Abstract
Background: Coronary Artery Disease (CAD) is the foremost single cause of mortality and loss of Disability Adjusted Life Years (DALYs) globally. A large percentage of this burden is found in low and middle income countries. This accounts for nearly 7 million deaths and 129 million DALYs annually and is a huge global economic burden.
Objective: To review epidemiological data of coronary artery disease and acute coronary syndrome in low, middle and high income countries.
Methods: Keyword searches of Medline, ISI, IBSS and Google Scholar databases. Manual search of other relevant journals and reference lists of primary articles.
Results: Review of the results of studies reveals the absolute global and regional trends of the CAD and the importance and contribution of CAD for global health. Data demonstrates which region or countries have the highest and lowest age-standardized DALY rates and what factors might explain these patterns. Results also show differences among the determinants of CAD, government policies, clinical practice and public health measures across the various regions of world.
Conclusion: CAD mortality and prevalence vary among countries. Estimation of the true prevalence of CAD in the population is complex. A significant number of countries have not provided data, the estimation of the exact figures for epidemiological data is a barrier. The incidence of CAD continues to fall in developed countries over the last few decades and this may be due to both effective treatment of the acute phase and improved primary and secondary preventive measures. Developing countries show considerable variability in the incidence of CAD. The globalization of the Western diet and increased sedentary lifestyle will have a dramatic influence on the progressive increase in the incidence of CAD in these countries.
Keywords: Coronary artery disease, acute coronary syndrome, coronary heart disease, epidemiology
1. INTRODUCTION
Coronary Artery Disease (CAD) is characterized by the presence of atherosclerosis in coronary arteries and it can be asymptomatic. Coronary Heart Disease (CHD)/Ischaemic Heart Disease (IHD) includes the diagnosis of Stable angina, Acute Coronary Syndrome (ACS) and silent myocardial ischaemia and mortality from CHD results from CAD. ACS almost always presents with a symptom and includes unstable angina and myocardial infarction. For simplicity, herein we will refer to CHD as CAD.
Coronary artery disease is the foremost single cause of mortality and loss of Disability Adjusted Life Years (DALYs) globally. A large number of this burden falls on low and middle income countries accounting for nearly 7 million deaths and 129 million DALYs annually [1–5]. In 2015 CAD accounted for 8.9 million deaths and 164.0 million DALYs [6]. The survivors of Myocardial Infarction (MI) are at high risk from recurrent infarction and have at least five to sixfold higher annual mortality rate compared to individuals who do not have CAD [7–11]. Overall, the age-adjusted rate of hospitalization due to MI was 215/100,000 individuals between 1979 and 1981, and this number increased till 1987, stabilized in the following decade, and then started to decline from 1996 onward, reaching 242/100,000 individuals in 2005 [7,12–15]. The risk of dying from CAD rises significantly with aging and systolic blood pressure is the most important modifiable risk factor explaining some additional CAD risks that come about with age [7,16,17].
Worldwide, the highest number of increases in the incidence of cardiac event has been in Latin America, the Middle East and to a lesser degree, the Far East, but shows some regional variation. The number of deaths from CAD was projected to increase in developing countries (India, China, Latin America, Sub-Sahara Africa and the Far East) from an estimated 9 million in 1990 to 19 million in 2010 [7]. Although the high occurrence of CAD in China is associated with traditional risk factors, the tendency of high incidence in India has not been explained by traditional risk factors [7]. In line with the Global Burden of Disease (GBD) estimates from 2001, 43% of all Cardio Vascular Disease (CVD) deaths are related to CAD [18]. It is observed that death rates and patterns differ between developed or high income countries and low and middle income countries [18]. In Latin America, the high incidence of CAD is explained by increased sedentary lifestyle, smoking and obesity [7]. When considering racial differences, mortality from CAD is higher in black compared to whites [7]. Therefore, the differences in disease prevalence in various parts of the world are possibly due to multiple factors [18]. Firstly, various phases of the epidemiological transition in different countries are a significant determinant [18]. When a country heads away from an agrarian economy to industrialization, there will be an increased level of risk factors and also upgraded medical facilities and public health for a large percentage of the general public. The balance of these two can lead to varying levels of CAD incidence, prevalence and CAD mortality [18]. Secondly, the presence of war or infection can bind the aging population and hence CAD mortality has not increased like in other regions [18]. Thirdly, various geographical regions may have genetic predisposition for CAD risk factors such as in South Asia, metabolic syndrome is a risk factor [18,19].
Though it is observed that the mortality rate from CAD has decreased over the last four decades, it still accounts for almost one third of deaths in individuals older than 35 years of age [7]. Approximately half of the reduction of mortality can be credited to the upgraded management of the acute phase of ACS and related complications like acute heart failure, improved primary and secondary prevention strategies and revascularization of chronic angina [7]. The balance 50% can be attributed to enhanced control of risk factors in the community, including reduction of total cholesterol, smoking, blood pressure and sedentary lifestyle [7].
The INTERHEART study showed that there were potentially modifiable risk factors for ACS including raised Apo B/Apo A ratio, current smoking status, psychosocial factors, diabetes, hypertension, abdominal obesity, alcohol consumption, regular physical activity and daily consumption of fruits and vegetables [20]. Further, a gender specific pattern of risk factors has become apparent globally, with women presenting with ACS having high rate of hypertension, diabetes mellitus and obesity as opposed to men [21,22]. Moreover, globally there is a tendency for female patients to receive less aggressive invasive and pharmacological treatment after ACS [21,22].
The purpose of this study was to review epidemiological data of CAD and ACS in low, middle and high income countries. This will help in making strategies for primary and secondary prevention of CAD and ACS according to the risk factors present and to availability of resources within the region.
2. MATERIALS AND METHODS
A literature search was done using PubMed/Medline, ISI, IBSS and Google Scholar databases to identify and evaluate all relevant English-language studies of epidemiological studies on CAD and ACS. Manual search of other relevant journals and references lists of primary articles was done by Udaya Ralapanawa. Reference lists of identified papers, relevant reviews and meta-analyses were scrutinized for additional articles. The study period was 2000–2019 and excluding letters, editorials, conference abstracts, reviews, and comments, we used the following key words “Coronary Artery Disease”, “Acute Coronary Syndrome”, “Coronary Heart Disease”, and “Epidemiology”. Then the selected articles were reassessed for relevance and duplication. Out of all studies found, the studies which do not have access to full article were excluded. The search strategy was conducted following previously published principles. All selected articles were read by authors. Detailed notes, impressions were written down and decided on which pieces of data possess values. Data was grouped in to relevant categories and subcategories (low income and high income etc.) allowing them to be examined together and searched. Pattern and relationship between data sets were identified and analyzed in details and interpretations were made.
3. RESULTS
Based on geography and income level, the World Bank has recognised six low and middle income regions globally and the rest of high income countries are not geographically distinct [18].
