Abstract
Objective
To analyse the impact of the COVID‐19 pandemic on a centralized specialist kidney cancer care pathway.
Materials and Methods
We conducted a retrospective analysis of patient and pathway characteristics including prioritization strategies at the Specialist Centre for Kidney Cancer located at the Royal Free London NHS Foundation Trust (RFH) before and during the surge of COVID‐19.
Results
On 18 March 2020 all elective surgery was halted at RFH to redeploy resources and staff for the COVID‐19 surge. Prioritizing of patients according to European Association of Urology guidance was introduced. Clinics and the specialist multidisciplinary team (SMDT) meetings were maintained with physical distancing, kidney surgery was moved to a COVID‐protected site, and infection prevention measurements were enforced. During the 7 weeks of lockdown (23 March to 10 May 2020), 234 cases were discussed at the SMDT meetings, 53% compared to the 446 cases discussed in the 7 weeks pre‐lockdown. The reduction in referrals was more pronounced for small and asymptomatic renal masses. Of 62 low‐priority cancer patients, 27 (43.5%) were deferred. Only one (4%) COVID‐19 infection occurred postoperatively, and the patient made a full recovery. No increase in clinical or pathological upstaging could be detected in patients who underwent deferred surgery compared to pre‐COVID practice.
Conclusion
The first surge of the COVID‐19 pandemic severely impacted diagnosis, referral and treatment of kidney cancer at a tertiary referral centre. With a policy of prioritization and COVID‐protected pathways, capacity for time‐sensitive oncological interventions was maintained and no immediate clinical harm was observed.
Keywords: COVID‐19, renal cell carcinoma, centralization of care, prioritization
Abbreviations
- AS
active surveillance
- EAU
European Association of Urology
- NCEL
North Central and East London Cancer Alliance
- RFH
Royal Free London NHS Foundation Trust
- SARS‐CoV‐2
severe acute respiratory syndrome coronavirus 2
- SCKC
Specialist Centre for Kidney Cancer
- SMDT
specialist multidisciplinary team
- SRM
small renal mass
- UCL
University College London
- UCLH
University College London Hospital
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) led to a viral outbreak of COVID‐19 initially in Wuhan, China in late 2019, before manifesting as a global pandemic [1]. Healthcare systems came under unprecedented strain, and many institutions triaged cancer care according to priority scenarios, balancing the risk of SARS‐CoV‐2 transmission against the clinical benefit deriving from a specific therapeutic approach [2]. In recent years, specialist multidisciplinary cancer services have been centralized in the UK to reduce variations in care and improve patient outcomes [3, 4]. Due to their complex network structure and high‐volume surgical capacity at a single‐site location [5], these centres may be particularly vulnerable to the pandemic.
The Specialist Centre for Kidney Cancer (SCKC) is located at the Royal Free London NHS Foundation Trust (RFH) and is part of the University College London (UCL) Partners Academic Health Science Network and the North Central and East London Cancer Alliance (NCEL). The centre offers evidence‐based management of RCC, TCC and benign renal diseases, and is one of the largest referral centres in the UK and Europe, receiving tertiary referrals from eight trusts in a population area of 3.4 million. In addition, patients are directly referred from primary care with suspected kidney cancer as part of the 2‐week‐wait pathway [6]. Reductions of up to 84% in 2‐week‐wait referrals have been reported during the first surge of the COVID‐19 pandemic in the UK [7].
We describe the impact of COVID‐19 on a high‐volume centre for kidney cancer during the first surge, and the subsequent restoration of care in an environment affected by physical distancing, infection prevention measures and repeat surges of the pandemic.
Methods
Analysis of Pre‐COVID Practice
To compare the impact of COVID‐19 on previous practice, SMDT referrals and surgical volume (stage and procedure) between 1 January and 31 December 2019 were retrospectively assessed. Collection of data for the pre‐COVID surgical interventions per month was extended until 18 March 2020.
