Abstract
Background
Patients with long-term complications associated with subglandular breast augmentation are being seen in increasing numbers in the Southern California community. Late deformities include a characteristic “slide-down” deformity as well as capsular contracture, implant wrinkling, and nipple-areola complex enlargement. Repositioning the implant to a subpectoral pocket is a recognized revisionary technique to treat this problem; however, technical details of how this is accomplished are lacking in the literature.
Objectives
To review our technique for treating long-term complications associated with subglandular implants using subpectoral repositioning with partial capsule preservation and mastopexy, without the need for an acellular dermal matrix (ADM) or mesh.
Methods
A retrospective review of all patients undergoing subpectoral repositioning over the course of 6 years was performed. Patient data and long-term outcomes were assessed. A technique is presented utilizing a partial capsulectomy that preserves a portion of the capsule as an ADM/mesh equivalent, ensuring adequate implant coverage and preventing window shading of the pectoralis major muscle.
Results
Twenty-four patients with subglandular implants and slide-down deformity as well as other associated complications including capsular contracture, implant wrinkling, and enlarged areolas underwent revision surgery with a subpectoral site change. Often, patients presented many years after their initial augmentation (mean 18 years, range 4-38 years). The average patient follow-up was 3.1 years (range 1.0-6.8 years). Two patients required minor revisions with local anesthetic, while another 2 revisions required general anesthesia.
Conclusions
Long-term deformities associated with subglandular breast augmentation can reliably be corrected by subpectoral repositioning, mastopexy, and utilization of residual breast capsule in the place of an ADM or mesh.
Level of Evidence: 4

Breast augmentation is one of the most common procedures that plastic surgeons perform.1 Some believe that a subglandular approach is appropriate when the upper pole pinch test is greater than 2 cm.2-6 Over the past 2 decades, we have seen an increasing number of long-term complications associated with subglandular breast augmentation in our practice and as reported by many plastic surgeons in various communities including Southern California. These include inferior migration of the implant, implant wrinkling, capsular contracture, enlarged areolas, and breast asymmetry.7 These patients characteristically present with unitary descent of the implant, breast tissue, and inframammary fold (IMF), which we term “slide-down deformity.”
Subglandular to subpectoral site change represents an important tool for dealing with these implant-related complications. This concept, introduced in the mid-1990s by Maxwell, has evolved to include total or partial capsulectomy and, more recently, the use of acellular dermal matrix (ADM) or mesh.8-16 Despite previous reports emphasizing the benefit of a site change from subglandular to submuscular or dual-plane position, there seems to be a paucity of information on how this is performed technically.
We describe a technique for repositioning the implant from the subglandular to subpectoral space wherein a partial capsulectomy is performed preserving the inferior and posterior aspects of the capsule as an ADM equivalent. This approach offers soft tissue coverage at the lower pole of the breast and prevents window shading of the pectoralis major muscle, while avoiding the increased cost and potential complications of an ADM. As part of a comprehensive approach to treating slide-down deformity, a mastopexy is performed concurrently. We report our 6-year experience using this technique to correct long-term deformities associated with initial subglandular implant placement.
METHODS
Written informed consent, including patient consent for photography for educational purposes, was obtained from all patients involved in the study. Institutional Review Board approval was not obtained as the study was retrospective in nature. The study was conducted in a manner consistent with the guiding principles defined by the World Medical Association Declaration of Helsinki. All procedures were performed by the senior author in a private American Association for Accreditation of Ambulatory Surgery Facilities (AAAASF) accredited facility.
Patient Selection and Indications
A retrospective review of all patients who underwent implant site change from a subglandular to subpectoral pocket over the course of nearly 6 years (August 2013-May 2019) was performed. The indications for site change were slide-down implant malposition, excessive nipple-areola complex enlargement, visible or palpable wrinkling, and recurrent capsular contracture.
