Abstract
Objective
To highlight the current global trends in mortality for cardiovascular disease and cancer.
Methods
The World Health Organization and the World Bank DataBank databases were used to analyze mortality rates for cancer and cardiovascular disease by calculating age-standardized mortality rates (ASRs) from 2000 to 2015 for high-income, upper-middle-income, and lower-middle-income countries. Data for cancer mortality and population for 43 countries representing 5 of the 7 continents (except Australia and Antarctica) were analyzed.
Results
From 2000 to 2015, there was an increase in the ASR for cancer for both men and women irrespective of a country’s income status, representing an overall 7% increase in cancer ASR (Pearson r, +0.99; P<.00001). We report a higher ASR for cancer in high-income countries than in upper-middle-income and lower-middle-income countries specifically; high-income countries saw a 3% increase in cancer ASR vs +31% for upper-middle-income and +19% for lower-middle-income countries (P<.01). There has been a decrease in the ASR for cardiovascular disease for the 15 years analyzed (P<.00001). In addition, high-income countries had a higher ASR for cardiovascular disease than upper-middle-income countries during the 15-year period (P<.05).
Conclusion
We suspect that because of early detection and targeted interventions, cardiovascular disease mortality rates have decreased during the past decade. On the basis of our results, cancer mortality rates continue to rise, with the projection of surpassing cardiovascular disease mortality rates in the near future.
Abbreviations and Acronyms: ASR, age-standardized mortality rate; GBD, Global Burden of Disease; GNI, gross national income; WHO, World Health Organization
The Centers for Disease Control and Prevention and the World Health Organization (WHO) have both recognized cancer and cardiovascular disease as a major global public health burden and the leading causes of death both nationally and internationally.1 Worldwide, cardiovascular disease and cancer accounted for 26.7 million deaths in 2015, with estimated health care cost in billions of dollars every year.1, 2, 3, 4, 5, 6, 7, 8, 9 In 2009, it was estimated that cancer cost the European Union nearly €75 billion.10 It estimated that in 2020, health care cost for cancer in the United States alone was upward of $150 billion.11 Moreover, both cancer and cardiovascular disease are associated with increased number of years lived with disability, years of life lost, and disability-adjusted life-years; thus, several billions of dollars have been dedicated to research and government policies to help understand the causes of these diseases and to improve outcomes for patients diagnosed with these conditions.1 Although cardiovascular disease mortality rates were twice as high as cancer mortality rates in 1970,12, 13, 14, 15 cardiovascular disease mortality rates have declined significantly in the past 3 decades, whereas cancer mortality rates have been on the rise.13, 14, 15 This could be due to improved early detection, prevention, and treatment measures of cardiovascular diseases, coupled with increasing longevity of the general population, which has led to high prevalence of cancer—a disease of aging. Despite significant research on both diseases, direct comparison between cardiovascular disease and cancer mortality rates has received limited attention. Within the United States, it has been noted that in low-income countries, cardiovascular disease is more likely to be the leading cause of death compared with cancer. In addition, these low-income countries have seen a substantially smaller decrease in cardiovascular mortality rates compared with high-income countries. Another recent report from the United States investigating cancer mortality rates of those younger than 65 years suggests that states that adopted Medicaid expansions saw a 29% decrease in cancer mortality rates between 2011-2013 and 2015-2017. These results highlight that even in high-income countries, increased access to quality cancer care is a key to reducing cancer mortality.16
In this article, we provide a direct comparison between cardiovascular disease and cancer mortality rates using the comprehensive WHO database and World Bank DataBank. We calculated age-standardized mortality rates (ASRs) from 2000 to 2015 for high-income, upper-middle-income, and lower-middle-income countries to assess recent trends in cardiovascular disease and cancer prevalence. We aimed to illuminate the current mortality trends for these 2 diseases so current and future leaders can examine strategies for the prevention and control of these leading causes of noncommunicable disease death in the world.
