Abstract
Purpose
To investigate the interaction between (1) sleep and the COVID-19 pandemic; and (2) social cumulative risk and COVID-19 pandemic on executive function (EF).
Methods
Forty late adolescents/young adults (19.25 ± 1.12 y.o.) completed sleep questionnaires and the Behavior Rating Inventory of Executive Function- Adults (BRIEF-A) before and during the COVID-19 pandemic, yielding 80 observations for data analysis. Multilevel random-effects models with interaction terms were used to estimate the associations.
Results
Compared to pre-pandemic sleep, participants slept 24 min longer (t = −2.07, p = 0.03) and also had increased sleep latency (t = −1.83, p = 0.07) during COVID-19. Mid-sleep times shifted 40 min later (t = −3.22, p = 0.003), and BRIEF-A scores increased (indicating greater dysfunction), during the pandemic (p < 0.05). The worsening in EF during the pandemic was attenuated by increasing sleep duration (B = -4.38, p = 0.04) and magnified by social cumulative risk (B = 3.19, p = 0.04). Poor sleep quality was independently associated with increase in EF problems (p < 0.05).
Conclusion
Sufficient sleep may represent a resilience factor against EF decline during this unprecedented crisis.
Keywords: Sleep, Executive function, COVID-19, Social determinants, Health disparity
1. Introduction
Coronavirus pandemic (COVID-19) has increased mental health issues, such as depressive symptoms and suicidal ideation, across age groups [1,2]. Executive function (EF) reflects cognitive processes underlying goal-directed behaviors, emotional responses and social interaction [3], and is essential for building resilience to cope with stressful life events such as COVID-19. The pandemic has also affected sleep patterns [4,5], which is known to influence EF [6,7]. Global investigation shows later self-reported bedtimes and wake-up times, increased sleep disturbances, and poorer sleep quality compared to pre-pandemic baseline, despite longer sleep duration [4,5,8]. Among all age groups, the greatest effect on sleep is observed in adolescents and young adults [4,8]. Given that EF shows continued development into early adulthood [3], poor sleep may have a more profound influence among adolescents/young adults under this unprecedented crisis. However, how sleep interacts with COVID-19 on affecting EF remains unclear.
The primary aim of this study was to track changes to sleep and EF before and during COVID-19, and examine whether sleep moderated the pandemic-related changes to EF, in adolescents/young adults. Additionally, both social disparities and COVID-19 are public health crises. As a second aim, we explored whether changes in EF varied by social risk factors. This study will contribute to a better understanding of the resilience and risk factors of adolescents and young adults during crises.
2. Material and methods
Leveraging an ongoing study on sleep and cardiovascular risk factors, this longitudinal study collected data via Research Electronic Data Capture [REDCap] system on sleep and EF before (baseline) and during COVID-19. Using a convenience sample from a public university, 60 participants completed self-reported assessments between April and December 2019 (baseline). After remote learning began, 40 of them completed follow-up assessments in April–May 2020 (age 19.25 ± 1.12 y.o., 37F:3M), yielding 80 observations (before and during COVID-19) for data analysis. There were no differences between baseline and follow-up data except gender (χ2 = 9.41, p = 0.002). The attrition rate of males (8 out of 11 dropped) was higher than females (12/49). All data were collected only during the academic year. Participants provided informed consent per Institutional Review Board-approved guidelines.
2.1. Measurements
2.1.1. Sleep
Participants completed a seven-day sleep diary and the Pittsburgh Sleep Quality Index (PSQI) before and during COVID-19. Diary responses provided variables of sleep duration, sleep latency (amount of time to fall asleep), sleep midpoint times (clock time halfway between sleep onset and offset), and social jetlag (absolute difference between mid-sleep times on weekdays and weekends). The PSQI is composed of 19 items categorized into seven subscales: sleep quality, sleep latency, duration, efficiency, sleep disturbances, sleep medication use and daytime dysfunction. The PSQI total score represents overall sleep quality, with poor sleeper defined as total scores>5 [9]. The PSQI has shown good psychometric properties in adolescents/young adults [9,10].
