On March 12th 2021 the Italian Government decided to implement a national lockdown in almost all the regions of the country. It was the second most severe measure taken after the March 2020 national lockdown, due to the rising of coronavirus disease 2019 (COVID‐19) cases and the overcrowding of the hospitals. Italy was the first European country hit by the COVID‐19 pandemic in February 2020. The first ‘red’ zones under severe lockdown in the Regions of Northern Italy were established on February 26th 2020, when all the schools were closed. Phase I of a nationwide lockdown began on March 8th and lasted until April 30th 2020. The Regions of Northern Italy were the most impacted by the COVID‐19 pandemic in the first months of 2020, with the highest incidence of COVID‐19 cases, leading to a dramatic surge in the need for emergency rooms (ERs) and wards, and a high mortality rate. 1 The first peak of 29 000 hospitalised individuals, including children, except those in intensive care units (ICUs) was recorded in April 2020. Most hospitals had to rapidly implement strategies to ensure care for non‐COVID‐19 patients. 2 The majority of children with sickle cell disease (SCD) live in the Northern regions of Italy. 3 Therefore, the dramatic scenario represented an opportunity to explore the challenges presented for children with SCD who lived in Italy during the first outbreak, so that the lessons learned could be used to guide clinical management in the upcoming months.
SCD is characterised by the presence of unpredictable and frequent acute events such as painful vaso‐occlusive crises (VOCs), acute chest syndrome (ACS) and febrile episodes with risk of severe infections. 4 VOCs, ACS and fever are the most frequent reasons for access to the ER and for hospitalisation. In previous years, data from the Network of Centres belonging to the Italian Association of Paediatric Haematology and Oncology [Associazione Italiana di Ematologia e Oncologia Pediatrica (AIEOP)] showed a high frequency of access to the ER and admission to hospital for VOCs, ACS and fever for children with SCD living in Italy during the coldest months, due to the trigger of seasonal infections (January–March). 3 , 5 , 6
The viral pandemic and the presence of febrile respiratory tract symptoms characteristic of the COVID‐19 infection suggested a greater risk of acute events in children with SCD. Several reports have focussed on service provision to children with SCD 7 or the clinical manifestations of COVID‐19 infection in children with SCD, 8 , 9 but to date, less information is available on the burden of acute events in children with SCD during the COVID‐19 pandemic.
The primary aim of the present multicentre retrospective study was to evaluate acute disease burden for children with SCD in Italy, measured as acute events (VOCs, ACS, fever), accesses to the ER and hospitalisations during the national lockdown of the first wave (21 February–30 April 2020), in which the same restrictive measures were applied homogeneously nationwide, compared to the same period in 2019. The secondary aim was to assess if the care provided to manage acute events had to be modified from the best practices recommended by the AIEOP National Guidelines due to the pandemic. 10
A standardised survey in Excel (Data S1) was sent to the AIEOP Centres. Summary data were collected from individual chart review, or through specific queries in health databases, according to the usual practices in place in each centre. Fisher’s exact test was used to compare dichotomous data or low frequencies and Pearson chi‐square test for analysing associations.
A total of 839 patients (male 419 and female 420) with SCD (63% SS, 10% Sβ°, 17% SC, 8% Sβ+, 2% other) were followed in 22 AIEOP Centres at the time of the survey in 2020; 782 were followed in 2019 (62% SS, 10% Sβ°, 17% SC, 8% Sβ+, 3% other). Overall, 721/839 (86%) and 671/782 (86%) were living in the Northern regions of Italy in 2020 and 2019 respectively.
In 2020, overall, there was a significant reduction in ER access compared to the previous year (43% vs. 73%, −40%; P = 0·001) with no differences in the three areas (Northern, Central, Southern) of the country. Hospitalisations also decreased (55% vs. 77%, −30%; P = 0·025), but the majority of the reduction occurred in the Northern Regions that were most impacted by the pandemic (P = 0·016) (Fig 1). Considering the causes of hospitalisation, admissions due to VOCs, ACS and fever were reduced overall, but those due to other causes (haemolytic crises/seizures/other) remained unchanged (Fig 2). No deaths occurred.
Fig 1.
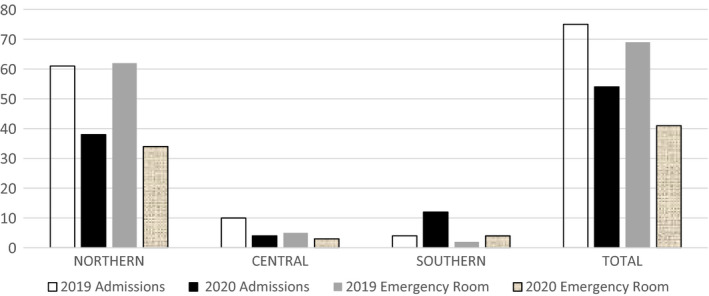
Inpatient admission and emergency room (ER) visits for acute events in children with sickle cell disease during the first national lockdown in Italy, showing a significant reduction in the number of admissions and ER visits overall (P = 0·025 and P = 0·001 respectively), but with uneven distribution in the country, with the majority of reductions occurring in Northern Italy (P = 0·016).
