Abstract
Objective
To assess demographic characteristics and perceptions of female physicians in attendance at a medical conference for women with content focused on growth, resilience, inspiration, and tenacity to better understand major barriers women in medicine face and to find solutions to these barriers.
Patients and Methods
A Likert survey was administered to female physicians attending the conference (September 20 to 22, 2018). The survey consisted of demographic data and 4 dimensions that are conducive to women’s success in academic medicine: equal access, work-life balance, freedom from gender biases, and supportive leadership.
Results
All of the 228 female physicians surveyed during the conference completed the surveys. There were 70 participants (31.5%) who were in practice for less than 10 years (early career), 111 (50%) who were in practice for 11 to 20 years (midcareer), and 41 (18.5%) who had more than 20 years of practice (late career). Whereas participants reported positive support from their supervisors (mean, 0.4 [SD 0.9]; P<.001), they did not report support in the dimensions of work-life balance (mean, −0.2 [SD 0.8]; P<.001) and freedom from gender bias (mean, −0.3 [SD 0.9]; P<.001).
Conclusion
Female physicians were less likely to feel support for work-life balance and did not report freedom from gender bias in comparison to other dimensions of support. Whereas there was no statistically significant difference between career stage, trends noting that late-career physicians felt less support in all dimensions were observed. Future research should explore a more diverse sample population of women physicians.
Abbreviations and Acronyms: CCWAS, culture conducive to women’s academic success; CME, continuing medical education; GRIT, growth, resilience, inspiration, and tenacity
Gender disparities remain a persistent problem in medical practice. Women compose more than half of medical school matriculates yet occupy only a minority of active leadership roles and academic appointments in health care centers in the United States. In 2015, only 14.6% of women were chairs of their clinical departments.1 Although female faculty in academic health centers grew quickly from less than 10% in 1975 to 33% in 2006, this growth has stalled at 38% since 2008.2 In the past decade, the proportion of women in executive positions has also plateaued.2
Women’s historical marginalization and continued exclusion from leadership in medicine is complex and multifactorial and surfaces at multiple levels. A wide spectrum in gender climate among institutions was found in 1 qualitative study involving phone interviews of senior leaders at 24 medical schools, with a prevailing lack of gender parity in leadership and rank across all institutions.3 Participants revealed a lack of retention of women, an inequity in compensation, and a disproportionate responsibility for household responsibilities, consistent with previous findings.4 Women in academic surgical positions identified gender as a barrier to their career development and reported anticipation or experiences of overt discrimination in the form of being treated unequally and being subjected to negative comments about their gender.5 A retrospective, observational study of video-archived speaker introductions at Internal Medicine Grand Rounds at a major academic medical center found evidence of gender bias.6 Male introducers of female speakers used professional titles for female colleagues 49.2% (31/63) of the time (P<.001) compared with 72.4% (110/152) of the time for men (P=.007).6
Gender discrimination and disparity in academic medicine are further exacerbated by inequity in compensation and advancement.7 Female faculty are reportedly less likely than men to be full professors with similar professional roles and achievements (similar years of seniority) and are underpaid in comparison to their male counterparts.8 Even with adjustment for differences in specialty, productivity, academic rank, and work hours, men were found to earn significantly more, averaging $12,194 more per year.4 Nearly 40% of academic medical institutions were found to lack dedicated programs for recruiting, promoting, or retaining women in 1 qualitative study.9 Where programs did exist, they focused on individual and interpersonal interventions simultaneously, including mentoring, training, and formal communication about promotion.9 At an institutional level, search committees, data tracking, child and elderly care, and spousal hiring programs were key methods used to begin to address gender inequities.9
Solutions to address gender discrimination and to mitigate gender disparity are slowly gaining traction, with emerging research identifying key impactful areas for improvement in academic medicine. A faculty survey across 13 medical schools found that having an office for women's affairs, trust in leadership, and satisfaction with mentoring were favorably associated with a positive climate for women and were inversely associated with perceived workplace discrimination and work-family conflict.10 Career development programs have been found to lead to slightly increased retention of women in leadership roles and a decreased likelihood of leaving academic medicine roles compared with men or non–career development program women.11
The culture of a work environment can inhibit women’s career success in academic medicine. In 2012, Westring et al12 developed a validated survey focusing on 4 distinct career aspects of culture conducive to women’s academic success (CCWAS), which included equal access to opportunities and resources, work-life balance (support from those at work), freedom from gender biases, and supportive department/division leadership.12 This survey was administered to female assistant professors at a single institution, and the authors found that women in the same departments/divisions were in agreement on the support in their sector; however, there was variability among the different sectors.13 Increased work demands were found to be associated with increased levels of work-family conflict, with the impact of positive work cultures and similar work demands being associated with less work-family conflict.13 The authors concluded that a comprehensive framework with an emphasis on equal access to resources and opportunities reduces unconscious gender bias, enhancing work-life balance and leadership engagement.14
In the current US sociopolitical context, with increasing press attention to occupational, cultural, and political manifestations of inequities, there is a strong need for further investigation into how women perceive, experience, and successfully mitigate gender discrimination and disparity in medicine. This study was created in response to the perceived gap in opportunities for women to build skills to move toward leadership positions, particularly in health care. This study provides a timely investigation to address this gap and to contribute findings with significant implications for policy and practice. With use of the validated survey created by Westring et al,12 with modifications specific to female physicians that did not alter the aim of the survey ( Supplemental Appendix A, available online at http://www.mayoclinicproceedings.org), the CCWAS survey was administered at a large organized gathering of female physicians with the specific intent to educate and to promote growth, resilience, inspiration, and tenacity (GRIT). GRIT is a national Mayo Clinic continuing medical education (CME) leadership conference, a pioneering initiative and novel collaboration across Mayo Clinic with representation and speakers and leaders from other health care institutions. The conference was advertised like other Mayo Clinic CME courses, through their website, social media, and course organizers. The objective of this study was to provide baseline demographic data of attendees and to use these demographic data to compare the workplace culture among the diverse variety of physicians to better understand the major barriers faced by female physicians in various dimensions of work at different phases of their career.