Preoperative Marking
Before surgery, and with the patient standing, the IMFs and breast meridians are marked. The position of the new nipple-areolar complex is approximated and marked by a blotting technique. Breast size and asymmetries are noted. Standard breast measurements including sternal notch (SN)-to-nipple distance are taken. Particular consideration is given to the nipple-to-IMF distance as a measurement of vertical excess, predicting the length of the horizontal excision that will be needed at the IMF. Finally, the distance from SN-to-IMF is measured. We have found that this nonstandard measurement is crucial in quantifying the extent of the breast mound and IMF descent in patients with slide-down deformity and thus determining the amount of elevation that will be required to restore them to an appropriate position (Figure 1).17,18
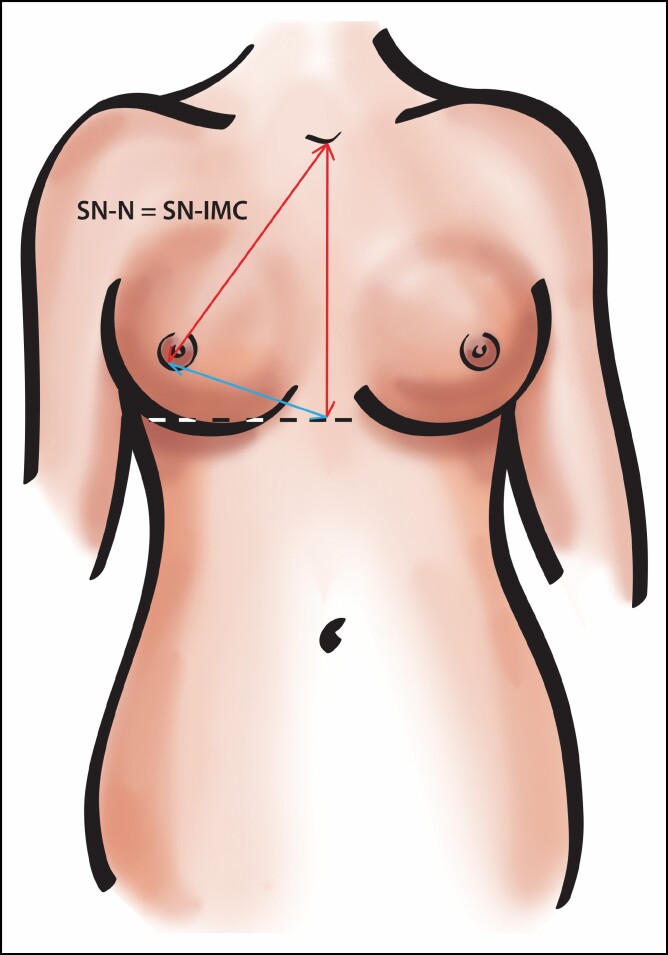
Figure 1.
The sternal notch-to-inframammary fold (IMF) (SN:IMF) distance estimates the necessary amount of elevation of the IMF. In an ideal breast, it should be 21–22 cm and approximately equal to the sternal notch-to-nipple (SN:N) distance.
Surgical Technique
The procedure is performed under general anesthesia with the patient positioned in akimbo. A vertical infra-nipple-areola complex incision is used to approach the breast capsule and remove the subglandular implant. A transverse incision is then made through the posterior breast capsule and muscle 1 to 2 cm superior to the inferior border of the pectoralis major. A subpectoral pocket is developed, into which an implant sizer is placed.
Tailor-tack mastopexies are performed with the patient in an upright seated position.19,20 The proposed mastopexy incisions are marked with ink and the staples removed. With sizers still in place, partial capsulectomies are performed beginning 1–2 cm superior to the access incision in the pectoralis major muscle and carried superiorly to the capsular reflection. Removal of the capsule from the surface of the pectoralis major allows for its expansion and thus better accommodation of the implant. Preservation of the inferior portion of the capsule serves to support the lower pole of the implant, prevents window shading of the pectoralis major muscle, and provides an additional layer of closure (Figure 2). There is no need to jeopardize the blood supply to the breast flaps by removing the anterior capsule. Additionally, IMF discrepancies were quite common based on the gravitational descent of the implant. The new IMF was set by the existing underlying anatomy that, in our series, was much higher on both sides than the preoperative position.
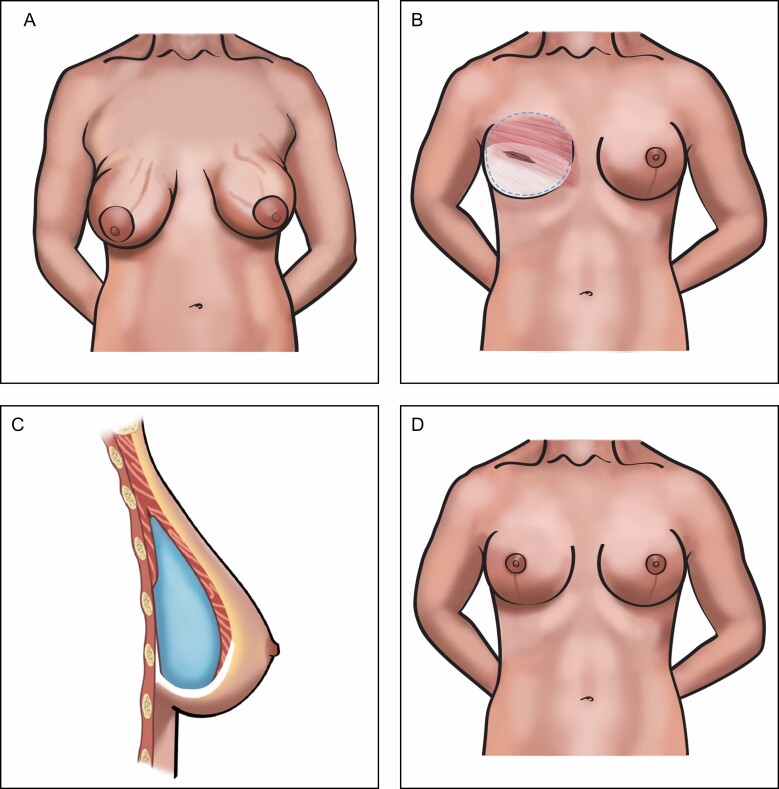
Figure 2.
