Abstract
Many psychosocial factors have been implicated in the onset and escalation of substance use in adolescence and young adulthood. Typically, each factor explains a small amount of the variance in substance use outcomes, and effects are typically applied across a broad range of ages or computed from cross-sectional data. The current study evaluated the association of factors including social influence (e.g., peer substance use), cognitive features (e.g., alcohol expectancies), and personality and emotional characteristics (e.g., impulsivity and typical responses to stress) in substance use throughout adolescence and emerging adulthood (ages 13-25; N = 798). Mixed-effects models tailored for the accelerated longitudinal design employed in this study were constructed with psychosocial and developmental factors predicting alcohol and cannabis use. As most participants in the sample exhibited little or no substance use at baseline by design, we excluded baseline assessments and examined data from follow-up years 1, 2, 3, and 4. Interactions between age cohort, change in age, and psychosocial predictors of substance use revealed differing associations over the developmental window for alcohol and cannabis use. For example, positive alcohol expectancies and sensation seeking were most strongly associated with greater drinking after age 18, whereas sensation seeking was associated with increased cannabis use as early as age 15. Higher emotion regulation skills led to less cannabis use in younger ages (i.e., shallower slopes below age 17), but this protective effect diminished after age 17. Results highlight developmentally important factors that differentially contribute to substance use in adolescence and young adulthood. We also demonstrate the importance of developmentally sensitive analyses that maximize the value of data from accelerated longitudinal designs.
Keywords: adolescence, substance use, coping, impulsivity
Investigations of adolescence and emerging adulthood have highlighted the multifaceted developmental changes that occur across levels of assessment, from the biological to the sociocultural. Physical maturation triggered by the onset of puberty occurs concurrently with social changes associated with increased independence from parents and family along with the emergence and eventual stabilizing of personality traits and emotional functioning. The trajectory of development through this critical period of growth is not always linear and environmental perturbations may disrupt or alter development. Biological changes in adolescence with the onset of puberty tend to orient motivational goals more toward social interactions highlighted by sensation-seeking and intensification of peer influences (Forbes & Dahl, 2010). Thus, underlying biological changes serve as the basis for the dramatic shifts in functional roles and responsibilities for adolescents and young adults, or “emerging adults” – from the development of physical and cognitive capabilities needed for assuming more adult roles, to the establishment of personal values and identity (Arnett et al., 2014).
The use of alcohol and other substances is a common experience for adolescents and young adults and has the potential to alter the course of development and eventual endpoints in adulthood (Callas et al., 2004; Costanzo et al., 2007). The onset of substance use in adolescence and early adulthood typically begins with experimentation and exploration of substance effects, and problematic use occurs with recurrent exposure. Epidemiological data indicates that the prevalence of alcohol use disorders peaks between ages 18-25 years old (SAMHSA, 2015), indicating that young adults may be at greater risk for problematic alcohol use. Better characterizing factors associated with initial use experiences as well as those associated with more recurrent use through this developmental period would help facilitate the development of targeted prevention and intervention strategies.
Managing social, cognitive, and emotional changes during adolescence pose challenges as youth begin to develop more flexible goals adapted for uncertain and changing environments and learn to navigate competing desires (Blakemore & Choudhury, 2006; Choudhury et al., 2006; Crone & Dahl, 2012). With age, adolescents develop richer understandings of adult-like behaviors and become more sensitive to social cues and pressures (Blakemore, 2018; Fuhrmann et al., 2015). Amidst these substantial social and emotional changes, brain development continues to both reflect and influence environmental factors including socioeconomic status, peer influences, and risk-taking behavior (Foulkes & Blakemore, 2018; van Duijvenvoorde et al., 2014; Van Leijenhorst et al., 2010). Social and emotional engagement increase as does sensitivity to social cues which may both serve a developmental purpose in supporting independence and carry a very real risk as evidenced by the increase of peer influence on substance use (Zucker et al., 2008). Furthermore, the nature of peer and other psychosocial influence varies from younger (Windle et al., 2008) to older adolescents (Brown et al., 2008).
Self-regulation, or the ability to control and plan behaviors, is one of the primary skills developed during adolescence and into early adulthood (Brown et al., 2008). Self-regulation includes the ability to resist impulses that may favor immediate over longer term rewards and that may put one at risk for negative consequences. A predisposition for risk-taking behavior exists in adolescence (Chein et al., 2011; Steinberg, 2007), yet self-regulation of emotion and behavior mature during this period, and the emergence of adaptive patterns of coping with negative emotions may be a key protective factor minimizing the use of substances as a coping strategy (Siegel, 2015; Veilleux et al., 2014).
In addition to cognitive control, adolescents begin to develop associations and cognitive appraisals of alcohol use, represented as alcohol expectancies. More positive expectancies have been shown to precede earlier initiation of alcohol use and are associated with a greater number of drinks consumed per drinking episode, higher frequency of drinking occasions, and frequency of getting drunk (Darkes et al., 2004; Goldman, 2002). During adolescence, alcohol expectancies tend to shift toward more positive and fewer negative associations, and earlier shifts have been correlated with more drinking (Anderson et al., 2011; Bekman et al., 2011). Indeed, an earlier report from our group affirmed peer and positive alcohol expectancy effects on binge drinking for the first two years of the National Consortium on Alcohol and NeuroDevelopment in Adolescence (NCANDA) sample (Boyd et al., 2018).
Current Study
While many studies have highlighted the influence of psychosocial factors on the initiation and increasing recurrence of alcohol consumption and other substance use, only largescale longitudinal studies have the ability to identify the dynamic interplay of various risk and protective factors. The NCANDA sample annually reported substance use as well as several domains of psychosocial functioning. As participants were recruited across adolescence through early adulthood and then followed over annual assessments (i.e., 13-26 years old in the current study), we can leverage this accelerated longitudinal design to examine the effects of psychosocial factors within individuals and as they shift across this developmental period in which initiation and escalation of substance use is most pronounced. Thus, we examined how changes in psychosocial variables are related to substance use across adolescence and young adulthood and sought to identify sensitive developmental periods in which particular psychosocial factors are most influential in substance use outcomes. We expected that psychosocial factors such as alcohol expectancies, impulsivity, and peer substance use would be related to increased substance use, based on prior literature. Furthermore, we predicted that having increased coping strategies in response to stress would be related to decreased substance use. We expected that effects of individual factors would differ across the developmental window, with some factors having greater influence earlier in development and others exerting stronger influence later in development, and our study is uniquely designed to be able to parse out these dynamic differences over time.
Method
Participants
The NCANDA study employs an accelerated longitudinal design to follow adolescents (age 12 to 21 at baseline) annually for up to nine years. A total of 831 healthy adolescents were recruited from the local communities and enrolled across five sites in the United States (University of California, San Diego, SRI International, Duke University Medical Center, University of Pittsburgh, and Oregon Health & Science University). Participants provided consent or assent based on age, and parental consent was acquired for participants under age 18. The study was approved by the IRB of each of the five sites. The majority of participants enrolled had no history of heavy drinking and a limited exposure to alcohol and other drugs at project entry (N = 692) and a portion were allowed to have some experience with substances to increase the ability to detect varying trajectories of substance use over time. The primary goals of the study are to elucidate neurodevelopmental trajectories as they relate to alcohol and other substance use (Brown et al., 2015; Pfefferbaum et al., 2018; Sullivan et al., 2016).
Additional exclusionary criteria at baseline included: a current diagnosis of severe psychiatric disorders (e.g., schizophrenia, bipolar disorder) that would interfere with valid completion of the protocol, substance dependence, current use of psychoactive medication, serious medical problems, intellectual disability or pervasive developmental disorder, lack of fluency in English, uncorrected sensory impairment, and known prenatal drug or alcohol exposure (for a full description of the recruitment and retention methods, see Brown et al., 2015). All enrolled participants were followed annually, regardless of substance use patterns during the follow-up years. To address the bias introduced at the baseline assessment when participants were required to report no or minimal substance use, this time point was not incorporated into the current analyses. Rather, data reported here were collected at the second through fifth annual assessments of the NCANDA project (i.e., follow-up years 1, 2, 3, and 4) to ensure inclusion of natural variation in substance use outcomes. Participants who met inclusion criteria and had valid substance use and psychosocial data for at least one of these four follow-up assessments were included in the analyses (N = 798 unique participants, 49% female; see Table 1 for details by assessment year).
Table 1.
Participant sex and age for four years of observations included in current report
| Female | Male | Total | Mean Age | Age Range | |
|---|---|---|---|---|---|
| Year 1 | 382 | 392 | 774 | 16.7 | 12.9-22.9 |
| Year 2 | 361 | 368 | 729 | 17.7 | 14.0-23.8 |
| Year 3 | 343 | 361 | 704 | 18.7 | 14.9-24.8 |
| Year 4 | 328 | 329 | 657 | 19.7 | 16.0-25.8 |
Measures
At each follow-up assessment point, the Customary Drinking and Drug Record (Brown et al., 1998) was administered to obtain quantity and frequency of lifetime and recent (past year) alcohol, cannabis, and other drug use, and withdrawal/hangover symptoms. The primary substance use metrics used for the current analyses were past year alcohol use days and past year cannabis use days. Family history of alcohol use disorders (FH Alc) was also assessed annually (Rice et al., 1995), summarized with a density score in which positive endorsements for biological parents count as 1 and for biological grandparents count as 0.5, yielding a score between 0-4. FH Alc is theoretically a stable trait, though endorsement may emerge over time; therefore, FH Alc at Year 4 was used here as a static predictor.
