Abstract
Introduction: Women with high-risk pregnancy are at increased risk of depression and anxiety during pregnancy, as well as a less favorable parent-infant interaction. This study aimed to investigate the effect of midwife-led psycho-education intervention on parental stress, competency, and postpartum depression in nulliparous women hospitalized with high-risk pregnancy.
Methods: This randomized controlled trial was carried out on 66 nulliparous women admitted to the high-risk pregnancy ward of Kamali Hospital, Karaj, Iran. Using convenient sampling method, the mothers were randomly assigned to control and intervention groups. In addition to routine care, the intervention group received four sessions of midwife-led psycho-education intervention in two group sessions in pregnancy and two individual sessions immediately after delivery. The parental stress, parental competency, and postpartum depression questionnaires were used for data collection before, after, and one month after the intervention. Data were analyzed using SPSS software ver. 13.0. Repeated-measures ANOVA test was used for comparing the mean scores of parenting stress, parental competency, and depression between and within both study groups before, after, and one month after delivery.
Results: While postpartum depression and parental stress decreased in intervention group, parental competency increased.
Conclusion: Our findings indicated that midwife-led psycho-education was effective on parental stress, competency, and postpartum depression in high-risk pregnancy mothers. Accordingly, prenatal distress in high-risk pregnancies should be assessed routinely.
Keywords: Stress disorders, Depression, Postpartum, High risk pregnancy, Parental competence
Introduction
Pregnancy is a physiologic event in the life of women. Although pregnancy is defined as an exciting period and a happy time, it is considered a stressful experience, and for a significant number of women, this stage is associated with anxiety and stress that can directly affect their mental health.1,2 Throughout the world, 20 million pregnant women (about 6-33%) are considered for high-risk pregnancies, which account for more than 800 deaths per day that is half of the pregnancy morbidity.3High-risk pregnant women are at risk of depression and stress during pregnancy.4 Hospitalization from days to weeks usually requires excessive control and care, and women with high-risk pregnancy are separated from the families with high levels of psychological stress and uncertainty about the health of the unborn child.5 High-risk pregnancy is extremely stressful due to limited physical activity within bed rest or hospitalization and limited housework for mothers.6 Increased complications, mortality, and morbidity due to anxiety and depression are among the most important concerns in high-risk pregnancies.7 Depression and anxiety during pregnancy are risk factors for postpartum depression. Prolonged and severe depression in the postpartum period affects maternal and infant attachment, breast feeding, and neonatal care, reducing mother’s response to neonatal needs, as well as any delay in the growth and development of the neonate.8 In a study, the prevalence of depression (29%) and postpartum anxiety (92.5%) in women with high-risk pregnancy were compared with depression (17%) and postpartum anxiety (79.5%) in women with low-risk pregnancy.9 Anxiety during pregnancy is associated with postpartum parental disorder behavior. Compared to postpartum, mental health during pregnancy is associated more with parental-neonatal interactions.10 The results of a study showed that, compared to parents with low-risk pregnancy, those who experience high-risk pregnancy show a less favorable parent-neonate interaction due to low sensitivity and adaptation to parental role.11 Education is an important part of pregnancy care for mothers admitted to hospital with pregnancy complications, and it can support early diagnosis and treatment of common symptoms of psychiatric disorders.7 Mothers with high-risk pregnancies speak with uncertainty about their health, pregnancy outcomes, and family responsibilities. Physicians and healthcare staff can assess and screen mental disorders and offer health education and care in the field of pregnancy and mental health, and thus improve the quality of care and pregnancy outcome.8,12 Midwife-led psycho-education is a type of intervention in the form of a brief counseling that does not require advanced psychotherapy and is provided by an obstetrician. According to reports, it has been effective in reducing stress and high levels of fear of birth, postpartum stress, cesarean section, and situational anxiety.
The results of a clinical trial showed the effect of education and telephone midwife-led psycho-education during pregnancy and after birth on the mental health of mothers in the 6 weeks of postpartum.13-15 Given the prevalence of high-risk pregnancies and the limited psychological studies on these vulnerable mothers,16 there is the need to assess the effect of psycho-education intervention on parental stress, competence, and postpartum depression of mothers with high-risk pregnancy. In the current randomized clinical trial, we educated the participants in two different time intervals (during pregnancy and during the postnatal period) to assess high-risk pregnancy, prenatal emotional distress, and later adaptation.
