Abstract
Background
The prevalence of hypothyroidism among Indian women is 15.8%. Depression is frequently reported in hypothyroidism. Yoga is an effective intervention for depression. However, the influence of yoga on depression in patients with hypothyroidism has not been studied.
Aim
The present study investigated the effect of a 3-month integrated yoga intervention (3-IY) on depression, lipid indices, and serum thyroid-stimulating hormone (sTSH) levels among female patients having hypothyroidism, and mild-to-moderate depression.
Method
The present single-arm pre–post design study was conducted in thirty-eight women (average age 34.2 ± 4.7 years). Participants received a 3-IY comprising asanas, pranayama, and relaxation techniques for 60 min daily (5 days a week). Depression, sTSH, lipid profile indices, Body Mass Index (BMI), fatigue, anxiety, and stress were assessed at baseline and after 12 weeks. Thyroid medication was kept constant during the study period. Data were analysed using R Studio software.
Result
A significant (P < 0.05) reduction in depression (58%), sTSH (37%), BMI (6%), fatigue (64%), anxiety (57%), lipid profile indices (HLD increased significanty), and stress (55%) levels was observed after 3 months, compared with the corresponding baseline levels.
Conclusion
The 3-IY is useful for reducing depression, dyslipidemia, and sTSH in women with hypothyroidism and depression. Further studies with a larger sample size and a robust research design using objective variables must be conducted to strengthen the study findings.
Keywords: Thyrotropin, Health, Complementary therapies, Women, Anxiety, Body mass index
Graphical abstract
1. Introduction
Hypothyroidism is highly prevalent among women. The overall prevalence of hypothyroidism in India is 10%, whereas its prevalence in Indian women is 15.8%.1 Deokar et al. (2014) studied 2076 participants with suspicion of hypothyroidism and reported a 9.4% prevalence of subclinical hypothyroidism and a 4.2% prevalence of overt hypothyroidism. Hypothyroidism in women contributes to infertility, menstrual disorders, cardiovascular disease, type 2 diabetes mellitus (T2DM), and psychiatric disorders.2
A relationship between hypothyroidism and psychiatric disorders has been suggested in literature.3 Thyroid dysfunction has been observed in the pathogenesis of many psychiatric disorders, including depression.4 Depression is the most commonly reported psychiatric condition in women with hypothyroidism. Hypothyroidism and depression have several common clinical symptoms.5 A higher risk of depression was observed among patients with subclinical and overt hypothyroidism as compared with controls.6 Recent meta-analysis of 12,315 individuals revealed that those with subclinical hypothyroidism had higher risk of depression than euthyroid controls (relative risk = 2.35).7 The patients with hypothyroidism should be screened for depression, and patients with depression should be screened for hypothyroidism.8 A recent study reported that 33.9% of patients with hypothyroidism have depression.9 Another study with a small sample size of 63 patients with hypothyroidism reported a 63% prevalence of depression.10
Depression is related to several biological factors involved in hypothyroidism. Serum thyroid-stimulating hormone (sTSH) levels are negatively associated with depression in hypothyroidism.11 Elevated thyroid peroxidase antibody (TPO-Ab) levels are associated with an increased risk of depression.12 Although improved sTSH levels with the administration of oral thyroxin improves depressive symptoms, the risk of lifetime depression remains high in patients with hypothyroidism compared with controls.
Thyroxin medication reduces depressive symptoms among women with hypothyroidism; however, the risk of depression in these patients remains high compared with the controls. The positive role of alternative and complementary therapies such as yoga has been reported in the effective management of chronic disorders, including depression. Such interventions may help in the effective treatment of hypothyroidism.
Yoga is a mind–body discipline and has numerous health benefits, such as the improvement of cardiorespiratory fitness, cognitive functions, mental health, and quality of life. The popularity of yoga as a complementary and alternative medicine in chronic disorders has increased worldwide in the last three decades. Yoga is a safe and effective intervention for several chronic health conditions such as endocrine and psychiatric disorders. Additionally, yoga is recommended as the first and standalone treatment for depression.
The present study investigated the effect of a 3-month integrated yoga intervention (3-IY) on depression and sTSH levels among women with hypothyroidism and depression. Other variables such as body mass index (BMI), lipid profile, fatigue, anxiety, and stress were also assessed.