2.1.2. Executive function
The Behavior Rating Inventory of Executive Function-Adults (BRIEF-A) assessed EF in everyday activities [11]. Seventy-five questions were grouped into behavioral regulation index (BRI) and metacognition index (MI). The BRI reflects regulatory control of behavior/emotional responses, and MI represents the ability to cognitively manage tasks through initiating, planning/organizing, sustaining working memory, and monitoring. The BRI and MI (secondary outcomes) form an overall summary score, the Global Executive Composite (GEC) scores (primary outcome). Age-adjusted T-scores were calculated, with higher scores indicating greater dysfunction. The BRIEF-A has demonstrated good internal consistency (Cronbach's alpha = 0.72–0.96) and construct and convergent validity [11].
2.1.3. Covariates
We collected socio-demographic information (eg age, sex, race, parental education) and body mass index at baseline. Social cumulative risk (SCR) was calculated as the total number of risk factors (non-White, parent education ≤ high school, family income below poverty threshold by family size and number of children, and <two parents in primary household). Additionally, we measured health behaviors [smoking, alcohol consumption and exercise from 0 = never to 3 = always (6–7 times/week)] and COVID status (unknown/infected/not infected) at the follow-up.
2.2. Statistical analyses
At the bivariate level, we compared sleep and EF before and during COVID-19 using paired t tests and the Wilcoxon signed-rank tests. Accounting for age, sex, SCR, BMI, COVID status, health behaviors, a series of linear mixed models tested whether GEC and BRI/MI domains were associated with COVID-19 (before/during) and sleep variables, modeling for by-participant random-intercepts. Sleep variables entered models separately due to collinearity. Next, interaction terms between (1) each sleep variable and COVID-19 and (2) SCR and COVID-19 were added into models separately to estimate the moderating effect of sleep/social risk. Goodness-of-fit statistics, including likelihood ratio (LR) test, AIC, BIC, were used to compare model fit. Data analyses were conducted using STATA 16.
3. Results
Thirty-one participants reported at least one social risk factors, such as non-White (40%) and mother/father's education level ≤ high school (25%). Participants slept 24 min longer (7.35 vs.7.76 h, t = −2.07, p = 0.03), but with increased sleep latency during COVID-19 (22.28 ± 14.18 min) compared to baseline (18.65 ± 12.98 min) (t = −1.83, p = 0.07). The PSQI total scores were consistently high (6.10 ± 2.04 vs.5.95 ± 2.97, p > 0.05), however worsened in 48% of participants during COVID-19. Midpoint sleep time shifted 40 min later (04:36 vs. 05:11, t = −3.22, p = 0.003) and the trend remained significant after adjusting for covariates. There were no significant changes in PSQI subscale scores and social jetlag (p > 0.05).
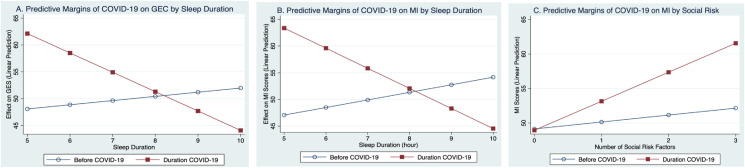
Regarding executive function, participants scored worse during the pandemic on GEC (49.95 ± 9.11 vs. 53.10 ± 11.47) and MI (50.38 ± 9.17 vs. 54.10 ± 12.19) compared with pre-COVID assessment. In multilevel models (Table 1 ), the differences in GEC scores (B = 3.15, p = 0.03) and MI (B = 3.73, p = 0.01) between times remained significant. There were interactions between sleep duration and COVID-19, and SCR and COVID-19, but no main effects of sleep duration or SCR. Specifically, increased sleep duration attenuated the worsening of GEC (B = −4.38, p = 0.04) and MI (B = -5.18, p = 0.02) during COVID-19, whereas SCR (B = 3.19, p = 0.04) intensified the deleterious impact of the COVID-19 on MI (Fig. 1 ). Adding interaction terms significantly improved model fit (LR test, p < 0.05). Poor sleep (PSQI>5) was associated with worse GEC (B = 4.69, p = 0.02) and MI (B = 4.20, p = 0.04) independent of COVID-19. We repeated analyses using PSQI total scores and found similar trends with GEC (B = 0.86, p = 0.03) and BRI (B = 1.07, p = 0.01). Sleep latency, midsleep times and social jetlag were not associated with EF nor moderated the association between pandemic and EF (p > 0.05).
Table 1.