Development and Implementation of Prioritization
Based on published evidence [8] patients were triaged into low, intermediate and high priority, with recommendations for deferral (Tables S1 and S2). On 19 March 2020, the recommendations were signed off by the NCEL Pathway Board and distributed to all referring trusts. These recommendations were further developed into the European Association of Urology (EAU) guideline panel triage for RCC and TCC and published on behalf of the Guideline Office Rapid Reaction Group [5] on 14 April 2020. Prioritization started on 19 March and continued until 5 August 2020 (Table S1). Patients who underwent surgery in 2019 were retrospectively assigned to a priority category to compare the average number of low‐, intermediate‐ and high‐priority patients per month to the respective numbers during the lockdown.
Impact of the Pandemic on the SMDT and Surgical Volume
Data were prospectively collected for tertiary and primary 2‐week‐wait referrals to the weekly SMDT meeting in the 7 weeks prior to the surge from 5 February 2020, and continued until 5 August 2020 throughout the lockdown and ‘stay alert’ phase in London. Lockdown was declared on 23 March 2020 (‘stay at home’) and ended with the beginning of the ‘stay alert’ phase on 10 May 2020. The analysis focused on the clinical reasons for SMDT discussion (Table S3a) and the management recommendation during the pandemic, based on EAU priority [5]. Patients with incomplete referral were not included in the analysis of SMDT volume until an SMDT decision could be made, to avoid multiple counts. For an overview of collected data items see Table S3b. Further, data of surgical interventions per month were analysed from 1 January 2019 until 30 September 2020 (Fig. S3a,b).
Reallocation to a COVID‐Protected Site
On 18 March 2020, all elective surgery was halted at the SCKC, and a Urological Cancer Hub model was instituted by NCEL at University College London Hospital (UCLH) at Westmoreland Street, a COVID‐protected site without emergency admissions. From 24 March 2020, the SCKC commenced surgery lists at Westmoreland Street while emergency interventions continued at the RFH site. Number of surgeries was assessed for each site until 30 September 2020.
Analysis of Harm
Priority and the time from SMDT discussion to surgery was assessed for all surgical interventions from lockdown until 30 September 2020. For RCC, clinical and pathological TNM (cTNM and pTNM) were assessed and compared to the respective TNM stages in patients with RCC who underwent surgery pre‐COVID from April 2019 to March 2020. Testing for SARS‐CoV‐2 RNA by nasal and pharyngeal swab and real‐time PCR was introduced for all surgical patients at the COVID‐protected site on 20 April 2020 (Table S1). Number and percentage of COVID‐19‐positive patients in the peri‐operative period were assessed.
Ethics
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Results
Impact of the Pandemic on the SMDT
In 2019, 4035 patients were discussed at the SMDT meeting, of which 1136 were new referrals and 2918 were follow‐ups. Of the former, 698 were tertiary referrals. Between 5 February and 5 August 2020, 1235 patients were discussed at the SMDT meeting. This was a reduction of 39% compared to the equivalent period in 2019. Of these, 446 patients (36%) were discussed in the 7 weeks prior to the start of lockdown, including 56 2‐week‐wait referrals, and represent pre‐COVID practice. In the 7‐week period of lockdown lasting until 10 May 2020, 234 patients (19%) were discussed and triaged (Table 1), including 23 2‐week‐wait referrals, a reduction of 50% compared to pre‐COVID. Prioritization continued after 10 May until 5 August 2020, during which a further 555 patients (45%) were discussed but for these patients treatment deferral was no longer recommended. COVID also impacted on the diagnostic pathway. Pre‐COVID, a mean of eight diagnostic renal mass biopsies were performed per week which decreased to a mean of one biopsy per week during the lockdown (Table 1).
Table 1.