We had several hypotheses involving how dimensions of support would vary by career stage and demographic factors. We hypothesized that early-career physicians (0 to 10 years) would have a decrease in the CCWAS dimension of support for work-life balance in comparison to late-career physicians (20+ years). We also hypothesized that women who scored positively in the dimension of supervisor support (the extent to which the unit leader supports important aspects of women’s careers) would also have higher scores in the dimensions of equal access and freedom from gender bias. Finally, we hypothesized that women would have lower scores in work-life balance if they had children or had a spouse who is a physician compared with a nonphysician.
Patients and Methods
This study was approved by Mayo Clinic Institutional Review Board (18-002325). Participants were female physicians attending the GRIT Mayo Clinic CME course. The event was open to the public, and registration was completed on the Mayo Clinic General Internal Medicine education website. This CME sponsored event occurred September 20 to 22, 2018, in Truckee, California. Female physician attendees who wished to participate were administered the survey in paper format. Participation in the survey was voluntary, and no incentive was offered for completion. The survey was announced and administered to all female physicians present at the conference at the commencement of the program on September 20 at 7:15 am. All surveys were collected as they were completed, by the end of the first day of the conference. Those who were registered for the conference but not present were excluded. Nonphysician health care practitioners were also excluded.
The CCWAS survey was adapted from a publication by Westring et al,12 and modifications were made with the publisher’s approval (Wolters Kluwer). The Mayo Clinic Survey Research Center, Rochester, Minnesota, was used in development of the survey, including design and printing (Supplemental Appendix A). Demographic data were collected (Table 1). Likert survey responses in each of the 4 dimensions (equal access, support for work-life balance, freedom from gender bias, and supervision) were included with 5 answer choices: strongly disagree, disagree, neither agree nor disagree, agree, and strongly agree. Each component that was selected as neither agree nor disagree was scored 0; a positive value was given for a more gender-neutral response and negative values for discriminatory responses (strongly agree/disagree, value of ±2; agree/disagree, value of ±1).
Table 1.
Demographic Data and Characteristics of Female Physician Participants From GRIT Leadership Conference (N=228)a,b
| Sociodemographic variables | ||
| Age (y) | (n=222) | |
| 25-35 | 32 | (14.4) |
| 36-44 | 113 | (50.9) |
| 45-54 | 60 | (27.0) |
| 55-64 | 16 | (7.2) |
| 65+ | 1 | (0.5) |
| Ethnicity | (N=228) | |
| Native American | 4 | (1.8) |
| African American | 7 | (3.1) |
| Hispanic/Latino | 12 | (5.3) |
| Asian/South Asian | 31 | (13.6) |
| Caucasian/white | 170 | (74.6) |
| Multiracial | 4 | (1.8) |
| Place of birth | (n=221) | |
| United States | 181 | (81.9) |
| Other | 40 | (18.1) |
| Current geographic location (US) | (n=222) | |
| Northeast | 13 | (5.9) |
| Midwest | 117 | (52.7) |
| South | 20 | (9.0) |
| West | 72 | (32.4) |
| Highest degree earned by either parent | (n=224) | |
| High-school diploma/GED | 28 | (12.5) |
| Associate degree | 15 | (6.7) |
| Bachelor's degree | 47 | (21.0) |
| Master's degree | 38 | (17.0) |
| Doctorate | 18 | (8.0) |
| Professional | 74 | (33.0) |
| Other | 2 | (0.9) |
| Less than high school | 2 | (0.9) |
| Marital status | (n=222) | |
| Married | 181 | (81.5) |
| Committed partnership | 11 | (5.0) |
| Divorced | 8 | (3.6) |
| Single | 22 | (9.9) |
| Partner works outside the home | (n=191) | |
| Yes, full time | 132 | (69.1) |
| Yes, part time | 25 | (13.1) |
| No | 34 | (17.8) |