(A) Slide-down deformity with wrinkling and nipple-areola complex enlargement. (B) Transverse incision made through the capsule above the inferior border of the pectoralis major muscle, allowing the development of a subpectoral pocket. A posterior capsulectomy off the pectoralis major muscle allows for the muscle to expand for the implant. The inferior portion of the capsule (white portion) acts as the auto-acellular dermal matrix (ADM) and serves to support the lower pole of the implant, prevents window shading of the pectoralis major muscle, and provides an additional layer of closure. (C) Saggital view of implant repositioned in a subpectoral pocket. Following limited capsulectomy over the anterior surface of the pectoralis major muscle, the pocket has been closed by reapproximation of the muscle to the inferior capsule. The inferior portion of the breast capsule acts as an ADM equivalent, supporting the implant and preventing window shading of the muscle. (D) Final view following mastopexy.
Standard superior-medial pedicle mastopexies are then completed. Bulkiness of the inferior pole and/or size disparities can be addressed by excising inferior pole breast tissue. Before closing the medial and lateral pillars, a Jackson-Pratt drain is placed on each side. Throughout the procedure, the patient is positioned upright at the completion of every maneuver for each side. This allows evaluation of breast shape and confirmation of symmetry in a step-wise fashion. In a typical case, the patient may be positioned upright 10 or more times (Figures 3 and 4). We prefer the akimbo position because we feel that it decreases tension on the pectoralis muscle compared with having the arms out making submuscular repositioning of the implant easier (Video 1).
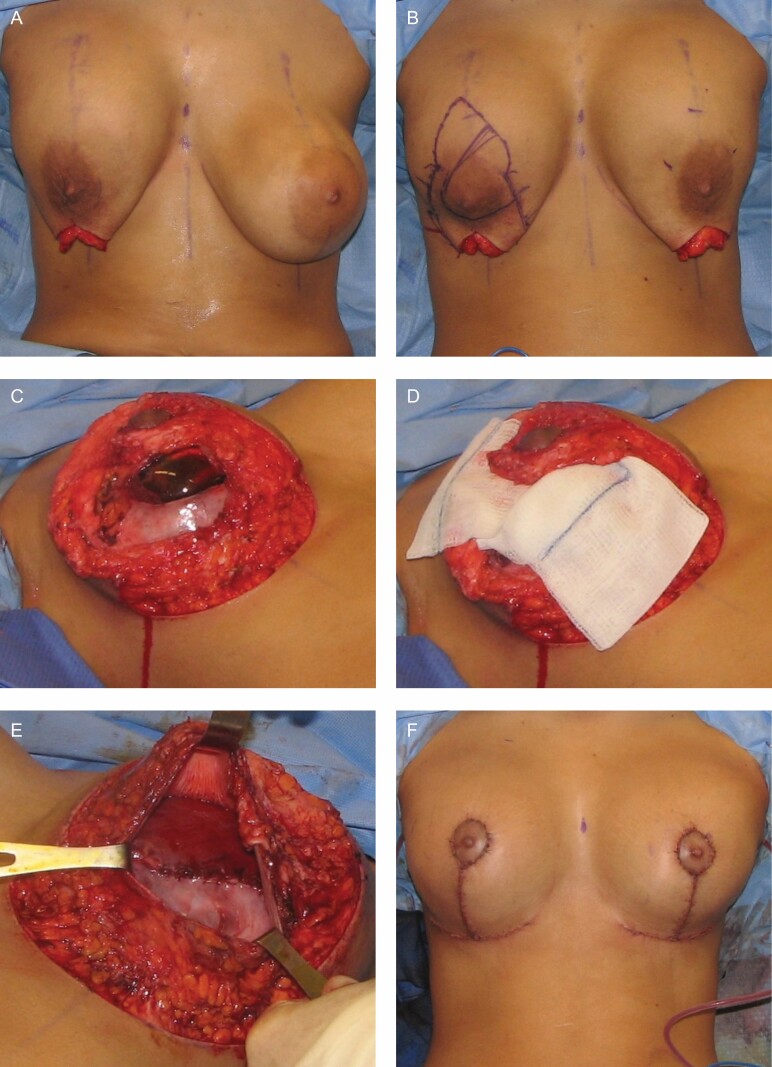
Figure 3.