Patients discussed and prioritized at the specialist multidisciplinary team meeting in the 7 weeks prior to the declaration of lockdown on 23 March 2020 and in the period of lockdown lasting until 10 May 2020.
| Condition and priority category for malignancy | Pre‐lockdown: 5 February to 18 March 2020 | Lockdown: 23 March to 10 May 2020 (% of pre‐lock‐down [95% CI]) |
|---|---|---|
| RCC cT1a, low priorty | 111 | 62 (56 [0.47–0.65]) |
| RCC cT1b‐T2a, intermediate priority | 42 | 25 (59 [0.44–0.73]) |
| RCC ≥cT2b, high priority | 13 | 6 (46 [0.23–0.70]) |
| TCC of the upper urinary tract ≥Ta G3/≥T1 Gx, high priority | 34 | 25 (73.5 [0.57–0.85]) |
| Total intermediate/high priority | 89 | 56 (63 [0.52–0.72]) |
| Metastatic RCC and TCC of the upper urinary tract for medical oncology management, high priority | 36 | 38 (105) |
| Renal tumour biopsies | 56 | 7 (12.5 [0.06–0.24]) |
| Postoperative histology discussions | 61 | 28 (46 [0.34–0.58]) |
| Cystic renal lesions, low priority | 38 | 23 (64 [0.47–0.77]) |
| Benign conditions | 55 | 20 (36 [0.25–0.49]) |
| Total number of patients | 446 | 234 (53 [0.48–0.57]) |
| 2‐week wait referrals | 56 | 23 (50 [0.29–0.54]) |
G, tumour grade; Gx, Gany.
The observed 50% SMDT volume decrease (Fig. 1a) coincides with the surge of COVID‐19 cases and deaths in the UK and the date of the lockdown (Fig. 1b) and is predominantly caused by a decrease in absolute number of referrals from the relatively large group of cT1‐cT2a tumours (Table 1).
Fig. 1.
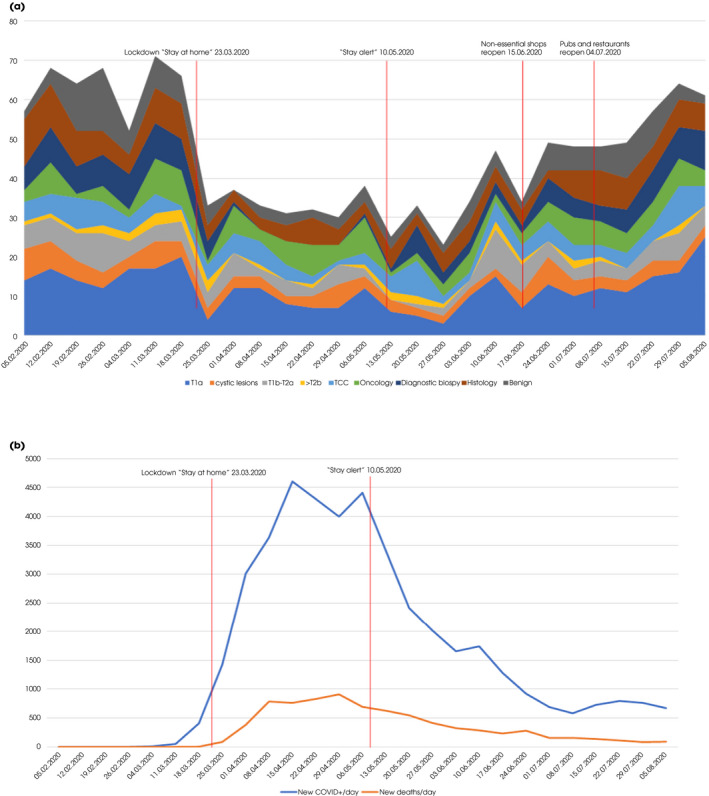
(a) Stacked graph of numbers of patients and conditions discussed at the Specialist Centre for Kidney Cancer (SCKC) specialist multidisciplinary team (SMDT) meeting between 5 February and 5 August. (b) Number of newly diagnosed COVID cases in the UK on the respective day of the SMDT meeting as well as the new number of deaths (source: https://www.ecdc.europa.eu/en/publications‐data/download‐todays‐data‐geographic‐distribution‐covid‐19‐cases‐worldwide).