| Partner is physician | (n=188) | |
| Yes | 57 | (30.3) |
| No | 131 | (69.7) |
| No. of children | (n=221) | |
| 0 | 50 | (22.6) |
| 1 | 23 | (10.4) |
| 2 | 91 | (41.2) |
| 3 | 45 | (20.4) |
| 4 | 8 | (3.6) |
| ≥5 | 4 | (1.8) |
| Occupational variables | ||
| Country of medical school | (n=224) | |
| United States | 205 | (91.5) |
| Other | 19 | (8.5) |
| Medical degree | (n=225) | |
| MD | 208 | (92.4) |
| DO | 14 | (6.2) |
| Other | 3 | (1.3) |
| Residency graduation year | (n=225) | |
| Before 1990 | 10 | (4.4) |
| 1991-2000 | 38 | (16.9) |
| 2001-2010 | 104 | (46.2) |
| 2011-current | 73 | (32.4) |
| Years of practice (including residency) | (n=222) | |
| 0-5 | 10 | (4.5) |
| 6-10 | 60 | (27.0) |
| 11-20 | 111 | (50.0) |
| 21-30 | 34 | (15.3) |
| ≥31 | 7 | (3.2) |
| Current job status | (n=220) | |
| Resident | 2 | (0.9) |
| Fellow | 2 | (0.9) |
| Attending | 212 | (96.4) |
| Working nonclinically | 4 | (1.8) |
| Main department affiliation | (n=223) | |
| Emergency Medicine | 13 | (6.3) |
| Internal Medicine/subspecialties | 41 | (18.3) |
| Surgery/specialties | 6 | (2.7) |
| Anesthesia | 24 | (10.7) |
| Ophthalmology | 4 | (1.8) |
| Gynecology | 24 | (10.7) |
| Radiology | 4 | (1.8) |
| Pathology/Laboratory Medicine | 2 | (0.9) |
| Neurology | 2 | (0.9) |
| Psychiatry | 6 | (2.7) |
| Dermatology | 5 | (2.2) |
| Other | 92 | (41.1) |
GRIT, Growth, Resilience, Inspiration, and Tenacity for Women in Medicine.
Values are reported as number (%).
Descriptive statistics were used to summarize demographic data and characteristics of survey participants. Before analysis of summary statistics for each dimension (equal access, support for work-life balance, freedom from gender bias, and supervision), standardized Cronbach α was performed for each 4-dimension question that encompassed each score, with all values above 0.70 for all scores (range, −2 to 2). Reasonable normality under the central limit theorem was assumed, and the t-test was used for the analysis of scores from each dimension. For comparative statistics, nonparametric testing (Kruskal-Wallis) was used as the data were ordinal and the sample size was small. Statistical analysis was performed with SAS software (SAS Institute). Significance was set at a P value of less than .05.
Results
There was a 100% response rate, with 228 female physicians participating in the paper survey. There were 70 participants (31.5%) who were in practice for less than 10 years (early career), 111 (50%) who were in practice for 11 to 20 years (midcareer), and 41 (18.5%) who had more than 20 years of practice (late career).
Demographic Characteristics
There were 192 women (86.5%) who were married or in committed partnerships, and of those, 57 (30.3%) were in dual-physician relationships. Of those who were married or partnered, 132 (69.1%) had partners who worked full time outside of the home, compared with 25 (13.1%) who worked part time and 34 (17.8%) who were not currently working outside the home (n=191). Of the participants, 171 (77.4%) had children. More than 90% of the survey participants had a medical degree from a US medical school. Most conference participants self-identified from the Midwest (117 [52.7%]), with the other large majority the West Coast (72 [32.4%]). Only 4 participants were residents and fellows (1.8%); 212 were active staff physicians (96.4%).
CCWAS Domains
Equal Access
Each nondemographic question that was administered as part of the CCWAS fell under the 4 dimensions of equal access, work-life balance, freedom from gender bias, and supervision support (Figure). The overall summary score for the questions in the dimension of equal access (Table 2) was not statistically different from 0 (mean, −0.1 [SD 0.9]; median, −0.2; P=.16) also when accounting for career stage (Table 3). However, midcareer physicians had higher scores in equal access (mean, 0.1 [SD 0.9]) compared with the early-career physicians (mean, −0.1 [SD 0.9]).