Fig 2.
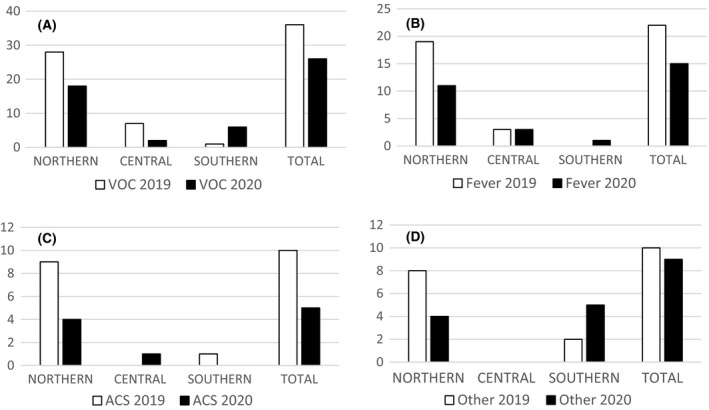
Causes of inpatient admissions for children with sickle cell disease during the first national lockdown in Italy, showing significant reduction in the number of vaso‐occlusive crisis (VOCs) (A), acute chest syndrome (ACS) (B) and fever admissions (C), especially in Northern Italy, but not in admissions for other reasons (aplastic crisis, acute haemolytic anaemia, splenic sequestration) (D).
In Italy, surprisingly, compared to all other European countries, 8 , 9 there were no positive cases of COVID‐19 in children with SCD during the first national lockdown, despite the very high number of COVID‐19‐positive cases in the general population, including children. 1 Moreover, unlike other European countries, 8 , 9 children with SCD had fewer accesses for acute events than are typical of SCD and they did not present serious acute events or deaths at home due to delayed treatment, or a lack of adequate care. In fact, between February and April 2020, only one of the 22 AIEOP expert centres implemented alternative pathways for fever management, suggesting that children with SCD should not come to the ER in cases of fever >38°C, but should remain at home and start oral antibiotic, in contrast to pre‐existing AIEOP guidelines. The other 21 centres continued to follow the usual AIEOP guidelines for fever, VOCs and ACS and advised patients and families to comply with the usual protocols. 10 Therefore, it is unlikely that the reduction of VOCs was due to more home pain management, although our survey was not designed to specifically assess consumption of pain medication at home. Most of the centres made organisational changes and established ad hoc ‘dirty/clean’ paths within the ER, nevertheless ensuring adequate access and management for the acute complications of SCD. All centres implemented telephone surveillance and when in good health, routine clinical laboratory checks were postponed. In some centres, chronic organ damage monitoring (including Transcranial Doppler) was delayed, and exchange transfusion sessions sometimes were rescheduled with a maximum delay of 4 weeks, without any impact on acute manifestations, or short‐term survival.
In Italy, in general, children experienced reduced access to the ER during the pandemic with short‐term worsening of underlying chronic conditions, delayed diagnosis, or increased severity of clinical manifestations upon admission. 11 , 12 , 13 This does not appear to be the case for children with SCD. Reduced access to ER services for the typical acute manifestations of SCD was not due to a barrier, but to a reduction of the clinical complications themselves. This could be due to several reasons. First of all, the general situation in Italy, with sudden widespread COVID‐19 fear prompted the entire population to stay at home and limit contacts. Parents, teenagers and children with SCD, immediately and willingly, complied with isolation measures with reduced opportunity to be infected by COVID‐19. 14 Secondly, the widely adopted infection containment measures, such as masks or social distancing, combined with early school closure, reduced the diffusion of seasonal infections (a known trigger for VOCs and ACS in children with SCD), the access to the ER for blood analysis and intravenous antibiotics administration in case of fever >38°C and hospitalisation for ACS. Finally, the prompt reorganisation of care for patients with SCD by telephone and long‐distance surveillance played a key role in encouraging patients and families to remain at home. 14
The above reasons were taken into consideration to plan care management, including acute events, during the successive waves of the pandemic, characterised by heterogeneous activation of lockdowns in various areas of the country up to March 12th 2021. The frequency and severity of acute complications during other periods, in which the restrictive measures were looser and heterogeneous, due to a lower infection rate, are still to be determined. At the beginning of the second national lockdown, in order to continue to guarantee a low incidence of the acute manifestations of SCD in the following months in which ERs and hospitals could continue to be overburdened, adequate telephone surveillance, maintaining the necessary access to ER for acute emergencies and reduced contacts are recommended. Our present survey has confirmed that infections are the most frequent trigger of morbidity in patients with SCD, especially in the paediatric age group and infection prevention measures can effectively limit acute events. The overall consumption of pain medication will need further evaluation.