Materials and Methods
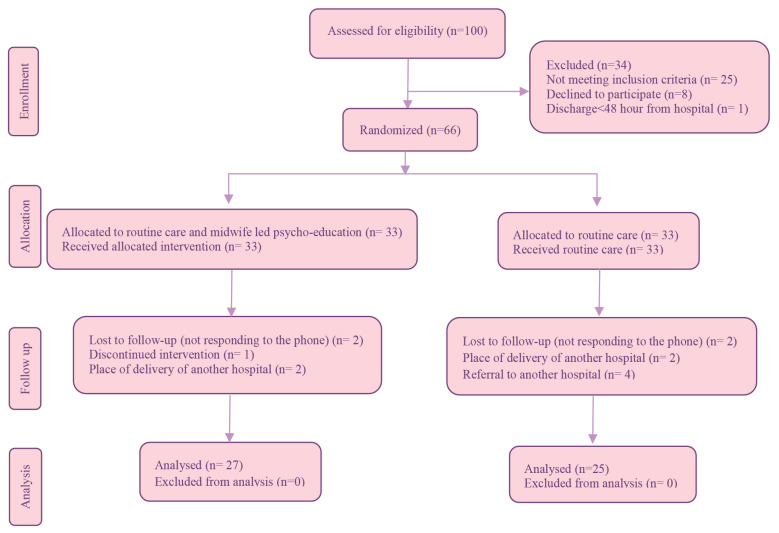
This was a randomized controlled trial study (IRCT20150119020719N10). The participants of this randomized controlled trial consisted of nulliparous mothers with high-risk pregnancy in the prenatal ward of Kamali Hospital in Karaj, Iran. This Hospital is a provincial referral center for mothers with high-risk pregnancy. The sample size in this study was based on the study carried out by Gao LL et al.,17 using the formula for comparing two means with type-1 error of 0.5%, power of 0.8 and also ( M1=33.66, SD1=6.12) and (M2=36.06, SD2=4.41) was considered. Thirty three individuals were selected for each group. Figure 1 shows the study algorithm.
Figure 1.
Flow chart of study
The inclusion criteria were being nulliparous, having the gestational age of 34 weeks and higher based on the last menstrual period or first sonography screening, being literate, being Iranian, being diagnosed with high-risk pregnancy, staying for at least three days in the prenatal ward of Kamali Hospital. Woman with lack of attendance to one group session, having a history of mental disorders, having a baby with physical and mental abnormalities, and place of delivery outside Kamali Hospital were excluded from this investigation. The researcher who conducted the midwife-led psycho-education program was a trained MSc student of Counselling in Midwifery.
The sampling method was convenient and the samples were randomly assigned to two groups of received counseling (intervention) and non-received counseling (control) by four-sized randomized blocks. There were six possibilities for inclusion in blocks (BABA, BBAA, ABBA, AABB, ABAB and BAAB). At the beginning of study, one of blocks was selected and four participants were put in that block, so that the number A belonged to the intervention group, and number B to the control group. The details of blocks were contained in asset of sealed envelopes; the person that did allocation did not have any information about research.
Before the onset of intervention, Parenting Stress Index-Short Form (PSI-SF), Edinburg Post-Natal Depression Scale (EPDS), and Parenting Sense of Competency (PSOC) questionnaires were completed in both groups. The intervention group received midwife-led psycho-education in 2 sessions for a period of approximately 60-90 minutes in addition to slides, booklets, and group discussions during admission to high-risk pregnancy ward. They were then followed up by telephone until delivery, alongside two individual training sessions for approximately 60 minutes immediately after the delivery. PSOC consists of a parental competence and satisfaction, and is a 17-item instrument on the 6-point Likert scale (from absolutely agree to absolutely disagree). The range of scores is 17-102, in which a higher score indicates a higher level of parental sense of competence. The reliability and validity of the scale were determined by Johnston and Mash.18 In Iran, the psychometry of the questionnaire was determined by Abdollahpour et al.19
The EPDS consists of 10 items with a 4-point Likert scale. The score is generally between 0-30. The highest score indicates negative emotions.The reliability of the Iranian version of this instrument was determined through test re-test (0.8), and the Cronbach’s alpha value was 0.77.20
The PSI-SF is a short version of 36 items with a 5-point Likert scale developed by Abidin & Brunner in 1995. Higher scores indicate higher stress levels.21 In Iran, the reliability of this instrument was obtained as 0.84 through test re-test and internal consistency coefficient for total stress and the alpha values for total stress index was 0.90.22
The content of 4 sessions of education was determined based on Fenwick et al., and Gamble et al.,15,23 confirmed by the faculty members of the Midwifery, Psychology, and Pediatric Faculty of Alborz University of Medical Sciences. At the end of each training session, the researcher obtained feedback from mothers.