2. Methodology
2.1. Study participants
The present single-arm study was conducted in a community setting in women of 20–50 years with overt hypothyroidism having clinical depression (mild-to-moderate) in Calicut, Kerala. The diagnosis of hypothyroidism was made on the basis of a clinical examination by an endocrinologist (elevated TSH with low T3 and T4 levels). Depression was diagnosed by a psychiatrist using DASS 21 (Chart 1).
Chart 1.
Study protocol.
2.1.1. Inclusion and exclusion criteria
Women within the age 20–50 years, diagnosed with hypothyroidism, taking thyroxin and had mild to moderate depression were included in the study. Patients with history of psychiatric disorders including addiction, antipsychotic medication, thyroid cancer, and abdominal surgery in the past one year; patients with morbid obesity; pregnant patients; regular yoga practitioners; and patients who had changed their thyroxin dosage in the preceding 3 months were excluded from the study.
2.2. Participant recruitment
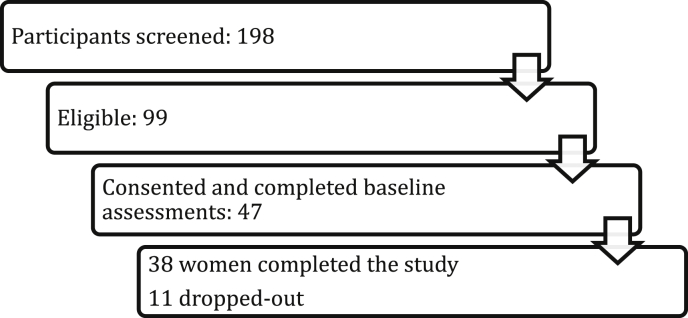
An advertisement about the study was placed in local newspaper. Total 198 hypothyroid women were screened for mild to moderate depression using Depression, Anxiety, and Stress Scale (DASS-21). DASS 21- Depression score between 10 & 20 was considered as mild-moderate depression. Of these 198 screened, 99 (50.1%) had clinical depression. Forty-seven women consented for the study.
2.3. Ethical consideration
All 47 participants declared their voluntary participation in this study by signing an informed consent form before study commencement. The present research was conducted according to the Helsinki Declaration, as revised in 2013. Participants were informed about their freedom to withdraw from the study at any point and the patient’s information was kept confidential. Institutional Project Evaluation/Ethics Committee of ÷÷÷÷÷÷÷ University approved the study (÷÷÷-021-2018). Duly signed Informed consent form was obtained prior to the study by all 47 women.
2.4. Assessment
All the outcome measures were assessed at baseline and after 3 months. The questionnaires were administered by the clinical psychology staff.
The primary outcome measures were depression and sTSH levels, whereas the secondary outcome measures were BMI, anxiety, fatigue, lipid proile, and stress.
2.5. Assessment methods
2.5.1. Biochemical variables
Participants were instructed to come for blood tests on empty stomach earlier in the morning with minimum 8 HRS fasting. Venous blood sample was collected. Fasting lipid profiles and sTSH levels were assessed in an authenticated laboratory. sTSH levels were assessed through immunometric assays of thyrotropin (for TSH).13
2.5.2. Psychological measures
Anxiety, depression, and stress were measured using the DASS-21 questionnaire.
DASS-21 is a self-reported questionnaire consisting of 21 items that measures anxiety, depression, and stress. The DASS-21 has been validated in the literature (Cronbach’s α values are 0.94, 0.87, and 0.91 for depression, anxiety, and stress, respectively) 18 and with similar values in the Indian population.14,15
2.5.3. Fatigue
The fatigue severity scale, published in 1989 by Krupp, has 9 items. For each question, the patient is asked to choose a number from 1 to 7, which indicates how much the patient agrees to each statement, with 1 indicating strong disagreement and 7 indicating strong agreement. A score of 4 or higher generally indicates severe fatigue.16
2.5.4. Intervention
The 3-IY was performed in three locations for the convenience of the participants. It comprised asana (yoga postures), pranayama (yogic breathing practices), relaxation techniques, and meditation (Table 1). The yoga intervention was designed by a team of one of the authors, a yoga consultant, and an endocrinologist with yoga knowledge.
Table 1.
