Abstract
Study Objectives
Nocturnal wakefulness is a risk factor for suicide and suicidal ideation in clinical populations. However, these results have not been demonstrated in general community samples or compared to sleep duration or sleep quality. The present study explored how the timing of wakefulness was associated with suicidal ideation for weekdays and weekends.
Methods
Data were collected from 888 adults aged 22–60 as part of the Sleep and Healthy Activity, Diet, Environment, and Socialization study. Suicidal ideation was measured by the Patient Health Questionnaire-9, while timing of wakefulness was estimated from the Sleep Timing Questionnaire. Binomial logistic regressions estimated the association between nocturnal (11 pm–5 am) and morning (5 am–11 am) wakefulness and suicidal ideation.
Results
Nocturnal wakefulness was positively associated with suicidal ideation on weekdays (OR: 1.44 [1.28–1.64] per hour awake between 11:00 pm and 05:00 am, p < 0.0001) and weekends (OR: 1.22 [1.08–1.39], p = 0.0018). Morning wakefulness was negatively associated with suicidal ideation on weekdays (OR: 0.82 [0.72–0.92] per hour awake between 05:00 am and 11:00 am, p = 0.0008) and weekends (OR: 0.84 [0.75–0.94], p = 0.0035). These associations remained significant when adjusting for sociodemographic factors. Additionally, nocturnal wakefulness on weekdays was associated with suicidal ideation when accounting for insomnia, sleep duration, sleep quality, and chronotype (OR 1.25 [1.09–1.44] per hour awake, p = 0.002).
Conclusion
Wakefulness at night was consistently associated with suicidal ideation. Additionally, morning wakefulness was negatively associated with suicidal ideation in some models. Although these findings are drawn from a non-clinical sample, larger longitudinal studies in the general population are needed to confirm these results.
Keywords: suicide, suicidal ideation, nocturnal wakefulness, chronotype
Statement of Significance.
Prior studies have shown that the risk of suicide is highest at night. This study expands on this research by showing that individuals who spent more time awake at night were likely to have more frequent suicidal ideation. Conversely, morning wakefulness was sometimes associated with less frequent suicidal ideation, which is a novel finding in the literature. Together, these results suggest that time of day may play an important role in vulnerability to, and protection against, suicidal thoughts and behaviors.
Introduction
Insomnia increases risk for suicidal thoughts and behaviors (STBs) [1]. Insomnia predicts subsequent suicidal ideation [2–5], intent to commit suicide [6], suicide attempts [7, 8], and death by suicide [9–11], often independent of comorbid mental illness. Moreover, preliminary data indicate that treating insomnia may reduce suicidal ideation [12–14], thus highlighting sleep as a modifiable risk factor for STBs.
At present, the mechanisms connecting sleep disturbance to STBs are unclear [15]. Psychological theories suggest that insomnia increases thwarted belongingness [16–18] and/or that insomnia confers vulnerability to acute stress via the effects of sleep loss [19, 20]. Recently, it has been suggested that nocturnal wakefulness—that is, simply being awake at night—may drive suicide risk [21] via hypo-frontality and/or the diminished executive function that occurs when one is awake but not biologically prepared to be awake. To date, there is epidemiological and experimental evidence that indicates nocturnal wakefulness is a substantial risk factor for STBs.
In general, death from suicide is most common during the midday. However, this fails to account for population wakefulness as a confounder; since most people are awake at midday, the “eligible” population for suicide is highest at midday. When adjusting for the number of people awake in the population, the risk for suicide is highest at night [22], regardless of month or mechanism of suicide [23]. Indeed, wakefulness between 2 am and 4 am predicts subsequent suicidal ideation in a clinical sample [24]. Whether the cause is a nightmare, inability to fall or stay asleep, or just not sleeping enough, wakefulness during the biological night may increase suicide risk because mood [25–28] and impulse control [29–32] are minimized.
Beyond death by suicide, nocturnal wakefulness may reasonably affect other STBs such as suicidal ideation, as has been shown in a small clinical sample [24]. However, no studies have explored this idea in the general community or on an epidemiological level. Additionally, it is possible that an increase in risk at night may be offset by a reciprocal decrease at another time of day. For example, morning wakefulness may be protective due to sleep satiety and naturally occurring circadian peaks in mood and cognition. If true, then these effects may vary from weekdays to weekends due to societal shifts in sleep/wake patterns (i.e. social jetlag). The present study used a large community sample to explore the relationship between timing of wakefulness and suicidal ideation. More specifically, analyses explored how clusters of wakefulness at night and in the morning were associated with suicidal ideation, even when accounting for mental health, sleep duration, sleep quality, and chronotype, and whether these associations varied for weekdays/workdays versus weekends/non-workdays.
Methods
Participants
Data were acquired from the Sleep and Healthy Activity, Diet, Environment, and Socialization study, an internet-based questionnaire study of adults aged 22–60 in the Philadelphia area. Subjects were recruited through advertisements and community centers without regard to medical or psychiatric comorbidity. Subjects were required to complete all elements of the questionnaire to receive compensation, and only completed data were used for analysis. The Institutional Review Board at the University of Pennsylvania approved this study, and informed consent was obtained from each subject through electronic signatures.
