Abstract
Background
With the current opioid crisis in the United States, infectious complications related to injection drug use are increasingly reported. Pennsylvania is at the epicenter of the opioid crisis, with the third highest rate of drug overdose deaths in the United States.
Methods
A retrospective cohort study was performed using the Pennsylvania Health Care Cost Containment Council database of all residents hospitalized for infective endocarditis (IE) in an acute care hospital from 1 January 2013 through 31 March 2017. Patients were separated into those with and those without substance use via diagnosis codes. The primary outcome was length of stay. Secondarily, we evaluated demographics, infection history, hospital charges, and insurance status.
Results
Of the 17 224 hospitalizations, 1921 (11.1%) were in patients with drug use–associated IE (DU-IE). Total quarterly IE admissions increased 20%, with a 6.5% increase in non–drug use–associated IE (non-DU-IE) admissions and a 238% increase in DU-IE admissions. In adjusted models, DU-IE was not associated with significant changes in length of stay (incidence rate ratio, 1.02; 95% confidence interval, .975–1.072; P = .36). Patients with DU-IE were predominantly insured by Medicaid (68.3% vs 13.4% for non-DU-IE), they had higher hospital charges ($86 622 vs $66 802), and they were more likely to leave against medical advice (15.7% vs 1.1%) (all P < .001).
Conclusions
Our study demonstrates an increase in IE admissions, driven by an increase in admissions for DU-IE. The higher charges, proportion of patients on Medicaid, and rates of leaving against medical advice among the DU-IE group shows the downstream effects of the opioid crisis.
Keywords: Endocarditis, Opioid epidemic, injection drug use
A retrospective cohort study of Pennsylvania infective endocarditis (IE) admissions showed a 20% increase in IE and a 238% increase in drug use–associated IE admissions, the latter with higher charges, longer stays, and a larger proportion insured through Medicaid.
The United States is currently in the midst of a national opioid crisis. Drug overdose is now the leading cause of injury death, surpassing human immunodeficiency virus (HIV) at the height of the HIV epidemic. The Centers for Disease Control and Prevention has reported a 9.6% increase in overdose deaths from 2016 to 2017, with 47 600 overdose deaths in the United States attributed to opioids [1]. Pennsylvania has been among the most affected states, with the third-highest age-adjusted overdose death rate (44.3 per 100 000) and the most overdose deaths overall (n = 5388) in 2017 [2]. The cities of Pittsburgh and Philadelphia have some of the highest overdose death rates of all cities in the United States [3].
Overdose deaths are just the tip of the iceberg of the opioid crisis affecting health systems and societies. In addition to overdose deaths, in Pennsylvania the number of opioid-related hospitalizations increased 103.6% between 2008 and 2015. Of the 36 712 opioid-related hospitalizations during this period, 83% involved patients admitted for other conditions such as mental health disorders and infections [4].
Infectious complications of opioid use disorder (OUD) and injection drug use are among the major downstream consequences of the opioid crisis [5]. Infective endocarditis (IE) is one such complication and requires prolonged intravenous antibiotics and hospitalizations for treatment and, in some cases, valve replacement surgery. Hospitalizations for drug use–associated IE (DU-IE) have increased in recent years [6–8]. Prior work in North Carolina showed that patients hospitalized with DU-IE had an extended length of stay (LOS), higher rates of leaving against medical advice, and higher spending on hospital-based care [7, 9]. In the current study, we examined IE trends in Pennsylvania, a state with high OUD prevalence, and evaluated for differences in hospitalization episodes, including LOS and disposition between those with and without opioid use disorder. We secondarily focused in on 2 urban areas in Pennsylvania with high OUD prevalence, namely Philadelphia and Pittsburgh (Alleghany County).
METHODS
Data Source
Data were obtained from the Pennsylvania Health Care Cost Containment Council (PHC4) database. The PHC4 collects data from all inpatient hospital admissions and ambulatory/outpatient procedure records from all hospitals and ambulatory surgery centers in the state. The data include both treatment information and financial data [10].
Study Population and Study Design
We conducted a retrospective cohort study. The study population consisted of all adult Pennsylvania residents hospitalized for IE from 1 January 2013 through 31 March 2017 in an acute care hospital.
