Abstract
Background
Automated Emergency Department syndromic surveillance systems (ED-SyS) are useful tools in routine surveillance activities and during mass gathering events to rapidly detect public health threats. To improve the existing surveillance infrastructure in a lower-resourced rural/remote setting and enhance monitoring during an upcoming mass gathering event, an automated low-cost and low-resources ED-SyS was developed and validated in Yukon, Canada.
Methods
Syndromes of interest were identified in consultation with the local public health authorities. For each syndrome, case definitions were developed using published resources and expert elicitation. Natural language processing algorithms were then written using Stata LP 15.1 (Texas, USA) to detect syndromic cases from three different fields (e.g., triage notes; chief complaint; discharge diagnosis), comprising of free-text and standardized codes. Validation was conducted using data from 19,082 visits between October 1, 2018 to April 30, 2019. The National Ambulatory Care Reporting System (NACRS) records were used as a reference for the inclusion of International Classification of Disease, 10th edition (ICD-10) diagnosis codes. The automatic identification of cases was then manually validated by two raters and results were used to calculate positive predicted values for each syndrome and identify improvements to the detection algorithms.
Results
A daily secure file transfer of Yukon’s Meditech ED-Tracker system data and an aberration detection plan was set up. A total of six syndromes were originally identified for the syndromic surveillance system (e.g., Gastrointestinal, Influenza-like-Illness, Mumps, Neurological Infections, Rash, Respiratory), with an additional syndrome added to assist in detecting potential cases of COVID-19. The positive predictive value for the automated detection of each syndrome ranged from 48.8–89.5% to 62.5–94.1% after implementing improvements identified during validation. As expected, no records were flagged for COVID-19 from our validation dataset.
Conclusions
The development and validation of automated ED-SyS in lower-resourced settings can be achieved without sophisticated platforms, intensive resources, time or costs. Validation is an important step for measuring the accuracy of syndromic surveillance, and ensuring it performs adequately in a local context. The use of three different fields and integration of both free-text and structured fields improved case detection.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-021-11132-w.
Keywords: Syndromic surveillance, Mass gathering, Detection algorithm, COVID-19, Case definitions
Introduction
Emergency department-based syndromic surveillance systems (ED-SyS) are effective tools that complement laboratory-based surveillance methods for the detection of infectious diseases and other public health aberrations, and enable effective control measures in a timely response [1–4]. These ED-SyS automate the use of existing (near-) real-time pre-diagnostic data routinely collected in hospitals and apply statistical algorithms to detect aberrations for immediate public health investigation. ED-SyS are routinely used in urban locations to monitor diseases of public health importance and have been leveraged globally during mass gathering events [5–8]. Many of these systems depend on (1) dedicated technical human resources (e.g., epidemiologists and data scientists), (2) sophisticated technological IT platforms (e.g., ESSENCE, BioSense, and NC-Detect in the U.S.; PHIDO and ACES in Canada) [9–12], and the use of (3) resource intensive syndrome case validation methods [1, 13]. Often, these resources and capacities are limited or unavailable in health departments serving rural and remote communities [14]. There is a need to identify methods that lower-resourced communities can use to develop and operate automated ED-SyS that approach the efficacy of a fully validated real-time system, without the steep setup time and resource costs required by more sophisticated platforms. This paper describes a novel, near real-time automated ED-SyS that was developed and validated using minimal resources in preparation of a mass gathering event in Yukon, a low resourced northern territory in Canada.
Yukon has a population of approximately 41,761 people with the majority (78%) living in the capital city of Whitehorse and 22% living in smaller remote communities [15]. Yukon’s Department of Health and Social Services (HSS) is responsible for the delivery of public health services and faces similar resource constraints to those experienced by rural local health departments in the U.S. including limited human resources (i.e., fewer staff, staff turnover, and a lack of specialty positions such as epidemiologists), information technology, and funding [14]. Yukon’s Department of HSS only recently created its first epidemiologist position, many program areas do not have the skills or capacity to manage data, IT supports are limited, and it is common for a single staff to be responsible for a wide range of acute care and public health functions. These are all factors taken into consideration while planning for enhanced surveillance of infectious diseases ahead of the Arctic Winter Games (AWG), a biennial international sporting and cultural event that rotates between major centers in the circumpolar North. In other mass-gathering sporting events, vaccine-preventable diseases such as measles, influenza, and meningococcal and gastrointestinal illnesses have been reported [7, 16].
Past gatherings for the Arctic Winter Games in Whitehorse have seen the use of syndromic surveillance systems successfully applied, with reports hand-collected from field medical staff, polyclinics, and the hospital emergency department. These data were then manually entered into a spreadsheet-based software and assessed using a cumulative-sum based approach to identify trends higher than anticipated during a short window of time [17]. It is generally accepted that investment in mass gathering surveillance should provide infrastructure that is sustainable for long-term use [7], however, this historically has not been the case in Yukon. While effective for short-term surge support, the resources required to run previous syndromic surveillance systems (e.g., refocusing full-time staff, mobilized federal field epidemiologists) were too steep to be maintained. To leverage the benefits provided by syndromic surveillance in the Yukon permanently, proposed tools must be simple to implement and train staff to use while requiring limited human and financial resources.
Similarly, to properly support an ED-SyS for long-term implementation, operational case definitions must be developed and validated. These algorithms influence the balance between identifying all possible cases (i.e., sensitivity) and excluding those without the disease of interest (i.e., specificity) [4, 18, 19]. There is no gold standard approach for developing or validating ED-SyS case definitions; methods described in the literature suggest developing definitions using expert-based consensus followed by an ongoing refinement process, with validation based on chart review by more than one clinician or comparison with a gold-standard dataset [18–26]. Most case definitions rely on natural language processing algorithms that identify keywords associated with a syndrome of interest in the chief complaint (CC) field and discharge diagnosis (DD) fields [3, 25, 27–33], with the use of clinical triage notes (CN) emerging more recently [25, 34–36]. Several studies have noted disagreement between syndrome definitions when using CC fields versus DD fields but, in general, case detection improves when leveraging information from both fields [20, 25, 32, 34, 35, 37, 38]. The use of CN fields also increases the sensitivity of the definition but may decrease specificity [25, 34–36].
Analyzing unstructured free-text commonly contained in these fields is not without its set of challenges, where spelling, abbreviations, and negating vocabulary issues can increase the risk of false-positives [25, 34, 36]. On the same note, case detection can be further limited by challenges in identifying all relevant syndrome terms or new terms introduced in documentation [38]. The lack of standardized codes can lead to variations in documentation between jurisdictions and/or facilities where application of one syndrome case definition may not fare as well in other without considering the local context [38]. While structured standardized codes can overcome many of these challenges, they may face sensitivity and specificity limitations [39]. Outside ICD diagnosis codes, the literature on the use of structured CC fields such as the use of CEDIS codes is limited.
The objectives of the present study are to describe the development and validation of Yukon’s first automated ED-SyS and evaluate the effectiveness of three different ED data fields. By measuring the contribution different sources of free-text (e.g., CN, and DD fields) with standardized codes (e.g., CEDIS), we aim to identify an optimal set of natural language processing algorithms to be used as part of a local ED-SyS to be implemented for surge support as well as lasting capacity in a resource-constrained setting where staff and technological infrastructure are limited.
