Abstract
Background
Severe blepharoptosis with poor levator function (LF) has traditionally been managed with exogenous frontalis suspension but complications such as lagophthalmos, infection, and rejection are often reported.
Objectives
The aim of this study was to design a function-preserving frontalis orbicularis oculi muscle (FOOM) flap to correct severe blepharoptosis with poor LF. The long-term surgical outcome of the technique was assessed.
Methods
This retrospective study included only adult patients with severe blepharoptosis and poor LF, all of whom had their surgery performed by the senior surgeon over a 6-year period. Clinical assessment of LF, palpebral fissure height (PFH), marginal reflex distance 1 (MRD1), duration of follow-up, and postoperative complications were recorded.
Results
A total of 34 patients and 59 eyelids were recorded during a mean follow-up period of 17.7 months. Postoperative evaluation yielded mean [standard deviation] improvements of PFH gain of 5.62 [1.61] mm (P < 0.001), and MRD1 and PFH increases of 4.03 [0.82] mm (P < 0.001) and 8.94 [0.81] mm (P < 0.001), respectively. All patients demonstrated normalization of orbicularis function: no lagophthalmos was observed at the 8-month postoperative follow-up. Recurrence of ptosis was recorded in 4 eyelids (6.78%). Revisions were performed in 2 eyelids (3.39%). No infection or granuloma was noted.
Conclusions
The function-preserving FOOM flap is a useful vector for frontalis suspension. Not only does it effectively address lagophthalmos as well as other complications, but it provides aesthetically pleasing outcomes in patients with severe blepharoptosis and poor LF.
Level of Evidence: 4

Severe blepharoptosis may result in impaired visual acuity, amblyopia, or astigmatism if left untreated. Traditional frontalis suspension has been used to treat patients with severe blepharoptosis and poor levator function (LF) (<5 mm).1-4 However, postoperative lagophthalmos remains a common complication that not only causes pain, dry eye syndrome, and blurry vision, but potentially leads to keratopathy (corneal ulceration). The use of autologous materials, such as tensor fascia lata, has been reported to result in lower infection, granuloma formation, and recurrence rates than encountered with alloplastic materials.5-10 The pliability of the autologous local muscular flaps of the eyelids makes these a suitable option for upper blepharoplasty and spares a second surgical donor site.11-13
In 1996, Knize first described the interdigitation of frontalis muscle and the orbital portion of the orbicularis oculi muscle (OOM).14 Lai et al15-17 established the concept of the “frontal orbicularis oculi muscle (FOOM) flap” to denote the cross-linkage of the longitudinally oriented frontalis muscle and the horizontally oriented OOM of the orbital portion. The distinct anatomic continuation of the frontalis muscle and orbital OOM exerts a dynamic action on the muscles involved, which is the concept that was applied to the inception of the FOOM flap-shortening technique to address upper lid blepharoptosis.16,17 The frontalis muscle transfer technique, on the other hand, involves advancement of the muscular flap that connects directly to the tarsus without disturbing the OOM.18-20 However, the direct transfer of pure frontalis muscle may cause overcorrection of ptosis. Therefore the concept of utilizing the OOM flap as a vector in situ was developed to mitigate the effects of overcorrection caused by a direct frontalis muscle transfer.21-25 Previous FOOM flap-shortening procedures inevitably required sacrifice of a variable portion of the OOM during upper eyelid adjustment, which potentially affected its function.16,17,23-25 As a result, the function-preserving FOOM flap was developed by the senior author to correct severe blepharoptosis with poor LF while preserving the anatomic and functional integrity of the OOM. This study aimed to assess the surgical outcomes of this innovative technique, particularly with respect to postoperative lagophthalmos.
METHODS
Data Collection
A total of 34 adults and 59 eyelids treated with function-preserving FOOM flap-advancement surgery in our medical institution between February 2013 and December 2018 were included in this review; children were excluded from this study due to the lack of standardization in clinical assessment of LF in this cohort. The retrospective study protocol was approved by the institutional review board of Kaohsiung Medical University Hospital. Data including patient demographics, family and medical history, laboratory studies, perioperative eyelid examination results, and ptotic etiologies were reviewed in detail. Postoperative complications including infection, granuloma formation, overcorrection, ptosis recurrence, and lagophthalmos were recorded. For the clinical measurement of lagophthalmos, we asked the patients, in a sitting position, to close their eyes gently without squinting, and measured the space between the upper and lower eyelid margins with a ruler. The presence of lagophthalmos is defined by 2 consecutive measurements of the space >0.5 mm. The chi-square test was used to compare changes in marginal reflex distance 1 (MRD1), LF, and palpebral fissure height (PFH) perioperatively. The perioperative evaluations and operations were performed by the senior surgeon (C.S.L.).