Admissions were identified using International Classification of Diseases (ICD) codes (Ninth Revision [ICD-9] and Tenth Revision [ICD-10]) for IE. The ICD codes used for this purpose were determined by (1) using ICD-9/ICD-10 codes described in prior literature identifying IE and (2) direct examination of the ICD codes for additional ICD codes related to IE [11, 12]. We separated this cohort of patients with IE into 2 groups: those with DU-IE and those with non–drug use–associated IE (non-DU-IE). DU-IE was identified using diagnosis codes indicating drug use (including the use of all opioids, cocaine, and stimulants), overdose, dependence, poisoning, or withdrawal, while excluding marijuana and alcohol use (Supplementary Table 1). All IE hospitalizations that did not have any of the above diagnosis codes was categorized as non-DU-IE.
We performed a secondary analysis on patients admitted in either Philadelphia or Alleghany counties, because they are the 2 regions in Pennsylvania with the highest opioid use rates in the United States. To test the validity of the database, we compared the number of IE admissions at our academic institution identified by the PHC4 with the number captured in a prior record review study completed at our institution [13].
The primary outcome was LOS. Secondary outcomes included (1) hospital charges, (2) discharge disposition (eg, leaving against medical advice), (3) and need for valve replacement surgery.
We collected baseline information on all subjects, including demographics (age, race, ethnicity, sex, and health insurance status) and coinfection history (HIV and hepatitis C virus [HCV] status) and healthcare use (LOS, disposition location, total hospital charges, and later valve replacement surgery). We also collected data on medical factors that increase a person’s risk for IE: congenital heart disease, coronary artery disease, liver disease, pacemaker, prior prosthetic valve, and recent home infusions with a central venous catheter for all subjects.
Analysis
Baseline characteristics were compared between the DU-IE and non-DU-IE groups using Student t or Wilcoxon rank sum tests for continuous variables, and χ 2 or Fisher exact test for categorical variables. For the county-level analysis, we also used Kruskal-Wallis tests.
For the adjusted analysis of LOS, we performed a multivariable negative binomial regression. We chose LOS for the model because LOS has previously been reported as longer in patients with DU-IE [7]. We wanted to determine whether drug use was actually associated with longer length of stay, when other factors were adjusted for. Candidates for the multivariable model included baseline factors with a P value <.20 on bivariable analysis, and those that were confounders of the relationship between OUD status and outcome (defined by a ≥15% change in the effect estimate of the association between DU-IE and LOS). The final model included the primary exposure (DU-IE), confounders, and covariates with a P value ≤.05. The strength of associations was measured based on incidence rate ratios and 95% confidence intervals.