Methods
The design and validation of Yukon’s ED-SyS occurred between November 2019 and February 2020, involving the following stages: (1) initial review of available data sources; (2) development of initial case definitions; (3) development of natural language processing algorithms and logic; (4) validation of ED-SyS using validation dataset; (5) refinements to algorithms and logic.
Data source
The Territorial Epidemiologist collaborated with health information analysts at Yukon’s Whitehorse General Hospital (WGH), the only hospital in Whitehorse and Yukon’s primary hospital to access records from the newly implemented real-time emergency department electronic records collection tool: Meditech ED-Tracker system. This system comprises of an electronic medical records database that captures the following information at the time of patient assessment (1) demographic characteristics and date of visit (2) clinical notes (CN) (e.g., free-text describing a brief history of the stated complaint, the recorded temperature (in °C) at triage) (3) the chief complaint (CC) containing the Canadian Emergency Department Information System (CEDIS) code [40, 41] and (4) the physician discharge diagnosis (DD) which is a free-text field providing the diagnosis at patient discharge from the ED. Collaboration between the territorial epidemiologist and WGH stakeholders (the custodians of the data) and the completion of a privacy impact assessment (PIA) led to the establishment of a daily (1 day lag) secure file transfer of ED visit data to the Office of the Chief Medical Officer of Health (OCMOH) in November 2019. Historical data of all ED visits from January 1, 2018 onwards were also made available for use. However, data between January 1, 2018 and September 30, 2018 were deemed inconsistent (e.g., incomplete data and/or missing fields) and therefore excluded from further use. National Ambulatory Care Reporting System (NACRS) records were used as a reference in our validation process for the inclusion of International Classification of Disease, 10th edition (ICD-10) codes; NACRS data were thus extracted for the time period of October 1, 2018 to April 30, 2019 and merged with ED-Tracker data. Observations without a match between the two datasets were dropped. All analyses were performed using Stata LP 15.1 (Texas, USA).
Development of initial case definitions
Syndromes of interest were identified via consensus between Yukon’s Communicable Disease Control program (YCDC) manager, the office of the Chief Medical Officer of Health (OCMOH), and the territorial epidemiologist. A review of existing syndromic surveillance platforms (e.g., NC-Detect, ESSENCE-II) [42, 43] along with current literature were used to inform the terms used in the initial case definitions for each syndrome [3, 13, 18, 21, 22, 24–29, 31, 32, 34, 44–50]. These sources enabled us to create an initial list of key terms that have been used for monitoring of similar syndromes of interest. Terms were then further refined for local context by review from stakeholders at YCDC and the OCMOH. For example, in clinical triage notes, the nurse attendant may capture inebriation or alcohol abuse by using the short-hand term ‘EtOH’; several examples such as this were included in our NLP algorithms to ensure adequate capture of these types of locally adapted data collection terms. In addition to key terms, CEDIS codes related to each syndrome were also identified and included in case definitions. Additionally, a syndrome related to COVID-19 was developed following recommendations published by the World Health Organization (WHO) [51] and local consensus with the OCMOH. This case-finding definition was further developed through extensive internal review, a review of WHO’s COVID-19 weekly Situation Reports [52], and recommendations made available online by the Public Health Agency of Canada [53].
For each syndrome, individual terms and codes that were identified through literature review or expert consensus were organized under more broadly defined concepts that were then used to determine whether a patient record met the case definition for the syndrome of interest (see Supplement A1). Using these key terms and concepts we developed natural language processing algorithms in Stata and applied these to query ED-Tracker records from October 1, 2018 to April 30, 2019 as this dataset coincided with available NACRS data that could be used to for downstream validation purposes. Algorithms were constructed using regular expressions (i.e., the “regexm” function in Stata) to detect full or partial strings from the list of key terms and concepts in either the CN, CC, or DD fields. In general, algorithms were applied for each syndrome to query data fields using a forward-inclusion strategy, starting with DD, then querying the CC and CN fields to determine whether or not a case record met the case definition for any of the syndromes of interest (see Table 1).
Table 1.
Case definitions and algorithm logic for syndromes of interest in Yukon’s ED-SyS
| Syndrome | Definition | Logic/Algorithm | Disease/condition of Interest |
|---|---|---|---|
| Gastrointestinal (GI) |
Match with the following diagnosis of interest OR Diarrhea Concept OR Vomiting/Nausea Concept OR Nausea Only Concept Anorexia Concept OR GI Concept GI related EXCLUSIONS TERMS |
1. Flag DD logic first if not blank or left without being seen related text 2. If logic step #1 not met and CN/CC logic =1 then flag 3. If DD = “Viral” and DD =0 and CN/CC logic = 1 then flag 4. If DD logic met and CN/CC logic met then then flag |
Verotoxigenic E. coli (e.g. O157:H7) enteric disease; Campylobacteriosis; Cryptosporidiosis; Salmonellosis; Shigellosis; Yersiniosis; Gastroenteritis (acute diarrheal)/ Enteric outbreaks all causes |
| Influenza-Like Illness (ILI) |
Match with the following diagnosis of interest OR ILI OR Fever Concept AND Cough Concept AND (sore throat Concept OR at least one constitutional sign/symptom: Anorexia Concept OR Dizziness Concept OR Malaise Concept OR Muscle Pain Concept OR Lymph Concept) |
1. If DD logic or CN/CC logic met then flag | Influenza |
| Respiratory (Resp) |
Match with the following diagnosis of interest OR Respiratory Concept OR Cough Concept OR Sore Concept AND (at least one constitutional sign/symptom: Anorexia Concept OR Dizziness Concept OR Fever Concept OR Malaise Concept OR Muscle Pain Concept OR Lymph Concept) |
1. Flag DD logic first if not blank or left without being seen related text 2. If logic step #1 not met and CN/CC =1 then flag 3. If DD logic met and CN/CC logic met then then flag |
Pertussis (whooping cough), Influenza, RSV |
| Rash |
Match with the following diagnosis of interest OR Rash Concept AND at least one constitutional sign/symptom: (Anorexia term OR Dizziness Concept OR Fever Concept OR Malaise Concept OR Muscle Pain Concept OR Lymph Concept) Rash related EXCLUSION terms |
1. If DD logic or CN/CC logic met then flag | Measles, Rubella, Chickenpox, Meningitis, Scarlet Fever |
| Mumps |
Match with the following diagnosis of interest OR parotitis OR orchitis OR Swelling Concept AND Face Concept Mumps related EXCLUSIONS |
1. Flag DD logic first if not blank or left without being seen related text 2. If logic step #1 not met and CN =1 then flag 3. If DD logic met and CN logic met then then flag |
Mumps |
| Neurological infections (Neuro) |
Match with the following diagnosis of interest OR Fever Concept AND (stiff neck Concept OR Seizures Concept OR Blurred Vision Concept OR Photophobia Concept OR Altered Mental Status Concept OR Headache Concept OR Paralysis Concept) |
1. Flag DD logic first if not blank or left without being seen related text 2. If logic step #1 not met and CN/CC logic =1 then flag 3. If DD = “Viral”|"Febrile seizure”|"Headache nyd”|"Malaise nyd”|"Sepsis” and DD logic =0 and CN/CC logic = 1 then flag 4. If DD logic met and CN/CC logic met then then flag |