Operative sequence for a 24-year-old female with a history of subglandular breast augmentation with saline implants. (A) Patient seated upright following sizer repositioning in the subpectoral location. (B) Markings made following tailor-tack mastopexy, including the outline of superior-medial pedicle. (C) Inferior portion of the capsule preserved following limited posterior capsulectomy. (D) Demonstration of superior-medial pedicle with gauze background. (E) Closure of preserved inferior capsule to pectoralis major muscle. (F) Final on-table result in sitting position.
Figure 4.
Operative sequence for a 70-year-old female with a history of subglandular breast augmentation with saline implants. (A, B) Elevation of breast mound following sizer placement in repositioned subpectoral pocket. (C) Tailor-tack mastopexy with demonstration of inframammary fold (IMF) elevation and redundancy of inferior pole breast tissue. (D) Final on-table result in sitting position. This figure has been reprinted from portions of a previously published figure from the study of Chasan with permission from Springer Nature © 2017 under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/).21
Postoperative Care
Postoperatively, the patient is placed in a standard compressive breast dressing, which is changed to an athletic brassiere on the first postoperative day. The drain is typically removed between postoperative days 3 and 5. The remainder of the postoperative care is similar to a standard augmentation-mastopexy.
RESULTS
Between August 2013 and May 2019, 24 patients underwent revisionary breast augmentation requiring implant site change from a subglandular to subpectoral position utilizing the described technique (Figures 5-7). The average patient age was 50 years (range 36-70 years). The average length of time from original surgery was 18 years (range 4-38 years). Of the previous operations performed prior to site change, 71% (n = 17) had augmentation alone, while 29% (n = 7) had undergone previous augmentation-mastopexy. Significant capsular contracture (≥ Grade 3) was present in 46% (n = 11) of the patients.
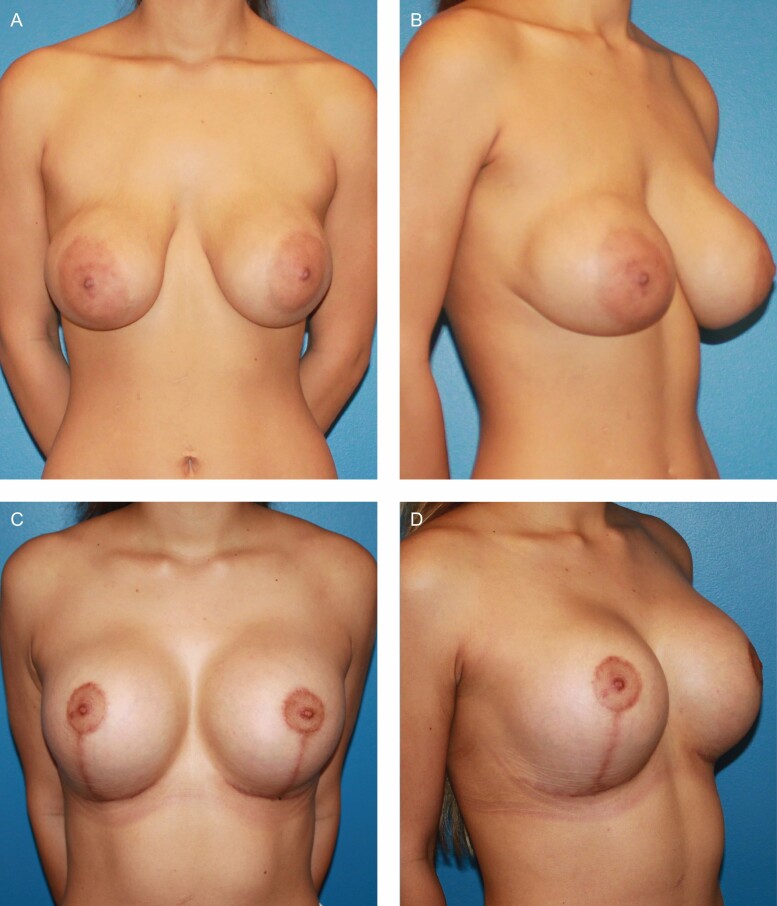
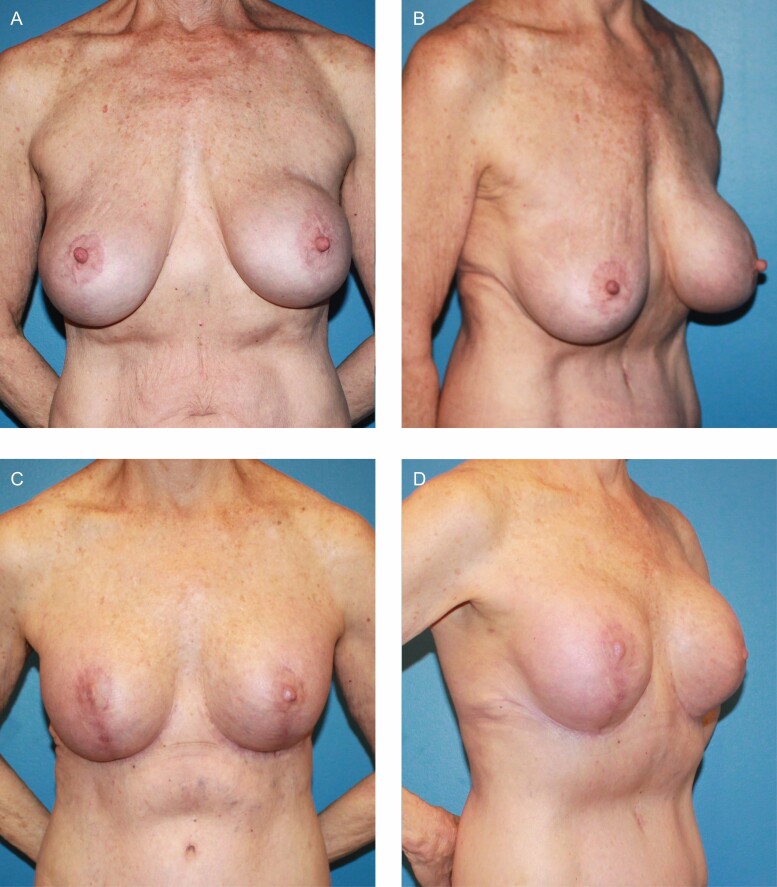
Figure 5.
Patient corresponding to operative sequence detailed in Figure 3. (A, B) Preoperative views of a 24-year-old female with a history of subglandular breast augmentation 4 years prior, with saline implants filled to 525 cc bilaterally. Sternal notch-to-inframammary fold (SN:IMF) distance measuring 26 cm. (C, D) One-year postoperative views following subpectoral repositioning with implant exchange to 600 cc ultra-high profile silicone implants and short-scar mastopexy.