3.1. Low-middle Income Regions
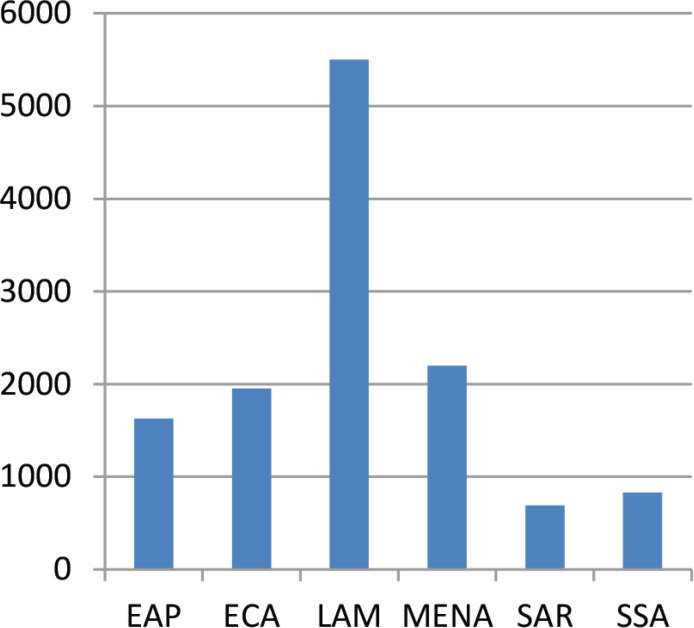
A country with Gross National Income (GNI) per capita of $1025 or less is considered as a low-income economy while GNI per capita between $1026–$12,375 is considered a middle-income economy [18,23]. The six low–middle income regions composed of East Asia and Pacific, Europe and Central Asia, Latin America and the Caribbean, the Middle East and North Africa, the South Asia region and Sub-Saharan Africa [18,23]. Figure 1 shows GNI ($US) per capita 2005 as per World Bank Development Indicators 2007 in low–middle income regions [18,23]. Though there is large decline in deaths of CAD in high income countries, low and middle income countries show a mixed trend [18,24,25]. Figure 2 shows percentage of total mortality attributable to CHD in 2001 by developing region as per WHO Global Burden of Disease and Risk Factors 2006 [18].
Figure 1.
Gross National Income ($US) per capita 2005 (World Bank Development Indicators 2007).
Figure 2.
Percentage of total mortality attributable to CHD in 2001 by developing region as per WHO Global Burden of Disease and Risk Factors 2006.
3.1.1. East Asia and Pacific region
The East Asia and Pacific Region (EAP) is the most populated (1885 million people) low and middle income regions where 70% of inhabitants of the region live in China. Some of the other countries of the region are Pacific islands, Thailand, Laos, Colombia and Malaysia. The life expectancy of the EAP region has risen rapidly [18,26]. The life expectancy in China increased from 37 to 71 years in the mid-1950s to 2000 respectively [18,27]. This increase of life expectancy can be aligned with rapid urban modernization, a large rural to urban migration, reduced birth rates, aging of the population, major dietary changes, increased tobacco and alcohol consumption and a movement toward work involving physical inactivity which all leads to changing patterns of CAD in the region [6,18]. The WHO GBD Project has shown that 1 million deaths in the region were due to CAD [18,28]. The prevalence of angina was 8.2 million people and the number of DALY due to CAD was 11.8 million [18,28]. Approximately 60–70% of CVD mortality in China resulted from stroke and CAD [18,29]. In contrast to Europe and the USA, stroke is the leading cause of CVD in most areas of EAP. In China, among men aged 35–64 years, stroke death rate is 217–243 per 100,000 versus CAD death rate is 64–106 per 100,000 [18,30]. In China, despite the high stroke rate, CAD rate has grown speedily over the last 20 years accounting for the second leading cause of death [31]. The incidence of CAD increased annually by 2.7% and 1.2% in men and women respectively [1,6]. In China ACS occurs 5 years earlier compared to Caucasian and Latin American countries [6,18].
As reported by the WHO, in 2012 in Malaysia 98.9 deaths per 100,000 population or 29,400 deaths (20.1% all deaths) were due to CAD [32,33]. The Malaysian burden of disease study conducted in 2000 exhibited that CAD accounts for 22,158 deaths or about one fifth of all deaths [32,34]. According to the National Cardiovascular Database of Malaysia, Malaysians present with ACS at a younger age (mean age 55.9–59.1 years) compared to the most developed countries [32,35].
3.1.2. Europe and Central Asia
The Europe and Central Asia (ECA) region consists of west of Poland, the Czech Republic, Hungary, Slovenia, Slovakia, and Croastia and Russia which is the most populated in ECA region with 30% inhabitants [18]. According to the GBD study, almost 30% of all deaths in the ECA region were due to CAD [18,36]. As per the data published in 2002, mortality due to CAD in all ECA countries was still much higher than that of North America and Western Europe. In 2015, the mean age-standardised CAD mortality in Eastern Europe (444.9) and Central Asia (425.2) was twice as high when compared to Central Europe (234.0) [37]. From the early 1990s, falls in death rate from CAD was observed in Some ECA countries like Poland, Slovenia, Hungary, the Czech Republics and Slovakia. However, in Soviet Republics and Ukraine the CAD mortality is in rising trend [18,38,39].
3.1.3. Latin America and Caribbean
The Latin America and Caribbean (LAM) region includes Central America, South America and the most islands of Caribbean [18]. According to the WHO GBD study CAD was ranked as a leading cause of mortality in this region accounting for 35% all deaths [18,40]. In Brazil, 1% of total hospital admissions were due to CAD [18,41,42]. CVD accounts for 300,000 deaths per year or 820 deaths per day in Brazil while CAD accounts for one third of CVD deaths [18,43]. Data illustrates that Latin American countries are at different stages of CVD epidemic. A falling trend in CAD mortality has been observed in most LAM countries except Mexico and Panama in the recent past [24,44]. The age-adjusted CAD mortality rate reduced in Colombia and Argentina while it increased in Mexico. Likewise, the same mortality rate for young adults (<35 years) showed a significant rise in Mexico for both genders while a lessening trend is seen in Colombia and Argentina [24,43].
3.1.4. Middle East and North Africa
Middle East and North Africa (MENA) comprises of over 17 countries and is home to nearly 6% of the world’s population with 306 million people [18]. In 2001, CAD was the leading cause of death in the MENA region accounting for 21% deaths [45]. In accordance with a study done on the global burden of CVD, there will be a 161% increase of CAD by 2020 in this region [18,46]. In the coming few decades, the prevalence of CAD will see an upsurge in the Gulf region owing to rapid urbanization and increases in the number of relatively young inhabitants [47]. Patients in the MEA present with myocardial infarction at a younger age compared to other regions [48,49]. As stated in the INTERHEART study, in the Middle East, region median age at presentation with myocardial infarction was 51 years and was 12 years lower than the same for Western Europe [49]. High prevalence of cardiovascular risk factors like hypertension, smoking, diabetes, dyslipidaemia and sedentary lifestyle in MENA region contribute to a high prevalence of CAD in the region [49]. The latest detailed national level epidemiological data are sparse for many countries in the Middle East region and a large number of temporary emigrant workforces in the region, cultural and environment barriers in the region complicate the development of such databases [49]. Data shows that the management of CAD in some Middle Eastern countries is not up to standard [49]. It is important that Gulf countries are accounting for higher ACS complications and mortality rate in women [49].