The Alcohol Expectancy Questionnaire (AEQ) was completed at each assessment (Brown et al., 1987). Participants indicated their agreement to 21 alcohol expectancy statements on a 5-point scale from 1 (strongly disagree) to 5 (strongly agree). An average of the 15 positive items indexing Positive Alcohol Expectancies (PAE) was used in the current study, as positive expectancies tend to have strongest relationships to drinking in adolescence (Bekman et al., 2011).
Several facets of impulsivity were measured using the short version of the UPPS-P Impulsive Behavior Scale (Cyders, 2013; Cyders et al., 2014; Lynam, 2006). Participants responded to 20 statements on a 1 (Agree strongly) to 4 (Disagree strongly) scale. Its five scales each reflect the average of four items in which higher scores reflect more impulsivity: Sensation Seeking (SS), Negative Urgency (NU), Lack of Premeditation (PSV), Lack of Perseverance (PSV), and Positive Urgency (PU). We chose a subset of these scales including PSV, NU, and SS in the current models based on prior research describing the influence of impulsivity traits on substance use outcomes (Johnson et al., 2017; McCarty et al., 2017; Sanchez-Roige et al., 2019; Whiteside & Lynam, 2003).
Peer alcohol and cannabis use were measured by individual items drawn from the Peer Group Deviance Scale (PGD; adapted from Bachman, Johnston, & O’Malley, 2011). Participants indicated the portion of their friends who engage in alcohol and cannabis use on a 5-point scale ranging from 0 (none) to 4 (all). The items used in the current study asked what proportion of their friends drink alcohol (PeerDrink) and use cannabis (PeerCan) as predictors of substance use (Curran et al., 1997).
Cognitive coping strategies employed to manage interpersonal stressors were measured using the Response to Stress Questionnaire (RSQ) (Connor-Smith et al., 2000). Participants rated how often they used each coping method or experienced each type of involuntary stress response, on a scale of 1 (Not at all) to 4 (A lot). The RSQ contains items to measure three types of coping and two types of involuntary stress responses, and, for the current study, two specific types of coping were considered, Cognitive Restructuring (CogRest) and Emotion Regulation (EmoReg), based on theories of the role of alcohol use in adolescents and young adults in coping with negative emotion (Siegel, 2015; Veilleux et al., 2014).
Procedure
Participants were invited to an in-person assessment annually. Assessment procedures were consistent across each study site and monitored annually for reliability (see Brown et al., 2015). Each visit includes a neuropsychological battery, neuroimaging session, and comprehensive assessment of substance use, urine and breath samples to confirm self-reported substance use, psychiatric symptoms and diagnoses, and functioning in major life domains. If participants were unable to complete the assessments in person (e.g., moved out of the area), interview and self-report data were collected via phone or self-administration (5-8% of sample at each assessment).
Data Analysis Plan
The accelerated longitudinal design of NCANDA allows for examining phenomena of interest across a wide developmental window, accounting for both between-person age effects and within-person change. To capture developmental influences, two age indices were included in all models: age cohort and change in age across observations. Age cohort (agem) was a continuous variable consisting of each participant’s mean age (M = 18.2 years; range: 12.9-25.8 years) and by design was static for each participant (i.e., each participant had one age cohort value across all four follow-up assessments). Age change (ageΔ) was computed as a participant’s current age minus agem (M = 0, range: −2.0–2.2). Two-way interactions between independent variables and agem reflect age cohort effects, two-way interactions with ageΔ reflect differences in longitudinal change (i.e., differences in slope), and three-way interactions of independent variables with agem and ageΔ reflect differences in longitudinal change as a function of age cohort (Thompson et al., 2011).
Mixed-effect models were constructed for the two primary substance use outcomes: past year alcohol use days and past year cannabis use days. Fixed effects were evaluated for each predictor and interaction and a random factor was entered for subject. Given the number of participants who did not endorse substance use at the follow-ups (see Figures 1a and 1b), a zero-inflated Poisson (ZIP) distribution was used for the substance use outcome variables. A ZIP model combines a Poisson component for amount of substance use with a logistic component that accounts for excess zeros beyond that which is predicted by a Poisson process (Loeys et al., 2012). The Bayesian Information Criterion (BIC) was examined for each model, though model comparisons were not an explicit goal of the current study. Models were deemed to fit sufficiently if they converged, based on the specifications included in the glmmTMB package which evaluate for data sparseness and will not converge if data are overly sparse (Brooks et al., 2017).
Figure 1.

Histogram of participants who endorsed: A) any alcohol use days in the past year, and B) any cannabis use days in the past year across 4 years of follow-up.
Note. Plots represent only participants who reported alcohol or cannabis use in the past year (i.e., non-users are excluded from the plots.
Independent variables were selected based on prior findings and with a goal of model parsimony with recognition that some variables would likely be correlated (see Table 2 and Supplementary Table S1). Models were first estimated for each combination of psychosocial factor (predictor) and substance use dimension (outcome); Each model was adjusted for sex (F = 0; M= 1) and FH Alc. This was followed by a model for each substance use outcome including multiple independent variables. Analyses were conducted in R Version 3.5.2, using the glmmTMB package with a ZIP distribution (Brooks et al., 2017).
Table 2.
Correlation matrix (Pearson) of predictors and substance use outcomes across all observations and time points
| Past Year Substance Use |
PAE | Peer Use | Coping Strategies | UPPS-P | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| age | FH Alc |
Alcohol days |
Cannabis Days |
Positive Expectancies |
PeerDrink | PeerCan | Cognitive Restructuring |
Emotion Regulation |
Sensation Seeking |
Negative Urgency |
Lack of Perseverance | |
| Age | -- | −0.01 | 0.37** | 0.12** | 0.13** | 0.48** | 0.22** | 0.02 | −0.01 | −0.08* | −0.09* | −0.09* |
| FH Alc | −0.01 | -- | −0.01 | 0.04 | 0.04 | 0.03 | 0.07 | 0.00 | −0.01 | 0.00 | 0.06* | 0.01 |
| Alcohol Days | 0.37** | −0.01 | -- | 0.29** | 0.23** | 0.45** | 0.33** | 0.01 | −0.03 | 0.07* | −0.02 | −0.02 |
| Cannabis Days | 0.12** | 0.04 | 0.29** | -- | 0.13** | 0.25** | 0.42** | −0.01 | −0.08* | 0.11** | 0.05 | 0.03 |
| PAE | 0.13** | 0.04 | 0.23** | 0.13** | -- | 0.32** | 0.27** | 0.05 | −0.04 | 0.14** | 0.19** | 0.07* |
| PeerDrink | 0.48** | 0.03 | 0.45** | 0.25** | 0.32** | -- | 0.71** | 0.03 | −0.02 | 0.12** | 0.02 | 0.02 |
| PeerCan | 0.22** | 0.07 | 0.33** | 0.42** | 0.27** | 0.71** | -- | 0.04 | −0.05 | 0.17** | 0.11** | 0.05 |
| Cog. Rest. | 0.02 | 0.00 | 0.04 | 0.02 | 0.05 | 0.03 | 0.04 | -- | 0.51** | 0.11** | −0.07* | −0.12** |
| Emo. Reg. | −0.01 | −0.01 | −0.03 | −0.08** | −0.04 | −0.02 | −0.05 | 0.51** | -- | 0.04 | −0.09* | −0.20** |
| SS | −0.08* | 0.00 | 0.07* | 0.11** | 0.14** | 0.12** | 0.17** | 0.11** | 0.04 | -- | 0.15** | 0.09* |
| NU | −0.09* | 0.06* | −0.02 | 0.05 | 0.19** | 0.02 | 0.11** | −0.07* | −0.09** | 0.15** | -- | 0.12** |
| PSV | −0.09* | 0.01 | −0.02 | 0.03 | 0.07* | 0.02 | 0.05 | −0.12** | −0.20** | 0.09* | 0.12** | -- |
Note. PAE = Positive Alcohol Expectancy Scale; Peer Drink = Proportion of peers who drink; PeerCan = Proportion of peers who use cannabis; SS = Sensation Seeking; NU = Negative Urgency; PSV = Lack of Perseverance; FH Alc = Density of family history of alcohol use disorders
p < .01
p < .001.