Measures
Sleep timing was assessed using the Sleep Timing Questionnaire [33], a retrospective questionnaire of sleep on weekdays/workdays and weekends/non-workdays. Subjects reported their time to bed as “the time at which you are finally in bed and trying to fall asleep” for nights before a work/school day and for nights before a day off. Subjects similarly reported their time out of bed as “the time at which you finally get out of bed and start your day.” Responses were based on a recent, average week.
Depression symptoms were assessed using the Patient Health Questionnaire-9 (PHQ-9) [34], which asks about the frequency of nine symptoms over the past 2 weeks. Participants could respond “Not at all,” “Several days,” “More than half the days,” and “Nearly every day.” Suicidal ideation was assessed using PHQ-9 item 9 (“thoughts that you would be better off dead or of hurting yourself in some way”). Individuals who reported “Not at all” were coded as “No Suicidal Ideation” and all other responses were coded as “Suicidal Ideation.” Overall depression severity was assessed by combining the remaining eight items into an adjusted PHQ-9 score. Anxiety symptoms were assessed using the Generalized Anxiety Disorder-7 (GAD-7) screening questionnaire [35], which asks about the frequency of seven symptoms over the past 2 weeks. Anxiety severity was measured as the total GAD-7 score.
Insomnia was assessed using the Insomnia Severity Index [36] total score, while sleep quality was assessed using the Pittsburgh Sleep Quality Index [37] total score. Respondents were asked “how much sleep do you usually get at night on weekdays or workdays?,” with responses coded as short (<7.00 h), typical (7–8.99 h), or long (>8.99 h) based on prior studies [38, 39]. To estimate chronotype, subjects were asked if they slept better if they went to bed before 9:00 pm and woke up before 5:30 am (advanced), or if they slept better if they went to bed after 1:00 am and woke up after 9:00 am (delayed). Subjects could respond with never, seldom (once/year), sometimes (once/month), often (once/week), or frequently (more than 3 times/week). These variables were then dichotomized with often or frequently as yes and never, seldom, or sometimes as no. Individuals with no preference were labelled “Typical.”
Subjects additionally reported their age, sex, race/ethnicity, income level, education level, and current employment status as covariates for analyses. Finally, if any subject reported evening or overnight shift work, they were eliminated from the sample.
Statistical analyses
All analyses were performed with R (v. 3.5.1). One-way ANOVAs and chi-squared tests evaluated how sociodemographic (age, sex, race/ethnicity, income, education, and employment) and clinical (adjusted PHQ score, GAD-7 score, PSQI score, ISI score, hours awake, total sleep time, advanced phase, and delayed phase) variables varied by suicidal ideation status. Graphical analyses investigated how wakefulness varied by suicidal ideation status and whether this differed significantly depending on chronotype. Multivariable binomial regression models then estimated the associations between hours of wakefulness across the day and suicidal ideation, with additional adjustment for sociodemographic factors and anxiety/depression severity. Additional multivariable binomial models then explored how timing of wakefulness compared to other sleep variables in associating with suicidal ideation. Finally, two-way ANOVAs tested for significant interactions between timing of wakefulness and other sleep variables in association with suicidal ideation.
Results
Sample characteristics
After removing shift workers, the final sample included N = 888 subjects with available weekday wakefulness data, and N = 854 subjects with available weekend/non-workday wakefulness data. The sample had a mean age of 34 years (SD 9.5) and was predominantly white (61%) and female (62%). Data from weekdays/workdays included 192 individuals with suicidal ideation (21.6%), while data from weekends/non-workdays included 147 individuals with suicidal ideation (21.0%). Suicidal ideation did not vary by age (p = 0.7409), race (p = 0.8311), or income (p = 0.0892), but did vary by sex (p = 0.0055), education (p = 0.0002), and employment (p < 0.0001). Post hoc testing showed that suicidal ideation was more associated with being male, having less than a college education, and not working. These results are presented in Table 1.
Table 1.