Invasive meningococcal disease (Neisseria meningitis) infection; Encephalitis/ meningitis (bacterial; parasitic; viral) |
| Coronavirus Disease 2019 (COVID-19) |
ED visits prior to April 16 *takes into consideration negating terms Match with the diagnosis of interest in DD OR CC (SOB, Cough, Fever) on or after Jan 1, 2020 AND Match with any of the following: -countries listed from WHO Sitrep to have “local transmission”-indicates locations where the source of infection is within the reporting location Jan 1, 2020 to March 19, 2020 -Mention of international or travel in CN on or after March 15, 2020 OR -Match with the diagnosis of interest (COVID) in CN ED visits on or after April 16 *takes into consideration negating terms -Match with the diagnosis of interest in DD OR -Match with the diagnosis of interest in CN OR -Match with any of the following: -CC on or after Jan 1, 2020- SOB, Cough, Fever -CC on or after April 16, 2020- Chestpnonc, Stridor, Wheezing, Sore Throat, Syncope, Genweak, Headache, URTI, Nasal congestion/hayfever, Altered LOC, Confusion, Sensory loss/parathesis, Rep Arrest, Cyanosis -CN- “Loss of taste” or “Loss of smell” AND Match with any of the following: -countries listed from WHO Sitrep to have local transmission-indicates locations where the source of infection is within the reporting location Jan 1, 2020 to March 19, 2020 -Mention of international or travel in CN on or after March 15, 2020 |
COVID-19 | |
Validation and refinement of initial syndromic surveillance case definitions
Records with an exact match between ED-Tracker and NACRS datasets (i.e., visits occurring between October 1st, 2018 and April 30th, 2019) were used to validate the ED-SyS. Note: algorithms for detecting gastrointestinal and respiratory syndromes resulted in what was pragmatically considered too many records for manual review with current staff resources (e.g., > 600 records per syndrome), therefore an abbreviated dataset containing records from November 1, 2018 to January 31, 2019 was used instead for validating these two syndrome groups. Following the example set by [24], records flagged for meeting syndromic case definitions were assigned one of three validation classifications: likely related to the disease of interest (true-positive) = “0”; unclear/conflicting information (false positive) = “1”; does not match case definition/not related (false positive) = “2” (Table 1). These assignments were carried out first by reviewing available ICD-10 codes; any flagged case with an ICD-10 code equivalent to the those outlined in [54] was assigned a zero (“0”). This step was accomplished using the US-CDC’s database of equivalent code translation [55]. Remaining records were validated manually by two epidemiologists reviewing the ICD-10 code, DD, CC and CN fields, typically in that order. After an initial review, a random sample of 10 cases was taken from the “0”, “1”, and “2” sub-groups for each syndrome (30 cases total per syndrome) and reviewed by both epidemiologists to ensure agreement and consistency among classification. Discrepancies in scoring were discussed, and corrections were retroactively applied to the validated datasets so that consensus for all scores was achieved.
Following validation, we manually reviewed the validated records from each syndrome to identify: (1) misspellings or shorthand among the free-text fields that were not considered during the development of the initial algorithms; (2) terms and CEDIS codes that could be used to further refine the inclusion or exclusion of true- and false-positives, respectively; and (3) adjustments to the algorithm structure to improve case classification.
Evaluating the performance of the ED-SyS
Each syndrome included in the ED-SyS was evaluated by measuring the positive predictive value (PPV) using the validated case records. The PPV was defined as the total number of true-positive records (classification = “0”) over the total number of records (classification = “0”, “1”, or “2”), as a percent. To evaluate the contribution of each data field on the overall performance of the ED-SyS, we measured the PPV from each component individually as well as in combination (e.g., CN; CC; DD; CN + CC; CN + CC + DD). Finally, to evaluate which terms were most influential in identifying each syndrome, the frequency of terms present among true-positive case records were measured and visually assessed using word clouds (NB: select terms for the construction of the word clouds were double-counted as some concept terms exist in both CN and DD algorithms).
Results
Description of Yukon’s ED-SyS
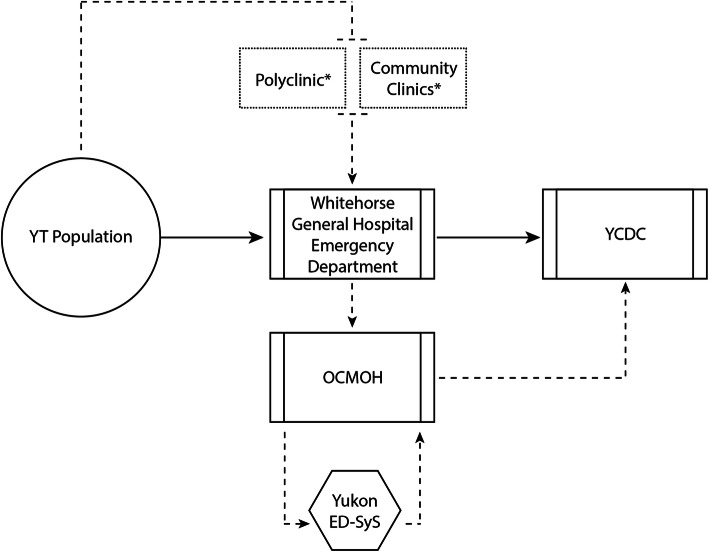
An overview of the Yukon ED-SyS is presented in Fig. 1. In Yukon, the general Whitehorse population can access emergency and primary care services through the WGH-ED, with primary care services also accessible through community clinics. These are both access points where symptomatic individuals with infectious diseases of interest present for clinical assessment. Positive results from the WGH hospital Laboratory serve as the territory’s laboratory-based surveillance system for reportable infectious diseases. The ED-SyS described here complements the laboratory component of the system, providing a source for pre-diagnosis data in Yukon sent electronically to the OCMOH daily for analysis. Once an extract of ED-SyS data is received at the OCMOH, the Territorial Epidemiologist runs the NLP syndrome algorithm and inputs the syndrome aggregate counts into the US CDC’s Early Aberration Reporting System (EARS-X) to detect any statistically significant increases in counts that may warrant further investigation. This adaptive control chart detection tool uses three algorithms (C1, C2, and C2) based on a positive 1-sided CUSUM calculation to detect aberrant data. The C1 algorithm generates an alert if counts are 3 standard deviations above the moving 7-day baseline, C2 incorporates an additional 2-day window between the observed count and baseline, and C3 uses the sum of C2 and the previous 2 days [11, 56]. EARS-X was selected for use as it required minimal historical baselines, minimal training for use, and was readily accessible. Alerts generated are then reviewed by the Territorial Epidemiologist for any evidence of clustering by age, geography, gender, chief complaint, and discharge diagnosis. Evidence of clustering are forwarded along to YCDC for clinical assessment resulting in one of the following: (1) an investigation, (2) continued monitoring, or (3) no action.
Fig. 1.
An overview of Yukon’s ED-SyS. Visit records from the Yukon population is entered into the ED-TRACKER system via Whitehorse General Hospital’s ED staff upon visit to the hospital. Data from this database are automatically downloaded daily by the OCMOH, where the territorial epidemiologist queries the dataset using the ED-SyS to identify syndromes of interest that may be flagging. When aberrations are detected that require follow-up, the OCMOH notifies YCDC to activate further investigation. Dashed boxes marked by an asterix (*) indicate modular components of the system that are designed to be used in a temporary surge capacity during mass-gathering events
In total, seven syndromes of interest were selected for daily monitoring: gastrointestinal illness (GI), influenza-like-illness (ILI), mumps, neurological infections (Neuro), rash, respiratory illnesses (Resp), and COVID-19. For each syndrome, diseases/conditions of interest were identified, and case definitions were developed based on algorithms that query information from the WGH ED-Tracker database (see Table 1). A complete list of terms used to query each syndrome is available in supplemental material (Supplement A1).