Significant predictors/moderators of EF from multilevel models.
| GEC (primary outcome) |
MI (secondary outcome) |
|||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| Moderator test 1, B (se) | ||||
| Social riska | 2.03 (1.58) | 1.00 (1.76) | 2.60 (1.61) | 1.01 (1.79) |
| Pandemicb | 3.15 (1.44)∗ | 0.64 (2.37) | 3.73 (1.46)∗ | −0.19 (2.34) |
| Social risk∗Pandemic | 2.05 (1.56) | 3.19 (1.53)∗ | ||
| Moderator test 2, B (se) | ||||
| Poor sleep (PSQI>5)c | 4.69 (2.02)∗ | 6.55 (2.60)∗ | 4.20 (2.06)∗ | 6.11 (2.64)∗ |
| Pandemic | 3.61 (1.43)∗ | 5.59 (2.20)∗ | 4.14 (1.44)∗∗ | 6.12 (2.23)∗∗ |
| Poor sleep∗Pandemic | −3.76 (3.25) | −3.75 (3.29) | ||
| Moderator test 3, B (se) | ||||
| Sleep duration | −1.52 (0.18) | 0.78 (1.59) | −1.30 (1.16) | 1.41 (1.58) |
| Pandemic | 3.17 (1.52)∗ | 35.96 (16.26)∗ | 3.44 (1.54)∗ | 42.18 (16.16)∗∗ |
| Sleep duration∗Pandemic | −4.38 (2.17)∗ | −5.18 (2.15)∗ | ||
Note: Sleep latency, midsleep times and social jetlag were not reported (results not significant). GEC = Global Executive Composite, MI = metacognition index. ∗∗p < 0.01 ∗p < 0.05.
Model fit: GEC model 2 VS 1: sleep duration (LR test: χ2 = 4.00, p = 0.04, AIC = 597.17, BIC = 630.51); MI model 2 VS 1: sleep duration (LR test: χ2 = 5.58, p = 0.02, AIC = 601.40, BIC = 634.75), social risk (LR test: χ2 = 4.11, p = 0.04; AIC = 600.57; BIC = 631.53); adding interaction term did not improve model fit of other models.
Social risk = the total number of following factors each participant had: non-White, parent education ≤ high school, poverty, and single-parent household.
Pandemic: during VS. before COVID-19.
Poor sleep (PSQI>5) VS. normal sleep.
Fig. 1.
Interactions between A) sleep duration and COVID-19 on GEC, B) sleep duration and COVID-19 on MI, and C) social risk and COVID-19 on MI. Note: high GEC and MI scores indicate greater dysfunction.
4. Discussion
Compared to baseline, late adolescents and young adults reported longer sleep duration, later midsleep times, increased sleep latency, and worse EF during the pandemic. The pandemic-related changes in EF varied by sleep duration and SCR, such that increasing sleep duration attenuated, and SCR intensified, declines in EF. In general, poor sleep quality was associated with worse EF.
These findings are consistent with earlier evidence from the pandemic, showing that shifted sleep phase and increased sleep latency were pronounced in adolescents/young adults [4,8]. Remote learning and pandemic measures (ie social distancing) may increase sleep opportunities. However, increased screen time and decreased light exposure and physical activity may disrupt sleep quality and chronobiological rhythm. Interestingly, composite sleep quality score in the PSQI did not change compared with the baseline level. Since sleep duration is one aspect of PSQI, increased sleep duration may have masked the decline in other PSQI domains.
Overall EF and metacognition subdomain decreased during COVID-19; this may relate to the reported changes in sleep patterns. Short sleep duration and poor sleep quality have been associated with impaired EF in adolescents and young adults [6,7], supporting our findings of sleep quality and EF. In the current study, sleep duration was not an independent factor for EF, but a moderator. Increasing sleep hours attenuated or even reversed the negative impact of the pandemic on EF. Thus, sufficient sleep may protect against EF decline during stressful events. This is particularly important for late adolescents and emerging young adults who navigate daily stress and report more mental health issues than other age groups during COVID-19 [1]. Although later midsleep times were evident during the pandemic, there was no interaction between midsleep times and COVID-19 on EF. Future research is needed to examine the individual and cumulative effect of multidimensions of sleep on EF. Additionally, late adolescents/young adults with greater social cumulative risk tended to experience greater decline in metacognition during COVID-19. The finding suggests that the negative impact of the pandemic is further exacerbated by socioeconomic disparity in EF [12].