The content of the first session, which was presented in person and in the form of group training over a period of approximately 60-90 minutes, included showing kindness, providing descriptions of the goals of the study, simple and open questions about birth, actively listening, encouraging expression of concern, identifying and responding to individual conflicts, teaching problem-solving skills, training and improving communication skills required for child care, the way the baby grows up, talking in the mother role, the provision of information for the participants to accept the mother role, attempts to remove preventive barriers to communication with the neonate, postpartum depression symptoms, facilitating barriers to communicate with the neonate, and educating them to adopt strategies for decreasing stress.
The second session, immediately after the first session, included reviewing previous session and assignments with a check list, providing information on the development of social support, discussion about exiting support network, talking about ways to receive additional emotional support, teaching problem-solving skills, asking about anything that should have been done differently during labor, teaching respiratory techniques, postpartum exercise, and strategies for focusing and reducing stress.
The third session was individual training held immediately after delivery, and included reviewing previous session and training respiratory techniques, training postpartum exercises, teaching strategies for reducing stress, the way the baby grows up, talking about motherhood transition, the provision of information to adapt the mother, attempts to remove preventive barriers to communicate with the neonate, facilitating barriers to communicate with the neonate, teaching how to cope with postpartum depression symptoms, teaching breast feeding, and problems that mothers usually encounter.
The fourth session was conducted on an individual basis and involved advice on the problems that occurred after birth, concerns raised with respect to the mother’s role, the emphasis on the support of their relatives for up to 10 days after childbirth training, improving communication skills with the spouse after the birth the baby, and repeating the respiration and relaxation technique.
At the end of intervention sessions, to observe the ethical considerations, an educational booklet was given to the control group, too. In the intervention and control groups, PSI-SF, EPDS, and PSOC questionnaires were completed simultaneously before the education, after the discharge from hospital, and one month after delivery.
Data were analyzed using SPSS software Ver.13.0 (SPSS Inc., Chicago, IL, USA). Normality of the data was also investigated via Kolmogorov-Smirnov test. T-test was correspondingly employed to compare baseline quantitative variables between the two study groups. The comparison of qualitative variables was also performed using chi-square test and Fisher’s exact test. To compare the mean scores of parenting stress, competency, and depression between both study groups before, after, and one month after delivery, repeated-measures ANOVA test was used. P-value less than 0.05 was considered significant. Data analysis was carried out based on per-protocol analysis.
Results
Table 1 shows the demographic characteristics of nulliparous mothers with high-risk pregnancy. There was not significant difference between the demographic characteristics in the control and intervention group.
Table 1. Demographic characteristic of mothers with high risk pregnancy .