ED-SyS validation and performance
The merged dataset of ED visit data from the ED Tracker and NACRS contained a total of 19,023 unique ED visits between October 1, 2018 and April 30, 2019. After applying the initial case definitions to this dataset, hits to the GI and Resp syndromes greatly exceeded our practical ability to manually validate flagged records (e.g., over 1000 results per syndrome). For these two syndromes, a subset of ED visits from November 1, 2018 to January 31, 2019 was used for validation (n = 8246 records). After adjustment, our case definitions flagged 3707 ED visits as potential cases for all syndromes (1793 for GI; 966 for Resp; 593 for ILI; 64 for Rash; 234 for Neuro; 57 for Mumps; and 0 for COVID-19). As no records were flagged for COVID-19, the syndrome was not included in validation procedures.
Results from our validation are presented in Table 2. Among our initial case definitions, DD consistently returned the highest proportion of true positive cases (PPV: 51.3 to 100%), compared to CN (PPV: 22.8 to 86.1%) and CC (PPV: 0 to 35.0%) when used individually. In general, the CN field produced the most sensitive results, flagging the highest number of visits for all syndromes, while CC and DD fields provided a lower number of hits with higher specificity. These trends were maintained after adjustment to the initial case definitions, with the largest improvements observed in the GI syndrome (e.g., PPV for DD improved from 51.3 to 86.9%).
Table 2.
Flagged cases for each syndrome from Whitehorse General Hospital ED-Tracker records, Oct. 1, 2018 – Apr. 30, 2019
| Flagged visits by separate fields | Flagged visits by combined fields | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Field | # Hits | PPV (CI) | # Hits | PPV (CI) | Field(s) | # Hits | PPV (CI) | # Hits | PPV (CI) |
| Gastrointestinal | Gastrointestinal | ||||||||
| Pre-validation | Post-Validation | Pre-validation | Post-Validation | ||||||
| CN | 1579 |
0.23 (0.18–0.27) |
746 |
0.44 (0.38–0.49) |
CN | 1579 |
0.23 (0.18–0.27) |
746 |
0.44 (0.38–0.49) |
| CC | 866 |
0.35 (0.30–0.40) |
295 |
0.40 (0.31–0.48) |
CN/CC | 1644 |
0.22 (0.18–0.26) |
759 |
0.45 (0.39–0.50) |
| DD | 485 |
0.51 (0.45–0.57) |
236 |
0.87 (0.82–0.91) |
CN/CC/DD | 601 |
0.49 (0.43–0.54) |
316 |
0.79 (0.74–0.84) |
| Respiratory | Respiratory | ||||||||
| Pre-validation | Post-Validation | Pre-validation | Post-Validation | ||||||
| CN | 639 |
0.75 (0.71–0.78) |
625 |
0.75 (0.71–0.78) |
CN | 639 |
0.75 (0.71–0.78) |
625 |
0.75 (0.71–0.78) |
| CC | 19 |
0.21 (0–0.59) |
19 |
0.21 (−0.19–0.59) |
CN/CC | 662 |
0.74 (0.70–0.77) |
647 |
0.74 (0.70–0.77) |
| DD | 76 |
0.92 (0.86–0.98) |
76 |
0.92 (0.86–0.98) |
CN/CC/DD | 548 |
0.84 (0.81–0.87) |
542 |
0.84 (0.81–0.87) |
| ILI | ILI | ||||||||
| Pre-validation | Post-Validation | Pre-validation | Post-Validation | ||||||
| CN | 361 |
0.86 (0.82–0.90) |
356 |
0.87 (0.83–0.91) |
CN | 361 |
0.86 (0.82–0.90) |
356 |
0.87 (0.83–0.91) |
| CC | 0 | – | 0 | – | CN/CC | 380 |
0.85 (0.81–0.89) |
375 |
0.86 (0.82–0.90) |
| DD | 141 |
0.96 (0.92–0.99) |
141 |
0.96 (0.92–0.99) |
CN/CC/DD | 482 |
0.87 (0.84–0.90) |
477 |
0.88 (0.85–0.91) |
| Rash | Rash | ||||||||
| Pre-validation | Post-Validation | Pre-validation | Post-Validation | ||||||
| CN | 9 |
0.56 0.12–0.97) |
9 |
0.56 (0.12–0.97) |
CN | 9 |
0.56 (0.12–0.97) |
5 |
0.56 (0.12–0.97) |
| CC | 0 | – | 0 | 0 (0) | CN/CC | 56 |
0.57 (0.40–0.73) |
56 |
0.57 (0.40–0.73) |
| DD | 10 |
0.90 (0.70–1.00) |
10 |
0.90 (0.70–1.09) |
CN/CC/DD | 64 |
0.63 (0.47–0.77) |
64 |
0.63 (0.47–0.77) |
| Neurological | Neurological | ||||||||
| Pre-validation | Post-Validation | Pre-validation | Post-Validation | ||||||
| CN | 201 |
0.35 (0.24–0.45) |
193 |
0.35 (0.24–0.46) |
CN | 201 |
0.35 (0.24–0.45) |
193 |
0.35 (0.24–0.46) |
| CC | 0 | – | 0 | – | CN/CC | 167 |
0.54 (0.44–0.64) |
160 |
0.56 (0.45–0.65) |
| DD | 2 |
1.00 (1.00–1.00) |
2 |
1.00 (1.00–1.00) |
CN/CC/DD | 6 |
0.83 (0.51–1.00) |
19 |
0.89 (0.75–1.03) |
| Mumps | Mumps | ||||||||
| Pre-validation | Post-Validation | Pre-validation | Post-Validation | ||||||
| CN | 43 |
0.37 (0.14–0.60) |
40 |
0.40 (0.16–0.63) |
CN | 43 |
0.37 (0.14–0.60) |
40 |
0.40 (0.16–0.63) |
| DD | 17 |
0.94 (0.83–1.00) |
17 |
0.94 (0.83–1.05) |
CN/DD | 57 |
0.51 (0.33–0.68) |
17 |
0.94 (0.83–1.05) |
Abbreviations: CN clinical notes; CC chief complaint; DD discharge diagnosis; PPV positive predictive value; CI confidence interval calculated using a 95% confidence level
Data Source: Meditech ED Tracker
Note: Subject who meet case definition were those whose ED visit was assessed to be related to the disease/condition of interest. Combined field may include OR statements and/or AND statements using information in the CN, CC, DD field. Post-validation results refer to application of NLP algorithms after improvements to the algorithms were made during the initial validation phase
Combining multiple levels of data from ED-Tracker produced an average of 6.7-fold more hits to each syndrome than querying each component individually (Table 2). The largest example of this was observed when querying for visits related to the Resp Syndrome; using CC alongside CN increased hits from our original case definitions over 33-fold. Using our final case definitions for the combined fields produced the largest improvements to the GI Syndrome, with the PPV for the CN/CC combination increasing to 44.5% from 22.3% and the CN/CC/DD combination increasing to 78.8% from 48.8%. Changes observed among the other syndromes were minimal, save for the PPV of detecting the Mumps Syndrome, which increased from 50.9 to 94.1%, although the total number of observed hits decreased from 57 to 17.