Egypt is the most populous of the MENA countries and recent studies revealed higher CAD mortality rates in Egypt in this region [50]. The earliest documented case of coronary atherosclerosis in Egypt was seen in a princess who died in her early 40s and lived between 1580 and 1550 BC [50]. In 2014, CAD accounted for 23.14% of all deaths in Egypt which ranks Egypt 23rd in the world [51,52]. Recent studies expressed that ACS patients in Egypt are relatively young (mean age 57 years) compared with patients living in the West (mean age 66 years) [53–56]. In line with the Cardio Risk study done across Egypt, central obesity, diabetes and hypertension were more prevalent in women with ACS and were acknowledged as major risk factors for ACS [50].
3.1.5. South Asia region
The South Asia Region (SAR) is one of the most heavily populated zones in the world, comprising almost one fifth of the global population [18,57,58]. India is the largest country in SAR, making up nearly 75% of inhabitants [18]. Other countries of the SAR include Afghanistan, Bangladesh, Bhutan, Maldives, Nepal, Pakistan and Sri Lanka. Statistics in 2001 revealed that more than one fourth of global low and middle income country CVD deaths were seen in this region [18]. In 2001, CAD accounts for 13.6% of total mortality or 1.8 million deaths in the region [18]. South Asians have a three to five times higher risk of myocardial infarction and also present at an earlier age with more severe disease compared to Caucasians [57,59,60]. South Asian origin is a well-known independent risk factor for mortality associated with CAD mortality [57,61,62]. There are two very important explanations for high CAD burden among South Asians. Firstly, inhabitants in the region have a high prevalence of traditional risk factors (e.g; age, hypertension, hyperlipidaemia, diabetes, smoking) leading to the development of CAD at a young age [57]. Prevalence of hypercholesterolaemia has gone up in Asia in the course of the past few decades and the smoking rate in Asian men is much higher than the West. Secondly, novel risk factors (e.g. Lipoprotein-a, apolipoprotein B 100, CRP) have been identified in South Asians contributing for CAD risk which is independent of traditional risk factors [57,63–65].
Non-communicable diseases account for nearly 60% of total deaths in India and CAD is one of the major aetiologies [66–68]. CAD accounts for 15.5% of total deaths globally and this has risen in epidemic proportion in India [66,69]. In India, CAD accounted for 26.9% of medically certified deaths in 2015 and 1,200,000 deaths in 2012 [69–71]. However, these figures are likely underrated when compared to the real situation due to the absence of consistent mortality data, non-accounting of silent myocardial infarctions and asymptomatic CAD deaths [62,72]. It was evident that in India there was a two and a sixfold increase in CAD in rural areas and in urban areas respectively from 1960 to 2002 and CAD has been considered to be of epidemic proportion in India [73–75]. The systematic review done by Rao et al. demonstrated that prevalence of CAD in urban areas was 2.5–12.6% and in rural areas, 1.4–4.6%. Moreover, they concluded that the high prevalence of CAD risk factors, treatment delays and suboptimal use of evidence based treatment when managing CADs are common in India [76].
The upsurge in CAD prevalence in India is linked to economic and social change and its after effects like changes in dietary habits, reduced physical activity and increased incidence of hypertension and diabetes [77]. As stated in the GBD Study 1990–2016, the burden from CAD in India varies widely between different states and the highest increase in the prevalence of CAD is seen in low developed states [78]. Today CAD has become a key public health issue in India and it also points to enormous economic burden [79].
The situation in Sri Lanka is also not much different to India. In Sri Lanka life expectancy for females is higher than males. Also over the last few decades, life expectancy for both genders is progressively going up [80,81]. Scientific studies carried out on CAD are limited in the Sri Lankan literature [82]. According to the Annual Health Bulletin of Sri Lanka in 2013, there was a rising trend of hospitalization due to CAD, which has been the leading cause of hospital deaths since 1995 [82,83]. In accordance with 2017 data, CAD is the main killer and is the leading cause of premature deaths in Sri Lanka [80,84]. Based on a publication in 1994 by Mendis and Ekanayakea [85] in one province in Sri Lanka, a high body mass index (>24 kg/m2), hypercholesterolemia (>6.5 mmol/l) and diabetes were more prevalent in urban rather than rural areas.
3.1.6. Sub-Saharan Africa
The epidemiology of CAD in Sub-Saharan Africa (SSA) remains largely uncertain [86]. Lack of reliable health statistics, insufficient diagnostic facilities, lack of health care professionals and misguided opinions are the major obstacles in this region [86,87]. In line with the World Bank, SSA consists of 31 islands and continental nations [18]. About 782 million people lived in SSA region in 2006 and the most populous nation was Nigeria (145 million) [18]. As stated in the INTERHEART Africa study, SSA men with diabetes and hypertension were having a two to threefold increased risk for myocardial infarction [88,89]. The estimated death rate in SSA ranged from 168 per 100,000 to 365 per 100,000 in Eastern and Central Africa respectively [88]. In SSA among men aged 50–69 years, around 87% of deaths due to CAD were credited to dietary risks, 27% to tobacco use and 29% to physical inactivity [88]. Usually, CAD is considered an insignificant cause of morbidity and mortality in SSA [90]. In 2010, CAD was placed as the fourth leading cause of death in SSA [88]. In accordance with the GBD study 2010, the estimated death rates secondary to CAD in SSA men ranged from low in Eastern Africa to very high in Central Africa [88]. In SSA in spite of considerable westernisation of lifestyle with increasing risk factors, CAD remains very low in occurrence [91]. In North America and Western Europe, CAD is the principle cause of acute heart failure, but in SSA acute heart failure is triggered mainly by hypertension, cardiomyopathy and rheumatic heart disease [92]. As in developed countries, CAD increases with age in SSA, but the gender difference in prevalence is not seen here like that in the West [90].
3.2. High Income Regions
A country is considered high income, when a GNI per capita exceeds $12,376 or more [23]. In 2019, the World Bank classified 81 countries and territories as high income countries [23]. Australia, Austria, Belgium, Brunei, Chile, Canada, France, Germany, Ireland, Israel, Italy, Japan, Kuwait, Malta, Netherland, New Zealand, Norway, Qatar, Saudi Arabia, Singapore, South Korea, Spain, Sweden, Taiwan, the UK and the USA are examples of high-income countries [23]. Among the more developed countries, the highest CAD death rates are seen in Ukraine and Russia accounting for 718 and 654 deaths per 100,000 population respectively, while the lowest are seen in South Korea and Japan with 36.5 and 47 deaths per 100,000 respectively [32,93–95].