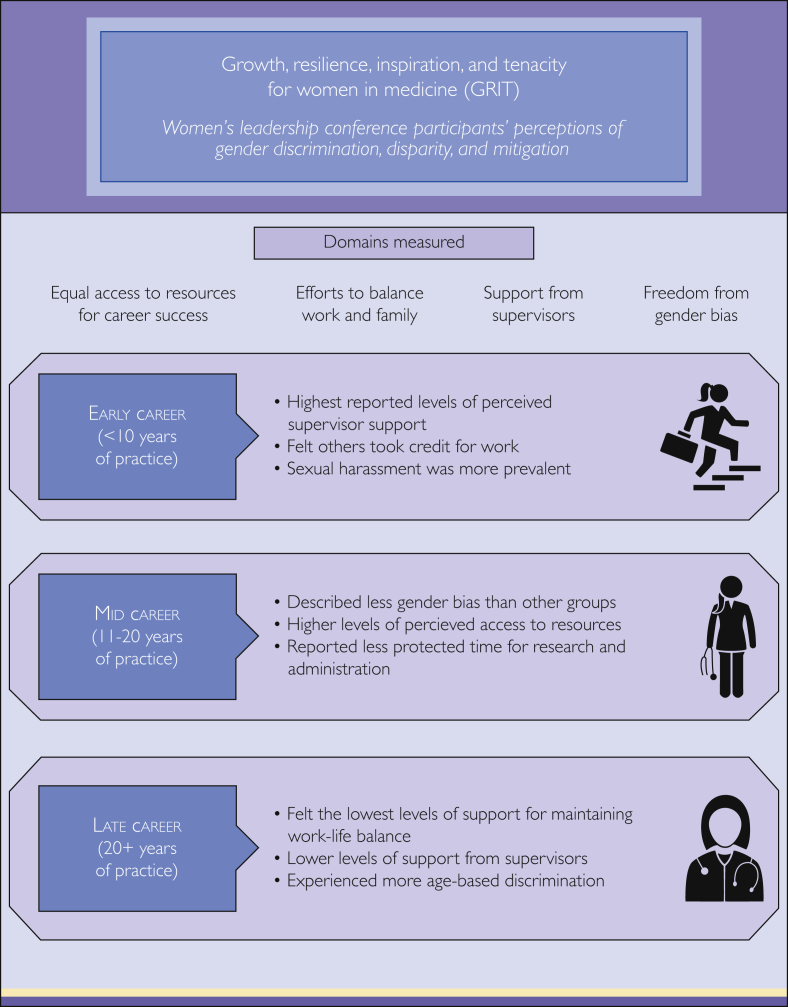
Figure.
Summary of results from Growth, Resilience, Inspiration, and Tenacity for Women in Medicine (GRIT) conference from 4 domains of career support (equal access to resources; efforts to balance work and family; support from supervisors; freedom from gender bias) based on stages of career (early, mid, and late career). Major findings are highlighted for each career stage.
Table 2.
Summary Statistics for 4 Dimensions of Career Aspects of Culture Conducive to Women’s Academic Success (CCWAS)
| Survey domain | No. | Mean (SD) (0=neutral) |
Median | Q1, Q3 | Range | P valuea |
|---|---|---|---|---|---|---|
| Equal accessb | 228 | −0.1 (0.9) | −0.2 | −0.8, 0.6 | (−2.0 to 2.0) | .16 |
| Support for work-life balancec | 220 | −0.2 (0.8) | −0.3 | −0.7, 0.3 | (−2.0 to 2.0) | <.001 |
| Freedom from gender biasd | 219 | −0.3 (0.9) | −0.5 | −1.0, 0.3 | (−2.0 to 2.0) | <.001 |
| Supervision supporte | 219 | 0.4 (0.9) | 0.4 | −0.2, 1.0 | (−1.7 to 2.0) | <.001 |
By t-test.
The extent to which women faculty have equal access to the resources that contribute to career success compared with men.
The extent to which women physicians are supported in their efforts to balance work and family for the achievement of both personal and professional success.
The extent to which women are able to work in an environment in which they are able to voice concerns about subtle and overt gender biases.
The extent to which the unit leader supports important aspects of women’s careers.
Table 3.
Mean Scores for 4 Dimensions of Career Aspects of Culture Conducive to Women’s Academic Success (CCWAS) by Career Stage and Age in GRIT Surveya
| CCWAS domain mean scores by career stage | ||||
|---|---|---|---|---|
| 0-10 y (n=70) | 11-20 y (n=111) | 20+ y (n=41) | P valueb | |
| Equal access | .11 | |||
| No. | 70 | 111 | 40 | |
| Mean (SD) | −0.1 (0.9) | 0.1 (0.9) | −0.3 (0.7) | |
| Median | −0.1 | 0.0 | −0.3 | |
| Q1, Q3 | −0.9, 0.6 | −1.7, −2.0 | −1.4, −1.6 | |
| Support for work-life balance | .03 | |||
| No. | 69 | 106 | 39 | |
| Mean (SD) | −0.2 (0.7) | −0.1 (0.8) | −0.4 (0.7) | |
| Median | −0.2 | −0.2 | −0.3 | |
| Q1, Q3 | −0.7, 0.3 | −0.7, 0.5 | −0.8, 0.0 | |
| Freedom from gender bias | .04 | |||
| No. | 69 | 105 | 39 | |
| Mean (SD) | −0.3 (0.9) | −0.2 (0.9) | −0.6 (0.8) | |
| Median | −0.5 | −0.5 | −0.8 | |
| Q1, Q3 | −0.8, 0.3 | −0.8, 0.5 | −1.3, 0.0 | |
| Supervision support | .05 | |||
| No. | 69 | 106 | 39 | |
| Mean (SD) | 0.5 (0.8) | 0.4 (0.9) | 0.3 (1.0) | |
| Median | 0.4 | 0.5 | 0.2 | |
| Q1, Q3 | −0.1, 0.9 | −0.2, 1.0 | −0.5, 0.2 | |
| CCWAS domain mean scores by age | ||||
|---|---|---|---|---|
| 25-44 y (n=145) | 45-54 y (n=60) | 55+ y (n=17) | P value | |
| Equal access | .47 | |||
| No. | 145 | 60 | 17 | |
| Mean (SD) | −0.1 (0.8) | 0.0 (1.0) | 0.1 (0.7) | |
| Median | −0.1 | −0.2 | 0.1 | |