Finally, we calculated the incidence rate for the last year period by using the admissions from the last 4 quarters in our data set and the 2017 population estimates for adults aged ≥18 years from the American Community Survey by the United States Census [14]. Analyses were performed using Stata software, version 15.0 (StataCorp). The study was reviewed by the Institutional Review Board at the University of Pennsylvania and was deemed exempt.
RESULTS
Overall Trends in IE in Pennsylvania During the Opioid Epidemic
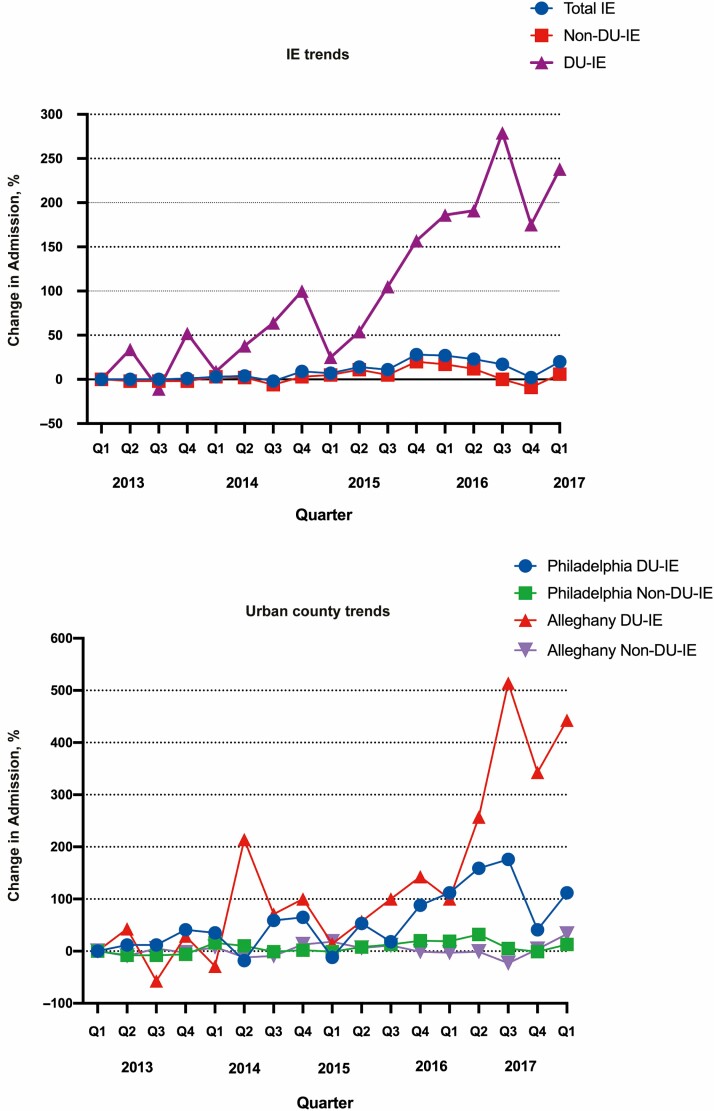
Between 1 January 2013 and 31 March 2017, there were 17 224 acute care hospitalizations for IE in Pennsylvania. Of those admissions, 15 303 (88.9%) were non-DU-IE and 1921 (11.1%) were DU-IE. Total quarterly IE admissions increased from 923 during the first quarter of 2013 to 1112 during the first quarter of 2017, representing a 20% increase, with a 6.5% increase in non-DU-IE admissions (from 867 to 923) and a 238% increase in DU-IE admissions (from 56 to 189) during that period. Comparing the first quarter of the study to the final quarter of the study, the proportion of overall IE admissions for DU-IE increased from 6.1% to 17% (Figure 1A and Supplementary Figure 1A). The incidence rate in the last year of our data was 42.3 per 100 000 persons for all endocarditis in Pennsylvania. The DU-IE group had an incidence of 7.1 per 100 000 persons and the non-DU-IE group, 35.2 per 100 000 persons.
Figure 1.
Percentage change in all Pennsylvania (A) and Pennsylvania urban county (B) infectious endocarditis (IE) admissions over time. Abbreviations: DU-IE, drug use–associated IE; non-DU-IE, non–drug use–associated IE.
Characteristics of Pennsylvania’s DU-IE Population
Patients admitted with DU-IE were younger than those admitted with non-DU-IE (median age [interquartile range (IQR)], 33 [27–45] vs 69 [56–80] years, respectively; P < .001). The predominant race was white in both groups, though there were slightly more white patients in the non-DU-IE than in the DU-IE group (83.3% vs 81.9%; P < .001). Primary insurance status differed significantly between the groups: patients with non-DU-IE were most commonly insured by Medicare (65.5%) or commercial insurance (19%); only 13.4% were insured by Medicaid, and 0.9% were uninsured. Patients with DU-IE were most commonly covered by Medicaid (68.3%) or commercial insurance (15.1%), only 11.4% were on Medicare (11.4%), and 2.4% were uninsured (P < .001). They were more likely than those with non-DU-IE to have infectious comorbid conditions (HIV, 2.4% vs 0.7%, respectively; HCV, 27.1% vs 3.3%) (P < .001). Both groups had comparable proportions of patients with predisposing medical conditions, except that preexisting prosthetic valves were seen more commonly in the non-DU-IE than in the DU-IE population (7.5% vs 5.5%, respectively; P = .02) (Table 1).
Table 1.