Results
Follow-up rates for the current study were: Year 1: 95%; Year 2: 90%; Year 3: 86%; Year 4: 82% (see Table 1) and the sex distribution was relatively stable over time. The majority of participants reported no alcohol drinking days or cannabis use days at Year 1, but substance use increased over time with nearly half of those who were non-drinkers at Year 1 having initiated drinking by Year 4 (see Figure 1A). Similarly, cannabis use increased over the 4-year period, with about 25% of non-users at Year 1 reporting cannabis use by Year 4 (Figure 1B; Supplementary Figure S1). Twenty-nine percent of the sample reported at least one first or second degree relative (i.e., parent or grandparent) with an alcohol use disorder.
Psychosocial variables largely exhibited expected correlations with substance use measures based on prior literature (see Table 2) and were consistent across assessments or increased as expected (e.g., Peer substance use increases with age; Supplementary Tables S1 & S2). PAE and peer substance use (PeerDrink and PeerCan) were positively associated with alcohol and cannabis use days. UPPS-P scales were positively correlated to each other as were coping measures (CogRest and EmoReg), each exhibiting minimal association with substance use (Table S1).
Alcohol Use Days
Social Influences and Alcohol Use
PAE and PeerDrink both predicted increases in alcohol drinking days (Table 3a). PAE also exhibited a significant three-way interaction with age variables (BIC = 38368.70). Figure 2 depicts the effect of PAE on alcohol use. The interaction with age is reflected in increased associations with PAE and drinking days for older cohorts. Peer drinking, though only marginally significant in the three-way age interaction (Table 3a) exhibited a similar relationship with alcohol use days (Supplementary Figure S2), with a positive within person change in age and stronger associations in older cohorts.
Table 3a.
Model parameters from zero-inflated Poisson models predicting past year alcohol use with positive alcohol expectancies and peer drinking
| Alcohol Use Days in the Past Year | ||||
|---|---|---|---|---|
| Predictors | Estimate | SE | z | p |
| Count Model | ||||
| (Intercept) | 0.02 | 0.10 | 0.22 | .826 |
| ageΔ | 0.21 | 0.05 | 4.64 | <.001 |
| agem | 0.26 | 0.03 | 8.46 | <.001 |
| sex | 0.23 | 0.01 | 20.60 | <.001 |
| FH Alc | −0.17 | 0.01 | −13.37 | <.001 |
| PAE | 0.20 | 0.03 | 6.07 | <.001 |
| PeerDrink | 0.69 | 0.02 | 35.04 | <.001 |
| ageΔ * agem | 0.06 | 0.01 | 4.21 | <.001 |
| ageΔ * PAE | 0.09 | 0.01 | 6.20 | <.001 |
| agem * PAE | 0.00 | 0.01 | 0.36 | .718 |
| ageΔ * PeerDrink | −0.06 | 0.01 | −7.35 | <.001 |
| agem * PeerDrink | −0.02 | 0.01 | −2.99 | .003 |
| ageΔ * agem * PAE | −0.02 | 0.00 | −4.99 | <.001 |
| ageΔ * agem * PeerDrink | 0.00 | 0.00 | −1.72 | .085 |
| Zero-Inflated Model | ||||
| (Intercept) | 5.37 | 0.77 | 6.95 | <.001 |
| ageΔ | −0.54 | 0.40 | −1.35 | .176 |
| agem | −0.73 | 0.33 | −2.24 | .025 |
| sex | 0.09 | 0.26 | 0.34 | .736 |
| FH Alc | −0.45 | 0.29 | −1.55 | .122 |
| PAE | −0.94 | 0.28 | −3.36 | .001 |
| PeerDrink | −1.55 | 0.16 | −9.44 | <.001 |
| ageΔ * agem | −0.12 | 0.17 | −0.70 | .486 |
| ageΔ * PAE | −0.10 | 0.16 | −0.66 | .509 |
| agem * PAE | 0.00 | 0.12 | 0.00 | .997 |
| ageΔ * PeerDrink | −0.07 | 0.08 | −0.90 | .367 |
| agem * PeerDrink | 0.05 | 0.06 | 0.87 | .385 |
| ageΔ * agem * PAE | 0.03 | 0.07 | 0.52 | .601 |
| ageΔ * agem * PeerDrink | −0.02 | 0.04 | −0.48 | .634 |
Note. Zero-inflated portion reflects likelihood of being a “zero” (i.e., no drinking reported in the past year). ageΔ = Age Change; agem = Age Cohort; FH Alc = Family history density of alcohol use disorders; PAE = Positive Alcohol Expectancies; PeerDrink = Peers who drink alcohol
Figure 2.

Predicted Past Year Alcohol Use Days for High and Low Positive Alcohol Expectancies Across Age
Note. Plots of the predicted values of alcohol use days days for 25th and 75th percentile groups on Positive Alcohol Expectancies (PAE). Lines represent five hypothetical age cohorts across age change (note: age cohort lines are selected for visualization across the age range of the sample). Predicted values are scaled by the zero-inflated probability.
Facets of Impulsivity (UPPS-P) and Alcohol Use
The ZIP models revealed interaction effects with age for each of the UPPS-P scale predictors (Table 3b). SS, PSV, and NU each exhibit three-way interactions with age variables indicating differential associations of the predictors with substances use across the developmental window of the study (BIC = 50845.62). Figure 3 depicts the effects of SS on alcohol use days over age and identifies that those higher in SS exhibit a steeper increasing slope of alcohol use days after age 17. Taken along with the zero-inflation portion of the model (see Figure S3), findings suggest being older (increases in both agem and ageΔ), male, and endorsing higher levels of SS and NU make one more likely to drink in the past year.
Table 3b.
Model parameters from the zero-inflated Poisson models predicting past year alcohol use days with UPPS-P scales
| Alcohol Use Days in the Past Year | ||||
|---|---|---|---|---|
| Predictors | Estimate | SE | z | p |
| Count Model | ||||
| (Intercept) | 2.32 | 0.09 | 24.54 | <001 |
| ageΔ | 0.12 | 0.04 | 3.08 | .002 |
| agem | 0.14 | 0.03 | 5.12 | <001 |
| sex | 0.14 | 0.01 | 12.93 | <001 |
| FH Alc | −0.22 | 0.01 | −17.86 | <001 |
| SS | −0.03 | 0.02 | −1.30 | .192 |
| NU | 0.04 | 0.02 | 1.78 | .074 |
| PSV | 0.06 | 0.03 | 1.89 | .059 |
| ageΔ * agem | −0.10 | 0.01 | −7.71 | <001 |
| ageΔ * SS | 0.04 | 0.01 | 4.84 | <001 |
| agem * SS | 0.01 | 0.01 | 2.02 | .043 |
| ageΔ * NU | 0.07 | 0.01 | 7.61 | <001 |
| agem * NU | −0.03 | 0.01 | −4.70 | <001 |
| ageΔ * PSV | −0.03 | 0.01 | −2.29 | .022 |
| agem * PSV | 0.08 | 0.01 | 7.57 | <001 |
| ageΔ * agem * SS | 0.01 | 0.00 | 3.34 | .001 |
| ageΔ * agem * NU | 0.01 | 0.00 | 3.03 | .002 |
| ageΔ * agem * PSV | 0.02 | 0.00 | 3.61 | <001 |
| Zero-Inflated Model | ||||
| (Intercept) | 7.06 | 1.29 | 5.49 | <.001 |
| ageΔ | −1.82 | 0.58 | −3.15 | .002 |
| agem | −2.16 | 0.54 | −4.02 | <.001 |
| sex | 0.37 | 0.41 | 0.89 | .372 |
| FH Alc | −0.77 | 0.47 | −1.65 | .100 |
| SS | −0.87 | 0.29 | −3.01 | .003 |
| NU | −1.06 | 0.29 | −3.69 | <.001 |
| PSV | −0.55 | 0.37 | −1.47 | .143 |
| ageΔ* agem | 0.15 | 0.25 | 0.58 | .565 |
| ageΔ* SS | −0.38 | 0.14 | −2.69 | .007 |
| age_m * SS | −0.11 | 0.13 | −0.88 | .382 |
| ageΔ* NU | 0.43 | 0.14 | 2.96 | .003 |
| agem * NU | 0.32 | 0.12 | 2.60 | .009 |
| ageΔ* PSV | 0.08 | 0.20 | 0.38 | .702 |
| agem * PSV | 0.05 | 0.17 | 0.27 | .784 |
| ageΔ* agem * SS | 0.02 | 0.06 | 0.31 | .759 |
| ageΔ* agem * NU | −0.07 | 0.06 | −1.20 | .232 |
| ageΔ * agem * PSV | −0.01 | 0.09 | −0.13 | .897 |
Note. Zero-inflated portion reflects likelihood of being a “zero” (i.e., no drinking reported in the past year). ageΔ = Age Change; agem = Age Cohort; SS = Sensation Seeking; NU = Negative Urgency; PSV = Lack of Perseverance; FH Alc = Family history density of alcohol use disorders
Figure 3.