Sociodemographic factors in the sample by suicidal ideation status
| Demographics | Total sample | No suicidal ideation | Suicidal ideation | P-value |
|---|---|---|---|---|
| N | 888 (100) | 696 (78.4) | 192 (21.6) | |
| Age | 34.1 ± 9.5 | 34 ± 9.4 | 34.3 ± 9.7 | 0.7409 |
| Sex | ||||
| Male | 334 (37.61) | 245 (35.2) | 89 (46.35) | 0.0055 |
| Female | 554 (62.39) | 451 (64.8) | 103 (53.65) | |
| Race/ethnicity | ||||
| White | 542 (61.04) | 429 (61.64) | 113 (58.85) | 0.8311 |
| Asian | 51 (5.74) | 40 (5.75) | 11 (5.73) | |
| Black | 207 (23.31) | 160 (22.99) | 47 (24.48) | |
| Hispanic | 38 (4.28) | 30 (4.31) | 8 (4.17) | |
| Other Race | 47 (5.29) | 34 (4.89) | 13 (6.77) | |
| Income | ||||
| <$20,000 | 164 (18.47) | 120 (17.24) | 44 (22.92) | 0.0892 |
| $20,000–$50,000 | 315 (35.47) | 239 (34.34) | 76 (39.58) | |
| $50,000–$100,000 | 336 (37.84) | 275 (39.51) | 61 (31.77) | |
| $100,000–$150,000 | 62 (6.98) | 51 (7.47) | 10 (5.21) | |
| $150,000+ | 11 (1.24) | 10 (1.44) | 1 (0.52) | |
| Education | ||||
| College | 522 (58.78) | 430 (61.78) | 92 (47.92) | 0.0002 |
| Some college | 257 (28.94) | 196 (28.16) | 61 (31.77) | |
| High school | 86 (9.68) | 58 (8.33) | 28 (14.58) | |
| Less than high school | 23 (2.59) | 12 (1.72) | 11 (5.73) | |
| Employment | ||||
| Full-time | 384 (43.24) | 324 (46.55) | 60 (31.25) | <0.0001 |
| Part-time | 132 (14.86) | 102 (14.66) | 30 (15.62) | |
| Multiple jobs | 60 (6.76) | 47 (6.75) | 13 (6.77) | |
| Student | 120 (13.51) | 99 (14.22) | 21 (10.94) | |
| Not working | 192 (21.62) | 124 (17.82) | 68 (35.42) |
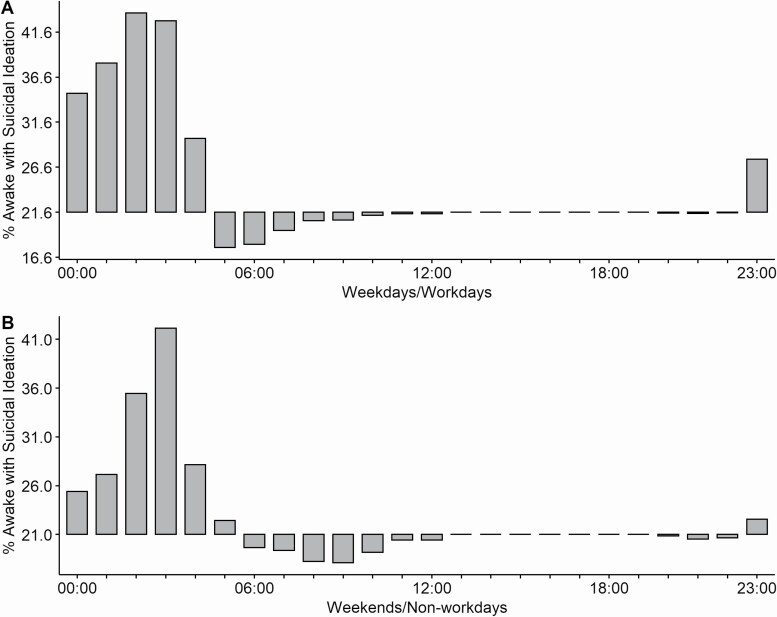
Weekday and weekend distribution of suicidal ideation by clock hour
To determine an individual’s wakefulness across the day, the time to bed and time out of bed data from the Sleep Timing Questionnaire were used to estimate wakefulness for each clock hour. A preliminary graphical analysis then determined whether the proportion of individuals awake with suicidal ideation varied across the day for weekdays/workdays and weekends/non-workdays. These results are presented in Figure 1. For weekdays, individuals with suicidal ideation were overrepresented among those awake from 11:00 pm to 4:59 am and underrepresented from 5:00 am to 10:00 am compared to their total proportion within the population (1A). Weekends showed a similar pattern with overrepresentation from 11:00 pm to 4:59 am and underrepresentation from 5:00 am to 12:59 pm (1B). Consequently, clock hours were categorized for weekdays and weekends as follows: Night (11:00 pm to 4:59 am); Morning (5:00 am to 10:59 am); Afternoon (11:00 am to 4:59 pm); and Evening (5:00 pm to 10:59 pm).
Figure 1.
The proportion of the awake sample reporting suicidal ideation across the day for weekdays (A) and weekends (B). The data are centered at the overall prevalence of suicidal ideation within each sample (21.6% for weekdays and 20.4% for weekends). In both cases, individuals with suicidal ideation are more prevalent between 11:00 pm and 4:59 am, and less prevalent between 5:00 am and 10:59 am.
Table 2 presents a comparison of individuals with and without suicidal ideation across measures of mental health and sleep, as well as weekday and weekend wakefulness. Individuals with suicidal ideation reported greater adjusted PHQ scores, greater GAD scores, greater PSQI scores, and greater ISI scores (all p < 0.0001). Total sleep time varied significantly by suicidal ideation status (p < 0.0001), with suicidal ideation overrepresented among short sleepers. While early sleepers showed no variation across suicidal ideation status, late sleepers were more likely to report suicidal ideation (p < 0.0001). Finally, individuals with suicidal ideation reported fewer morning hours awake on weekdays (p = 0.0007) and weekends (p = 0.0033), and more nighttime hours awake on weekdays (p < 0.0001) and weekends (p = 0.0016). Individuals with suicidal ideation went to bed 30 min later and woke up 24 min later on weekdays and weekends. Wakefulness on weekday afternoons and evenings was not significantly different for individuals with suicidal ideation (p > 0.05). While weekend differences for afternoon and evening wakefulness were statistically significant, they were not functionally meaningful—individuals with suicidal ideation reported 6 min less wakefulness in the afternoon (p < 0.0001) and 4.2 min less in the evening (p = 0.0297). Consequently, afternoon and evening wakefulness were not analyzed further.