Demographic Characteristics of Patients Admitted for Infective Endocarditis in Pennsylvania
| Patients, No. (%)a | |||
|---|---|---|---|
| Characteristic | Non-DU-IE (n = 15 303) | DU-IE (n = 1921) | P Value |
| Age, median (IQR), y | 69 (56–80) | 33 (27–45) | <.001 |
| Female sex | 6737 (44) | 909 (47.3) | <.001 |
| Race | |||
| White | 12 747 (83.3) | 1573 (81.9) | |
| Black | 1780 (11.6) | 180 (9.4) | |
| Asian | 101 (0.7) | 2 (0.1) | |
| American Indian | 12 (0.08) | 0 (0) | <.001 |
| Biracial | 12 (0.08) | 4 (0.2) | |
| Other | 243 (1.6) | 87 (4.5) | |
| Unknown | 236 (1.5) | 75 (3.9) | |
| Ethnicity | |||
| Hispanic | 280 (1.8) | 97 (5.05) | <.001 |
| Non-Hispanic | 15 016 (98.2) | 1824 (95) | |
| Insurance | |||
| Medicare | 10 020 (65.5) | 218 (11.4) | |
| Medicaid | 2043 (13.4) | 1312 (68.3) | |
| Commercial | 2898 (19) | 290 (15.1) | <.001 |
| Unknown | 72 (0.47) | 12 (0.6) | |
| Uninsured | 143 (0.9) | 70 (3.7) | |
| HIV positive | 114 (0.7) | 46 (2.4) | <.001 |
| HCV seropositive | 503 (3.3) | 521 (27.1) | <.001 |
| Congenital heart disease | 1994 (13) | 237 (12.3) | .39 |
| Hypertension | 2740 (18) | 83 (4.32) | <.001 |
| Coronary artery disease | 10 947 (71.5) | 1486 (77.4) | <.001 |
| Prosthetic valve | 1140 (7.5) | 105 (5.5) | .02 |
| Pacemaker | 21 (0.14) | 0 (0) | .10 |
Abbreviations: DU-IE, drug use–associated infective endocarditis; HCV, hepatitis C virus; HIV, human immunodeficiency virus; IQR, interquartile range; non-DU-IE, non–drug use–associated infective endocarditis.
aData represent no. (%) of patients unless otherwise specified.
Discharge Disposition
Discharge dispositions differed significantly between the 2 groups, with more patients in the non-DU-IE group going to a facility (43.5% vs 38.8% for DU-IE) or home with services (21.2% vs 8.8%). Those in the DU-IE group were more frequently discharged to home without services (28% vs 20.2%, respectively) and more frequently left the hospital against medical advice (15.7% vs 1.1%).
Hospital Charges
Median [IQR] hospital charges were higher in the DU-IE than in the non-DU-IE group ($86 622 [$37 894–$210 258] vs $66 802 [$30 880–$162 498], respectively; P < .001) (Table 2).
Table 2.
Hospital Use Outcomes for Infective Endocarditis Admissions
| Patients, No. (%)a | |||
|---|---|---|---|
| Outcomes | Non-DU-IE (n = 15 303) | DU-IE ( n = 1921) | P Value |
| LOS, median (IQR), d | 7 (4–13) | 10 (4–21) | <.001 |
| Charges, median (IQR), $ | 66 802 (30 880–162 498) | 86 622 (37 894–210 258) | <.001 |
| Discharge status | |||
| In-hospital death | 1307 (8.5) | 87 (4.5) | |
| SNF/post-acute care facilities | 6659 (43.5) | 744 (38.8) | <.001 |
| Home with services | 3237 (21.2) | 168 (8.8) | |
| Home | 3094 (20.2) | 518 (27) | |
| AMA | 162 (1.1) | 302 (15.7) | |
| Valve replacement | 1255 (8.2) | 217 (11.3) | <.001 |
| Multiple valve | 854 (68) | 117 (53.9) | .36 |
| Tricuspid | 65 (5.2) | 66 (30.4) | <.001 |
| Pulmonic | 18 (1.4) | 3 (1.4) | .65 |
| Mitral | 670 (53.4) | 78 (35.9) | .52 |
| Aortic | 602 (48) | 86 (39.6) | .25 |
| Unspecified | 825 (68) | 112 (51.6) | .42 |
Abbreviations: AMA, against medical advice; DU-IE, drug use–associated infective endocarditis; IQR, interquartile range; LOS, length of stay; non-DU-IE, non–drug use–associated infective endocarditis; SNF, skilled nursing facility.
aData represent no. (%) of patients unless otherwise specified.
Valve Replacement Surgery
Valve surgery was more common in the DU-IE population (11.3% vs 8.2% for non-DU-IE; P < .001). The distribution of valve procedures differed between groups: more patients in the non-DU-IE group had multiple valves replaced, although this difference was not statistically significant (68% vs 53.9% for DU-IE; P = .36). Patients with DU-IE had significantly more tricuspid valve replacements (30.4% vs 5.2% for non-DU-IE; P < .001) (Table 2).
Mortality
The in-hospital mortality rate was lower in the DU-IE group (4.5% vs 8.5% for non-DU-IE; P < .001).