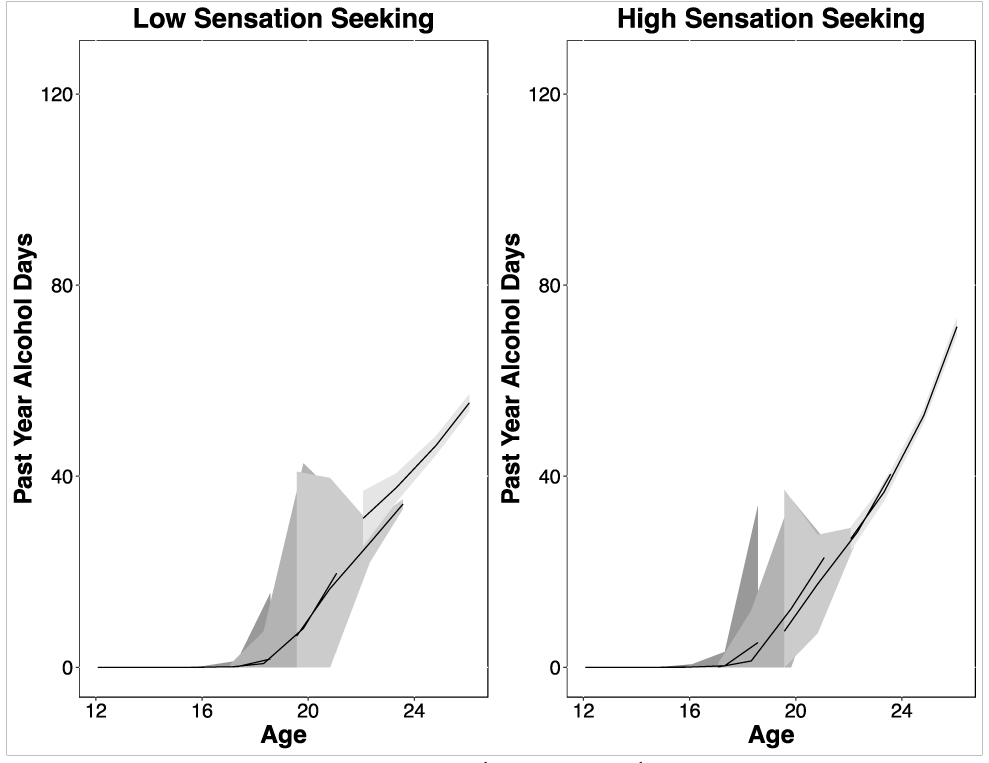
Predicted Past Year Alcohol Use Days for High and Low Sensation Seeking Across Age
Note. Plots of predicted alcohol use days for 25th (Low) and 75th (High) percentile groups on the UPPS-P Sensation Seeking scale with 95% confidence intervals. Lines represent five hypothetical age cohorts across age change (note: age cohort lines are selected for visualization across the age range of the sample). Predicted values are scaled by the zero-inflated probability, which accounts for the increase in standard error around the ages in which participants move from non-drinkers to drinkers (see Supplemental Figure S2).
Stress Responses and Alcohol Use
Endorsing the use of more cognitive restructuring techniques and more emotion regulation techniques when faced with interpersonal stressors (i.e., CogRest and EmoReg) was associated with fewer drinking days (Table 3c). EmoReg and CogRest exhibited three-way interactions with age (BIC = 51762.79). EmoReg specifically exhibited associations with age was most notable between ages 16-21 as participants aged (i.e., steeper slopes leading to higher consumption in low emotion regulation participants).
Table 3c.
Model parameters from zero-inflated Poisson models predicting past year alcohol use with coping strategies
| Alcohol Use Days in the Past Year | ||||
|---|---|---|---|---|
| Predictors | Estimate | SE | z | p |
| Count Model | ||||
| (Intercept) | 2.75 | 0.08 | 35.48 | <.001 |
| ageΔ | 0.20 | 0.03 | 5.96 | <.001 |
| agem | 0.16 | 0.02 | 6.77 | <.001 |
| sex | 0.18 | 0.01 | 17.25 | <.001 |
| FH Alc | −0.19 | 0.01 | −15.08 | <.001 |
| EmoReg | −0.08 | 0.03 | −2.60 | 0.009 |
| CogRest | −0.05 | 0.03 | −1.95 | 0.051 |
| ageΔ * agem | 0.05 | 0.01 | 4.61 | <.001 |
| ageΔ * EmoReg | −0.04 | 0.01 | −3.37 | 0.001 |
| agem * EmoReg | 0.10 | 0.01 | 10.09 | <.001 |
| ageΔ * CogRest | 0.09 | 0.01 | 7.98 | <.001 |
| agem * CogRest | −0.07 | 0.01 | −7.77 | <.001 |
| ageΔ * agem * EmoReg | −0.04 | 0.00 | −9.84 | <.001 |
| ageΔ * agem * CogRest | 0.02 | 0.00 | 4.03 | <.001 |
| Zero-Inflated Model | ||||
| (Intercept) | 1.84 | 0.97 | 1.90 | <.001 |
| ageΔ | −1.93 | 0.50 | −3.83 | .176 |
| agem | −2.26 | 0.45 | −4.98 | .025 |
| sex | 0.03 | 0.41 | 0.07 | .736 |
| FH Alc | −0.96 | 0.47 | −2.05 | .122 |
| EmoReg | −0.45 | 0.34 | −1.32 | .001 |
| CogRest | 0.40 | 0.29 | 1.41 | <.001 |
| ageΔ * agem | 0.28 | 0.22 | 1.26 | .486 |
| ageΔ * EmoReg | 0.24 | 0.19 | 1.29 | .509 |
| agem * EmoReg | 0.10 | 0.16 | 0.67 | .997 |
| ageΔ * CogRest | −0.18 | 0.15 | −1.16 | .367 |
| agem * CogRest | 0.09 | 0.13 | 0.70 | .385 |
| ageΔ * agem * EmoReg | 0.00 | 0.09 | −0.05 | .601 |
| ageΔ * agem * CogRest | −0.08 | 0.07 | −1.21 | .634 |
Note. Zero-inflated portion reflects likelihood of being a “zero” (i.e., no drinking reported in the past year). ageΔ = Age Change; agem = Age Cohort; FH Alc = Family history density of alcohol use disorders; EmoReg = Emotion Regulation Coping; CogRest = Cognitive Restructuring Coping
Combined Psychosocial Factors and Alcohol Use
When all the psychosocial predictors were simultaneously entered into the model the overall model did not converge, indicating a lack of power to parse the variance across a large number of three-way interactions. A more parsimonious model incorporating the strongest predictors from each of the earlier models (PSV, PAE, and EmoReg) corroborated results of the separate models with significant three-way interactions for each of the included predictors (see Supplementary Table S3; BIC = 48366.47). This model supports the robustness of the individual predictor domains in leading to dynamic variation in alcohol use days over the age range of the sample.
Cannabis Use
Social Influences and Cannabis Use
Peer cannabis use exhibited a significant positive association with cannabis use and also exhibited a three-way interaction with age such that higher peer use is associated with steeper slopes at earlier ages (Table 4a).
Table 4a.
Model parameters from zero-inflated Poisson models predicting past year cannabis use with Peer Cannabis Use
| Cannabis Use Days in the Past Year | ||||
|---|---|---|---|---|
| Predictors | Estimate | SE | z | p |
| Count Model | ||||
| (Intercept) | 0.62 | 0.04 | 14.02 | <.001 |
| ageΔ | 0.42 | 0.02 | 21.47 | <.001 |
| agem | 0.42 | 0.02 | 24.20 | <.001 |
| Sex | 0.51 | 0.01 | 49.50 | <.001 |
| FH Alc | 0.00 | 0.01 | −0.29 | .744 |
| PeerCan | 1.01 | 0.02 | 65.97 | <.001 |
| ageΔ* PeerCan | −0.06 | 0.01 | −7.96 | .226 |
| agem * PeerCan | −0.07 | 0.01 | −10.49 | <.001 |
| ageΔ* agem * PeerCan | −0.12 | 0.01 | −19.71 | <.001 |
| Zero-Inflated Model | ||||
| (Intercept) | 5.14 | 0.42 | 12.20 | <.001 |
| ageΔ | −0.27 | 0.15 | −1.80 | .072 |
| agem | −0.07 | 0.12 | −0.57 | .569 |
| Sex | −0.43 | 0.26 | −1.63 | .104 |
| FH Alc | −0.23 | 0.29 | −0.79 | .430 |
| PeerCan | −2.10 | 0.18 | −11.53 | <.001 |
| ageΔ* PeerCan | −0.03 | 0.06 | −0.52 | .606 |
| agem * PeerCan | −0.19 | 0.09 | −2.13 | .033 |
| ageΔ* agem * PeerCan | −0.15 | 0.07 | −2.05 | .041 |
Note. Zero-inflated portion reflects likelihood of being a “zero” (i.e., no drinking reported in the past year). ageΔ = Age Change; agem = Age Cohort; FH Alc = Family history density of alcohol use disorders; PeerCan = Peer Cannabis Use
Facets of Impulsivity (UPPS-P) and Cannabis Use
As with alcohol use, being male and older were associated with increases cannabis use when the facets of impulsivity were evaluated (Table 4b). There were main effects of NU and PSV, and all three scales exhibited three-way interactions with age indicating a dynamic influence of these facets of impulsivity across the age range. For example, Figure 4 depicts the predicted values of high and low sensation seeking on cannabis use, and reflects steeper slopes starting as early as age 15 and continuing throughout the age range of the study. The interaction reflects a minimal association of SS with cannabis use days at Year 1 (i.e., where ‘ageΔ’ = 0), but increasing influence as participants age (i.e., steeper slopes).