| Q1, Q3 | −0.8, 0.4 | −0.9, 0.9 | −0.4, 0.4 | |
| Freedom from gender bias | .72 | |||
| No. | 139 | 58 | 16 | |
| Mean (SD) | −0.3 (0.9) | −0.3 (1.0) | −0.2 (0.8) | |
| Median | −0.5 | −0.5 | 0.0 | |
| Q1, Q3 | −0.8. 0.3 | −1.0, 0.5 | −0.8, 0.3 | |
| Supervision support | .40 | |||
| No. | 140 | 58 | 16 | |
| Mean (SD) | 0.4 (0.8) | 0.5 (0.9) | 0.7 (1.1) | |
| Median | 0.4 | 0.6 | 0.8 | |
| Q1, Q3 | −0.2, 1.0 | −0.2, 1.2 | 0.0, 1.6 | |
| CCWAS domain mean scores by number of children (physician family characteristics) | ||||
|---|---|---|---|---|
| 0 (n=50) | 1+ (n=171) | P value | ||
| Equal access | .59 | |||
| No. | 50 | 171 | ||
| Mean (SD) | 0.0 (0.9) | −0.1 (0.9) | ||
| Median | 0.1 | −0.2 | ||
| Q1, Q3 | −0.7, 0.6 | −0.8, 0.6 | ||
| Support for work-life balance | .25 | |||
| No. | 50 | 163 | ||
| Mean (SD) | −0.1 (0.7) | −0.2 (0.8) | ||
| Median | −0.1 | −0.3 | ||
| Q1, Q3 | −0.5, 0.3 | −0.8, 0.3 | ||
| Freedom from gender bias | .26 | |||
| No. | 49 | 163 | ||
| Mean (SD) | −0.2 (0.7) | −0.3 (0.9) | ||
| Median | −0.3 | −0.5 | ||
| Q1, Q3 | −0.8, 0.3 | −1.0, 0.3 | ||
| Supervision support | .82 | |||
| No. | 50 | 163 | ||
| Mean (SD) | 0.5 (0.9) | 0.4 (0.9) | ||
| Median | 0.5 | 0.4 | ||
| Q1, Q3 | −0.1, 1.1 | −0.2, 1.0 | ||
GRIT, Growth, Resilience, Inspiration, and Tenacity for Women in Medicine.
By Kruskal-Wallis test.
Work-Life Balance
In the dimension of support for work-life balance, women physicians overall did not report feeling supported (mean, −0.2 [SD 0.8]; median, −0.3; P<.001), which was statistically significant. Similarly, women physicians experienced gender bias (mean, −0.3 [SD 0.9]; median, −0.5; P<.0001). However, a statistically significant number of participants did feel support from their supervisors (mean, 0.4 [SD 0.9]; median, 0.4; P<.0001; Table 2).
It was hypothesized that early-career physicians (0-10 years) would have a decrease in the CCWAS dimension of support for work-life balance in comparison to late-career physicians (>20 years). The results demonstrated that early-career physicians (mean, −0.2 [SD 0.7]) and midcareer physicians (11-20 years in practice; mean, −0.1 [SD 0.8]) did have a decreased feeling of support for work-life balance, but the lowest support for work-life balance was identified by the late-career physicians (mean, −0.4 [SD 0.7]); however, these results were not statistically significant (P=.16). In addition, individuals who graduated before 2000 scored significantly lower (mean, −0.4 [SD 1.1]; P=.04; n=46) when asked if it was frowned on to take care of personal needs, such as taking time off for sick children (Table 4). Interestingly, when asked if they had less protected time for research and administration, individuals who graduated between the years of 2001 and 2010 indicated that they perceived they had less time by scoring significantly higher (mean, 0.1 [SD 1.2]; P=.04; n=103).
Table 4.