Methods
Data Source
Data were obtained from the WHO Mortality Database and the World Bank DataBank.17,18 The WHO Mortality Database collects mortality data broken down by age, sex, and cause of death from individual countries across the world. The WHO has collected mortality data annually since 1979. However, not every country has consistently reported their data. The World Bank DataBank contains population data by country and sex from 1960 to 2017. Data were collected from 2000 to 2015 for select countries, which were chosen on the basis of the availability of complete data from both databases for the years covered in the study (see details in Inclusion Criteria). Raw mortality data were abstracted by sex (male, female, or unknown), International Classification of Diseases, Tenth Revision (ICD-10) code for cardiovascular disease (I00-09, I11, I13, and I20-51) and cancer (C00-C97),18,19 and age. Because of a lack of data from many countries before 2000, we restricted the data range from 2000 to 2015; the Cause of Death Query Online tool was used to draw data from 2000 to 2015. The ICD-10 codes C00-C97 (cancer) and I00-09, I11, I13, and I20-51 (cardiovascular disease) were extracted.18,19 Because this study used publicly available deidentified data, the study was determined to be exempt from Institutional Review Board review.
Inclusion Criteria
Countries were chosen on the basis of data availability; 43 countries (in alphabetical order: Argentina, Aruba, Belgium, Belize, Bermuda, Brazil, Chile, Colombia, Croatia, Czech Republic, Denmark, Ecuador, Arab Republic of Egypt, Estonia, Finland, Germany, Hungary, Iceland, Israel, Japan, Kyrgyz Republic, Latvia, Lithuania, Luxembourg, Malta, Mexico, Moldova, Netherlands, Nicaragua, Norway, Panama, Peru, Poland, Puerto Rico, Republic of Korea, Romania, Serbia, Slovenia, South Africa, Spain, Sweden, Switzerland, United States of America) had data from 2000 to 2015 in both the WHO Mortality Database with ICD-10 coding and the World Bank DataBank (Supplemental Table, available online at http://mcpiqojournal.org). We defined cancer and cardiovascular disease on the basis of the Centers for Disease Control and Prevention and WHO standards.17, 18, 19, 20, 21 Mortality counts were grouped by age (0 to 20 years, 20 to 64 years, 65+ years, or unknown), sex (male, female, or unknown), country, and cause of death (ICD-10 codes). Countries were classified using the World Bank Atlas method, which groups country economies on the basis of gross national income (GNI) per capita (high income, upper middle income, lower middle income, low income; Supplemental Table).19 However, because of the unavailability of data, our analysis did not include any low-income countries.
Variables
Based on data from the WHO database and the World Bank DataBank, we calculated the ASR stratified by a country’s income status, sex, and time (per year) per 100,000 persons. The ASR per 100,000 persons calculated in a standardized population and by a country’s income status was grouped into high (>$12,056 GNI per capita), upper middle ($3896-$12,055 GNI per capita), and lower middle ($996-$3895 GNI per capita).18 Sex was classified as male or female; deaths due to cardiovascular disease or cancer of individuals with unknown sex were included only in the total mortality counts.
Statistical Analyses
The ASRs per 100,000 persons were calculated using the WHO mortality data and the World Bank DataBank population data. The rates were standardized to 5-year interval age groups using the world standard population adapted from the WHO. Rates were calculated by year, sex (male or female), and age (0 to 20 years, 20 to 64 years, 65+ years). Linear regression analyses with Pearson correlation were performed to study mortality trends from 2000 to 2015. Additional bivariate statistical analyses that included Wilcoxon test and analysis of variance testing were performed to determine differences between income status groups and sexes.
Results
Standard mortality rates instead of counts were analyzed among 43 countries to account for differences in population sizes across countries and across different time periods. However, because mortality counts are easier to comprehend, we present both the raw count data and the standardized age-adjusted rates. Breakdown of countries by income status is presented in the Supplemental Table. Data for cancer and cardiovascular disease mortality and population for 43 countries representing 5 of the 7 continents (except Australia and Antarctica) were analyzed.