| Variable | Intervention | Control | P-Value |
| N (%) | N (%) | ||
| The cause of high risk pregnancy | |||
| Preeclampsia | 8(24.24) | 7(21.21) | -¥ |
| Gestational diabetes mellitus | 7(21.21) | 6(18.18) | |
| Pre-term labor | 5(15.16) | 3(9.09) | |
| Vaginal bleeding | 4(12.12) | 5(15.16) | |
| Varicella | 4(12.12) | 0(0.00) | |
| Thrombocytopenia | 2(6.06) | 0(0.00) | |
| Oligohydramnios | 1(3.03) | 7(21.21) | |
| Pre mature rupture of membrane | 1(3.03) | 2(6.06) | |
| Pyelonephritis | 1(3.03) | 2(6.06) | |
| Intra uterine growth deficiency | 0(0.00) | 1(3.03) | |
| Mother's Job | -¥ | ||
| Housewife | 30(90.9) | 31(93.9) | |
| Employee | 2(6.1) | 2(6.1) | |
| Others | 1(3.0) | 0(0.00) | |
| Type of delivery | ᵪ2= 1.06 0.80£ |
||
| Natural childbirth | 16(48.5) | 17(51.5) | |
| Cesarean section | 17(51.5) | 16(48.5) | |
| Level of education | ᵪ2= 0.542 0.33£ |
||
| Elementary | 16(48.5) | 17(51.5) | |
| Diploma | 7(21.2) | 10(30.3) | |
| University | 10(30.3) | 6(18.2) | |
| Baby sex | ᵪ2=0.06 0.62£ |
||
| Girl | 16(48.5) | 18(54.5) | |
| Boy | 17(51.5) | 15(45.5) | |
| Intention to pregnancy | F=1.07 0.72€ |
||
| Wanted | 29(87.9) | 28(84.8) | |
| Unwanted | 4(12.1) | 5(15.2) | |
| Economic | -¥ | ||
| Poor | 6(18.2) | 6(18.2) | |
| Moderate | 25(75.8) | 26(78.8) | |
| Good | 2(6) | 1(3.0) | |
| Excellent | 0(0.00) | 0(0.00) | |
| Abortion history | ᵪ2=0.85 0.59£ |
||
| Yes | 11(33.3) | 9(27.3) | |
| No | 22(66.7) | 24(72.7) | |
| Hospitalization of infant | ᵪ2=0.44 0.49£ |
||
| Yes | 6(18.2) | 4(12.1) | |
| No | 27(81.8) | 29(87.9) | |
¥Statistical calculation was not possible due to low frequency;£Chi-square test;€Fisher test
The results of repeated-measures ANOVA showed that the variable of paternal stress had a significant change over time in the counselling group (P<0.001) and there was a significant difference between the two groups (P<0.001). Therefore, midwife-led psycho-education had a significant effect on parental stress in the intervention group (Table 2).
Table 2. Parental stress, postpartum depression, and maternal sense of competency in women with high-risk pregnancy .
| Variable |
Before
Mean (SD) |
After
Mean (SD) |
One month after
Mean (SD) |
Repeated measure | |
| P (Within group) | P (Between group) | ||||
| Parental stress | |||||
| Intervention | 68.12 (12.16) | 52.22 (8.53) | 47.00 (11.51) | F=37.46, P<0.001* | F=1319.9, P<0.001* |
| Control | 67.09 (15.90) | 72.78 (13.82) | 58.84 (8.59) | F=39.41, P<0.001* | |
| Postpartum depression | |||||
| Intervention | 10.96 (5.78) | 10.64 (5.83) | 8.33 (4.70) | F=2.7033, P<0.001* | F=79.91, P<0.001* |
| Control | 12.12 (6.39) | 12.60 (5.78) | 14.16 (5.51) | F=3.642, P<0.07 | |
| parental competency | |||||
| Intervention | 71.15 (19.9) | 82.35 (8.68) | 89.70(11.27) | F=13.7, P<0.001* | F=2022.4, P<0.001* |
| Control | 69.82 (9.36) | 75.03 (9.67) | 83.12 (8.73) | F=12.6, P<0.001* | |
*Statistically significant
Moreover, the variable of postpartum depression had a significant change over time in the intervention group (P<0.001) and there was a significant difference between the two groups (P<0.001). Therefore, midwife-led psycho-education had a significant effect on postpartum depression in the intervention group (Table 2).
Furthermore, the variable of parental competence had a significant change over time in the intervention group (P<0.001) and there was a significant difference between the two groups (P<0.001). Therefore, midwife-led psycho-education had a significant effect on parental competence in the intervention group (Table 2).
Discussion
The results of the current study showed midwife-led psycho- education had a significant effect on parental stress, postpartum depression and parental competency in high risk pregnancy women. Midwife-led psycho- education had effect on reduction parental stress in intervention group. In a prospective study, the prevalence and severity of anxiety among 310 mothers admitted to a high-risk pregnancy ward in Vancouver in the second trimester to 6 months postpartum was reported to be between 13% and 21% in the pregnancy, and 11% to 17% after delivery.24 In another study on 62 mothers admitted to high-risk pregnancy ward, 27% of women experienced depression symptoms, 13% experienced symptoms of anxiety, and 77% of them reported that group psychological education was very helpful in treating them. Only 5% of women received treatment for their depression during pregnancy.6 Another study showed that group education of nulliparous women with high-risk pregnancy reduced their anxiety, which is consistent with our findings. Group training increases self-confidence, improves mental status, and creates a friendly and intimate environment for more communication and expression of their experiences.16 In a systematic study on prenatal stress and anxiety in women with a history of high-risk pregnancy, it was reported that anxiety and perinatal depression significantly increased the risk of postpartum depression in women high-risk pregnancy women.25
The results of this study indicated the effect of midwife-led psycho-education intervention on postpartum depression. The results of a study on the effect of prenatal psychological training on postpartum depression and the increasing satisfaction of couples showed the positive impact of psychological education.26 Moreover, in another study, the effect of relaxation on the depression score in women with high-risk pregnancy in hospitals was highlighted.4 The results of these studies were consistent with those of the current study.