Figure 7.
(A, B) Preoperative views of a 41-year-old female with Grade 3 capsular contracture and a history of subglandular breast augmentation 15 years prior, with saline implants filled to 300 cc bilaterally. Sternal notch-to-inframammary fold (SN:IMF) distance measuring 23 cm. (C, D) Two-year postoperative views following subpectoral repositioning and exchange for 350 cc high profile silicone implants with short-scar mastopexy.
Figure 6.
Patient corresponding to operative sequence detailed in Figure 4. (A, B) Preoperative views of a 70-year-old female with Grade 3 capsular contracture and a history of subglandular breast augmentation 30 years prior with saline implants filled to 275 cc on the right and 450 cc on the left. Preoperative views demonstrate slide-down deformity with sternal notch-to-inframammary fold (SN:IMF) distance measuring 28 cm. (C, D) One-year postoperative views following subpectoral repositioning with exchange to high profile silicone implants (325 cc on the right and 345 cc on the left), excision of inferior pole breast tissue (230 g from the right and 155 g from the left), and full mastopexy with IMF elevation. Figure portions 6A and 6C have been reprinted from portions of a previously published figure from the study of Chasan with permission from Springer Nature © 2017 under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0/).21
Preoperative breast measurements demonstrated an average SN-to-nipple distance of 24 cm (range 20-29 cm) and an average SN-to-IMF distance of 25 cm (range 24-28 cm).
Following implant removal, 13% (n = 3) of patients were found to have ruptured implants, with 8% (n = 2) of patients having gross calcification of the implant capsule. Near-total capsulectomies were performed in 17% (n = 4) of patients bilaterally and unilaterally in 8% (n = 2) of patients, due to either calcification or severe capsular contracture. Average tissue resection per breast was 48 g (range 0-175 g) and 25% (n = 6) of the patients required significant resection of breast tissue of greater than 100 g per breast. The range of implant volumes placed was from 240 to 520 cc. Only smooth round silicone implants were used. Reasons for revisions were mixed with a slight majority being for upsizing.