Comparison of DU-IE Populations for Philadelphia and Allegheny Counties
When Philadelphia and Allegheny counties were analyzed separately and compared with the rest of Pennsylvania, we found significant difference between the 2 counties. We found an even larger increase in the proportion of IE cases associated with drug use during the study period: there was a 112% increase in DU-IE admissions in Philadelphia County, and a 443% increase in Allegheny County Figure 1B). Philadelphia and Allegheny counties both had higher incidence rates, with 12.3 and 13.8 per 100 000 persons, respectively, compared with 5.5 per 100 000 persons in the nonurban counties. The racial composition of patients admitted for DU-IE differed between counties: 65.2% white and 19.3% black in Philadelphia vs 84.5% white and 13.4% black in Allegheny (P < .001). Philadelphia had a higher proportion of Medicaid patients than Allegheny County (83.2% vs 65.7% respectively; P < .001) and higher rates of HIV and HCV seropositive status than Allegheny County (P = .01 and P = .006, respectively) and the overall state (both P < .001) (Table 3 and Supplementary Figure 1B).
Table 3.
Demographic Characteristics of Patients Admitted for Drug Use–Associated Infective Endocarditis in Pennsylvania Urban and Other Counties
| Patients, No. (%)a | |||||
|---|---|---|---|---|---|
| Characteristic | Philadelphia (n = 451) | Allegheny County (n = 283) | P Value | Patients in Other Counties, No. (%)a (n = 1187) | P Value |
| Age, median (IQR), y | 34 (29–47) | 34 (20–46) | .53 | 33 (27–43) | <.001 |
| Female sex | 206 (45.7) | 158 (55.8) | .007 | 545 (45.9) | .008 |
| Race | <.001 | <.001 | |||
| White | 294 (65.2) | 239 (84.5) | 1040 (87.62) | ||
| Black | 87 (19.3) | 38 (13.4) | 55 (4.63) | ||
| Asian | 0 (0) | 1 (0.35) | 1 (0.08) | ||
| American Indian | 0 (0) | 0 (0) | 0 (0) | ||
| Biracial | 0 (0) | 0 (0) | 4 (0.34) | ||
| Other | 52 (11.5) | 0 (0) | 35 (2.95) | ||
| Unknown | 18 (4) | 5 (1.8) | 52 (4.38) | ||
| Ethnicity | <.001 | <.001 | |||
| Hispanic | 34 (7.5) | 0 (0) | 63 (5.31) | ||
| Non-Hispanic | 417 (92.5) | 283 (100) | 1124 (94.7) | ||
| Insurance | <.001 | <.001 | |||
| Medicare | 46 (10.2) | 39 (13.8) | 133 (11.2) | ||
| Medicaid | 375 (83.2) | 186 (65.7) | 751 (63.3) | ||
| Commercial | 18 (4) | 38 (13.4) | 234 (19.7) | ||
| Unknown | 1 (0.2) | 2 (0.7) | 9 (0.8) | ||
| Uninsured | 10 (2.2) | 18 (6.4) | 42 (3.5) | ||
| HIV positive | 23 (5.1) | 4 (1.4) | .01 | 19 (1.6) | <.001 |
| HCV seropositive | 155 (34.4) | 70 (24.7) | .006 | 296 (24.9) | <.001 |
| Charges, median (IQR), $ | 108 528 (43 895–252 086) | 89 997 (39 528–211 734) | .056 | 77 660 (35 803–198 624) | .001 |
| LOS, median (IQR), d | 12 (5–21) | 11 (4–23) | .50 | 9 (4–200) | .006 |
| Discharge status | .01 | <.001 | |||
| In-hospital death | 16 (3.6) | 11 (3.9) | 60 (5) | ||
| SNF/post-acute care facilities | 177 (39.2) | 121 (42.8) | 448 (37.8) | ||
| Home with services | 25 (5.5) | 26 (9.2) | 117 (9.9) | ||
| Home | 115 (25.5) | 61 (21.6) | 342 (28.8) | ||
| AMA | 92 (20.4) | 56 (19.8) | 154 (13) | ||
| Valve replacement | 33 (7.3) | 43 (15.2) | .001 | 141 (11.9) | .003 |
| Multiple valve | 21 (63.6) | 25 (58) | .04 | 72 (51) | .11 |
| Tricuspid | 15 (45.5) | 16 (37.2) | .13 | 35 (25) | .08 |
| Pulmonic | 1 (3.03) | 0 (0) | .43 | 2 (1.4) | .75 |
| Mitral | 9 (27.3) | 17 (39.5) | .004 | 52 (36.9) | .02 |
| Aortic | 12 (36.4) | 16 (37.2) | .04 | 58 (41.1) | .09 |
| Unspecified | 19 (57.6) | 22 (51.2) | .04 | 71 (50) | .13 |
Abbreviations: AMA, against medical advice; HCV, hepatitis C virus; HIV, human immunodeficiency virus; IQR, interquartile range; LOS, length of stay; SNF, skilled nursing facility.