Cancer Mortality Rate Trends
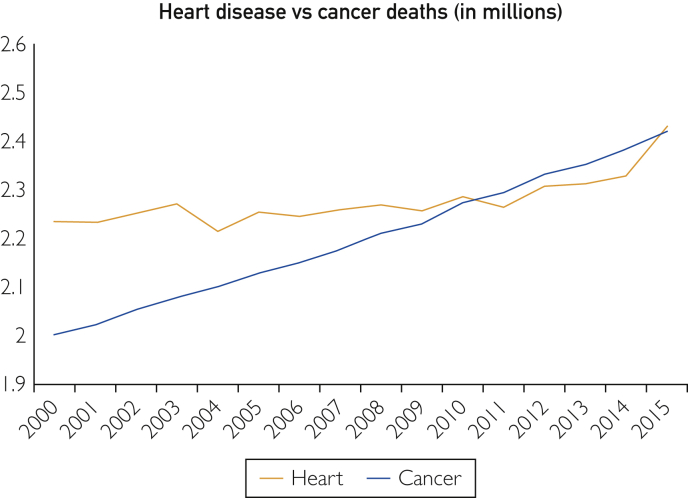
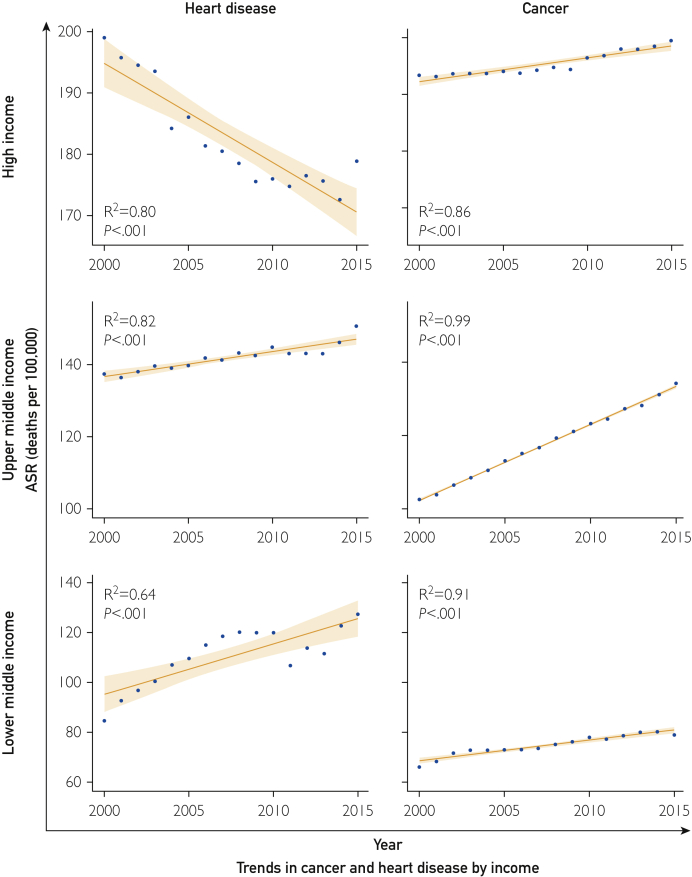
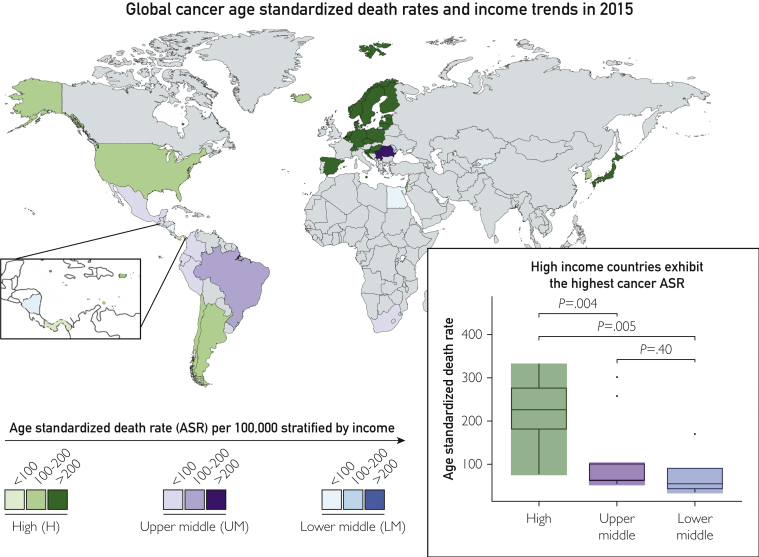
From the period between 2000 and 2015, there was an increase in cancer ASR irrespective of sex or country income status (Figures 1 and 2; Table). Overall, there was an approximately 7% increase in mortality rates for cancer (Figure 1; Table). During the 15-year study period, the average annual percentage change (a measure of the standard annual change in mortality rate) was an increase of 1.2% in cancer deaths. There was a strong positive trend in cancer mortality rates during the study period (Pearson r, +0.99; P<.00001). The trend was similar for both men and women; male deaths due to cancer increased by 7%, and female deaths increased by 6%. There were differences in cancer mortality trends according to a country’s income classification; high-income countries saw a 3% increase in cancer mortality rates compared with 31% for upper-middle-income and 19% for lower-middle-income countries (Table; Figures 2 and 3). In terms of raw counts, high-income countries experienced the smallest increase in cancer mortality deaths (14.1%), upper-middle-income countries had a 51.8% increase, and lower-middle-income countries had a 45.8% increase.