The average patient follow-up was 3.1 years (range 1.0-6.8 years). There were no instances of nipple-areolar complex necrosis. No capsular contractures were observed postoperatively. Eight percent (n = 2) of the patients required minor revision performed under local anesthesia. An additional 8% (n = 2) underwent revision requiring general anesthesia, one to correct implant malposition and the other for exchange to larger implants.
DISCUSSION
Previously reported algorithms have suggested that placement of implants in the subglandular plane is permissible when soft tissue pinch thickness of the upper pole is sufficient.2-6 This “upper pole pinch test” offers a potentially valid prediction as to the likelihood of wrinkling following the placement of subglandular implants. Its use as the primary determinant for subglandular augmentation, however, neglects the long-term effect a subglandular implant has on the lower pole of the breast. Although not previously described in the literature, we have observed in our practice and through discussions with plastic surgeons in the Southern California community that over time these implants slide down the chest wall, leading to the descent of the implant, breast tissue, and IMF as a unit. The IMF itself is a coalescence of thickened tissue from the skin and subcutaneous tissues to the periosteum. Implant placement in the subglandular space with subsequent descent will stretch and disrupt the integrity of the IMF; however, the tissues deep to the surgical plane remain intact as residual IMF. We term this “slide-down deformity” to distinguish it from “waterfall deformity,” in which relative descent of the breast tissue occurs over a stable implant, and from pseudoptosis/bottoming-out, in which implant and breast tissue descent occurs over a relatively stable IMF.7,22
Since IMF descent is not a hallmark of waterfall deformity or pseudoptosis, the key measurement defining slide-down deformity is, therefore, the SN-to-IMF distance, which will be longer than normal. We routinely collect this data point and have observed that in an ideal breast it is 21–22 cm and approximately equal to the SN-to-nipple distance. Three-dimensionally, the anterior projection of the nipple relative to the chest wall adds length to the SN-to-nipple distance, while the SN-to-IMF distance is essentially vertical in the frontal plane. We have noticed in our technique that once the implant has been placed and the implant pocket elevated, the degree of descent of nipple-areolar complex and IMF becomes apparent. Depending on the extent of slide-down deformity, substantial elevation of each may be required in the subsequent mastopexy design. The ideal breast in a non-augmented patient has a ratio of 45:55—upper breast pole to lower pole ratio as published by Mallucci and Branford in 2015.23 We have found, however, that the ideal augmented breast has a reverse ratio of 55:45. With the slide-down deformity, we often see this ratio excessively out of balance up to 25:75. The procedure we described restores this balance.
Other long-term complications we have commonly encountered with subglandular implants include implant wrinkling, capsular contracture, and nipple-areola complex enlargement.7,22 Frequently, these occur in combination, resulting in a particularly dissatisfying appearance as subjectively reported by the senior surgeon and his patients (Figure 2). Overall, it would seem that there is a subset of patients undergoing subglandular breast augmentation with acceptable short-term results who go on to display a distinct constellation of deformities in the long term.
We propose that these late complications suggest the inadequacy of the upper pole pinch test in assessing the long-term consequences of subglandular breast augmentation. Rather, slide down results from the disruption of the posterior breast tissue attachments to the pectoralis major muscle, leading to the uninterrupted gravitational pull on the implant/capsule and breast tissue. The accompanying attenuation of inferior pole tissue and skin stretching seem to result in thinning of the skin, wrinkling, and nipple-areola complex enlargement.
Revisionary breast surgery that reproducibly corrects these late complications of subglandular breast augmentation requires an additional set of techniques that is distinct from other aesthetic breast surgery. A variety of recommendations have been described for the management of implant malposition and capsular contracture following breast augmentation. There is evidence supporting the efficacy of subpectoral site change when subglandular breast augmentation is complicated by capsular contracture.10,22
Several previous studies have described the use of a capsular flap to create a sling of vascularized tissue to reinforce capsulorrhaphy and correct implant malposition.24-27 However, they do not use the capsular flap in conjunction with implant site change. The largest of the studies, by Wessels et al, employed the technique in 12 patients with inferior malposition and demonstrated a stable position of the IMF at 40.4 months follow-up.27 Capsular flaps involve disrupting the native conformation of the capsule as well as the blood supply. Others have found their reliability to be inconsistent, which we have also observed anecdotally.16 The durability of capsular tissue without its structural continuity or full-thickness soft tissue attachments is questionable. A key advantage of capsule preservation, as we describe, is that the structural integrity of the inferior capsule is undisturbed and that most of its soft tissue attachments are left intact.