List of practices.
| Type of practices | Name of the practice |
|---|---|
| Loosening | Loosening of all joints from toes to neck Twisting, forward backward bending, side bending, jogging, drill walking |
| Surynamaskar: 20 rounds | |
| Breathing practices | Hands in and out breathing, hands stretch breathing, ankle stretch breathing, dog breathing, tiger breathing, sectional breathing dynamic kalapabhati, Bhastrika |
| Asana | Emphasis on asanas involving backward bends, chest opening and supine relaxation. Ardhachakrasana, ardhakati-chakrasana, padahasthasana, ustrasana, bhunamanasana, vajrasana, setubandhasana, sarvangasana, matsyasana, shavasana, bhujangasana, shalabhasana, navasana, navakasana, janushirshasana were administered. |
| Pranayama | Right nostril breathing (for activating sun channel). Ujjayi breath with antar kumbhaka and Chandra bhedana |
| Meditation | Sun Meditation, Gayatri Mantra Chant |
Participants received 60 min of yoga intervention every day for 3 months (5 days in a week) under the supervision of a trained yoga therapist.
The participants were constrained from eating anything before the yoga sessions. They were instructed to wear loose and comfortable clothing.
2.6. Data analysis
Data were statistically analysed using SPSS 16 (IBM, Chicago, 2016). The data are presented as mean and standard deviations. A paired sample t-test was used to measure pre to post changes. A P value of <0.05 was considered statistically significant. The % change in the mean score was calculated using the following formula: post mean − pre mean/pre mean × 100. Microsoft excels and R Studio software was used for data analysis.
3. Results
3.1. Participation
Out of 47 consented; thirty-eight women completed the study. Eleven women lost the follow-up of these, 4 women discontinued the study due to shift of the location and 3 women discontinued intervention to due non-suitability of timings and 4 women attended less than 10 sessions.
Thirty-eight women completed the study. Of these, more than 92% of the participants attended at least 58 of the 60 yoga sessions, suggestive of good acceptance, adherence and feasibility of yoga intervention in the community settings.
3.2. Demographic characteristics
Most of the participants were belonging to middle class socio-economic status and most of these were house wives. The average age of the group was 34.2 ± 4.7 years. At the baseline the average score depression was 13.3. The average thyroxin medication score was 45.7 mcgs/day.
Most of the participants were belonging to upper middle class families. Majority of them were job holders and house-wives. Thirty-three participants were married, of who 2 were 3 were widows and 2 had divorce. 14 participants had co-morbidities; three had type 2 diabetes mellitus (T2DM) and 5 had hypertension. 6 patients had non-specific occasional musculoskeletal pain (See Table 2).
Table 2.
Demographic details of the participants.
| Age (years) | 34.2 ± 4.7 |
|---|---|
| Marital status | Married – 33; widows - 3, divorced – 2 & Unmarried - 2 |
| Education | Below UG – 5 Completed UG - 22, PG – 8, PG+ = 3 |
| Socio-economic background | Lower middle class – 8, Upper middle class – 27, higher - 3 |
| Other comorbidities | T2DM – 3, hypertension – 5 & non-specific musculoskeletal pain - 6 |
| Employment | 14 – job holders, 8 self-employed and 16 house-wives |
3.3. Changes in the mental health measures
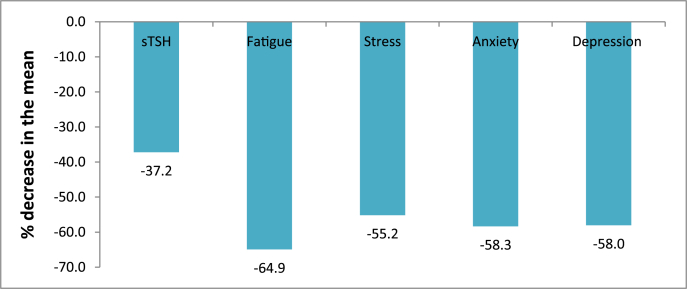
There was a statistically significant decrease with larger effect size in the depression (p > 0.001, ES- 4.9), anxiety (p > 0.001, ES- 3.1), fatigue (p > 0.001, ES- 5.5), sTSH (p > 0.001, ES- 1.1) and stress (p > 0.001, ES- 3) after 3 months compared to the baseline.