Perioperative Evaluation and Clinical Presentations
Clinical measurement of LF, PFH, MRD1, and ptosis severity were evaluated in each patient. MRD1 is a standardized measurement for upper eyelid ptosis to determine the distance from the corneal light reflex on the patient to the central portion of the upper eyelid in primary gazing.26 Bell’s phenomenon, tear secretion, and Herring’s phenomenon were carefully examined. Ophthalmic and neurologic tests were performed if indicated. The anti-acetylcholine receptor antibody test was conducted for diagnostic workup of myasthenia gravis (MG) or ocular myasthenia gravis (OMG). A preoperative eye-closing power test was performed. The patients were asked to close their eyes and hold them firmly shut. If the examiner’s finger could open the eyelid easily, insufficient eye-closing power was present, and the surgery was not indicated for this condition.
Surgical Technique of Function-Preserving FOOM Flap Advancement
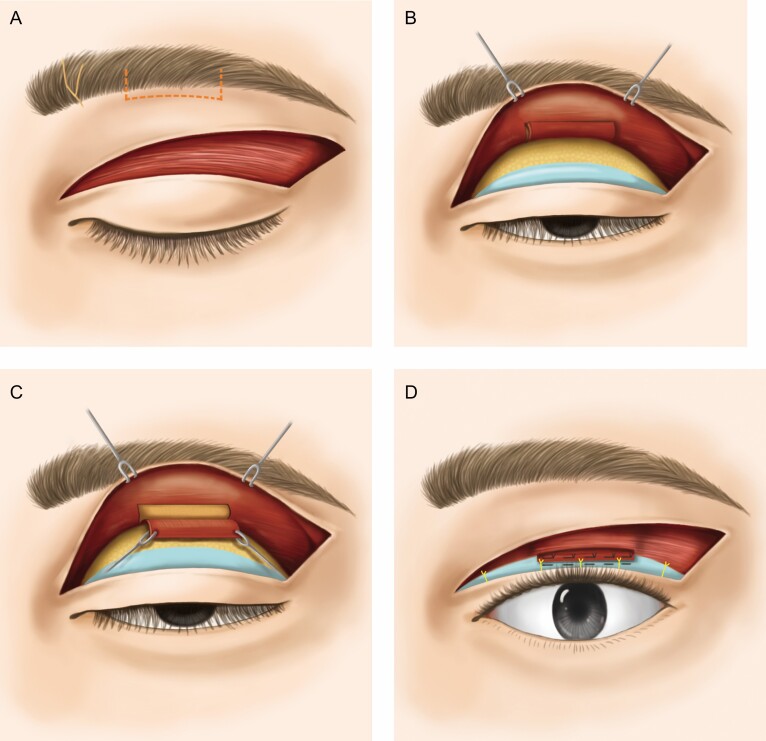
A video is provided to demonstrate the surgical technique (Video). The supraorbital foramen must be localized by palpation and marked to avoid nerve injury during the flap dissection. The operation was performed under local anesthesia except for patients who were pain-intolerant and required general anesthesia. Nerve block of the supraorbital, supratrochlear, and lacrimal nerves was completed first, followed by injection of local anesthetic mixture of 2% lidocaine containing 1:200,000 adrenaline to the eyelids. The desired muscular flap, measuring between 20 mm × 10 mm and 25 mm × 15 mm in size, was marked on the upper lid skin along the superior orbital rim. After excising redundant skin of the upper eyelid, a submuscular blunt dissection beneath the OOM was performed beyond the superior orbital rim to the sub-eyebrow area with meticulous hemostasis by bipolar electrocauterization. The orbital septum was left intact unless fat bag removal was indicated. The rectangular-shaped FOOM flap corresponding to the skin marking was then harvested and freed by subcutaneous dissection. Any tethered fiber was released until the FOOM flap was free for downward traction. The entire preseptal and orbital OOM was preserved and kept intact. The upper eyelid margin was adjusted and positioned at the upper border of the corneal limbus to determine the appropriate advancement of the FOOM flap when the patient was supine. The upper lid margin was adjusted to rest at 1 mm below the limbus when the patient was in a sitting position.13,22 The muscular flap was then anchored to the central and upper one-third of the tarsus with 6-0 nylon sutures. The excised excess muscle was diced into several pieces and used to fill in the gap above the FOOM flap to generate a smoother contour of the upper eyelid. A final evaluation of the upper eyelid margin position with the patient in a sitting position was performed for patients under local anesthesia before wound closure. Double-eyelid blepharoplasty was created at the last step. Five interrupted stitches were implanted for the double-eyelid creation. Three of these stitches were placed at the level of the midpupil and on either side, corresponding to medial and lateral corneal limbus. These key stitches included partial thickness of the upper third of the tarsus, a portion of the muscle flap, and the dermis of the eyelid skin edge. Two further stitches were placed in the pretarsal aponeurosis and the subdermal layer on the medial and lateral side of the upper eyelid. Securing the sutures between the tarsus and the FOOM flap is the key to avoiding dehiscence of the double-eyelid crease (Figure 1).