The results of qualitative studies in explaining the life experiences of mothers with high-risk pregnancy for more than three days in hospital showed the need for support as the most important factor. Also, educating patients for their needs and raising awareness about the stressors in the long-term hospitalization period within pregnancy could help mothers improve their self-confidence to seek better care.5,27
The results of repeated-measures ANOVA showed the effect of time on the score of parental competence in both the intervention and control groups. Over time, parental competency increased in the two groups, but this increase was higher in the intervention group. The reason for increasing parental competence in the control group could be the transition of time and adaption to motherhood role in the two groups. In a longitudinal study, the effect of high-risk pregnancy and parental stress during pregnancy was measured and parental competency was measured in the first days after birth; high-risk pregnant mothers experienced more stress, less sense of competency, and less satisfaction, and the adaption to the motherhood role in high-risk pregnancy was considered difficult and problematic.11 In another study of women with high-risk and low-risk pregnancies, the level of postpartum fear was associated with concerns about maternal role, and there was a significant relationship between depression and attachment, with depressed women showing less attachment to their child.28,29 These results did not agree with those of the current study, because parental competency was measured during the first days after birth in that study, but in the current study, we measured parental competency one month after birth, and time transition might have affected motherhood role adaption. The results of studies showed that mindfulness-based interventions were effective in enhancing maternal roles in nulliparous women. Most nulliparous women often lack parental competence to play a role in motherhood, most of which is due to the lack of experience.30-32 The results of that study was consistent with those of the current study. Parental competency requires psychological and emotional preparation. The need for support on the part of the spouse is one of the most important issues in high-risk pregnancies.11
This study educated the participants in two different time intervals (during pregnancy and after delivery); moreover, we followed the mothers from high-risk pregnancy ward to delivery room and postpartum ward. The main limitation of the current study was the participation of mothers with high-risk pregnancies with a gestational age of 34 weeks or higher delivered in hospital during hospitalization in high-risk pregnancy ward. It is recommended that a longitudinal study be conducted on mothers with lower gestational age. Another limitation was that only mothers with high-risk pregnancy participated in this study; thus, it is suggested that further studies investigate the effect of education on high-risk pregnancies, with the fathers involved in the educational program. In this study, we held four sessions of training in the period of pregnancy and two postpartum sessions. Accordingly, it is suggested that a study with more educational sessions be designed in the long time and at least 3 months after delivery in high-risk pregnant mothers.
Conclusion
The findings of current study indicated that midwife-led psycho-education was effective on stress, competency, and postpartum depression in high-risk pregnancy mothers. It is suggested that prenatal distress be assessed routinely, and especially if high-risk pregnancies are diagnosed. Furthermore, midwife-led psycho-education should be offered to distressed mothers during the perinatal and postpartum period. Trained health care providers should be available for mothers who experience high-risk pregnancy.
Acknowledgments
The authors wish to thank the Clinical Research Development Center of Kamali Hospital in Alborz Province for collaboration to carry out this study and deputy of research and technology of Alborz University of Medical Sciences for financial support.
Ethical Issues
This study was approved by the Research Deputy of Alborz University of Medical Sciences and approved by the ethics committee of Alborz University of Medical Sciences (Code: Abzums.Rec.1396.215). Moreover, it was recorded in the Iranian Clinical Trial Center (No: IRCT20150119020719N10). All participants signed informed consent forms and the researcher considered all the material and moral rights of the research subjects.
Conflict of Interest
The authors state that there is no conflict of interests in this research.
Author’s Contributions
SES: is supervision, designed and performed the study; LC: is student that performed the studies and intervention; MA: designed and consulted about the educational program for high risk pregnant counselling; MAK: consulted about content of educational program and data analysis.