Figure 1.
Death counts for cancer and heart disease from 2000 to 2015 are displayed. All deaths are displayed regardless of age and sex.
Figure 2.
Trends in the age-standardized death rate (ASR) per 100,000 from 2000 to 2015 for cancer and heart disease broken down by income status.
Table.
Age-Standardized Mortality Rates Globally and by Income Group
| Year | Globally |
High income |
Upper middle income |
Lower middle income |
||||
|---|---|---|---|---|---|---|---|---|
| Heart | Cancer | Heart | Cancer | Heart | Cancer | Heart | Cancer | |
| 2000 | 175.5 | 162.5 | 199.0 | 193.4 | 137.5 | 102.5 | 84.6 | 66.0 |
| 2001 | 173.7 | 162.8 | 195.7 | 193.1 | 136.5 | 103.8 | 92.6 | 68.3 |
| 2002 | 173.6 | 164.0 | 194.5 | 193.6 | 138.1 | 106.4 | 96.8 | 71.6 |
| 2003 | 173.6 | 164.6 | 193.5 | 193.7 | 139.7 | 108.5 | 100.4 | 72.8 |
| 2004 | 167.6 | 165.0 | 184.2 | 193.7 | 139.1 | 110.4 | 107.0 | 72.8 |
| 2005 | 169.3 | 165.8 | 186.0 | 194.0 | 139.8 | 113.1 | 109.7 | 72.9 |
| 2006 | 166.9 | 166.1 | 181.4 | 193.8 | 141.9 | 115.0 | 115.0 | 73.0 |
| 2007 | 166.5 | 166.8 | 180.5 | 194.3 | 141.3 | 116.6 | 118.5 | 73.5 |
| 2008 | 165.7 | 167.8 | 178.5 | 194.8 | 143.3 | 119.3 | 120.2 | 75.1 |
| 2009 | 163.5 | 168.1 | 175.6 | 194.4 | 142.6 | 121.0 | 120.0 | 76.2 |
| 2010 | 164.3 | 170.1 | 176.0 | 196.4 | 144.9 | 123.2 | 119.9 | 77.9 |
| 2011 | 161.8 | 170.5 | 174.8 | 196.8 | 143.1 | 124.5 | 106.7 | 77.1 |
| 2012 | 163.7 | 172.1 | 176.5 | 198.0 | 143.1 | 127.3 | 113.7 | 78.6 |
| 2013 | 162.9 | 172.4 | 175.7 | 198.0 | 143.1 | 128.2 | 111.5 | 80.0 |
| 2014 | 162.4 | 173.4 | 172.6 | 198.5 | 146.2 | 131.1 | 122.7 | 80.1 |
| 2015 | 168.2 | 174.6 | 178.9 | 199.5 | 150.7 | 134.2 | 127.3 | 78.9 |
Figure 3.
World map showing the cancer age-standardized death rate (ASR) per 100,000 in 2015 broken down by income status.