When we consider CAD patterns in high income regions, in the USA, CAD is the leading cause of death in adults accounting for one third of all deaths in individuals older than 35 years [7,96,97]. It is projected that nearly a half of the middle aged men and one third of the middle age women in the United State of America (USA) will experience some symptoms of CAD [7]. In each year, more than 600,000 individuals will have their first myocardial infarction, and approximately 300,000 patients with diagnosed CAD will have recurrence [98,99]. It is predicted that each year an additional 195,000 silent first myocardial infarction will occur in the USA [100]. Overall, the incidence of CAD has declined in the USA between 114 and 133 cases for every 100,000 person-years of follow up [7]. As stated in a study done between 2001 and 2012, Yoon et al. described that there was a significant downward trend in the prevalence of CAD [101]. It was forecasted that in 2013 one citizen in the US will have a MI every 44 s, and almost every 1 min, someone will die of coronary event [7,100]. Although the incidence of CAD has decreased in the USA over the last few decades, there is comparative rise in the incidence of Non-ST-Elevation ACS (NSTEACS) in comparison with ST-Elevation Myocardial Infarction (STEMI) (7). As reported by the United States National Registry of Myocardial Infarction, the percentage of NSTEACS has gone up from 19% in 1994 to 59% in 2006 [7]. In conformity with a study done by the Global Burden of Cardiovascular Disease Collaboration across the USA, between 1990 and 2016, age-standardized CVD DALYs for all the US states has reduced [70]. Cardiovascular disease DALYs in men was twice as high as that in women. CAD was the foremost cause of CVD DALYs in all states. About 12 CVD risk factors were recognized and the largest attributable CVD burden is owing to dietary risk exposures followed by high systolic blood pressure [70].
In the UK, CVD mortality is declining [102]. Between 1979 and 2013 CAD deaths at all ages reduced by 72% in England, 71% in Scotland, 70% in Wales and 76% in Northern Ireland. Premature CAD mortality followed a similar pattern [102]. In 2014, CAD was the principle cause of deaths for both males (15%) and females (10%). The death rate of CAD in European region also was dropping in the last decade, but CAD remains the leading cause of mortality in the UK and Europe [103,104].
In Japan, the mortality from CAD is lower than the USA and Europe [7,105–109]. Age-adjusted mortality rates in Japan decreased by 61% from 1980 to 2012 [110,111]. Though stroke incidence is decreasing in Japan, the number of population based epidemiological studies has seen a rise in CAD incidence among men in some parts of Japan in recent decades [105]. This rise in incidence of CAD is attributable to westernization of lifestyle since 1960 [112]. CAD accounts for nearly a half of heart disease related deaths [112,113]. The risk of dying from CAD and its incidence among Japanese women are half or lower than in Japanese men [112].
4. DISCUSSION
Even though CAD mortality and prevalence vary among countries it is the top cause of death in countries of all income groups. Estimation of the true prevalence of CAD in the population is complex [7]. As a significant number of countries have not provided data, the provision of exact figures for epidemiological data is a barrier [2]. Further, the scientific studies carried out on CAD are limited in some regions especially in low and middle income countries including Sri Lanka.
The incidence of CAD continues to fall in developed countries, but due to immigration and progressive population aging the absolute number of coronary events and as a consequence of the prevalence of CAD will not reduce but it may even go up in near the future [7]. Developing countries display considerable variability in the incidence of CAD. The globalization of Western diet and increased sedentary lifestyle will have a dramatic impact on the progressive rise in the incidence of CAD in these countries [7]. The progressive decrease in mortality from CAD in developed countries over the recent few decades may be due to both effective treatment for the acute phase and improved primary and secondary preventive measures [7]. However, ethnic difference, social inequalities, and difference in availability of effective treatment and preventive measures in different regions of the same country may affect overall outcome and this needs more studies and evaluation of different regions within the country.
Economic and social transformation is occurring much more rapidly in a post-industrial world with rapid globalization and this is a major challenge to low and middle income countries, unlike developed countries. This has led to much more rapid changes in risk factors and incidence rate compared to the development of health care facilities, human resources and the infrastructure to manage CAD. Implementing public health strategies focused on primary prevention supported by a primary care infrastructure in both low and middle income countries and in groups with low socioeconomic status in high-income countries is a way forward.
Mortality from non-communicable diseases including CAD is expected to rise in the coming decades due to worsening of metabolic risk factors. Hence, the reduction in the CAD burden will require changes at both the policy as well as at the individual levels. Stake holders should target these risk factors through public health policies and this may be the best way to interrupt this trend. Risk factor prevention campaigns and mass media campaigns promoting healthy behavior may play a significant role in overcoming this problem.
5. CONCLUSION
Coronary artery disease mortality and prevalence vary among countries. Estimation of the true prevalence of CAD in the population is complex. As a significant number of countries have not provided data, the estimation of the exact figures for epidemiological data is a barrier. While the incidence of CAD continues to fall in developed countries over the last few decades, the developing countries show considerable variability in the incidence of CAD.
All countries should make an effort to provide correct epidemiological data and to conduct studies and research on CAD risk factors, prevention and new treatment windows regionally as well as globally which will help in making future strategies.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
UR conceived the research idea and conducted the literature searches, collected and collated articles and drafted this paper. UR and RS commented in details on drafts and contributed to the final version of the manuscript.