Table 4b.
Model parameters from zero-inflated Poisson models predicting past year cannabis use with UPPS-P factors
| Cannabis Use Days in the Past Year | ||||
|---|---|---|---|---|
| Predictors | Estimate | SE | z | p |
| Count Model | ||||
| (Intercept) | 2.76 | 0.08 | 35.36 | <.001 |
| ageΔ | −0.22 | 0.03 | −6.53 | <.001 |
| agem | 0.51 | 0.03 | 16.65 | <.001 |
| sex | 0.43 | 0.01 | 39.86 | <.001 |
| FH Alc | 0.12 | 0.01 | 12.27 | <.001 |
| SS | 0.00 | 0.02 | 0.28 | .777 |
| NU | −0.13 | 0.02 | −8.43 | <.001 |
| PSV | 0.29 | 0.02 | 13.03 | <.001 |
| ageΔ * agem | −0.05 | 0.01 | −4.18 | <.001 |
| ageΔ * SS | 0.11 | 0.01 | 14.85 | <.001 |
| agem * SS | 0.02 | 0.01 | 2.17 | .030 |
| ageΔ * NU | 0.08 | 0.01 | 11.70 | <.001 |
| agem * NU | 0.00 | 0.01 | 0.43 | .665 |
| ageΔ * PSV | 0.01 | 0.01 | 1.21 | .226 |
| agem * PSV | −0.25 | 0.01 | −25.07 | <.001 |
| ageΔ * agem * SS | −0.01 | 0.00 | −4.32 | <.001 |
| ageΔ * agem * NU | 0.02 | 0.00 | 6.21 | <.001 |
| ageΔ * agem * PSV | 0.04 | 0.00 | 9.50 | <.001 |
| Zero-Inflated Model | ||||
| (Intercept) | 9.12 | 1.13 | 8.06 | <.001 |
| ageΔ | −1.18 | 0.46 | −2.59 | .010 |
| agem | −0.30 | 0.44 | −0.68 | .496 |
| sex | −0.53 | 0.36 | −1.50 | .133 |
| FH Alc | −0.49 | 0.37 | −1.31 | .189 |
| SS | −0.70 | 0.24 | −2.88 | .004 |
| NU | −1.01 | 0.23 | −4.33 | <.001 |
| PSV | −0.88 | 0.32 | −2.73 | .006 |
| ageΔ * agem | 0.08 | 0.19 | 0.45 | .653 |
| ageΔ * SS | −0.08 | 0.10 | −0.79 | .430 |
| agem * SS | 0.01 | 0.11 | 0.14 | .890 |
| ageΔ * NU | −0.01 | 0.11 | −0.06 | .954 |
| agem * NU | −0.10 | 0.10 | −0.99 | .320 |
| ageΔ * PSV | 0.25 | 0.16 | 1.58 | .114 |
| agem * PSV | −0.15 | 0.14 | −1.05 | .293 |
| ageΔ * agem * SS | 0.01 | 0.05 | 0.24 | .814 |
| ageΔ * agem * NU | 0.02 | 0.05 | 0.49 | .623 |
| ageΔ * agem * PSV | 0.02 | 0.07 | 0.30 | .763 |
Note. Zero-inflated portion reflects likelihood of being a “zero” (i.e., no drinking reported in the past year). ageΔ = Age Change; agem = Age Cohort; SS = Sensation Seeking; NU = Negative Urgency; PSV = Lack of Perseverance; FH Alc = Family history density of alcohol use disorders
Figure 4.

Predicted Past Year Cannabis Use Days for High and Low Sensation Seeking Across Age
Note. Plots of the predicted values of cannabis use days for 25th (Low) and 75th (High) percentile groups on Sensation Seeking. Lines reprensent age cohorts over 4 assessments, and grey ribbons reflect 95% confidence intervals.
Stress Responses and Cannabis Use
Coping strategies reflected a curious association with cannabis use, as both CogRest and EmoReg exhibited significant relationships with cannabis use; however, EmoReg appears to be protective in that is it associated with fewer cannabis use days while CogRest was positively associated with cannabis use days (Table 4c). EmoReg exhibited a three-way interaction with age and higher levels appear to be associated with shallower slopes at earlier ages (15-19), but this effect diminishes at older ages (Figure 5). Furthermore, the probabilities from the zero-inflated portion of the model indicate that younger age cohorts show an increasing probability of becoming a cannabis user over time while cohorts over age 21 do not, which suggests that few participants begin using cannabis after age 21 if they haven’t already begun (Supplemental Figure S4).
Table 4c.
Model parameters from zero-inflated Poisson models predicting past year cannabis use with coping strategies
| Cannabis Use Days in the Past Year | ||||
|---|---|---|---|---|
| Predictors | Estimate | SE | z | p |
| Count Model | ||||
| (Intercept) | 3.82 | 0.05 | 70.10 | <.001 |
| ageΔ | 0.24 | 0.02 | 10.15 | <.001 |
| agem | 0.19 | 0.02 | 8.88 | <.001 |
| sex | 0.41 | 0.01 | 39.79 | <.001 |
| FH Alc | 0.12 | 0.01 | 12.23 | <.001 |
| CogRest | 0.31 | 0.02 | 17.95 | <.001 |
| EmoReg | −0.57 | 0.02 | −27.99 | <.001 |
| ageΔ * agem | −0.09 | 0.01 | −8.80 | <.001 |
| ageΔ * CogRest | −0.04 | 0.01 | −4.94 | <.001 |
| agem * CogRest | −0.04 | 0.01 | −5.09 | <.001 |
| ageΔ * EmoReg | 0.04 | 0.01 | 4.67 | <.001 |
| agem * EmoReg | 0.01 | 0.01 | 1.01 | 0.311 |
| ageΔ * agem * CogRest | 0.00 | 0.00 | 0.87 | 0.383 |
| ageΔ * agem * EmoReg | 0.04 | 0.00 | 9.00 | <.001 |
| Zero-Inflated Model | ||||
| (Intercept) | 3.77 | 0.84 | 4.46 | <.001 |
| ageΔ | −0.65 | 0.37 | −1.75 | .080 |
| agem | −0.45 | 0.33 | −1.37 | .171 |
| sex | −0.85 | 0.36 | −2.36 | .018 |
| FH Alc | −0.57 | 0.38 | −1.48 | .138 |
| CogRest | −0.07 | 0.25 | −0.28 | .776 |
| EmoReg | 0.09 | 0.29 | 0.30 | .768 |
| ageΔ * agem | 0.12 | 0.16 | 0.76 | .445 |
| ageΔ * CogRest | −0.11 | 0.12 | −0.88 | .378 |
| agem * CogRest | 0.04 | 0.11 | 0.40 | .691 |
| ageΔ * EmoReg | 0.02 | 0.15 | 0.12 | .902 |
| agem * EmoReg | −0.12 | 0.13 | −0.94 | .347 |
| ageΔ * agem * CogRest | −0.04 | 0.05 | −0.81 | .416 |
| ageΔ * agem * EmoReg | 0.07 | 0.06 | 1.04 | .080 |
Note. Zero-inflated portion reflects likelihood of being a “zero” (i.e., no drinking reported in the past year). ageΔ = Age Change; agem = Age Cohort; FH Alc = Family history density of alcohol use disorders; EmoReg = Emotion Regulation Coping; CogRest = Cognitive Restructuring Coping
Figure 5.