Figure 1.
The function-preserving FOOM flap advancement. (A) The rectangular flap is designed and marked on the upper eyelid skin. (B) The submuscular dissection proceeds superiorly beyond the superior orbital rim while the septum is maintained intact. (C) All tethered fibers are dissected until the FOOM flap is free for downward traction. (D) The flap is anchored to the central and upper third of the tarsus followed by the double-eyelid blepharoplasty (shown in yellow sutures). Excess muscle is diced into several pieces and placed in the flap base to generate a smoother contour of the upper eyelid. FOOM, frontalis orbicularis oculi muscle.
Postoperative Care
Temporary lagophthalmos may occur in all cases after surgery. Hence, immediate postoperative eye protection in the operating room is important. Moisture wrap dressing was used to cover the eyes with an ice pack during sleep. Application of artificial tear solutions during the day and eye lubricants at night were recommended to prevent exposure keratopathy and chemosis. Active eyeball movement was encouraged with the use of TobraDex eye suspension (dexamethasone and tobramycin; Alcon, Fort Worth, TX) to help prevent chemosis.27
RESULTS
A synopsis of the pertinent perioperative features of the 34 patients (12 males and 22 females) is given in Table 1. The mean [standard deviation] age was 45.3 [16.4] years (range, 18-74 years). The major etiology of blepharoptosis was myogenic type as presented in 54 eyelids of 31 cases (91.53%), followed by aponeurotic type in 4 eyelids of 2 cases (6.78%), and neurogenic type in a unilateral eyelid of 1 case (1.69%). Among the myogenic blepharoptosis group, intractable MG and OMG were diagnosed in 10 eyelids of 5 patients (16.95%). Oculopharyngeal muscular disorder (OPMD) was reported in 4 eyelids of 2 patients (6.78%). The follow-up period ranged from 6 months to 2 years and 7 months (average, 17.7 months). In Table 2, among all ptotic eyelids on which the function-preserving FOOM flap advancement was performed, improvements in MRD1 and PFH by 4.03 [0.82] mm (P < 0.001) and 8.94 [0.81] mm (P < 0.001) compared with their preoperative measurements of –2.51 [1.93] mm and 3.02 [1.67] mm, respectively, were recorded. A mean PFH gain of 5.62 [1.61] mm was achieved after surgery. All patients (100%) demonstrated lagophthalmos at 1 month follow-up due to temporary eyelid swelling. The number of lagophthalmos cases continued to decrease to 31 cases (52.54%) at 2 months, 8 cases (13.56%) at 4 months, and only 2 cases of minimal lagophthalmos (3.39%) at 6 months follow-up. Follow-up investigation of these 2 cases revealed no residual lagophthalmos (0%) at 8 months after surgery. Recurrence of mild ptosis was recorded in 4 eyelids (6.78%). Two patients (3.39%) underwent second revision with an eventual desirable outcome. The other 2 patients declined revision because they were satisfied with the results. No infection or granuloma formation was reported.
Table 1.