Summary Statistics for Select Individual Questions in GRIT Surveya
| Individual questions by years in practice | ||||
|---|---|---|---|---|
| 0-10 y (n=70) | 11-20 y (n=111) | 20+ y (n=41) | P valueb | |
| Women physicians are more likely to have others take credit for their work. | .02 | |||
| No. | 70 | 111 | 40 | |
| Mean (SD) | −0.8 (1.1) | −0.3 (1.2) | −0.8 (1.0) | |
| Median | −1.0 | −1.0 | −1.0 | |
| Q1, Q3 | −2.0, 0.0 | −1.0, 1.0 | −2.0, 0.0 | |
| Women physicians have less protected time for research and/or administrative tasks. | .03 | |||
| No. | 47 | 103 | 71 | |
| Mean (SD) | −0.3 (1.1) | 0.1 (1.2) | −0.2 (1.0) | |
| Median | −1.0 | 0.0 | 0.0 | |
| Q1, Q3 | −1.0, 0.0 | −1.0, 1.0 | −1.0, 0.0 | |
| Attending to personal needs, such as taking time off for sick children, is frowned upon. | .04 | |||
| No. | 46 | 99 | 72 | |
| Mean (SD) | −0.4 (1.1) | 0.1 (1.2) | 0.1 (1.3) | |
| Median | −0.5 | 0.0 | 0.0 | |
| Q1, Q3 | −1.0, 0.0 | −1.0, 1.0 | −1.0, 1.0 | |
| Individual questions by dual-physician couple | ||||
|---|---|---|---|---|
| Missing (n=40) | No (n=131) | Yes (n=57) | P valueb | |
| Women physicians have equal access to career development opportunities and mentoring. | .05 | |||
| No. | 40 | 130 | 57 | |
| Mean (SD) | −0.2 (1.3) | 0.3 (1.2) | 0.2 (1.3) | |
| Median | −1.0 | 1.0 | 0.0 | |
| Q1, Q3 | −1.0, 1.0 | −1.0, 1.0 | −1.0, 1.0 | |
| Women physicians have less protected time for research and/or administrative tasks. | .05 | |||
| No. | 40 | 127 | 57 | |
| Mean (SD) | −0.1 (1.3) | 0.1 (1.2) | -0.4 (1.1) | |
| Median | 0.0 | 0.0 | 0.0 | |
| Q1, Q3 | −1.0, 0.0 | −1.0, 1.0 | −2.0, 2.0 | |
| Women physicians are frequently recognized for their work. | .03 | |||
| No. | 40 | 131 | 57 | |
| Mean (SD) | −0.4 (1.1) | 0.1 (1.2) | −0.2 (1.2) | |
| Median | 0.0 | 0.0 | −1.0 | |
| Q1, Q3 | −1.0, 1.0 | −1.0, 1.0 | −1.0, 1.0 | |
| Women physicians who temporarily reduce their workload for parenting responsibilities are expected to take on extra work when they return to full time. | .03 | |||
| No. | 39 | 124 | 55 | |
| Mean (SD) | −0.2 (1.2) | 0.2 (1.1) | 0.4 (1.3) | |
| Median | 0.0 | 0.0 | 0.0 | |
| Q1, Q3 | −1.0, 1.0 | −1.0, 1.0 | 0.0, 2.0 | |
GRIT, Growth, Resilience, Inspiration, and Tenacity for Women in Medicine.
By Kruskal-Wallis test.
Freedom From Gender Bias
The most discriminatory domain of the 4 was freedom from gender bias (P=.04) in comparing by career stage (Table 3). Midcareer physicians had higher scores in freedom from gender bias (mean, −0.2 [SD 0.9]) compared with the early-career physicians’ freedom from gender bias (mean, −0.3 [SD 0.9]).
Supervision Support
Last, it was hypothesized that women with higher average scores in the dimension of supervisor support (the extent to which the unit leader supports important aspects of women’s careers) would have higher average scores compared with peers in the dimensions of equal access and freedom from gender bias. In comparing career stage (Table 3), the early-career physicians (0 to 10 years; n=69) had the highest score for leadership/supervision support (mean, 0.5; [SD 0.8]) compared with the midcareer (mean, 0.4 [SD 0.9]), and late-career (mean, 0.3 [SD 1.0]) physicians.
Interestingly, individuals aged 55+ years reported the highest supervisor support mean score (n=16; mean, 0.7 [SD=1.1]; Table 3) and the highest scores for equal access to means and freedom of gender bias compared with those younger than 55 years. It is notable that these are the largest standard deviations and smallest sample sizes in our comparisons.
Physician Family Characteristics
In comparing women physicians with and without children (Table 3), it was observed that respondents who did not have children (n=50 [22%]), reported that they had support from supervision (mean, 0.5 [SD 0.9]), with slightly higher scores in equal access (mean, 0.0 [SD 0.9]) and freedom from gender bias (mean, −0.2 [SD 0.7]) than those with children (n=171 [75%]; equal access: mean, −0.1 [SD 0.9]; freedom from gender bias: mean, −0.3 [SD 0.9]), but these were not statistically significant (P=.59 and P=.26, respectively). Although not significant (P=.25), women physicians who did not have children (n=50) scored higher for support on work-life balance (mean, −0.1 [SD 0.7]) in comparison to women physicians who have 1 or more children (n=171; mean, −0.2 [SD 0.8]).
In comparison of couples who had a spouse who was also a physician (n=57) with those who did not (n=131), women physicians in dual-physician couples tended to have a lower support of work-life balance (mean, −0.2 [SD 0.9]) than those whose spouse was not a physician (mean, −0.1 [SD 0.7]; P=.17). Individuals whose spouse was a physician reported significantly lower scores (mean, −0.4 [SD 1.1]) when asked if they had less protected time for research and administrative tasks in comparison with those who did not have a spouse who was a physician (mean, 0.1 [SD 1.2]; P=.05; Table 4). Similarly, women physicians in dual-physician couples reported a significantly lower score (mean, −0.2 [SD 1.2]; P=.03) when asked if they were recognized for their work. Conversely, women physicians in dual-physician couples did not significantly (mean, 0.4 [SD=1.3]; P=.03;) report they were expected to take on more work when they came back from a reduced workload compared with women physicians whose partner is not a physician.
