LD, Neopaney A, et al. Potential impact of the COVID‐19 pandemic on financial toxicity in cancer survivors. Head Neck. 2020;42:1332‐1338. doi: 10.1002/hed.26187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hershman DL, Tsui J, Wright JD, Coromilas EJ, Tsai WY, Neugut AI. Household net worth, racial disparities, and hormonal therapy adherence among women with early‐stage breast cancer. J Clin Oncol. 2015;33:1053‐1059. doi: 10.1200/JCO.2014.58.3062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pothuri B, Alvarez Secord A, Armstrong D, et al. Anti‐Cancer Therapy and Clinical Trial Considerations for Gynecologic Oncology Patients During the COVID‐19 Pandemic Crisis. Society for Gynecologic Oncology; 2020. Accessed April 15, 2020. https://www.sgo.org/clinical‐practice/management/covid‐19‐resources‐for‐health‐care‐practitioners/anti‐cancer‐therapy‐and‐clinical‐trial‐considerations‐for‐gyn‐onc‐patients/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Marron JM, Joffe S, Jagsi R, Spence RA, Hlubocky FJ. Ethics and resource scarcity: ASCO recommendations for the oncology community during the COVID‐19 pandemic. J Clin Oncol. 2020;38:2201‐2205. doi: 10.1200/JCO.20.00960 [DOI] [PubMed] [Google Scholar]
- 17. Society of Gynecologic Oncology . Gynecology Considerations During the COVID‐19 Pandemic. Society of Gynecologic Oncology; 2020. Accessed May 2, 2020. https://www.sgo.org/clinical‐practice/management/covid‐19‐resources‐for‐health‐care‐practitioners/gyn‐onc‐considerations‐during‐covid‐19/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Custers J, van den Berg S, van Laarhoven H, Bleiker E, Gielissen M, Prins J. The Cancer Worry Scale: detecting fear of recurrence in breast cancer survivors. Cancer Nurs. 2014;37:E44‐E50. [DOI] [PubMed] [Google Scholar]
- 19. Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD‐7. Arch Intern Med. 2006;166:1092‐1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 20. Ruiz MA, Zamorano E, Garcia‐Campayo J, Pardo A, Freire O, Rejas J. Validity of the GAD‐7 scale as an outcome measure of disability in patients with generalized anxiety disorders in primary care. J Affect Disord. 2011;128:277‐286. doi: 10.1016/j.jad.2010.07.010 [DOI] [PubMed] [Google Scholar]
- 21. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. JAMA. 2020;323:1061‐1069. doi: 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Andersen BL, Derubeis RJ, Berman BS, et al. Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: an American Society of Clinical Oncology guideline adaptation. J Clin Oncol. 2014;32:1605‐1619. doi: 10.1200/JCO.2013.52.4611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Department of Health, New York State . Medicaid in New York State. Accessed July 7, 2020. https://www.health.ny.gov/health_care/medicaid/#trusts
- 24. Pfefferbaum B, North CS. Mental health and the Covid‐19 pandemic. N Engl J Med. 2020;383:510‐512. doi: 10.1056/NEJMp2008017 [DOI] [PubMed] [Google Scholar]
- 25. Jin B, McGill A. Who is most at risk in the coronavirus crisis: 24 million of the lowest‐income workers. Politico; 2020. Accessed July 15, 2020. https://www.politico.com/interactives/2020/coronavirus‐impact‐on‐low‐income‐jobs‐by‐occupation‐chart/ [Google Scholar]
- 26. Gould E, Shierholz E. Not everybody can work from home: Black and Hispanic workers are much less likely to be able to telework. Economic Policy Institute, Working Economics Blog. Economic Policy Institute; 2020. Accessed July 15, 2020. https://www.epi.org/blog/black‐and‐hispanic‐workers‐are‐much‐less‐likely‐to‐be‐able‐to‐work‐from‐home/ [Google Scholar]
- 27. Pollack CE, Chideya S, Cubbin C, Williams B, Dekker M, Braveman P. Should health studies measure wealth? A systematic review. Am J Prev Med. 2007;33:250‐264. doi: 10.1016/j.amepre.2007.04.033 [DOI] [PubMed] [Google Scholar]
- 28. Westrick AC, Bailey ZD, Schlumbrecht M, et al. Residential segregation and overall survival of women with epithelial ovarian cancer. Cancer. 2020;126:3698‐3707. doi: 10.1002/cncr.32989 [DOI] [PubMed] [Google Scholar]
- 29. Frey MK, Ellis AE, Zeligs K, et al. Impact of the coronavirus disease 2019 pandemic on quality of life for women with ovarian cancer. Am J Obstet Gynecol. 2020;223:725.e1‐725.e9. doi: 10.1016/j.ajog.2020.06.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