Cardiovascular Disease Trends
During the study period (2000 to 2015), the overall cardiovascular mortality rate fell by 4% (Table). Globally, for men, the ASR for cardiovascular disease fell by 4% compared with 10% for women. There was a strong negative trend in cardiovascular disease ASR during the study period (Pearson r, −0.91; P<.00001), indicating a generally decreasing mortality across time. The decreasing trend in cardiovascular disease was not as strong in men as in women but still achieved statistical significance in men (Pearson r, −0.82; P<.00001; data not shown). Cardiovascular disease ASR, however, decreased by 10% in high-income countries, increased by 10% in upper-middle-income countries, and increased by 50% in lower-middle-income countries (Table; Figure 2).
Discussion
In this observational comparative analysis of the worldwide mortality trends of cancer and cardiovascular disease during a 15-year period, our observations indicate that cancer-related mortality rate increased by 6%, whereas cardiovascular disease mortality rate decreased by 4%. In 2000, the 43 countries analyzed experienced more than 1.9 million cancer-related deaths, and despite improvements in therapies and detection systems, this number rose to 2.3 million deaths in 2015.
Trends by Income Status
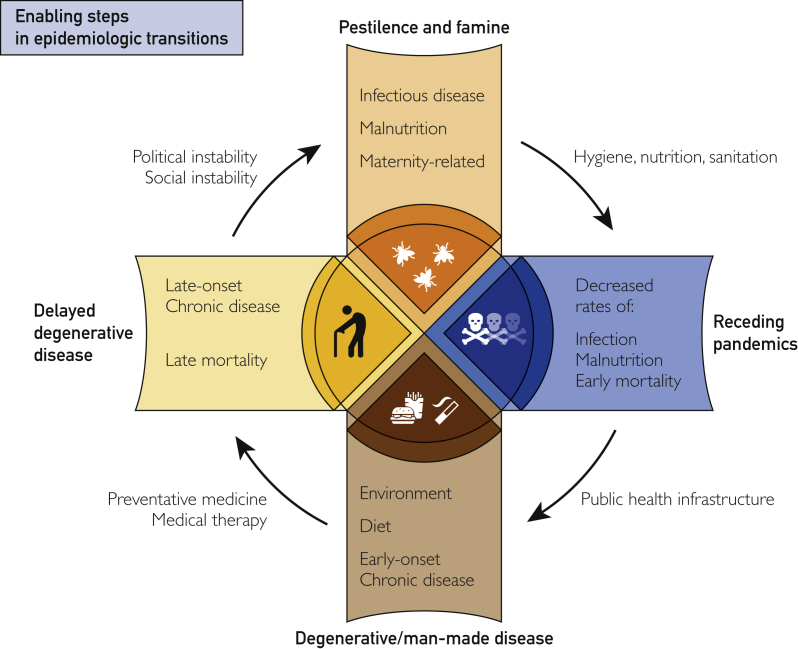
Our observations showed that the mortality trends for both cancer and cardiovascular diseases varied by a country’s income status. High-income countries have seen a small increase in cancer mortality rates and a decrease in cardiovascular disease mortality rates. Comparatively, upper-middle-income and lower-middle-income countries saw large increases in both cancer- and cardiovascular disease–related mortality (Figure 3). These differences might be due to differences in interventions and early detection programs between the income groups. In addition, these differences have been largely theorized to be due to stage of epidemiologic transition of the countries (Figure 4).9,22, 23, 24, 25 Epidemiologic transition is the process by which countries “advance” through stages on the basis of the types of diseases most affecting their population.22,23 The transition is broken down into 4 stages: pestilence and famine, receding pandemics, degenerative and man-made diseases, and delayed degenerative diseases.22,23
Figure 4.
Enabling steps in epidemiologic transitions. Schematic representing transitions of countries through 4 stages of pestilence and famine, receding pandemics, degenerative and man-made disease, and delayed degenerative disease and the key changes required for each transition.
