To the Editor:
Henoch-Schönlein purpura (HSP) is a systemic vasculitic syndrome mostly observed in children. Herein, we present the case of a 40-year-old female with history of occasional headaches and Hashimoto’s thyroiditis (euthyroid, not on medication) who presented for evaluation of a new purpuric rash on her gluteal region of unknown duration (Fig. 1 ). The patient reported a severe headache the day before. Twenty days prior to presentation, she received the second dose of the Pfizer‐BioNTech BNT16B2b2 mRNA vaccine, reporting mild fatigue and myalgias lasting 2 days post injection. Fourteen days prior to presentation, she had intrauterine insemination (IUI) preceded by choriogonadotropin alfa injection 2 days prior and letrozole a week prior, a regimen she had received previously without complications. Physical exam was otherwise unremarkable. Laboratory results revealed a mild leukocytosis of 12.98 K/uL (neutrophil predominant). Platelet count, coagulation profile, fibrinogen, haptoglobin, quantitative immunoglobulins (Ig) including IgA/G/M, electrolytes, kidney and liver function, kappa and lambda free light chains, and urine protein level were all within normal levels. The urinalysis showed 2 red blood cells per high power field. Pregnancy test was negative. Rheumatology, hematology, and fertility doctors agreed the rash was consistent with early-stage HSP triggered by Pfizer‐BioNTech BNT16B2b2 mRNA vaccination. Given lack of systemic involvement, she was asked to monitor symptoms. Rash resolved within a week.
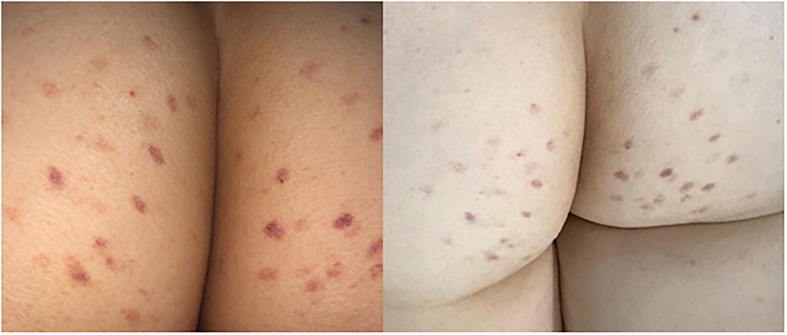
Fig. 1.
Multiple purpuric lesions, some with darker centers. The rash was non-palpable, non-pruritic, non-blanching, and only localized to the gluteal region.
HSP is a diagnosis of exclusion without specific diagnostic tests. While HSP is the most common form of primary childhood vasculitis in Europe and North America, it is significantly less common in adults (3–14 cases per million) [1]. Clinical presentation is variable and, in addition to purpuric lesions, additional organ involvement and associated complications can be observed [2]. The etiology of HSP is not well understood and seems to be a combination of genetic, environmental, and infectious causes. HSP has previously been reported following immunization with various vaccines, mostly within 12 weeks post vaccination [3].
The aim of this report is to highlight a possible association between COVID-19 vaccination (Pfizer‐BioNTech BNT16B2b2 mRNA vaccine) and first onset of HSP in a previously well adult. There were no cases reported amongst 43,448 participants in the Pfizer‐BioNTech BNT16B2b2 mRNA vaccine trial [4]. Although confounding, the hormonal exposure for IUI was brief and without prior history of side effects. She denied recent infections or exposure to SARS-CoVID-2. Skin lesions with features of vasculitis have been reported in COVID-19 infections ranging from asymptomatic to fatal [5]. Given the appearance and typical distribution of the rash, the dermatology team felt that a skin biopsy was not necessary for the diagnosis of HSP. Although the mRNA vaccine field developed extremely rapid with two mRNA vaccines under Emergency Use Authorization, the platform is safe and lacks the potential risk of infection or insertional mutagenesis. To our knowledge, this is the first case of HSP after the administration of a COVID mRNA vaccine which was likely the cause. Given the temporal association, this vaccine has the potential to induce post-vaccination vasculitis, a rare adverse event. As mass vaccination campaigns start worldwide, particularly of younger patients where HSP is more frequently observed, physicians should be aware of this complication, but should continue to encourage vaccination efforts given the well documented safety profile and efficacy of the Pfizer‐BioNTech BNT16B2b2 mRNA vaccine.
There was no funding provided for this manuscript.
COI: JCB receives research funding from AstraZeneca, Oncternal, TG therapeutics, Pharmacyclics/Abbvie, honoraria from Janssen, and has worked as a consultant for AstraZeneca, Pharmacyclics/Abbvie, Beigene, Genentech, Gilead, Innate.
The patient consented to the publication of images and/or information regarding this case.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Watts R.A., Scott D.G. Epidemiology of the vasculitides. Semin Respir Crit Care Med. 2004;25(5):455–464. doi: 10.1055/s-2004-836139. PMID: 16088491. [DOI] [PubMed] [Google Scholar]
- 2.Schnabel A., Hedrich C.M. Childhood Vasculitis. Front Pediatr. 2019;10(6):421. doi: 10.3389/fped.2018.00421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Felicetti P., Trotta F., Bonetto C., et al. Spontaneous reports of vasculitis as an adverse event following immunization: A descriptive analysis across three international databases. Vaccine. 2016;34(51):6634–6640. doi: 10.1016/j.vaccine.2015.09.027. [DOI] [PubMed] [Google Scholar]
- 4.Polack F.P., Thomas S.J., Kitchin N., et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGonagle D, Bridgewood C, Ramanan AV, Meaney JFM, Watad A. COVID-19 vasculitis and novel vasculitis mimics. Lancet Rheumatol. Published online January 7, 2021. doi:10.1016/S2665-9913(20)30420-3. [DOI] [PMC free article] [PubMed]