Clinical Summary of the Patients Receiving the Function-Preserving Frontalis Orbicularis Oculi Muscle Flap
| Patient information | |
|---|---|
| Number of cases | 34 |
| Age (years) | 45.3 ± 16.4 |
| Gender | Male: 12; female: 22 |
| Etiology of ptosis | |
| Myogenic | 54 (94.7%) |
| Aponeurotic | 4 (6.8%) |
| Neurogenic | 1 (1.8%) |
| Clinical evaluation | |
| Bilateral lids | 25 |
| Unilateral lids | 9 (left: 5; right: 4) |
| Follow-up (months) | 17.7 [9.5] |
| Postoperative complications after 8 months | |
| Lagophthalmos | 0% (0/59) |
| Recurrence | 6.8% (4/59) |
| Second revision | 3.4% (2/59) |
Table 2.
The Preoperative and Postoperative Ocular Measurements
| Clinical measurements | Preoperative | Postoperative | P value | ||
|---|---|---|---|---|---|
| 1 month | 3 months | 5 months | |||
| Lf (mm) | 3.5 [1.3] | 3.5 [1.7] | 3.6 [1.2] | 3.7 [0.6] | P = 0.63 |
| Mrd1 (mm) | -2.5 [1.9] | 3.1 [1.5] | 3.8 [0.9] | 4.0 [0.8] | P < 0.001 |
| Pfh (mm) | 3.4 [1.6] | 8.0 [1.4] | 8.7 [1.0] | 8.9 [0.8] | P < 0.001 |
| Mrd1 gaina (mm) | 4.0 [0.8] | ||||
| Pfh gaina (mm) | 5.6 [1.6] |
Values are numbers with percentages or mean [standard deviation]. Lf, levator function; mrd1, marginal reflex distance; pfh, palpebral fissure height.
aComparison between preoperative and postoperative results ≥6 months.
Case Reports
Case 1
This 18-year-old female had the history of MG diagnosed at the age of 2 years with thymus hyperplasia. She was referred from the neurologic department of another hospital due to refractory blepharoptosis despite medical treatment. She had been taking pyridostigmine 60 mg 4 times a day and presented with severe bilateral myogenic blepharoptosis. Her anti-acetylcholine receptor antibody level was 11.8 nmol/L. The PFH, MRD1, ptosis severity, and LF of her right/left eyelid were 3/3 mm, –2/–2 mm, 7/7 mm, and 5/5 mm, respectively. The extraocular muscle test showed voluntary movement; her eye-closing power was normal. Function-preserving FOOM flaps measuring 15 mm × 20 mm were designed for each eyelid. The eye-closing strength remained good without lagophthalmos postoperatively. Significant improvement of the bilateral ptosis was recorded with normalization of PFH 2 years and 7 months after surgery. Postoperative PFH, MRD1, ptosis severity, and LF of the eyelids were 9/9 mm, 4/4 mm, 1/1 mm, and 5/5 mm, respectively (Supplemental Figure 1).
Case 2
This 59-year-old female, referred from the ophthalmologic office, had a 10-year history of progressive bilateral blepharoptosis that had obscured her visual field. She had associated symptoms of progressive dysphagia, dysphonia, and slurred speech. The patient had the family history of OPMD that was diagnosed by genetic testing. She presented with long-term backward thrusting of the head, which enabled her to maintain a limited visual field through the narrow palpebral fissures. Preoperative PFH, MRD1, ptosis severity, and LF of her right/left eyelids were 1/1 mm, –4/–4 mm, 9/9 mm, and 4/4 mm, respectively. A function-preserving FOOM flap 20 mm × 25 mm was designed for frontalis suspension. At 18-month follow-up, the patient displayed normalized PFH, eye-closing function, and satisfactory upper eyelid contours. Postoperative PFH, MRD1, ptosis severity, and LF of the right/left eyelid were 8/8 mm, 3/3 mm, 2/2 mm, and 4/4 mm, respectively. The patient’s head and neck posture had returned to a normal position (Supplemental Figure 2).