Table 2.
Sleep, mental health, and time of day wakefulness by suicidal ideation status
| Questionnaire scores | Total sample | No suicidal ideation | Suicidal ideation | P-value |
|---|---|---|---|---|
| Adjusted PHQ-9 | 8.0 ± 5.9 | 6.4 ± 4.9 | 13.7 ± 5.3 | <0.0001 |
| GAD-7 | 7.0 ± 5.6 | 5.5 ± 4.8 | 12.2 ± 5.2 | <0.0001 |
| PSQI | 8.1 ± 4.1 | 7.4 ± 3.8 | 10.6 ± 4.3 | <0.0001 |
| ISI | 10.3 ± 6.3 | 9.2 ± 5.9 | 14.1 ± 6.1 | <0.0001 |
| Total sleep time | ||||
| Short | 412 (46.4) | 291 (41.8) | 121 (63.0) | <0.0001 |
| Normal | 437 (49.2) | 375 (53.9) | 62 (32.3) | |
| Long | 39 (4.4) | 30 (4.3) | 9 (4.7) | |
| Advanced phase | ||||
| No | 797 (89.8) | 631 (90.7) | 166 (86.5) | 0.1059 |
| Yes | 91 (10.2) | 65 (9.3) | 26 (13.5) | |
| Delayed phase | ||||
| No | 592 (66.7) | 489 (70.3) | 103 (53.6) | <0.0001 |
| Yes | 296 (33.3) | 207 (29.7) | 89 (46.4) | |
| Hours awake weekday/workday | ||||
| Time to bed | 11:23 PM | 11:18 PM | 11:48 PM | <0.0001 |
| Time out of bed | 7:11 AM | 7:06 AM | 7:30 AM | 0.0005 |
| Morning | 4.34 ± 1.30 | 4.42 ± 1.24 | 4.06 ± 1.46 | 0.0007 |
| Afternoon | 5.99 ± 0.12 | 6.00 ± 0.08 | 5.98 ± 0.20 | 0.0577 |
| Evening | 5.86 ± 0.48 | 5.87 ± 0.46 | 5.85 ± 0.52 | 0.6799 |
| Night | 0.99 ± 1.21 | 0.87 ± 1.10 | 1.46 ± 1.44 | <0.0001 |
| Hours awake weekend/non-workday | ||||
| Time to bed | 12:20 AM | 12:12 AM | 12:42 AM | 0.0002 |
| Time out of bed | 8:41 AM | 8:36 AM | 9:00 AM | 0.0043 |
| Morning | 2.87 ± 1.59 | 2.96 ± 1.53 | 2.53 ± 1.76 | 0.0033 |
| Afternoon | 5.97 ± 0.24 | 5.99 ± 0.14 | 5.89 ± 0.44 | <0.0001 |
| Evening | 5.93 ± 0.36 | 5.95 ± 0.31 | 5.88 ± 0.51 | 0.0297 |
| Night | 1.80 ± 1.42 | 1.72 ± 1.37 | 2.13 ± 1.55 | 0.0016 |
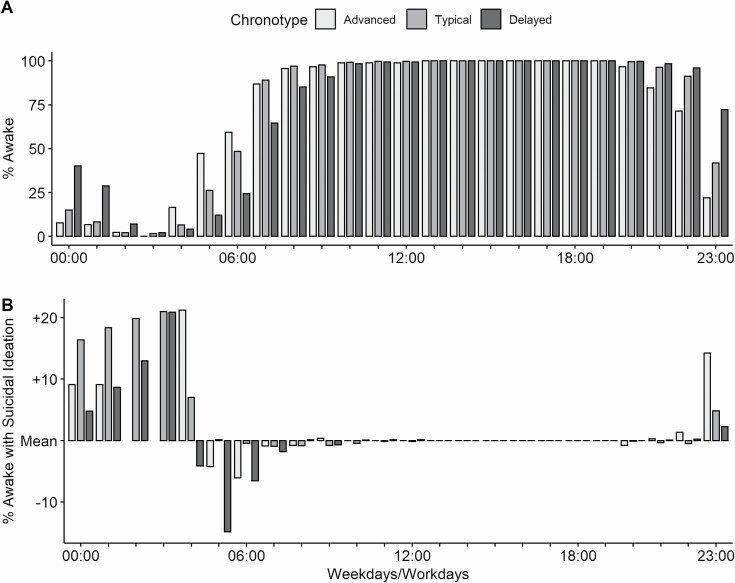
Exploring wakefulness and chronotype
Because some individuals in the sample endorsed advanced or delayed sleep timing, it is possible that the clock hour groupings described above may not apply equally to all individuals. An additional graphical analysis was conducted to address this issue, which is presented in Figure 2. Compared to individuals without a sleep phase preference (“Typical”), advanced chronotypes tended to go to bed early and get up early, while delayed individuals did the opposite (Figure 2, A), thus adding some validity to the two-item assessment of chronotype in the sample. Despite these variations, the prevalence of suicidal ideation among the awake sample followed the same pattern as the overall sample (Figure 2, B). Specifically, individuals with suicidal ideation were overrepresented between 11:00 pm and 4:59 am, underrepresented between 5:00 am and 10:59 am, and otherwise as expected throughout the afternoon and evening. Thus, the grouping of clock hours seems appropriate despite variations in sleep timing due to chronotype.