High-Income Countries
High-income countries are increasingly transitioning from degenerative and man-made diseases (such as cardiovascular disease) to delayed degenerative diseases (such as cancer). This fairly can explain why high-income countries have seen a decrease in cardiovascular disease but a relatively slower rise in cancer death rates.24 This observation should be interpreted with caution as cardiovascular disease has been the focus of research and funding for a longer period than cancer has, and through preventive and life-prolonging interventions created during the last 20 years, we have seen a decline in age-standardized cardiovascular disease–related deaths.8, 9, 10,24, 25, 26 A study by Carrión Donderis et al24 in 2016 in Panama, a high-income country, found similar results of reduced cardiovascular disease mortality due to improved treatment, lower tobacco consumption, and reduction of comorbidities. Within cancer research, there have been notably fewer curative developments for the most advanced cancers and the cancer types that contribute the most to mortality. This, in part, could explain why cancer mortality trends still demonstrate a slight upward slope.1, 2, 3, 4,8, 9, 10,12, 13, 14,27
Upper-Middle-Income and Lower-Middle-Income Countries
We observed a drastic increase in cardiovascular mortality trends (up nearly 50% during the last 20 years) in lower-middle-income countries, whereas upper-middle-income countries showed a 10% increase. This observation must be explained with care as during the last 15 years, lower-middle-income and upper-middle-income countries have been transitioning through the epidemiology stages from pestilence and famine and receding pandemics to degenerative and man-made diseases and delayed degenerative diseases.10,24,28 As part of this transition, we expect a rise in cardiovascular disease and cancer mortality rates in lower-middle-income and upper-middle-income countries.10,24,25,28 In addition, there is a difference in research and funding for cardiovascular disease in these countries compared with high-income countries.10,24,26,29, 30, 31 The rise in cancer and cardiovascular disease mortality in upper-middle-income and lower-middle-income countries might be due to increased screening and identification of patients. As a result, this may increase the likelihood that the primary cause of death is recognized as cancer or cardiovascular disease.10
Cardiovascular vs Cancer Mortality
Despite large increases in cardiovascular disease mortality trends in upper-middle-income and lower-middle-income countries, cardiovascular disease–related mortality has shown a decline globally. This can be explained through examination of the aggregated ASR for each income group and understanding the population percentages. Whereas cardiovascular disease rates increased by 50% in lower-middle-income countries and by 10% in upper-middle-income countries, the overall cardiovascular ASR decreased because high-income countries saw a 10% decrease and high-income countries make up nearly 70% of the countries examined. Next, cancer mortality rates increased for all income statuses, and the total global cancer rates, again because of population distributions, are much closer to those of high-income countries than to those of upper-middle-income or lower-middle-income nations at nearly 174 deaths per 100,000.
In previous literature, the Global Burden of Disease (GBD) group reported a 9.4 per 100,000 decrease in cancer ASR between 2006 and 2016.1 When examining data extracted from the WHO Mortality Database between 2000 and 2015, we saw an approximate 6% cancer mortality increase corresponding to an approximate 10 per 100,000 rise in cancer ASR. This observation should be interpreted with caution as the GBD group uses the “GBD cause of death database,” a database built and organized by their group, whereas we used the publicly available WHO Mortality Database.1,17 This difference in findings highlights the importance of creating guidelines and agencies to improve the accuracy of reporting and the quality of the data in global-level mortality databases. We believe the differences in our results and those of the GBD group are 2-fold: difference in included countries and difference in data availability and analysis techniques. Specifically, the GBD group uses statistical techniques to attempt to account for missing data; however, the general public is not privy to this information and therefore cannot replicate the numbers. With this in mind, we believe that as a community we must create a combined publicly available database for all diseases, and we hope that with such a database, differences between studies should decrease and more accurate numbers can be reported.