REFERENCES
- [1].Vedanthan R, Seligman B, Fuster V. Global perspective on acute coronary syndrome: a burden on the young and poor. Circ Res. 2014;114:1959–75. doi: 10.1161/CIRCRESAHA.114.302782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Nowbar AN, Howard JP, Finegold JA, Asaria P, Francis DP. 2014 Global geographic analysis of mortality from ischaemic heart disease by country, age and income: statistics from World Health Organisation and United Nations. Int J Cardiol. 2014;174:293–8. doi: 10.1016/j.ijcard.2014.04.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Moran AE, Oliver JT, Mirzaie M, Forouzanfar MH, Chilov M, Anderson L, et al. Assessing the Global Burden of Ischemic Heart Disease: part 1: methods for a systematic review of the Global Epidemiology of Ischemic Heart Disease in 1990 and 2010. Glob Heart. 2012;7:315–29. doi: 10.1016/j.gheart.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Forouzanfar MH, Moran AE, Flaxman AD, Roth G, Mensah GA, Ezzati M, et al. Assessing the Global Burden of Ischemic Heart Disease: part 2: analytic methods and estimates of the Global Epidemiology of Ischemic Heart Disease in 2010. Glob Heart. 2012;7:331–42. doi: 10.1016/j.gheart.2012.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ounpuu S, Yusuf S. Singapore and coronary heart disease: a population laboratory to explore ethnic variations in the epidemiologic transition. Eur Heart J. 2003;24:127–9. doi: 10.1016/s0195-668x(02)00611-5. [DOI] [PubMed] [Google Scholar]
- [6].Zhang G, Yu C, Zhou M, Wang L, Zhang Y, Luo L. Burden of ischaemic heart disease and attributable risk factors in China from 1990 to 2015: findings from the global burden of disease 2015 study. BMC Cardiovasc Disord. 2018;18:18. doi: 10.1186/s12872-018-0761-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ferreira-González I. The epidemiology of coronary heart disease. Rev Esp Cardiol (Engl Ed) 2014;67:139–44. doi: 10.1016/j.rec.2013.10.002. [DOI] [PubMed] [Google Scholar]
- [8].Yusuf S, Reddy S, Ôunpuu S, Anand S. Global burden of cardiovascular diseases: part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104:2855–64. doi: 10.1161/hc4701.099488. [DOI] [PubMed] [Google Scholar]
- [9].Viera AJ, Sheridan SL. Global risk of coronary heart disease: assessment and application. Am Fam Physician. 2010;82:265–74. https://pubmed.ncbi.nlm.nih.gov/20672791/ [PubMed] [Google Scholar]
- [10].Joseph P, Leong D, McKee M, Anand SS, Schwalm JD, Teo K, et al. Reducing the global burden of cardiovascular disease, part 1: the epidemiology and risk factors. Circ Res. 2017;121:677–94. doi: 10.1161/CIRCRESAHA.117.308903. [DOI] [PubMed] [Google Scholar]
- [11].Leong DP, Joseph PG, McKee M, Anand SS, Teo KK, Schwalm JD, et al. Reducing the global burden of cardiovascular disease, part 2: prevention and treatment of cardiovascular disease. Circ Res. 2017;121:695–710. doi: 10.1161/CIRCRESAHA.117.311849. [DOI] [PubMed] [Google Scholar]
- [12].Webster R, Rodgers A. WHO; 2013. Background Paper 6.3. Ischaemic heart disease. [Google Scholar]
- [13].Tardif JC. Coronary artery disease in 2010. Eur Heart J Suppl. 2010;12:2–10. doi: 10.1093/eurheartj/suq014. [DOI] [Google Scholar]
- [14].Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70:1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Dai X, Busby-Whitehead J, Alexander KP. Acute coronary syndrome in the older adults. J Geriatr Cardiol. 2016;13:101–8. doi: 10.11909/j.issn.1671-5411.2016.02.012. https://pubmed.ncbi.nlm.nih.gov/27168733/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Bauersachs R, Zeymer U, Brière JB, Marre C, Bowrin K, Huelsebeck M. Burden of coronary artery disease and peripheral artery disease: a literature review. Cardiovasc Ther. 2019;2019 doi: 10.1155/2019/8295054. 8295054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Mensah GA, Roth GA, Fuster V. The global burden of cardiovascular diseases and risk factors: 2020 and beyond. J Am Coll Cardiol. 2019;74:2529–32. doi: 10.1016/j.jacc.2019.10.009. [DOI] [PubMed] [Google Scholar]
- [18].Gaziano TA, Bitton A, Anand S, Abrahams-Gessel S, Murphy A. Growing epidemic of coronary heart disease in low- and middle-income countries. Curr Probl Cardiol. 2010;35:72–115. doi: 10.1016/j.cpcardiol.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Gupta P, Gan ATL, Man REK, Fenwick EK, Tham YC, Sabanayagam C, et al. Risk of incident cardiovascular disease and cardiovascular risk factors in first and second-generation Indians: the Singapore Indian eye study. Sci Rep. 2018;8:14805. doi: 10.1038/s41598-018-32833-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Oliveira GBF, Avezum A, Roever L. Cardiovascular disease burden: evolving knowledge of risk factors in myocardial infarction and stroke through population-based research and perspectives in global prevention. Front Cardiovasc Med. 2015;2:32. doi: 10.3389/fcvm.2015.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Reda A, Ashraf M, Soliman M, Ragy H, Elkersh A, Abdou W, et al. Gender-related differences in risk factors and treatment strategies in patients with acute coronary syndrome across Egypt: part of the Cardio-Risk Project. Atheroscl Suppl. 2018;33:E2. doi: 10.1016/j.atherosclerosissup.2018.07.045. [DOI] [Google Scholar]
- [22].Pagidipati NJ, Peterson ED. Acute coronary syndromes in women and men. Nat Rev Cardiol. 2016;13:471–80. doi: 10.1038/nrcardio.2016.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].The World Bank World Bank Country and Lending Groups. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- [24].Arroyo-Quiroz C, Barrientos-Gutierrez T, O’Flaherty M, Guzman-Castillo M, Palacio-Mejia L, Osorio-Saldarriaga E, et al. Coronary heart disease mortality is decreasing in Argentina, and Colombia, but keeps increasing in Mexico: a time trend study. BMC Public Health. 2020;20:162. doi: 10.1186/s12889-020-8297-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].World Health Organization (WHO) The World Health Report 2013. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- [26].Chan MY, Du X, Eccleston D, Ma C, Mohanan PP, Ogita M, et al. Acute coronary syndrome in the Asia-Pacific region. Int J Cardiol. 2016;202:861–9. doi: 10.1016/j.ijcard.2015.04.073. [DOI] [PubMed] [Google Scholar]
- [27].World Health Organization (WHO) World Health Report 2003: shaping the future. Geneva, Switzerland: World Health Organization; 2003. [Google Scholar]