DISCUSSION
The choice of frontalis suspensory material may determine the surgical outcome in the treatment of patients with severe blepharoptosis and poor LF. Autologous materials such as tensor fascia lata, palmaris longus, and temporal fascia have the advantages of reducing postoperative extrusion (0%–8.3%) and recurrence rate (4%–22%) compared with synthetic materials.28 Nevertheless, autologous tendon or fascia transfer has the disadvantage of creating a second surgical site that may cause donor-site morbidity. Banked allogenic fascia lata also poses the risks of premature absorption, cross-infection, and subsequent fibrous tissue formation that in turn will affect the long-term success rate. Easy accessibility of synthetic grafts (eg, silicone implants, nylon monofilament sutures and polytetrafluoroethylene sheets) and avoidance of donor-site morbidity are the main reasons for their widespread use.5-10 However, the complication rates with synthetic materials, including postoperative lagophthalmos, graft breakage, granuloma formation, and infection, continue to remain high (7%–45%).9,29-31
Local muscle flaps are a good alternative because they mitigate the need for a second donor site and the complications associated with implantation of foreign bodies. However, direct transfer of frontalis muscle to the tarsus, in spite of its comparatively shorter operative time, may cause prolonged postoperative lagophthalmos and loss of normal forehead wrinkles in cases of overcorrection.18,19 During the evolution of the FOOM flap surgery from our previous studies, the superiorly based OOM flap improved postoperative upper eyelid movement, but the resulting dynamic imbalance and antagonistic equilibrium during eyelid closure remained unresolved postoperatively. Wide dissection of the OOM for harvesting the double-breasted FOOM flap required longer operative time and yielded longer downtime.13,22 The function-preserving FOOM flap addresses lagophthalmos by performing submuscular dissection from the lower part of the orbital OOM, thereby leaving most OOM in situ without disturbing the integrity of the muscle.
The function-preserving FOOM flap has the following key properties: (1) it is an autologous muscular flap which is readily available in the same operative field of upper blepharoplasty, hence donor-site incision is not required; (2) the preservation of the orbital OOM allows near-normal eye-closing power; (3) the interlocking strength created by the horizontal fibers of OOM and the longitudinal fibers of frontalis muscle reinforces the durability of the FOOM flap and prevents it from attenuating. The frontalis muscle flap has demonstrated long-term elasticity and contractility, which is consistent with the histologic findings in our previous reports.16,17,32 Unlike the interdigital OOM flap suspension described by Wang et al,32 who successfully treated moderate to severe blepharoptosis, the rectangular function-preserving FOOM flap with minimal involvement of the lower part of the orbital OOM creates an evenly distributed force in the frontalis movement. Additionally, in order to keep the orbital septum intact, submuscular dissection was performed at the upper margin of the eyebrow, thereby minimizing surgical interruption of the anatomic integrity of the upper eyelid.
The 2 patients with aponeurotic blepharoptosis who demonstrated poor LF were the oldest patients (aged 71 and 74 years, respectively) in this study group. In fact, in our previous study of 126 patients and 231 eyelids, 4.3% of the severe ptotic eyelids displayed fair LF (6-9 mm). Kim and Lee33 reported 30% of their patients having fair even poor LF (<10 mm) in their involutional ptosis series. Poor LF was identified in about 1% of these patients with aponeurotic ptosis. LF was inversely proportional to the degree of fat tissue infiltration in patients of advanced age with aponeurotic ptosis.33,34
To achieve the ideal upper eyelid position and bilateral eyelid margin symmetry, the FOOM flap should be carefully anchored to the central and upper third of the tarsus with nonabsorbable sutures in at least partial thickness of the tarsus. We recommend placing the ptotic upper lid margin 1 mm below the limbus with the patient in a sitting position, and placing the upper limbus margin intraoperatively with the patient supine.13,22
The function-preserving FOOM flap significantly improves PPH and MRD1, and eliminates lagophthalmos 8 months postoperatively with a revision rate of 3.39%, and hence offers a functional and aesthetic outcome.
CONCLUSIONS
Functional preservation of the OOM is the key point in the correction of severe blepharoptosis with poor LF. In function-preserving FOOM flap advancement, we utilized the autologous muscle flap in the same operative field via a minimally invasive approach. The technique preserves the maximal anatomic integrity of the OOM, thereby maintaining its pliability during dynamic movements of the eyelids. The surgical technique not only corrects severe blepharoptosis effectively but also eliminates postoperative lagophthalmos and other complications better than traditional frontalis suspension.
Supplementary Material
Acknowledgments
Shu-Hung Huang and Chia-Chen Lee made an equal contribution to this work as co-first authors.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
We acknowledge the support for the study provided by the Ministry of Science and Technology of Taiwan (109-2314-B-037-020-MY3) and by the Kaohsiung Medical University Research Center (KMU-TC108A02-5) and KMUH109-9R30.