Figure 2.
Timing of wakefulness by chronotype and suicidal ideation. Variations in population wakefulness are presented for individuals with advanced, typical, or delayed chronotypes (A). Despite these variations, individuals of all chronotypes with suicidal ideation were overrepresented at night and underrepresented in the morning (B). The data in (B) are centered at the mean prevalence of suicidal ideation within each chronotype (16.5% for typical, 24.2% for advanced, and 29.2% for delayed).
Timing of wakefulness is associated with suicidal ideation
Three binomial logistic regression models estimated the associations between morning and nighttime wakefulness on weekdays and weekends with suicidal ideation. Model 1 was unadjusted, model 2 adjusted for sociodemographic factors (age, sex, race/ethnicity, income, and education), and model 3 adjusted for sociodemographic factors as well as adjusted PHQ-9 and GAD-7 scores. The results for morning and nighttime wakefulness are presented in Table 3, with the full models with all parameters are detailed in Supplementary Table S1. In unadjusted analyses, each hour awake in the morning reduced the likelihood of suicidal ideation (weekday OR: 0.82 [0.72–0.92]; weekend OR: 0.84 [0.75–0.94]), and each hour awake at night increased the likelihood of suicidal ideation (weekday OR: 1.44 [1.28–1.64]; weekend OR 1.22 [1.08–1.39]). Although all associations remained significant when adjusting for sociodemographic factors, only weekday nocturnal wakefulness remained associated with suicidal ideation when adjusting for anxiety and depression severity (OR 1.22 [1.04–1.43]). To determine why morning wakefulness was no longer significant, post hoc analysis explored whether individuals with higher levels of depression or anxiety were less awake in the mornings. Individuals with elevated anxiety (GAD score > 10) were less awake in the morning (−14.4 min, t-test p = 0.0123) as were individuals with elevated depression (adjusted PHQ > 9, −19 min, t-test p = 0.0006).
Table 3.
The associations between suicidal ideation and morning / night wakefulness
| Time of day | Weekday/workday | Weekend/Non-workday | ||||
|---|---|---|---|---|---|---|
| Unadjusted | Odds ratio | 95% CI | P-value | Odds ratio | 95% CI | P-value |
| Morning | 0.82 | [0.72, 0.92] | 0.0008 | 0.84 | [0.75, 0.94] | 0.0035 |
| Night | 1.44 | [1.28, 1.64] | <0.0001 | 1.22 | [1.08, 1.39] | 0.0018 |
| Adjusted for demographics | ||||||
| Morning | 0.87 | [0.77, 0.99] | 0.0316 | 0.89 | [0.8, 0.99] | 0.0399 |
| Night | 1.35 | [1.19, 1.55] | <0.0001 | 1.26 | [1.11, 1.43] | 0.0002 |
| Adjusted for mental health | ||||||
| Morning | 0.89 | [0.76, 1.03] | 0.1252 | 0.94 | [0.83, 1.07] | 0.3760 |
| Night | 1.22 | [1.04, 1.43] | 0.0147 | 1.15 | [0.99, 1.33] | 0.0622 |
Comparing timing of wakefulness and other sleep parameters
A second series of binomial logistic regression models investigated how timing of wakefulness compared to other sleep variables in associating with suicidal ideation. Night and morning wakefulness for weekdays and weekends were included as predictors along with sleep duration, insomnia severity, sleep quality, and advanced or delayed phase preferences. These results are presented in Table 4. Weekday nocturnal wakefulness was positively associated with suicidal ideation (OR 1.25 [1.09–1.44] per hour awake), along with insomnia severity (OR 1.06 [1.01–1.11] per additional point on the ISI), and sleep quality (OR 1.12 [1.05–1.21] per additional point on the PSQI), while there was no association between weekend nocturnal wakefulness and suicidal ideation (p = 0.2337). Weekday morning wakefulness was marginally negatively associated with suicidal ideation (OR 0.88 [0.76–1.00] per hour awake), along with insomnia severity (OR 1.06 [1.02–1.11] per additional point on the ISI), sleep quality (OR 1.11 [1.04–1.20] per additional point on the PSQI), and delayed phase preference (OR 1.46 [1.01–2.1]). Weekend morning wakefulness was not associated with suicidal ideation (p = 0.0826).
Table 4.