aData represent no. (%) of patients unless otherwise specified.
The median LOS for IE admissions was comparable in the Philadelphia and Allegheny subpopulations (median [IQR],12 [5–21] vs 11 [4–23] days, respectively; P = .50). Valve surgery was performed in a higher proportion of patients in Allegheny County (15.2%) than in Philadelphia (7.3%) (P = .001). Despite the higher valve surgery rates in Allegheny County, total hospital charges were similar in Philadelphia (median [IQR], $108 528 [$43 895–$252 086] vs $89 997 [$39 528–$211 733] for Allegheny County; P = .056). Both groups had higher proportions of patients who left against medical advice (20.4% in Philadelphia and 19.8% in Allegheny County), compared with the state level (P < .001) (Table 3).
Length of Stay
Patients with DU-IE had longer stays than those with non-DU-IE (median LOS [IQR], 10 [4–21] vs 7 [4–13] days; P < .001). However, in the multivariable model, we found that a history of OUD or injection drug use was not significantly associated with LOS (incidence rate ratio, 1.02; 95% confidence interval, .98–1.07; P = .36) (Table 4).
Table 4.
Multivariable Regression Model for Analysis of Length of Stay
| Factors Analyzed | IRR (95% CI) | P Value |
|---|---|---|
| Injection drug use/opioid use disorder | 1.02 (.975–1.072) | .36 |
| Age | 0.99 (.992–.994) | <.001 |
| Medicare | 1.04 (1.001–1.076) | .046 |
| Medicaid | 1.21 (1.156–1.257) | <.001 |
| Congenital heart disease | 1.12 (1.079–1.161) | <.001 |
| Coronary artery disease | 1.17 (1.137–1.203) | <.001 |
| Preadmission home intravenous catheter | 1.3 (1.216–1.387) | <.001 |
| Pacemaker | 1.37 (.968–1.953) | .08 |
| Liver disease | 1.07 (1.043–1.098) | <.001 |
| HIV positivity | 1.22 (1.076–1.391) | .002 |
| HCV seropositivity | 1.06 (1.000–1.122) | .36 |
Abbreviations: CI, confidence interval; HCV, hepatitis C virus; HIV, human immunodeficiency virus; IRR, incidence rate ratio.
Testing Validity
When we compared the number of IE admissions at our academic institute identified by the PHC4 with the number captured in the prior record review at our institution, we found that the PHC4 cohort underestimated the number of IE cases. In the earlier record review we found 37 admissions for DU-IE and 152 non-DU-IE admissions during the period from 1 July 2016 to 30 June 2017 [13]. Within the PHC4 database, we found only 13 DU-IE and 64 non-DU-IE admissions during a similar time frame.
Discussion
In the current study, we examined one of the most morbid infectious sequelae of OUD—IE—in a state, Pennsylvania, and 2 of its counties that have been heavily affected by the opioid epidemic. We found significant increases in the number of drug-use associated IE cases between 2013 and 2017, both in Pennsylvania overall and in its 2 largest urban counties. Furthermore, we found that patients admitted with DU-IE had longer LOS (differences that were no longer significant in adjusted models), higher charges, and higher rates of leaving the hospital against medical advice and were more likely to be insured through Medicaid, which we interpreted as a marker of poverty and vulnerability.
The large increase in the overall number of admissions for IE in the state during this period of time was driven primarily by the 238% increase in DU-IE admissions between the first and last quarters of the study. This increase was seen statewide as well in the 2 largest urban centers. Although increases have been noted in other studies, the proportion of IE that is DU-IE is higher in our Pennsylvania study (17% in Pennsylvania in 2017 vs 12.1% in a national study), clearly showing that the impact of the opioid epidemic goes beyond overdose deaths and visits to emergency rooms, putting a severe strain on health systems and society, and, most importantly, the patients affected [5, 7, 8, 12].