During the 7‐week lockdown, 62 patients with suspected cT1a RCC were discussed at the SMDT meeting (Fig. S2), including 27 patients (43.5%) who received the EAU COVID‐recommendation of ‘active surveillance (AS) for 6 months followed by repeat imaging’. Of these, 25 (91%) accepted the SMDT recommendation of temporary AS. Only two patients (9%) requested a partial nephrectomy, which was performed after lockdown. When re‐invited after 10 May 2020 to discuss preference for intervention vs continued surveillance, nine patients (33.3%) preferred to continue with AS. At 6‐month follow‐up no progression was observed.
Impact of the Pandemic on Surgical Volume and Reallocation to a COVID‐Protected Site
In 2019, 423 surgeries were performed, 338 of which robot‐assisted (Fig. S1).
Surgery at the SCKC reduced from 26 to 40 interventions/month in 2019 and at the beginning of 2020 to 18 in March 2020, with only two in the last week of March following declaration of lockdown (Fig. 2). This increased to 12 interventions per month in April and May after reallocation to the UCLH COVID‐protected site until regaining pre‐COVID levels in September 2020.
Fig. 2.
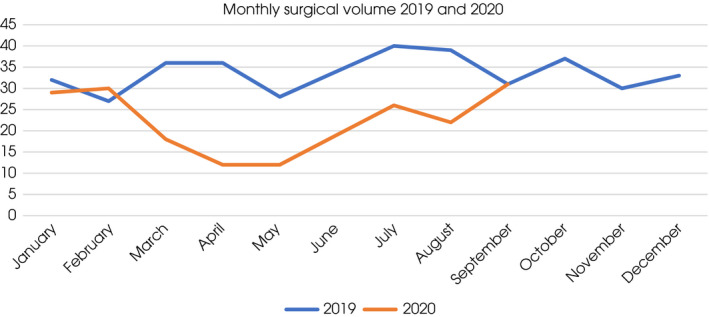
Monthly surgical volume before and during COVID‐19 pandemic.
In 2019, the average number and proportion corresponding to low‐, intermediate‐ and high‐priority patients treated per month were 10 (28.6%), 19 (54.3%) and six (17.1%), respectively. During the lockdown this changed to one (11%), four (44.4%) and four (44.4%), respectively (Table S4). Compared to the pre‐COVID period, the marked reduction of interventions for low‐priority tumours and benign conditions during the lockdown is reflected in a decrease of partial nephrectomy and pyeloplasties (Fig. S3a,b). From August 2020 renal surgical interventions were repatriated to RFH (Fig. S4).
Analysis of Harm
From 18 March 2020 until 30 September 2020, 130 patients underwent renal surgery, of whom 25 underwent this during the lockdown and 105 during the ‘stay alert’ phase. Comparing cTNM and pTNM stages for patients who underwent surgery for RCC to the 12‐month pre‐COVID period, no differences in stage presentation nor stage migration could be detected (Table S5). Between March and May 2020 the focus was on intermediate‐ and high‐priority cases (Fig. S5). The median (range; interquartile range) time for high‐, intermediate‐ and low‐priority tumours from SMDT discussion to surgery during the pandemic was 21 (14–37.5; 23.5), 34 (20.5–48.5; 28) and 64 (36.5–126.5; 90) days vs 29 (22–44; 22), 37 (23–54; 45) and 36 (21–51; 30) days in 2019, respectively. Two patients with high‐priority tumours developed progressive disease 6 and 8 weeks after surgery. Both had Leibovich score 11 (high‐risk) chromophobe RCCs with sarcomatoid differentiation, with times from SMDT discussion to surgery of 7 and 8 days. During lockdown, only one patient was diagnosed with COVID‐19 (4%; 95% CI 0.007–0.19) in the peri‐operative period prior to preoperative testing for SARS‐CoV‐2 RNA for all surgical patients. None of the patients were diagnosed with COVID‐19 in the postoperative period in the ‘stay alert’ phase. In addition, renal surgery in three patients who fully recovered from previous COVID‐19 was without peri‐operative complications. All COVID‐19‐affected patients are alive at a minimum of 6 months' follow‐up.