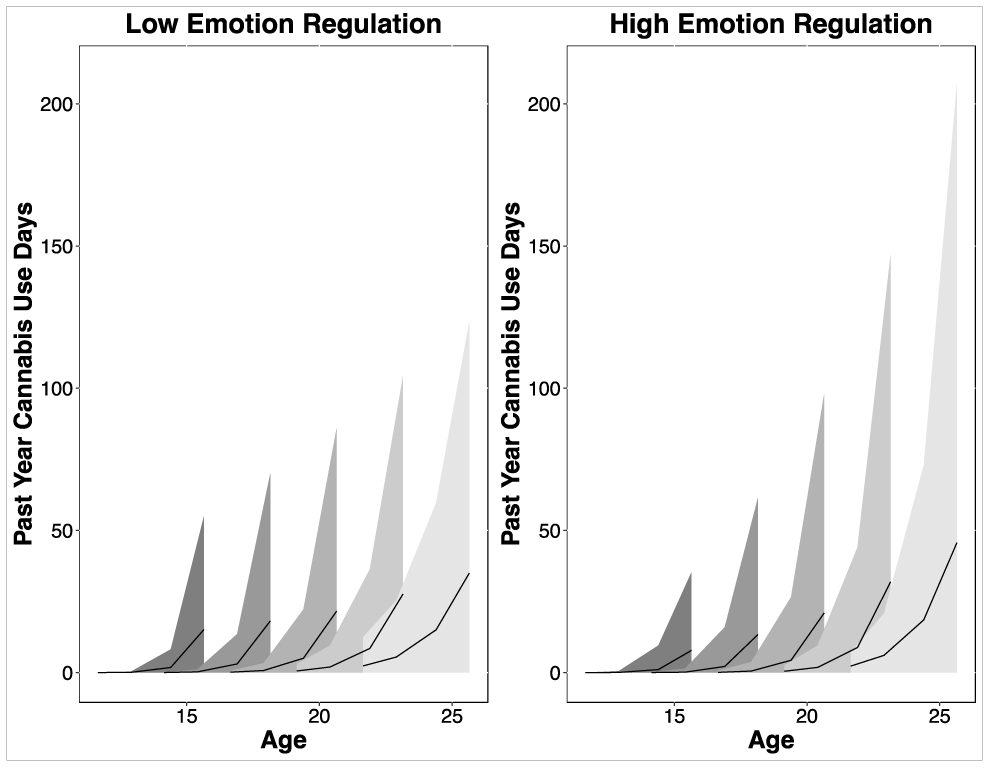
Predicted Past Year Cannabis Use Days for High and Low Emotion Regulation Across Age
Note. Plots of the predicted values of cannabis use days for 25th (Low) and 75th (High) percentile groups on Emotion Regulation coping strategies. Lines reprensent age cohorts over 4 assessments, and grey ribbons reflect 95% confidence intervals.
Combined Psychosocial Factors and Cannabis Use
As with models of alcohol use, a multivariate model with all variables did not converge. A focused multivariable model including the strongest associations from each constituent model (i.e., PSV, PeerCan, and EmoReg) was consistent with the results of the individual models with each predictor exhibiting a three-way interaction with age variables reflecting the dynamic influence of psychosocial variables on cannabis use over the age range of the sample (see Supplementary Table S4).
Discussion
The current report highlights significant psychosocial factors that vary widely during adolescence and young adulthood and contribute to substance use. The main findings replicate and extend many prior reports of social, cognitive, and emotional factors associated with substance use across adolescence and emerging adulthood (Bekman et al., 2011; Chassin et al., 2002; Hanson et al., 2014; Jester et al., 2015; Martin et al., 2002; Pieters et al., 2014). For example, sensation seeking has been associated with increased substance use in prior literature, but we highlight that in our sample the effect of higher sensation seeking appears to increase the number of alcohol use days after age 17 and on cannabis use days after age 15. Our results move beyond prior literature by identifying varying influence over development. For example, we show that coping skills are particularly important in decreasing alcohol use between 16-21 years old, but the effect of emotion regulation skills on alcohol use diminishes after age 21.
We also highlight the importance of utilizing longitudinal data to better understand the unfolding influences of psychosocial variables as adolescents mature. Our results reinforce the movement in substance use research to evaluate outcomes in the developmental context in which they occur (Chassin et al., 2013). By examining within person maturation over time, we were able to identify factors that alter trajectories of substance use across the age range of the sample. Furthermore, our results highlight risk factors associated with increases in substance use (e.g., sensation seeking, peer substance use, and positive expectancies) and protective factors (e.g., emotional coping strategies in the face of interpersonal stressors) that are dependent on the developmental status of youth.
We underscore numerous influences on substance use that go well beyond simple associations that are consistent across the entirety of adolescent development. For example, it is well established that several facets of impulsivity are associated with increased substance use (Whiteside & Lynam, 2003), but our sample clarifies that some facets of impulsivity (e.g., sensation seeking) may be more influential earlier in development for cannabis use, while it appears more influential for alcohol use after age 17. Such differences may reflect the environmental factors interacting with personality, in that our sample encompasses the transition period in which the behavior moves from an illegal to a legal behavior, for both alcohol and cannabis (in at least a portion of our sample that lives in states that have legalized cannabis use), and from abnormal to normative behavior. These influences may also reflect changes in the expectations and experience as proposed in Acquired Preparedness Models (McCarthy et al., 2001). These models posit that sensation seeking increases substance use initiation and positive expectancies coupled with impulsivity (e.g., urgency and lack of perseverance) facilitate sustained use later in adolescence and adulthood (Settles et al., 2010; Vangsness et al., 2005). Our study is one of the first that has been able to characterize the dynamic influence of risk and protective factors throughout adolescence in a longitudinal sample. Disentangling the role of psychosocial factors across a wide age range of a normally developing sample is critical to better characterizing risk for substance misuse and resulting problems in adolescence and young adulthood.
Despite the strengths of the large cohort sequential design several limitations exist in the current report. We did not predict particular substance use outcomes (e.g., onset of binge drinking or onset of alcohol use disorder criteria), but rather were looking at naturally escalating substance use patterns based on retrospective self-report data over the past year. Other reports from our study have focused (Boyd et al., 2018), and future reports could focus, on chronological predictions of particular variables and substance use outcomes. In addition, due to the complexity of the models aimed at examining the dynamic influence of psychosocial factors longitudinally, we examined predictors by domain which led to higher probability of Type I error. A single omnibus model testing the facets of psychosocial influences on alcohol use days is preferable, though the limits of our data and computing power restricted our ability to evaluate a model with all predictors in a single model. Additionally, the use patterns are somewhat similar to those of recent epidemiological reports (Johnston et al., 2018), but our sample still uses substances at relatively lower levels which limits the power we have to predict substance use outcomes with psychosocial variables.
These results lay the groundwork for further evaluation of psychosocial risk and protective factors influences on substance use in adolescence. Future studies will seek to connect many of the behavioral and cognitive traits assessed in the current study with underlying brain structure and function. A key benefit of the multimodal assessment in the NCANDA project is the potential to identify and evaluate hypotheses about mechanisms related to the onset and intensification of substance use over the course of development. When coupled with cross-lagged or chronological prediction models, we will be able to characterize directional and reciprocal cause and effects in substance use. Furthermore, we will be able to evaluate these risks in conjunction with changes in activities and emotional states using assessments that provide greater temporal and contextual specificity of use, as well as connecting these risk factors with other objective measures of behavior and cognition including neuropsychological functioning (Sullivan et al., 2016) and sleep (Baker et al., 2016; Hasler et al., 2017)
This study points the way toward greater specificity in prevention and early intervention efforts for alcohol and cannabis involvement in youth. In particular, the salience of individual risks across certain age ranges provides targets for intervention that may be more influential in arresting the progression into alcohol use and progression to regular drinking. In early adolescents, intervention goals are likely to remain focused on delaying initiation (Grant & Dawson, 1997; Hingson et al., 2006); however, in later adolescents and young adults, interventions may be oriented toward diminished heavy drinking with an emphasis on psychosocial factors (e.g., sensation seeking and emotional regulation skills) identified in the current study to be most influential in particular developmental windows (Carey et al., 2007; Marlatt & Witkiewitz, 2002; Tanner-Smith & Lipsey, 2015). Additionally, differential interventions may be necessary given distinct factors that influence cannabis use and alcohol use. Targeting age sensitive risk factors may be more effective in individual as well as public health interventions. For example, while the role of expectancies in alcohol use onset has been long known, the present study suggests that attention to these factors in prevention efforts during early adolescence may be more impactful. By contrast, public health messaging regarding alternative emotion-focused coping strategies may disrupt progression to more regular cannabis use among emerging adults, and perhaps should be targeted at teens and young adults before age 21, as our results indicate those who do not use cannabis by age 21 are less likely to move to cannabis use. While increased developmentally tailored content and format of early interventions have been recommended (Brown et al., 2008; Conrod et al., 2013), few studies have provided sufficient detail regarding the age-specific influence of risk factors to add direction to these efforts. Understanding the important features influencing use progression in the context of age may change the public health messages and increase the effectiveness of prevention and intervention efforts.
Supplementary Material
Highlights.
Psychosocial factors influence alcohol and cannabis use across adolescence
Positive alcohol expectancies and sensation seeking are associated with more drinking
Emotion regulation strategies exhibit protective effects and are associated with less substance use in adolescents
Longitudinal data highlight that psychosocial factors influence substance use differently across adolescence
Acknowledgements:
The authors would like to thank all members of the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA) who contributed to the data collection.
Role of Funding Sources:
This research was supported by grants from the U.S. National Institute on Alcohol Abuse and Alcoholism with co-funding from the National Institute on Drug Abuse, the National Institute of Mental Health, and the National Institute of Child Health and Human Development [NCANDA grant numbers: AA021697 (Multiple Principal Investigators (MPI), Drs. Pfefferbaum and Pohl), AA021695 (MPI, Drs. Brown and Tapert), AA021692 (PI, Dr. Tapert), AA021696 (MPI, Drs. Colrain and Baker), AA021681 (PI, Dr. De Bellis), AA021690 (PI, Dr. Clark), AA021691 (PI, Dr. Nagel)] and NIAAA R37 AA010723 (PI, Dr. Sullivan). Ancillary support was provided to T. Brumback through the National Institute of General Medical Science (P20 GM103436).