- [28].World Health Organization (WHO) The Global Burden of Disease: 2004 update. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- [29].Liu L. Cardiovascular diseases in China. Biochem Cell Biol. 2007;85:157–63. doi: 10.1139/O07-004. [DOI] [PubMed] [Google Scholar]
- [30].Zhang XH, Lu ZL, Liu L. Coronary heart disease in China. Heart. 2008;94:1126–31. doi: 10.1136/hrt.2007.132423. [DOI] [PubMed] [Google Scholar]
- [31].Huang J, Zeng Q, Pan X, Guo X, Li G. Projections of the effects of global warming on the disease burden of ischemic heart disease in the elderly in Tianjin, China. BMC Public Health. 2019;19:1465. doi: 10.1186/s12889-019-7678-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Ang CS, Chan KMJ. A review of coronary artery disease research in Malaysia. Med J Malaysia. 2016;71:42–57. https://pubmed.ncbi.nlm.nih.gov/27801387/ [PubMed] [Google Scholar]
- [33].World Health Organization (WHO) Country statistics and global health estimates. Geneva, Switzerland: World Health Organization; 2015. [Google Scholar]
- [34].Yusoff AF, Mustafa AN, Kaur GK, Omar MA, Vos T, Rao VPC, et al. Malaysian burden of disease and injury study. Forum 9; 2005; Mumbai, India. UQ espace; pp. 1–24. [Google Scholar]
- [35].Lu HT, Nordin RB. Ethnic differences in the occurrence of acute coronary syndrome: results of the Malaysian National Cardiovascular Disease (NCVD) Database Registry (March 2006-February 2010) BMC Cardiovasc Disord. 2013;13:97. doi: 10.1186/1471-2261-13-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL, editors. Global burden of disease and risk factors. Washington, DC: The World Bank; 2006. [DOI] [PubMed] [Google Scholar]
- [37].Murphy A, Johnson CO, Roth GA, Forouzanfar MH, Naghavi M, Ng M, et al. Ischaemic heart disease in the former Soviet Union 1990–2015 according to the Global Burden of Disease 2015 Study. Heart. 2020;104:58–66. doi: 10.1136/heartjnl-2016-311142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Mirzaei M, Truswell AS, Taylor R, Leeder SR. Coronary heart disease epidemics: not all the same. Heart. 2009;95:740–6. doi: 10.1136/hrt.2008.154856. [DOI] [PubMed] [Google Scholar]
- [39].Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. Household catastrophic health expenditure: a multicounty analysis. Lancet. 2003;362:111–7. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- [40].Lanas F, Serón P, Lanas A. Coronary heart disease and risk factors in Latin America. Glob Heart. 2013;8:341–8. doi: 10.1016/j.gheart.2013.11.005. [DOI] [PubMed] [Google Scholar]
- [41].Laurenti R, Buchalla CM, de S Caratin VC. Ischemic heart disease. Hospitalization, length of stay and expenses in Brazil from 1993 to 1997. Arq Bras Cardiol. 2000;74:483–92. doi: 10.1590/s0066-782x2000000600001. [DOI] [PubMed] [Google Scholar]
- [42].Neto GB, da Silva EN. The costs of cardiovascular disease in Brazil: a brief economic comment. Arq Bras Cardiol. 2008;91:198–9. 217–18. doi: 10.1590/s0066-782x2008001600002. [DOI] [PubMed] [Google Scholar]
- [43].Gus I, Fischmann A, Medina C. Prevalence of risk factors for coronary artery disease in the Brazilian State of Rio Grande do Sul. Arq Bras Cardiol. 2002;78:484–90. doi: 10.1590/s0066-782x2002000500005. [Article in En, Portuguese]. [DOI] [PubMed] [Google Scholar]
- [44].Pagan E, Chatenoud L, Rodriguez T, Bosetti C, Levi F, Malvezzi M, et al. Comparison of trends in mortality from coronary heart and cerebrovascular diseases in north and South America: 1980 to 2013. Am J Cardiol. 2017;119:862–71. doi: 10.1016/j.amjcard.2016.11.040. [DOI] [PubMed] [Google Scholar]
- [45].See S, Jeppsson A, Stafström M. What is killing? People’s knowledge about coronary heart disease, attitude towards prevention and main risk reduction barriers in Ismailia, Egypt (Descriptive cross-sectional study) Pan Afr Med J. 2013;15:137. doi: 10.11604/pamj.2013.15.137.1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104:2746–53. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- [47].Aljefree N, Ahmed F. Prevalence of cardiovascular disease and associated risk factors among adult population in the Gulf region: a systematic review. 2015;2015 doi: 10.1155/2015/235101. 235101. [DOI] [Google Scholar]
- [48].Jamee Shahwan A, Abed Y, Desormais I, Magne J, Preux PM, Aboyans V, et al. Epidemiology of coronary artery disease and stroke and associated risk factors in Gaza community - Palestine. PLoS One. 2019;14 doi: 10.1371/journal.pone.0211131. e0211131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Almahmeed W, Arnaout MS, Chettaoui R, Ibrahim M, Kurdi MI, Taher MA, et al. Coronary artery disease in Africa and the Middle East. Ther Clin Risk Manag. 2012;8:65–72. doi: 10.2147/TCRM.S26414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].American College of Cardiology . American College of Cardiology; Earliest case of coronary artery disease found in Egyptian Princess. Available from: https://www.acc.org/about-acc/press-releases/2011/04/05/16/22/mummies (cited April 9, 2020). [Google Scholar]
- [51].El-Moselhy EA, Mohammed AS, El-Aziz AA, Sadek I, Hagrass SA, Farag GAS. Coronary artery disease among elderly Egyptian patients: I. socio-demographic, lifestyle, psychosocial, medical, and biochemical risk factors. Am J Gerentol Geriatr. 2018;1:1006. [Google Scholar]
- [52].World Health Organization Rankings (WHOR) Egypt, coronary heart disease. 2013.
- [53].Abdelmoneim HM, Hasan-Ali H, Abdulkader SS. Demographics of acute coronary syndrome (ACS) Egyptian patients admitted to Assiut University Hospital: validation of TIMI and GRACE scores. Egypt J Crit Care Med. 2014;2:3–11. doi: 10.1016/j.ejccm.2014.07.001. [DOI] [Google Scholar]
- [54].Yan AT, Yan RT, Tan M, Casanova A, Labinaz M, Sridhar K, et al. Risk scores for risk stratification in acute coronary syndromes: useful but simpler is not necessarily better. Eur Heart J. 2007;28:1072–8. doi: 10.1093/eurheartj/ehm004. [DOI] [PubMed] [Google Scholar]
- [55].Fox KAA, Eagle KA, Gore JM, Steg PhG, Anderson FA, GRACE and GRACE2 power Investigators The global registry of acute coronary events, 1999 to 2009—GRACE. Heart. 2010;96:1095–101. doi: 10.1136/hrt.2009.190827. [DOI] [PubMed] [Google Scholar]
- [56].Tawfeek H, Nour MK, Bary AA, Fattah AA. Contemporary retrospective analysis of acute coronary syndrome. An Egyptian study. Egypt J Crit Care Med. 2016;4:79–84. doi: 10.1016/j.ejccm.2016.05.001. [DOI] [Google Scholar]
- [57].Coronary Artery Disease in South Asians [Internet] J Asian Health. 2020 Available from: http://journalofasianhealth.com/coronary-artery-disease-in-south-asians/ (cited April 9, 2020).