Discussion
COVID‐19 severely impacted elective and acute care in London during the first surge in spring 2020. The SCKC saw a decrease of referrals and SMDT discussions by almost 50% during the lockdown compared to an equivalent pre‐lockdown period. Other urological departments in the UK and Europe reported a similar decline in referrals [9, 10]. In addition to a decrease in referrals there was reduced SMDT discussion of histology results of diagnostic biopsies and surgeries. These procedures were less frequently performed because theatres and recovery units were requisitioned to treat COVID‐19‐infected patients and anaesthetists, surgeons and nurses redeployed to intensive care units.
The decrease in referrals of patients with cT1a tumours is not surprising as most small renal masses (SRMs) are diagnosed incidentally by imaging for other conditions, which were likely to be deferred or cancelled during lockdown. Interestingly, referrals of patients with EAU intermediate‐ and high‐priority tumours (≥cT1b) were also reduced (Table 1). This may be attributable to most of these tumours being asymptomatic despite their size. By contrast, symptomatic TCC presenting with visible haematuria decreased by only 26.5% and referrals of metastatic patients remained stable.
As our analyses demonstrate, low‐priority patients with SRMs are the majority of referrals to the SMDT. Despite a significant decrease in referral during the lockdown, they remained the largest group discussed at the SMDT meeting. From 18 March until 10 May 2020 they constituted 26% of all referrals. Pre‐COVID, except for the frail, these patients received the recommendation of ‘all cT1a options’, which include biopsy, (partial) nephrectomy, ablation or AS, to be decided in a shared decision process during a clinical visit. During lockdown, shared decision was deferred, resulting in potential delays for those harbouring malignancy and who wish to have active treatment. Ninety‐one percent of patients with ‘cT1a options’ accepted the COVID recommendation of ‘AS for 6 months’. Interestingly, 33% preferred to continue with AS without a biopsy when reinvited to discuss management options for cT1a lesions after the lockdown was lifted. The predominant reason was fear of contracting COVID‐19.
Deferring low‐priority patients during the surge was aimed at freeing up surgical capacity for high‐ and intermediate‐priority cases. However, with Europe and the UK experiencing repeat surges, some low‐priority patients with SRMs may be at risk of being deferred beyond acceptable time frames. Published data from the largest AS studies of SRMs suggest a cumulative delayed intervention rate of 10% per year due to tumour growth [11, 12]. These data support treating low‐priority patients early after the surge although this needs to be balanced against the risk that surgery in patients contracting peri‐operative COVID‐19 may be harmful with a high mortality rate [13]. Therefore, patients should be counselled and tested for COVID‐19, as was introduced from 20 April 2020 at the COVID‐protected site. Nevertheless, the absence of peri‐operative COVID‐19 after the introduction of testing supported that it was safe to invite back patients who were willing to discuss management of their SRMs. A recent analysis of 500 patients who underwent urological surgery at the COVID‐protected Westmoreland site, including the patients from the present analysis, confirmed a low peri‐operative SARS‐CoV‐2 infection rate of 2%, with no mortality [14]. This is in line with studies reporting a low prevalence of SARS‐COV‐2 infection among cancer patients (0.4%) and a low risk of 2.1% of contracting peri‐operative COVID‐19 with elective cancer surgery at COVID‐protected sites during the surge [15]. Proactive re‐invitation allowed us to assess the patients with biopsy‐proven cT1a RCC wishing to undergo an intervention.