We must acknowledge limitations in our analysis. First, high-income countries accounted for 66% of the population analyzed; therefore, rates in high-income countries had a higher “weight.” The results might be skewed to favor trends seen in high-income countries. Along the same lines, no low-income countries were included. However, countries were chosen on the basis of data availability, which helps explain why no low-income country data were available and 66% of countries fell into the high-income bracket; hence, this is the most “accurate” analysis possible currently. Data from China and India (which represent 37% of the world population) were not included in this study because of data unavailability. However, some data from these 2 countries were available if 1 disease was reported using the ICD-10 code, which we did not include in this study, but that might be considered for future studies. An additional limitation inherent in our analysis was the assumption of a standardized population; however, establishing age and sex distributions for each country for each year in the analysis was not feasible because of data availability. Second, owing to improvements in database and information-gathering technology, reporting for cancer and cardiovascular disease may have increased over time without an actual increase in the incidence or prevalence of these diseases. This finding should be interpreted carefully as this might suggest that the cancer rates have falsely increased because of the accurate reporting and the quality of the data. However, these biases are likely to affect cardiovascular disease and cancer in a similar fashion, and we would expect to see an increase in cardiovascular disease, which was not the case. Increases in reporting would affect low-income and upper-middle-income countries more than high-income countries, which made up 66% of our analysis; therefore, effects due to reporting improvements would be partly masked. Finally, databases such as the WHO Mortality Database used in this study contain a certain percentage of improperly recorded reasons for mortality, and this varies by country and time. These inherent inaccuracies might skew trends and rates of cancer and heart disease, and unfortunately there is no way to account for these with the data currently available. As databases improve in their trustworthiness over time, we hope these inaccuracies will be less impactful in future studies.
Conclusion
Cancer and cardiovascular disease are the 2 leading causes of noncommunicable disease mortality worldwide. Our study, based on the 2 databases used, observed that between 2000 and 2015, cardiovascular disease mortality rates have been declining, which may be largely due to targeted interventions and early detection programs. However, cancer mortality rates appear to be increasing steadily despite similar interventions and early detection programs, partially from the demographic changes of the population. Innovative approaches in early detection and treatment would be helpful in attenuating the rate of increase in deaths due to cancer, particularly in high-income countries.
Footnotes
Grant Support: A.Q.-H. was supported by the Mayo Clinic Professorship and a Clinician Investigator award, Florida State Department of Health Research Grant, and Mayo Clinic Graduate School as well as by the NIH (R43CA221490, R01CA200399, R01CA195503, and R01CA216855). K.R. was supported by the NIH/NINDS (U01-NS108916).
Potential Competing Interests: The authors report no competing interests.
Supplemental material can be found online at http://www.mayoclinicproceedings.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
Contributor Information
Karim ReFaey, Email: karimrefaey1@gmail.com.
Alfredo Quinones-Hinojosa, Email: quinones@mayo.edu.
Supplemental Online Material
References
- 1.GBD 2017 Causes of Death Collaborators Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017 [erratum appears in Lancet. 2019;393(10190):e44; Lancet. 2018;392(10160):2170] Lancet. 2018;392(10159):1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2015 Mortality and Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015 [erratum appears in Lancet. 2017;389(10064):e1] Lancet. 2016;388(10053):1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Global Burden of Disease Cancer Collaboration The global burden of cancer 2013 [erratum appears in JAMA Oncol. 2015;1(5):690] JAMA Oncol. 2015;1(4):505–527. doi: 10.1001/jamaoncol.2015.0735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Global Burden of Disease Cancer Collaboration Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the Global Burden of Disease Study [erratum appears in JAMA Oncol. 2017;3(3):418] JAMA Oncol. 2017;3(4):524–548. doi: 10.1001/jamaoncol.2016.5688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Department of Health and Social Care 2003-04 to 2010-11 programme budgeting data. https://www.gov.uk/government/publications/2003-04-to-2010-11-programme-budgeting-data
- 6.National Institute for Public Health and the Environment. Cost of diseases trend 2003-2017. Available at: https://www.rivm.nl/en/news/disease-burden-and-cost-of-illness-of-food-related-pathogens-in-netherlands. Accessed December 18, 2018.
- 7.The Federal Health Monitoring System. Cost of illness in millions of Euro for Germany. Available at: https://www.gbe-bund.de/gbe/. Accessed March 20, 2020.