3.3.1. Changes in the lipid profile, BMI, and thyroxin dosage
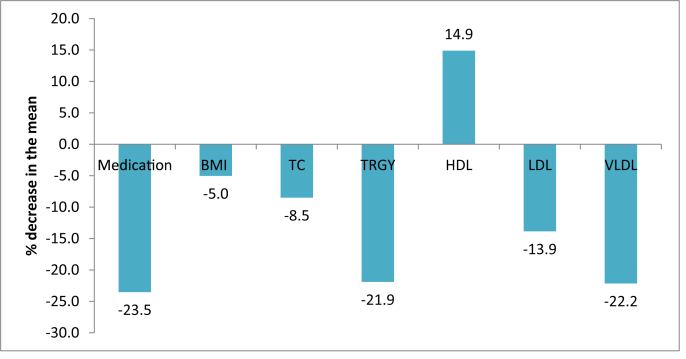
Medication also improved significantly. After 3-IY out of 38 women, only 3 had depression score >10 suggestive of mild depression, whereas, 35 women achieved non-depressive score. There was 58% (from 13.3 to 5.6) decrease in the mean depression score and 23.5% (from 45.7 to 35) decrease in the mean thyroxin requirement following the 3-IY intervention (See Table 3).
Table 3.
Pre–post changes of the parameters.
| Measures | Baseline | follow-up | % difference in the mean | Mean difference | 95% CI |
Cohen’s d | |
|---|---|---|---|---|---|---|---|
| Upper bond | Lower bond | ||||||
| Medication | 45.77 ± 25.61 | 35.00 ± 19.16∗∗ | −23.5 | 9.2 | 4.7 | 13.6 | 0.4 |
| BMI | 26.44 ± 2.67 | 24.8 ± 2.23∗ | −6.0 | 1.3 | .8 | 1.9 | 0.5 |
| TC | 218.42 ± 29.88 | 199.85 ± 14.53∗∗ | −8.5 | 25.9 | 10.46 | 24.7 | 0.7 |
| TRGY | 117.34 ± 34.06 | 91.63 ± 19.95∗∗ | −21.9 | −6.6 | 16.58 | 35.3 | 0.9 |
| HDL | 46.35 ± 8.75 | 53.25 ± 5.39∗∗ | 14.9 | 19.5 | −9.5 | −3.7 | 0.9 |
| LDL | 148.91 ± 28.75 | 128.27 ± 14.10∗∗ | −13.9 | 5.0 | 11.6 | 27.4 | 0.91 |
| VLDL | 23.52 ± 7.17 | 18.31 ± 4.00∗ | −22.2 | 25.9 | 3.0 | 6.9 | 0.9 |
| sTSH | 5.24 ± 2.2 | 3.29 ± 1.03∗∗ | −37.2 | 1.9 | 1.3 | 2.5 | 1.1 |
| Fatigue | 46.37 ± 6.2 | 16.26 ± 4.4∗∗ | −64.9 | 30.1 | 27.6 | 32.6 | 5.5 |
| Stress | 16.26 ± 3.0 | 7.29 ± 2.9∗∗ | −55.2 | 8.9 | 7.8 | 10.0 | 3.05 |
| Anxiety | 12.89 ± 2.5 | 5.37 ± 2.2∗∗ | −58.3 | 7.5 | 6.6 | 8.4 | 3.1 |
| Depression | 13.37 ± 1.8 | 5.61 ± 1.3∗∗ | −58.0 | 7.7 | 6.75 | 8.7 | 4.9 |
All lipid profile measures; total cholesterol, triglycerides, HDL, LDL and VLDL decreased significant and HDL increased significantly after 3 months compared to the baseline. These changes suggest the positive impact of yoga in hypothyroidism (See Table 3).
The decrease in the mean scores was >30% for all the variables. Percentage change >30% is considered as clinically significant change.17
The table depicts the paired sample t-test results. ∗∗ Statistically significant (P < 0.01) (Figs. 1 and 2).
Fig. 1.
% Decrease in the mean of sTSH, mental health and fatigue assessments after 3-IY Intervention.
Fig. 2.
% Change in the mean of BMI, lipid profile and thyroxin dose after 3-IY Intervention.