In addition, diagnostic and surgical capacity increased 16 weeks after declaration of lockdown which was earlier than anticipated and reached pre‐COVID levels in September (Figs 1 and S4). Therefore, no significant delays occurred and all patients were treated, with priority given to highest urgency first. This is in contrast to a published model that predicted a cancellation rate of 37.7% globally for elective cancer surgery which would take 45 weeks to clear even after increasing capacity by 20% [16].
Limitations of this study include the retrospective assignment of prioritization to the pre‐COVID practice when in fact such a triage system did not exist at that time. In addition, the influence of patient characteristics such as age and comorbidities on shielding recommendations and referral has not been captured in detail. Our analysis is further limited by uncertainty about the number of undetected kidney cancers due to lockdown measures. This is of concern as pathologically high‐risk cancers are also found in asymptomatic and smaller tumours, many of which have not been diagnosed since 23 March 2020 [17]. Delay in diagnosing kidney cancer may affect survival. A recent publication found that a 3‐month delay in the 2‐week‐wait referral pathway reduces 10‐year net survival of kidney cancer stages I–III by 5–17%, depending on age group [6]. Based on 2459 kidney cancers diagnosed annually on the 2‐week‐wait primary care referral pathway in the UK, a 3‐ and 5‐month delay would result in 168 and 309 attributable lives lost, respectively. During the lockdown we observed a 50% decline in 2‐week‐wait referrals for kidney cancer compared to the 7 weeks prior to the surge which took almost 5 months to recover to pre‐COVID levels.
Several lessons drawn from this audit (Fig. S6) helped us to respond rapidly to the current second surge which is influenced by two external factors that differ from the first surge. Importantly, a novel and more transmissible SARS‐CoV‐2 variant emerged in southeast England in November 2020, impacting rapidly on available healthcare resources [18]. In addition, compared to the ‘stay‐at‐home’ policy and the encouraged shielding of patients during the first surge, access to primary healthcare improved in the UK by remote consulting, with noticeably more referrals during the ongoing surge [19]. First, we rapidly reintroduced prioritization of patients according to clinical urgency. This ensures all prognostically high‐risk patients will be treated in due time. Prioritization requires clear communication with care providers and patients to ensure that all referrals are managed in the safest possible way. Further, based on established contacts and contractual agreements, we were able to reallocate our theatre capacity within 72 h through the NCEL Urological Cancer Hub to the COVID‐protected site for elective cancer surgery with infection prevention protocols in place. Infection prevention measures are supported by data emerging during the first surge and are required for the safe treatment of cancer patients [2021]. In addition, surgical capacity has been rapidly adapted to accommodate intermediate‐ and high‐priority interventions. Finally, we reintroduced tracking of deferred patients to proactively invite patients back after the current surge to allow dynamic use of increasing capacity.
Disclosure of Interest
None.
Supporting information
Table S1. Timeline of events at the Specialist Centre for Kidney Cancer during the first surge of the COVID‐19 pandemic.
Table S2. Specialist Centre for Kidney Cancer recommendations to prioritize treatment during the COVID‐19 pandemic developed 16 March 2020 and communicated with referring trusts 19 March 2020 after approval of University College London Hospital Cancer Collaborative Pathway Board.
Table S3. (a and b) Clinical reasons for specialist multidisciplinary team (SMDT) discussion collected per patient referred to the SMDT in the 7 weeks leading up to the surge and during the lockdown until 5 August 2020 and overview of the data collected in an Excel registry during COVID.
Table S4. Distribution of patients who had an intervention in 2019 at the Specialist Centre for Kidney Cancer according to COVID recommendations.
Table S5. Clinical and pathological TNM stages and histological subtypes of patients with biopsy‐proven or suspected renal cancer on imaging who underwent surgery during lockdown and 'stay alert' phase and pre‐COVID from April 2019 to March 2020.