- [58].Tan ST, Scott W, Panoulas V, Sehmi J, Zhang W, Scott J, et al. Coronary heart disease in Indian Asians. Glob Cardiol Sci Pract. 2014;2014:13–23. doi: 10.5339/gcsp.2014.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Gupta M, Singh N, Verma S. South Asians and cardiovascular risk: what clinicians should know. Circulation. 2006;113:e924–e9. doi: 10.1161/CIRCULATIONAHA.105.583815. [DOI] [PubMed] [Google Scholar]
- [60].Gupta M, Doobay AV, Singh N, Anand SS, Raja F, Mawji F, et al. Risk factors, hospital management and outcomes after acute myocardial infarction in South Asian Canadians and matched control subjects. CMAJ. 2002;166:717–22. https://pubmed.ncbi.nlm.nih.gov/11944758/ [PMC free article] [PubMed] [Google Scholar]
- [61].Anand SS, Yusuf S, Vuksan V, Devanesen S, Teo KK, Montague PA, et al. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE) Lancet. 2000;356:279–84. doi: 10.1016/s0140-6736(00)02502-2. [DOI] [PubMed] [Google Scholar]
- [62].Goyal A, Yusuf S. The burden of cardiovascular disease in the Indian subcontinent. Indian J Med Res. 2006;124:235–44. https://pubmed.ncbi.nlm.nih.gov/17085827/ [PubMed] [Google Scholar]
- [63].Sasayama S. Heart disease in Asia. Circulation. 2008;118:2669–71. doi: 10.1161/CIRCULATIONAHA.108.837054. [DOI] [PubMed] [Google Scholar]
- [64].Mohan V, Deepa R. Risk factors for coronary artery disease in Indians. J Assoc Physicians India. 2004;52:95–7. https://pubmed.ncbi.nlm.nih.gov/15656040/ [PubMed] [Google Scholar]
- [65].Krishnan MN. Coronary heart disease and risk factors in India—On the brink of an epidemic? Indian Heart J. 2012;64:364–7. doi: 10.1016/j.ihj.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Bodkhe S, Jajoo SU, Jajoo UN, Ingle S, Gupta SS, Taksande BA. Epidemiology of confirmed coronary heart disease among population older than 60 years in rural central India—A community-based cross-sectional study. Indian Heart J. 2019;71:39–44. doi: 10.1016/j.ihj.2019.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Prabhakaran D, Jeemon P, Roy A. Cardiovascular diseases in India: current epidemiology and future directions. Circulation. 2016;133:1605–20. doi: 10.1161/CIRCULATIONAHA.114.008729. [DOI] [PubMed] [Google Scholar]
- [68].Sekhri T, Kanwar RS, Wilfred R, Chugh P, Chhillar M, Aggarwal R, et al. Prevalence of risk factors for coronary artery disease in an urban Indian population. BMJ Open. 2014;4 doi: 10.1136/bmjopen-2014-005346. e005346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].World Health Organization (WHO) Global Health Observatory (GHO) Data. Vol. 3. Geneva, Switzerland: World Health Organization; 2015. (Retrieved 23, 2015). [Google Scholar]
- [70].Roth GA, Johnson CO, Abate KH, Abd-Allah F, Ahmed M, et al. Global Burden of Cardiovascular Diseases Collaboration The burden of cardiovascular diseases among US states, 1990-2016. JAMA Cardiol. 2018;3:375–89. doi: 10.1001/jamacardio.2018.0385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].World Health Organization (WHO) Global health estimates: deaths by cause, age, sex and country, 2000-2012. Vol. 9. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- [72].Ahmad N, Bhopal R. Is coronary heart disease rising in India? A systematic review based on ECG defined coronary heart disease. Heart. 2005;91:719–25. doi: 10.1136/hrt.2003.031047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Krishnan MN, Zachariah G, Venugopal K, Mohanan PP, Harikrishnan S, Sanjay G, et al. Prevalence of coronary artery disease and its risk factors in Kerala, South India: a community-based cross-sectional study. BMC Cardiovasc Disord. 2016;16:12. doi: 10.1186/s12872-016-0189-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Gupta R, Joshi P, Mohan V, Reddy KS, Yusuf S. Epidemiology and causation of coronary heart disease and stroke in India. Heart. 2008;94:16–26. doi: 10.1136/hrt.2007.132951. [DOI] [PubMed] [Google Scholar]
- [75].Bhardwaj R, Kandoria A, Marwah R, Vaidya P, Dhiman P, Singh B. Coronary heart disease in rural population of Himachal—a population based study. J Assoc Phys India. 2009;57:505–7. https://pubmed.ncbi.nlm.nih.gov/20329408/ [PubMed] [Google Scholar]
- [76].Rao M, Xavier D, Devi P, Sigamani A, Faruqui A, Gupta R, et al. Prevalence, treatments and outcomes of coronary artery disease in Indians: a systematic review. Indian Heart J. 2015;67:302–10. doi: 10.1016/j.ihj.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Goyal A, Kahlon P, Jain D, Soni RK, Gulati R, Chhabra ST, et al. Trend in prevalence of coronary artery disease and risk factors over two decades in rural Punjab. Heart Asia. 2017;9 doi: 10.1136/heartasia-2017-010938. e010938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Prabhakaran D, Jeemon P, Sharma M, Roth GA, Johnson C, Harikrishnan S, et al. The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990–2016. Lancet Glob Health. 2018;6:e1339–e51. doi: 10.1016/S2214-109X(18)30407-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Gupta R, Mohan I, Narula J. Trends in coronary heart disease epidemiology in India. Ann Glob Health. 2016;82:307–15. doi: 10.1016/j.aogh.2016.04.002. [DOI] [PubMed] [Google Scholar]
- [80].Sri Lanka. Institute for Health Metrics and Evaluation Available from: http://www.healthdata.org/sri-lanka.