Our study identifies several important findings related to healthcare use. DU-IE cases were more expensive for hospitals and had higher rates of patients leaving against medical advice, a known risk factor for readmissions. Furthermore, Medicaid was overwhelmingly the primary payer among patients with DU-IE (responsible for two-thirds of cases). This payer distribution has also been shown in prior studies from other states and nationwide [15]. It is also important to note that not all Medicare plans cover outpatient parenteral antimicrobial therapy, which may be why the proportion of patients going home rather than to a skilled nursing facility is not more pronounced between the groups [16]. This suggests that states, in their role administering Medicaid and as public health authorities, must be central to efforts to address acute healthcare needs related to OUD, as well preventive efforts to reduce medical complications.
Our findings also highlight the difficulties with disposition after acute care hospitalization in patients with DU-IE. This has been previously demonstrated in qualitative work by Bearnot et al [17], which captured frustrations among both patients and providers regarding disposition. Prior studies have also shown low completion rates for antibiotics [17, 18]. In our study, we found that that the median LOS was only 10 days among patients with DU-IE, even though IE treatment typically requires 6 weeks of intravenous antibiotics and patients with DU-IE are rarely discharged home with intravenous access. This finding raises the concerning question whether patients with DU-IE are inadequately treated and face the risk of further complications.
Our study uniquely includes 2 urban counties that are among the 3 regions with the highest opioid overdose death rates in the United States. Both counties had higher rates of DU-IE admissions and patients leaving against medical advice (approximately 1 in 5), and Philadelphia specifically had higher hospital charges compared with the state and even with the Pittsburgh area. These rates are high even though both counties have syringe exchange programs available in their high-risk communities. Philadelphia County is unique because it has a higher poverty rate with a higher proportion of persons on Medicaid and is more uniformly urban than Allegheny County. The findings in these high-prevalence counties should serve as a warning for areas with rising rates of OUD about the changing epidemiologic profile of IE disease and the associated challenges in delivering adequate care to this vulnerable population.
Our study had several limitations. First, we collected billing and administrative data that are reliant on appropriate coding and documentation. We used ICD codes for the diagnosis of drug use and were unable to confirm these diagnoses and what routes patients were using, however, we believe that if anything our data underestimate the prevalence of DU-IE. Second, we reported total charges as opposed to costs, which would be a more accurate representation of the financial impact of the IE trends. Third, the study included the period when ICD-9 transitioned to ICD-10 codes, which may have affected our ability to identify outcomes and exposures in the 2 periods; given trends were consistent throughout the switch, however, we suspect this change had a limited impact on our conclusions. Fourth, our analysis lacks finer details of patients’ hospitalizations, including microbiologic data, prior IE, HCV and HIV loads, and antibiotic exposures. We were unable to access data on inpatient consultations or medications to determine whether patients received any addiction medicine consultation or medications for OUD. Furthermore, we were unable to see discharge medications to determine whether patients with DU-IE were discharged with antibiotics (either intravenous or oral), naloxone, or medications for OUD. Finally, we were unable to see longer-term outcomes, such as readmission or posthospital mortality rates, both of which would be important in this patient population.
In terms of validity, the comparison of the number of IE admissions at our academic institution identified by the PHC4 with the number captured in a prior record review study at our institution showed that PHC4 database underestimates the number of IE cases [13]. This could be due either to inaccuracies in billing or the fact that our prior hospital-specific study included non-Pennsylvania residents as well. We were not permitted to reidentify our institution’s cases from the PHC4 database to clarify this difference, owing to the deidentified nature of the PHC4 database. We suspect that substance use disorders are often undercoded and thus our current study may underestimate the burden of DU-IE in the state [12, 19]. Concerningly, this would suggest that DU-IE rates may be even higher than we estimated.
In summary, our study demonstrated not only an increase in IE over time in Pennsylvania, but specifically a significant increase in DU-IE cases in one of the states hardest hit by the opioid epidemic. The higher hospital charges, higher proportion of patients on Medicaid, and high rates of patients leaving against medical advice among those with DU-IE demonstrate the notable burden that the opioid epidemic is having on the healthcare system. There is an urgent need to develop innovative and integrative models to improve treatment for patients with substance use and its many downstream consequences.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. The authors acknowledge Helen Koenig, MD, MPH, and Pablo Tebas, MD, for their assistance in reviewing and commenting on the manuscript.