Evaluating terms and logic used to identify syndromes
After an initial review of the ED-SyS performance using our validation dataset, several adjustments were made to the terms and algorithms used in our ED-SyS to improve the system’s performance within the local context. In general, three areas were useful in redefining ED-SyS queries to provide more accurate results in the Yukon setting: (1) Misspellings or shorthand among the free-text fields that were not considered during the development of the initial algorithms. For example, the acronym “LWBS” in the DD field was often used to indicate a patient had “left without being seen”, and additional acronyms were needed to describe the diarrhea, nausea, and vomit concepts within the GI syndrome case definition including “N&V” (nausea and vomiting), “N, V, D” (nausea, vomiting, diarrhea), and “V/D” (vomiting/diarrhea). (2) Terms and CEDIS code that could be used to further refine the inclusion or exclusion of true- and false-positives, respectively. For example, additional negating terms were identified for several syndromes; the inclusion of “no”, “denies” and “–” were therefore added to indicate negation within the diarrhea, nausea, vomit, fever, and cough concepts. Several CEDIS codes were consistently present among true- and false-positive results for each syndrome; we used these codes to help provide additional specificity to our inclusion and exclusion criteria based on local context (Table 3). For example, a high proportion of visits flagged by our GI case definition presented with abdominal pain (CEDIS 251), but were validated as unclear/conflicting information (n = 91/571, classification = “1”) or unrelated (n = 365/571, classification = “2”). For this reason, we elected to remove CEDIS 251 from the final GI syndrome case definition in addition to several related terms that were present in the original syndromic case definition at the CN and DD level (e.g., “ascites”, “LUQ”, “LLQ”, “RLQ”, “RUQ”, “diverticulitis”, “appendicitis”, “abdominal bloating”, and “flatus”) that were also associated with false-positive records. (3) Adjustments to the algorithm logic that could improve the application of our algorithms. For example, the original algorithm for detecting the Neuro syndrome queried the CN and CC fields only if the information from the DD field was blank. We modified this process to query CN and CC when the DD field contained at least one of the terms “febrile seizure,” “headache nyd,” “malaise nyd”, or “sepsis” without mention of the term “mening”. This improved both the sensitivity and specificity of the algorithm, increasing the number of hits from six to 19, while concomitantly increasing PPV from 83.3 to 89.5%.
Table 3.
Positive Predictive Value (PPV) of selected CEDIS codes used to inform local inclusion or exclusion criteria for each syndrome using Whitehorse General Hospital ED-Tracker records from Oct. 1, 2018 – Apr. 30, 2019 (n = 19,023 records)
| Syndrome and CEDIS code | Description | Hits (PPV%) | Inclusion / Exclusion |
|---|---|---|---|
| Gastrointestinal a | |||
| CEDIS-254 | “diarrhea” | 49 (22.8) | Inclusion |
| CEDIS-257 | “vomiting and/or nausea” | 170 (35.0) | Inclusion |
| CEDIS-852 | “fever” | 53 (51.3) | Inclusion |
| CEDIS-407 | “head injury” | 67 (0.0%) | Exclusion |
| CEDIS-307 | “UTI” | 30 (0.0%) | Exclusion |
| CEDIS-753 | “withdrawl” | 11 (0.0%) | Exclusion |
| CEDIS-251 | “abdominal pain” | 572 (20.1) | Exclusion |
| Respiratory a | |||
| CEDIS-653 | “cough” | 278 (85.6) | Inclusion |
| CEDIS-103 | “sorethroat” | 105 (84.8) | Inclusion |
| CEDIS-852 | “fever” | 103 (84.5) | Inclusion |
| ILI | |||
| CEDIS-653 | “cough” | 284 (77.5) | Inclusion |
| CEDIS-103 | “sorethroat” | 97 (57.7) | Inclusion |
| CEDIS-852 | “fever” | 68 (92.6) | Inclusion |
| Rash | |||
| CEDIS-708 | “rash” | 71 (73.2) | Inclusion |
| Neurological | |||
| CEDIS-852 | “fever” | 33 (72.7) | Inclusion |
| CEDIS-404 | “headache” | 25 (68.0) | Inclusion |
| Mumps | |||
| CEDIS-709 | “localized swelling/redness-abscess” | 17 (77.8) | Inclusion |
| CEDIS-104 | “neck swelling/pain” | 9 (73.2) | Inclusion |
| CEDIS-101 | “dental gum” | 3 (33.3) | Exclusion |
| CEDIS-102 | “facial trauma” | 3 (0.0) | Exclusion |
Abbreviations: CEDIS Canadian Emergency Department Information System; PPV positive predictive value
a These syndromes were applied to a subset of the total data containing 8246 records from November 1, 2018 to January 31, 2019
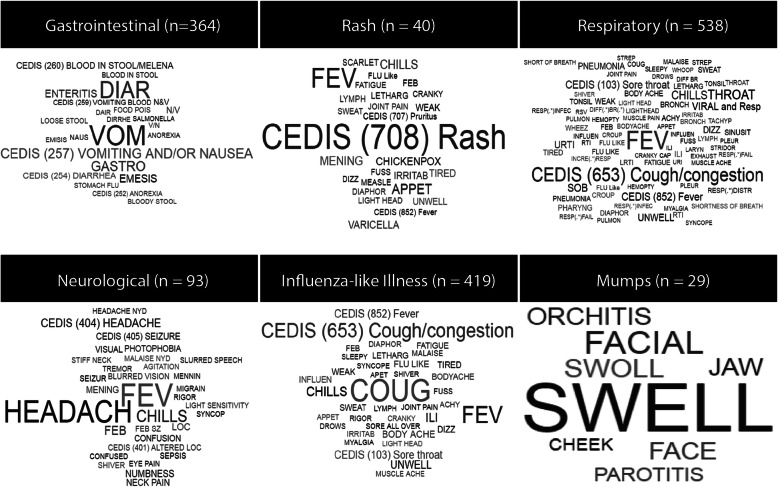
After completing the above adjustments to improve case-finding, we visualized the most influential terms among the true-positive case records for each syndrome (Fig. 2). Each syndrome appeared to have several terms that were essential to identifying the syndrome of interest. In three syndromes (Rash, Resp, and ILI) CEDIS codes appeared among the most frequent terms.
Fig. 2.
Word cloud of key terms and CEDIS codes found among true-positive validated case records. The size of each term is proportional to its frequency among validated case records
Discussion
Our ED-SyS is the first automated system to be implemented in Yukon, and, to our knowledge in northern Canada. The advancements in data collection and management at the WGH made it possible to leverage this data source to develop an electronic ED-SyS for the territory. Partnerships between WGH, OCMOH and the Public Health Agency of Canada also greatly contributed to the timely design and implementation of the ED-SyS. The ED-SyS described here requires minimal resources to set up, can be adapted for local context, and does not require highly specialized or expensive software to run. Most importantly, the Yukon ED-SyS can be used for not only short-term surge capacity during mass gathering events but is useful as a permanent early-cluster detection system, improving the existing surveillance capacity for an otherwise low-resourced public health setting.