Fig. S1. Surgical volume at the Specialist Centre for Kidney Cancer in 2019, subdivided into procedure and surgical approach.
Fig. S2. Breakdown of small renal masses (cT1a tumours) presented at the specialist multidisciplinary team meeting during the lockdown and subsequent treatment decisions.
Fig. S3. (a and b) Monthly surgeries per stage and condition (a) and type of intervention (b) at the Specialist Centre for Kidney Cancer from January 2019 until September 2020.
Fig. S4. Surgical interventions for kidney and upper tract cancer at the Royal Free (RFH) and Westmoreland Street (WMS) COVID‐protected site from 18 March until September 2020.
Fig. S5. Distribution of priority levels of patients who underwent surgery from 18 March until 30 September 2020 in numbers per month.
Fig. S6. Threats and actions at the Specialist Centre for Kidney Cancer during the pandemic.
Acknowledgements
We are very grateful to all our colleagues, NHS management and the EAU guidelines panel rapid reaction group for efficient and comprehensive actions during the pandemic period. Also, we would like to thank all the patients for their alliance during that unprecedented time.
References
- 1. Zhu NA, Zhang D, Wang W et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020; 382: 727–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Curigliano G. How to guarantee the best of care to patients with cancer during the COVID‐19 epidemic: the Italian experience. Oncologist 2020; 25: 463–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tran MGB, Aben KKH, Werkhoven E et al. Guideline adherence for the surgical treatment of T1 renal tumours correlates with hospital volume: an analysis from the British Association of Urological Surgeons Nephrectomy Audit. BJU Int 2020; 125: 73–81 [DOI] [PubMed] [Google Scholar]
- 4. Fulop NJ, Ramsay AIG, Vindrola‐Padros C et al. Reorganising specialist cancer surgery for the twenty‐first century: a mixed methods evaluation (RESPECT‐21). Implement Sci 2016; 11: 155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ribal MJ, Cornford P, Briganti A et al. European Association of Urology Guidelines Office Rapid Reaction Group: an organisation‐wide collaborative effort to adapt the European Association of Urology guidelines recommendations to the coronavirus disease 2019 era. Eur Urol 2020; 78: 21–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dodds W, Morgan M, Wolfe C, Raju KS. Implementing the 2‐week wait rule for cancer referral in the UK: general practitioners' views and practices. Eur J Cancer Care (Engl) 2004; 13: 82–7 [DOI] [PubMed] [Google Scholar]
- 7. Sud A, Torr B, Jones ME et al. Effect of delays in the 2‐week‐wait cancer referral pathway during the COVID‐19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol 2020; 21: 1035–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wallis CJD, Novara G, Marandino L et al. Risks from deferring treatment for genitourinary cancers: a collaborative review to aid triage and management during the COVID‐19 pandemic. Eur Urol 2020; 78: 29–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Collins PM, Madden A, O’Connell C et al. Urological service provision during the COVID‐19 period: the experience from an Irish tertiary centre. Ir J Med Sci. 2020; 27: 1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Oderda M, Roupret M, Marra G et al. The impact of COVID‐19 outbreak on uro‐oncological practice across Europe: which burden of activity are we facing ahead? Eur Urol 2020; 78: 124–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McIntosh AG, Ristau BT, Ruth K et al. Active surveillance for localized renal masses: tumor growth, delayed intervention rates, and >5‐yr clinical outcomes. Eur Urol 2018; 74: 157–64 [DOI] [PubMed] [Google Scholar]
- 12. Pierorazio PM, Johnson MH, Ball MW et al. Five‐year analysis of a multi‐institutional prospective clinical trial of delayed intervention and surveillance for small renal masses: the DISSRM registry. Eur Urol 2015; 68: 408–15 [DOI] [PubMed] [Google Scholar]