4. Discussion
Hypothyroidism and depression share many common symptoms. According to literature, the prevalence of depression in patients with hypothyroidism is high. Depression in hypothyroidism may worsen the symptoms and aggravate the disease process because it is positively associated with the TPO-Ab level in hypothyroidism. Therefore, the prevention and management of depression must be considered in hypothyroidism.
Studies have demonstrated the positive roles of yoga in depression as well as in hypothyroidism.18,19 The present study assessed the effect of a 3-IY on depression and sTSH levels among women having hypothyroidism with clinical depression. The BMI, lipid profiles, anxiety, stress, and fatigue relevant to both hypothyroidism and depression were also evaluated. A significant decrease in depression and sTSH levels was observed following the 3-IY compared with the corresponding baseline levels. Fatigue, stress, BMI, lipid profile (HDL improved) and anxiety were also reduced significantly. This preliminary pilot study suggests a positive effect of yoga on women with hypothyroidism associated with clinical depression.
To the best of our knowledge, this is the first study to evaluate the efficacy of yoga in women having hypothyroidism associated with depression.
Studies have demonstrated the positive effects of yoga intervention on sTSH levels among women with hypothyroidism. Neelakanthan et al. (2016) observed a significant reduction in sTSH levels, lipid profile, and BMI following 6 months of yoga intervention. Other studies have reported improvement in pulmonary function tests and quality of life following yoga intervention in women with hypothyroidism.20,21 Studies on yoga in depression have reported improvement in depression symptoms, mood, cognitive functions, and serum cortisol levels22,23; findings of the present study are consistent with those of these studies.
The present study suggests yoga as an effective intervention for the prevention and management of depression in hypothyroidism. Depression often leads to reduced interest in activity and aversion to exercise. This may lead to the worsening of hypothyroidism. Minimisation of depression in hypothyroidism would encourage physical activity in patients, which further helps in reducing BMI and improving the thyroid function. We recommend yoga for patients with hypothyroidism because it helps in improving both hypothyroidism and depression.
Dyslipidaemia and depression are the independent risk factors of heart disease. Hypothyroidism contributes to increased risk of heart disease as it characterized by dyslipidaemia and increased risk of depression. Previous study by Nilankatan and the present study have demonstrated a positive impact of yoga on lipid profile. Hence, yoga may have cardio-protective effect in hypothyroidism by reducing dyslipidaemia and depression. It also lead to decrease in the BMI.
The exact mechanism of yoga is yet to be explored. The decrease in TSH levels and depression may be attributed to increased levels of physical activity following the 3-IY as it involves several dynamic movements.24,25 Stress may aggravate the underlying autoimmunity, whereas yoga helps in reducing sympathetic arousal and the activity of the hypothalamus–pituitary–adrenal axis, which in turn reduces stress and anxiety levels. Yoga is found to be effective in improving Gamma amino butyric acid levels (GABA), and brain-derived neurotrophic hormone (BDNF) which are known to have positive role in depression.26,27
The present study is the first to assess the efficacy of yoga in depression among women with hypothyroidism having mild-to-moderate depression. At screening 50.6% females had mild-to-moderate depression. Although the sample size of 198 is insufficient to draw a conclusion regarding the prevalence rate, we observed a depression prevalence rate of 50.6%. More than 92% of the participants attended at least 58 of the 60 yoga sessions, suggesting the acceptance and feasibility of the intervention. The % decrease in depression and sTSH levels was statistically significant, supported by a larger effect size. The study showed a significant improvement in all the measures this suggests that 1) women with hypothyroidism are sensitive to such interventions, 2) 3 months yoga intervention is adequate to bring the change in HPA axis and psychological measures. Previous studies have also demonstrated similar results. A study by Mischalsen reported significant decrease in anxiety, depression, joint pain, mood state wellbeing, psychological quality of life and bodily complaints well among distressed women following 3-months yoga intervention.25,28
The present study has several limitations such as a small sample size, lack of a control group, and lack of objective parameters of depression.
Further studies with a large sample size, longer duration of intervention, and active control groups are recommended to generalise the findings. Additionally, we recommend the study of objective variables such as salivary cortisol levels, serotonin, and TPO-Ab.
5. Conclusion
The present study indicates the positive effect of 3-IY on reduced depression and sTSH levels in women with hypothyroidism. Further studies with a larger sample size and a robust research design using more objective variables are required to strengthen the findings.