REFERENCES
- 1. Hague S, Collin R. Blepharoplasty and ptosis. Curr Opin Ophthalmol. 1994;5(5):67-73. [PubMed] [Google Scholar]
- 2. Ishii CH. Aesthetic plastic surgery in Asians: principles and techniques. Aesth Surg J. 2016;36(8):NP269-NP270. [DOI] [PubMed] [Google Scholar]
- 3. Finsterer J. Ptosis: causes, presentation, and management. Aesthetic Plast Surg. 2003;27(3):193-204. [DOI] [PubMed] [Google Scholar]
- 4. Clauser L, Tieghi R, Galiè M. Palpebral ptosis: clinical classification, differential diagnosis, and surgical guidelines: an overview. J Craniofac Surg. 2006;17(2):246-254. [DOI] [PubMed] [Google Scholar]
- 5. Wilson ME, Johnson RW. Congenital ptosis. Long-term results of treatment using lyophilized fascia lata for frontalis suspensions. Ophthalmology. 1991;98(8):1234-1237. [PubMed] [Google Scholar]
- 6. Philandrianos C, Galinier P, Salazard B, Bardot J, Magalon G. Congenital ptosis: long-term outcome of frontalis suspension using autogenous temporal fascia or fascia lata in children. J Plast Reconstr Aesthet Surg. 2010;63(5):782-786. [DOI] [PubMed] [Google Scholar]
- 7. Arajy ZY. Open loop fascial sling for severe congenital blepharoptosis. J Craniomaxillofac Surg. 2012;40(2):129-133. [DOI] [PubMed] [Google Scholar]
- 8. Manners RM, Tyers AG, Morris RJ. The use of prolene as a temporary suspensory material for brow suspension in young children. Eye (Lond). 1994;8(Pt 3):346-348. [DOI] [PubMed] [Google Scholar]
- 9. Hayashi K, Katori N, Kasai K, Kamisasanuki T, Kokubo K, Ohno-Matsui K. Comparison of nylon monofilament suture and polytetrafluoroethylene sheet for frontalis suspension surgery in eyes with congenital ptosis. Am J Ophthalmol. 2013;155(4):654-663.e1. [DOI] [PubMed] [Google Scholar]
- 10. Friedhofer H, Nigro MV, Sturtz G, Ferreira MC. Correction of severe ptosis with a silicone implant suspensor: 22 years of experience. Plast Reconstr Surg. 2012;129(3):453e-460e. [DOI] [PubMed] [Google Scholar]
- 11. Pan Y, Zhang H, Yang L, et al. Correction of congenital severe ptosis by suspension of a frontal muscle flap overlapped with an inferiorly based orbital septum flap. Aesthetic Plast Surg. 2008;32(4):604-612; discussion 613. [DOI] [PubMed] [Google Scholar]
- 12. Hou D, Li G, Fang L, Li B. Frontalis muscle flap suspension for the correction of congenital blepharoptosis in early age children. PLoS One. 2013;8(1):e53185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lai CS, Chang KP, Lee SS, et al. The role of frontalis orbicularis oculi muscle flap for correction of blepharoptosis with poor levator function. Ann Plast Surg. 2013;71(Suppl 1):S29-S36. [DOI] [PubMed] [Google Scholar]
- 14. Knize DM. An anatomically based study of the mechanism of eyebrow ptosis. Plast Reconstr Surg. 1996;97(7):1321-1333. [DOI] [PubMed] [Google Scholar]
- 15. Lai CS. New trend for correction of upper lid ptosis: frontalis orbicularis oculi muscle flap technique. Invited by Dr Hung-Chi Chen, education presentation at E-Da/I-Shou University, Kaohsiung, Taiwan, October 20, 2005. [Google Scholar]
- 16. Lai CS, Chang KP, Lai CH, Huang SH, Tsai CC, Lin SD. A dynamic technique for the treatment of severe or recurrent blepharoptosis: frontalis-orbicularis oculi muscle flap shortening. Ophthalmologica. 2009;223(6):376-382. [DOI] [PubMed] [Google Scholar]
- 17. Lai CS, Lai CH, Huang SH, et al. A new trend for the treatment of blepharoptosis: frontalis-orbicularis oculi muscle flap shortening technique. J Plast Reconstr Aesthet Surg. 2010;63(2):233-239. [DOI] [PubMed] [Google Scholar]