Results from our validation indicated that for each syndrome tested, free text from the CN field generally provided the most sensitive results, whereas the DD field was most specific. These results were not surprising to us, as the information stored in each field tended towards specificity of a diagnosis moving from CN to CC and DD and these findings were similar to those found in other studies [25, 34–36]. Our findings also highlight the value of leveraging the three fields together to improve case detection. This finding is noteworthy as a significant number of cases could be missed without considering one or more fields. This was particularly evident with our respiratory and ILI syndromes, where a significant number of cases could be missed without using the CN field. Other studies have noted improvements in case detection with combined fields. For example, one study noted that sensitivity improved for gastrointestinal, rash/fever, and ILI syndromes when CC, CN, and temperature fields were used together to more than 80% from 17 to 40% [36]. South et al. (2008) also improved sensitivity for detecting ILI up to 75% when combining multiple fields from the ED record (e.g., CC and CN) compared to sole chief complaint (27%) [26]. Similarly, another study also concluded that case detection for acute respiratory infections was improved by leveraging multiple fields (e.g., temperature, ICD-9 diagnosis code, treatment remedies field, and free text clinical notes) [34]. Results for the performance of individual fields towards the overall surveillance system should be interpreted with caution, however, as many of the algorithms were intended to pull information from CC and CN data only in the absence of a confirmed case or non-case from the DD field. For a more accurate assessment of the performance of each field, algorithms should be structured with the intent to use information uniquely from each data source, instead of in a combined fashion.
An important step in designing our ED-SyS was refining the system for local context with public health and emergency department nurses and collaborators operating the existing surveillance system in Yukon. The original iteration of our ED-SyS was built using terms and case definitions informed by relevant literature, which did not capture the range of nuances inherent in our local data source. By reviewing and validating records on a case-by-case basis using our pragmatic approach tailored to the scarce resources available, we were able to identify additional terms and patterns of chart record-keeping that allowed us to make adjustments to the syndromic case definitions that improved the predictive ability of the ED-SyS. We found the CEDIS terms used in the CC field were especially useful for exploring false- positive cases flagged in our results. Having a standard terminology allowed us to group false positive cases from each syndrome by their CEDIS term and explore whether it was necessary to build additional exclusions into our syndromic case algorithms. This was not as feasible with either of the CN or DD fields, as they both contained free-text input, which proved much more variable than the CEDIS-codes and their standardized terms.
We were motivated to establish an ED-SyS to not only support surveillance activities during the mass-gathering events including the AWG, but also enhance Yukon’s ongoing surveillance infrastructure for detection and response capabilities. Our approach and ability to leverage multiple ED record fields resulted in final case definitions with moderate to high PPVs (62.5–94.1%). Moving forward, the acceptable balance between case detection and accuracy will need to depend on the risk posed by missing a case vs the burden of dealing with false positives. Under short term, high-risk situations including future AWG events, and for monitoring high profile conditions such as COVID-19, maximizing sensitivity will likely be prioritized. Where disease risk may be low, surveillance of syndromes with lower PPV may not warrant ongoing routine surveillance. For example, Yukon may consider discontinuing surveillance for the rash syndrome, given the low frequency of measles in the territory and lower PPV. Since validation, the ED- SyS was leveraged for example to support ongoing enhanced surveillance for respiratory, ILI, and COVID-19 during the influenza season and COVID-19 pandemic. Our ED-SyS did not detect any potential COVID-19 cases from our October 1, 2018 to April 30, 2019 study dataset likely due to the lack of travel related documentation in the ED record. Travel related screening questions for respiratory presentations to the ED were more widely implemented in early 2020. However, since mid-February 2020, the system has flagged a small number of ED visits that meet the COVID-19 case definition (data not included in present analysis), and while follow-up on these potential cases did not result in identifying anyone positive for COVID-19 infection, it does indicate our system is working as intended. Further validation of the COVID-19 algorithm may be warranted in a future analysis. As the dynamics of the COVID-19 outbreak progress, we will continue to adapt the algorithm as needed.
The US-CDC’s EARS-X tool required minimal resources, was easy to operate, and provided a quick means to identify aberrations for further investigation. While the ED-Tracker was recently launched and baseline data is limited at this time, other automated statistical algorithms may be explored that consider historical trends, seasonal, and day-of-week effects [4]. Future development of the ED-SyS will include expanding to the syndromic surveillance of other public health issues in Yukon, including opioids, cannabis, forest fires, and secondary health impacts of the COVID-19 pandemic.
Conclusions/practice implications
Our study highlights the feasibility of implementing an automated ED-SyS and validating syndrome case definitions in a low-resourced/remote setting using simple tools, resources, and adapted gold standard methods. Our approach to developing an ED-SyS allowed Yukon to move away from “drop-in” paper-based methods to create a “low-tech” sustainable system that can be leveraged for other mass-gathering events, other emerging health issues of concern, and general ongoing surveillance. Our study also reinforces the importance and value of validating syndrome case definitions using local data. Importantly, our study provides a path forward for other lower-resourced rural/remote settings on how to develop and validate syndrome case definitions.
Supplementary Information
Acknowledgements
The authors acknowledge the contributions of Yukon Center for Disease Control and the Whitehorse General Hospital who provided consultation for the project and provided the dataset used for validating the surveillance system. The authors would also like to acknowledge technical contributions from Rohit Kasbekar, and proof-reading services by Alexandrea Anderson.
Abbreviations
- AWG
Arctic winter games
- ED
Emergency department
- SyS
Syndromic surveillance system
- CC
Chief complaint
- DD
Discharge diagnosis
- CN
Clinical (triage) notes
- WHG
Whitehorse general hospital
- CEDIS
Canadian emergency department information system
- NACRS
National ambulatory care reporting system
- ICD
International classification of disease
- YCDC
Yukon center for disease control
- OCMOH
Office of the chief medical officer of health
- NC Detect
North Carolina disease event tracking and epidemiologic collection tool
- ESSENCE-II
Electronic surveillance system for the early notification of community-based epidemics
- COVID-19
Coronavirus-disease 2019
- US-CDC
United States centers for disease control and prevention
- GI
Gastrointestinal illness
- ILI
Influenza-like illness
- Neuro
Neurological illness
- Resp
Respiratory illness
- PPV
Positive predictive value
- LUQ
Left upper quadrant
- LLQ
Left lower quadrant
- RLQ
Right lower quadrant
- RUQ
Right upper quadrant
- nyd
Not yet determined
Authors’ contributions
EB designed and led the study and wrote the original code for the surveillance system. EB and BMH performed validation, analysis and interpretation, produced the final Stata code used for the ED-SyS, and drafted and edited the manuscript. BH contributed to study design, provided consultation and oversight, and contributed to proofreading and editing the manuscript. All authors read and approved the final manuscript.
Funding
The authors wish to acknowledge funding from the Public Health Agency of Canada to provide a Field Epidemiologist to support the analysis and writing of this project.
Availability of data and materials
All programming code, including natural language processing algorithms that were developed for this manuscript have been made available publicly [57]. The data that support the findings of this study are available from Yukon Health and Social Services, but restrictions apply to the availability of these data, which were used under license for the current study and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Yukon government.