Ethics committee reference
Institutional Project Evaluation/Ethics Committee of Distance Education, SVYASA University approved the study (DDE-PEC-021-2018). The study was approved by the research project evaluation committee.
Declaration of competing interest
All authors have reviewed and approved the final version of the article for publication.
All authors declare no conflict of interest in publishing the article in eJTCM.
This study is not funded by any government or non-government funding agency.
Acknowledgement
We are thankful to all the female participants for their participation in this study.
Footnotes
Peer review under responsibility of The Center for Food and Biomolecules, National Taiwan University.
Contributor Information
S. Rani, Email: ranishakti123@gmail.com.
Satyapriya Maharana, Email: trisatyapriya77@gmail.com.
Kashinath G. Metri, Email: kashinath@curaj.ac.in, kgmhetre@gmail.com.
Hemant Bhargav, Email: drbhargav.nimhans@gmail.com.
R. Nagaratna, Email: rnagaratna@gmail.com.
References
- 1.Deokar P.G., Nagdeote A.N., Lanje M.J., Basutkar D.G. Prevalence of thyroid disorders in a tertiary care center. International Journal of Current Research and Review. 2016 May 1;8(9):26. [Google Scholar]
- 2.Hak A.E., Pols H.A., Visser T.J., Drexhage H.A., Hofman A., Witteman J.C. Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: the Rotterdam Study. Ann Intern Med. 2000 Feb 15;132(4):270–278. doi: 10.7326/0003-4819-132-4-200002150-00004. [DOI] [PubMed] [Google Scholar]
- 3.Wolkowitz O.M., Rothschild A.J. first ed. American Psychiatric; Washington, DC, USA: 2003. Psychoneuroendocrinology: The Scientific Basis of Clinical Practice. [Google Scholar]
- 4.Tappy L., Randin J.P., Schwed P., Wertheimer J., Lemarchand-Béraud T. Prevalence of thyroid disorders in psychogeriatric inpatients A possible relationship of hypothyroidism with neurotic depression but not with dementia. J Am Geriatr Soc. 1987 Jun;35(6):526–531. doi: 10.1111/j.1532-5415.1987.tb01399.x. [DOI] [PubMed] [Google Scholar]
- 5.Whybrow P.C., Prange A.J., Jr., Treadway C.R. Mental changes accompanying thyroid gland dysfunction. A reappraisal using objective psychological measurement. Arch Gen Psychiatr. 1969;20(1):48–63. doi: 10.1001/archpsyc.1969.01740130050004. [DOI] [PubMed] [Google Scholar]
- 6.Haggerty J.J., Stern R.A., Mason G.A., Beckwith J., Morey C.E., Prange A.J. Subclinical hypothyroidism: a modifiable risk factor for depression? Am J Psychiatr. 1993;150(3):508–510. doi: 10.1176/ajp.150.3.508. [DOI] [PubMed] [Google Scholar]
- 7.Loh H.H., Lim L.L., Yee A., Loh H.S. Association between subclinical hypothyroidism and depression: an updated systematic review and meta-analysis. BMC Psychiatr. 2019 Dec 1;19(1):12. doi: 10.1186/s12888-018-2006-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rack S.K., Makela E.H. Hypothyroidism and depression: a therapeutic challenge. Ann Pharmacother. 2000 Oct;34(10):1142–1145. doi: 10.1345/aph.10022. [DOI] [PubMed] [Google Scholar]
- 9.Mohammad M.Y., Bushulaybi N.A., AlHumam A.S. Prevalence of depression among hypothyroid patients attending the primary healthcare and endocrine clinics of King Fahad Hospital of the University (KFHU) J Fam Med Prim Care. 2019 Aug;8(8):2708. doi: 10.4103/jfmpc.jfmpc_456_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Demartini B., Masu A., Scarone S., Pontiroli A.E., Gambini O. Prevalence of depression in patients affected by subclinical hypothyroidism. Panminerva Med. 2010 Dec;52(4):277–282. [PubMed] [Google Scholar]