- [81].Jayawardena JB, Samarutilake GD, Zackie MH, De Silva PV, Karunanayake A, Weerasooriya MA. Prevalence of coronary artery disease in a semi urban population in Southern Sri Lanka. Ceylon Med J. 2017;62:34–9. doi: 10.4038/cmj.v62i1.8432. [DOI] [PubMed] [Google Scholar]
- [82].Ralapanawa U, Kumarasiri PVR, Jayawickreme KP, Kumarihamy P, Wijeratne Y, Ekanayake M, et al. Epidemiology and risk factors of patients with types of acute coronary syndrome presenting to a tertiary care hospital in Sri Lanka. BMC Cardiovasc Disord. 2019;19:229. doi: 10.1186/s12872-019-1217-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Galappatthy P, Bataduwaarachchi VR, Ranasinghe P, Galappatthy GKS, Wijayabandara M, Warapitiya DS, et al. Management, characteristics and outcomes of patients with acute coronary syndrome in Sri Lanka. Heart. 2018;104:1424–31. doi: 10.1136/heartjnl-2017-312404. [DOI] [PubMed] [Google Scholar]
- [84].Tennakoon S, Kumar B, Nugegoda D, Meyer H. Comparison of cardiovascular risk factors between Sri Lankans living in Kandy and Oslo. BMC Public Health. 2010;10:654. doi: 10.1186/1471-2458-10-654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Mendis S, Ekanayakea EM. Prevalence of coronary heart disease and cardiovascular risk factors in middle aged males in a defined population in central Sri Lanka. Int J Cardiol. 1994;46:135–42. doi: 10.1016/0167-5273(94)90034-5. [DOI] [PubMed] [Google Scholar]
- [86].Mensah GA. Ischaemic heart disease in Africa. Heart. 2008;94:836–43. doi: 10.1136/hrt.2007.136523. [DOI] [PubMed] [Google Scholar]
- [87].Keates A, Mocumbi AO, Ntsekhe M, Sliwa K, Stewart S. Cardiovascular disease in Africa: epidemiological profile and challenges. Nat Rev Cardiol. 2017;14:273–93. doi: 10.1038/nrcardio.2017.19. [DOI] [PubMed] [Google Scholar]
- [88].Ayinde H, Gillum R. Cardiovascular disease mortality in sub-Saharan Africa and the Caribbean. Ethn Dis. 2014;24:495–501. https://pubmed.ncbi.nlm.nih.gov/25417435/ [PubMed] [Google Scholar]
- [89].Steyn K, Sliwa K, Hawken S, Commerford P, Onen C, Damasceno A, et al. Risk factors associated with myocardial infarction in Africa: the INTERHEART Africa study. Circulation. 2005;112:3554–61. doi: 10.1161/CIRCULATIONAHA.105.563452. [DOI] [PubMed] [Google Scholar]
- [90].Akinboboye O, Idris O, Akinkugbe O. Trends in coronary artery disease and associated risk factors in sub-Saharan Africans. J Hum Hypertens. 2003;17:381–7. doi: 10.1038/sj.jhh.1001562. [DOI] [PubMed] [Google Scholar]
- [91].Walker AR, Walker BF, Segal I. Some puzzling situations in the onset, occurrence and future of coronary heart disease in developed and developing populations, particularly such in sub-Saharan Africa. J R Soc Promot Health. 2004;124:40–6. doi: 10.1177/146642400312400112. [DOI] [PubMed] [Google Scholar]
- [92].Mensah GA. Public health: cardiovascular disease insights—something new out of Africa. Nat Rev Cardiol. 2013;10:433–4. doi: 10.1038/nrcardio.2013.96. [DOI] [PubMed] [Google Scholar]
- [93].Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- [94].Deckert A, Winkler V, Paltiel A, Razum O, Becher H. Time trends in cardiovascular disease mortality in Russia and Germany from 1980 to 2007 - are there migration effects? BMC Public Health. 2010;10:488. doi: 10.1186/1471-2458-10-488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [95].Nowbar A, Gitto M, Howard J, Francis D, Al-Lamee R. 112 Global and temporal trends in mortality from ischaemic heart disease: statistics from the World Health Organisation. Heart. 2019;105:A93. [Google Scholar]
- [96].Mensah GA, Brown DW. An overview of cardiovascular disease burden in the United States. Health Aff (Millwood) 2007;26:38–48. doi: 10.1377/hlthaff.26.1.38. [DOI] [PubMed] [Google Scholar]
- [97].Nowbar AN, Gitto M, Howard JP, Francis DP, Al-Lamee R. Mortality from ischemic heart disease. Circ Cardiovasc Qual Outcomes. 2019;12 doi: 10.1161/CIRCOUTCOMES.118.005375. e005375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Barstow C, Rice M, McDivitt JD. Acute coronary syndrome: diagnostic evaluation. Am Fam Physician. 2017;95:170–7. https://pubmed.ncbi.nlm.nih.gov/28145667/ [PubMed] [Google Scholar]
- [99].Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, et al. Executive summary: heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2010;121:948–54. doi: 10.1161/CIRCULATIONAHA.109.192666. [DOI] [PubMed] [Google Scholar]
- [101].Yoon SS, Dillon CF, Illoh K, Carroll M. Trends in the prevalence of coronary heart disease in the U.S.: National Health and Nutrition Examination Survey, 2001-2012. Am J Prev Med. 2016;51:437–45. doi: 10.1016/j.amepre.2016.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Bhatnagar P, Wickramasinghe K, Wilkins E, Townsend N. Trends in the epidemiology of cardiovascular disease in the UK. Heart. 2016;102:1945–52. doi: 10.1136/heartjnl-2016-309573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Andersen K, Aspelund T, Bandosz P. CVD mortality projections to 2020, comparing different policy scenarios. Euroheart II Work Package 6. European Heart Health II Strategy project; 2014. [Google Scholar]
- [104].Townsend N, Wilson L, Bhatnagar P, Wickramasinghe K, Rayner M, Nichols M. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J. 2016;37:3232–45. doi: 10.1093/eurheartj/ehw334. [DOI] [PubMed] [Google Scholar]
- [105].Ohira T, Iso H. Cardiovascular disease epidemiology in Asia: an overview. Circ J. 2013;77:1646–52. doi: 10.1253/circj.cj-13-0702. [DOI] [PubMed] [Google Scholar]
- [106].Hata J, Kiyohara Y. Epidemiology of stroke and coronary artery disease in Asia. Circ J. 2013;77:1923–32. doi: 10.1253/circj.cj-13-0786. [DOI] [PubMed] [Google Scholar]
- [107].Kita T. Coronary heart disease risk in Japan – an East/West divide? Eur Heart J Suppl. 2004;6:A8–A11. [Google Scholar]
- [108].Kitamura A, Sato S, Kiyama M, Imano H, Iso H, Okada T, et al. Trends in the incidence of coronary heart disease and stroke and their risk factors in Japan, 1964 to 2003: the Akita-Osaka study. J Am Coll Cardiol. 2008;52:71–9. doi: 10.1016/j.jacc.2008.02.075. [DOI] [PubMed] [Google Scholar]
- [109].Sekikawa A, Miyamoto Y, Miura K, Nishimura K, Willcox BJ, Masaki KH, et al. Continuous decline in mortality from coronary heart disease in Japan despite a continuous and marked rise in total cholesterol: Japanese experience after the Seven Countries Study. Int J Epidemiol. 2015;44:1614–24. doi: 10.1093/ije/dyv143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].Ogata S, Nishimura K, Guzman-Castillo M, Sumita Y, Nakai M, Nakao YM, et al. Explaining the decline in coronary heart disease mortality rates in Japan: contributions of changes in risk factors and evidence-based treatments between 1980 and 2012. Int J Cardiol. 2019;291:183–8. doi: 10.1016/j.ijcard.2019.02.022. [DOI] [PubMed] [Google Scholar]
- [111].Rumana N, Kita Y, Turin TC, Murakami Y, Sugihara H, Morita Y, et al. Trend of increase in the incidence of acute myocardial infarction in a Japanese population: Takashima AMI Registry, 1990-2001. Am J Epidemiol. 2008;167:1358–64. doi: 10.1093/aje/kwn064. [DOI] [PubMed] [Google Scholar]
- [112].Iso H. Changes in coronary heart disease risk among Japanese. Circulation. 2008;118:2725–9. doi: 10.1161/CIRCULATIONAHA.107.750117. [DOI] [PubMed] [Google Scholar]
- [113].Iso H. Lifestyle and cardiovascular disease in Japan. J Atheroscler Thromb. 2011;18:83–8. doi: 10.5551/jat.6866. [DOI] [PubMed] [Google Scholar]