Declarations
Ethics approval and consent to participate
A privacy impact assessment was completed between the Whitehorse General Hospital and the Office of the Chief Medical Officer of Health; no privacy concerns were found. The study was conducted in accordance with the Yukon Health Information Privacy and Management Act (http://www.gov.yk.ca/legislation/acts/hipm_c.pdf) and with approval from the Yukon Chief Medical Officer of Health, Whitehorse General Hospital, and the Yukon Center for Communicable Disease.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fleischauer AT, Gaines J. Enhancing surveillance for mass gatherings: the role of syndromic surveillance. Public Health Rep. 2017;132:95S–98S. doi: 10.1177/0033354917706343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lauper U, Chen JH, Lin S. Window of opportunity for new disease surveillance: developing keyword lists for monitoring mental health and injury through syndromic surveillance. Disaster Med Public Health Prep. 2017;11:173–178. doi: 10.1017/dmp.2016.99. [DOI] [PubMed] [Google Scholar]
- 3.May LS, Griffin BA, Bauers NM, Jain A, Mitchum M, Sikka N, et al. Emergency department chief complaint and diagnosis data to detect influenza-like illness with an electronic medical record. West J Emerg Med. 2010;11:1–9. http://www.ncbi.nlm.nih.gov/pubmed/20411066%0A, http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC2850833. [PMC free article] [PubMed]
- 4.Faverjon C, Berezowski J. Choosing the best algorithm for event detection based on the intend application: A conceptual framework for syndromic surveillance. J Biomed Inform. 2018;85 August:126–135. doi:10.1016/j.jbi.2018.08.001. [DOI] [PubMed]
- 5.Mandl KD, Overhage JM, Wagner MM, Lober WB, Sebastiani P, Mostashari F, et al. Implementing syndromic surveillance: a practical guide informed by the early experience. J Am Med Inform Assoc. 2004;11:141–150. doi: 10.1197/jamia.M1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berry AC. Syndromic surveillance and its utilisation for mass gatherings. Epidemiol Infect. 2019;147. 10.1017/S0950268818001735. [DOI] [PMC free article] [PubMed]
- 7.Kajita E, Luarca MZ, Wu H, Hwang B, Mascola L. Harnessing syndromic surveillance emergency department data to monitor health impacts during the 2015 Special Olympics World Games. Public Health Rep. 2017;132(1_suppl):99S–105S. [DOI] [PMC free article] [PubMed]
- 8.Deyneka L, Faigen Z, Hakenewerth A, Lee N, Ising A, Li M. Using state and National Surveillance Systems during world equestrian games in NC. Online J Public Health Inform. 2019;11:1–4. 10.5210/ojphi.v11i1.9691.
- 9.Waller AE, Scholer M, Ising AI, Travers DA. Using Emergency Department Data For Biosurveillance: The North Carolina Experience. Infectious Disease Informatics and Biosurveillance. 2010;27:45–66. 10.1007/978-1-4419-6892-0_3.
- 10.Gould DW, Walker D, Yoon PW. The evolution of BioSense: lessons learned and future directions. Public Health Rep. 2017;132:7–11. doi: 10.1177/0033354917706954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moore KM, Edgar BL, McGuinness D. Implementation of an automated, real-time public health surveillance system linking emergency departments and health units: rationale and methodology. CJEM. 2008;10(2):114–9. [DOI] [PubMed]
- 12.Hu W. Use of Public Health Intelligence for Disease Outbreaks (PHIDO) to Enhance Provincial Routine Reportable Disease Surveillance in Manitoba. https://cupdf.com/document/use-of-public-health-intelligence-for-disease-outbreaks-phido-to-enhance.html. Accessed 10 Apr 2021.
- 13.May L, Chretien JP, Pavlin JA. Beyond traditional surveillance: applying syndromic surveillance to developing settings-opportunities and challenges. BMC Public Health. 2009;9:1–11. doi: 10.1186/1471-2458-9-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris JK, Beatty K, Leider JP, Knudson A, Anderson BL, Meit M. The double disparity facing rural local health departments. The Annual Review of Public Health. 2016;37:167–184. doi: 10.1146/annurev-publhealth-031914-122755. [DOI] [PubMed] [Google Scholar]
- 15.Yukon Government. Yukon bureau of statistics population report, fourth quarter 2019. 2020. https://yukon.ca/sites/yukon.ca/files/ybs/populationq4_2019_0.pdf. Accessed 10 Apr 2021.
- 16.Gautret P, Steffen R. Communicable diseases as health risks at mass gatherings other than hajj: what is the evidence? Int J Infect Dis. 2016;47:46–52. doi: 10.1016/j.ijid.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 17.Zhu Y, Wang W, Atrubin D, Wu Y. Initial evaluation of the early aberration reporting system. Morb Mortal Wkly Rep. 2005;54(Suppl):123–130. [PubMed] [Google Scholar]
- 18.Chapman WW, Dowling JN, Baer A, Buckeridge DL, Cochrane D, Conway MA, et al. Developing syndrome definitions based on consensus and current use. J Am Med Inform Assoc. 2010;17:595–601. doi: 10.1136/jamia.2010.003210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scholer MJ, Ghneim GS, Wu S, Westlake M, Travers DA, Waller AE, et al. Defining and applying a method for improving the sensitivity and specificity of an emergency department early event detection system. AMIA Ann Symp Proc. 2007;8:651–655. [PMC free article] [PubMed] [Google Scholar]
- 20.Fleischauer AT, Silk BJ, Schumacher M, Komatsu K, Santana S, Vaz V, et al. The validity of chief complaint and discharge diagnosis in emergency department-based syndromic surveillance. Acad Emerg Med. 2004;11:1262–1267. doi: 10.1197/j.aem.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 21.Chapman WW, Christensen LM, Wagner MM, Haug PJ, Ivanov O, Dowling JN, et al. Classifying free-text triage chief complaints into syndromic categories with natural language processing. Artif Intell Med. 2005;33:31–40. doi: 10.1016/j.artmed.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 22.MacRae J, Love T, Baker MG, Dowell A, Carnachan M, Stubbe M, et al. Identifying influenza-like illness presentation from unstructured general practice clinical narrative using a text classifier rule-based expert system versus a clinical expert. BMC Med Inform Dec Mak. 2015;15:1–11. doi: 10.1186/s12911-015-0201-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kotzen M, Sell J, Mathes RW, Dentinger C, Lee L, Schiff C, et al. Using syndromic surveillance to investigate tattoo-related skin infections in new York City. PLoS One. 2015;10:1–7. doi: 10.1371/journal.pone.0130468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ivanov O, Wagner MM, Chapman WW, Olszewski RT. Accuracy of three classifiers of acute gastrointestinal syndrome for syndromic surveillance. Proc AMIA Symp. 2002:345–9. [PMC free article] [PubMed]
- 25.Haas SW, Travers D, Waller A, Mahalingam D, Crouch J, Schwartz TA, et al. Emergency medical text classifier: new system improves processing and classification of triage notes. Online J Public Health Inform. 2014;6:1–19. 10.5210/ojphi.v6i2.5469. [DOI] [PMC free article] [PubMed]
- 26.South BR, Chapman WW, DeLisle S, Shen S, Kalp E, Perl T, et al: Optimizing a Syndromic Surveillance Text Clasifier for Influenza-Like Illness: Does Document Source Matter? Proc AMIA Symp. 2008:692–6. [PMC free article] [PubMed]
- 27.Travers D, Haas SW, Waller AE, Schwartz TA, Mostafa J, Best NC, et al. Implementation of emergency medical text classifier for syndromic surveillance. AMIA Annu Symp Proc. 2013;2013 Cc:1365–1374. [PMC free article] [PubMed]