Comparing suicidal ideation, timing of wakefulness, and other sleep variables
| Weekday or weekend | Weekdays/workdays | Weekends/Non-workdays | ||||
|---|---|---|---|---|---|---|
| Predictors | OR | 95% CI | P-value | OR | 95% CI | P-value |
| Morning wakefulness | 0.88 | [0.76, 1] | 0.0562 | 0.89 | [0.78, 1.01] | 0.0826 |
| Short sleep | 1.13 | [0.74, 1.73] | 0.5640 | 1.15 | [0.72, 1.83] | 0.5645 |
| Long sleep | 1.48 | [0.59, 3.37] | 0.3757 | 1.55 | [0.56, 3.84] | 0.3626 |
| ISI score | 1.06 | [1.02, 1.11] | 0.0083 | 1.05 | [1, 1.1] | 0.0729 |
| PSQI score | 1.11 | [1.04, 1.2] | 0.0027 | 1.11 | [1.03, 1.21] | 0.0104 |
| Advanced phase | 1.33 | [0.77, 2.26] | 0.3006 | 1.34 | [0.69, 2.47] | 0.3691 |
| Delayed phase | 1.46 | [1.01, 2.1] | 0.0449 | 1.55 | [1.01, 2.37] | 0.0447 |
| Predictors | ||||||
| Nighttime wakefulness | 1.25 | [1.09, 1.44] | 0.0020 | 1.09 | [0.94, 1.26] | 0.2337 |
| Short sleep | 0.94 | [0.61, 1.43] | 0.7641 | 1.07 | [0.67, 1.71] | 0.7771 |
| Long sleep | 1.70 | [0.69, 3.82] | 0.2205 | 1.66 | [0.61, 4.09] | 0.2889 |
| ISI score | 1.06 | [1.01, 1.11] | 0.0150 | 1.04 | [0.99, 1.1] | 0.1019 |
| PSQI score | 1.12 | [1.05, 1.21] | 0.0014 | 1.12 | [1.03, 1.21] | 0.0068 |
| Advanced phase | 1.44 | [0.83, 2.45] | 0.1865 | 1.31 | [0.67, 2.44] | 0.4095 |
| Delayed phase | 1.38 | [0.96, 1.99] | 0.0843 | 1.66 | [1.09, 2.5] | 0.0170 |
Two-way ANOVAs assessed whether there were any significant interactions between timing of wakefulness and other sleep measures (e.g. weekday nighttime wakefulness by sleep duration). A marginally significant weekday nighttime wakefulness by advanced phase interaction was observed (p = 0.0433), but post hoc Wald testing showed the interaction term was not significant (p = 0.0617). No other significant interactions were identified.
Discussion
In this exploratory study of a community sample, individuals with suicidal ideation were consistently more likely to report being awake between 11:00 pm and 5:00 am across all models. Moreover, individuals with suicidal ideation were less likely to report wakefulness between 5:00 am and 11:00 am in some cases. These findings were replicated for weekday/workday and weekend/non-workday wakefulness when adjusting for sociodemographic covariates. Additionally, weekday nighttime wakefulness was associated with suicidal ideation even when considering total sleep time, insomnia severity, sleep quality, and chronotype. These findings suggest that nocturnal wakefulness is independently associated with suicidal ideation, though further studies are needed to confirm the role of sleep timing in STBs.
Associations between timing of wakefulness and suicidal ideation
Unlike previous investigations where nighttime was defined a priori as the interval between 12:00 am and 6:00 am [22, 23], this study used an exploratory approach to categorize hours when suicidal ideation was more or less present among the awake sample. Since suicidal ideation was more evident between 11:00 pm and 5:00 am and less so between 5:00 am and 11:00 pm, time of day categories were shifted by 1 h to maximize these differences. In the logistic regression models, morning wakefulness reduced and nocturnal wakefulness increased the likelihood of suicidal ideation, even when adjusting for sociodemographic factors such as employment status. However, when accounting for depression and anxiety, only weekday nocturnal wakefulness remained significant (albeit mitigated in strength); weekend nocturnal wakefulness became marginally insignificant, while morning wakefulness was no longer significant. These changes seem reasonable considering how strongly anxiety and depression have been linked to sleep disturbances [40, 41] which often alter sleep timing. For example, an individual with anxiety or depression may go to bed later due to difficulty with sleep, thus delaying when they get out of bed and reducing next-day morning wakefulness. Alternatively, these changes may stem from changes in daytime commitments on weekdays versus weekends, although logistic models did adjust for employment status to reduce this effect. The marginal non-significance of weekend nocturnal wakefulness may also be related to study power in addressing so many covariates.
Comparing timing of wakefulness against sleep duration, quality, and chronotype
Mounting research supports disrupted sleep as an evidence-based risk factor for suicide [42]. Consistent with previous reports, individuals with suicidal ideation in this sample reported worse sleep quality [43, 44], worse insomnia [3, 45], sleep duration of less than 7 h [44–46], and preferred a delayed sleep schedule [47, 48] (Table 2). The present study expands previous findings by exploring how each of these variables compare to each other and to the timing of wakefulness. As reported in Table 4, weekday nocturnal wakefulness, insomnia severity, and sleep quality increased the likelihood of suicidal ideation while sleep duration and chronotype preferences were not significant predictors. Although all three metrics were determined by self-report, nocturnal wakefulness contrasts with the ISI and PSQI scores by assessing when people sleep, not their subjective ability to sleep or perceived sleep quality. Thus, nocturnal wakefulness may represent a more biologically oriented risk factor for STBs. Interestingly, weekend nocturnal wakefulness was not associated with suicidal ideation, unlike preference for a delayed sleep phase which was a significant predictor. This difference may arise because the definition of “night” changes from weekdays to weekends: 1:00 am may be late on a worknight but normal for a weekend, while individual phase preferences may not shift across days. Conversely, the negative association between suicidal ideation and morning wakefulness was only marginally insignificant when accounting for other sleep variables, which may reflect a sample size limitation when accounting for so many variables.