In a 2012 review of the use of ADMs in revisionary breast augmentation, Kaufman mentions that during subglandular repositioning to the submuscular pocket it is often necessary to use the inferior capsule to extend the reach of the pectoralis muscle and provide additional implant coverage.16 However, he does not elaborate on technical details or outcomes. He does criticize capsular flaps as being inconsistent in quality and quantity, ultimately advocating for the use of ADMs with the caution that they are a source for potential complications.16
Proponents for the use of ADMs in this context assert that they effectively reinforce inferior capsulorrhaphy, reduce tension on the suture line, define the IMF, and maintain proper implant position in a neopocket.13-16 Their expense, however, is an important consideration, particularly for a patient paying out of pocket. Additionally, data are limited regarding recurrence rates with these matrices when used for capsular contracture and implant malposition.14,16 In our experience with subpectoral implant repositioning, we have found that ADMs and mesh are unnecessary when the inferior portion of the subglandular capsule is preserved. In addition to cost savings, avoiding the placement of a foreign body also has implications with respect to potential complications and surgical expediency.
In some cases, such as calcified capsule and severe capsular contracture, more extensive capsulectomies including both anterior and posterior capsules may be required. Whenever possible, it is important to preserve the inferior aspect of the capsule to prevent pectoralis major window shading and provide lower pole support. However, if complete capsulectomy is required, the use of ADM or mesh (which were never needed in this series) can still be avoided by elevating the inferior insertion of the pectoralis major along with the superior aspect of the rectus abdominis fascia off the ribs to support the lower pole.
Finally, over the course of this series, there were no instances of nipple-areolar complex necrosis. This can be attributed to minimizing dissection under the nipple-areolar complex and leaving the anterior capsule under the pedicle intact, whenever possible. (Figure 2).
There are several limitations and shortcomings to our study. Admittedly, this is a retrospective review of a single surgeon’s experience with subglandular implant repositioning to a subpectoral pocket combined with mastopexy and utilization of the residual breast capsule for support in the place of an ADM or mesh. Additionally, objective measurements or a validated subjective aesthetic scoring system were not employed in this study. Exploring long-term results using such scoring systems is certainly warranted by future studies.
Although the procedure has been previously described, the technical details associated with implant repositioning are extremely limited in the literature. Treating long-term complications associated with subglandular implants using subpectoral repositioning with partial capsule preservation and mastopexy without the need for an ADM or mesh is a uniquely described technique that we hope can be replicated by surgeons elsewhere.
CONCLUSIONS
Revision surgery addressing the long-term consequences of subglandular breast augmentation can be challenging. The technique of subpectoral repositioning utilizing residual breast capsule as an ADM equivalent, along with mastopexy, is an effective, 1-stage method for correction of slide-down deformity and other associated complications. In the hands of an experienced revisionary breast surgeon, it can reliably produce an aesthetically pleasing breast position and shape.
Acknowledgment
We would like to thank Jim McConlogue for his help with creating the illustrations for this paper (Figures 1 and 2).