- 13. COVIDSurg Collaborative . Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS‐CoV‐2 infection: an international cohort study. Lancet. 2020; 396: 27–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kasivisvanathan V, Lindsay J, Rakshani‐Moghadam S et al. A cohort study of 30 day mortality after NON‐EMERGENCY surgery in a COVID‐19 cold site. Int J Surg 2020; 84: 57–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Glasbey JC, Nepogodiev D, Simoes JFF et al. Elective cancer surgery in COVID‐19–free surgical pathways during the SARS‐CoV‐2 pandemic: an international, multicenter, comparative cohort study. J Clin Oncol 2021; 39: 66–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. COVIDSurg Collaborative . Elective surgery cancellations due to the COVID‐19 pandemic: global predictive modelling to inform surgical recovery plans. Surg Br J 2020; 12: 1440–9. 10.1002/bjs.11746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Di trapani E, Dell'oglio P, Larcher A et al. Pathological high‐risk renal cell carcinoma: trends in clinical characteristics over 25 years. Anticancer Res 2018; 38: 4123–30 [DOI] [PubMed] [Google Scholar]
- 18. Davies NG, Abbott S, Barnard RC et al. Estimated transmissibility and impact of SARS‐CoV‐2 lineage B.1.1.7 in England. Science 2021: 372: eabg3055. 10.1126/science.abg3055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Murphy M, Scott LJ, Salisbury C et al. Implementation of remote consulting in UK primary care following the COVID‐19 pandemic: a mixed‐methods longitudinal study. Br J Gen Pract 2021; 71: e166–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Glasbey JC, Bhangu A, COVIDSurg Collaborative . Elective cancer surgery in COVID‐19‐free surgical pathways during the SARS‐CoV‐2 pandemic: an international, multicenter, comparative cohort study. J Clin Oncol 2021; 39: 66–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Berghoff AS, Gansterer M, Bathke AC et al. SARS‐CoV‐2 testing in patients with cancer treated at a tertiary care hospital during the COVID‐19 pandemic. J Clin Oncol 2020; 38: 3547–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Timeline of events at the Specialist Centre for Kidney Cancer during the first surge of the COVID‐19 pandemic.
Table S2. Specialist Centre for Kidney Cancer recommendations to prioritize treatment during the COVID‐19 pandemic developed 16 March 2020 and communicated with referring trusts 19 March 2020 after approval of University College London Hospital Cancer Collaborative Pathway Board.
Table S3. (a and b) Clinical reasons for specialist multidisciplinary team (SMDT) discussion collected per patient referred to the SMDT in the 7 weeks leading up to the surge and during the lockdown until 5 August 2020 and overview of the data collected in an Excel registry during COVID.
Table S4. Distribution of patients who had an intervention in 2019 at the Specialist Centre for Kidney Cancer according to COVID recommendations.
Table S5. Clinical and pathological TNM stages and histological subtypes of patients with biopsy‐proven or suspected renal cancer on imaging who underwent surgery during lockdown and 'stay alert' phase and pre‐COVID from April 2019 to March 2020.
Fig. S1. Surgical volume at the Specialist Centre for Kidney Cancer in 2019, subdivided into procedure and surgical approach.
Fig. S2. Breakdown of small renal masses (cT1a tumours) presented at the specialist multidisciplinary team meeting during the lockdown and subsequent treatment decisions.
Fig. S3. (a and b) Monthly surgeries per stage and condition (a) and type of intervention (b) at the Specialist Centre for Kidney Cancer from January 2019 until September 2020.
Fig. S4. Surgical interventions for kidney and upper tract cancer at the Royal Free (RFH) and Westmoreland Street (WMS) COVID‐protected site from 18 March until September 2020.
Fig. S5. Distribution of priority levels of patients who underwent surgery from 18 March until 30 September 2020 in numbers per month.
Fig. S6. Threats and actions at the Specialist Centre for Kidney Cancer during the pandemic.