Footnotes
Conflicts of Interest:
All authors declare they have no conflicts of interest in this study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ty Brumback, Department of Psychological Science, Northern Kentucky University.
Wesley K. Thompson, Division of Biostatistics, Herbert Wertheim School of Public Health and Human Longevity Science, University of California, San Diego
Kevin Cummins, Department of Psychiatry, University of California, San Diego.
Sandra A. Brown, Departments of Psychology and Psychiatry, University of California, San Diego
Susan F. Tapert, Department of Psychiatry, University of California, San Diego.
References
- Anderson KG, Grunwald I, Bekman N, Brown SA, & Grant A (2011). To drink or not to drink: Motives and expectancies for use and nonuse in adolescence. Addictive Behaviors, 36(10), 972–979. 10.1016/j.addbeh.2011.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnett JJ, Žukauskienė R, & Sugimura K (2014). The new life stage of emerging adulthood at ages 18–29 years: implications for mental health. The Lancet Psychiatry, 1(7), 569–576. 10.1016/S2215-0366(14)00080-7 [DOI] [PubMed] [Google Scholar]
- Bachman JG, Johnston LD, & O'Malley PM (2011). Monitoring the Future: Questionnaire responses from the nation's high school seniors, 2010. [Google Scholar]
- Baker FC, Willoughby AR, Massimiliano d. Z., Franzen PL, Prouty D, Javitz H, Hasler B, Clark DB, & Colrain IM (2016). Age-related differences in sleep architecture and electroencephalogram in adolescents in the national consortium on alcohol and neurodevelopment in adolescence sample. Sleep, 39(7), 1429–1439. 10.5665/sleep.5978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekman NM, Anderson KG, Trim RS, Metrik J, Diulio AR, Myers MG, & Brown SA (2011). Thinking and drinking: alcohol-related cognitions across stages of adolescent alcohol involvement [Research Support, N.I.H., Extramural]. Psychology of Addictive Behavior, 25(3), 415–425. 10.1037/a0023302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakemore S-J (2018). Avoiding Social Risk in Adolescence. Current Directions in Psychological Science, 27(2), 116–122. 10.1177/0963721417738144 [DOI] [Google Scholar]
- Blakemore SJ, & Choudhury S (2006). Development of the adolescent brain: Implications for executive function and social cognition [Research Support, Non-U.S. Gov't Review]. Journal of Child Psychology and Psychiatry, 47(3-4), 296–312. 10.1111/j.1469-7610.2006.01611.x [DOI] [PubMed] [Google Scholar]
- Boyd SJ, Sceeles EM, Tapert SF, Brown SA, & Nagel BJ (2018). Reciprocal relations between positive alcohol expectancies and peer use on adolescent drinking: An accelerated autoregressive cross-lagged model using the NCANDA sample. Psychology of Addictive Behaviors, 32(5), 517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks M, Kristensen K, van Benthem K, Magnusson A, Berg C, Nielsen A, Skaug H, Maechler M, & Bolker B (2017). glmmTMB Balances Speed and Flexibility Among Packages for Zero-inflated Generalized Linear Mixed Modeling. The R Journal, 9(2), 378–400. https://journal.r-project.org/archive/2017/RJ-2017-066/index.html. [Google Scholar]
- Brown SA, Brumback T, Tomlinson K, Cummins K, Thompson WK, Nagel BJ, Bellis MDD, Hooper SR, Clark DB, Chung T, Hasler BP, Colrain IM, Baker FC, Prouty D, Pfefferbaum A, Sullivan EV, Pohl KM, Rohlfing T, Nichols BN, Chu W, & Tapert SF (2015). The National Consortium on Alcohol and NeuroDevelopment in Adolescence (NCANDA): A Multisite Study of Adolescent Development and Substance Use. Journal of Studies on Alcohol and Drugs, 76(6), 895–908. 10.15288/jsad.2015.76.895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, Christiansen BA, & Goldman MS (1987). The Alcohol Expectancy Questionnaire: An instrument for the assessment of adolescent and adult alcohol expectancies. Journal of Studies on Alcohol, 48(5), 483–491. [DOI] [PubMed] [Google Scholar]
- Brown SA, McGue M, Maggs J, Schulenberg J, Hingson R, Swartzwelder S, Martin C, Chung T, Tapert SF, Sher K, Winters KC, Lowman C, & Murphy S (2008). A Developmental Perspective on Alcohol and Youths 16 to 20 Years of Age. Pediatrics, 121(Supplement 4), S290–S310. 10.1542/peds.2007-2243D [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callas PW, Flynn BS, & Worden JK (2004). Potentially modifiable psychosocial factors associated with alcohol use during early adolescence. Addictive Behaviors, 29(8), 1503–1515. [DOI] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Carey MP, & DeMartini KS (2007). Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors, 32(11), 2469–2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L, Pitts SC, & Prost J (2002). Binge drinking trajectories from adolescence to emerging adulthood in a high-risk sample: Predictors and substance abuse outcomes. Journal of Consulting and Clinical Psychology, 70(1), 67–78. 10.1037/0022-006X.70.1.67 [DOI] [PubMed] [Google Scholar]
- Chassin L, Sher KJ, Hussong A, & Curran P (2013). The developmental psychopathology of alcohol use and alcohol disorders: Research achievements and future directions. Development and Psychopathology, 25(25th Anniversary Special Issue 4pt2), 1567–1584. 10.1017/S0954579413000771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chein J, Albert D, O’Brien L, Uckert K, & Steinberg L (2011). Peers increase adolescent risk taking by enhancing activity in the brain’s reward circuitry. Developmental Science, 14(2), F1–F10. 10.1111/j.1467-7687.2010.01035.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choudhury S, Blakemore SJ, & Charman T (2006). Social cognitive development during adolescence [Research Support, Non-U.S. Gov't]. Social Cognitive and Affective Neuroscience, 1(3), 165–174. 10.1093/scan/nsl024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, & Saltzman H (2000). Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology, 68(6), 976–992. [PubMed] [Google Scholar]
- Conrod PJ, O’Leary-Barrett M, Newton N, & et al. (2013). Effectiveness of a selective, personality-targeted prevention program for adolescent alcohol use and misuse: A cluster randomized controlled trial. JAMA Psychiatry, 70(3), 334–342. 10.1001/jamapsychiatry.2013.651 [DOI] [PubMed] [Google Scholar]
- Costanzo PR, Malone PS, Belsky D, Kertesz S, Pletcher M, & Sloan FA (2007). Longitudinal Differences in Alcohol Use in Early Adulthood. Journal of Studies on Alcohol and Drugs, 68(5), 727–737. 10.15288/jsad.2007.68.727 [DOI] [PubMed] [Google Scholar]
- Crone EA, & Dahl RE (2012). Understanding adolescence as a period of social-affective engagement and goal flexibility [ 10.1038/nrn3313]. Nature Reviews: Neuroscience, 13(9), 636–650. 10.1038/nrn3313 [DOI] [PubMed] [Google Scholar]
- Curran PJ, Stice E, & Chassin L (1997). The relation between adolescent alcohol use and peer alcohol use: A longitudinal random coefficients model. Journal of Consulting and Clinical Psychology, 65(1), 130–140. 10.1037/0022-006X.65.1.130 [DOI] [PubMed] [Google Scholar]
- Cyders MA (2013). Impulsivity and the Sexes: Measurement and Structural Invariance of the UPPS-P Impulsive Behavior Scale. Assessment, 20(1), 86–97. 10.1177/1073191111428762 [DOI] [PubMed] [Google Scholar]
- Cyders MA, Littlefield AK, Coffey S, & Karyadi KA (2014). Examination of a short English version of the UPPS-P Impulsive Behavior Scale. Addictive Behaviors, 39(9), 1372–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darkes J, Greenbaum PE, & Goldman MS (2004). Alcohol Expectancy Mediation of Biopsychosocial Risk: Complex Patterns of Mediation. Experimental and Clinical Psychopharmacology, 12(1), 27–38. 10.1037/1064-1297.12.1.27 [DOI] [PubMed] [Google Scholar]
- Forbes EE, & Dahl RE (2010). Pubertal development and behavior: Hormonal activation of social and motivational tendencies [Review]. Brain and Cognition, 72(1), 66–72. 10.1016/j.bandc.2009.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foulkes L, & Blakemore S-J (2018). Studying individual differences in human adolescent brain development. Nature neuroscience, 21(3), 315–323. 10.1038/s41593-018-0078-4 [DOI] [PubMed] [Google Scholar]
- Fuhrmann D, Knoll LJ, & Blakemore S-J (2015). Adolescence as a Sensitive Period of Brain Development. TRENDS in Cognitive Sciences, 19(10), 558–566. 10.1016/j.tics.2015.07.008 [DOI] [PubMed] [Google Scholar]
- Goldman MS (2002). Expectancy and risk for alcoholism: The unfortunate exploitation of a fundamental characteristic of neurobehavioral adaptation. Alcoholism: Clinical and Experimental Research, 26(5), 737–746. 10.1097/00000374-200205000-00021 [DOI] [PubMed] [Google Scholar]