Financial support. This work was supported by the National Institutes of Health (grant T32-HP10026) and the National Institute on Drug Abuse (grant R25DA013582).
Potential conflicts of interest. The authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
- 1. Centers for Disease Control and Prevention. Drug overdose deaths. Available at: https://www.cdc.gov/drugoverdose/data/statedeaths.html. Accessed 28 September 2019.
- 2. Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999–2017. National Center for Health Statistics, Centers for Disease Control and Prevention. November 2018. Available at: https://www.cdc.gov/nchs/products/databriefs/db329.htm. Accessed 28 September 2019. [Google Scholar]
- 3. Centers for Disease Control and Prevention. CDC WONDER. Available at: https://wonder.cdc.gov/. Accessed 28 September 2019.
- 4. PA Health Care Cost Containment Council. Hospital admissions for opioid overdose and opioid use disorder. Available at: http://www.phc4.org/reports/researchbriefs/overdoses/101618/docs/researchbrief_overdoses101618.pdf. Accessed 28 September 2019.
- 5. Rapoport AB, Beekmann SE, Polgreen PM, Rowley CF. Injection drug use and infectious disease practice: a national provider survey. Open Forum Infect Dis 2017; 4(suppl 1):S340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wurcel AG, Anderson JE, Chui KK, et al. Increasing infectious endocarditis admissions among young people who inject drugs. Open Forum Infect Dis 2016; 2:ofw157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schranz AJ, Fleischauer A, Chu VH, Wu LT, Rosen DL. Trends in drug use–associated infective endocarditis and heart valve surgery, 2007 to 2017: a study of statewide discharge data. Ann Intern Med 2019; 170:31–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hartman L, Barnes E, Bachmann L, Schafer K, Lovato J, Files DC. Opiate Injection-associated Infective Endocarditis in the Southeastern United States. Am J Med Sci 2016; 352:603–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fleischauer AT, Ruhl L, Rhea S, Barnes E. Hospitalizations for endocarditis and associated health care costs among persons with diagnosed drug dependence—North Carolina, 2010–2015. MMWR Morb Mortal Wkly Rep 2017; 66:569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. PA Health Care Cost Containment Council. About the council. Available at: http://www.phc4.org/council/mission.htm. Accessed 28 September 2019.
- 11. Ball LJ, Sherazi A, Laczko D, et al. Validation of an algorithm to identify infective endocarditis in people who inject drugs. Med Care 2018; 56:e70–5. [DOI] [PubMed] [Google Scholar]
- 12. Janjua NZ, Islam N, Kuo M, et al. ; BC Hepatitis Testers Cohort Team . Identifying injection drug use and estimating population size of people who inject drugs using healthcare administrative datasets. Int J Drug Policy 2018; 55:31–9. [DOI] [PubMed] [Google Scholar]
- 13. Meisner J, Koenig H, Tebas P. Synergizing infectious diseases and substance use treatment to improve the outcomes of endocarditis in people who inject drugs at a large academic hospital. Open Forum Infect Dis 2018; 5(suppl 1):S306–7. [Google Scholar]
- 14. US Census Bureau . Quick facts. US Census Bureau, 2018. Available at: https://www.census.gov/quickfacts/fact/table/alleghenycountypennsylvania,philadelphiacountypennsylvania,PA/PST045218. Accessed 27 September 2019. [Google Scholar]
- 15. Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002-12. Health Aff 2016; 35:832–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Keller S, Pronovost P, Cosgrove S. What Medicare is missing. Clin Infect Dis 2015; 61:1890–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bearnot B, Mitton JA, Hayden M, Park ER. Experiences of care among individuals with opioid use disorder-associated endocarditis and their healthcare providers: results from a qualitative study. J Subst Abuse Treat 2019; 102:16–22. [DOI] [PubMed] [Google Scholar]
- 18. Libertin CR, Camsari UM, Hellinger WC, Schneekloth TD, Rummans TA. The cost of a recalcitrant intravenous drug user with serial cases of endocarditis: need for guidelines to improve the continuum of care. IDCases 2017; 8:3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stimson G, Hickman M, Quirk A, Frischer M, Taylor C. Estimating the prevalence of problem drug use in Europe. EMCDDA Scientific Monograph Series (No. 1). Luxembourg: Office for Official Publications of the European Communities, 1997. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.