Strengths and limitations
Previous data have shown that nighttime wakefulness is a predictor of death by suicide [22]. However, data evaluating nocturnal wakefulness as a risk factor for other STBs remain limited. Ballard and colleagues previously reported that nocturnal wakefulness measured by polysomnography was associated with next-day suicidal ideation [24], but this finding was limited to a small sample of depressed and bipolar patients. The present study generalizes this clinical finding to a large, non-clinical population and indicates that wakefulness during an individual’s biological night may increase the likelihood of STBs, while wakefulness during the morning may reduce it. Together, these findings hint at a temporal rhythm of suicide risk which may be influenced by sleep and circadian factors.
This study has several limitations. First, the results are drawn from a cross-sectional survey, which means that the directionality of these associations cannot be assessed. Longitudinal studies of sleep timing and suicidal ideation are needed to confirm these results. Additionally, the accuracy of these findings is limited to the accuracy of individual self-report, including single-item assessments of sleep duration and chronotype. However, the usual concerns about over or underestimating sleep duration are not as relevant because the primary goal was to explore timing of wakefulness, not sleep duration. Thus, while an individual who reports going to bed at 9:00 pm may not actually fall asleep for several hours, it seems safe to assume that individual is not asleep prior to 9:00 pm. Of course, more objective measures of sleep are needed to confirm this assumption. Another concern is that, while this sample was drawn from a community-dwelling population, the high prevalence of insomnia (N = 223) and suicidal ideation (N = 192) suggests these results may not generalize broadly. However, the large number of suicidal ideators in the sample increases confidence that these results are accurate for those reporting suicidal ideation.
Conclusion
Previous data show that nocturnal wakefulness is a risk factor for death by suicide and suicidal ideation in clinical samples. The present study explored the timing of wakefulness among individuals with and without suicidal ideation from an online recruited non-clinical sample. After adjusting for sociodemographic factors, wakefulness between 11:00 pm and 5:00 am was associated with more prevalent suicidal ideation. Additionally, wakefulness between 5:00 am and 11:00 am was associated with reduced ideation in some models. Moreover, the relationship between nocturnal wakefulness and suicidal ideation remained significant after adjusting for anxiety and depression severity, sleep duration, sleep quality, insomnia severity, and chronotype. Additional research is needed to confirm these findings in a larger nationally representative sample, and to explore potential mechanisms connecting the timing of wakefulness to suicide risk.
Supplementary Material
Acknowledgments
F.X.F. acknowledges financial support from the Velux Stiftung (Proj. No. 1360). Additionally, this paper is dedicated to the late Dr Marna Barrett, who contributed to this manuscript and the broader mood disorders research community.
Disclosure Statement
Financial disclosure: This work was funded by National Institute of Environmental Health Sciences (NIEHS) R21 ES022931.
Non-financial disclosure: None declared.
References
- 1. Pigeon WR, et al. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73(9):e1160–e1167. [DOI] [PubMed] [Google Scholar]
- 2. Wang HE, et al. Pre-deployment insomnia is associated with post-deployment post-traumatic stress disorder and suicidal ideation in US Army soldiers. Sleep. 2019;42(2). doi: 10.1093/sleep/zsy229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zuromski KL, et al. Insomnia symptoms drive changes in suicide ideation: a latent difference score model of community adults over a brief interval. J Abnorm Psychol. 2017;126(6):739–749. [DOI] [PubMed] [Google Scholar]
- 4. Rössler W, et al. Sleep disturbances and suicidality—A longitudinal analysis from a representative community study over 30 years. Front Psychiatry. 2018;9:320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McCall WV, et al. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Med. 2010;11(9):822–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ferentinos P, et al. Sleep disturbance as a proximal predictor of suicidal intent in recently hospitalized attempters. Sleep Med. 2016;19:1–7. [DOI] [PubMed] [Google Scholar]
- 7. Li SX, et al. Nocturnal sleep disturbances as a predictor of suicide attempts among psychiatric outpatients: a clinical, epidemiologic, prospective study. J Clin Psychiatry. 2010;71(11):1440–1446. [DOI] [PubMed] [Google Scholar]
- 8. Lin HT, et al. Insomnia as an independent predictor of suicide attempts: a nationwide population-based retrospective cohort study. BMC Psychiatry. 2018;18(1):117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sun L, et al. Insomnia symptom, mental disorder and suicide: a case-control study in chinese rural youths. Sleep Biol Rhythms. 2015;13(2):181–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fujino Y, et al. Prospective cohort study of stress, life satisfaction, self-rated health, insomnia, and suicide death in Japan. Suicide Life Threat Behav. 2005;35(2):227–237. [DOI] [PubMed] [Google Scholar]
- 11. Pigeon WR, et al. Sleep disturbance preceding suicide among veterans. Am J Public Health. 2012;102Suppl 1:S93–S97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Trockel M, et al. Effects of cognitive behavioral therapy for insomnia on suicidal ideation in veterans. Sleep. 2015;38(2):259–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McCall WV, et al. Reducing suicidal ideation through insomnia treatment (REST-IT): a randomized clinical trial. Am J Psychiatry. 2019;176(11):957–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pigeon WR, et al. Brief CBT for insomnia delivered in primary care to patients endorsing suicidal ideation: a proof-of-concept randomized clinical trial. Transl Behav Med. 2019;9(6):1169–1177. [DOI] [PubMed] [Google Scholar]