- 18. Song R, Song Y. Treatment of blepharoptosis. Direct transplantation of the frontalis muscle to the upper eyelid. Clin Plast Surg. 1982;9(1):45-48. [PubMed] [Google Scholar]
- 19. Goldey SH, Baylis HI, Goldberg RA, Shorr N. Frontalis muscle flap advancement for correction of blepharoptosis. Ophthalmic Plast Reconstr Surg. 2000;16(2):83-93. [DOI] [PubMed] [Google Scholar]
- 20. Ramirez OM, Peña G. Frontalis muscle advancement: a dynamic structure for the treatment of severe congenital eyelid ptosis. Plast Reconstr Surg. 2004;113(6):1841-1859; discussion 1850. [DOI] [PubMed] [Google Scholar]
- 21. Pereira MV, Glória AL. Lagophthalmos. Semin Ophthalmol. 2010;25(3):72-78. [DOI] [PubMed] [Google Scholar]
- 22. Lai CS, Lai YW, Huang SH, Lee SS, Chang KP, Chen AD. Surgical correction of the intractable blepharoptosis in patients with ocular myasthenia gravis. Ann Plast Surg. 2016;76(Suppl 1):S55-S59. [DOI] [PubMed] [Google Scholar]
- 23. Baik BS, Lee JH, Cho BC. Severe blepharoptosis: correction by orbicularis oculi muscle and orbital septum resection and advancement. Ann Plast Surg. 1998;40(2):114-122. [DOI] [PubMed] [Google Scholar]
- 24. Park DH, Ahn KY, Han DG, Baik BS. Blepharoptosis repair by selective use of superiorly based muscle flaps. Plast Reconstr Surg. 1998;101(3):592-603. [DOI] [PubMed] [Google Scholar]
- 25. Tsai CC, Lin TM, Lai CS, Lin SD. Use of orbicularis oculi muscle flap for undercorrected blepharoptosis with previous frontalis suspension. Br J Plast Surg. 2000;53(6):473-476. [DOI] [PubMed] [Google Scholar]
- 26. Putterman AM. Margin reflex distance (MRD) 1, 2, and 3. Ophthalmic Plast Reconstr Surg. 2012;28(4):308-311. [DOI] [PubMed] [Google Scholar]
- 27. McCord CD, Kreymerman P, Nahai F, Walrath JD. Management of postblepharoplasty chemosis. Aesthet Surg J. 2013;33(5):654-661. [DOI] [PubMed] [Google Scholar]
- 28. Baroody M, Holds JB, Vick VL. Advances in the diagnosis and treatment of ptosis. Curr Opin Ophthalmol. 2005;16(6):351-355. [DOI] [PubMed] [Google Scholar]
- 29. de la Torre JI, Martin SA, De Cordier BC, Al-Hakeem MS, Collawn SS, Vasconez LO. Aesthetic eyelid ptosis correction: a review of technique and cases. Plast Reconstr Surg. 2003;112(2):655-660; discussion 661-652. [DOI] [PubMed] [Google Scholar]
- 30. Wasserman BN, Sprunger DT, Helveston EM. Comparison of materials used in frontalis suspension. Arch Ophthalmol. 2001;119(5):687-691. [DOI] [PubMed] [Google Scholar]
- 31. Ben Simon GJ, Macedo AA, Schwarcz RM, Wang DY, McCann JD, Goldberg RA. Frontalis suspension for upper eyelid ptosis: evaluation of different surgical designs and suture material. Am J Ophthalmol. 2005;140(5):877-885. [DOI] [PubMed] [Google Scholar]
- 32. Wang T, Li X, Wang X, et al. Evaluation of moderate and severe blepharoptosis correction using the interdigitated part of the frontalis muscle and orbicularis oculi muscle suspension technique: a cohort study of 235 cases. J Plast Reconstr Aesthet Surg. 2017;70(5):692-698. [DOI] [PubMed] [Google Scholar]
- 33. Kim CY, Lee SY. Distinct features in Koreans with involutional blepharoptosis. Plast Reconstr Surg. 2015;135(6): 1693-1699. [DOI] [PubMed] [Google Scholar]
- 34. Lai HT, Weng SF, Chang CH, et al. Analysis of levator function and ptosis severity in involutional blepharoptosis. Ann Plast Surg. 2017;78(3 Suppl 2):S58-S60. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.