- 28.Gerbier S, Yarovaya O, Gicquel Q, Millet AL, Smaldore V, Pagliaroli V, et al. Evaluation of natural language processing from emergency department computerized medical records for intra-hospital syndromic surveillance. BMC Med Inform Dec Mak. 2011;11:50. doi: 10.1186/1472-6947-11-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gerbier-Colomban S, Gicquel Q, Millet AL, Riou C, Grando J, Darmoni S, et al. Evaluation of syndromic algorithms for detecting patients with potentially transmissible infectious diseases based on computerised emergency-department data. BMC Med Inform Dec Mak. 2013;13:1–10. doi: 10.1186/1472-6947-13-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Conway M, Dowling JN, Chapman WW. Using chief complaints for syndromic surveillance: a review of chief complaint based classifiers in North America. J Biomed Inform. 2013;46:734–743. doi: 10.1016/j.jbi.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heffernan R, Mostashari F, Das D, Karpati A, Kulidorff M, Weiss D. Syndromic surveillance in public health practice, New York City. Emerg Infect Dis. 2004;10:858–864. doi: 10.3201/eid1005.030646. [DOI] [PubMed] [Google Scholar]
- 32.Begier EM, Sockwell D, Branch LM, Davies-Cole JO, Jones LVH, Edwards L, et al. The National Capitol Region’s emergency department syndromic surveillance system: do chief complaint and discharge diagnosis yield different results? Emerg Infect Dis. 2003;9:393–396. doi: 10.3201/eid0903.020363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lazarus R, Kleinman KP, Dashevsky I, DeMaria A, Platt R. Using automated medical records for rapid identification of illness syndromes (syndromic surveillance): the example of lower respiratory infection. BMC Public Health. 2001;1:1–9. doi: 10.1186/1471-2458-1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.DeLisle S, South B, Anthony JA, Kalp E, Gundlapallli A, Curriero FC, et al. Combining free text and structured electronic medical record entries to detect acute respiratory infections. PLoS One. 2010;5. [DOI] [PMC free article] [PubMed]
- 35.DeYoung K, Chen Y, Beum R, Askenazi M, Zimmerman C, Davidson AJ. Validation of a syndromic case definition for detecting emergency department visits potentially related to marijuana. Public Health Rep. 2017;132:471–479. doi: 10.1177/0033354917708987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ising AI, Travers DA, MacFarquhar J, Kipp A, Waller Anna E. Triage note in emergency department-based syndromic surveillance. Adv Dis Surveill. 2006;1:34. [Google Scholar]
- 37.Raven MC, Lowe RA, Maselli J, Hsia RY. Comparison of presenting complaint vs discharge diagnosis for identifying “nonemergency” emergency department visits. JAMA. 2013;309:1145–1153. doi: 10.1001/jama.2013.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Harduar Morano L, Waller AE. Evaluation of the components of the North Carolina syndromic surveillance system heat syndrome case definition. Public Health Rep. 2017;132:40S–47S. doi: 10.1177/0033354917710946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lu HM, Zeng D, Trujillo L, Komatsu K, Chen H. Ontology-enhanced automatic chief complaint classification for syndromic surveillance. J Biomed Inform. 2008;41:340–356. doi: 10.1016/j.jbi.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 40.Innes G, Murray M, Grafstein E. A consensus-based process to define standard national data elements for a Canadian emergency department information system. Can J Emerg Med. 2001;3:277–284. doi: 10.1017/S1481803500005777. [DOI] [PubMed] [Google Scholar]
- 41.Grafstein E, Bullard MJ, Warren D, Unger B. Revision of the Canadian emergency department information system (CEDIS) presenting complaint list version 1.1. Can J Emerg Med. 2008;10:173. doi: 10.1017/S1481803500009878. [DOI] [PubMed] [Google Scholar]
- 42.Lombardo J, Burkom H, Elbert E, Magruder S, Happel Lewis S, Loschen W, et al. A systems overview of the electronic surveillance system for the early notification of community-based epidemics (ESSENCE II) J Urban Health. 2003;80:32–42. doi: 10.1007/PL00022313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Morano LH, Waller AE. Evaluation of the components of the North Carolina syndromic surveillance system heat syndrome case definition. Public Health Rep. 2017;132:40–47. doi: 10.1177/0033354917710946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Overview of influenza monitoring in Canada - Canada.ca. https://www.canada.ca/en/public-health/services/diseases/flu-influenza/influenza-surveillance/about-fluwatch.html#a2.3. Accessed 10 Apr 2021.
- 45.Fitzner J, Qasmieh S, Mounts AW, Alexander B, Besselaar T, Briand S, Brown C, Clark S, Dueger E, Gross D, Hauge S. Revision of clinical case definitions: influenza-like illness and severe acute respiratory infection. Bull World Health Organ. 2018;96(2):122. 10.2471/BLT.17.194514. [DOI] [PMC free article] [PubMed]
- 46.Hiller KM, Stoneking L, Min A, Rhodes SM. Syndromic surveillance for influenza in the emergency department-a systematic review. PLoS One. 2013;8. 10.1371/journal.pone.0073832. [DOI] [PMC free article] [PubMed]
- 47.Cadieux G, Buckeridge DL, Jacques A, Libman M, Dendukuri N, Tamblyn R. Accuracy of syndrome definitions based on diagnoses in physician claims. BMC Public Health. 2011;11. 10.1186/1471-2458-11-17. [DOI] [PMC free article] [PubMed]
- 48.Centers for Disease Control and Prevention. Syndrome Definitions for Diseases Associated with Critical Bioterrorism-associated Agents. 2003. https://emergency.cdc.gov/surveillance/syndromedef/pdf/syndromedefinitions.pdf. Accessed 10 Apr 2021.
- 49.Ansaldi F, Orsi A, Altomonte F, Bertone G, Parodi V, Carloni R, et al. Emergency department syndromic surveillance system for early detection of 5 syndromes: a pilot project in a reference teaching hospital in Genoa, Italy. J Prev Med Hyg. 2008;49:131–135. [PubMed] [Google Scholar]
- 50.The SSO Research group. Syndromic Surveillance Ontology http://surveillance.mcgill.ca/projects/sso/index.html. Accessed 10 Apr 2021.
- 51.Aylward, Bruce (WHO); Liang W (PRC). Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). The WHO-China Joint Mission on Coronavirus Disease 2019. 2020;2019 February:16–24. https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
- 52.The World Health Organization. Coronavirus Disease (COVID-19) Situation Reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed 10 Apr 2021.
- 53.The World Health Organization. Coronavirus disease (COVID-19): Outbreak update - Canada.ca. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection.html. Accessed 10 Apr 2021.
- 54.Sloane PD, MacFarquhar JK, Sickbert-Bennett E, Mitchell CM, Akers R, Weber DJ, et al. Syndromic surveillance for emerging infections in office practice using billing data. Ann Fam Med. 2006;4:351–358. doi: 10.1370/afm.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.ICD.Codes. Conversion of ICD-9-CM to ICD-10-CM. 2021. https://icd.codes/convert/icd9-to-icd10-cm. Accessed 10 Apr 2021.
- 56.Johns Hopkins Applied Physics Laboratory. OpenESSENCE User Guide. 2014. https://www.jhuapl.edu/sages/guides/OEUserGuide_JUL_2014.pdf. Accessed 9 Apr 2021.
- 57.Hetman B, Bouchouar E. DoFile_EDTRACKER.do. 2020. https://doi.org/10.6084/m9.figshare.12649364.v1. Accessed 10 Apr 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All programming code, including natural language processing algorithms that were developed for this manuscript have been made available publicly [57]. The data that support the findings of this study are available from Yukon Health and Social Services, but restrictions apply to the availability of these data, which were used under license for the current study and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the Yukon government.