Conclusion
The GRIT for Women in Medicine conference was created to describe and to offer solutions, resources, and skills to tackle gender discrimination and disparities in medical practice for women physicians. The goal of this research was to understand the major barriers facing this group of women physicians who sought to empower themselves and to understand in which dimensions women felt the least support to help improve content at future conferences and to focus future research in creation of strategies to address these disparities. Female physician participants spanned a wide range of ages, level of training, and ethnicities and had variable home situations. Most were married or in a committed relationship, with a significant other working outside the home in some capacity; almost a third of these significant others were physicians. The overall findings of this study suggest that women physicians feel support from their supervisors across different institutions, but they do not feel support for work-life balance, nor do they feel free from gender bias. These results are consistent across age of physicians, level of career, dual-physician couples, and physicians with children or without children. This was also supported by prior studies using the CCWAS by Westring et al,12 which reported that a supportive work culture appears to buffer the adverse effects of long work hours on work-family conflict, but at a certain point, the protective effect of a supportive culture is lost.13 The aforementioned study was conducted at a single institution with women assistant professors, and in comparison, the results of this study are broadened to female physicians across multiple institutions and practice settings.
Whereas findings comparing early- and late-career physicians were statistically significant, the opposite of what was hypothesized actually occurred: late-career physicians self-reported more negative scores (increased discriminatory scores in all 4 dimensions of support) on the CCWAS compared with early-career physicians. These findings suggest that late-career women physicians tend to face challenges different from those of their early-career colleagues, leading to lower scores in all dimensions, most notably freedom from gender bias. Recently published literature surveying older female physicians nationally reported that these physicians face struggles of financial insecurity, family responsibilities including caretaker roles for family members (20% of late career physicians), and continued occurrence of sexual harassment.15 Whereas this study found that sexual harassment was more prevalent early in careers (51.9%) vs late in a career (27.4%), data from focus groups that included participants of this study (reported elsewhere) suggest that the nature of the sexual harassment is related to clinical competence and technical incompetence associated with age (or being “out of date”). Age-based discrimination has been reported in 28.1% of late-career physicians, and the authors noted that loneliness prevalence in this group included more than one-third of respondents.15 Further study of this specific group of women physicians is needed as the struggles they faced as the initial pioneers as women in medicine may be different. This is in contrast to the current early-career physicians who matriculated into medical school when there was an increased prevalence of women in their classes and as mentors. Specific targeted strategies must be studied and developed for later career women physicians, although this is not enough alone to improve the lives and careers of all women physicians.
Women physicians with children had scores demonstrating less support in all 4 dimensions; however, none of these were statistically significant. Buddeberg-Fischer et al16 reported that women physicians who had children viewed their career success and feeling of support less highly than male colleagues did. In addition, work-life balance struggles were noted to be more prevalent.16 Solutions that have been noted as possible options include mentoring programs, flexible career structures, and expanded onsite support for childcare.16,17
Women in dual-physician relationships did not have statistically significant scores compared with their colleagues who were in a non–dual-physician relationship. A previous study18 surveying female physicians in academic medicine reported that having a partner who is a physician was beneficial because their spouses were understanding and supportive. Difficulties in this scenario include scheduling conflicts, especially surrounding childcare.18 Although not statistically significant, the results of this study indicating that women not in relationships had lower scores (in all dimensions) than those in relationships may suggest that women physicians without a supportive significant other at home may actually need more support. We do know from past literature that women physicians struggle with the work-family conflict more than other professionals do.17 Having a supportive spouse at home and a mentor at work are methods for enhancing work-family balance.18 Further studies analyzing specific and targeted interventions that have been briefly mentioned here in much of the literature should be conducted to create structural and organizational changes to support women both at home and at work.
Whereas it is difficult to extrapolate data solely on the basis of demographic characteristics alone, it is notable that the women physicians who seek out this type of CME and professional development conferences may be those typically juggling family commitments outside of work. Lectures, including time management strategies, leadership skills, emotional intelligence, and boosting resilience, may be attracting this demographic of female physicians, suggesting a need for methods to support female physicians’ careers. Further study on what skills female physicians perceive themselves to be lacking in their career development would be an opportunity for capitalization on supporting this demographic of physicians and understanding their motivations for attendance at academic meetings.
Several limitations should be noted. First, the population of female physicians participating in this survey was a self-selecting group, with a likely passion for gender equity, as they are on the forefront in attending this novel conference designed to bolster GRIT for women in medicine. However, a majority of our participants were white, midcareer physicians from the Midwest. More than half of the participants were from the Midwest, and a large number were from Mayo Clinic, Rochester, Minnesota. Thus, this study’s sample population may not be representative of all academic medical centers. Furthermore, not all participants at the conference were in academic medicine, and this was not elicited on the survey but could be a confounding factor because of the survey’s being designed for the sole use of academia. The study is also limited in diversity in regard to race/ethnicity and was unable to note differences in the data on the basis of this demographic sample, possibly because of smaller sample sizes.
Women physicians who attended a CME conference geared toward developing GRIT in medicine were surveyed. Whereas there was general agreement that supervisors were supportive, scores revealed that women were more likely to feel low levels of support for work-life balance and did not feel free from gender bias. Although there were no statistically significant differences between career stages (early, mid, and late), trends noting that late-career physicians felt less support overall were observed. Further research is needed to better understand and to create solutions around the barriers to support at an institutional level and how different dimensions of support affect women physicians in the workplace. Future studies focused on the barriers of senior physicians and conducting this modified survey on a more diverse group of women physicians would continue to build on this work. This study has already helped inform programming for upcoming GRIT conferences in the hope of continuing to empower women physicians to understand barriers they face in medicine for creating solutions for the future.