- 11.Talaei A., Rafee N., Rafei F., Chehrei A. TSH cut off point based on depression in hypothyroid patients. BMC Psychiatr. 2017 Dec 1;17(1):327. doi: 10.1186/s12888-017-1478-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fountoulakis K.N., Iacovides A., Grammaticos P., St Kaprinis G., Bech P. Thyroid function in clinical subtypes of major depression: an exploratory study. BMC Psychiatr. 2004 Dec;4(1):6. doi: 10.1186/1471-244X-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spencer C.A., Takeuchi M., Kazarosyan M., MacKenzie F., Beckett G.J., Wilkinson E. Interlaboratory/intermethod differences in functional sensitivity of immunometric assays of thyrotropin (TSH) and impact on reliability of measurement of subnormal concentrations of TSH. Clin Chem. 1995 Mar 1;41(3):367–374. [PubMed] [Google Scholar]
- 14.Henry J.D., Crawford J.R. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005 Jun 1;44(2):227–239. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- 15.Singh K., Junnarkar M., Sharma S. Anxiety, stress, depression, and psychosocial functioning of Indian adolescents. Indian J Psychiatr. 2015 Oct;57(4):367. doi: 10.4103/0019-5545.171841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee K.A., Hicks G., Nino-Murcia G. Validity and reliability of a scale to assess fatigue. Psychiatr Res. 1991 Mar 1;36(3):291–298. doi: 10.1016/0165-1781(91)90027-m. [DOI] [PubMed] [Google Scholar]
- 17.Spratt K.F. Minimal clinically important difference based on clinical judgment and minimally detectable measurement difference: a rationale for the SF-36 Physical Function scale in the SPORT Intervertebral disc herniation cohort. Spine. 2009 Jul 15;34(16):1722. doi: 10.1097/BRS.0b013e3181a8faf2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Banerjee S. Study on yoga intervention along with diet on hypothyroidism associated with obesity among sedentary working women in West Bengal. International Journal of Yoga and Allied Sciences. 2019;1:2278–5159. [Google Scholar]
- 19.Cramer H., Lauche R., Langhorst J., Dobos G. Yoga for depression: a systematic review and meta-analysis. Depress Anxiety. 2013 Nov;30(11):1068–1083. doi: 10.1002/da.22166. [DOI] [PubMed] [Google Scholar]
- 20.Halder K., Chatterjee A., Kain T.C., Pal R., Tomer O.S., Saha M. Improvement in ventilatory function through yogic practices. Al Ameen J Med Sci. 2012;5(2):197–202. [Google Scholar]
- 21.Swami G, Singh S, Singh KP, Gupta M. Effect of yoga on pulmonary function tests of hypothyroid patients. Indian J Physiol Pharmacol. 2010 Mar;54(1):51–56. [PubMed] [Google Scholar]
- 22.Cramer H., Lauche R., Langhorst J., Dobos G. Yoga for depression: a systematic review and meta-analysis. Depress Anxiety. 2013 Nov;30(11):1068–1083. doi: 10.1002/da.22166. [DOI] [PubMed] [Google Scholar]
- 23.Woolery A., Myers H., Sternlieb B., Zeltzer L. A yoga intervention for young adults with elevated symptoms of depression. Alternative Ther Health Med. 2004 Mar 1;10(2):60–63. [PubMed] [Google Scholar]
- 24.Steptoe A. Depression and physical activity. Depression and physical illness. 2006 Jan 1:348–368. [Google Scholar]
- 25.Ciloglu F., Peker I., Pehlivan A. Exercise intensity and its effects on thyroid hormones. Neuroendocrinol Lett. 2005 Dec 1;26(6):830–834. [PubMed] [Google Scholar]
- 26.Streeter C.C., Gerbarg P.L., Saper R.B., Ciraulo D.A., Brown R.P. Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Med Hypotheses. 2012 May 1;78(5):571–579. doi: 10.1016/j.mehy.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 27.Cahn B.R., Goodman M.S., Peterson C.T., Maturi R., Mills P.J. Yoga, meditation and mind-body health: increased BDNF, cortisol awakening response, and altered inflammatory marker expression after a 3-month yoga and meditation retreat. Front Hum Neurosci. 2017 Jun 26;11:315. doi: 10.3389/fnhum.2017.00315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Michalsen A., Grossman P., Acil A. Rapid stress reduction and anxiolysis among distressed women as a consequence of a three-month intensive yoga program. Med Sci Mon Int Med J Exp Clin Res. 2005 Dec 1;11(12):CR555–C561. [PubMed] [Google Scholar]