- 15. Tubbs AS, et al. Surviving the long night: the potential of sleep health for suicide prevention. Sleep Med Rev. 2019;44:83–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hom MA, et al. Thwarted belongingness as an explanatory link between insomnia symptoms and suicidal ideation: findings from three samples of military service members and veterans. J Affect Disord. 2017;209:114–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chu C, et al. Is insomnia lonely? Exploring thwarted belongingness as an explanatory link between insomnia and suicidal ideation in a sample of South Korean university students. J Clin Sleep Med. 2016;12(5):647–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chu C, et al. Insomnia and suicide-related behaviors: a multi-study investigation of thwarted belongingness as a distinct explanatory factor. J Affect Disord. 2017;208:153–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mann JJ. A current perspective of suicide and attempted suicide. Ann Intern Med. 2002;136(4):302–311. [DOI] [PubMed] [Google Scholar]
- 20. Mann JJ, et al. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156(2):181–189. [DOI] [PubMed] [Google Scholar]
- 21. Perlis ML, et al. Suicide and sleep: is it a bad thing to be awake when reason sleeps? Sleep Med Rev. 2016;29:101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Perlis ML, et al. Nocturnal wakefulness as a previously unrecognized risk factor for suicide. J Clin Psychiatry. 2016;77(6):e726–e733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tubbs AS, et al. Relationship of nocturnal wakefulness to suicide risk across months and methods of suicide. J Clin Psychiatry. 2020;81(2):19m12964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ballard ED, et al. Nocturnal wakefulness is associated with next-day suicidal ideation in major depressive disorder and bipolar disorder. J Clin Psychiatry. 2016;77(6):825–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Boivin DB, et al. Complex interaction of the sleep-wake cycle and circadian phase modulates mood in healthy subjects. Arch Gen Psychiatry. 1997;54(2):145–152. [DOI] [PubMed] [Google Scholar]
- 26. Monk TH, et al. Circadian rhythms in human performance and mood under constant conditions. J Sleep Res. 1997;6(1):9–18. [DOI] [PubMed] [Google Scholar]
- 27. Wirz-Justice A. Diurnal variation of depressive symptoms. Dialogues Clin Neurosci. 2008;10(3):337–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Murray G, et al. Mood and the circadian system: investigation of a circadian component in positive affect. Chronobiol Int. 2002;19(6):1151–1169. [DOI] [PubMed] [Google Scholar]
- 29. Adan A, et al. Relationship between circadian typology and functional and dysfunctional impulsivity. Chronobiol Int. 2010;27(3):606–619. [DOI] [PubMed] [Google Scholar]
- 30. Kuula L, et al. Naturally occurring circadian rhythm and sleep duration are related to executive functions in early adulthood. J Sleep Res. 2018;27(1):113–119. [DOI] [PubMed] [Google Scholar]
- 31. McGowan NM, et al. Sleep and circadian rhythm function and trait impulsivity: an actigraphy study. Psychiatry Res. 2018;268:251–256. [DOI] [PubMed] [Google Scholar]
- 32. Russo PM, et al. Circadian preference and the big five: the role of impulsivity and sensation seeking. Chronobiol Int. 2012;29(8):1121–1126. [DOI] [PubMed] [Google Scholar]
- 33. Monk TH, et al. Measuring sleep habits without using a diary: the sleep timing questionnaire. Sleep. 2003;26(2):208–212. [DOI] [PubMed] [Google Scholar]
- 34. Spitzer RL, et al. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. [DOI] [PubMed] [Google Scholar]
- 35. Spitzer RL, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. [DOI] [PubMed] [Google Scholar]
- 36. Bastien CH, et al. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. [DOI] [PubMed] [Google Scholar]
- 37. Buysse DJ, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 38. Grandner MA, et al. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med. 2014;15(1):42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Whinnery J, et al. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37(3):601–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Li L, et al. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry. 2016;16(1):375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Cox RC, et al. A systematic review of sleep disturbance in anxiety and related disorders. J Anxiety Disord. 2016;37:104–129. [DOI] [PubMed] [Google Scholar]
- 42. Bernert RA, et al. Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatry Rep. 2015;17(3):554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Bernert RA, et al. Association of poor subjective sleep quality with risk for death by suicide during a 10-year period: a longitudinal, population-based study of late life. JAMA Psychiatry. 2014;71(10):1129–1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Littlewood DL, et al. Short sleep duration and poor sleep quality predict next-day suicidal ideation: an ecological momentary assessment study. Psychol Med. 2019;49(3):403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Chakravorty S, et al. Sleep duration and insomnia symptoms as risk factors for suicidal ideation in a nationally representative sample. Prim Care Companion CNS Disord. 2015;17(6). doi: 10.4088/PCC.13m01551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Gunnell D, et al. Sleep and suicide: an analysis of a cohort of 394,000 Taiwanese adults. Soc Psychiatry Psychiatr Epidemiol. 2013;48(9):1457–1465. [DOI] [PubMed] [Google Scholar]
- 47. Rumble ME, et al. The relationship of person-specific eveningness chronotype, greater seasonality, and less rhythmicity to suicidal behavior: a literature review. J Affect Disord. 2018;227:721–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Park H, et al. Chronotype and suicide: the mediating effect of depressive symptoms. Psychiatry Res. 2018;269:316–320. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.