Research Highlights
What is the current knowledge?
High risk pregnant women are at risk of depression and stress during pregnancy.
What is new here?
Midwife-led psycho-education was effective on parental stress, competency and postpartum depression in high risk pregnancy mothers.
References
- 1.Araújo WS, Romero WG, Zandonade E, Amorim MH. Effects of relaxation on depression levels in women with high-risk pregnancies: a randomised clinical trial. Rev Lat Am Enfermagem. 2016;24(1):2806. doi: 10.1590/1518-8345.1249.2806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zelkowitz P, Papageorgiou A. Easing maternal anxiety: an update. Womens Health. 2012;8(2):205–13. doi: 10.2217/whe.11.96. [DOI] [PubMed] [Google Scholar]
- 3.Holness N. High-risk pregnancy. Nurs Clin North Am. 2018;53(2):241–51. doi: 10.1016/j.cnur.2018.01.010. [DOI] [PubMed] [Google Scholar]
- 4.Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry. 2012;25(2):141–8. doi: 10.1097/FYCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kent RA, Yazbek M, Heyns T, Coetzee I. The support needs of high-risk antenatal patients in prolonged hospitalization. Midwifery. 2015;31(1):164–9. doi: 10.1016/j.midw.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Byatt N, Hicks Courant K, Davidson A, Levesque R, Mick E, Allison J. et al. Depression and anxiety among high-risk obstetric inpatients. Gen Hosp Psychiatry. 2014;36(6):644–9. doi: 10.1016/j.genhosppsych.2014.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kendig S, Keats JP, Hoffman MC, Kay LB, Miller ES, Simas TAM. et al. Consensus bundle on maternal mental health: perinatal depression and anxiety. J Obstet Gynecol Neonatal Nurs. 2017;46(2):272–81. doi: 10.1016/j.jogn.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Harris AL. Barriers to and facilitators of perinatal depression screening. Nurs Womens Health. 2017;20(6):601–7. doi: 10.1016/j.nwh.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Akbar Zadeh M, Khajehei M, Sharif F, Hadzic M. High-risk pregnancy: effects on postpartum depression and anxiety. Br J Midwifery. 2012;20(2):104–13. doi: 10.12968/bjom.2012.20.2.104. [DOI] [Google Scholar]
- 10.Parfitt Y, Pike A, Ayers S. The impact of parents’ mental health on parent–baby interaction: A prospective study. Infant Behav Dev. 2013;36(4):599–608. doi: 10.1016/j.infbeh.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 11.Dollberg DG, Rozenfeld T, Kupfermincz M. Early parental adaptation, prenatal distress, and high-risk pregnancy. J Pediatr Psychol. 2016;41(8):915–29. doi: 10.1093/jpepsy/jsw028. [DOI] [PubMed] [Google Scholar]
- 12. Panella H. Development of an educational video on perinatal depression and anxiety for women hospitalized with high-risk pregnancies [master’s thesis]. Davis: University of California; 2018.
- 13.Toohill J, Callander E, Gamble J, Creedy D, Fenwick J. A cost effectiveness analysis of midwife psycho-education for fearful pregnant women–a health system perspective for the antenatal period. BMC Pregnancy Childbirth. 2017;17(1):217. doi: 10.1186/s12884-017-1404-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Serçekuş P, Başkale H. Effects of antenatal education on fear of childbirth, maternal self-efficacy and parental attachment. Midwifery. 2016;34:166–72. doi: 10.1016/j.midw.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 15.Fenwick J, Toohill J, Gamble J, Creedy DK, Buist A, Turkstra E. et al. Effects of a midwife psycho-education intervention to reduce childbirth fear on women’s birth outcomes and postpartum psychological wellbeing. BMC Pregnancy Childbirth. 2015;15(1):284. doi: 10.1186/s12884-015-0721-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rahimi F, Islami F, Kahangi MM. Effects of prenatal education on maternal and neonatal outcomes in high risk pregnant women. Pajouhan Scientific Journal. 2018;16(3):48–57. (Persian) [Google Scholar]