- 8.GBD 2016 Healthcare Access and Quality Collaborators Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet. 2018;391(10136):2236–2271. doi: 10.1016/S0140-6736(18)30994-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jonsson B., Hofmarcher T., Lindgren P., Wilking N. The cost and burden of cancer in the European Union 1995-2014. Eur J Cancer. 2016;66:162–170. doi: 10.1016/j.ejca.2016.06.022. [DOI] [PubMed] [Google Scholar]
- 10.Luengo-Fernandez R., Leal J., Gray A., Sullivan R. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol. 2013;14(12):1165–1174. doi: 10.1016/S1470-2045(13)70442-X. [DOI] [PubMed] [Google Scholar]
- 11.Aggarwal A., Ginsburg O., Fojo T. Cancer economics, policy and politics: what informs the debate? Perspectives from the EU, Canada and US. J Cancer Policy. 2014;2(1):1–11. [Google Scholar]
- 12.Taksler G.B., Rothberg M.B. Assessing years of life lost versus number of deaths in the United States, 1995-2015. Am J Public Health. 2017;107(10):1653–1659. doi: 10.2105/AJPH.2017.303986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weir H.K., Anderson R.N., Coleman King S.M. Heart disease and cancer deaths—trends and projections in the United States, 1969-2020. Prev Chronic Dis. 2016;13:E157. doi: 10.5888/pcd13.160211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu J., Murphy S.L., Kochanek K.D., Bastian B.A. Deaths: final data for 2013. Natl Vital Stat Rep. 2016;64(2):1–119. [PubMed] [Google Scholar]
- 15.US Department of Health and Human Services. National Center for Health Statistics. Available at: https://www.cdc.gov/nchs/index.htm. Accessed August 18, 2019.
- 16.Lee A., Shah K., Chino J.P., Chino F. Changes in cancer mortality rates after the adoption of the Affordable Care Act. J Clin Oncol. 2020;38(15, suppl):2003. [Google Scholar]
- 17.World Health Organization. WHO mortality database. Available at: https://www.who.int/data/data-collection-tools/who-mortality-database. Accessed June 2, 2017.
- 18.The World Bank . World Bank; Washington, DC: 2016. Global Economic Prospects: Spillovers Amid Weak Growth. [Google Scholar]
- 19.World Health Organization Global health risks: mortality and burden of disease attributable to selected major risks. https://apps.who.int/iris/handle/10665/44203
- 20.International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10) World Health Organization; Geneva: 2016. [Google Scholar]
- 21.US Department of Health and Human Services . National Center for Health Statistics; Hyattsville, MD: 2018. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) [Google Scholar]
- 22.Yusuf S., Reddy S., Ounpuu S., Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104(22):2746–2753. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- 23.Reddy K.S. Cardiovascular disease in non-Western countries. N Engl J Med. 2004;350(24):2438–2440. doi: 10.1056/NEJMp048024. [DOI] [PubMed] [Google Scholar]
- 24.Carrión Donderis M., Moreno Velasquez I., Castro F., Zuniga J., Gomez B., Motta J. Analysis of mortality trends due to cardiovascular diseases in Panama, 2001-2014. Open Heart. 2016;3(2):e000510. doi: 10.1136/openhrt-2016-000510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.GBD 2016 Lifetime Risk of Stroke Collaborators Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N Engl J Med. 2018;379(25):2429–2437. doi: 10.1056/NEJMoa1804492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Welch H.G., Schwartz L.M., Woloshin S. Are increasing 5-year survival rates evidence of success against cancer? JAMA. 2000;283(22):2975–2978. doi: 10.1001/jama.283.22.2975. [DOI] [PubMed] [Google Scholar]
- 27.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67(1):7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- 28.The World Bank. World development indicators. Available at: https://datacatalog.worldbank.org/dataset/world-development-indicators. Accessed July 10, 2018.
- 29.Benjamin E.J., Muntner P., Alonso A. Heart disease andstroke statistics—2019 update: a report from the American Heart Association [erratum appears in Circulation. 2020;141(2):e33] Circulation. 2019;139(10):e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 30.Pestana J.A., Steyn K., Leiman A., Hartzenberg G.M. The direct and indirect costs of cardiovascular disease in South Africa in 1991. S Afr Med J. 1996;86(6):679–684. [PubMed] [Google Scholar]
- 31.Gaziano T.A., Bitton A., Anand S., Abrahams-Gessel S., Murphy A. Growing epidemic of coronary heart disease in low- and middle-income countries. Curr Probl Cardiol. 2010;35(2):72–115. doi: 10.1016/j.cpcardiol.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.