Author contributions
Vania Munaretto, Laura Sainati, Raffaella Colombatti, Giovanni Palazzi, Giovanna Russo designed the study and drafted the manuscript; Beatrice Coppadoro performed statistical analysis; all authors reviewed the abstract; all authors contributed to data collection, data interpretation.
Supporting information
Data S1. 2019 and 2020 survey.
Acknowledgements
The research was partially supported by a grant from the Fondazione Città della Speranza.
References
- 1. Megna R. First month of the epidemic caused by COVID‐19 in Italy: current status and real‐time outbreak development forecast. Glob Health Res Policy. 2020;5:43;eCollection 2020. https://ghrp.biomedcentral.com/articles/10.1186/s41256‐020‐00170‐3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sainati L, Biffi A. How we deal with the COVID‐19 epidemic in an Italian paediatric onco‐haematology clinic located in a region with a high density of cases. Br J Haemathol. 2020;189:640–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Colombatti R, Palazzi G, Masera N, Notarangelo LD, Bonetti E, Samperi P, et al. Hydroxyurea prescription, availability and use for children with sickle cell disease in Italy: results of a National Multicenter survey. Pediatr Blood Cancer. 2018;65:e26774 [DOI] [PubMed] [Google Scholar]
- 4. Piel FB, Steinberg MH, Rees DC. Sickle cell disease. N Engl J Med. 2017;376:1561–73. [DOI] [PubMed] [Google Scholar]
- 5. Po’ C, Colombatti R, Cirigliano A, Dalt LD, Agosto C, Benini F, et al. The management of sickle cell pain in the emergency department: a priority for health systems. Clin J Pain. 2013;29:60–3. [DOI] [PubMed] [Google Scholar]
- 6. Munaretto V, Colombatti R, Tripodi SI, Paola C, Cesaro S, Arcioni F, et al. Acute chest syndrome in children with sickle cell disease in Italy: results of a national survey from the Italian association of pediatric hematology oncology (AIEOP). Blood. 2019;134(Suppl 1):2301. [Google Scholar]
- 7. Roy NB, Telfer P, Eleftheriou P, de la Fuente J, Drasar E, Shah F, et al. Protecting vulnerable patients with inherited anaemias from unnecessary death during the COVID‐19 pandemic. Br J Haematol. 2020;189:635–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Arlet JB, de Luna G, Khimoud D, Odièvre MH, de Montalembert M, Joseph L, et al. Prognosis of patients with sickle cell disease and COVID‐19: a French experience. Lancet Haematol. 2020;7:e632–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Appiah‐Kubi A, Acharya S, Fein Levy C, Vlachos A, Ostovar G, Murphy K, et al. Varying presentations and favourable outcomes of COVID‐19 infection in children and young adults with sickle cell disease: an additional case series with comparisons to published cases. Br J Haematol. 2020;190:e221–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Colombatti R, Perrotta S, Samperi P, Casale M, Masera N, Palazzi G, et al. Organizing national responses for rare blood disorders: the Italian experience with sickle cell disease in childhood. Orphanet J Rare Dis. 2013;8:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID‐19. Lancet Child Adolesc Health. 2020;4:e10–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ferraro VA, Zamunaro A, Spaggiari S, Di Riso D, Zanconato S, Carraro S. Pediatric asthma control during the COVID‐19 pandemic. Immun Inflamm Dis. 2021 (Online ahead of print). DOI: 10.1002/iid3.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lubrano R, Villani A, Berrettini S, Caione P, Chiara A, Costantino A, et al. Point of view of the Italians pediatric scientific societies about the pediatric care during the COVID‐19 lockdown: what has changed and future prospects for restarting. Ital J Pediatr. 2020;46:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Perdibon M, Munaretto V, Maran E, Marin C, Biffi A, Colombatti R, Sainati L. Psychological effects of isolation during the COVID‐19 pandemic on caregivers and patients with sickle cell disease in Northern Italy: a qualitative analysis. HemaSphere, 2020;4:S3, 15th Annual Sickle Cell and Thalassaemia, 1st EHA European Sickle Cell Conference, and 60th Anniversary of BSH Abstract Book, 10.1097/HS9.000000000000049 [DOI]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. 2019 and 2020 survey.