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
- 1.The Aesthetic Society’s Cosmetic Surgery National Data Bank: Statistics 2019. Aesthet Surg J. 2020;40 (Supplement_1): 1-26. [DOI] [PubMed] [Google Scholar]
- 2.Tebbetts JB. A system for breast implant selection based on patient tissue characteristics and implant-soft tissue dynamics. Plast Reconstr Surg. 2002;109(4):1396-1409; discussion 1410. [DOI] [PubMed] [Google Scholar]
- 3.Tebbetts JB, Adams WP. Five critical decisions in breast augmentation using five measurements in 5 minutes: the high five decision support process. Plast Reconstr Surg. 2005;116(7):2005-2016. [PubMed] [Google Scholar]
- 4.Adams WP Jr, Spear SL. Augmentation mammaplasty. Plast Reconstr Surg. 2006;118(7):5S-6S. [DOI] [PubMed] [Google Scholar]
- 5.Adams WP. The high five process: tissue-based planning for breast augmentation. Plast Surg Nurs. 2007;27(4):197-201. [DOI] [PubMed] [Google Scholar]
- 6.Adams WP Jr. The process of breast augmentation: four sequential steps for optimizing outcomes for patients. Plast Reconstr Surg. 2008;122(6):1892-1900. [DOI] [PubMed] [Google Scholar]
- 7.Handel N. Managing complications of augmentation mammaplasty. In: Spear SL, Willey SC, Robb GL, Hammond DC, Nahabedian MY, eds. Surgery of the Breast: Principles and Art. 2nd ed. Philadelphia, PA: Lippincott-Raven Publishers; 2006:1417-1435. [Google Scholar]
- 8.Maxwell GP, Tebbetts JB, Hester TR. Site change in breast surgery. Paper presented at the American Association of Plastic Surgeons, May 1994, St Louis, MO. [Google Scholar]
- 9.Spear SL, Carter ME, Ganz JC. The correction of capsular contracture by conversion to “dual-plane” positioning: technique and outcomes. Plast Reconstr Surg. 2003;112(2):456-466. [DOI] [PubMed] [Google Scholar]
- 10.Wan D, Rohrich RJ. Revisiting the management of capsular contracture in breast augmentation: a systematic review. Plast Reconstr Surg. 2016;137(3):826-841. [DOI] [PubMed] [Google Scholar]
- 11.Maxwell GP, Gabriel A. The neopectoral pocket in revisionary breast surgery. Aesthet Surg J. 2008;28(4):463-467. [DOI] [PubMed] [Google Scholar]
- 12.Maxwell GP, Birchenough SA, Gabriel A. Efficacy of neopectoral pocket in revisionary breast surgery. Aesthet Surg J. 2009;29(5):379-385. [DOI] [PubMed] [Google Scholar]
- 13.Maxwell GP, Gabriel A. Revisionary breast surgery with acellular dermal matrices. Aesthet Surg J. 2011;31(6):700-710. [DOI] [PubMed] [Google Scholar]
- 14.Maxwell GP, Gabriel A. Acellular dermal matrix for reoperative breast augmentation. Plast Reconstr Surg. 2014;134(5):932-938. [DOI] [PubMed] [Google Scholar]
- 15.Spear SL, Seruya M, Clemens MW, Teitelbaum S, Nahabedian MY. Acellular dermal matrix for the treatment and prevention of implant-associated breast deformities. Plast Reconstr Surg. 2011;127(3):1047-1058. [DOI] [PubMed] [Google Scholar]
- 16.Kaufman D. Pocket reinforcement using acellular dermal matrices in revisionary breast augmentation. Clin Plast Surg. 2012;39(2):137-148. [DOI] [PubMed] [Google Scholar]
- 17.Isaac KV, Murphy BD, Beber B, Brown M. The reliability of anthropometric measurements used preoperatively in aesthetic breast surgery. Aesthet Surg J. 2016;36(4):431-437. [DOI] [PubMed] [Google Scholar]
- 18.Atiye B, Chahine F. Metrics of the aesthetically perfect breast. Aesthetic Plast Surg. 2018;42(5):1187-1194. [DOI] [PubMed] [Google Scholar]
- 19.Brown RW, Cheng YC, Kurtay M. A formula for surgical modifications of the breast. Plast Reconstr Surg. 2000;106(6):1342-1345. [DOI] [PubMed] [Google Scholar]
- 20.Whidden PG. The tailor-tack mastopexy. Plast Reconstr Surg. 1978;62(3):347-354. [DOI] [PubMed] [Google Scholar]
- 21.Chasan PE. Reductive augmentation of the breast. Aesthetic Plast Surg. 2018;42(3):662-671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chopra K, Gowda AU, Kwon E, Eagan M, Grant Stevens W. Techniques to repair implant malposition after breast augmentation: a review. Aesthet Surg J. 2016;36(6):660-671. [DOI] [PubMed] [Google Scholar]
- 23.Mallucci P, Branford OA. Shapes, proportions, and variations in breast aesthetic ideals: the definition of breast beauty, analysis, and surgical practice. Clin Plast Surg. 2015;42(4):451-464. [DOI] [PubMed] [Google Scholar]
- 24.Voice SD, Carlsen LN. Using a capsular flap to correct breast implant malposition. Aesthet Surg J. 2001;21(5):441-444. [DOI] [PubMed] [Google Scholar]
- 25.Yoo G, Lee PK. Capsular flaps for the management of malpositioned implants after augmentation mammoplasty. Aesthetic Plast Surg. 2010;34(1):111-115. [DOI] [PubMed] [Google Scholar]
- 26.de Benito J, Sanchez K. Secondary breast augmentation: managing each case. Aesthetic Plast Surg. 2010;34(6):691-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wessels L, Murphy S, Merten S. The capsular hammock flap for correction of breast implant ptosis. Aesthetic Plast Surg. 2014;38(2):354-357. [DOI] [PubMed] [Google Scholar]