- Grant BF, & Dawson DA (1997). Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: results from the National Longitudinal Alcohol Epidemiologic Survey. J Subst Abuse, 9, 103–110. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=9494942 [DOI] [PubMed] [Google Scholar]
- Hanson KL, Thayer RE, & Tapert SF (2014). Adolescent marijuana users have elevated risk-taking on the balloon analog risk task. Journal of Psychopharmacology, 28(11), 1080–1087. 10.1177/0269881114550352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasler BP, Franzen PL, de Zambotti M, Prouty D, Brown SA, Tapert SF, Pfefferbaum A, Pohl KM, Sullivan EV, & De Bellis MD (2017). Eveningness and later sleep timing are associated with greater risk for alcohol and marijuana use in adolescence: initial findings from the national consortium on alcohol and neurodevelopment in adolescence study. Alcoholism: Clinical and Experimental Research, 41(6), 1154–1165. 10.1111/acer.13401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, & Winter MR (2006). Age at drinking onset and alcohol dependence: Age at onset, duration, and severity. Archives of Pediatrics and Adolescent Medicine, 160(7), 739–746. [DOI] [PubMed] [Google Scholar]
- Jester JM, Wong MM, Cranford JA, Buu A, Fitzgerald HE, & Zucker RA (2015). Alcohol expectancies in childhood: change with the onset of drinking and ability to predict adolescent drunkenness and binge drinking. Addiction, 110(1), 71–79. 10.1111/add.12704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SL, Tharp JA, Peckham AD, Carver CS, & Haase CM (2017). A path model of different forms of impulsivity with externalizing and internalizing psychopathology: Towards greater specificity. British Journal of Clinical Psychology, 56(3), 235–252. 10.1111/bjc.12135 [Record #2029 is using a reference type undefined in this output style.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeys T, Moerkerke B, De Smet O, & Buysse A (2012). The analysis of zero-inflated count data: Beyond zero-inflated Poisson regression. British Journal of Mathematical and Statistical Psychology, 65(1), 163–180. 10.1111/j.2044-8317.2011.02031.x [Record #898 is using a reference type undefined in this output style.] [DOI] [PubMed] [Google Scholar]
- Marlatt GA, & Witkiewitz K (2002). Harm reduction approaches to alcohol use: Health promotion, prevention, and treatment. Addictive Behaviors, 27(6), 867–886. [DOI] [PubMed] [Google Scholar]
- Martin CA, Kelly TH, Rayens MK, Brogli BR, Brenzel A, Smith WJ, & Omar HA (2002). Sensation Seeking, Puberty, and Nicotine, Alcohol, and Marijuana Use in Adolescence. Journal of the American Academy of Child & Adolescent Psychiatry, 41(12), 1495–1502. http://www.sciencedirect.com/science/article/pii/S0890856709607450 [DOI] [PubMed] [Google Scholar]
- McCarthy DM, Kroll LS, & Smith GT (2001). Integrating disinhibition and learning risk for alcohol use. Experimental and Clinical Psychopharmacology, 9(4), 389–398. 10.1037/1064-1297.9.4.389 [DOI] [PubMed] [Google Scholar]
- McCarty KN, Morris DH, Hatz LE, & McCarthy DM (2017). Differential Associations of UPPS-P Impulsivity Traits With Alcohol Problems. Journal of Studies on Alcohol and Drugs, 78(4), 617–622. 10.15288/jsad.2017.78.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum A, Kwon D, Brumback T, Cummins WKTK, Tapert SF, Brown SA, Colrain IM, Baker FC, Prouty D, Clark MDDBDB, Chu BJNW, Park SH, Pohl KM, & Sullivan EV (2018). Altered Brain Developmental Trajectories in Adolescents After Initiating Drinking. American Journal of Psychiatry, 175(4), 370–380. 10.1176/appi.ajp.2017.17040469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieters S, Burk WJ, Van der Vorst H, Engels RCME, & Wiers RW (2014). Impulsive and reflective processes related to alcohol use in young adolescents [Original Research]. Frontiers in Psychiatry, 5. 10.3389/fpsyt.2014.00056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice JP, Reich T, Bucholz KK, Neuman RJ, Fishman R, Rochberg N, Hesselbrock VM, Nurnberger JI Jr., Schuckit MA, & Begleiter H (1995). Comparison of direct interview and family history diagnoses of alcohol dependence. Alcoholism Clin Exp Res, 19(4), 1018–1023. [DOI] [PubMed] [Google Scholar]
- SAMHSA. (2015). Behavioral Health Barometer, United States, 2014. http://www.samhsa.gov/data/sites/default/files/National_BHBarometer_2014/National_BHBarometer_2014.pdf [PubMed]
- Sanchez-Roige S, Fontanillas P, Elson SL, Gray JC, de Wit H, MacKillop J, & Palmer AA (2019). Genome-Wide Association Studies of Impulsive Personality Traits (BIS-11 and UPPS-P) and Drug Experimentation in up to 22,861 Adult Research Participants Identify Loci in the CACNA1I and CADM2 genes. The Journal of Neuroscience, 39(13), 2562–2572. 10.1523/jneurosci.2662-18.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Settles RF, Cyders M, & Smith GT (2010). Longitudinal validation of the acquired preparedness model of drinking risk. Psychology of Addictive Behavior, 24(2), 198–208. 10.1037/a0017631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel JP (2015). Emotional Regulation in Adolescent Substance Use Disorders: Rethinking Risk. Journal of Child & Adolescent Substance Abuse, 24(2), 67–79. 10.1080/1067828X.2012.761169 [DOI] [Google Scholar]
- Steinberg L (2007). Risk taking in adolescence. Current Directions in Psychological Science, 16(2), 55–59. 10.1111/j.1467-8721.2007.00475.x [DOI] [Google Scholar]
- Sullivan EV, Brumback T, Tapert SF, Fama R, Prouty D, Brown SA, Cummins K, Thompson WK, Colrain IM, Baker FC, De Bellis MD, Hooper SR, Clark DB, Chung T, Nagel BJ, Nichols BN, Rohlfing T, Chu W, Pohl KM, & Pfefferbaum A (2016). Cognitive, emotion control, and motor performance of adolescents in the NCANDA study: Contributions from alcohol consumption, age, sex, ethnicity, and family history of addiction. Neuropsychology, 30(4), 449–473. 10.1037/neu0000259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner-Smith EE, & Lipsey MW (2015). Brief Alcohol Interventions for Adolescents and Young Adults: A Systematic Review and Meta-Analysis. Journal of Substance Abuse Treatment, 51, 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson WK, Hallmayer J, & O'Hara R (2011). Design Considerations for Characterizing Psychiatric Trajectories Across the Lifespan: Application to Effects of APOE-ε4 on Cerebral Cortical Thickness in Alzheimer's Disease. American Journal of Psychiatry, 168(9), 894–903. 10.1176/appi.ajp.2011.10111690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Duijvenvoorde ACK, Op de Macks ZA, Overgaauw S, Gunther Moor B, Dahl RE, & Crone EA (2014). A cross-sectional and longitudinal analysis of reward-related brain activation: Effects of age, pubertal stage, and reward sensitivity. Brain and Cognition, 89, 3–14. 10.1016/j.bandc.2013.10.005 [DOI] [PubMed] [Google Scholar]
- Van Leijenhorst L, Moor BG, Op de Macks ZA, Rombouts SARB, Westenberg PM, & Crone EA (2010). Adolescent risky decision-making: Neurocognitive development of reward and control regions. Neuroimage, 51(1), 345–355. [DOI] [PubMed] [Google Scholar]
- Vangsness L, Bry BH, & LaBouvie EW (2005). Impulsivity, negative expectancies, and marijuana use: A test of the acquired preparedness model. Addictive Behaviors, 30(5), 1071–1076. [DOI] [PubMed] [Google Scholar]
- Veilleux JC, Skinner KD, Reese ED, & Shaver JA (2014). Negative affect intensity influences drinking to cope through facets of emotion dysregulation. Personality and Individual Differences, 59, 96–101. [Google Scholar]
- Whiteside SP, & Lynam DR (2003). Understanding the role of impulsivity and externalizing psychopathology in alcohol abuse: application of the UPPS impulsive behavior scale. Experimental and Clinical Psychopharmacology, 11(3), 210. [DOI] [PubMed] [Google Scholar]
- Windle M, Spear LP, Fuligni AJ, Angold A, Brown JD, Pine D, Smith GT, Giedd J, & Dahl RE (2008). Transitions Into Underage and Problem Drinking: Developmental Processes and Mechanisms Between 10 and 15 Years of Age. Pediatrics, 121(Supplement 4), S273–S289. 10.1542/peds.2007-2243C [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker RA, Donovan JE, Masten AS, Mattson ME, & Moss HB (2008). Early developmental processes and the continuity of risk for underage drinking and problem drinking. Pediatrics, 121(Suppl 4), S252–272. 10.1542/peds.2007-2243B [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