- 17.Gao LL, Sun K, Chan SW. Social support and parenting self-efficacy among Chinese women in the perinatal period. Midwifery. 2014;30(5):532–8. doi: 10.1016/j.midw.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 18.Johnston C, Mash EJ. A measure of parenting satisfaction and efficacy. J Clin Child Psychol. 1989;18(2):167–75. doi: 10.1207/s15374424jccp1802_8. [DOI] [Google Scholar]
- 19.Abdollahpour N, Seyedfatemi N, Shooshtari MH, Mehran A.. The effect of education on sense of competence of mothers of children with hyperactivity disorder. Iranian Journal of Psychiatic Nursing. 2017;5(4):19–26. (Persian) [Google Scholar]
- 20.Montazeri A, Torkan B, Omidvari S. The edinburgh postnatal depression scale (EPDS): translation and validation study of the Iranian version. BMC Psychiatry. 2007;7(1):11. doi: 10.1186/1471-244X-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abidin RR, Brunner JF. Development of a parenting alliance inventory. Journal of Clinical Child Psychology. 1995;24(1):31–40. doi: 10.1207/s15374424jccp2401_4. [DOI] [Google Scholar]
- 22.Fadaei Z, Dehghani M, Tahmasian K, Farhadei M. Investigating reliability, validity and factor structure of parenting stress-short form in mothers of 7-12 year-old children. Journal of Research in Behavioural Sciences. 2010;8(2):81–91. (Persian) [Google Scholar]
- 23.Gamble J, Creedy D, Moyle W, Webster J, McAllister M, Dickson P. Effectiveness of a counseling intervention after a traumatic childbirth: a randomized controlled trial. Birth. 2005;32(1):11–9. doi: 10.1111/j.0730-7659.2005.00340.x. [DOI] [PubMed] [Google Scholar]
- 24.Fairbrother N, Young AH, Janssen P, Antony MM, Tucker E. Depression and anxiety during the perinatal period. BMC Psychiatry. 2015;15(1):206. doi: 10.1186/s12888-015-0526-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kingston D, Tough S, Whitfield H. Prenatal and postpartum maternal psychological distress and infant development: a systematic review. Child Psychiatry Hum Dev. 2012;43(5):683–714. doi: 10.1007/s10578-012-0291-4. [DOI] [PubMed] [Google Scholar]
- 26.Moosavi Sahib S, Fathi Ashtiani A, Ahmadi A, Shafi Y, Alimadadi Z, Sedghi Taromi A. Effect of antenatal psychological education to reduce postpartum depression and improve marital satisfaction: a randomized controlled trial in first time mothers referred to Baghatalah and Najmiyeh hospitals, 2013. Nursing and Midwifery Journal. 2016;13(10):892–902. (Persian) [Google Scholar]
- 27.Rubarth LB, Schoening AM, Cosimano A, Sandhurst H. Women’s experience of hospitalized bed rest during high‐risk pregnancy. J Obstet Gynecol Neonatal Nurs. 2012;41(3):398–407. doi: 10.1111/j.1552-6909.2012.01349.x. [DOI] [PubMed] [Google Scholar]
- 28.Koss J, Bidzan M, Smutek J, Bidzan L. Influence of perinatal depression on labor-associated fear and emotional attachment to the child in high-risk pregnancies and the first days after delivery. Med Sci Monit. 2016;22:1028–37. doi: 10.12659/MSM.895410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zdolska-Wawrzkiewicz A, Bidzan M, Chrzan-Dętkoś M, Pizuńska D. The dynamics of becoming a mother during pregnancy and after childbirth. Int J Environ Res Public Health. 2019;17(1):57. doi: 10.3390/ijerph17010057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coatsworth JD, Duncan LG, Nix RL, Greenberg MT, Gayles JG, Bamberger KT. et al. Integrating mindfulness with parent training: effects of the mindfulness-enhanced strengthening families program. Dev Psychol. 2015;51(1):26–35. doi: 10.1037/a0038212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miller KE, Ghalayini H, Arnous M, Tossyeh F, Chen A, van den Broek M. et al. Strengthening parenting in conflict-affected communities: development of the caregiver support intervention. Glob Ment Health (Camb) 2020;7:e14. doi: 10.1017/gmh.2020.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Han ZR, Ahemaitijiang N, Yan J, Hu X, Parent J, Dale C. et al. Parent mindfulness, parenting, and child psychopathology in China. Mindfulness. 2021;12:334–43. doi: 10.1007/s12671-019-01111-z. [DOI] [Google Scholar]