Acknowledgments
The authors would like to thank the organizers, speakers, and participants of the GRIT Mayo Clinic CME course.
Footnotes
Grant Support: Survey and statistical support was provided by funding from the Mayo Clinic General Internal Medicine Continuing Medical Education Committee.
Potential Competing Interests: The authors report no competing interests.
Supplemental material can be found online at http://www.mayoclinicproceedings.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
Supplemental Online Material
References
- 1.Association of American Medical Colleges Statistics—Group on Women in Medicine and Science (GWIMS) https://www.aamc.org/members/gwims/statistics/
- 2.Helitzer D.L., Newbill S.L., Cardinali G., Morahan P.S., Chang S., Magrane D. Changing the culture of academic medicine: critical mass or critical actors? J Womens Health (Larchmt) 2017;26(5):540–548. doi: 10.1089/jwh.2016.6019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carr P.L., Gunn C., Raj A., Kaplan S., Freund K.M. Recruitment, promotion, and retention of Women in academic medicine: how institutions are addressing gender disparities. Womens Health Issues. 2017;27(3):374–381. doi: 10.1016/j.whi.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carr P.L., Gunn C.M., Kaplan S.A., Raj A., Freund K.M. Inadequate progress for women in academic medicine: findings from the national faculty study. J Womens Health (Larchmt) 2015;24(3):190–199. doi: 10.1089/jwh.2014.4848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cochran A., Hauschild T., Elder W.B., Neumayer L.A., Brasel K.J., Crandall M.L. Perceived gender-based barriers to careers in academic surgery. Am J Surg. 2013;206(2):263–268. doi: 10.1016/j.amjsurg.2012.07.044. [DOI] [PubMed] [Google Scholar]
- 6.Files J.A., Mayer A.P., Ko M.G., et al. Speaker introductions at internal medicine grand rounds: forms of address reveal gender bias. J Womens Health (Larchmt) 2017;26(5):413–419. doi: 10.1089/jwh.2016.6044. [DOI] [PubMed] [Google Scholar]
- 7.Acosta D.A. February 9-10, 2018. Setting the stage: the current state of affairs—diversity in medical education. Presented at: Pathways to Physician Diversity: A National Summit. Phoenix, AZ. [Google Scholar]
- 8.Ash A.S., Carr P.L., Goldstein R., Friedman R.H. Compensation and advancement of women in academic medicine: is there equity? Ann Intern Med. 2004;141(3):205–212. doi: 10.7326/0003-4819-141-3-200408030-00009. [DOI] [PubMed] [Google Scholar]
- 9.U.S. medical school acceptance rate by select race and ethnicity . February 9-10, 2018. 2015. AAMC Data Warehouse: Applicant and Matriculant File. Presented at: Pathways to Physician Diversity: A National Summit. Phoenix, AZ. [Google Scholar]
- 10.Carapinha R., McCracken C.M., Warner E.T., Hill E.V., Reede J.Y. Organizational context and female faculty's perception of the climate for women in academic medicine. J Womens Health (Larchmt) 2017;26(5):549–559. doi: 10.1089/jwh.2016.6020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang S., Morahan P.S., Magrane D., et al. Retaining faculty in academic medicine: the impact of career development programs for women. J Womens Health (Larchmt) 2016;25(7):687–696. doi: 10.1089/jwh.2015.5608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Westring A.F., Speck R.M., Sammel M.D., et al. A culture conducive to women’s academic success: development of a measure. Acad Med. 2012;87(11):1622–1631. doi: 10.1097/ACM.0b013e31826dbfd1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Westring A.F., Speck R.M., Sammel M.D., et al. Culture matters: the pivotal role of culture for women’s careers in academic medicine. Acad Med. 2014;89(4):658–663. doi: 10.1097/ACM.0000000000000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Westring A., McDonald J.M., Carr P., Grisso J.A. An integrated framework for gender equity in academic medicine. Acad Med. 2016;91(8):1041–1044. doi: 10.1097/ACM.0000000000001275. [DOI] [PubMed] [Google Scholar]
- 15.Templeton K., Nilsen K.M., Walling A. Issues faced by senior women physicians: a national survey. J Womens Health (Larchmt) 2020;29(7):980–988. doi: 10.1089/jwh.2019.7910. [DOI] [PubMed] [Google Scholar]
- 16.Buddeberg-Fischer B., Stamm M., Buddeberg C., et al. The impact of gender and parenthood on physicians' careers—professional and personal situation seven years after graduation. BMC Health Serv Res. 2010;10:40. doi: 10.1186/1472-6963-10-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Treister-Goltzman Y., Peleg R. Female physicians and the work-family conflict. Isr Med Assoc J. 2016;18(5):261–266. [PubMed] [Google Scholar]
- 18.Schrager S., Kolan A., Dottl S.L. Is that your pager or mine: a survey of women academic family physicians in dual physician families. WMJ. 2007;106(5):251–255. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.