Study limitations include self-reported measurement, generalizability of data collected from a small convenience sample with mostly female participants, potential seasonal effect and other unobserved confounders such as mental health symptoms. Given the high co-morbidity between sleep and mental health as well as the sharp increase in mental health disorders during the pandemic, the association between sleep and EF may be confounded by mental health symptoms. Additionally, multiple hypothesis tests may raise concerns about Type I error. Whereas we found similar patterns for associations of sleep with overall EF and subdomains at the significance level of 0.05, we did not adjust for familywise error rate due to the exploratory nature of this study. Despite the limitations, this study is one of the first to investigate the role of sleep and social determinants in pandemic-related changes in EF. Our findings may inform sleep-related interventions, in conjunction with social support programs, to mitigating the negative impact of crises such as COVID-19 for adolescents and young adults.
5. Conclusions
Late adolescents and young adults report longer sleep, yet poorer sleep quality and declined executive function during the pandemic versus pre-COVID baseline. Sufficient sleep duration attenuates, but social risk factors exacerbate, EF declines during COVID-19. Our findings suggest the importance of promoting sleep health and eliminating social disparity to youth health during COVID-19, and shed light on public health strategies in coping with future crises.
Credit author statement
Xiaopeng Ji: Conceptualization, Methodology, Investigation, Formal analyses, Writing- Original draft preparation, review & editing; Jennifer Saylor: Conceptualization and Writing - Review & Editing. F. Sayako Earle: Writing - Review & Editing.
Funding
The parent study was supported by the American Nurses Foundation Research Award (18A01422) and the follow-up data collection was supported by the University of Delaware College of Health Science Start-up funding.
Ethical committee permission
University of Delaware IRB #1231039-7.
Acknowledgments
We would like to thank students who participated in this study. A deep gratitude is extended to Ms.Yiqi Wang, an undergraduate student during the time of the study, who helped with enrollment and data collection.
Footnotes
On behalf of all authors, the corresponding author states that there is no conflict of interest.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2021.06.027.
Conflict of interest
The following is the supplementary data related to this article:
References
- 1.O'Connor R.C., Wetherall K, Cleare S, et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatr. 2020:1–8. doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li DJ, Ko NY, Chen YL, et al. COVID-19-related factors associated with sleep disturbance and suicidal thoughts among the Taiwanese public: a Facebook survey. Int J Environ Res Publ Health. 2020;17(12):4479. doi: 10.3390/ijerph17124479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson P. Assessment and development of executive function (EF) during childhood. Child Neuropsychol. 2002;8(2):71–82. doi: 10.1076/chin.8.2.71.8724. [DOI] [PubMed] [Google Scholar]
- 4.Cycle S. 2020. Sleep and mental health amidst the 2020 Coronavirus Pandemic.https://www.sleepcycle.com/coronavirus/ [cited 2020 December 20]; Available from: [Google Scholar]
- 5.Benham G. Stress and Health; 2020. Stress and sleep in college students prior to and during the COVID-19 pandemic. [DOI] [PubMed] [Google Scholar]
- 6.Kuula L., Pesonen AK, Martikainen S, et al. Poor sleep and neurocognitive function in early adolescence. Sleep Med. 2015;16(10):1207–1212. doi: 10.1016/j.sleep.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 7.Kuula L., Pesonen AK, Heinonen K, et al. Naturally occurring circadian rhythm and sleep duration are related to executive functions in early adulthood. J Sleep Res. 2018;27(1):113–119. doi: 10.1111/jsr.12581. [DOI] [PubMed] [Google Scholar]
- 8.Marelli S., Castelnuovo A, Somma A, et al. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J Neurol. 2021;268(1):8–15. doi: 10.1007/s00415-020-10056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buysse D.J., Reynolds CF, III, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatr Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 10.Zhou H.Q., Shi WB, Wang XF, et al. An epidemiological study of sleep quality in adolescents in South China: a school-based study. Child Care Health Dev. 2012;38(4):581–587. doi: 10.1111/j.1365-2214.2011.01300.x. [DOI] [PubMed] [Google Scholar]
- 11.Roth R.M., Gioia G.A. Psychological Assessment Resources; Lutz, FL: 2005. Behavior rating inventory of executive function--adult version. [Google Scholar]
- 12.Last B.S., Lawson GM, Breiner K, et al. Childhood socioeconomic status and executive function in childhood and beyond. PloS One. 2018;13(8) doi: 10.1371/journal.pone.0202964. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.